Abstract
Background
Music therapy (MT) programs have been used in various health care settings to reduce patients’ pain, anxiety, and stress. However, few studies have investigated its effects on patients with spinal cord injury (SCI), a frequently serious event requiring extensive rehabilitation.
Objective
This pilot study evaluated the feasibility of offering music-assisted relaxation (MAR) during rehabilitation for patients with SCI. We also measured the effect of MAR on the patients’ pain, anxiety, and stress levels.
Methods
Patients were hospitalized at Mayo Clinic (Rochester, Minnesota) from September 2015 through September 2017 for rehabilitation of an SCI. Eligible patients received 2, 20-minute, personalized MAR sessions. Interventions were facilitated by a board-certified music therapist (MT-BC) and included diaphragmatic breathing, guided imagery, and passive muscle relaxation with live guitar accompaniment and spoken, improvised, or singing voice. Two surveys (Generalized Anxiety Disorder [GAD-7] and Perceived Stress Scale [PSS-10]) were used at the time of study consent and again upon hospital dismissal. Pain, anxiety, and relaxation were assessed before and after both MT sessions with visual analog scales (VASs), scored from 0 to 10. Participants completed a 7-question satisfaction survey after the second MAR session.
Results
Twenty patients were enrolled (12 men, 8 women); 13 (65%) completed the MAR interventions. The mean (SD) age was 53.7 (17.7) years. VAS scores for pain significantly improved after both sessions (P ≤ .02). VAS scores for anxiety also significantly improved after both sessions (P ≤ .02), as did VAS scores for relaxation (P ≤ .02 for both). The satisfaction survey indicated that patients generally believed that they benefited from MT. Rehabilitation staff indicated that MT did not interfere with routine clinical care.
Conclusion
MT with live MAR is a feasible treatment for patients with SCI and may be effective for reducing their pain and anxiety.
Keywords: music, music therapy, rehabilitation, relaxation, spinal cord injury
Introduction
Spinal cord injury (SCI) is frequently a catastrophic event and is estimated to affect more than 275 000 persons in the United States. 1 Medical complications after SCI (e.g., orthostatic hypotension, autonomic dysreflexia, bradyarrhythmia, and instability of temperature) are common and often severe. Functional recovery after an SCI begins in the acute care setting with range-of-motion and resistive exercise, upright positioning, and transfer work. In the inpatient setting, physical and occupational therapists develop individualized programs that focus on strengthening, joint protection, and compensatory strategies by using assistive devices and equipment to maximize function. 2 Neuropathic pain and anxiety affect much of the SCI population and are particularly intractable to treatment; these concerns can be psychologically and physically debilitating and have a negative impact on quality of life.3,4
Relaxing music is a nonpharmacologic intervention that can reduce anxiety and potentially reduce the need for medications.5,6 Music can refocus attention and alter perceptions of anxiety by replacing stressful environmental stimuli with novel auditory stimuli in the attention channels in the brain. 7 Anxiety may be reduced by listening to preferred, relaxing music, 8 and this approach can be effective for patients with various medical conditions, during procedures, and in surgical arenas. 9 An increased relaxation response is initiated when music dampens activity in the sympathetic nervous system. 10 When the sympathetic activity decreases, patients show positive physiologic changes such as decreased respiratory and cardiovascular rates 11 and decreased cortisol levels. 12
Although listening to music can certainly facilitate relaxation, music therapy (MT) interventions guided by a music therapist can address a broader range of patients’ needs during a hospital admission. Board-certified music therapists (MT-BCs) personalize music interventions (e.g., adjust tempo, volume, pitch, or timbre of the music, or even modify lyrics) to meet specific goals in the care plan such as pain management, coping, procedural support, and functional rehabilitation. One MT intervention that may be effective for addressing the needs of patients with SCI is music-assisted relaxation (MAR). MAR is a receptive approach with guided prompts for relaxation, breathing, imagery, or a combination thereof. 13 Although many studies have reported a benefit with music-guided relaxation programs in various clinical settings,14–18 relatively little in the literature addresses the effect of MAR on patients with SCI. Because of the considerable physical and psychological challenges associated with SCI, every effort must be made to improve coping support for patients. The purpose of this pilot study was to examine the feasibility and preliminary effectiveness of MAR, facilitated by an MT-BC, for addressing pain and anxiety in patients with SCI.
Methods
This study was approved by the Mayo Clinic Institutional Review Board (protocol number 15-005031). Patients provided written, informed consent. The reporting of this study is in compliance with the Strengthening the Reporting of Observational Studies in Epidemiology statement. 19
Study Design
We conducted a pilot study within the Integrative Medicine and Health section of the Division of General Internal Medicine at Mayo Clinic (Rochester, Minnesota). This study used a pretest-posttest design, which was chosen to provide beginning and end point measures of anxiety, pain, and relaxation. The measures also were used to help the research team and medical personnel determine the feasibility of a future, larger-scale study in this setting.
Patients and Setting
This study was conducted in our inpatient rehabilitation unit from September 1, 2015, through September 30, 2017. The inpatient rehabilitation unit at Mayo Clinic Hospital—Rochester, Saint Marys Campus, is a 38-bed acute unit that admits patients from a broad age range (from pediatric to geriatric) with conditions such as brain injury, stroke, SCI, limb amputation, and debility attributable to cardiovascular disease, cancer, organ transplantation, or prolonged hospitalization. Requirements for inpatient rehabilitation include the need for 2 or more therapy modalities, physician oversight, and rehabilitation nursing. Patients must be able to participate in 3 hours of therapy a day. Patients were recruited to the study by a study coordinator and were included if they met the following criteria: (1) had an SCI; (2) were admitted to the inpatient rehabilitation unit; and (3) were able to complete the study forms. Patients with clinically significant hearing impairment were excluded from this study. We enrolled a convenience sample of 20 patients.
MT Intervention
The MT-BC met with patients in their private rooms. The MT-BC invited family members and visitors to stay if they wanted to passively observe the session, or they were welcomed to take their own self-care break if needed. The MT-BC began the intervention by explaining MT and asking the patient to rate his or her pain and anxiety level before the start of the session. A nurse also obtained vital signs before the start of each session. The MT-BC invited the patient to choose a comfortable place in the room, such as seated in a wheelchair or lying in bed. Lights were dimmed, curtains were drawn, and other stimuli (e.g., television) were turned off to create a relaxing environment.
The MT-BC guided the patient through a 20-minute, personalized MAR exercise. The therapist played an acoustic classical guitar in the key of G major. The MT-BC improvised various embellished chords in this key in a finger-picking style. 20 The tempo of the music was personalized, based on the MT-BC’s clinical observations of the patient’s respiratory rate. Concepts of entrainment were incorporated throughout the exercise by slowing the tempo of the music as the intervention progressed (to cue the patient to breathe more deeply) and then increasing the tempo at the end of the session, when the patient’s awareness was brought back to the present space. The music was used primarily to facilitate relaxation and provide a container for the relaxation experience. Cues for diaphragmatic breathing, guided imagery, and muscle relaxation were also provided.
The MAR script had a standardized format that was created by the MT-BC (a template for the relaxation script is shown in Appendix A). This overall format was adapted to each patient to support their individual needs, in accordance with MT practice principles. The imagery used in the sessions was framed in a manner such that each patient could imagine or create a place or space that brought them peace or comfort. Each patient was invited to imagine incorporating all their senses to paint a mental picture of that place. Simple prompts were provided to encourage each patient to imagine what they saw (e.g., colors, objects, and people), smelled, heard, and felt.
After the intervention, relaxation techniques (diaphragmatic breathing, guided imagery, and muscle relaxation) were reviewed with the patient, and they were directed to practice these relaxation techniques independently at least once daily between rehabilitation therapy sessions or in the evening, after therapy was completed. The medical center’s designated relaxation and wellness channel on the television was recommended for these independent practice sessions.
The MT-BC contacted the patient and provided a second session within 72 hours after the initial MAR session. The second session used the same protocol of personalized MAR with live music. Appendix B shows the procedural flowchart (summary of the intervention).
Survey Instruments
All patient outcome measures were collected by a study coordinator. Patients rated their pain, anxiety, and relaxation levels with visual analog scales (VASs). Possible scores ranged from 0 to 10. For the pain or anxiety scales, 0 represented no pain or anxiety and 10 represented the worst possible pain or anxiety. For the relaxation scales, 0 represented not relaxed and 10 represented the most relaxed. Patients rated how they felt before and after each MT intervention.
Patients also completed the Generalized Anxiety Disorder, 7 items (GAD-7) 21 and Perceived Stress Scale, 10 items (PSS-10) 22 at the time of hospital admission and dismissal. Lastly, patients completed a 7-question satisfaction survey, designed by the authors of the current study, when the second MAR session was completed.
Data Collection and Analysis
Study data, including all answers to the pre and postintervention questionnaires, were collected and managed using REDCap (Research Electronic Data Capture) tools hosted at Mayo Clinic.23,24 REDCap is a secure, web-based software platform designed to support data capture for research studies, providing (1) an intuitive interface for validated data capture; (2) audit trails for tracking data manipulation and export procedures; (3) automated export procedures for seamless data downloads to common statistical packages; and (4) procedures for data integration and interoperability with external sources.
Analyses were performed with Excel software (Microsoft Corp) and SAS 9.4 with JMP 10 software (SAS Institute Inc). The analysis used descriptive and inferential statistics to assess outcome measures. Effectiveness was assessed by using a paired t test to compare VAS scores for symptoms and feelings before and after the intervention. The α level for statistical significance was set at .05.
Results
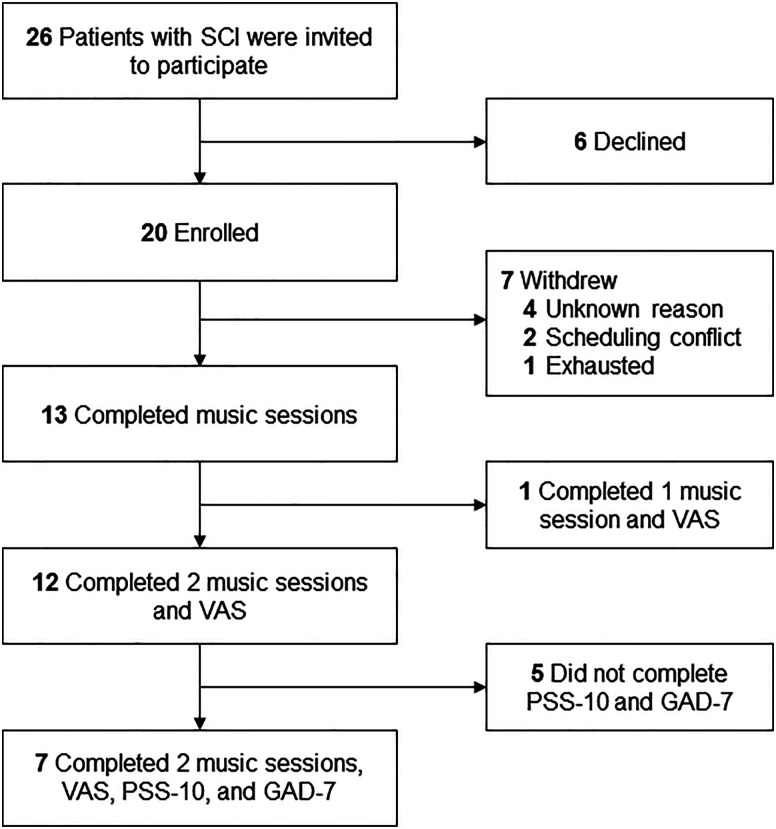
We invited 26 patients with SCI to participate in the study. Of these, 20 patients (77%) enrolled in the study by signing the consent form and 6 (23%) declined. Of the 20 enrolled patients, 12 (60%) completed both MT sessions and 1 (5%) completed only one MT session. Seven patients (35%) withdrew from the study, citing reasons such as exhaustion or scheduling conflicts (Figure 1). Table 1 summarizes characteristics of the 12 patients who completed the full study intervention plus 1 patient who completed a single MT session. The mean (SD) length of hospitalization was 11.9 (8.2) days for the enrolled patients.
Figure 1.
Patient Flow Diagram. GAD-7 indicates Generalized Anxiety Disorder, 7 items; PSS-10, Perceived Stress Scale, 10 items; SCI, spinal cord injury; VAS, visual analog scale.
Table 1.
Participant Characteristics (N = 13).
| Characteristic | Patients | |
|---|---|---|
| No | % | |
| Sex | ||
| Male | 7 | 54 |
| Female | 6 | 46 |
| Age, y | ||
| 18–40 | 3 | 23 |
| 41–50 | 3 | 23 |
| 51–60 | 2 | 15 |
| 61–70 | 2 | 15 |
| >15 | 3 | 23 |
| Length of hospital stay, day | ||
| 3–6 | 4 | 31 |
| 7–10 | 4 | 31 |
| 11–15 | 3 | 23 |
| >15 | 2 | 15 |
| Spinal cord injury | ||
| Lumbar | 1 | 8 |
| Thoracic | 5 | 38 |
| Cervical | 7 | 54 |
The effectiveness of MT was assessed by evaluating VAS scores for pain, anxiety, and relaxation before and after each session (Table 2). VAS scores for pain were significantly improved by the intervention, with a mean (SD) difference of −1.6 (1.5) (P = .002) after the first MT session and −1.6 (2.0) (P = .02) after the second session. VAS scores for anxiety and relaxation were also significantly improved by the intervention after both MT sessions. For anxiety, the mean (SD) difference was −.9 (1.2) (P = .02) after the first session and −1.1 (1.2) (P = .01) after the second session. For relaxation, the mean (SD) difference was 2.0 (2.4) (P = .01) after the first MT session and 1.7 (2.2) (P=.02) after the second session. Seven patients completed the PSS-10 and GAD-7 surveys at the time of hospital admission and dismissal (Table 3). We noted improvements in PSS-10 and GAD-7 scores but acknowledge that the sample size was small.
Table 2.
VAS Scores Before and After MT.
| >Category a | VAS score before MT, mean (SD) | VAS score after MT, mean (SD) | Difference in VAS scores, mean (SD) | P value |
|---|---|---|---|---|
| Session 1 (n = 13) | ||||
| Pain | 4.2 (2.2) | 2.6 (2.4) | −1.6 (1.5) | .002 |
| Anxiety | 1.9 (1.7) | .9 (1.4) | −.9 (1.2) | .02 |
| Relaxation | 6.4 (2.0) | 8.4 (1.0) | 2.0 (2.4) | .01 |
| Session 2 (n = 12) | ||||
| Pain | 4.2 (2.4) | 2.6 (1.8) | −1.6 (2.0) | .02 |
| Anxiety | 1.7 (1.7) | .6 (1.0) | −1.1 (1.2) | .01 |
| Relaxation | 6.9 (2.1) | 8.6 (1.1) | 1.7 (2.2) | .02 |
AbbreviationsMT, music therapy; VAS, visual analog scale.
aFor pain and anxiety, VAS scores were 0, no pain or anxiety; 10, worst possible pain or anxiety. For relaxation, VAS scores were 0, not relaxed; 10, most relaxed I could be.
Table 3.
PSS-10 and GAD-7 Scores at Time of Hospital Admission and Dismissal (n = 7).
| Anxiety or stress scale | Score a | ||
|---|---|---|---|
| Admission, mean (SD) | Dismissal, mean (SD) | Difference in scores, mean (SD) | |
| PSS-10 | 18.29 (4.89) | 11.0 (6.53) | 7.29 (7.39) |
| GAD-7 | 7.0 (3.21) | 3.71 (3.64) | 3.29 (4.39) |
Abbreviations: GAD-7, Generalized Anxiety Disorder, 7 items; PSS-10, Perceived Stress Scale, 10 items.
aRange of possible scores for GAD-7, 0–21. Range of possible scores for PSS-10, 0–40.
Responses to the patient satisfaction survey and feedback about the usefulness of MT are summarized in Table 4. Overall, the patients believed that they benefited from MT. The rehabilitation staff anecdotally indicated that providing MT in the patient’s room did not interfere with routine clinical care.
Table 4.
Patient Satisfaction and Feedback about MT (n = 10).
| Survey question | N (%) |
|---|---|
| MT positively impacted my ability to cope: | |
| Strongly agree Somewhat agree |
6 (60) 4 (40) |
| MT negatively interrupted the flow of the medical experience for me: | |
| Strongly disagree Somewhat disagree |
8 (80) 2 (20) |
| MT helped me with the following: | |
| Decreased perception of pain Decreased anxiety Decreased nausea Increased motivation Increased relaxation Normalized the medical environment Sensory stimulation Increased perception of control Spiritual needs Increased family interaction Increased quality of life Other |
8 (80) 9 (90) 2 (20) 3 (30) 8 (80) 5 (50) 1 (10) 5 (50) 3 (30) 3 (30) 6 (60) 2 (20) |
| As a patient, I feel that I benefited from MT (e.g., felt less stressed, more relaxed, and could stay more relaxed): | |
| Strongly agree Somewhat agree |
8 (80) 2 (20) |
| As a patient, I would recommend MT services to others: | |
| Strongly agree Somewhat agree |
8 (80) 2 (20) |
| How satisfied were you with MT services received? | |
| Very satisfied No response |
8 (80) 2 (20) |
| I would pay out-of-pocket for MT services in future if my insurance would not cover it: | |
| Strongly agree Somewhat agree Somewhat disagree Strongly disagree |
1 (10) 4 (40) 4 (40) 1 (10) |
Abbreviation: MT, music therapy.
Discussion
SCI is a traumatic event, and conducting interventional research studies in this patient population (and in a hospital setting) can be quite challenging. However, we were able to successfully complete this pilot study, which incorporated MT interventions for patients with SCI who had a busy schedule in a rehabilitation unit. The results of this pilot study provide preliminary data that can be helpful for planning a larger-scale study. Pain, anxiety, and relaxation scores improved significantly after the MT intervention. Patients’ perceptions of the experience were positive.
Unfortunately, the effect of MT had a short duration, with VAS scores for pain, anxiety, and relaxation essentially returning to baseline (pre-session 1 levels) by the time MT session 2 commenced. Enhanced practice instructions and a longer allotment of time for MAR exercises may have resulted in a longer period of improvement. However, MT did improve pain, anxiety, and relaxation on an intermittent basis, which is an encouraging finding. We were surprised to see low anxiety scores at baseline in our study cohort and assumed that the low anxiety was attributable to the supportive environment of our rehabilitation unit. As expected, baseline pain scores were moderate. Future research should focus on investigating the effects of MT interventions for patients reporting moderate to severe pain or anxiety (or both).
The GAD-7 and PSS-10 scores (measuring anxiety and stress, respectively) improved between hospital admission and dismissal. This improvement most certainly is the result of the entire “rehabilitation package” provided by Mayo Clinic’s SCI rehabilitation program, which strives to develop a customized program for each patient. The program relies on the team efforts of physicians, nurses, physical therapists, occupational therapists, and social workers who offer and encourage various rehabilitation interventions, including access to relaxation methods and coping skills. A television program is accessible in each patient’s room that includes relaxing music. We assume that the additional individualized MT sessions, with live music and various activities led by an MT-BC, further benefitted these patients, although these outcomes need to be evaluated in detail in the future.
Our results are consistent with those of other studies in similar populations. A few small studies have reported a positive effect of live MT on well-being, pain, cognitive function, independent function, and mobility in patients with brain and spinal injuries.14,18,25–29 A study by Mondanaro et al. 25 examined the effects of MT on the recovery of patients after spine surgery. Patients had 1 live MT intervention within 72 hours after surgery. Patients reported significant reductions in VAS pain levels, but they did not show significant differences in scores for Hospital Anxiety and Depression Scale (HADS) anxiety, HADS depression, or Tampa Scale for Kinesiophobia. 25 The authors suspected that the lack of significant change in HADS anxiety, HADS depression, and Tampa Scale for Kinesiophobia scores could be partly attributable to the timing of the intervention, which occurred soon after surgery.
In concordance with o\ur study findings, several other studies reported a benefit with music-guided relaxation programs.14,26,28,30 Nelson et al 18 reported that MT using MAR with controlled breathing and imagery was helpful for adolescents undergoing spinal fusion surgery. Live music-based relaxation exercises for terminally ill persons receiving palliative care is reported to positively affect wellbeing. 27 Preoperative anxiety also has been successfully reduced with MAR. 31
Limitations
This pilot study had a small sample size (convenience sample) and had no control arm. Patients in our rehabilitation unit have a very busy schedule, and time constraints allowed only 2 MT sessions. Survey outcomes may have been influenced by various factors unrelated to MT (for example, respondents feeling uncomfortable when providing honest answers or answer options being interpreted differently). We recognize that the GAD-7 and PSS-10 are generally considered more sensitive to long-term changes, so the relatively short length of stay of our participants may have further reduced our ability to detect significant changes over the course of a few days. Finally, multiple studies have reported patient satisfaction with MT interventions that used recorded or live music and MAR.4,14,26,28,30,32,33 In our study, the MT intervention for all patients was MAR, led by an MT-BC playing an acoustic guitar. However, we acknowledge that music preference likely varies considerably among patients. Future protocols that incorporate patient preferences for music may provide more individualized and effective therapy. Future studies should incorporate a larger sample size and a single-blind randomized design.
Conclusion
Our study suggests that MAR can be offered as an integrative intervention to patients with SCI who are admitted to a rehabilitation unit. MAR may help patients with SCI manage anxiety, stress, and pain. Large, single-blind, randomized controlled trials that incorporate patients’ music preferences are needed to build on the findings of this pilot study and to determine the efficacy of MT for patients with SCI.
Appendix A. Music-Assisted Relaxation Script Template
Please note that this template was adapted to fit each individual patient’s needs, and pauses were inserted as the board-certified music therapist (MT-BC) observed the patient’s responses throughout the intervention.
As we begin, I invite you to find a comfortable place where you are sitting (or laying). Give yourself permission to be fully present in this moment. Allow yourself to focus on the music and my voice to the best of your ability and ignore other sounds that we may hear around us. We may get interrupted, and if that happens, I will continue to play guitar quietly in the background and answer any questions the other medical team members may have. Once they are done, we will continue.
As you continue to settle into that comfortable place, you may wish to close your eyes; but if you are more comfortable leaving them open, that is ok, too. Begin by noticing your breathing. Allow yourself to notice the gentle rise and fall of your chest (or abdomen) with each breath that you take in and out… in and out… Notice the natural way you relax as you exhale or breathe out. Imagine that you are breathing in comfort and relaxation and blowing out any tension, worry, anxiety, stress, or thoughts you may be having. As you feel comfortable, take in a few slow, deep breaths. Breathe in through your nose and out through your mouth. Perhaps you may imagine a favorite smell that brings you a sense of comfort or peace. You may do that, if you wish. Let us practice a few of these slow deep breaths together. Continue to take those slow, deep breaths. With each one, imagine that you are becoming more relaxed and comfortable. You may choose to continue these slow deep breaths or allow your breathing to become smooth and natural. Whatever your body needs in this moment is ok.
Begin to allow your imagination to take you on a journey to a place that is relaxing, comforting, and/or calming. Allow yourself to explore what this place would look like. Discover with your imagination what things you would see. Notice the objects or colors. Allow yourself to imagine what types of things you might smell. Allow yourself to imagine what types of things your body might feel. Continue to imagine this peaceful and relaxing place as your imagination creates this place.… And allow yourself to enjoy it.
Allow yourself to continue creating this peaceful and relaxing place in your imagination. If you become distracted, you can always go back to your breathing or to this peaceful place.
As you continue to rest in this peaceful place, you begin to notice a gentle light shining down on you. This light brings your body comfort, peace, and deep relaxation. The light can be whatever color you choose. Allow this light to gently shine on your head, almost like a gentle scalp massage. Allow this light to slowly and gently relax each part of your face/head (slowly proceed through forehead, eyebrows, temple, nose, jaw, cheeks, lips, tongue, chin). Allow those feelings of relaxation and comfort to continue flowing throughout your head/face as that gentle light shifts its focus to your neck. Allow all the muscles and tissues in your neck to begin relaxing, releasing any tension or stress you may have there. Continue to allow these feelings as the light gently shifts its focus to your shoulders, upper extremities or arms, wrists, hands, chest/abdomen, back, pelvis, hips, knees, calves, ankles, feet, and toes.
Allow yourself to stay in this peaceful place for as long as you need, yet also know you may create this place at any time on your own. As the music begins to slowly change, begin to wiggle your fingers and toes, becoming slowly aware of your surroundings again. Begin to notice your breathing again.… Maybe take in a few of those slow deep breaths, but this time, allow each breath to bring you the strength and energy that you need for the rest of your day. Continue to wiggle your fingers and toes as your awareness shifts back to this room. When the music stops and you are ready, you may open your eyes and join me back in your room.
Appendix B. Music Therapy Intervention Procedural Flowchart. MAR Indicates
Music-Assisted Relaxation; MT-BC, Board-Certified Music
Therapist.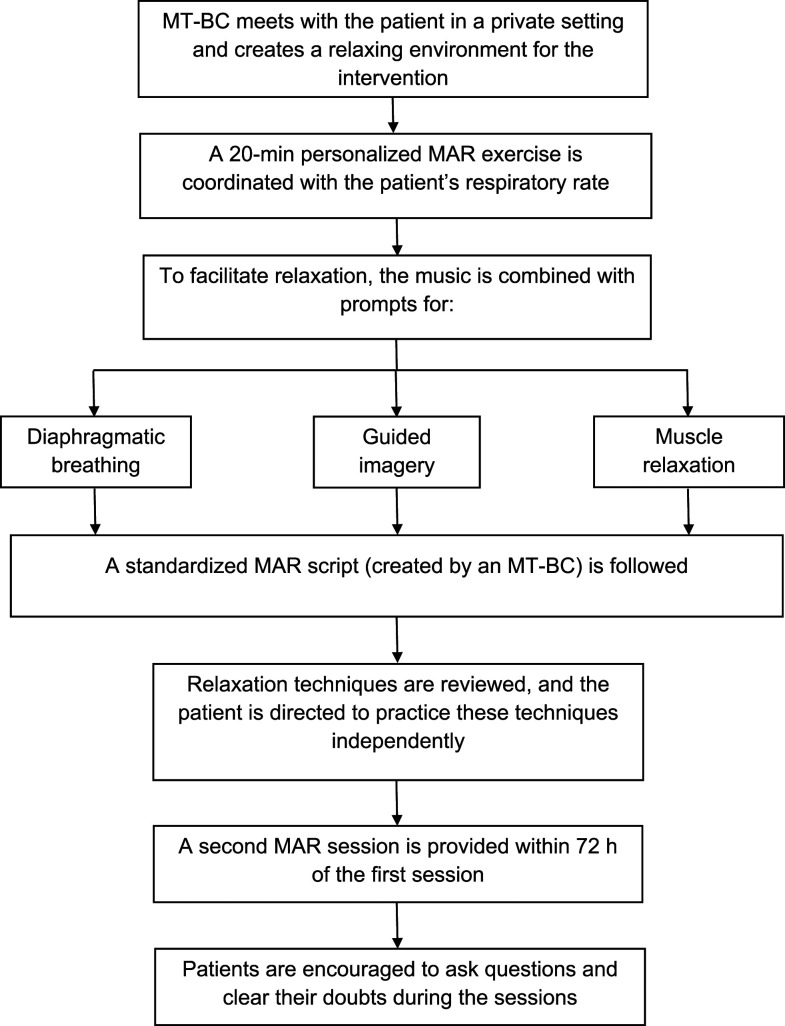
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article. Dr Bauer’s time was made available in part due to general support from The HEAD Foundation, Singapore.
Abbreviations
GAD-7, Generalized Anxiety Disorder, 7 items;
HADS, Hospital Anxiety and Depression Scale;
MAR, music-assisted relaxation;
MT, music therapy;
MT-BC, board-certified music therapist;
PSS-10, Perceived Stress Scale, 10 items;
REDCap, Research Electronic Data Capture;
SCI, spinal cord injury;
VAS, visual analog scale
ORCID iDs
Brent A. Bauer https://orcid.org/0000-0003-3453-6906
Saswati Mahapatra https://orcid.org/0000-0002-6929-1382
Dietlind L. Wahner-Roedler https://orcid.org/0000-0002-5974-0578
References
- 1.Devivo MJ. Epidemiology of traumatic spinal cord injury: trends and future implications. Spinal Cord. May 2012;50(5):365-372. doi: 10.1038/sc.2011.178. [DOI] [PubMed] [Google Scholar]
- 2.Abrams GM, Wakasa M. Chronic complications of spinal cord injury and disease. http://www.uptodatefree.com/topic/chronic-complications-of-spinal-cord-injury-and-disease. Accessed August 19, 2019.
- 3.Middleton J, Tran Y, Craig A. Relationship between quality of life and self-efficacy in persons with spinal cord injuries. Arch Phys Med Rehabil. Dec 2007;88(12):1643-1648. doi: 10.1016/j.apmr.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 4.Cardenas DD, Felix ER. Pain after spinal cord injury: A review of classification, treatment approaches, and treatment assessment. PM R. 2009;1(12):1077-1090. doi: 10.1016/j.pmrj.2009.07.002. [DOI] [PubMed] [Google Scholar]
- 5.Lee DWH, Chan KW, Poon CM, et al. Relaxation music decreases the dose of patient-controlled sedation during colonoscopy: a prospective randomized controlled trial. Gastrointest Endosc. 2002;55(1):33-36. doi: 10.1067/mge.2002.120387. [DOI] [PubMed] [Google Scholar]
- 6.Lepage C, Drolet P, Girard M, Grenier Y, DeGagné R. Music decreases sedative requirements during spinal anesthesia. Anesth Analg. Oct 2001;93(4):912-916. doi: 10.1097/00000539-200110000-00022. [DOI] [PubMed] [Google Scholar]
- 7.Thaut MH, Davis WB. The influence of subject-selected versus experimenter-chosen music on affect, anxiety, and relaxation. J Music Ther. 1993;30(4):210-223. [Google Scholar]
- 8.Chlan LL, Weinert CR, Heiderscheit A, Tracy MF, Skaar DJ, Guttormson JL, et al. Effects of patient-directed music intervention on anxiety and sedative exposure in critically Ill patients receiving mechanical ventilatory support. J Am Med Assoc. Jun 12 2013;309(22):2335-2344. doi: 10.1001/jama.2013.5670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maranto CD. Applications of music in medicine. In: M Heal, T Wigram, eds Music therapy in health and education. London: Jessica Kingsley Publishers; 1993. chap 15. [Google Scholar]
- 10.Tan X, Yowler CJ, Super DM, Fratianne RB. The interplay of preference, familiarity and psychophysical properties in defining relaxation music. J Music Ther. 2012;49(2):150-179. doi: 10.1093/jmt/49.2.150. [DOI] [PubMed] [Google Scholar]
- 11.Bernardi L, Porta C, Sleight P. Cardiovascular, cerebrovascular, and respiratory changes induced by different types of music in musicians and non-musicians: the importance of silence. Heart. 2006;92(4):445-452. doi: 10.1136/hrt.2005.064600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Uedo N, Ishikawa H, Morimoto K, Ishihara R, Narahara H, Akedo I, et al. Reduction in salivary cortisol level by music therapy during colonoscopic examination. Hepato-Gastroenterology. 2004;51(56):451-453. [PubMed] [Google Scholar]
- 13.Grocke DE, Wigram T. Receptive Methods in Music Therapy Techniques and Clinical Applications for Music Therapy Clinicians, educators, and students; 2007. [Google Scholar]
- 14.Mandel SE, Davis BA, Secic M. Effects of music therapy and music-assisted relaxation and imagery on health-related outcomes in diabetes education. Diabetes Educat. Jul-Aug 2013;39(4):568-581. doi: 10.1177/0145721713492216. [DOI] [PubMed] [Google Scholar]
- 15.Robb SL. Music assisted progressive muscle relaxation, progressive muscle relaxation, music listening, and silence: A comparison of relaxation techniques. J Music Ther. 2000;37(1):2-21. [DOI] [PubMed] [Google Scholar]
- 16.Robb SL, Nichols RJ, Rutan RL, Bishop BL, Parker JC. The effects of music assisted relaxation on preoperative anxiety. J Music Ther. 1995;32(1):2-21. [Google Scholar]
- 17.Warth M, Kessler J, Hillecke TK, Bardenheuer HJ. Music therapy in palliative care. Dtsch Arztebl Online. 2015;13112(46):788-794. doi: 10.3238/arztebl.2015.0788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nelson K, Adamek M, Kleiber C. Relaxation training and postoperative music therapy for adolescents undergoing spinal fusion surgery. Pain Manag Nurs. 2017;18(1):16-23. doi: 10.1016/j.pmn.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 19.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344-349. doi: 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 20.Robb SL, Hanson-Abromeit D, May L, et al. Reporting quality of music intervention research in healthcare: A systematic review. Compl Ther Med. 2018;38:24-41. doi: 10.1016/j.ctim.2018.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder. Arch Intern Med. May 22 2006;166(10):1092-1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 22.Cohen S, Williamson GM. Perceived stress in a probability sample of the United States. In: S Spacapan, S Oskamp, eds The social psychology of health. Thousand Oaks, CA: Sage Publications; 1988:31-67. [Google Scholar]
- 23.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)-A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inf. 2009;42(2):377-381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inf. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mondanaro JF, Homel P, Lonner B, Shepp J, Lichtensztein M, Loewy JV. Music therapy increases comfort and reduces pain in patients recovering from spine surgery. Am J Orthoped. Jan/Feb 2017;46(1):E13-E22. [PubMed] [Google Scholar]
- 26.Goldenberg RB. Singing lessons for respiratory health: A literature review. J Voice. 2018;32(1):85-94. doi: 10.1016/j.jvoice.2017.03.021. [DOI] [PubMed] [Google Scholar]
- 27.Bailey LM. The Effects of Live Music versus Tape-Recorded Music on Hospitalized Cancer Patients. Music Ther. 1983;3(1):17-28. [Google Scholar]
- 28.Bradt J, Potvin N, Kesslick A, et al. The impact of music therapy versus music medicine on psychological outcomes and pain in cancer patients: a mixed methods study. Support Care Cancer. May 2015;23(5):1261-1271. doi: 10.1007/s00520-014-2478-7. [DOI] [PubMed] [Google Scholar]
- 29.Kirshblum S. New rehabilitation interventions in spinal cord injury. J Spinal Cord Med. 2004;27(4):342-350. doi: 10.1080/10790268.2004.11753772. [DOI] [PubMed] [Google Scholar]
- 30.Barksdale AL. Music Therapy and Leisure for Persons with Disabilities. Sagamore Pub.; 2003. [Google Scholar]
- 31.Walworth DD. Effect of live music therapy for patients undergoing magnetic resonance imaging. J Music Ther. 2010;47(4):335-350. [DOI] [PubMed] [Google Scholar]
- 32.Lee B, Nantais T. Use of electronic music as an occupational therapy modality in spinal cord injury rehabilitation: an occupational performance model. Am J Occup Ther. 1996;50(5):362-369. doi: 10.5014/ajot.50.5.362. [DOI] [PubMed] [Google Scholar]
- 33.Bashiri M, Akcali D, Akcali D, et al. Evaluation of pain and patient satisfaction by music therapy in patients with endoscopy/colonoscopy. Turk J Gastroenterol. 2018;29(5):574-579. doi: 10.5152/tjg.2018.18200. [DOI] [PMC free article] [PubMed] [Google Scholar]