Objective:
The aim was to compare short-term and long-term reproducibilities of in-office unattended blood pressure (BP), namely automated office blood pressure (AOBP), conventionally measured attended office BP, and self-measured home BP.
Methods:
A multicentre, clinical study was conducted in Japan, and 287 Japanese outpatients on antihypertensive drug medication were followed-up for 1 year.
Results:
The intensity of drug treatment was sustained consistently throughout the study period (defined daily doses, 1.62–1.68; P = 0.12). The mean SBP differences between baseline and 1 month later, as well as baseline and 1 year later, were less than 1.5 mmHg, whereas the standard deviations of the differences for home, AOBP, and attended office measurements for the 1-year interval were 7.7, 14.5, and 15.3 mmHg, respectively. The coefficients of variation were significantly smaller for home BP than for AOBP among all patients at both 1-month and 1-year intervals (P < 0.0001). In the 1-month interval, partial correlation coefficients of home BP (r, 0.73/0.88 for systolic/diastolic measures) were significantly higher than of conventional BP (r, 0.47/0.69). However, the correlations converged to the modest level regardless of BP information (r, 0.49–0.54/0.63–0.73) when the 1-year interval was assessed. Results were confirmatory when patients on the same drug regimen (n = 167) were analysed.
Conclusion:
A higher reproducibility of home BP was demonstrated compared with in-office BP, including AOBP. However, the modest correlations for the 1-year interval support the importance of regular assessment of BP, regardless of in-office or home measurements for treatment of hypertension.
Keywords: attended and unattended measurement, automated office blood pressure, conventional office blood pressure, home blood pressure, patient population
INTRODUCTION
Antihypertensive drug treatment is likely to be conducted for a long-term period, and continual monitoring of blood pressure is essential [1–3]. Recent guidelines recommended self-measured home blood pressure ‘to confirm the diagnosis of hypertension and for titration of blood pressure-lowering medication’ [2] and as a tool for monitoring blood pressure control [3]. In the untreated population, home blood pressure measurements have high reproducibility for short-term [4–6], as well as 1-year long-term intervals [7]. However, there has been no robust evidence for the reproducibility of home blood pressure with respect to the catchment intervals in patients on antihypertensive medication, which would be a fundamental prerequisite to using home blood pressure measurement widely in clinical practice.
The COmparison of Self-measured home, Automated unattended office and Conventional attended office blood pressure (COSAC) study [8] showed that unattended automated office blood pressure (AOBP), which is measured in office by an automated blood pressure measurement device under stringent conditions including the absence of an observer (unattended) [9–13], provides better in-office blood pressure information but it requires more medical resources than conventional office blood pressure, and AOBP cannot replace the self-measured home blood pressure [8,13]. Similar to home blood pressure, little attention has been given to the reproducibility of AOBP [14], and this issue was not discussed even in recent debates [15–17]. Furthermore, no previous studies compared the reproducibility of AOBP with that of self-measured home blood pressure. Therefore, the enrolled COSAC study patients were followed-up for 1 year, and the aim was to directly compare the short-term to long-term reproducibility of in-office unattended and attended blood pressures with self-measured home blood pressure.
METHODS
Study population
The COSAC study is a multicentre, clinical study that assesses the self-measured home blood pressure, AOBP, and conventionally measured attended office blood pressure using automated devices in patients with hypertension. The COSAC protocol complies with the recent Declaration of Helsinki with respect to the ‘ethical principles for medical research involving human subjects’ [18] and is registered with the UMIN Clinical Trial Registry as an observational study, number UMIN000026721 (http://www.umin.ac.jp/ctr). The institutional review board of the University of the Ryukyus approved the study protocol (#1042 on 2 February 2017), and all study participants gave their informed consent.
The Baseline survey was conducted from March to September 2017. Eligible patients were those with essential hypertension, at least 50 years of age, who were able to measure and record their home blood pressure by themselves regularly. Patients who declined to participate in the study or were considered not to be eligible as judged by their doctors were excluded. Of the 308 patients across all three clinics who completed the initial assessment, 21 were excluded as they moved (n = 6) or did not visit the clinic (n = 13) during follow-up, or as they did not measure home blood pressure at the end of follow-up (n = 2). Therefore, the current analysis of the 1-year follow-up data included a total of 287 eligible patients.
Blood pressure measurement
In daily clinical practice, the study doctors who were hypertension specialists had regularly instructed patients on home blood pressure measurement and confirmed the effective use of the validated upper-arm cuff oscillometric blood pressure monitor, including the appropriate cuff size for individuals. According to the Japanese Guidelines [1,19], patients were asked to measure their home blood pressure in the sitting position twice every morning after at least 2 min of rest. They had to obtain these measurements within 1 h of waking, after urination, before breakfast, and before taking antihypertensive medication. They were also asked to measure their home blood pressure twice every evening just before going to bed. In the COSAC study, the enrolled patients recorded their home blood pressure over 5 days just before each clinic visit (visits 1–3; Supplementary Figure 1).
Conventional attended office blood pressure was measured in accordance with the JSH 2014 Guidelines [19]. All three study doctors used two validated [20] upper arm cuff-oscillometric Omron HEM-907 (Omron Healthcare Co. Ltd., Kyoto, Japan) automated sphygmomanometers, and they used one device for the attended office blood pressure measurement, which was directly performed in a consultation room. After a few minutes of rest, they measured the office blood pressure twice at Katsuya Clinic and Yokohama Sotetsu bldg. Clinic with a 1– 2 min interval (n = 190), whereas it was measured only once at Miyakawa Clinic (n = 97), while maintaining the arm-cuff position at the level of the heart in a seated position.
AOBP as unattended office blood pressure was captured using the other Omron HEM-907 device; the same model was also used in the Systolic Blood Pressure Intervention Trial (SPRINT) [11,21,22]. After the conventional attended office blood pressure measurement in the consultation room, patients moved to an examination room at each clinic, and trained medical staff set the device to automatically wait 5 min and then activate to measure the blood pressure three times consecutively at 1-min intervals. Once the staff left the examination room after attaching a proper-size arm-cuff to the study patient, the patient sat alone in a back-supported chair for the resting period, after which the measurement was automatically performed. Throughout the process, the patient was at rest without talking or texting. This measurement procedure complied fully with the most stringent conditions of AOBP used in SPRINT – patients were left alone during the antecedent rest, as well as during the blood pressure measurements [11,13].
Other measurements
For the general assessment at visit 1, a questionnaire was used to obtain information on medical history and related conditions in each patient. We asked the doctors to define patients’ complications according to the common definitions used in Japan, for example, diabetes mellitus was the use of antidiabetic drugs, a fasting blood glucose concentration of at least 7.0 mmol/l, a random blood glucose concentration of at least 11.1 mmol/l, or diabetes documented in the clinic records. A history of cardiovascular disease included both nonfatal stroke and nonfatal myocardial infarction. Th BMI was the body weight in kilograms divided by the height in meters squared. Information on antihypertensive drug regimens, including prescribed timing, such as morning, noon, evening, or bedtime, was also collected.
Follow-up
During the follow-up period, blood pressures of the patients were captured 1 month later (visit 2) and 1 year later (visit 3). Just before each visit, the study patients similarly recorded their home blood pressure over 5 days while maintaining the same antihypertensive medications. Office blood pressures were measured at visits 2 and 3 under the same measurement conditions as at visit 1. The study centre did not make any treatment recommendations, and doctors continued antihypertensive treatment at their discretion and reported the antihypertensive drug regimen accordingly.
Quality control
Patients recorded home blood pressure values with the measurement times, dates, and remarks on paper. The study doctors collected the paper at each outpatient visit and checked the measurements. All blood pressure and other measurement data were sent to the data management centre at the University of the Ryukyus, where they were further checked by the data manager (Y.I.) independently, and the data manager followed up with the study doctors with any questions as necessary. To ensure the quality of the study, the investigators had biannual meetings in connection with the major scientific conferences and regularly monitored the three clinic sites before and during the study period.
Statistical analyses
We used SAS software, version 9.4 (SAS Institute Inc., Cary, North Carolina, USA) for database management and statistical analyses. significance was defined as α less than 0.05 on two-sided tests. All data are expressed as means (SD) unless otherwise stated.
Home blood pressure refers to the average of the morning and evening measurements. Furthermore, each of the average morning and evening home blood pressures was analysed separately as previous studies have shown that these measurements have different prognostic meanings [23,24]. For the AOBP and attended office blood pressure values, all of the readings were averaged for the analysis.
The amount of antihypertensive medication for each individual was standardized using the defined daily doses [25], which is the assumed average maintenance dose per day for a drug used for its main indication in adults developed by the World Health Organization Collaborating Centre for Drug Statistics Methodology System of Defined Daily Doses. When a patient took two or more antihypertensive drugs, the defined daily dose for the patient is the sum of them. The definition of the same drug regimen is that a patient took the same antihypertensive agent at the same dose with the same prescribed timing during the day on the different assessed visits.
The Kruskal–Wallis test and Fisher's exact test were used to compare means and proportions, respectively. The inter-individual coefficient of variation was calculated as the mean of the SD of the differences divided by the mean blood pressure of the paired measurements. The total number of participants required to detect a difference between the two antihypertensive drug effects was calculated by setting the power at 0.90 and the significance level at 0.05 in a parallel-group design clinical trial [26,27]. Bland and Altman (difference against mean) plots [28] were used to examine the agreement between blood pressure values. Blood pressure values and defined daily doses were compared among visits 1–3 by a repeated-measures mixed linear model while taking missing values into account. Pearson's correlation coefficients were calculated to determine the correlation between each blood pressure value as blood pressures can be treated as normally distributed. These correlation analyses were done using residuals, in which the contribution of confounders and covariables to the variance of the trait under study was removed. Adjusted estimates accounted for sex, age, overweight (BMI ≥25 kg/m2), current smoking and drinking status, diabetes mellitus, dyslipidaemia, cardiovascular disease history, clinic sites, and defined daily doses. We further applied multiple linear regression models to explore independent factors associated with the mean difference between blood pressure information. In the regression models, change in defined daily doses between visits was further adjusted, in addition to the aforementioned factors.
RESULTS
The baseline characteristics of the 287 eligible patients and the 21 excluded patients are shown in Table 1. The mean age of the eligible patients was 71.7 (SD 9.7) years, 57.8% were women, and 97.5% received antihypertensive drug treatment at baseline. Compared with the baseline survey as visit 1, 8 (2.8%) and 120 (41.8%) patients changed their antihypertensive drug regimen at visits 2 (1 month later) and 3 (1 year later), respectively. Of the 287 analysed patients, 284, 285, and 283 measured morning home BP over 5 days at visits 1–3, respectively (completion rate ≥98.6%). Similarly, evening home BPs were measured by 279 patients, of whom 275, 274, and 266 completed 5 days’ measurement at visits 1–3, respectively (≥95.3%). As demonstrated in Table 2, the intensity of drug treatment represented by defined daily doses was sustained consistently throughout the study period (defined daily doses, 1.62–1.68; P = 0.12), and no significant differences in blood pressure values were observed among visits 1–3 (P ≥ 0.064).
TABLE 1.
Baseline characteristics of the patients
| Variable | Eligible patients (n = 287) | Excluded patients (n = 21) | P |
| Women [n (%)] | 166 (57.8) | 12 (57.1) | >0.99 |
| Age (years) | 71.7 (9.7) | 72.7 (15.3) | 0.25 |
| BMI (kg/m2) | 25.0 (3.9) | 23.8 (2.3) | 0.20 |
| Current smoker [n (%)] | 23 (8.0) | 5 (23.8) | 0.031 |
| Current habitual drinking [n (%)] | 121 (42.2) | 11 (52.4) | 0.37 |
| Diabetes mellitus [n (%)] | 54 (18.8) | 1 (4.8) | 0.14 |
| Dyslipidaemia [n (%)] | 178 (62.0) | 11 (52.4) | 0.49 |
| Previous cardiovascular disease [n (%)] | 13 (4.5) | 2 (9.5) | 0.27 |
| Antihypertensive drug treatment [n (%)] | 277 (96.5) | 20 (95.2) | 0.55 |
| Interval between visits 1 and 2 (days) | 32.9 (8.7) | N/A | – |
| Interval between visits 1 and 3 (days) | 377.0 (20.4) | N/A | – |
| Drug regimen changed at visit 2 [n (%)] | 8 (2.8) | N/A | – |
| Drug regimen changed at visit 3 [n (%)] | 120 (41.8) | N/A | – |
Values are shown as the numbers of patients (percentage) or means (SD) for continuous variables. Definitions of each complication of the patients were reported by study clinics according to the most commonly used definition in Japan. Each drug regimen change was in comparison with visit 1 at baseline.
TABLE 2.
Defined daily doses and blood pressures of 287 patients at visits 1–3
| Variable | Visit 1 baseline | Visit 2 1 month later | Visit 3 1 year later | P |
| Defined daily doses (units) | 1.63 (1.12) | 1.62 (1.12) | 1.68 (1.17) | 0.12 |
| Attended office measurement | ||||
| SBP (mmHg) | 139.2 (16.9) | 138.0 (15.5) | 138.3 (17.1) | 0.39 |
| DBP (mmHg) | 74.6 (12.0) | 74.1 (12.1) | 75.0 (12.7) | 0.20 |
| Pulse rate (beats per minute) | 76.9 (12.7) | 76.0 (12.4) | 76.4 (11.6) | 0.23 |
| Unattended office measurement | ||||
| SBP (mmHg) | 128.9 (15.9) | 127.4 (14.8) | 127.8 (14.4) | 0.17 |
| DBP (mmHg) | 70.5 (11.6) | 70.0 (11.7) | 69.8 (11.2) | 0.30 |
| Pulse rate (beats per minute) | 72.8 (11.8) | 72.2 (12.1) | 72.1 (11.3) | 0.32 |
| Combined home measurement | ||||
| SBP (mmHg) | 125.7 (8.4) | 124.9 (9.1) | 125.8 (8.4)∗ | 0.083 |
| DBP (mmHg) | 72.9 (8.6) | 72.4 (8.8) | 72.6 (8.2) | 0.22 |
| Pulse rate (beats per minute) | 67.7 (8.5) | 67.4 (8.3) | 67.8 (8.3) | 0.33 |
| Morning home measurement | ||||
| SBP (mmHg) | 127.9 (9.3) | 127.0 (9.8)∗ | 127.8 (9.1) | 0.094 |
| DBP (mmHg) | 75.1 (8.9) | 74.4 (9.2)∗ | 74.4 (8.6) | 0.064 |
| Pulse rate (beats per minute) | 66.3 (9.0) | 66.1 (8.7) | 66.5 (8.7) | 0.42 |
| Evening home measurement | ||||
| SBP (mmHg) | 123.4 (9.9) | 122.8 (10.5) | 123.7 (9.8) | 0.16 |
| DBP (mmHg) | 70.6 (9.3) | 70.2 (9.4) | 70.7 (8.8) | 0.29 |
| Pulse rate (beats per minute) | 69.1 (9.2) | 68.8 (9.0) | 69.2 (9.1) | 0.34 |
Values are shown as means (SD). Evening home measurements were unavailable in seven patients at visit 1 [one from Katsuya Clinic (KC) and six from Yokohama Sotetsu bldg. Clinic (YSBC)], eight patients at visits 2 (two from KC and six from YSBC), and 11 patients at visit 3 (one from KC and 10 from YSBC). P values were calculated by a repeated-measures mixed linear model to take missing values into account and represent the differences among the visits. BP, blood pressure. Significance of differences from the left adjacent visit: ∗P < 0.05.
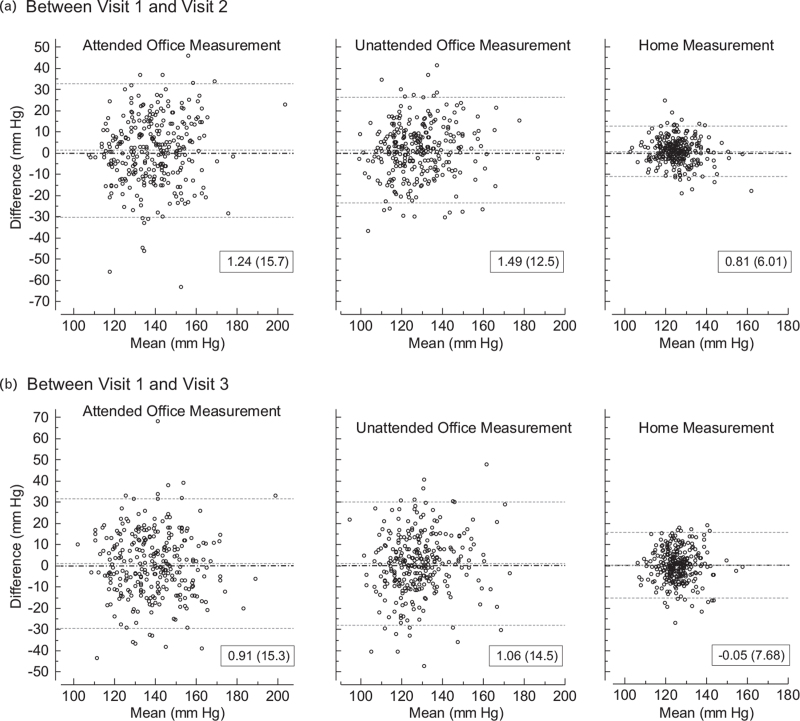
The Bland and Altman plots (Fig. 1) demonstrated that the mean SBP differences between visits 1 and 2 were less than 1.5 mmHg, whereas the SD of the differences in home, unattended office, and attended office blood pressures varied by 6.0, 12.5, and 15.7 mmHg, respectively. The results were essentially similar when blood pressure values measured at visits 1 and 3 were compared; although the mean SBP differences were less than 1.1 mmHg regardless of blood pressure information, SDs in the same order were 7.7, 14.5, and 15.3 mmHg. Similar plots were drawn when patients with the same drug regimen during 1 month or 1 year, separately, were assessed (Supplementary Figure 2). The plots based on diastolic measurements of all participants and of those with the same drug regimen are shown in Supplementary Figures 3 and 4, respectively. The coefficient of variation was significantly smaller for home blood pressure compared with unattended office blood pressure in all patients (P < 0.0001; Table 3), as well as in those with the same drug regimen (P ≤ 0.0008; Supplementary Table 1). On the basis of the SD of the differences, as shown in the same tables, the total number of participants needed to detect a significant difference in home self-measurements was approximately half to a quarter when compared with that needed to detect a significant difference of attended office readings. For example, the total numbers of participants needed to detect a significant difference based on the combined home blood pressure for systolic measurements were 18 and 28 for visits 1 and 2 and for visits 1–3, respectively.
FIGURE 1.
Bland and Altman plots for the comparison of SBP measurements between (a) visit 1 and visit 2 and between (b) visit 1 and visit 3. Scales of the three y-axes are aligned. Mean differences and ±2 SD between paired measurements are represented by dotted lines, and the values of the mean (SD) difference are in boxes in each panel. Dash-dotted lines are placed where the difference is zero.
TABLE 3.
Blood pressure and pulse rate differences from visit 1 to visit 2 and visit 1 to visit 3
| Between visits 1 and 2 | Between visits 1 and 3 | |||||||
| Measurement | n | Difference [mean (SD)] | CV [mean (SD)] | Sample size | N | Difference, mean (SD) | CV, mean (SD) | Sample size |
| SBP (mmHg) | ||||||||
| Attended office | 287 | 1.24 (15.71) | 6.22 (5.03) | 106 | 287 | 0.91 (15.27) | 6.25 (4.79) | 102 |
| Unattended office | 287 | 1.49 (12.49) | 5.41 (4.45)† | 68 | 287 | 1.06 (14.47) | 6.16 (5.21) | 92 |
| Combined home | 287 | 0.81 (6.01) | 2.59 (2.21)§ | 18 | 287 | −0.05 (7.68) | 3.31 (2.73)§ | 28 |
| Morning home | 287 | 0.97 (6.77) | 2.82 (2.54)∗ | 22 | 287 | 0.11 (8.91) | 3.77 (3.12)§ | 36 |
| Evening home | 279 | 0.63 (7.41) | 3.16 (2.82) | 26 | 276 | −0.29 (8.57) | 3.77 (3.10) | 34 |
| DBP (mmHg) | ||||||||
| Attended office | 287 | 0.51 (7.91) | 5.70 (4.88) | 108 | 287 | −0.39 (8.78) | 6.43 (5.40) | 132 |
| Unattended office | 287 | 0.46 (6.77) | 5.47 (4.68) | 80 | 287 | 0.70 (8.39) | 6.62 (5.71) | 122 |
| Combined home | 287 | 0.51 (3.78) | 2.95 (2.40)§ | 28 | 287 | 0.32 (5.58) | 4.17 (3.45)§ | 56 |
| Morning home | 287 | 0.65 (4.13) | 3.16 (2.63) | 32 | 287 | 0.68 (6.23) | 4.46 (3.88)∗ | 68 |
| Evening home | 279 | 0.33 (4.66) | 3.62 (3.09)∗ | 40 | 276 | −0.18 (5.96) | 4.76 (3.67) | 62 |
| Pulse rate (beats per minute) | ||||||||
| Attended office | 287 | 0.94 (8.48) | 5.68 (5.31) | 124 | 287 | 0.55 (9.79) | 6.81 (5.37) | 164 |
| Unattended office | 287 | 0.60 (7.44) | 5.24 (4.79) | 96 | 287 | 0.67 (8.37) | 6.29 (5.11)∗ | 120 |
| Combined home | 287 | 0.31 (3.71) | 2.79 (2.58)§ | 26 | 287 | −0.05 (4.98) | 3.84 (3.14)§ | 44 |
| Morning home | 287 | 0.26 (4.25) | 3.19 (3.07)‡ | 34 | 287 | −0.12 (5.69) | 4.40 (3.75)‡ | 58 |
| Evening home | 279 | 0.32 (4.25) | 3.17 (2.82) | 34 | 276 | −0.09 (5.64) | 4.39 (3.47) | 56 |
Values are means (SD) of the variables. CV denotes inter-individual coefficient of variation (units are dimensionless), and significances of differences from the superjacent row (those with full evening measurement information were compared in the comparison between morning and evening blood pressures) are marked: ∗P less than 0.05; †P less than 0.01; ‡P less than 0.001; and §P less than 0.0001. Sample size is the number of total participants required for a parallel-group design clinical trial in order to detect a difference between the two drug effects of 10/5 mmHg in SBP/DBP, or 5 beats per minute pulse rate, with a power of 0.90 and significance level of 0.05 in each measurement.
Between visits 1 and 2, partial correlation coefficients (r values) of systolic/diastolic measurements were significantly higher for home blood pressure, 0.73 [95% CI 0.67–0.78)/0.88 (0.85–0.91), than for conventional blood pressure (0.47 (0.37-0.56)/0.69 (0.63–0.75); P < 0.0001], as shown in Table 4. Correlation r values increased from attended, unattended office, to home blood pressure. Differences in correlations between attended office and unattended office blood pressure were significant for the systolic measurements (P = 0.0036/0.16), and those between home and unattended office blood pressure were significant (P = 0.031/<0.0001). However, the correlations were similar within a modest level when baseline SBP and that captured 1 year later (visit 3) were compared in all patients (r values, 0.49–0.59; P ≥ 0.10). Results were confirmatory when patients who changed their drug regimen were excluded as shown in the lower rows of Table 4.
TABLE 4.
Partial correlations between visits
| SBP | DBP | Pulse rate | ||
| Blood pressures | n | r (95% CI) | r (95% CI) | r (95% CI) |
| All patients | ||||
| Visit 1–visit 2 | ||||
| Attended office | 287 | 0.47 (0.37–0.56) | 0.69 (0.63–0.75) | 0.75 (0.70–0.80) |
| Unattended office | 287 | 0.64 (0.56–0.70) | 0.75 (0.69–0.80) | 0.78 (0.73–0.82) |
| Combined home | 287 | 0.73 (0.67–0.78) | 0.88 (0.85–0.91) | 0.90 (0.87–0.92) |
| Morning home | 287 | 0.71 (0.65–0.76) | 0.87 (0.84–0.90) | 0.87 (0.84–0.90) |
| Evening home | 275 | 0.70 (0.64–0.76) | 0.85 (0.81–0.88) | 0.89 (0.86–0.91) |
| Visit 1–visit 3 | ||||
| Attended office | 287 | 0.54 (0.45–0.62) | 0.64 (0.57–0.71) | 0.64 (0.56–0.70) |
| Unattended office | 287 | 0.49 (0.39–0.57) | 0.63 (0.55–0.70) | 0.70 (0.63–0.76) |
| Combined home | 287 | 0.54 (0.45–0.62) | 0.73 (0.67–0.78) | 0.81 (0.77–0.85) |
| Morning home | 287 | 0.49 (0.39–0.57) | 0.68 (0.61–0.74) | 0.77 (0.72–0.82) |
| Evening home | 275 | 0.59 (0.51–0.66) | 0.75 (0.69–0.80) | 0.80 (0.76–0.84) |
| Same drug regimen | ||||
| Visit 1–visit 2 | ||||
| Attended office | 279 | 0.50 (0.41–0.59) | 0.71 (0.65–0.76) | 0.76 (0.70–0.80) |
| Unattended office | 279 | 0.66 (0.58–0.72) | 0.77 (0.71–0.81) | 0.78 (0.73–0.82) |
| Combined home | 279 | 0.74 (0.67–0.79) | 0.88 (0.86–0.91) | 0.90 (0.87–0.92) |
| Morning home | 279 | 0.71 (0.65–0.77) | 0.88 (0.85–0.90) | 0.87 (0.84–0.90) |
| Evening home | 267 | 0.71 (0.64–0.76) | 0.85 (0.81–0.88) | 0.89 (0.86–0.91) |
| Visit 1–visit 3 | ||||
| Attended office | 167 | 0.57 (0.45–0.67) | 0.65 (0.55–0.73) | 0.69 (0.60–0.76) |
| Unattended office | 167 | 0.61 (0.50–0.70) | 0.69 (0.60–0.77) | 0.75 (0.67–0.81) |
| Combined home | 167 | 0.48 (0.35–0.59) | 0.70 (0.61–0.77) | 0.83 (0.78–0.88) |
| Morning home | 167 | 0.43 (0.30–0.55) | 0.66 (0.57–0.74) | 0.78 (0.71–0.84) |
| Evening home | 159 | 0.55 (0.43–0.66) | 0.71 (0.62–0.78) | 0.83 (0.77–0.87) |
Values are shown as Pearson's correlation coefficient r [95% confidence intervals (CI)] values. Adjusted estimates accounted for sex, age, overweight (BMI ≥25 kg/m2), current smoking and drinking, diabetes mellitus, dyslipidaemia, cardiovascular diseases history, clinic sites, and defined daily doses. Evening home blood pressures (BPs) were not fully measured in 12 patients; they were thus excluded from the corresponding analysis. Unattended and attended denote unattended office BP and conventionally measured attended office BP, respectively.
The multiple linear regression model demonstrated that only a few independent factors were associated with differences in the SBP taken at visits 1 and 2, as well as visits 1 and 3 (Table 5). Of them, changes in defined daily doses had the only consistent impact on the difference in all sorts of blood pressures between visits 1 and 2 (≥8.75 mmHg per change of defined daily doses); however, the impact of changes in defined daily doses was significantly but weakly associated with the home blood pressure changes for the 1-year interval (1.55 mmHg per change, P = 0.042), and impacts of the other factors were inconsistent. Similar results were obtained when patients were limited to those with the same antihypertensive drug regimen for visits 1 and 2 (Supplementary Table 2), as well as visits 1 and 3 (Supplementary Table 3). In the comparison between visits 1 and 3, overweight at baseline was associated with lower office blood pressure in patients with the same drug regimen (P ≤ 0.042), but the association was not observed for home blood pressure (P ≥ 0.22).
TABLE 5.
Independent factors associated with differences in the SBP
| Attended | Unattended | Combined home | Morning home | Evening home | ||||||
| Variable | PE | 95% CI | PE | 95% CI | PE | 95% CI | PE | 95% CI | PE | 95% CI |
| Between visit 1 and visit 2 | ||||||||||
| Average BP (per 1 mmHg) | 0.09 | (−0.05 to 0.22) | 0.04 | (−0.06 to 0.15) | −0.13 | (−0.22 to −0.04)† | −0.11 | (−0.21 to −0.02)∗ | −0.07 | (−0.17 to 0.03) |
| Women (vs. men) | −0.64 | (−4.88 to 3.61) | −0.21 | (−3.58 to 3.15) | −1.55 | (−3.18 to 0.08) | −1.80 | (−3.64 to 0.05) | −1.43 | (−3.52 to 0.67) |
| Age (per 10 years) | −1.29 | (−3.25 to 0.67) | −0.31 | (−1.87 to 1.25) | 0.62 | (−0.13 to 1.37) | 0.61 | (−0.25 to 1.46) | 0.53 | (−0.44 to 1.50) |
| Overweight | −3.25 | (−7.03 to 0.54) | −1.21 | (−4.22 to 1.79) | −1.26 | (−2.72 to 0.19) | −1.64 | (−3.29 to 0.01) | −0.93 | (−2.80 to 0.93) |
| Current smoker | −0.28 | (−7.13 to 6.57) | 2.04 | (−3.39 to 7.47) | −0.21 | (−2.84 to 2.42) | −0.28 | (−3.26 to 2.70) | −0.28 | (−3.65 to 3.09) |
| Current habitual drinking | 1.10 | (−2.94 to 5.14) | 1.84 | (−1.37 to 5.05) | −0.15 | (−1.70 to 1.41) | 0.26 | (−1.51 to 2.03) | −0.44 | (−2.46 to 1.57) |
| Diabetes mellitus | 0.51 | (−4.21 to 5.24) | −1.10 | (−4.83 to 2.64) | −0.12 | (−1.94 to 1.70) | −0.67 | (−2.73 to 1.38) | 0.53 | (−1.80 to 2.86) |
| Dyslipidaemia | 2.25 | (−1.65 to 6.15) | 2.56 | (−0.53 to 5.65) | 1.29 | (−0.21 to 2.79) | 0.96 | (−0.74 to 2.66) | 1.64 | (−0.29 to 3.56) |
| Previous CV disease | −2.22 | (−11.2 to 6.78) | −2.90 | (−10.0 to 4.23) | 0.00 | (−3.45 to 3.46) | −0.30 | (−4.21 to 3.61) | 0.11 | (−4.43 to 4.65) |
| Katsuya Clinic (vs. MC) | 1.70 | (−3.14 to 6.54) | 0.13 | (−3.76 to 4.02) | −0.10 | (−2.00 to 1.80) | 0.37 | (−1.80 to 2.54) | −0.64 | (−3.03 to 1.75) |
| YSBC (vs. MC) | −0.79 | (−5.65 to 4.06) | −2.05 | (−5.87 to 1.77) | 0.93 | (−0.84 to 2.71) | 1.08 | (−0.91 to 3.08) | 0.30 | (−1.98 to 2.58) |
| DDD at baseline (per unit) | 2.63 | (0.96 to 4.31)† | 1.86 | (0.53 to 3.18)† | 0.54 | (−0.14 to 1.21) | 0.51 | (−0.25 to 1.26) | 0.43 | (−0.42 to 1.28) |
| Changes in DDD (per unit) | 32.0 | (17.9 to 46.0)§ | 26.8 | (15.6 to 38.0)§ | 10.2 | (4.76 to 15.6)‡ | 11.6 | (5.49 to 17.8)‡ | 8.75 | (1.90 to 15.6)∗ |
| Between visit 1 and visit 3 | ||||||||||
| Average BP (per 1 mmHg) | −0.02 | (−0.15 to 0.11) | 0.11 | (−0.03 to 0.25) | −0.09 | (−0.22 to 0.04) | −0.05 | (−0.19 to 0.09) | −0.02 | (−0.15 to 0.10) |
| Women (vs. men) | 0.62 | (−3.64 to 4.87) | −1.08 | (−5.06 to 2.91) | −0.80 | (−2.90 to 1.30) | −0.92 | (−3.35 to 1.51) | −1.07 | (−3.52 to 1.39) |
| Age (per 10 years) | −0.51 | (−2.49 to 1.47) | −0.25 | (−2.11 to 1.60) | 0.20 | (−0.78 to 1.18) | 0.35 | (−0.79 to 1.49) | −0.10 | (−1.24 to 1.05) |
| Overweight | −3.99 | (−7.78 to −0.20)∗ | −3.11 | (−6.66 to 0.44) | −1.60 | (−3.48 to 0.27) | −2.04 | (−4.21 to 0.13) | −1.33 | (−3.51 to 0.85) |
| Current smoker | −1.37 | (−8.24 to 5.49) | −0.28 | (−6.72 to 6.17) | −0.58 | (−3.98 to 2.81) | −0.45 | (−4.38 to 3.49) | −0.93 | (−4.92 to 3.06) |
| Current habitual drinking | 3.67 | (−0.39 to 7.73) | 0.02 | (−3.78 to 3.82) | 0.09 | (−1.91 to 2.10) | 1.11 | (−1.21 to 3.43) | −1.18 | (−3.54 to 1.18) |
| Diabetes mellitus | 2.78 | (−1.95 to 7.52) | 0.71 | (−3.72 to 5.14) | −1.19 | (−3.53 to 1.16) | −1.77 | (−4.48 to 0.94) | 0.08 | (−2.65 to 2.80) |
| Dyslipidaemia | 1.06 | (−2.86 to 4.98) | 1.40 | (−2.29 to 5.08) | 0.93 | (−1.01 to 2.87) | 1.40 | (−0.86 to 3.65) | 0.34 | (−1.91 to 2.60) |
| Previous CV disease | −0.20 | (−9.23 to 8.82) | 0.82 | (−7.63 to 9.26) | 0.42 | (−4.04 to 4.87) | −1.27 | (−6.44 to 3.89) | 1.71 | (−3.56 to 6.98) |
| Katsuya Clinic (vs. MC) | −1.55 | (−6.42 to 3.33) | −2.82 | (−7.43 to 1.80) | 1.46 | (−0.97 to 3.90) | 1.51 | (−1.34 to 4.35) | 1.20 | (−1.57 to 3.96) |
| YSBC (vs. MC) | −3.63 | (−8.51 to 1.24) | −1.39 | (−6.04 to 3.26) | 3.24 | (0.94 to 5.53)† | 3.49 | (0.83 to 6.14)∗ | 2.74 | (0.05 to 5.43)∗ |
| DDD at baseline (per unit) | 0.07 | (−1.64 to 1.78) | 0.93 | (−0.67 to 2.53) | 0.88 | (−0.01 to 1.77) | 1.01 | (−0.01 to 2.03) | 0.51 | (−0.50 to 1.52) |
| Changes in DDD (per unit) | 3.42 | (0.43 to 6.41)∗ | 4.71 | (1.91 to 7.51)† | 1.55 | (0.07 to 3.03)∗ | 1.47 | (−0.25 to 3.19) | 1.53 | (−0.19 to 3.25) |
Point estimates (PEs) reflect the increase in the SBP difference per variable unit. Combined home BPs were the average of morning and evening home BPs at each visit. Changes in defined daily doses (DDD) were calculated from that at the later visit (visit 2 or visit 3) minus that at visit 1. Evening home measurements were unavailable in eight patients at visits 1 and/or 2, and in 11 patients at visits 1 and/or 3. Unattended and attended denote unattended office BP and conventionally measured attended office BP, respectively. The variance inflation factors were 1.82 or less. CI, confidence interval; CV, cardiovascular; MC, Miyakawa Clinic; YSBC, Yokohama Sotetsu bldg. Clinic. Significance of differences: ∗P < 0.05; †P < 0.01; ‡P < 0.001; and §P < 0.0001.
Whenever the patients were limited to those whose unattended office blood pressures were measured during the same time period (within a 3 h, as well as within a 1 h, difference), confirmatory results were obtained (Supplementary Table 4). Among those who measured unattended office blood pressure within a 1 h difference between the visits, the mean of the difference (SD) and the CV (SD) of the systolic/diastolic measurements were 1.44 (12.84)/0.41 (6.55) mmHg and 5.51 (4.62)/5.27 (4.51) for the comparison between visits 1 and 2 (n = 221), and 1.44 (14.18)/0.80 (7.85) mmHg and 5.98 (4.99)/6.41 (5.26) for the comparison between visits 1 and 3 (n = 193), respectively. Meanwhile, even when patients from Miyakawa Clinic, where attended office blood pressures were taken once at each visit, were excluded, essentially similar results were observed, as shown in Supplementary Table 5.
DISCUSSION
In the present study, short-term and long-term reproducibilities of home and office blood pressure measurements were assessed in Japanese outpatients on antihypertensive drug treatment. According to the Bland and Altman plots and coefficients of variation, which can be treated as the standardized size of the variation in differences, home blood pressure variation was the smallest, followed by unattended office and attended office blood pressures in this order, regardless of 1-month or 1-year intervals, despite using the same Omron HEM-907 devices for both unattended and attended office blood pressures. In the 167 participants with the same drug regimen, baseline antihypertensive drug use represented by the defined daily doses did not affect 1-year reproducibility, and this was also found in all patients when changes of the defined daily doses during the follow-up were taken into account in the multivariable-adjusted models. The higher reproducibility of home blood pressure was also supported by the correlation analysis for the 1-month interval. However, correlation coefficients between visits 1 and 3 converged to the modest level regardless of blood pressure information.
The reproducibility of home blood pressure was high compared with attended office blood pressure, as in previous reports [4–7,29]. High correlations of home blood pressure (correlation r for systolic/diastolic measurements, 0.91/0.86) compared with attended office blood pressure (0.77/0.76) at 3-week intervals were observed in the Greek untreated population (n = 133, 45% women, mean 48.4 years old) [4], although their average home blood pressure level from days 2 to 6 was 138.7/89.3 mmHg [4]. Kawabe and Saito measured morning home, evening home, and office blood pressures in 503 untreated healthy volunteers (34.6% women, mean age 39.4 years) at approximately 6-month intervals from autumn to spring, and they found that the correlations were r = 0.91/0.90, 0.90/0.87, and 0.74/0.72, respectively [5]. The mean blood pressures were less than 120/less than 75 mmHg irrespective of the type of blood pressure measurement [5]. In the 136 residents of Ohasama, Japan (70.6% women, mean age 56 years, all not taking antihypertensive medication), the SDs of the mean differences in systolic/diastolic home morning and attended office blood pressures at the 1-year interval were 7.7/5.5 and 13.8/10.2 mmHg, respectively [7]. Compared with the baseline blood pressure levels, those measured 1 year later were 0.8 (7.7)/0.9 (5.5) mmHg higher in the home measurement, whereas they were 3.9 (13.8)/3.1 (10.2) mmHg lower in the office measurement [7]. Their average home blood pressure levels were 120.1/71.2 mmHg at the initial assessment, which is 7.8/3.9 mmHg lower than the current COSAC-treated patients. In the Arsakeion school study [29] of 51 Greek children with elevated blood pressures, home and attended office blood pressures were measured at baseline (43.7% girls; mean age, 11.3 years) and an average of 17 months later (range, 10–26 months). The home blood pressure measured later was 3.8 (8.3)/1.2 (6.5) mmHg lower than the baseline measurement, although the children had grown (the reason for this unlikely increase is not clear). The SDs of the mean differences in home and office blood pressures were 8.3/6.5 and 13.9/10.7 mmHg, respectively, and the coefficients of variation were 5.3/6.6 and 8.2/10.9, respectively.
In the present study, the reproducibility of home blood pressure was high compared with unattended AOBP. The essentially similarly poor reproducibility of AOBP compared with conventional attended office blood pressure, even in those with the same drug regimen, might reduce the usefulness of AOBP, as stringent AOBP measurement is resource-intensive, and therefore, less feasible compared with conventional office blood pressure measurement [8,12,13]. Nevertheless, we would like to emphasize that usual office blood pressure is measured poorly [16], despite the recommended protocol provided by the guidelines [1–3,30]. The feasibility of the conventional office blood pressure measurement would be overestimated as it is relatively time efficient; however, we should be cautious as office blood pressure is likely to be measured inappropriately and inaccurately [16]. AOBP theoretically enhances the office blood pressure measurement condition if practitioners and healthcare providers are able to prepare the environment for AOBP [12,16]. As we previously reported, the three consecutive AOBP readings within one patient had high reproducibility (r ≥ 0.90) [8]. Furthermore, in 62 Canadian patients referred by a hypertension specialist for 24-h ambulatory monitoring (50% women; mean age, 65 years; 94% took antihypertensive medication), AOBP readings on three different occasions [median (range) interval between first and second visits was 61 (25–307) days, and that between second and third visits was 26 (5–162) days] had high reproducibility (intra-class correlation coefficients r = 0.90/0.87 for SBP/DBP) [14]. AOBP technique with the strict measurement protocol can, therefore, capture reliable office blood pressure values on each occasion. As the average attended office blood pressure was 11/4 mmHg higher than AOBP [8], AOBP has less of a white-coat effect. The prognostic ability of AOBP was also reported based on the Cardiovascular Health Awareness Program (CHAP) in Ontario, Canada, in community-dwelling residents aged more than 65 years without [31] and with [32] antihypertensive medication (published in succession). However, compared with the vast evidence from clinical trials and these meta-analyses of conventional office measurement, the prognostic value of AOBP remains largely unsettled [15], and the feasibility of the repeated assessment of AOBP measurement will be the main concern when considering AOBP to be incorporated widely in clinical practice.
Whenever based on the correlation coefficient statistic, the differences in the three blood pressures were significant at the 1-month interval but they tended to converge to a modest level at the 1-year interval. In the Ohasama population, the crude correlation coefficients were 0.84/0.83 for home measurements and 0.69/0.57 for conventional attended office measurements [7]. However, 34.6% (72 of 208) of them dropped out from the final assessment [7]. In the Arsakeion school study [29], the crude correlation coefficients of home and office blood pressures were 0.58/0.52 and 0.51/0.44, respectively, similar to the present study. Nevertheless, the investigators concluded that the reproducibility of home blood pressure was higher than that of office measurement as the correlation coefficient is not appropriate for assessing reproducibility, although it can determine the strength of the linear association between two assessments and complements the other criteria [29]. The high dropout rate of children, 46.9% (45 of the 96 eligible children whose blood pressures were measured at baseline) [29], implies the difficulty of both this sort of long-term study in children and appropriate assessment of long-term reproducibility. Stergiou et al.[27] recently reported that, in another Greek paediatric population (n = 58; 39.7% girls; mean age, 13 years), the SDs of the mean difference in systolic/diastolic home and attended office blood pressures at intervals of 1–6 months were 5.9/5 and 7.7/5.8 mmHg, respectively, with correlation coefficients of 0.87/0.83 and 0.85/0.86, respectively. Although the number of participants was small, their findings [27] support the results of the Arsakeion study and the current COSAC study in terms of the SD of the mean difference.
Though checked by doctors, the reported home blood pressure measurements were recorded on paper, and the long-term reproducibility of home blood pressure represented by the correlation coefficient was lower than the previous report [7]. The previous report was based on a semiautomatic device (Omron HEM401C), and patients recorded the displayed blood pressure values manually [7]. Reliability of reporting home blood pressure values by patients with hypertension varied and was unpredictable [33]. To improve the management of hypertension, the use of memory-equipped automated home blood pressure devices would make us free from observer, selection, and reporting biases [33,34].
The present study must be interpreted within the context of potential limitations. First, blood pressure values were recorded in device memory for unattended AOBP but they were recorded on paper for attended office and home measurements. Though it is not likely that doctors reported the wrong numbers at the office, we cannot guarantee the accuracy of self-reporting as aforementioned [33]. Nevertheless, the lowest variation of self-measured home blood pressure demonstrated in the Bland and Altman plot supports the usefulness of home blood pressure for long-term management of hypertension. Second, the current population consisted of Japanese outpatients on antihypertensive drug treatment. The mean age was 71.7 years, and such elderly people may be more anxious with self-measurement than younger individuals. Although the present results are in partial agreement with the previous studies [4,7,29], they might not be generalizable to other populations. Third, home blood pressures were measured using the patients’ own devices, and there may be some lack of precision with self-measurement of blood pressure at home. As mentioned earlier, the reported home values were recorded on paper, which is affected by reporting bias, for example, patients might discard their higher or unexpected readings. Furthermore, though not reported, some patients might have replaced their measurement devices during the study period. However, doctors and staff of the three clinic sites are used to conducting home blood pressure-based management of hypertension as they had contributed to a clinical trial using home blood pressure during the first decade of the 2000s [34], and instruction on home blood pressure measurement for the patients, as well as office measurements, was reliably performed in accordance with the contemporaneous JSH 2014 Guidelines [19]. Fourth, as many patients had their AOBP measured for the first time during participation in the study, a first-time effect may have had some effect on the blood pressure values. However, the patients in the present study had been taken care of by each doctor for a long time, and general assessment including routine laboratory tests had been performed repeatedly. They had also measured home blood pressure continuously since before the study was initiated. It is, therefore, fair to say that the general assessment minimally affected the findings, and the first-time effect on home blood pressure was none or minimal, if any, as reported from another Japanese patient population [35]. Fifth, the attended office blood pressure was always measured before the AOBP measurement. The intention was to prevent an unexpected effect of the AOBP measurement on the conventional office BP values; however, the nonrandomized order of office measurements may cause bias. Nevertheless, this order effect, which favoured the reproducibility of AOBP, would enhance the current finding that home blood pressure had more reproducibility than even AOBP measured under the strict condition. Finally, the socioeconomic status and its changes in each patient were not assessed in the present study. Even though none of the 287 patients experienced life-threatening events during the study period, a patient might encounter a health outcome that can shift the blood pressure level. However, the relatively high 1-year follow-up rate (287 of the 308 patients at baseline; 93.2%), despite patients being recruited from general clinical practice, would ensure the robustness of the present findings.
In conclusion, home blood pressures had high reproducibility when compared with in-office measurements, irrespective of the reproducibility indices in a short-term assessment. When blood pressures measured at the 1-year interval were assessed, the home blood pressure reproducibility based on correlation r values became similar to that of in-office blood pressure measurements, although the Bland and Altman plots with variability indices supported the higher reproducibility of home blood pressure. Beyond drug treatment, continual intervention for participants, such as lifestyle modification and dietary advice, may alter blood pressure levels. The current findings support frequent assessment of in-office and home blood pressures in individuals as being useful, in addition to their surrounding environmental factors and socioeconomic status, for the long-term management and treatment of hypertension.
ACKNOWLEDGEMENTS
COSAC Study Coordination and Management
The COmparison of Self-measured home, Automated unattended office and Conventional attended office blood pressure (COSAC) study working group: T Ohkubo (Chair; Teikyo University), H Rakugi (Vice Chair; Osaka University), K Asayama (Teikyo University), S Ito (Tohoku University), S Ueda (University of Ryukyus), S Umemura (Yokohama Rosai Hospital), Y Ohya (University of Ryukyus), T Tsuchihashi (Yawata Hospital), K Kario (Jichi University), K Miura (Shiga University).
Clinical Investigators: H Mori (Yokohama Sotetsu bldg. Clinic), M Miyakawa (Miyakawa Clinic), T Katsuya (Katsuya Clinic).
Secretariat and Data Management Committee: S Ueda (chair; University of Ryukyus), Y Ikehara (University of Ryukyus), K Une (University of Ryukyus).
Statistical Analysis Committee: K Miura (chair; Shiga University), K Asayama. (Teikyo University).
Conflicts of interest
K.A., T.O., K.K., and K.M. received research support from Omron Healthcare. The remaining authors declare no conflicts of interest in association with the present study. This study was supported solely by the Japanese Society of Hypertension.
Supplementary Material
Footnotes
Abbreviations: AOBP, automated office blood pressure; COSAC, COmparison of Self-measured home, Automated unattended office and Conventional attended office blood pressure; SPRINT, Systolic Blood Pressure Intervention Trial
Supplemental digital content is available for this article.
Contributor Information
Collaborators: The Japanese Society of Hypertension Working Group on the COmparison of Self-measured home, Automated unattended office, Conventional attended office blood pressure (COSAC) study
REFERENCES
- 1.Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res 2019; 42:1235–1481. [DOI] [PubMed] [Google Scholar]
- 2.Whelton PK, Carey RM, Aronow WS, Casey DE, Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018; 71:e127–e248. [DOI] [PubMed] [Google Scholar]
- 3.Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. ESC Scientific Document Group. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J 2018; 39:3021–3104. [DOI] [PubMed] [Google Scholar]
- 4.Stergiou GS, Baibas NM, Gantzarou AP, Skeva II, Kalkana CB, Roussias LG, Mountokalakis TD. Reproducibility of home, ambulatory, and clinic blood pressure: implications for the design of trials for the assessment of antihypertensive drug efficacy. Am J Hypertens 2002; 15 (2 Pt 1):101–104. [DOI] [PubMed] [Google Scholar]
- 5.Kawabe H, Saito I. Reproducibility of masked hypertension determined from morning and evening home blood pressure measurements over a 6-month period. Hypertens Res 2007; 30:845–851. [DOI] [PubMed] [Google Scholar]
- 6.Fujiwara T, Hoshide S, Kanegae H, Nishizawa M, Kario K. Reliability of morning, before-dinner, and at-bedtime home blood pressure measurements in patients with hypertension. J Clin Hypertens (Greenwich) 2018; 20:315–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sakuma M, Imai Y, Nagai K, Watanabe N, Sakuma H, Minami N, et al. Reproducibility of home blood pressure measurements over a 1-year period. Am J Hypertens 1997; 10 (7 Pt 1):798–803. [DOI] [PubMed] [Google Scholar]
- 8.Asayama K, Ohkubo T, Rakugi H, Miyakawa M, Mori H, Katsuya T, et al. Japanese Society of Hypertension Working Group on the COmparison of Self-measured home, Automated unattended office and Conventional attended office blood pressure (COSAC) study. Comparison of blood pressure values-self-measured at home, measured at an unattended office, and measured at a conventional attended office. Hypertens Res 2019; 42:1726–1737. [DOI] [PubMed] [Google Scholar]
- 9.Myers MG. Automated office blood pressure-incorporating SPRINT into clinical practice. Am J Hypertens 2017; 30:8–11. [DOI] [PubMed] [Google Scholar]
- 10.Stergiou GS, Doumas M, Kollias A, Papademetriou V. Important practice lessons from the SPRINT study beyond the blood pressure goal: all well known and now confirmed. J Am Soc Hypertens 2016; 10:613–617. [DOI] [PubMed] [Google Scholar]
- 11.Johnson KC, Whelton PK, Cushman WC, Cutler JA, Evans GW, Snyder JK, et al. SPRINT Research Group. Blood pressure measurement in SPRINT (Systolic Blood Pressure Intervention Trial). Hypertension 2018; 71:848–857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Asayama K, Ohkubo T, Imai Y. In-office and out-of-office blood pressure measurement. J Hum Hypertens 2021; doi: 10.1038/s41371-021-00486-8 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Asayama K, Ohkubo T. Unattended automated measurements—office and out-of-office blood pressure affected by medical staff and environment. Hypertension 2019; 74:1294–1296. [DOI] [PubMed] [Google Scholar]
- 14.Myers MG, Valdivieso M, Kiss A. Consistent relationship between automated office blood pressure recorded in different settings. Blood Press Monit 2009; 14:108–111. [DOI] [PubMed] [Google Scholar]
- 15.Zhang ZY, Vanassche T, Verhamme P, Staessen JA. Implementing automated office blood pressure measurement. Hypertension 2019; 74:441–449. [DOI] [PubMed] [Google Scholar]
- 16.Jones DW. Implementing automated office blood pressure measurement. Hypertension 2019; 74:436–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Elias MF, Goodell AL. Human errors in automated office blood pressure measurement: still room for improvement. Hypertension 2021; 77:6–15. [DOI] [PubMed] [Google Scholar]
- 18.World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 2013; 310:2191–2194. [DOI] [PubMed] [Google Scholar]
- 19.Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, et al. Japanese Society of Hypertension Committee for Guidelines for the Management of Hypertension. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014). Hypertens Res 2014; 37:253–390. [DOI] [PubMed] [Google Scholar]
- 20.White WB, Anwar YA. Evaluation of the overall efficacy of the Omron office digital blood pressure HEM-907 monitor in adults. Blood Press Monit 2001; 6:107–110. [DOI] [PubMed] [Google Scholar]
- 21.Ambrosius WT, Sink KM, Foy CG, Berlowitz DR, Cheung AK, Cushman WC, et al. SPRINT Study Research Group. The design and rationale of a multicenter clinical trial comparing two strategies for control of systolic blood pressure: the Systolic Blood Pressure Intervention Trial (SPRINT). Clin Trials 2014; 11:532–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.SPRINT Research Group, Wright JT, Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med 2015; 373:2103–2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Asayama K, Kikuya M, Schutte R, Thijs L, Hosaka M, Satoh M, et al. Home blood pressure variability as cardiovascular risk factor in the population of Ohasama. Hypertension 2013; 61:61–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Asayama K, Ohkubo T, Kikuya M, Obara T, Metoki H, Inoue R, et al. Prediction of stroke by home “morning” versus “evening” blood pressure values: the Ohasama study. Hypertension 2006; 48:737–743. [DOI] [PubMed] [Google Scholar]
- 25. World Health Organization. World Health Organization Collaborating Centre for Drug Statistics Methodology System of Defined Daily Doses. Available at: https://www.whocc.no/atc_ddd_index. [Accessed 13 September 2021] [Google Scholar]
- 26.Imai Y, Ohkubo T, Hozawa A, Tsuji I, Matsubara M, Araki T, et al. Usefulness of home blood pressure measurements in assessing the effect of treatment in a single-blind placebo-controlled open trial. J Hypertens 2001; 19:179–185. [DOI] [PubMed] [Google Scholar]
- 27.Stergiou GS, Bountzona I, Alamara C, Vazeou A, Kollias A, Ntineri A. Reproducibility of office and out-of-office blood pressure measurements in children: implications for clinical practice and research. Hypertension 2021; 77:993–1000. [DOI] [PubMed] [Google Scholar]
- 28.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986; 1:307–310. [PubMed] [Google Scholar]
- 29.Stergiou GS, Nasothimiou EG, Giovas PP, Rarra VC. Long-term reproducibility of home vs. office blood pressure in children and adolescents: the Arsakeion school study. Hypertens Res 2009; 32:311–315. [DOI] [PubMed] [Google Scholar]
- 30.Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension 2020; 75:1334–1357. [DOI] [PubMed] [Google Scholar]
- 31.Myers MG, Kaczorowski J, Paterson JM, Dolovich L, Tu K. Thresholds for diagnosing hypertension based on automated office blood pressure measurements and cardiovascular risk. Hypertension 2015; 66:489–495. [DOI] [PubMed] [Google Scholar]
- 32.Myers MG, Kaczorowski J, Dolovich L, Tu K, Paterson JM. Cardiovascular risk in hypertension in relation to achieved blood pressure using automated office blood pressure measurement. Hypertension 2016; 68:866–872. [DOI] [PubMed] [Google Scholar]
- 33.Mengden T, Hernandez Medina RM, Beltran B, Alvarez E, Kraft K, Vetter H. Reliability of reporting self-measured blood pressure values by hypertensive patients. Am J Hypertens 1998; 11:1413–1417. [DOI] [PubMed] [Google Scholar]
- 34.Asayama K, Ohkubo T, Metoki H, Obara T, Inoue R, Kikuya M, et al. Cardiovascular outcomes in the first trial of antihypertensive therapy guided by self-measured home blood pressure. Hypertens Res 2012; 35:1102–1110. [DOI] [PubMed] [Google Scholar]
- 35.Sano H, Hara A, Asayama K, Miyazaki S, Kikuya M, Imai Y, Ohkubo T. Antihypertensive drug effects according to the pretreatment self-measured home blood pressure: the HOMED-BP study. BMJ Open 2020; 10:e040524. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.