Purpose of review
Established social gradients across a wide range of child health issues including obesity, anxiety, infectious diseases, injuries, prematurity and low birth weight suggest that much illness is avoidable and there is an imperative to intervene in this whole of society issue. This review examines recent advances in understanding of the pathways to health and health inequalities and their application to interventions to improve health equity.
Recent findings
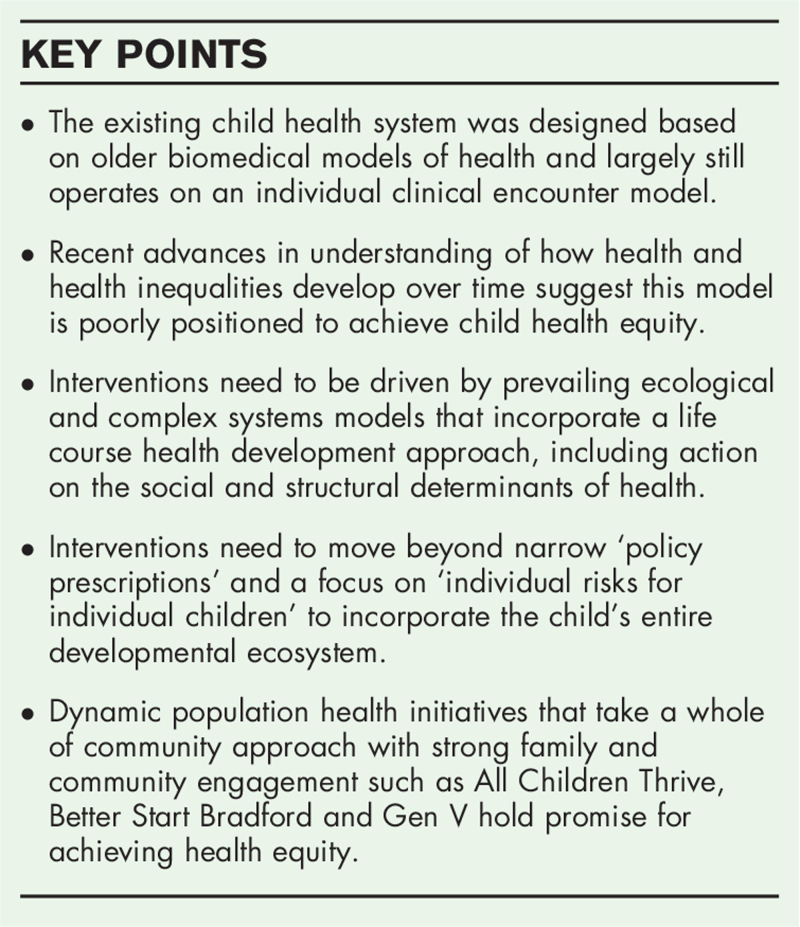
Children's health develops over the life course in ways that are profoundly influenced by their entire developmental ecosystem including individual, family, community and system-level factors. Interventions to address child health inequalities must include action on the structural determinants of health, a greater focus on family and community health development, and attention to the acquisition of developmental capabilities. Nascent dynamic population health initiatives that address whole developmental ecosystems such as All Children Thrive, Better Start Bradford and Generation V, hold real promise for achieving child health equity.
Summary
Pathways to health inequalities are driven by social and structural determinants of health. Interventions to address inequalities need to be driven less by older biomedical models, and more by prevailing ecological and complex systems models incorporating a life course health development approach.
Keywords: capabilities, child health, health inequalities, intervention, life course
INTRODUCTION
Children living in disadvantaged or marginalized circumstances have worse physical and mental health than their more advantaged peers [1▪▪,2–4]. This relationship holds true for conditions ranging from obesity to anxiety, infectious diseases to low birthweight [5]. There is an established social gradient in health from the bottom to the top of the socio-economic spectrum making this a societal issue [6]. Guided by a deeper understanding of the complex, multilayered, inter-connected pathways linking socioeconomic circumstances and child health [1▪▪], interventions need to disrupt suboptimal pathways to create more equitable health trajectories. In this paper, we review recent advances in models of health and health inequality and their implications for health equity interventions, considering the need for dynamic population health interventions based on a life course health development (LCHD) approach [7].
Box 1.
no caption available
MODELS OF HEALTH
For much of human history, children's healthcare focused more on surviving than thriving- if children could survive the perils of birth and infectious diseases, it was thought, they would be ‘healthy’ through to the declines of old age. Broad public health measures including improved sanitation, coupled with safety-net programs for the poor dramatically improved infant mortality and the probability of surviving to adulthood [8] at the start of the last century.
Biomedical models
Biomedical models of health and disease initially took a reductionist, linear view of acute and chronic illness, searching primarily for single-cause, single-disease associations that emphasized physical health over mental health or social-emotional well-being. Interventions focused on surgical treatments and pharmaceuticals. Our children's healthcare system was designed and largely still operates on, this individual clinical encounter model[9,10], focused on discrete treatments for discrete conditions. Providers can attempt to address specific social needs [11] relevant to a presenting problem, e.g., advocating for family housing relocation for a child with chronic respiratory problems who is living in a home with damp or mold, or referring to a food bank if there is household food insecurity, but there is little opportunity to consider and address other interrelated risk and protective factors in that child's broader ecosystem.
Biopsychosocial models and the social determinants of health
Gradually, more holistic, multilevel and dynamic biopsychosocial models of health [12] emerged demonstrating how social circumstances and health might influence each other in nonlinear, adaptive (and maladaptive) ways. Bronfenbrenner's Ecological Model of Human Development provided an organizing framework for influences on human development, the most proximal being child and family factors, followed by school and community factors, and finally the larger social, cultural and policy systems. Several models have proposed a similar ecological framework for the factors influencing child health [13,14]. The conditions in which children are born, grow up, work, and live – the social determinants of health – are now understood to be major drivers of children's health trajectories, that interact with the child and with each other both within and across ecological layers in complex ways. Not just one or two, but all of these factors impact a child's health.
Life course health development model
The LCHD approach attempts to improve on the biopsychosocial model, incorporating recent principles from a range of life course sciences including life course sociology, life span developmental psychology, chronic disease epidemiology and epigenetics. It integrates the developmental orientation of Bronfenbrenner's Ecological Model of Human Development into a more robust explanatory model regarding human health development that has major implications for pediatric practice [15▪▪]. Health is regarded as an emergent, dynamic and developmental characteristic resulting from complex adaptive relational interactions between biology, behaviors, and social ecological conditions [16–18]. Although the magnitude and later mutability of early effects are debated, some time frames, many in the prenatal, postnatal and early years, appear critical for healthy development and adaptation, and key to improving health. Humans are designed to adapt to circumstances purposefully and continuously and the ecosystems into which children are born are also continuously adapting and changing. Aligning all these systems in ways that support health development will foster good outcomes [19]. If they are misaligned, or ‘health diminishing’ then sub-optimal health trajectories may become established in childhood and worsen during adult life. For example, adverse childhood experiences (ACEs) have strong associations with alterations in structural mid-life brain integrity [20▪], whereas increasing breastfeeding duration could flatten the social gradient in adult chronic inflammation by as much as 80% [21▪].
MODELS OF HEALTH INEQUALITY
Researchers draw a distinction between the social determinants of health and the social determinants of health inequalities[1▪▪,22], rightly arguing that overall improvements to population health do not necessarily lead to greater health equity. In considering pathways to health inequalities, Diderichson proposes differential power and resources, exposures, vulnerabilities and consequences of being sick as four main mechanisms [23]. Similarly, Pearce et al. distinguish between four major factors:
Material: social advantage confers greater access to healthy living conditions, such as a safe, uncrowded home with access to a garden or green space, warm clothing and footwear, and nutritious foods.
Psychosocial: social inequality produces feelings of subordination and lack of control influencing neuroendocrine pathways.
Behavioral: inequalities in parent and adolescent health behaviors, including smoking and physical activity, exhibit social gradients leading to later health inequalities.
Structural: these are outer layers of Bronfenbrenner's model such as access to healthcare and childcare, the system of taxes and benefits, ‘classism’ and structural racism that many theorists regard as the ‘root cause” of health inequalities [24].
The LCHD Model adds considerations of time and health development to understanding pathways to health inequalities [25,26]. Inequalities in family living conditions, psychosocial health, stability and health behaviors prior to conception, during pregnancy and in the early years have implications for life-long health. These early inequalities may be potent drivers of an unequal ability to acquire key developmental capacities or capabilities that support children's healthy adaptation to their early environments and also buffer against future adversity. The unequal acquisition of these capacities may be driving much of the observed later-life health inequalities.
IMPLICATIONS FOR INTERVENTIONS
Models of health and health inequality provide an analytic framework for understanding and potentially disrupting sub-optimal pathways between social circumstances and poorer health. They inform intervention design [27] and research priorities.
The challenges of addressing the structural determinants of health
Acting on the structural determinants of health to produce a fairer, more equitable society and reduce childhood illness and mortality is a public health priority. The difficulty comes in designing policies to achieve this. Social determinants of health might be best represented as a three-dimensional system of interlocking microsystems, i.e., a complex adaptive system of systems[28▪▪,29,30]. These systems are not linear, with simple cause and effect paradigms, but complex and adaptive [31], multilayered and reciprocal, with bi- and multidirectional forces all affecting the whole. Simple policy changes that ignore the need for a systems approach, that fail to address the complexity and inter-relatedness of these systems or that fail to address the relevance of newer theories like critical race theory [32] may have unanticipated, even counter-intuitive effects, and fail to bring about improvements. Advocates are calling for a shift from health policy to health public policy, where the impact of policies on well-being is a key consideration across government sectors [33▪,34].
Multilevel interventions and the inverse evidence law
Interventions with components that impact the first order microsystem (direct effect on the child and family), second-order mesosystem (operate through schools, community or neighborhood services) and the third-order macrosystem (cultural, policy and social systems) are more likely to impact health inequalities than isolated policy changes or programs addressing only proximal risks e.g., maternal depression. More research on second and third-order interventions would address the existing evidence base imbalance, with its focus on proximal interventions [1▪▪].
Life Course interventions
The Life Course Intervention Research Network, https://lcirn.ucla.edu is a collaborative network of researchers, service providers, family and community representatives and thought leaders committed to improving life course trajectories and outcomes for children. The group is working to apply the seven principles of life course health development: health development, unfolding, complexity, timing, plasticity and harmony to interventions in ways that will also reduce health disparities [35,36]. This will include more integrated, networked strategies for developing and implementing multi-level interventions that transcend divisions between individual and population health. Multigenerational interventions [37], that acknowledge community history and structural constraints, and build on intergenerational strengths could provide new opportunities to address factors such as intergenerational trauma and improve the health status of children and grandchildren.
Interventions that address emerging health development capabilities
The developing child is an active participant in a dynamic relational process during which capabilities [38,39], e.g., the capacity to regulate one's emotions, to make meaningful social connections, to become a lifelong learner, develop over time. Just as individual developmental stages and health development are important to the health of the individual, so too are family stages and family health development along with community health development, each with an attendant set of capabilities that need to be acquired. Interventions to address family and community capabilities, so that these components of a child's ecosystem will be maximally health giving, is an area ripe for research.
Dynamic population health interventions
Although these types of interventions are not yet the norm, nascent programs are attempting to put these principles into practice.
All Children Thrive (ACT) is a dynamic population health initiative focused on building a movement within and between communities working to optimize children's health and well-being. ACT Cincinnati, launched in 2015 (https://www.actnowcincy.org/) pioneered this approach, focusing on selected outcomes, e.g., thriving at kindergarten entry and reducing healthcare inequities. Consistent with LCIR principles, key elements of the approach include a focus on the whole population, building equity into measures, and co-designing with families and users. Given the need for emergent, adaptive, multilevel interventions, progress is driven by theory-based testing and learning rather than the implementation and spreading of predesigned programs. The Model for Improvement [40] is at the core of moving the ‘ecosystem’ of partners toward results [41]. Scale-up is driven in part by identifying systems issues at the root of individual poor outcomes. In one neighborhood in which the extreme prematurity rate was high for many years, the portfolio of interventions resulted in three years without a single extreme premature birth. Using similar strategies, the children's hospital achieved a 20% reduction in admissions [42]. ACT Cincinnati has developed practices for pursuing equity through its learning health system including: measuring for equity; leading from lived experience; co-producing interventions; redistributing power; practicing a growth mindset; and engaging beyond the healthcare system to catalyze change [43].
This success inspired the city of Long Beach to launch a similar program (ACT Long Beach) (https://www.lbunplug.org/) followed by the 2019 launch of the ACT California (https://act-ca.org/) pilot program which by December 2021 will reach 18 cities. This equity-focused, community-driven ‘whole ecosystem’ initiative aims to develop, test and refine the tools that support diverse communities in preventing and healing ACEs and to promote child and family well-being. Strategies include:
-
(1)
Engaging and activating ACT cities to implement evidence-based policies and practices to improve child well-being.
-
(2)
Helping cities employ user-centered design, networked improvements, and rapid cycle innovation and improvement strategies to achieve priority outcomes.
-
(3)
Building capacity to implement systems improvements including creating permanent city-level leadership on child well-being, and
-
(4)
Monitoring key measures of child development and well-being.
Better Start Bradford (www.betterstartbradford.org.uk), launched in 2015, incorporates over 20 interventions within the context of the Born in Bradford longitudinal cohort study (https://borninbradford.nhs.uk) designed to improve children's healthy development [44]. These interventions target developmental capabilities including social emotional development, communication and language development and healthy nutrition, embracing a complex systems approach in a community-wide learning system. Considering the dynamic complexity of the social and environmental determinants of health the study links research and administrative data on parents and family, their genes, economic circumstances, the way families live, the environment, and services with a focus not just on observation but on change and community empowerment [44,45▪▪].
The even more ambitious Generation Victoria (Gen V) (https://genv.org.au/) will integrate intervention research within or alongside a whole-state Australian birth cohort study [46]. This prospective study targets all expected 150,000 newborns and their parents over two years starting late 2021 and provides an opportunity to study the effects of both simple and complex interventions in a life course framework that incorporates biological, physical, demographic, and generational measures. The information gleaned holds great potential to drive precision policies to improve health equity [47].
CONCLUSION
Although studies of health inequalities frequently conclude that child health providers should be more mindful of the social determinants of health and better advocates for policy change on the structural determinants [1▪▪,48], many providers feel they have been doing just that for decades, with limited impact on either interventions or outcomes. Instead, these providers seek to play a more active role in working within communities to develop and deliver dynamic population interventions that harness all that we know about children's health development to improve children's long-term health trajectories. The LCHD Approach integrates knowledge from multiple disciplines in ways that inform intervention development, suggesting new avenues for multilevel interventions that are horizontally and longitudinally aligned across the entire ecosystem [49▪▪] in a whole-community response to contemporary child health challenges. These interventions require new approaches to funding, planning, testing and evaluation and will require the development of robust measures and data systems that can inform continuous policy development in a process that mirrors one of continuous quality improvement with strong stakeholder engagement. Community-based, whole-ecosystem programs like ACT are the first step toward realizing this vision with a clear focus on achieving child health equity.
Acknowledgements
The authors would like to thank Mary Berghaus MPH for her invaluable assistance in producing this manuscript.
Financial support and sponsorship
This project is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under award UA6MC32492, the Life Course Intervention Research Network. The information, content and/or conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1▪▪.Pearce A, Dundas R, Whitehead M, Taylor-Robinson D. Pathways to inequalities in child health. Arch Dis Child 2019; 104:998–1003. [DOI] [PMC free article] [PubMed] [Google Scholar]; This paper presents a remarkably through and analytically rich examination of models of child health and of what is understood about potential pathways between social disadvantage and poorer child health with suggestions for interventions to improve health equity.
- 2.Keating DP. Social inequality in population developmental health: an equity and justice issue. Adv Child Dev Behav 2016; 50:75–104. [DOI] [PubMed] [Google Scholar]
- 3.Pillas D, Marmot M, Naicker K, et al. Social inequalities in early childhood health and development: a European-wide systematic review. Pediatr Res 2014; 76:418–424. [DOI] [PubMed] [Google Scholar]
- 4.Solar O, Irwin A. World Health Organization (2010) A Conceptual Framework for Action on the Social Determinants of Health. Discussion Paper. WHO Document Production Services. Geneva, Switzerland. [Google Scholar]
- 5.Carrilero N, Dalmau-Bueno A, García-Altés A. Socioeconomic inequalities in 29 childhood diseases: evidence from a 1,500,000 children population retrospective study. BMC Public Health 2021; 21:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Di Cesare M, Sorić M, Bovet P, et al. The epidemiological burden of obesity in childhood: a worldwide epidemic requiring urgent action. BMC Med 2019; 17:212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Halfon N, Larson K, Lu M, et al. Life course health development: past, present and future. Matern Child Health J 2014; 18:344–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bhatia A, Krieger N, Subramanian SV. Learning From History About Reducing Infant Mortality: Contrasting the Centrality of Structural Interventions to Early 20th-Century Successes in the United States to Their Neglect in Current Global Initiatives. Milbank Q 2019; 97:285–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brosco JP. NAVIGATING the future through the past: the enduring historical legacy of federal children's health programs in the United States. Am J Public Health 2012; 102:1848–1857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Markel H, Golden J. Successes and missed opportunities in protecting our children's health: critical junctures in the history of children's health policy in the United States. Pediatrics 2005; 115: (4 Suppl): 1129–1133. [DOI] [PubMed] [Google Scholar]
- 11.Tallon MM, Kendall GE, Priddis L, et al. Barriers to addressing social determinants of health in pediatric nursing practice: an integrative review. J Pediatr Nurs 2017; 37:51–56. [DOI] [PubMed] [Google Scholar]
- 12.Engel GL. The need for a new medical model: a challenge for biomedicine. Science 1977; 196:129–136. [DOI] [PubMed] [Google Scholar]
- 13.Dahlgren G, Whitehead M. The Dahlgren-Whitehead model of health determinants: 30 years on and still chasing rainbows [published online ahead of print, 2021 Sep 14]. Public Health 2021; 199:20–24. [DOI] [PubMed] [Google Scholar]
- 14.Mistry KB, Minkovitz CS, Riley AW, et al. A new framework for childhood health promotion: the role of policies and programs in building capacity and foundations of early childhood health. Am J Public Health 2012; 102:1688–1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15▪▪.Schor EL. Life course health development in pediatric practice. Pediatrics 2021; 147:e2020009308. [DOI] [PubMed] [Google Scholar]; Preventive pediatric care that incorporates a life course health development approach can promote better health and prevent chronic illness during adulthood. This will require purposeful partnerships with other entities with which children and families interact, and improvements in patient care processes.
- 16.Halfon N, Forrest CB, Lerner RM, et al. Springer, Handbook of life course health development [Internet]. Cham:2018. [PubMed] [Google Scholar]
- 17.Halfon N, Forrest CB. Halfon N, Forrest CB, Lerner RM, Faustman E. The emerging theoretical framework of life course health-development. Springer, Handbook of life course health development. New York:2018. [PubMed] [Google Scholar]
- 18.Halfon N, Hochstein M. Life course health development: an integrated framework for developing health, policy, and research. Milbank Q 2002; 80:433-iii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pan American Health Organization. Building health throughout the life course. concepts, implications, and application in public health. Washington, DC: Pan American Health Organization; 2020. [Google Scholar]
- 20▪.Gehred MZ, Knodt AR, Ambler A, et al. Long-term neural embedding of childhood adversity in a population-representative birth cohort followed for 5 decades. Biol Psychiatry 2021; 90:182–193. [DOI] [PMC free article] [PubMed] [Google Scholar]; This new publication from the Dunedin longitudinal cohort study demonstrated that both prospectively ascertained childhood adversity and retrospectively reported adversity were associated with alterations in midlife structural brain integrity, but prospective associations were consistently stronger. These data add support to calls to find better ways to address adverse childhood experiences which are influencing later life mental health and cognition.
- 21▪.McDade TW, Koning SM. Early origins of socioeconomic inequalities in chronic inflammation: evaluating the contributions of low birth weight and short breastfeeding. Soc Sci Med 2021; 269:113592. [DOI] [PMC free article] [PubMed] [Google Scholar]; This analysis of data from the National Longitudinal Study of Adolescent to Adult Health (Add Health) finds a strong association between breastfeeding duration and chronic inflammation based on concentrations of C-reactive protein (CRP). Incresing breastfeeding duration to 3 or more months corresponds to a flattening of the SES gradient by 80%, and 83% when low birthweight is eliminated.
- 22.Crear-Perry J, Correa-de-Araujo R, Lewis Johnson T, et al. Social and structural determinants of health inequities in maternal health. J Womens Health 2021; 30:230–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Diderichsen F, Evans T, Whitehead M. Evans T, Whitehead M, Diderichsen F, Bhuiya A, Wirth M. The social basis of disparities in health. Oxford University Press, Challenging inequities in health – from ethics to action. New York:2001. [Google Scholar]
- 24.Slopen N, Heard-Garris N. Structural racism and pediatric health-a call for research to confront the origins of racial disparities in health [published online ahead of print, 2021 Oct 11]. JAMA Pediatr 2021. [DOI] [PubMed] [Google Scholar]
- 25.Larson K, Russ SA, Kahn RS. Halfon N, Forrest CB, Lerner RM, Faustman EM, et al. Health disparities: a life course health development perspective and future research directions. Handbook of life course health development. Cham: Springer; 2017. 499–520. [PubMed] [Google Scholar]
- 26.Braveman P. What is health equity: and how does a life-course approach take us further toward it? Matern Child Health J 2014; 18:366–372. [DOI] [PubMed] [Google Scholar]
- 27.O’Cathain A, Croot L, Duncan E, et al. Guidance on how to develop complex interventions to improve health and healthcare. BMJ Open 2019; 9:e029954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28▪▪.Apostolopoulos Y, Lich KH, Lemke MK. Complex systems and population health a primer. New York NY: Oxford University Press; 2020. [Google Scholar]; This ground-breaking book provides a knowledge base for the introduction of a complex systems paradigm to population health science. It integrates complex systems theory, methodology, modeling and computer simulation with real world applications in an approach that holds great promise for addressing pressing health and health equity challenges.
- 29.Diez Roux AV. Complex systems thinking and current impasses in health disparities research. Am J Public Health 2011; 101:1627–1634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rutter H, Savona N, Glonti K, et al. The need for a complex systems model of evidence for public health. Lancet 2017; 390:2602–2604. [DOI] [PubMed] [Google Scholar]
- 31.Kroelinger CD, Rankin KM, Chambers DA, et al. Using the principles of complex systems thinking and implementation science to enhance maternal and child health program planning and delivery. Matern Child Health J 2014; 18:1560–1564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ford CL, Airhihenbuwa CO. Critical race theory, race equity, and public health: toward antiracism praxis. Am J Public Health 2010; 100S1: (suppl 1): S30–S35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33▪.Horton M, Perman-Howe PR, Angus C, et al. The SPECTRUM Consortium: a new UK Prevention Research Partnership consortium focused on the commercial determinants of health, the prevention of noncommunicable diseases, and the reduction of health inequalities. Wellcome Open Res 2021; 6:6. [DOI] [PMC free article] [PubMed] [Google Scholar]; Exposure to unhealthy commodity products including tobacco, alcohol and sugar are preventable but these commodities are highly profitable. SPECTRUM is a group of UK researchers seeing to understand the complex systems driving consumption of these commodities with the aim of reducing harm and health inequalities caused by their consumption.
- 34.Meier P, Purshouse R, Bain M, et al. The SIPHER Consortium: Introducing the new UK hub for systems science in public health and health economic research. Wellcome Open Res 2019; 6:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Springer, Halfon N, Forrest CB, Lerner RM, Faustman EM, Tullis E, Son J. Halfon N., et al. Life Course Research Agenda (LCRA), Version 1.0. Handbook of Life Course Health Development 2017. 623–645. [Google Scholar]
- 36.Russ SA, Larson K, Tullis E, Halfon N. A lifecourse approach to health development: implications for the maternal and child health research agenda. Maternal and child health journal 2014; 18:497–510. [DOI] [PubMed] [Google Scholar]
- 37.Narayan AJ, Lieberman AF, Masten AS. Intergenerational transmission and prevention of adverse childhood experiences (ACEs). Clin Psychol Rev 2021; 85:101997. [DOI] [PubMed] [Google Scholar]
- 38.Sen A. Nussbaum Sen. Capability and Well Being. Clarendon Press, The quality of life. Oxford:1993. [Google Scholar]
- 39. Gardner, B. The Developmental Capability Model of Child Well-Being. Chapter 4 in The Well- Being of Children: Philosophical and Social Scientific Approaches Eds. Gottfried Schhweiger & Gunter Graf, Warsaw, Poland.: De Gruyer Open Poland, (2015). [Google Scholar]
- 40.Langley GL, Moen R, Nolan KM, et al. the improvement guide: a practical approach to enhancing organizational performance (2nd edition). San Francisco: Jossey-Bass Publishers; 2009. [Google Scholar]
- 41.Kahn RS, Iyer SB, Kotagal UR. Development of a child health learning network to improve population health outcomes; presented in honor of Dr Robert Haggerty. Acad Pediatr 2017; 17:607–613. [DOI] [PubMed] [Google Scholar]
- 42.Beck AF, Anderson KL, Rich K, et al. Cooling the hot spots where child hospitalization rates are high: a neighborhood approach to population health. Health Aff 2019; 38:1433–1441. [DOI] [PubMed] [Google Scholar]
- 43.Parsons A, Unaka NI, Stewart C, et al. Seven practices for pursuing equity through learning health systems: Notes from the field. In Special Issue: Collaborative learning health systems: Science and practice. Learning Health Systems 2021; 5:e10230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dickerson J, Bird PK, McEachan RC, et al. Born in Bradford's Better Start: an experimental birth cohort study to evaluate the impact of early life interventions. BMC Public Health 2016; 16:711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45▪▪. Wright J, McEachan R, Mathai M. Why is the Born in Bradford cohort study important for child health?. Arch Dis Childhood. 2021. Advance online publication. doi: 10.1136/archdischild-2020-321231. [DOI] [PubMed] [Google Scholar]; This article analyzes lessons learned from the Born in Bradford study that are applicable to other cities wishing to tackle health inequalities. These include the importance of including the whole of the life course and understanding the importance of place and diversity.
- 46.Wake M, Hu YJ, Warren H, et al. Integrating trials into a whole-population cohort of children and parents: Statement of Intent (Trials) for the Generation Victoria (GenV) cohort. BMC Med Res Methodol 2020; 20:238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Goldfeld S, Gray S, Azpitarte F, et al. Driving precision policy responses to child health and developmental inequities. Health Equity 2019; 3:489–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Marmot M. The health gap: doctors and the social determinants of health. Scand J Public Health 2017; 45:686–693. [DOI] [PubMed] [Google Scholar]
- 49▪▪.Wojcik O, Miller CE, Plough AL. Aligning health and social systems to promote population health, well being, and equity. Am J Public Health 2020; 110:S176–S177. [DOI] [PMC free article] [PubMed] [Google Scholar]; This introduction to a Special Issue of the American Journal of Public Health explains how strengthening the alignment of healthcare, public health and social service systems is a vital part of promoting health equity and building a culture of health, work that is of heightened relevance in the face of the Covid 19 pandemic.