Abstract
Objective:
Little is understood about the mechanisms for improving the adoption and implementation of Total Worker Health® (TWH) in workplace settings. The primary objective of this study was to identify whether the delivery of TWH advising is associated with subsequent changes in TWH in small-to-medium sized businesses.
Methods:
We conducted a longitudinal study of a TWH intervention in 200 organizations completing Health Links Healthy Workplace Assessments™ between October 2016 and December 2019. Organizations were offered consultation via telephonic and live web-based advising sessions.
Results:
Organizations exhibited non-significant albeit positive change in assessment scores from baseline to assessment 2. Businesses receiving advising showed significant score improvements from assessment 2 to 3, versus those without advising.
Conclusions:
TWH consultation may enhance adoption of organizational behaviors that promote worker health, safety, and well-being over time.
Keywords: Total Worker Health, Employee Well-being, Occupational Safety and Health, Small Business, Employer Health Promotion, Organizational Leadership, Dissemination and Implementation
Introduction
While workplace safety remains its primary goal, the Total Worker Health® (TWH) model for occupational safety and health (OSH) practice extends the scope of the OSH professions to incorporate a more holistic approach to include promoting worker health and well-being.1,2 TWH builds on the recognition that work is a social determinant of health and that work-related factors such as workload, job stress, social interactions, and access to employer-sponsored benefits all have an impact on the health and well-being of workers, their families, organizations, and communities.3 The TWH approach specifically emphasizes the priority of improving physical, organizational, and psychosocial factors in the work environment.2 TWH researchers have determined that key organizational elements, such as leadership support culture, employee participation, and communication, are linked to positive business and worker outcomes as well as with high levels of health and safety integration.4,5 Although there have been few studies of TWH in small and mid-sized businesses, there is evidence that these employers are motivated to implement health and safety programs for workers, but very often lack the time, knowledge and financial resources to get started and to sustain efforts.6,7 Attention to the value that health and safety play in every business is growing, and as a result, organizations and business leaders are increasingly seeking support and guidance to identify priorities and strategies that align with TWH principles.6
The U.S. business landscape is composed of firms of all sizes, industry sectors, and locales. Small businesses make up the largest proportion of enterprises, employ nearly half of American workers, and can be expected to create the largest number of jobs. In 2019, there were 30.7 million small businesses in the U.S. defined by the Small Business Administration as less than 500 employees, employing nearly 60 million people. Organizations with fewer than 100 employees contributed the largest share of small business employment.8 Emerging evidence has found that leadership support in small businesses is associated with higher levels of health and safety climate.9 Previous studies have shown that small business leaders care about the health of their employees but may lack the knowledge and skills to successfully implement TWH.10 Our research suggests that dissemination and implementation research on ways of implementing TWH interventions is needed, if we expect to see widespread adoption in the small business sectors of the economy.6,9,11
In 2015, the National Institutes of Health (NIH) hosted the Pathways to Prevention Workshop as part of a larger systematic review to inform a research agenda focused on TWH. Findings from the workshop addressed key questions around the benefits and harms, effectiveness, contextual factors of TWH interventions.2 Determining what types of TWH interventions best help create positive organizational change have suggested the need for greater focus on TWH dissemination and implementation research. NIOSH, for example, offers employers many “do-it-yourself” TWH resources.12 The NIOSH Total Worker Health Affiliates group is comprised of predominately large corporations that have implemented elements of TWH on their own, with little guidance or systematic research on effectiveness.12 However, given the breadth and complexity of their needs, it is not surprising that we have observed an emerging number of organizations, especially small and medium sized enterprises, that want to work with consultants who can guide them in the adoption of evidence-based TWH principles and practices.13–15 In addition to the ongoing need to promote safety, organizations that seek to adopt a TWH framework are requesting specific guidance and advice on the integration of worker health and well-being elements including, but not limited to, improved safety programs, wellness programs, chronic disease management, employee benefits, and leadership training for promotion of safety and health climates.6,13
Occupational safety consultation services have been shown to be effective in reaching small businesses and providing specific services in industrial hygiene, ergonomics, engineering, and general safety. For example, the Occupational Safety and Health Administration (OSHA) On-Site Consultation Service aims to assist small businesses through the use of a worksheet to assess organizations and provide feedback on how to improve safety management systems.16 From a health promotion perspective, coaching has been largely applied by large employers and health plans for health promotion interventions.17 Compared to the long-established practices of wellness professionals and safety professionals, TWH consulting is a new, unproven strategy for businesses to adopt effective, scalable, and sustainable TWH programs.1 In fact, we are aware of no studies that have evaluated the merit of TWH consulting as a tool for those organizations that seek to adopt TWH interventions. The domain of TWH has expanded the multiplicity of factors that employers need to be prepared to address across working conditions, home and community life, and personal health behaviors which all contribute to employees’ risk of injury and disease.18 Our experience working with diverse small and medium-sized organizations suggested the need to conduct research on the dissemination of effective, scalable, and sustainable TWH interventions to address these factors.6
The primary objective of this study was to examine the contribution of TWH advising as an element of an implementation tool that targets TWH adoption by workplaces, Health Links™, a program launched by our TWH Center of Excellence to provide organizations with TWH assessment, certification, and advising.19 We hypothesized that the inclusion of TWH advising would result in subsequent changes in TWH policies and practices in small-to-medium sized businesses.
Intervention Elements
The Health Links program was built as a model for organizations to facilitate adoption and implementation of TWH strategies.6,14 Health Links was developed with input from stakeholder groups including business professionals, health and safety professionals, employees, and community partners representing public health and workers’ compensation. Health Links consists of three main components: an online organizational assessment, certification, and advising. The intervention takes a TWH approach to, 1) enhance the adoption of TWH evidence-based policies and practices, 2) accommodate the needs of many different types of businesses and workforces, 3) be feasible for small and mid-sized businesses to access and adopt, meaning inexpensive and not resource/time intensive, 4) be scalable to large numbers of businesses, 5) apply basic principles of organizational change management, and 6) generate metrics so that the program could be evaluated in five domains of the RE-AIM model: Reach, Efficacy, Adoption, Implementation and Maintenance of the intervention.20 The program is utilized by organizations representing private, non-profit, and governmental agencies across a range of industries.
Core Components
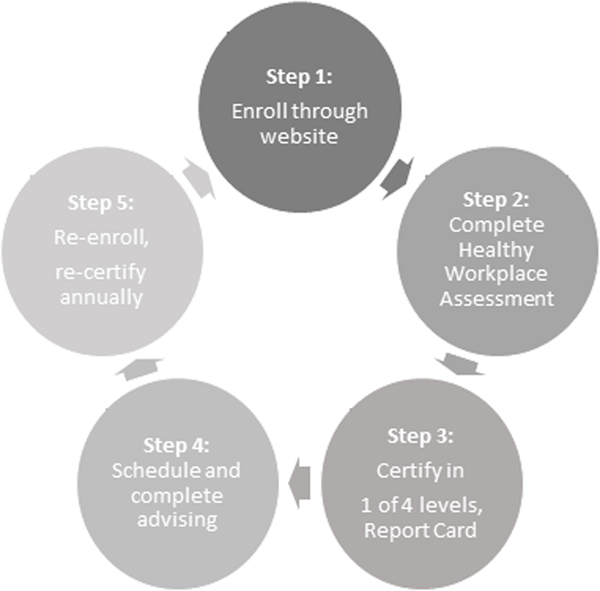
The core components that we studied were 1) the completion of the Health Links Healthy Workplace Assessment™ and 2) business advising over a three-year period. The assessment covers six benchmarks around an organization’s organizational supports, workplace assessments, health policies and programs, safety policy and programs, engagement, and evaluation.6 Although advising was considered as a core component and was encouraged by our research team, not all businesses that completed the assessment completed an advising session. The process for enrollment is illustrated in Figure 1. Participating businesses enrolled through the website by a designated representative from the organization.19 Throughout participation in Health Links, businesses had access to ‘My Dashboard’, an online portal that houses the Healthy Workplace Assessment. The portal also provides access to a report card that is generated based on the responses from the assessment to provide specific feedback and recommendations based on the business’s total and benchmark scores. After completing the assessment, businesses were recognized in one of four levels depending on their benchmark and overall scores: Kick-Start, Certified Healthy Workplace, Certified Healthy Workplace Partner, or Certified Healthy Workplace Leader. The person completing the assessment was then prompted to schedule advising through an online platform called Acuity Scheduling.21 After completing advising, organizations were provided an action plan, presented as a professional report, including the goals, a description of next steps to take, and links to resources for implementing goals. Businesses were provided links to download a formal certificate, badges for embedding and sharing, and open access to a resource center with evidence-based tools. Businesses also received announcements by email marketing, access to trainings and webinars, community resources, program enhancements, and events including annual awards. Businesses were prompted to reenroll every 12 months to update their assessment, to get certified, and to complete advising.
Figure 1.
The Health Links enrollment and employer engagement process.
Advising
Health Links advising sessions focused on reviewing results from the assessment, goal setting, and designing an action plan aimed at helping the business implement changes that addressed gaps and priority areas. Action plans were customized based on the priorities of the business, their employees’ needs for health and safety, and with consideration of weakest scores on the report card. Advising sessions were between 45–60 minutes. They followed a process for setting SMART goals that were matched to where the business scored lowest on the assessment. These goals were then incorporated into an action plan that was provided back to each business with the purpose of providing guidance through check-ins conducted by the advisor. Advisors were trained on core TWH components, the benchmarks, standard recommendations, and consulting skills for providing evidence-based recommendations. Principles of motivational interviewing were applied to the advising approach to probe specifics on organizational goals, barriers, and facilitators for TWH. The sessions were conducted with representatives from the businesses who were designated to be responsible for TWH. These people included a range of positions in the organizations including owners, human resource managers, health and safety professionals, and administrators. The core components of the Health Links advising we studied were completion of assessment and advising.
Methods
We conducted a longitudinal study of Health Links. Organizations were included if they completed two or more Healthy Workplace Assessments between October 1, 2016 and December 31, 2019. Organizations self-selected to receive advising. Organizational level data were collected annually through the business completing/updating the assessment. Change in performance on a set of the six benchmarks and total score was compared before and after advising and assessed relative to businesses selecting not to receive advising.
Participants & Recruitment
The organizations included in this study participated in the Health Links program described above between October 1, 2016 and December 31, 2019. To be included in this study, organizations needed to have completed two or more annual assessments, including a baseline “initial” assessment, and up to two subsequent assessments. Figure 2 illustrates the number of businesses that completed the assessment and advising during the study period. We recruited businesses through outreach efforts, including email marketing, events, trainings, and channel partners. These groups included chambers of commerce, workers’ compensation insurers, local public health agencies, health and wellness coalitions, and trade associations. All participating organizations were offered assessment and advising. Businesses were eligible to participate if they 1) enrolled, 2) were an established company, non-profit, government agency or other type of organization, and 3) were operating in Colorado or Oregon. Businesses were offered different types of incentives to participate throughout the life of the program to date. These incentives included sponsored enrollment (i.e. no cost enrollment), eligibility for awards, and eligibility to receive funding from our “accelerator award program” to use towards workplace health and safety improvements.
Figure 2.
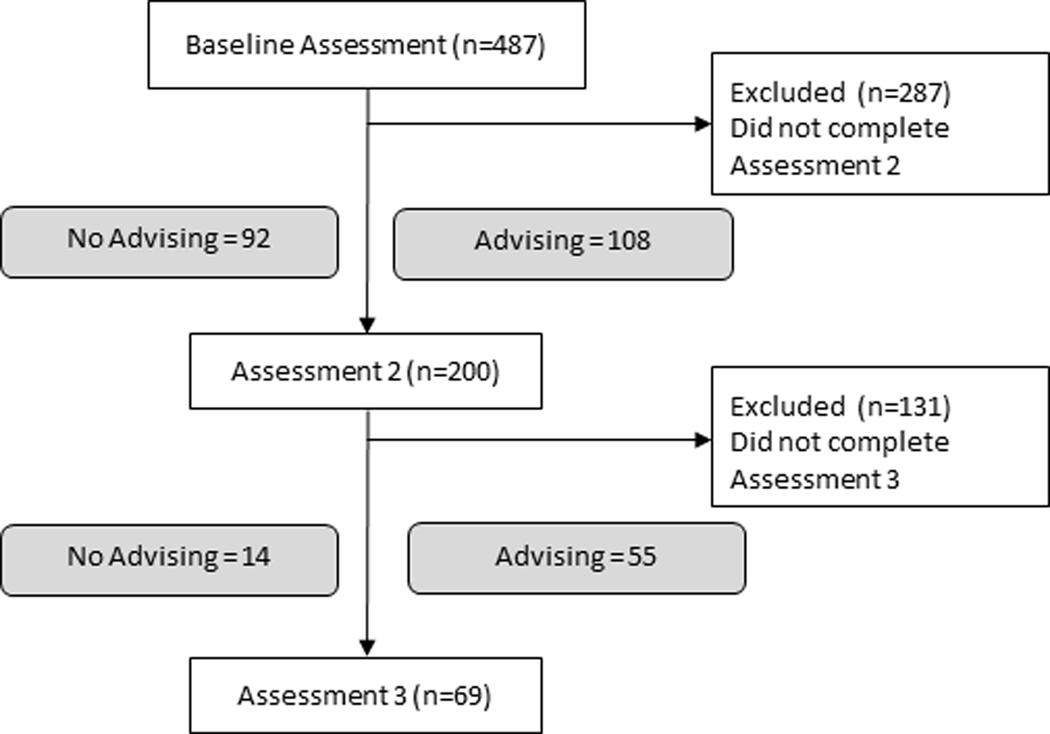
Flow diagram of number of businesses that completed the Healthy Workplace Assessment™ and advising at each timepoint.
Data Collection and Measures
For the purpose of this study, we utilized longitudinal data collected at the organizational level. One person from each business completed the online Healthy Workplace Assessment through the Health Links website – www.healthlinkscertified.org - with consensus from team members including health and safety team.19 The respondents represented individuals in senior leadership, management, human resources, health and safety, and administration. The assessment contained 35 questions and took approximately 30–60 minutes to complete. The tool was developed based on key principles distilled from the CDC Worksite Health ScoreCard,22 the NIOSH Total Worker Health® approach,23 and the WHO Healthy Workplace Framework.24 All items referred to the previous 12 months and were answered with a “yes” or “no” response. After completing the assessment, organizations were certified in one of four certification levels (Kick-Start, Certified, Partner or Leader).
The assessment scored organizations across six benchmarks to evaluate TWH strategies: 1) organizational support (30 maximum points), 2) workplace assessment (12 maximum points), 3) health policies and programs (16 maximum points), 4) safety policies and programs (16 maximum points), 5) engagement (16 maximum points), and 6) evaluation (10 maximum points).6 We calculated a total score (100 maximum points), which represented a sum of all benchmark scores. Employer demographics such as size, industry and employee age groups were also collected from the assessment. The questionnaire collected information on how businesses are implementing health and safety through workplace policies, education, leadership and management commitment, and in specific areas including tobacco control, stress, chronic disease prevention, mental health, ergonomics, and emergency preparedness. Questions asked in each benchmark measured policies and practices that were being implemented at the organization at the time. An example question for organizational support is, “In the last 12 months, what resources have you dedicated to workplace health and safety?”
The 200 businesses that are included in the study completed an initial assessment (baseline) plus at least one follow-up assessment approximately 1 year later (assessment 2). Out of the 200 businesses, 69 of them completed a third assessment (assessment 3) two years following baseline. There were 108 businesses (54%) that completed advising between baseline and assessment 2 and 55 businesses (80%) that completed advising between assessments 2 and 3.
Statistical Analyses
Our primary outcome variable of interest was the change in assessment total score between baseline and follow up assessments and the impact of advising on the change in total score. Preliminary analyses included Pearson chi-square test to evaluate differences in categorical certification levels and Student t-test (2-tailed) for comparison of mean assessment score data. To address if the receipt of advising by a business positively impacted a change in assessment score, we performed an analysis using linear mixed effects models. Specifically, these models included the change from baseline assessment to second, from second assessment to third, and from baseline to third assessment, with a positive change in score representing a favorable outcome. Random intercept for businesses were included to account for repeated measures. Analyses were first run to address the association between advising and total score change. Additional models were run to address the association between advising and each benchmark score change. To adjust for potential confounding by business size, all models were adjusted for size of business.
A secondary analysis of change in the six individual benchmark scores was performed to determine the effects of advising on each of the benchmark categories between assessments. Differences in the individual benchmark scores were determined as the difference in score between assessments as described for the total score change.
We further investigated the dose-response of advising on total score change by subsetting the data to organizations completing three Health Links Assessments and stratifying into the following four groups: 1) those with advising only after the baseline assessment, 2) those with advising only between assessments 2 and 3, 3) those receiving advising following baseline and assessment 2, 4) those businesses with no advising following any assessment. Analysis of variance was employed to assess the change in total score between the 4 groups of businesses, with a Bonferroni correction applied to reduce chance of Type I error.
Statistical analyses were performed using SAS version 9.4 (SAS Institute, Inc., Cary, North Carolina).25
Results
A total of 487 unique businesses completed Health Links Healthy Workplace Assessments between October 1, 2016 and December 31, 2019 with 287 organizations completing only one assessment, resulting in 200 businesses that completed two or more assessments and were eligible for this analysis. Of the 200 unique businesses in the cohort, 108 received advising following baseline (54%), while the remaining 92 did not receive advising (Figure 2). For those 69 businesses completing more than 2 assessments, 55 of these businesses received advising following assessment 2 (80%), with 65 of the 69 businesses receiving at least 1 advising session during the study period. Average time between baseline and assessment 2 was 11.3 months, compared to 12.7 months between assessments 2 and 3.
Seventy percent of the businesses in the study had fewer than 250 employees, a third (36%) had fewer than 50 employees. They represented both urban (68%) and rural (32%) regions in Colorado and Oregon (Table 1). Mean baseline scores were slightly different between groups completing 2 versus 3 assessments (p=0.054). Baseline scores for the 131 businesses completing 2 assessments averaged 51.1 points (95%CI: 47.69, 54.47) whereas a mean score of 56.9 points (95%CI: 51.83, 61.93) was observed for the 69 employers with 3 assessments.
Table 1.
Participating Employer Characteristics (October 2016 – December 2019)
| Number of businesses completing assessments (%) | ||
|---|---|---|
| Participating Employer Characteristics | Baseline and Assessment 2 (n=200) | Baseline, Assessment 2 and Assessment 3 (n=69) |
| Employer size (by employee number) | ||
| <10 | 18 (9.0) | 6 (8.7) |
| 10–49 | 53 (26.5) | 19 (27.5) |
| 50–99 | 29 (14.5) | 9 (13.0) |
| 100–249 | 41 (20.5) | 12 (17.4) |
| 250+ | 59 (29.5) | 23 (33.3) |
| Geographic region | ||
| Urban | 136 (68.0) | 46 (66.7) |
| Rural | 64 (32.0) | 23 (33.3) |
| Industry type | ||
| Accommodation & Food Service | 6 (3.0) | 2 (2.9) |
| Administration & Support & Waste Management | 1 (0.5) | 0 (0.0) |
| Agriculture, Forestry, Fishing and Hunting | 4 (2.0) | 1 (1.5) |
| Arts, Entertainment and Recreation | 2 (1.0) | 0 (0.0) |
| Construction | 10 (5.0) | 7 (10.1) |
| Educational Services | 18 (9.0) | 7 (10.1) |
| Finance and Insurance | 10 (5.0) | 2(2.9) |
| Health Care & Social Assistance | 37 (18.5) | 12 (17.4) |
| Information | 3 (1.5) | 0 (0.0) |
| Manufacturing | 20 (10.0) | 1 (1.5) |
| Public Administration | 23 (11.5) | 8 (11.6) |
| Real Estate & Rental & Leasing | 5 (2.5) | 1 (1.5) |
| Retail/Wholesale Trade | 2 (1.0) | 0 (0.0) |
| Transportation, Warehousing & Utilities | 6 (3.0) | 1 (1.5) |
| Other | 53 (26.5) | 27 (39.1) |
| Completed Advising | 108(54.0) | 55 (79.7) |
| Certification Level | ||
| Kickstart | 73 (36.5) | 18 (26.1) |
| Certified | 18 (9.0) | 4 (5.8) |
| Partner | 45 (22.5) | 17 (24.6) |
| Leader | 64 (32.0) | 30 (43.5) |
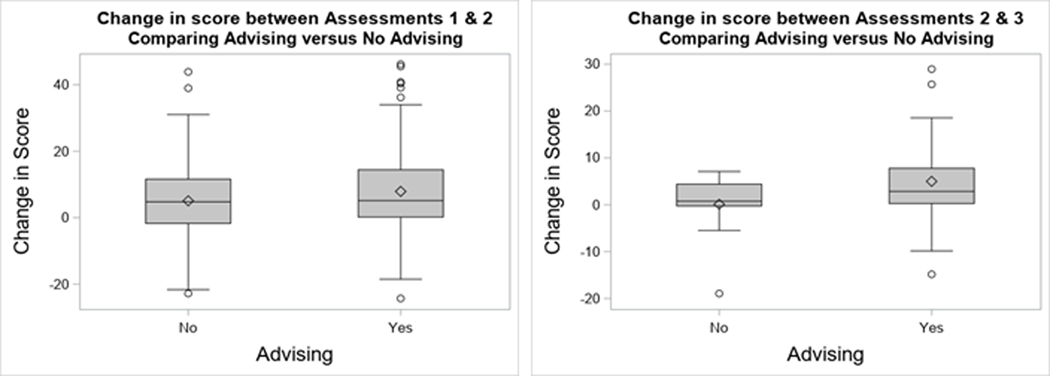
Assessment groups were dichotomized into business organizations receiving advising and those declining advising sessions between assessments. Mean score differences between assessments, comparing businesses with advising versus those with no advising, are presented in Figure 3.
Figure 3.
Mean score differences between baseline and assessment 2 (n=200) and assessments 2 and 3 (n=69) for businesses with advising or without advising.
Associations of Advising and Score Changes
Overall, a signal emerged to suggest that improvements in total assessment score were linked to advising completed regularly over time. A lesser signal was detected for the influence of limited advisement compared to no advisement. Advising seemed to make the most difference between assessments 2 and 3. Between the baseline and 2nd assessment, those businesses which received advising increased their total score an average of 2.4 points more than those that did not (95%CI: −0.97, 5.69), and businesses receiving any advisement increased their score from the first to the third assessment by 6.33 points more than those who received no advising (95%CI: −2.00, 14.66), albeit these findings were not statistically significant. Businesses that received no advising improved their scores between baseline and second assessment (95%CI: 2.49,7.67). However, among businesses that completed three assessments in total, businesses with advising between the 2nd and 3rd assessments displayed significant improvement in their third assessment scores, as compared to those without advising (Mean difference: 4.5 points, 95%CI: 0.115, 8.84). Among the 69 businesses without advising that completed the three assessments there was a decrease in total scores between 2nd and 3rd assessments and baseline and 3rd assessment timepoints. A summary of these results is found in Table 2.
Table 2.
Change in total assessment scores between baseline, second and third assessments comparing businesses receiving advising with businesses without advising.
| Change in Total Assessment Scores | Mean Score Change, no Advising (95% CI) | Mean Score Change, with Advising (95% CI) | Mean Score Difference (95% CI)* | p-value |
|---|---|---|---|---|
| Baseline v. Assessment 2 (n=200) | 5.08 (2.49, 7.67) | 7.92 (5.53, 10.30) | 2.36 (−0.97, 5.69) | 0.16 |
| Assessment 2 v. Assessment 3 (n=69) | 0.10 (−3.75, 3.95) | 4.99 (3.05, 6.93) | 4.48 (0.115, 8.84) | 0.05 |
| Baseline v. Assessment 3 (n=69) | 6.54 (−1.34, 14.42) | 12.14 (8.17, 16.11) | 6.33 (−2.00, 14.66) | 0.13 |
Mean score difference adjusted for size of business.
There was also a suggestion that advising improved scores across domains, but that Evaluation may have been particularly influenced. Businesses that received advising increased their benchmark scores between assessment 1 and assessment 2 more than those that did not receive advising for every benchmark except Evaluation, albeit these changes were not statistically significant (Table 3). For 4 of 6 benchmarks, the magnitude of score change between assessment 1 and assessment 2 was greater for those organizations that received advising than those that did not (Table 3). The greatest increase among businesses with advising was seen in the organizational supports benchmark (average increase of 3.2), followed by safety (average increase of 1.6). Evaluation was the only individual benchmark between assessment 2 and 3 that was statistically significant between advising vs. no advising, yet between assessment 1 and 2, the evaluation benchmark score was worse with advising vs. without advising.
Table 3.
Change in individual benchmark scores between assessments comparing businesses receiving advising versus businesses who did not receive advising.
| Benchmark | Mean score difference between baseline and assessment 2 (95% CI)* | Mean score difference between assessments 2 and 3 (95% CI)* | Mean score difference between baseline and assessment 3 (95% CI)* |
|---|---|---|---|
| Organizational Supports | 1.11 (−0.56, 2.78) | 1.07 (−0.87, 3.01) | 3.46 (−0.81, 7.72) |
| Workplace Assessment | 0.37 (−0.23, 0.97) | 0.80 (−0.11, 1.72) | 0.74 (−0.41, 1.90) |
| Healthy Programs/Policies | 0.57 (−0.16, 1.29) | 0.42 (−0.43, 1.27) | −0.11 (−1.74, 1.52) |
| Safety Programs/Policies | 0.34 (−0.38, 1.05) | 0.29 (−0.65, 1.23) | 1.05 (−0.85, 2.96) |
| Engagement | −0.003 (−0.66, 0.65) | 0.85 (−0.12, 1.81) | 0.62 (−1.06, 2.29) |
| Evaluation | −0.35 (−0.93, 0.23) | 0.76 (0.04, 1.47) | 0.66 (−0.78, 2.09) |
Mean score difference adjusted for size of business.
Dose-Response of Advising on Total Score Changes
Of the 69 businesses that completed three assessments, 65 (94%) received at least one advising session (Table 4). Only four businesses that completed all three assessments declined any advising. Businesses that received advising at least once showed an increased total score between assessments 2 and 3, and baseline to 3 whereas those with no advising on average experienced no change. There were no statistically significant differences between the groups of advising vs. no advising or between assessments.
Table 4.
Mean score changes between assessments, grouped by those businesses receiving or not receiving advising post-assessment.
| Advising 1 | Advising 2 | Change between baseline and assessment 2 (95% CI) | Number of Businesses (n=200) | Change between assessments 2 and 3 (95% CI) | Number of Businesses (n=69) | Change between baseline and assessment 3 (95% CI) | Number of Businesses (n=69) |
|---|---|---|---|---|---|---|---|
| Yes | Yes | 7.53 (4.32, 10.74) | 78 | 4.78 (2.88, 6.68) | 44 | 11.97 (7.39, 16.55) | 44 |
| Yes | No | 8.91 (4.85, 12.97) | 30 | 1.26 (−1.34, 3.86) | 10 | 9.43 (−0.27, 19.12) | 10 |
| No | No | 4.60 (1.56, 7.65) | 67 | −2.81 (−20.68, 15.05) | 4 | −0.67 (−17.99, 16.64) | 4 |
| No | Yes | 6.36 (−0.41, 13.13) | 25 | 5.83 (−1.68, 13.34) | 11 | 12.81 (2.09, 23.53) | 11 |
Discussion
This study provides direction to our hypothesis that advising is a signal for improvements in the adoption of TWH organizational policies and practices. As the first study to evaluate a TWH advising intervention, the study highlights differences between improvements among different groups of program engagement which included assessments and advising over time. Our results show that the more dedicated group of businesses performed better than the initial sample. Businesses with the largest increases in total and assessment benchmark scores, although not statistically significant, were those that participated in advising, with the stronger signal of advising shown in the smaller sample of those businesses that completed all three assessments and advising. Our results indicate that businesses received some value from advising between baseline and the assessment 3 as measured by the largest score changes between the 24-month time period and that businesses that received no advising during those same periods had decreased scores. Businesses that received a higher dose of advising received the most value of TWH improvements between assessments 2 and 3.
As far as the association between advising and the magnitude of TWH changes implemented in participating businesses, our results suggest that there is a range of readiness to change that may impact when and how organizations receiving advising apply recommendations. Some businesses made greater changes between baseline and assessment 2 and others made more significant changes between assessments 2 and 3. With businesses improving more in the first year compared to the second round of advising, we illustrate that the impact of a TWH intervention like Health Links may be greater in the early stages of implementation when businesses have more to gain from the initial technical advice/consultation. These findings also indicate that TWH advising can continue to benefit businesses. This speaks to the potential role TWH consulting may play in the maintenance of policies and practices in organizations.
The focus of this study is on the effect of TWH advising. Although our central hypothesis and study approach were not designed to evaluate the effect of Health Links on TWH benchmark improvements, it is worth noting that participating businesses demonstrated improvements in four out of the six benchmarks. A formal test of Health Link’s impact on assessment scores will require future research that includes a referent group that has not participated in the program. Importantly, although there were no statistically significant differences in benchmark score changes between advising vs. no advising, the confidence intervals for each support a strong association between mean score changes and advising. Further research is needed to understand how businesses implement action plans to determine if the changes in assessment scores can be directly linked to the goals made in advising. Specifically, our findings show that scores in health policies and programs decreased between baseline and the 3rd assessment which warrants an area of further assessment in relation to how advising may impact changes in businesses and whether those changes are a positive or negative benefit to the organization and employees. It is possible that in some cases, advising leads to focusing on reducing the number of activities to focus on higher employee engagement or more targeted interventions addressing high need workplace health and safety efforts.
It is important to note that baseline assessment scores were significantly different between those businesses that completed 2 vs. 3 assessments. This may imply that those with more TWH practices at the start were more likely to proactively stay engaged and participate in advising. The businesses that received advising from first to third assessments showed an average of 6.33 points higher overall scores from the first to the third assessment than those who received no advising. To explore this possibility further, we conducted a post hoc analysis of the differences observed between the businesses that did not meet study inclusion criteria (single assessment) versus the sample that completed two or more assessments during the two-year period. The data suggest that there may differences of motivation between the two groups. There was a small proportion of businesses that completed two or more assessments which were recognized as Kick-Start (the lowest level of Health Links Certification) compared to the employer group that was excluded from the study (p=<0.0001). The businesses that have been recognized at the higher certification levels, i.e. Partner or Leader levels, were more likely to have met study entry criteria, suggesting higher engagement. Anecdotally, businesses that remain with Health Links for multiple years start to assign a dedicated staff person or team for TWH implementation, provide more resources (time, budget, services), and display explicit leadership support for ongoing participation in Health Links.
We acknowledge a number of study strengths and limitations. The Health Links model was developed as a multipronged approach to help employers assess, adopt, and implement TWH best practices. Our results show that not only are businesses of different sizes representing multiple industries motivated and committed to TWH, they are willing to actively participate in a TWH intervention that involves a form of consulting over multiple years. Previous studies have demonstrated the differences between business size and TWH adoption.6 This is the first study to evaluate a TWH consulting model and associations with changes to TWH policies and programs across different groups of program engagement. It also consists of a large cohort of businesses across two states (Colorado and Oregon) representing multiple industries and sizes, suggesting a degree of generalizability. Our results provide the support for future research in the field of TWH dissemination and implementation science to identify strategies for integrating evidence-based strategies into TWH interventions to test effectiveness and maintenance. Importantly, the Health Links model demonstrates the role consulting will serve in the adoption of TWH by providing the technical support to help businesses implement and evaluate workplace policies and strategies. The TWH intervention studied was designed as a “package” that other consultants could offer to businesses. Importantly, it was implemented in a way where advisors were trained on the same approach with standard recommendations to pull from, prioritized with mapping them to the benchmarks where businesses had room for most improvement. This study demonstrates the range of changes to TWH practice one could expect from this “TWH consultation package” across 200 heterogeneous small to mid-size businesses.
One limitation is that we included only those businesses (n=200) that had completed two or more assessments in the time frame of the study. To examine the potential for selection bias, we analyzed baseline mean assessment scores for all businesses at baseline (n=487) and determined that our study group did not significantly differ from those who were excluded from the study. It is possible that the use of incentives may have influenced participation and engagement rate. Based on our program evaluation, we have found higher retention among businesses that have not received an incentive to participate, suggesting those that completed more assessments in this study are more committed to TWH intrinsically. We recognize there may have been response bias due to using a self-response survey. We attempted to control for this by validating responses during advising sessions. In a very few cases, respondents actually underreported TWH activities due to lack of clarity concerning definitions and terminology used in the assessment. In these cases, the response was corrected on the current assessment to reflect a true response. While we did not have an assigned control group, we were able to treat those businesses that completed the Assessment and received no advising as a comparison group to measure differences between advising and no advising. It is a limitation that we adjusted for size of business but could not adjust for other factors that differed between studies that did/did not receive advising. We also recognize that businesses may have been engaging in efforts aside from advising that would impact changes to TWH reflected by assessment scores. This has been observed in studies where attrition in workplace interventions has been associated with businesses wanting more than what the intervention offers.26 The tracking of the time lag between advising sessions for each business was limited for the first half of the study period, making it more difficult for us to measure time to event as a cofounder or covariate of change. We also did not evaluate advising quality which could be a potential influence on the applicability of the findings.
The future for scaling up TWH depends on identifying approaches that are effective in strengthening organizational support; leadership; health promotion for addressing stress, chronic disease, fatigue, and mental health; safety; employee engagement; and evaluation. Due to the diverse nature of small business organizations and their workforces, these approaches need to be flexible in identifying TWH strategies that meet the goals, values and needs of each. Future research is needed to better understand how advising is being implemented and to understand why businesses choose to pursue advising or not. One opportunity is to evaluate the impact of action plans and goal setting on score changes to assess whether businesses implement what they learn in advisement sessions and their rationale for either adopting or not adopting recommendations from advisors. It would also be valuable to identify specific motivations and barriers to program engagement to tailor outreach and dissemination strategies that aid retention and program evaluation. Ongoing research is also being conducted to link TWH changes measured by the Healthy Workplace Assessment to changes in employee perceptions of health and safety climate.
Conclusions
Total Worker Health consultation that includes one-on-one advising enhances the adoption of organizational behaviors that promote worker health, safety, and well-being. A subset of particularly engaged businesses that completed advising and assessments over 2 years demonstrated improved TWH compared to those that didn’t receive advising. Future TWH interventions should consider developing and testing consultation models to provide different levels of technical assistance, practical guidance, and tools tailored to small business.
Acknowledgments
Funding Sources: This publication was supported by Cooperative Agreement number, 1 U19 OH 011227, funded by the Centers for Disease Control and Prevention. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention or the Department of Health and Human Services.
Footnotes
Conflict of Interest: None Declared
Ethical considerations and disclosures: This evaluation was determined to be non-human subjects research by the Colorado Multiple Institutional Review Board and was approved for exemption.
References
- 1.Newman LS, Scott JG, Childress A, et al. Education and Training to Build Capacity in Total Worker Health®: Proposed Competencies for an Emerging Field. J Occup Environ Med. 2020;62(8):e384–e391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tamers SL, Goetzel R, Kelly KM, et al. Research Methodologies for Total Worker Health®: Proceedings From a Workshop. J Occup Environ Med. 2018;60(11):968–978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tamers SL, Chosewood LC, Childress A, Hudson H, Nigam J, Chang CC. Total Worker Health(®) 2014⁻2018: The Novel Approach to Worker Safety, Health, and Well-Being Evolves. Int J Environ Res Public Health. 2019;16(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McLellan DL, Williams JA, Katz JN, et al. Key Organizational Characteristics for Integrated Approaches to Protect and Promote Worker Health in Smaller Enterprises. J Occup Environ Med. 2017;59(3):289–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sorensen G, McLellan D, Sabbath E, et al. Integrating worksite health protection and health promotion: A conceptual model for intervention and research. Preventative Medicine. 2016;91:188–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tenney L, Fan W, Dally M, et al. Health links™ assessment of total worker health® practices as indicators of organizational behavior in small business. J Occup Environ Med. 2019;61(8):623–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McCoy K, Stinson K, Scott K, Tenney L, Newman LS. Health promotion in small business: a systematic review of factors influencing adoption and effectiveness of worksite wellness programs. J Occup Environ Med. 2014;56(6):579–587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.U.S. Small Business Administration Office of Advocacy. United States Small Business Profile [SBA web site]. 2016. Available at: https://www.sba.gov/sites/default/files/advocacy/United_States.pdf. Accessed August 30, 2018.
- 9.Schwatka NV, Dally M, Tenney L, Shore E, Brown CE, Newman LS. Total Worker Health Leadership and Business Strategies Are Related to Safety and Health Climates in Small Business. Int J Environ Res Public Health. 2020;17(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thompson J, Schwatka NV, Tenney L, Newman LS. Total Worker Health: A Small Business Leader Perspective. Int J Environ Res Public Health. 2018;15(11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schwatka NV, Tenney L, Newman LS. Health protection and health promotion in small business. In: Burke RJ, Richardson AM, eds. Increasing Occupational Health and Safety in Workplaces. Northampton, MA: Edgar Elgar Publishing Limited; 2019:371–392. [Google Scholar]
- 12.Centers for Disease Control and Prevention - National Institute for Occupational Safety and Health. Total Worker Health, Promising Practices from Employers [CDC/NIOSH web site]. 2019. Available at: https://www.cdc.gov/niosh/twh/practices.html. Accessed December 20, 2020.
- 13.Rohlman DS, Campo S, Hall J, Robinson EL, Kelly KM. What Could Total Worker Health® Look Like in Small Enterprises? Ann Work Expo Health. 2018;62(suppl_1):S34–s41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schwatka NV, Tenney L, Dally MJ, et al. Small business Total Worker Health: A conceptual and methodological approach to facilitating organizational change. Occup Health Sci. 2018;2(1):25–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pronk NP, McLellan DL, McGrail MP, et al. Measurement Tools for Integrated Worker Health Protection and Promotion: Lessons Learned From the SafeWell Project. J Occup Environ Med. 2016;58(7):651–658. [DOI] [PubMed] [Google Scholar]
- 16.Autenrieth DA, Brazile WJ, Sandfort DR, Douphrate DI, Román-Muñiz IN, Reynolds SJ. The associations between occupational health and safety management system programming level and prior injury and illness rates in the US dairy industry. Safety science. 2016;84:108–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chapman LS, Lesch N, Baun MP. The role of health and wellness coaching in worksite health promotion. Am J Health Promot. 2007;21(6):suppl 1–10, iii. [DOI] [PubMed] [Google Scholar]
- 18.Punnett L, Cavallari JM, Henning RA, Nobrega S, Dugan AG, Cherniack MG. Defining ‘Integration’ for Total Worker Health®: A New Proposal. Ann Work Expo Health. 2020;64(3):223–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Health Links Certified [Health Links Certified web site] 2018. Available at: https://www.healthlinkscertified.org. Accessed March 15, 2020.
- 20.Glasgow RE, Harden SM, Gaglio B, et al. RE-AIM Planning and Evaluation Framework: Adapting to New Science and Practice With a 20-Year Review. Front Public Health. 2019;7:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Acuity Scheduling [Acuity web site] 2020. Available at: https://acuityscheduling.com/. Accessed March 15, 2020.
- 22.Centers for Disease Control and Prevention. Worksite Health ScoreCard [CDC web site]. 2018. Available at: https://www.cdc.gov/workplacehealthpromotion/initiatives/healthscorecard/index.html. Accessed August 30, 2018.
- 23.Centers for Disease Control and Prevention - National Institute for Occupational Safety and Health. NIOSH Total Worker Health® Program [CDC/NIOSH web site]. 2018. Available at: https://www.cdc.gov/niosh/TWH/. Accessed August 30, 2018.
- 24.World Health Organization. Healthy workplaces: a WHO global model for action [WHO web site]. 2018. Available at: http://www.who.int/occupational_health/healthy_workplaces/en/. Accessed August 30, 2018.
- 25.SAS Institute, Inc. [computer program]. Version 9.4. Cary, NC: SAS Institute, Inc.; 2016. [Google Scholar]
- 26.Newman LS, Stinson KE, Metcalf D, et al. Implementation of a worksite wellness program targeting small businesses: the Pinnacol Assurance health risk management study. J Occup Environ Med. 2015;57(1):14–21. [DOI] [PMC free article] [PubMed] [Google Scholar]