Abstract
Context:
Medication and low salt diet adherence play as an essential factor in blood pressure target achievement. Community health worker empowerment was reported to be a highly effective social intervention to medication and low salt diet adherence.
Aims:
This study aimed to investigate the effect of structured health education regarding hypertension on community health workers on medication and low salt diet adherence among hypertensive patients in Malang.
Subjects and Methods:
A quasi-experimental study was conducted in health workers and their hypertensive patients who join in the Integrated Health Service Post for the Elderly (IHSP-Elderly) program in Malang. Medication adherence was measured by the medication adherence questionnaire and low salt diet adherence was measured by dietary salt restriction questionnaire. The data were analyzed by Chi-square analysis for categorical data and independent t-test for numerical data.
Results:
This study showed that hypertensive patients in the intervention group had better knowledge regarding hypertension compared to those of the control group (P < 0.05). The patients' satisfaction in intervention group improved significantly after health education (P < 0.01). The proportion of patients with good medication adherence improved significantly (P < 0.01) from 20% to 70% after health education in intervention group. Moreover, the proportion of patients with good low salt diet compliance improved significantly (P < 0.01) from 39% to 85%. Conversely, the proportion of good medication and low salt diet adherence in control group relatively similar between pre- and post-test.
Conclusions:
This study showed that health education on community health workers improved hypertensive patients' medication and low salt diet adherence.
Keywords: Community health workers, education, health, hypertension
INTRODUCTION
Blood pressure target achievement is the cornerstone component of cardiovascular event prevention. In Indonesia, more than 80 million people have hypertension, and only 9% of them achieved adequate blood pressure control.[1] Antihypertensive therapy in patients with uncomplicated hypertension reduced the incidence of cardiovascular disease by 25%–30%.[2] Moreover, dietary interventions are essential behavioral strategies for cardiovascular risk reduction in hypertensive patients.[3] The combination of sodium intake reduction and the DASH diet has lowered blood pressure in 412 participants.[4] Furthermore, The Eighth Joint National Committee 8 outlined nine specifications for pharmacotherapy and lifestyle combinations for hypertensive patients.[5] Hence, medication and low salt diet adherence are essential in reducing hypertension complications.
Community-based organizations are reported to be a beneficial social intervention to improve adherence.[6] Community health workers are expected to play an important role, especially on any issues related to health. The community health workers' performance is disrupted when they receive inadequate health information sources.[7] Thus, community health workers' level of knowledge has an ultimate impact on the efficacy of community health workers' roles. Therefore, health education on community health workers might increase their role in encouraging the patients to be compliant with their medication and diet.[8] Moreover, previous study showed that community-based interventions might improve hypertension management and reduce the risk factors for cardiovascular disease.[9] Many studies revealed the benefit of community health worker health education on hypertension self-management and medication adherence.[9,10,11] Still there are limited studies that focused on medication and low salt diet adherence improvement trough community health-care knowledge improvement. Therefore, this study aimed to investigate the medication and low salt diet adherence of hypertensive patients after health education on community health worker.
SUBJECTS AND METHODS
The protocol for this analysis was approved by the Ethics Committee of Saiful Anwar Hospital, Malang, Indonesia (approval number, 427/EC/KEPK-PSIK/12/2017). Written informed consent was obtained from each hypertension patient in this study at the first meeting.
This study is a quasi-experimental study. This study was conducted on 73 community health-care workers who work in the Integrated Health Service Post for the Elderly (IHSP-Elderly) program in Malang. IHSP Elderly was a health management and monitoring program for elderly (≥46 years old). They were in charge of 225 hypertensive patients. Thirty-seven community health-care workers and their hypertensive patients were assigned as intervention group. The community health-care workers in intervention group received structured health-care education with supervision from trained nurses. On the other hand, 36 community health-care workers and their hypertensive patients was assigned as control group. The community health-care workers in control group received general health education regarding hypertension. For health education effectiveness evaluation, we used purposive sampling and included 164 hypertensive patients who have actively attended the IHSP-Elderly program with the criteria was they attended at least 3–5 times of IHSP-Elderly program during the last 6 months or committed to attend the program. We excluded 61 hypertensive patients due to their irregular attendance.
This study was started with pretest regarding patients' satisfaction on community health workers' role, medication, and low salt diet adherence on hypertensive patients in both groups using the Medication Adherence Questionnaire dan Dietary Sodium Restriction Questionnaire. They received an ID card that should be shown on the follow-up session to make sure that the data were collected from the same patients during the study. After the pretest was done we provided health education to the health-care workers in the intervention group regarding (1) hypertension as cardiovascular event risk factor; (2) early detection and awareness of hypertension; (3) the importance of medication adherence in hypertension management; (4) the importance of low salt diet in hypertension management; and (5) blood pressure measurement workshop. Furthermore, they are equipped with health education media such as flip chart. The educated health-care workers had to share the knowledge to the hypertensive patients in IHSP-Elderly program, then the trained nurses provided the direct supervision to the health care workers regarding their practices in educating the hypertensive patients. After a month of supervision, we evaluate the hypertensive patients' knowledge regarding hypertension, medication, and low salt diet adherence using the same questionnaire. The data were analyzed using t tests for numerical data and χ2 statistics for categorical variable.
RESULTS
The baseline characteristics of community health workers and their hypertensive patients presented in Tables 1 and 2, respectively. Table 1 shows that the community health workers in the intervention group were significantly older and being a community health worker for a more extended period compared to those of the control group. Hypertensive patients' baseline characteristics showed that there was no significant difference on age, gender, the amount of anti-hypertensive medicine consumed, systolic and diastolic blood pressure, the presence of diabetes mellitus, hypertension awareness, and alternative medicine usage between control and intervention group. However, the proportion of hypertensive patients who had family history of hypertension in the intervention group was significantly higher than that of the control group.
Table 1.
Community health care characteristics
| Variable | Control (n=36) | Intervention (n=37) | P |
|---|---|---|---|
| Duration (years) being a community health worker, mean±SD | 9.97±13.269 | 13.49±10.543 | 0.000 |
| Age (years), mean±SD | 57.03±10.630 | 61.19±9.492 | 0.000 |
| Blood pressure measurement skill, n (%) | |||
| Capability | 22 (61.1) | 15 (40.5) | 0.079 |
Table 2.
Patients’ characteristics
| Variable | Control (n=82) | Intervention (n=82) | P |
|---|---|---|---|
| Age, mean±SD | 60.54±8.74 | 61.42±9.84 | 0.547 |
| Gender, n (%) | |||
| Male | 15 (18.3) | 13 (15.9) | 0.836 |
| Female | 67 (81.7) | 69 (84.1) | |
| Amount of anti-hypertensive medicine consumed, mean±SD | 1.29±1.22 | 1.04±0.77 | 0.373 |
| Systolic blood pressure , mean±SD | 149.94±11.57 | 154.60±20.11 | 0.173 |
| Diastolic blood pressure , mean±SD | 91.46±4.81 | 92.66±11.01 | 0.299 |
| Diabetes mellitus, n (%) | 5 (6.1) | 6 (7.3) | 0.350 |
| Using alternative medicine, n (%) | 25 (30.5) | 19 (23.2) | 0.378 |
| Aware of hypertension, n (%) | 60 (73.2) | 69 (84.1) | 0.127 |
| Family history of hypertension, n (%) | 25 (30.5) | 60 (73.2) | 0.000 |
Data were presented as n (%) or mean±SD. SD: Standard deviation
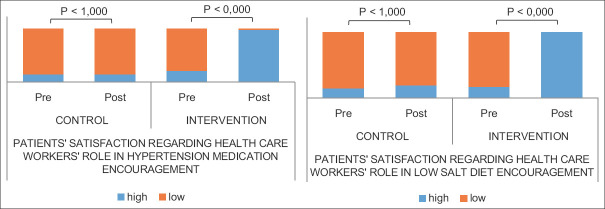
Hypertensive patients' satisfaction on community health workers' roles regarding medication and low salt diet compliance is shown in Figure 1. Before health education intervention, the patients' satisfaction was low in both issues. The patients' satisfaction improved significantly after health education. Hypertensive patients compliance is shown in Figure 2. The proportion of patients with high compliance to medication and low salt improved significantly after health education by community health workers.
Figure 1.
Patients' satisfaction on community health workers' roles before and after health education regarding hypertension management
Figure 2.
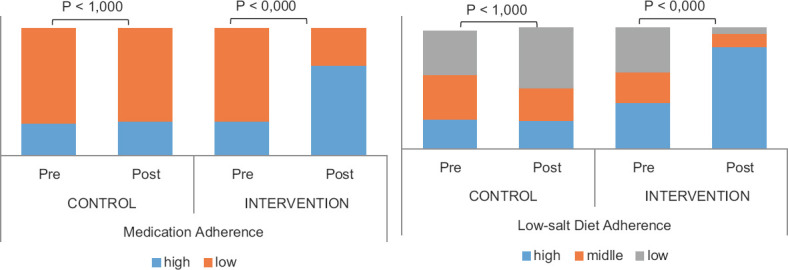
Patients' medication compliance before and after health education regarding hypertension management on community health workers
DISCUSSION
This study revealed that health education on community health workers improved medication and low salt diet adherence among patients with hypertension in Malang. Community health workers play as an extension of primary health-care centers because they interact with patients with meaningful relationships regularly over a long period through home visits, meetings and integrated health service post for the elderly.[12] Health activities carried out by community health workers in the community are related to promotive and preventive activities with a comprehensive approach that centered on patient self-management.[13] The role of community health worker was emphasized as a facilitator of behavioral change by linking self-health management in the public health system. They provide community-based information and care that enables better and intensive communication regarding hypertension self-management with patients.[11,13,14,15] Community health worker involvement in community-based hypertension self-care promotion could improve blood pressure and cardiovascular outcomes.[9,10,11,13]
Community health workers need some supports to be productive. Their competencies, knowledge, and skills should be improved through training, monitoring, and follow-up to support their works.[7,15] Community perception regarding community health worker knowledge, skills, and abilities in assisting their health needs is essential to influence their awareness and acceptance of community health worker services.[16] This study showed that patient satisfaction on community health workers' role increased significantly after health education intervention. Moreover, there was a significant difference in hypertension knowledge level regarding the definition, complications, medical treatment, and compliance with hypertension medication between the control group and the intervention group. It showed that well-informed community health workers were able to transfer and affect hypertensive patients' knowledge and perception regarding hypertension management.
Health education from well informed community health workers has indeed became a factor that improved hypertensive patients practice on hypertension self-management such as medication adherence and low salt diet compliance.[11,13,15,17,18,19,20,21] In this study, the proportion of hypertensive patients' with good medication adherence and low salt diet compliance were increased after health education on community health worker. It showed that community health workers were able to affect the hypertensive patients' behavior in the community. The previous study showed that actions based on knowledge would last longer when compared to that of actions that were not based on knowledge.[18,19]
CONCLUSIONS
This study showed that health education on community health workers improved hypertensive patients' medication and low salt diet adherence.
Limitation of study
This study suggested that health care professional should consider collaboration with community health workers to achieve better patient satisfaction, hypertension self-management practice, and cardiovascular event prevention. However, limitation of this study was that the effect of health education on community health worker observed only for a month. Thus, further study is needed to investigate the long term effect of the health education on hypertensive patient self-management practice.
Financial support and sponsorship
This study was granted by Ministry of Research, Technology and Higher Education of the Republic of Indonesia.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Hussain MA, Mamun AA, Reid C, Huxley RR. Prevalence,awareness, treatment and control of hypertension in Indonesian adults aged≥40 years: Findings from the Indonesia family life survey (IFLS) PLoS One. 2016 doi: 10.1371/journal.pone.0160922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Erem C, Hacihasanoglu A, Kocak M, Deger O, Topbas M. Prevalence of prehypertension and hypertension and associated risk factors among Turkish adults: Trabzon hypertension study. J Public Health (Oxf) 20099 doi: 10.1093/pubmed/fdn078. [DOI] [PubMed] [Google Scholar]
- 3.Stuart-Shor EM, Berra KA, Kamau MW, Kumanyika SK. Behavioral strategies for cardiovascular risk reduction in diverse and underserved racial/ethnic groups. Circulation. 2012 doi: 10.1161/CIRCULATIONAHA.110.968495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Juraschek SP, Gelber AC, Choi HK, Appel LJ, Miller ER., 3rd Effects of the dietary approaches to stop hypertension (DASH) diet and sodium intake on serum uric acid. Arthritis Rheumatol. 2016 doi: 10.1002/art.39813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Armstrong C, Joint National Committee. JNC8 guidelines for the management of hypertension in adults. Am Fam Physician. 2014 [PubMed] [Google Scholar]
- 6.Tapp H, White L, Steuerwald M, Dulin M. Use of community-based participatory research in primary care to improve healthcare outcomes and disparities in care. J Comp Eff Res. 2013 doi: 10.2217/cer.13.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Agarwal S, Kirk K, Sripad P, Bellows B, Abuya T, Warren C. Setting the global research agenda for community health systems: Literature and consultative review. Hum Resour Health. 2019 doi: 10.1186/s12960-019-0362-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Campbell N, Young-Whitford A, Jacobs D. Hypertension: Are the Guidelines Being Followed? Heart, Lung and Circulation. Australia: Elsevier; 2007. [Google Scholar]
- 9.Ursua RA, Aguilar DE, Wyatt LC, Katigbak C, Islam NS, Tandon SD, et al. A community health worker intervention to improve management of hypertension among Filipino Americans in New York and New Jersey: A pilot study. Ethn Dis. 2014 [PMC free article] [PubMed] [Google Scholar]
- 10.Sharma KK, Gupta R, Mathur M, Natani V, Lodha S, Roy S, et al. Nonphysician health workers for improving adherence to medications and healthy lifestyle following acute coronary syndrome: 24-month followup study. Indian Heart J. 2016 doi: 10.1016/j.ihj.2016.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Newman PM, Franke MF, Arrieta J, Carrasco H, Elliott P, Flores H, et al. Community health workers improve disease control and medication adherence among patients with diabetes and/or hypertension in Chiapas, Mexico: An observational stepped-wedge study. BMJ Glob Health. 2018 doi: 10.1136/bmjgh-2017-000566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gunderson JM, Wieland ML, Quirindongo-Cedeno O, Asiedu GB, Ridgeway JL, O'Brien MW, et al. Community health workers as an extension of care coordination in primary care: A community-based cosupervisory model. J Ambul Care Manage. 2018 doi: 10.1097/JAC.0000000000000255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stupplebeen DA, Sentell TL, Pirkle CM, Juan B, Barnett-Sherrill AT, Humphry JW, et al. Community health workers in action: communityclinical linkages for diabetes prevention and hypertension management at 3 community health centers. Hawaii J Med Public Health. 2019 [PMC free article] [PubMed] [Google Scholar]
- 14.Allen CG, Brownstein JN, Satsangi A, Escoffery C. Community health workers as allies in hypertension self-management and medication adherence in the United States, 2014. Prev Chronic Dis. 2016 doi: 10.5888/pcd13.160236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jaskiewicz W, Tulenko K. Increasing community health worker productivity and effectiveness: A review of the influence of the work environment. Hum Resour Health. 2012 doi: 10.1186/1478-4491-10-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oliver M, Geniets A, Winters N, Rega I, Mbae SM. What do community health workers have to say about their work, and how can this inform improved programme design? A case study with CHWs within Kenya. Glob Health Action. 2015 doi: 10.3402/gha.v8.27168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.He J, Irazola V, Mills KT, Poggio R, Beratarrechea A, Dolan J, et al. Effect of a community health worker-led multicomponent intervention on blood pressure control in low-income patients in Argentina: A randomized clinical trial. JAMA. 2017 doi: 10.1001/jama.2017.11358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Muhihi AJ, Urassa DP, Mpembeni RN, Leyna GH, Sunguya BF, Kakoko D, et al. Effect of training community health workers and their interventions on cardiovascular disease risk factors among adults in Morogoro, Tanzania: Study protocol for a cluster randomized controlled trial. Trials. 2018 doi: 10.1186/s13063-018-2924-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abdel-All M, Putica B, Praveen D, Abimbola S, Joshi R. Effectiveness of community health worker training programmes for cardiovascular disease management in low-income and middle-income countries:A systematic review. BMJ Open. 2017 doi: 10.1136/bmjopen-2016-015529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shapiro MF, Shu SB, Goldstein NJ, Victor RG, Fox CR, Tseng CH, et al. Impact of a patient-centered behavioral economics intervention on hypertension control in a highly disadvantaged population:A randomized trial. J Gen Intern Med. 2020 doi: 10.1007/s11606-019-05269-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Han HR, Kim KB, Kim MT. Evaluation of the training of Korean community health workers for chronic disease management. Health Educ Res. 2007 doi: 10.1093/her/cyl112. [DOI] [PubMed] [Google Scholar]