Abstract
Mucopolysaccharidosis (MPS) syndrome is an inherited metabolic disorder. In more than half of the patients with MPS syndrome, heart valve involvement is reported; however, combined aortic and mitral valve stenosis in MPS syndrome type I-S is very rare. We describe a 39-year-old man with severe mitral and aortic valve stenosis due to MPS syndrome type I-S. Transthoracic and transesophageal echocardiography revealed severe thickening and calcification in the aortic and mitral valves with severe left ventricular hypertrophy. The coronary arteries were normal in angiography.
Key Words: Mucopolysaccharidosis I, Mitral valve stenosis, Aortic valve stenosis, Heart valve diseases
Introduction
Mucopolysaccharidosis (MPS) syndrome is a hereditary disorder of proteoglycan-degrading enzymes,1 resulting in the lysosomal accumulation of sulfated glycosaminoglycans (GAGs) in many tissues.
Based on biochemical, clinical, and genetic aspects, 9 subtypes are defined for MPS syndrome. Cardiac involvement has been reported as a common and early feature of MPS syndrome subtypes I, II, and VI.2 Cardiac involvement is present in 50% to 76% of patients with Scheie syndrome. The mitral valve is the most commonly involved valve (42% clinically symptomatic), followed by the aortic valve (20%). A combination of mitral and aortic valve lesions associated with MPS syndrome type I-S (a mild form of MPS syndrome I) is very rare.3, 4
Case Report
A 39-year-old man presented with a history of fatigue and dyspnea of 4 years’ duration. In the patient’s past medical history, based on clinical features such as joint stiffness, corneal opacity, hepatosplenomegaly, the urinary excretion of MPS, and positive family history, MPS syndrome type I-S had been confirmed when he was 20. Skeletal deformities such as thoracolumbar kyphosis, pigeon chest, and joint stiffness had occurred progressively since he was 7 years old.
One year before his referral to us, he lost his visual perception in the right eye. He was short (150 cm), and his left eye was hyperopic. He was of normal intelligence and had a university degree.
The first echocardiography (about 5 years earlier) revealed moderate mitral valve stenosis, based on which his cardiologist recommended medical treatment and yearly echocardiographic evaluations.
Despite medical treatment, the patient’s symptoms exacerbated and he experienced several episodes of syncope due to ventricular fibrillation, which resulted in multiple coronary care unit admissions during the year prior to his referral.
The patient was referred to Tehran Heart Center for further evaluation. Electrocardiographic findings revealed normal sinus rhythm with the right bundle branch block. On physical examination, the notable findings were short stature, claudication, and joint stiffness. Auscultation of the heart revealed diastolic rumbles in the apex and systolic ejection murmurs at the aortic area with early diastolic murmurs.
Two-dimensional (2D) transthoracic and transesophageal echocardiography demonstrated a non-dilated, albeit concentrically hypertrophied, left ventricle with normal global and segmental systolic function (ejection fraction = 55%).
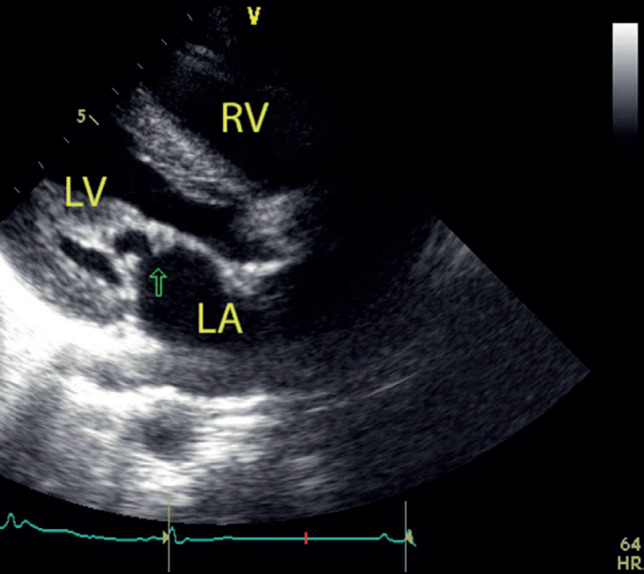
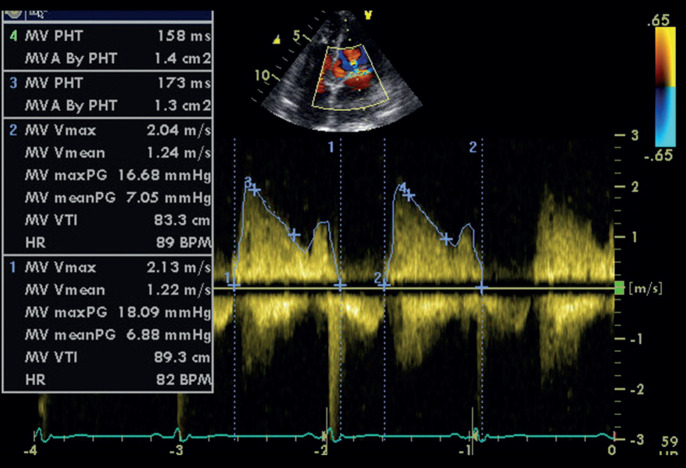
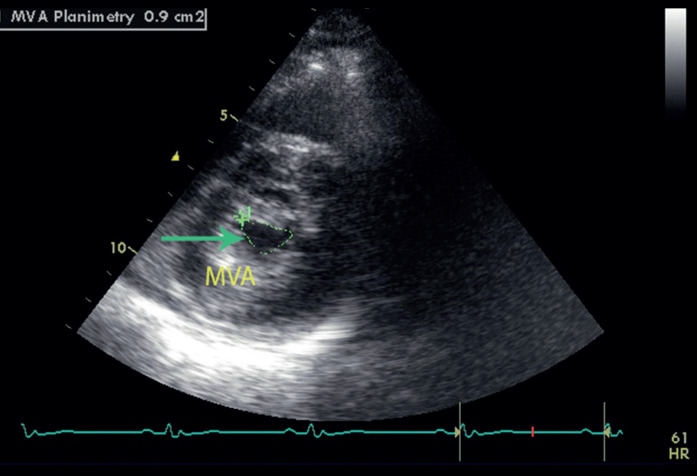
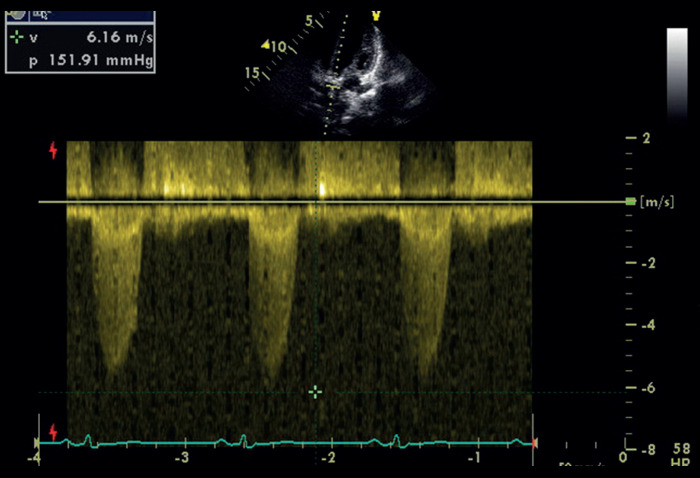
Transthoracic echocardiography showed that the left atrium was mildly dilated without any clot. Both mitral leaflets were very thick (Figure 1) with severe stenosis (mean diastolic gradient = 7 mmHg and peak diastolic gradient =17 mmHg) (Figure 2), and there was mild regurgitation. The mitral valve area was 0.9 cm² via planimetry (Figure 3) with a score of 10 to 11. The aortic valve was severely thick and stenotic (peak systolic gradient = 152 mmHg and mean systolic gradient = 85 mmHg) (Figure 4) with moderately severe regurgitation. According to 2D transesophageal echocardiography, the aortic valve area was 0.8 cm² via the continuity equation method and 0.7 cm2 via the direct planimetry method (Figure 5). Additionally, the annulus was 18 mm in diameter. Further, the right ventricle was normal in size and function, the tricuspid valve had trivial regurgitation, and pulmonary artery pressure was 40 mmHg.
Figure 1.
Transthoracic echocardiography (parasternal long-axis view) shows LV hypertrophy and the involvement of the mitral leaflets (arrow) and the subvalvular apparatus by deposits in a patient with mucopolysaccharidosis syndrome type I-S.
RV, Right ventricle; LV, Left ventricle; LA, Left atrium
Figure 2.
Transthoracic echocardiography (apical 4-chamber view) by continuous-wave Doppler shows a mean mitral valve gradient of 7 mmHg and a mitral valve area of 1.3 cm2 via the pressure half-time method.
Figure 3.
Transthoracic echocardiography (short-axis view) shows an MVA of 0.9 cm2 (arrow) via the planimetry method.
MVA, Mitral valve area
Figure 4.
Transthoracic echocardiography (apical 5-chamber view) by continuous-wave Doppler shows a peak aortic valve gradient of 152 mmHg.
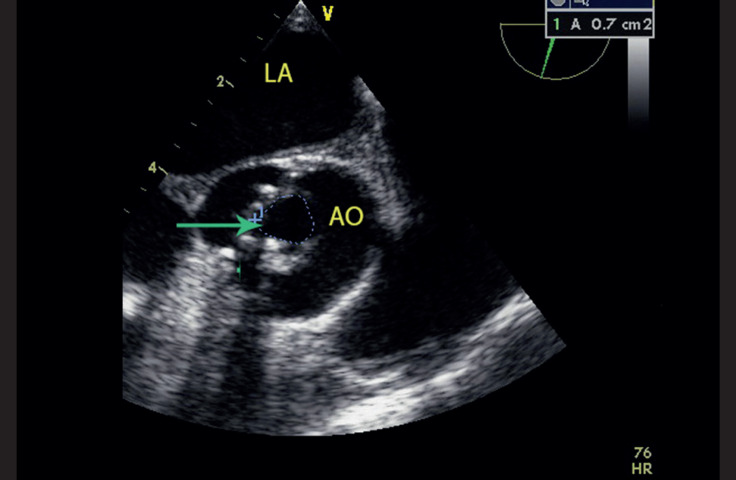
Figure 5.
Transesophageal echocardiography (short-axis view) shows an aortic valve area of 0.7 cm2 (arrow) via the direct planimetry method.
Coronary angiography revealed normal findings, and pressure gradients, measured through cardiac catheterization, confirmed the echocardiography-based diagnosis.
Aortic and mitral valve replacement, postoperative reevaluation for syncope, and implantable cardioverter-defibrillator implantation, if needed, were recommended.
Discussion
MPS syndrome is a heterogeneous group of inheritable storage diseases due to lysosomal enzyme deficiencies, which destroy GAGs. Enzyme deficiency results in the tissue accumulation and excessive urinary excretion of GAGs, various degrees of progressive mental and physical deterioration, and premature death in severe forms. In MPS syndrome type-I, as an autosomal recessive disorder, acid hydrolase-α-l-iduronidase deficiency leads to the intracellular accumulation of heparan sulfate and dermatan sulfate, a hallmark of MPS syndrome type-I.5 Scheie syndrome or MPS syndrome type I-S is characterized by joint stiffness, cardiac disease, and corneal clouding.6 Other clinical manifestations of Scheie syndrome are short stature, short neck, claw hands, and special features such as a high forehead, a flat nasal bridge, and skeletal and joint malformations. A diagnostic point for MPS syndrome type I-S (in contrast to MPS syndrome type I-H) is normal intelligence and behavior in these patients.1, 3
Yearly echocardiographic evaluations in patients with MPS syndrome are recommended.7 The main heart disease in MPS syndrome is valvular abnormalities, which occur at a young age8 and most commonly affect the mitral valve, followed by the tricuspid and aortic valves. Reports on combined aortic and mitral valve stenosis are very rare.3, 4 Valve dysfunction includes valve fibrosis, calcification, and thickening due to GAGs accumulation.3 Meanwhile, lysosomal GAG deposits in the myocardium lead to myocardial hypertrophy and subsequently diastolic dysfunction.1
Based on autopsy reports, coronary artery disease has also been described in patients with MPS syndrome.7 In our case, coronary angiography revealed normal coronary arteries.
Because of irregular valve structure due to GAG accumulation, patients with significant left-sided heart valve disease require surgical valve replacement.3
Conclusion
Our patient was an adult man, a known case of MPS syndrome type I-S with the clinical manifestations of Scheie syndrome, who presented with severe left heart valve involvement (aortic and mitral stenosis) and was candidated for surgery.
Notes:
This paper should be cited as: Combined Aortic and Mitral Valve Stenosis in Mucopolysaccharidosis Syndrome Type I-S: A Report of a Rare Case. J Teh Univ Heart Ctr 2021;16(1):31-33.
References
- 1.Kitabayashi K, Matsumiya G, Ichikawa H, Matsue H, Shimamura K, Sawa Y. Surgical treatment for mitral stenosis in Scheie's syndrome: mucopolysaccharidosis type I-S. Ann Thorac Surg. 2007;84:654–655. doi: 10.1016/j.athoracsur.2007.03.042. [DOI] [PubMed] [Google Scholar]
- 2.Leal GN, de Paula AC, Leone C, Kim CA. Echocardiographic study of paediatric patients with mucopolysaccharidosis. Cardiol Young. 2010;20:254–261. doi: 10.1017/S104795110999062X. [DOI] [PubMed] [Google Scholar]
- 3.Butman SM, Karl L, Copeland JG. Combined aortic and mitral valve replacement in an adult with Scheie's disease. Chest. 1989;96:209–210. doi: 10.1378/chest.96.1.209. [DOI] [PubMed] [Google Scholar]
- 4.Fischer TA, Lehr HA, Nixdorff U, Meyer J. Combined aortic and mitral stenosis in mucopolysaccharidosis type I-S (Ullrich-Scheie syndrome) Heart. 1999;81:97–99. doi: 10.1136/hrt.81.1.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ellinwood NM, Colle MA, Weil MA, Casal ML, Vite CH, Wiemelt S, Hasson CW, O'Malley TM, He X, Prociuk U, Verot L, Melniczek JR, Lannon A, Aguirre GD, Knox VW, Evans SM, Vanier MT, Schuchman EH, Walkley SU, Haskins ME. Bone marrow transplantation for feline mucopolysaccharidosis I. Mol Genet Metab. 2007;91:239–250. doi: 10.1016/j.ymgme.2007.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beck M, Arn P, Giugliani R, Muenzer J, Okuyama T, Taylor J, Fallet S. The natural history of MPS I: global perspectives from the MPS I Registry. Genet Med. 2014;16:759–765. doi: 10.1038/gim.2014.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Giugliani R, Federhen A, Rojas MV, Vieira T, Artigalás O, Pinto LL, Azevedo AC, Acosta A, Bonfim C, Lourenço CM, Kim CA, Horovitz D, Bonfim D, Norato D, Marinho D, Palhares D, Santos ES, Ribeiro E, Valadares E, Guarany F, de Lucca GR, Pimentel H, de Souza IN, Correa J Sr, Fraga JC, Goes JE, Cabral JM, Simionato J, Llerena J, Jr , Jardim L, Giuliani L, da Silva LC, Santos ML, Moreira MA, Kerstenetzky M, Ribeiro M, Ruas N, Barrios P, Aranda P, Honjo R, Boy R, Costa R, Souza C, Alcantara FF, Avilla SG, Fagondes S, Martins AM. Mucopolysaccharidosis I, II, and VI: brief review and guidelines for treatment. Genet Mol Biol. 2010;33:589–604. doi: 10.1590/S1415-47572010005000093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sugiura K, Kubo T, Ochi Y, Baba Y, Hirota T, Yamasaki N, Kitaoka H. Cardiac manifestations and effects of enzyme replacement therapy for over 10 years in adults with the attenuated form of mucopolysaccharidosis type I. Mol Genet Metab Rep. 2020;25:100662. doi: 10.1016/j.ymgmr.2020.100662. [DOI] [PMC free article] [PubMed] [Google Scholar]