Abstract
Background:
Literature suggests that the presence of the current Bacillus Calmette Guerin (BCG) policy appears to mitigate COVID-19 disease burden but no information exists on the nature of the BCG strain and disease burden.
Objectives:
To study the association between type of BCG strain, BCG coverage (%), and COVID-19 disease burden.
Methodology:
An audit of global data on strains and disease burden was done. Country-specific data for COVID-19 cases and deaths, BCG-related data, and income level were obtained from the online databases, and the association was analyzed using linear regression.
Results:
Data of 139 countries were studied and 117 (84%) had a current BCG policy. Data on BCG strains were available for 51 countries and 18/51 (35%) used the Danish strain. While the choice of strain did not impact COVID-19-related disease burden, the presence of a current BCG policy was significantly associated with lower COVID-19 mortality.
Conclusion:
The presence of current BCG policy is associated with decreased COVID-19-related disease burden, but the type of strain used by a country in its vaccination program does not impact disease burden.
Keywords: HIC, lower middle income, vaccination policy
INTRODUCTION
The COVID-19 pandemic has seen differential morbidity and mortality worldwide and diverse Bacillus Calmette Guerin (BCG) national vaccination policies have been thought to contribute to this.[1] The use of BCG appears to protect from mortality to COVID-19 where BCG vaccination is part of the country's universal immunization program (UIP).[2] India, for example, continues to use the BCG vaccine as a part of its UIP and has seen fewer deaths relative to many other countries.[3] Many developed nations (Sweden, Spain) have withdrawn the BCG vaccine from their UIPs[3] and their mortality has been high.[1] While there is some controversy about its protection from tuberculosis, a number of beneficial (protective) effects against other infections including respiratory tract infections are known.[4] The vaccine is capable of inducing metabolic and epigenetic changes that boost the innate immune response, a mechanism known as trained immunity.[5,6]
BCG vaccination strains are classified into “early strains” and “late strains” based on their timing of distribution from the original source (before or after 1926).[2,6] Early strains (BCG Japan and BCG Russia) appear to be associated with lower COVID-19 mortality. BCG Denmark, which seems to induce less protection against COVID-19, is a late strain.[6] Unlike vaccination policy itself, there is limited data on the association of disease burdens with diverse BCG strains as well as nationwide BCG coverage (%) and this formed the objective of the present study.
METHODOLOGY
Source of data
Data on Universal BCG vaccination policies for different countries were collected from http://www.bcgatlas.org/[Last accessed on 24th May 2020].
Data collection
We collected information on (a) Current BCG policy (Yes/No); (b) The type of BCG strains used in UIP; (c) BCG recommendation type-ongoing/past policy/policy only for special groups; (d) Nation-wide BCG coverage; and (e) income group of country (based on World Bank data).[7] The data of COVID-19-related morbidity (number of cases) and mortality (number of deaths) for countries was collected from https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200507covid-19-sitrep-108.pdf?sfvrsn = 44cc8ed8_2 [accessed on 19th May 2020]. The world population data was collected from https://www.worldometers.info/world-population/population-by-country/[Last accessed on 24th May 2020].[7] The countries with a population of >1 million regardless of BCG vaccine used and regardless of nature of BCG strain and with overall data on COVID-19-related morbidity and mortality were included. Countries with population <1 million and a lack of said data were excluded.
Statistical analysis
Both descriptive and inferential statistics were applied. Categorical data (income group, current policy, past BCG policy and BCG policy in special group, BCG strain, and BCG coverage) were presented as proportions. The association between the BCG strains and morbidity/mortality was assessed in univariate analysis followed by multivariate regression analysis with post hoc Tukey test. Morbidity/mortality was the dependent variable while Current policy, BCG strain, BCG coverage, and Income group were considered as independent covariates. All statistical analysis was done using the Statistical Package for the Social Sciences (SPSS) version 20, IBM Corporation, Armonk, New York, USA, and statistical significance was set at <0.05.
RESULTS
Demographic data
The database search yielded 222 countries. Of these, the population was <1 million in 60 countries; the population data were not available for five countries; COVID-19 and BCG data were not available for 11 and seven countries, respectively. Hence, a total n = 139 countries were finally included for the analysis [Figure 1]. BCG strain type was available only for 51 countries and this formed the final sample.
Figure 1.
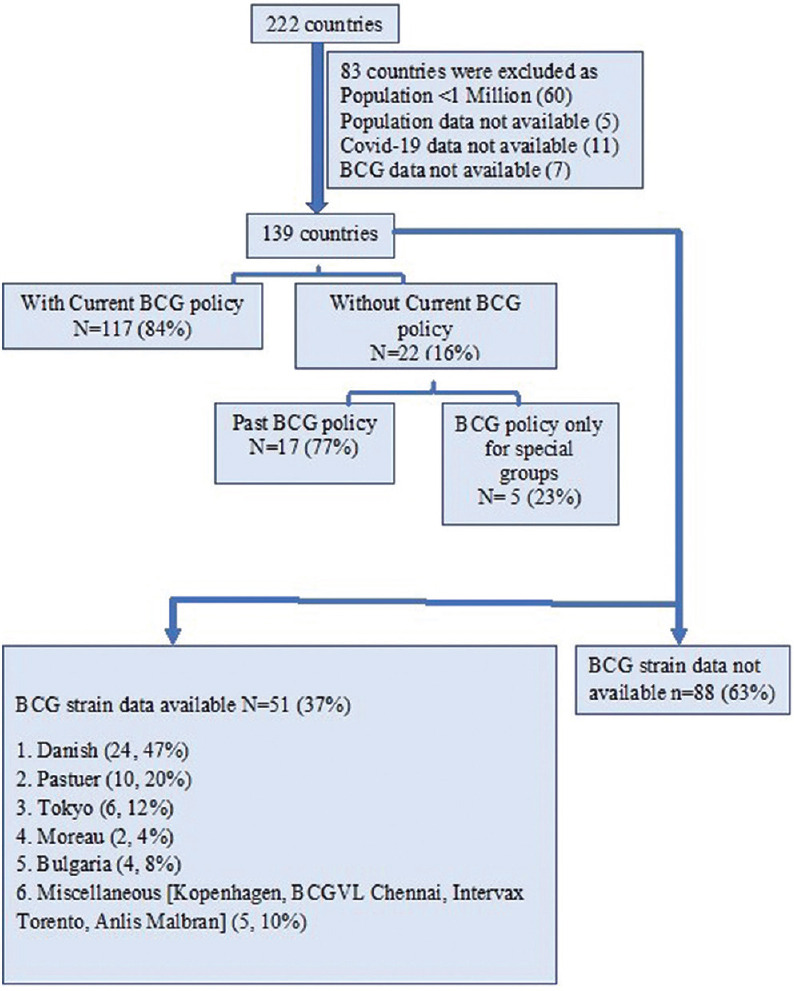
Flow chart explaining the sample collection for final analysis
Bacillus Calmette Guerin policy
Of these 139 countries, 117 (84%) countries had a current BCG policy, while 22 (16%) countries did not. Among these 22 countries, 17 (77%) countries had a past BCG policy while in five (23%) countries BCG is recommended for special groups only (such as health care workers who are dealing with TB patients or specimens).
Bacillus Calmette Guerin strains
Of the 51 countries where the data on strain were available, the BCG Danish strain was the most common (18/51, 35%) followed by the BCG Pasteur strain (10/51, 20%) both of which are late strains [Figure 1].
Nation-wide Bacillus Calmette Guerin coverage
Among the 139 countries, 80 (58%) did not mention the nationwide BCG vaccination coverage. Thirty-six (26%) countries had >90% BCG coverage, while 13 (9%) had coverage between 81% and 90%, six (4%) had BCG coverage between 71% and 80% and only four (3%) countries had BCG coverage <70%.
Income group
Of the total 139 countries, 39 (28%) belonged to upper income (UIC), 40 (29%) to upper middle income, 33 (24%) to lower middle income and 27 (19%) to lower-income group.
Linear regression analysis
No statistically significant difference in COVID-19 morbidity and mortality per one million population among various BCG strains [Figure 2]. Furthermore, the extent of BCG coverage (%) did not impact morbidity and mortality [Figure 3]. However, a significant difference (P < 0.001) was found between current BCG policy, BCG policy for special groups and income groups. Multivariate analysis showed a significant difference (P < 0.001) among the countries with higher morbidity among UIC relative to the other countries (non-HIC). The mortality rate between the income groups however did not differ significantly (P > 0.05).
Figure 2.
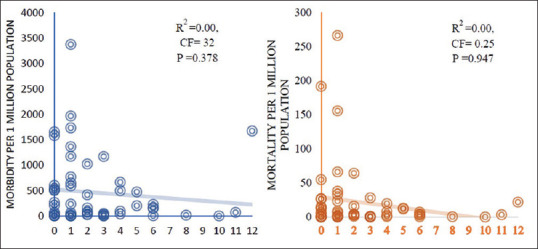
Association between Bacillus Calmette Guerin strains and COVID-19-related morbidity and mortality (n = 51)
Figure 3.
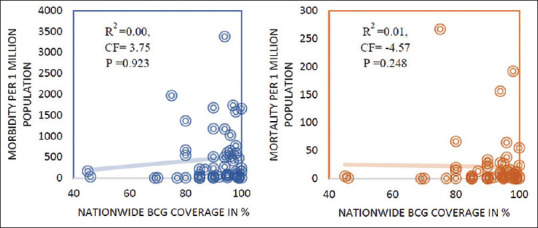
Association between nationwide Bacillus Calmette Guerin coverage in percentage and COVID-19-related morbidity and mortality (n = 59)
Similarly, a statistically significant difference (P < 0.001) was seen among various types of BCG recommendation (Current policy vs. past BCG policy vs. BCG policy for special groups) with COVID-19 related mortality per one million population [Table 1]. The countries having a current BCG policy had a significantly lower mortality rate relative to the countries with a past BCG policy or a BCG policy only for special groups (P < 0.001). Furthermore, the countries with a past BCG policy had lower mortality rates relative to the countries following BCG policy only for special groups.
Table 1.
Multivariate linear regression analysis
| Dependent variable | Covariates | Adjusted R2 | P |
|---|---|---|---|
| Morbidity (per 1 million population) | Income group | 0.45 | <0.001 |
| Current BCG policy | 0.624 | ||
| Type of BCG policy | 0.058 | ||
| Mortality (per 1 million population) | Income group | 0.42 | 0.105 |
| Current BCG policy | 0.128 | ||
| Type of BCG policy | <0.001 | ||
| Post hoc analysis using Tukey’s test | |||
| Income groups versus COVID-19 morbidity | Upper | Upper middle | <0.001 |
| Lower middle | <0.001 | ||
| Lower | <0.001 | ||
| Type of BCG policy versus COVID-19 mortality | Current BCG policy | Past BCG policy | <0.001 |
| BCG policy for special groups | <0.001 | ||
| Past BCG policy | BCG policy for special groups | <0.001 | |
BCG: Bacillus Calmette-Guerin
DISCUSSION
The present study evaluated the association of the type of BCG strain used in a given country with COVID-19 morbidity and mortality and found no impact of the nature of the strain. Our analysis though confirmed literature findings with regard to BCG vaccination itself.
In 1924, initial BCG lots were distributed to various countries for local preparation of the vaccine.[2] The original strain was passaged under similar conditions as at the Pasteur Institute. Many laboratories generated their own strain of BCG, typically named after the laboratory, the city, or the country.[8] Our finding of no relationship between various BCG strains and the COVID-19-related mortality and morbidity is probably due to the fact that all BCG strains are derived from the same parent genome or seed (which is Pasteur) leading to the same nonspecific immunity due to increase in NK cells activity.[9] Horwitz et al.[10] in an animal model of pulmonary tuberculosis found both early and late strains found to be equally efficacious supporting our findings.
In India, the BCG Chennai strain is used since 1948 (late strain) and COVID-19 related disease burden is relatively low in the country. In contrast to this, Miyasak[6] has shown that early BCG strains (e.g. BCG Japan and BCG Russia) are associated with lower COVID-19 mortality, while BCG Denmark (late strain), offers less protection against COVID-19. This difference could be attributed to the fact that this Miyasaka conducted their study earlier in the course of the pandemic and only among 17 countries.
We found no significant difference in COVID-19 disease burden and the extent of BCG coverage (%) in line with findings of Wickramasinghe et al.[11] We also found that morbidity was higher in countries with UIC compared to others consistent with findings of other authors.[2,11] We also confirmed that countries having a current BCG policy had a significantly lower mortality rate relative to the countries having a past BCG policy or a BCG policy only for special groups.[1,6,11]
While studies with BCG vaccines are aplenty (NCT04327206, NCT04328441, NCT04537663, NCT04417335, NCT04475302)[12,13] in COVID-19, we could not find any study that was making a head-to-head comparison among strains. The only completed study that has a head-to-head comparison of two strains (BCG Japan vs. BCG Russia) has been completed (no results available) in 15,600 infants (NCT03400878) and is an RCT evaluating the impact of the two strains on early life hospitalization and deaths.[14] Our study is limited by the fact that the data on only 51 countries was available for evaluation of the impact of different BCG strains on the COVID-19 disease burden. In addition, we have not evaluated the impact of confounders such as age as UIC has more elderly populations.
In summary, our study confirmed that the presence of a current BCG policy does seem to be associated with lower COVID-19 mortality though the type of BCG strain does not appear to matter.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors would to thank the Indian Council of Medical Research (ICMR) Center for Product Development under whose aegis this study was carried out.
REFERENCES
- 1.Miller A, Reandelar MJ, Fasciglione K, Roumenova V, Li Y, Otazu GH. Correlation between universal BCG vaccination policy and reduced morbidity and mortality for COVID-19: An Epidemiological Study. [Last accessed on 2021 Nov 10];medRxiv. 2020 3:1–15. Available from: https://www.medrxiv.org/content/10.1101/2020.03.24.20042937v2.full.pdf+html . [Google Scholar]
- 2.Behr MA. BCG – Different strains, different vaccines? Lancet Infect Dis. 2002;2:86–92. doi: 10.1016/s1473-3099(02)00182-2. [DOI] [PubMed] [Google Scholar]
- 3.The BCG World Atlas. Database of Global BCG Vaccination Policies and Practices. 3rd ed. Montreal, Canada: National Prevention Information Network; 2020. [Last accessed on 2020 May 24]. Available from: http://www.bcgatlas.org/ [Google Scholar]
- 4.Curtis N, Sparrow A, Ghebreyesus TA, Netea MG. Considering BCG vaccination to reduce the impact of COVID-19. Lancet. 2020;395:1545–6. doi: 10.1016/S0140-6736(20)31025-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goodridge HS, Ahmed SS, Curtis N, Kollmann TR, Levy O, Netea MG, et al. Harnessing the beneficial heterologous effects of vaccination. Nat Rev Immunol. 2016;16:392–400. doi: 10.1038/nri.2016.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Miyasaka M. Is BCG vaccination causally related to reduced COVID-19 mortality? EMBO Mol Med. 2020;12:e12661. doi: 10.15252/emmm.202012661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organisation. Population Data by World Bank Income Group. [Last accessed on 2021 Jan 16]. Available from: https://apps.who.int/gho/data/view.main.POP2030 .
- 8.Osborn TW. Changes in BCG strains. Tubercle. 1983;64:1–3. doi: 10.1016/0041-3879(83)90044-2. [DOI] [PubMed] [Google Scholar]
- 9.Kleinnijenhuis J, Quintin J, Preijers F, Joosten LA, Jacobs C, Xavier RJ, et al. BCG-induced trained immunity in NK cells: Role for non-specific protection to infection. Clin Immunol. 2014;155:213–9. doi: 10.1016/j.clim.2014.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Horwitz MA, Harth G, Dillon BJ, Maslesa-Galić S. Commonly administered BCG strains including an evolutionarily early strain and evolutionarily late strains of disparate genealogy induce comparable protective immunity against tuberculosis. Vaccine. 2009;27:441–5. doi: 10.1016/j.vaccine.2008.10.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wickramasinghe D, Wickramasinghe N, Kamburugamuwa SA, Arambepola C, Samarasekera DN. Correlation between immunity from BCG and the morbidity and mortality of COVID-19. Trop Dis Travel Med Vaccines. 2020;6:17. doi: 10.1186/s40794-020-00117-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hensel J, McAndrews KM, McGrail DJ, Dowlatshahi DP, LeBleu VS, Kalluri R. Protection against SARS-CoV-2 by BCG vaccination is not supported by epidemiological analyses. Sci Rep. 2020;10:18377. doi: 10.1038/s41598-020-75491-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kantor IN. BCG versus COVID-19? Medicina (Buenos Aires) 2020;80:1–3. [PubMed] [Google Scholar]
- 14.United States National Library of Medicine. [Last accessed on 2021 Mar 09]. Available from: https://clinicaltrials.gov/ct2/show/NCT03400878 .


