Abstract
Introduction: Alpha gal syndrome (AGS) is an acquired allergy to mammalian products correlates with a tick bite(s) that appears to cause immune sensitization to an oligosaccharide in meat. Most publications on AGS describe no management other than avoidance of the offending agent(s). The objective of this study is to describe 2 populations of subjects who underwent Soliman Auricular Allergy Treatment (SAAT) for significant AGS meat and/or dairy allergy.
Methods: We performed a retrospective review of subjects treated at 2 different medical clinics that apply the same method of auricular acupuncture (SAAT) to AGS patients.
Results: A total of 137 patients presented to the 2 sites included in this study. The majority of patients were mammal product eaters before AGS; however, at the time of treatment only 7.3% of individuals (n = 10) actively consumed mammal products. Most subjects were reactive to beef (n = 135) and dairy (n = 95). The most common organ system involved in prior allergic reactions associated with AGS were gastrointestinal (n = 82, 59.9%) and dermatologic (n = 61, 44.5%). For those individuals with available outcome data on SAAT effectiveness (n = 126), 121 (96%) patients indicated that their symptoms were in remission after SAAT. Five individuals indicated that their symptoms were not in remission. Eleven individuals were unsure of treatment response or unable to be reached for follow-up.
Conclusion: The SAAT method showed effectiveness in the large majority of patients. No adverse reactions were noted as a result of auricular acupuncture. This alternative medicine approach to AGS management should be further studied in prospective trials with laboratory confirmation both before and after the procedure. This low-risk treatment shows promise in treating a medical condition that causes distress in an increasing number of patients.
Keywords: alpha gal allergy, Soliman Auricular Allergy Treatment, SAAT
Introduction
Ticks and tickborne diseases continue to gain recognition as health concerns rise in the United States.1,2 Alpha-gal syndrome (AGS) is “a complex allergy with high clinical relevance regarding mammalian-derived food and drugs and is characterized by the presence of IgE antibodies directed at the carbohydrate galactose-alpha-1,3-galactose.”3 This acquired allergy to mammalian products correlates with a tick bite(s) that appears to cause immune sensitization to the oligosaccharide in meat. AGS has affected individuals in 17 countries across 6 continents, with different species of tick implicated (depending on the territory), and different types of meat.4 Very few of the publications on AGS describe any management other than avoidance of the offending agent. With no effective allopathic treatment, and increasing incidence of disease,5 AGS will become more burdensome in the United States and the world.
A recent review of AGS pathology by Platts-Mills devoted a brief section to alternative medicine approaches to treatment, mentioning auricular acupuncture (and kinesiology) approaches.6 Auricular acupuncture was incorporated into acupuncture practice in 1956 by the French physician Paul Nogier. He theorized that the various body organs and structures are somatotopically projected onto the ear in a homunculus similar to that of the cerebral cortex.7 Since its introduction, ear acupuncture has been practiced by most acupuncturists all over the world and proved its efficacy as a replacement for or adjunct to body acupuncture.8
Nader Soliman, MD, after years of study aimed at identifying an allergy treatment through the auricular acupuncture microsystem, identified a different area on the ear that yielded superior results in comparison with the Nogier allergy point. The new area (a zone rather than a point) is known as Soliman Allergy Zone “SAZ.” Soliman Auricular Allergy Treatment (SAAT) treats a variety of allergic conditions: environmental, food related, and medications. Research has shown efficacy of the SAAT technique for eliminating reactions to various allergens.9 After the treatment, patients tolerate exposure to environmental allergens and can consume the food or medication that had caused an allergic reaction or anaphylaxis in the past. Patients who receive this form of allergy treatment remain free of any allergic reactions to the same allergen for many years.
The objective of this study is to describe 2 populations of subjects who underwent SAAT for significant AGS from meat and dairy allergy. If feasible and successful, this treatment could provide insight into AGS treatment and revolutionize the approach to allergy and anaphylaxis.
Methods
Setting and Participants
We performed a retrospective review of subjects treated at 1 of 2 medical clinics that apply the same method of auricular acupuncture (SAAT) to AGS patients. Clinical sites and dates are as follows: Community Supported Acupuncture (CSA) (Louisville, KY) (date range July 1, 2019 to January 15, 2020) and Alternative Medicine Center (AMC) (Rockville, MD) (date range June 1, 2019 to January 15, 2020). The provider at CSA is Mateo Bernal, a licensed practitioner of Traditional Chinese Medicine. The provider at AMC is Dr. Nader Soliman, an MD residency trained and board certified in anesthesia, and the founder of the SAAT technique. Subjects were referred to each of the providers, often traveling many hours for the SAAT technique.
Data Collection
The study was deemed exempt by the (University Blinded for Review) Institutional Review Board (IRB) UofL IRB #20.0063, and no protected health information (PHI) was transferred from the clinic EMRs to our study team. Deidentified data were stored in a secure encrypted device in Microsoft Excel format. Only individuals on the IRB had access to the deidentified data. Only the clinical providers had access to PHI. Variables collected include demographics, past medical history, AGS symptoms, diagnostic workup, and prior treatment, follow-up information including success or failure of reintroduction of the offending agent.
Clinical Diagnosis and Treatment
After obtaining a consent for the procedure, complete medical history (including prior allergic reactions and medical diagnosis and treatment) was obtained. History related specifically to the alpha gal allergy was extensively gathered: onset of allergic reactions to alpha gal, temporal association of mammalian product ingestion/exposure to the development of symptoms, relationship to tick bites, nature of allergic reactions, and body systems involved.
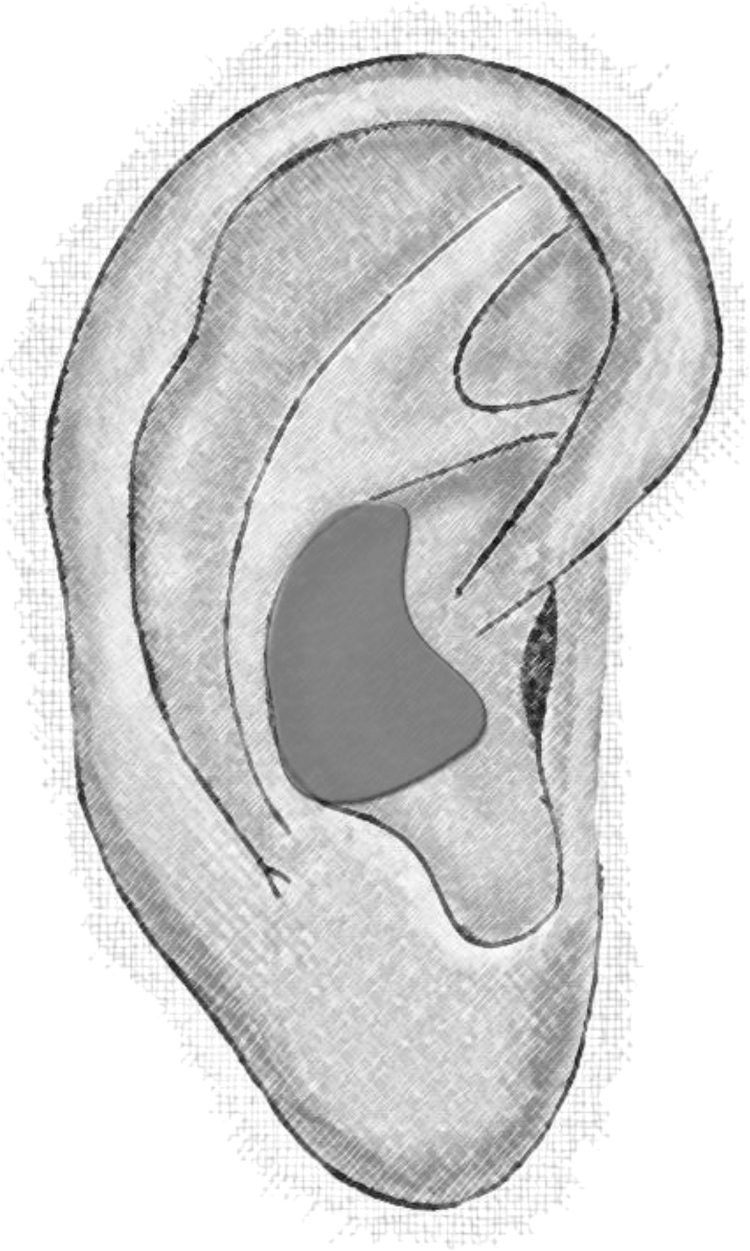
To treat the allergy to alpha gal, the individual is indirectly exposed to the alpha gal carbohydrate through simply touching a vial containing this allergen. The procedure does not involve any direct application of the alpha gal orally or on/into the skin of the patient. The skin contact with the vial appears to trigger the materialization of an auricular point that corresponds to the alpha gal allergy in the SAZ (Fig. 1). This auricular point can be identified using electrical equipment capable of identifying areas on the ear with different electrical gradients. Under sterile conditions, this point is needled with a sterilized Spinex acupuncture needle (Fig. 2). The needle is threaded subcutaneously to avoid traumatizing the auricular cartilage, and is taped to secure in place. The needle is removed at the time of the patient's 3 weeks follow-up visit.
FIG. 1.
Soliman allergy zone. © Copyright Nader Soliman, MD.
FIG. 2.
Seirin spinex needle in place. © Copyright Nader Soliman, MD.
All patients receive instructions on symptoms of potential infection and are directed to remove the needle immediately should these symptoms arise. Patients who experienced anaphylaxis before the treatment were not recommended to reintroduce mammal products (the treatment was performed to prevent symptoms in case of future accidental exposure).
After the follow-up visit (at 3 weeks post-treatment), patients who had no prior anaphylaxis were instructed to slowly reintroduce the mammalian food products if comfortable (or the prior offending allergen). They were directed to introduce very small amounts of the allergen or allergens initially. If tolerated, the amount could be gradually increased over a period of 2 weeks. In the majority of cases, no reactions occur after such reintroduction. If no reactions are noted, patients could gradually increase portion/exposure.
Results
Subject Characteristics
A total of 137 patients presented to the 2 sites included in this study. Demographic comparisons can be found in Table 1. The majority of patients were mammal product eaters before AGS (72.3% yes; 2.9% no; 24.8% unknown). However, at the time of treatment only 7.3% of individuals (n = 10) actively consumed mammal products. Most subjects were reactive to beef (n = 135). Furthermore, patients noted having reactions to dairy (n = 95), pork (n = 71), lamb (n = 32), and venison (n = 10).
Table 1.
Sample Demographics
| Site A (n = 84) | Site B (n = 53) | Total (n = 137) | |
|---|---|---|---|
| Age, median (IQR) | 45 (23.5–55.8) | 38 (24.5–52) | 42 (24.5–55) |
| Gender (%) | |||
| Female | 55 (65.5) | 24 (45.3) | 79 (57.7) |
| Male | 29 (34.5) | 28 (52.8) | 57 (41.6) |
| Unknown | 0 (0) | 1 (1.9) | 1 (0.7) |
| Race (%) | |||
| Asian | 2 (2.4) | 0 (0) | 2 (1.5) |
| Black or African American | 1 (1.2) | 0 (0) | 1 (0.7) |
| White | 65 (77.4) | 52 (98.1) | 117 (85.4) |
| Unknown | 16 (19) | 1 (1.9) | 17 (12.4) |
IQR, interquartile range.
The most common organ system involved in prior allergic reactions associated with AGS were gastrointestinal (n = 82, 59.9%) and dermatologic (n = 61, 44.5%). Most patients experienced urticarial skin eruptions up to a few hours after exposure. Respiratory symptoms were found in 35 (25.5%) individuals. Oral symptoms were found in 27 patients (19.7%). Other known symptoms included cardiovascular (n = 16), psychologic symptoms (n = 12), and ocular symptoms (n = 2).
Treatment Before Auricular Acupuncture
Subjects had attempted a variety of treatment methods to alleviate symptoms associated with AGS. Ninety-four out of 137 patients (68.6%) had received a formal AGS diagnosis from an allergist. Anaphylaxis was formally diagnosed in 34 patients (24.8%). The majority of patients (n = 69, 50.4%) attempted simple avoidance of alpha gal. Twenty-eight subjects (20.4%) used antihistamine medications, and 8 (5.8%) had taken oral corticosteroids.
SAAT Treatment
All patients received treatment for AGS using the SAAT method. For those individuals with available outcome data on SAAT effectiveness (n = 126), 121 (96%) patients indicated that their symptoms were in remission after SAAT. At the time of data analysis, a period of at least 9 months had transpired for all patients, with some being in remission for years. Five individuals indicated that their symptoms were not in remission. Eleven individuals were unsure of treatment response or unable to be reached for follow-up. A small number of patients had a second treatment only due to the needle falling out before the 3-week timeline.
For the 34 individuals with a prior diagnosis of anaphylaxis, there were available outcome data for 29 individuals. Twenty-seven (93.1%) patients indicated that they had no subsequent symptoms from either accidental, or in some cases intentional, exposure.
Discussion
To our knowledge, this is the first published series of patients with AGS mammalian allergy successfully treated with auricular acupuncture by the physician who invented the SAAT method. While reintroduction of animal products could present some risk to patients, the SAAT method itself involves no risk of anaphylaxis, and patients tolerated the procedure well. Of 137 patients who received SAAT for AGS, 121 have subsequently consumed the offending mammalian meat with no allergic symptoms. All individuals who reported remission expressed so over the phone or in one of the clinics.
Although well described in the medical literature since discovery in 2007 by Van Nunen et al., AGS remains somewhat puzzling.10,11 Humans cannot synthesize Galα1-3Galβ1-(3)4GlcNAc-R and some, therefore, produce high levels of IgE antibodies when exposed, identified by the ImmunoCAP test.5 Skin prick tests are less reliable, and the basophil activation test, although accurate, requires high technical expertise and is mostly used in experimental settings.5 The presence of antibodies alone does not sufficiently predict allergic reaction to mammalian products; tick exposure is usually involved (and can increase antibody levels >20-fold) and the clinical presentation must be consistent.5
The reaction to meat when consumed orally often occurs more than 2 hours after ingestion, making the diagnosis challenging.10 Subjects most commonly have urticaria and gastrointestinal symptoms, but can have anaphylaxis (which often is associated with higher IgE levels).12 The condition can occur in children13 (1 child was treated successfully with desensitization).14 One of the earliest cases involved an anaphylactic reaction to the drug cetuximab, found to be due to an “anti-oligosaccharide IgE antibodies specific for galactose-a-1,3-galactose (a-Gal) oligosaccharide present on the mouse-derived Fab portion of the cetuximab heavy chain.”15
Prevalence of α-Gal-sIgE levels >0.10 kUA/L ranges from around 5.5%–8.1% in urban environments up to 24.7% in 1 rural European area.5,10 In a study of 118 patients in Australia, 84.6% of patients with clinical AGS had anti-alpha-Gal IgE above the threshold.16 In 121 patients in the United States, 97% of patients with clinical AGS had anti-alpha-Gal IgE above the threshold.17 Many tick species have been implicated in the sensitization of humans to the alpha gal molecule.18,19 Although the confirmatory diagnostic test involves alpha-gal-sIgE-positive (≥0.10kUA/L), a clinical history of tick exposure preceding a new meat allergy appears sufficient to diagnose the condition.3,5,16,20
Alpha gal allergy is currently considered by most allergists to be untreatable, other than avoidance of the allergen.6 We know of only 1 recent publication (in the American Journal of Biomedical and Life Sciences) that describes a cohort of patients who received treatment for AGS with auricular acupuncture, with a high reported success rate.21 Our data from 2 unrelated clinical sites support the possibility that AGS can be treated using auricular acupuncture, with no apparent risk to patients.
Based on this study, the SAAT approach is safe and effective to treat AGS. Owing to absence of direct exposure to the actual allergen, patients have no risk of severe allergic reaction or anaphylaxis (in contrast to allergy shots). SAAT does not require availability of intramuscular epinephrine (e.g., EpiPen). The technique is specific to a particular allergen, and patients have noted remission of disease for long periods of time without repeated treatments.
Some risk is inherent in the return to eating mammal products; however, we did not recommend that any patients with anaphylaxis attempt intentional reintroduction. The directions for reintroduction involve a small amount of the offending agent, and we encouraged continued treatment under the care of an allergist. Providers note anecdotal observation that presence/severity of symptoms does not correlate with serologic findings or changes after treatment.
Limitations
This study is limited by its retrospective approach. Laboratory values were not available for many patients, with a good deal of subjects simply reintroducing meat without any confirmatory testing. The long-term durability of the response/remission is unknown. We remain unsure as to the mechanism of effect with the SAAT method, although auricular acupuncture is well established as a treatment for many medical conditions. Researchers remain unsure of the exact mechanisms of sensitization and clinical presentation of AGS. This study did not have access to serologic follow-up testing in patients after treatment.
Spontaneous remission of alpha gal allergy can occur, but a recent systematic review of 236 post-tick exposure AGS cases reported in 79 case report and series studies found only 7 cases (3%) of alpha-Gal de-sensitization through consumption of small amounts of animal-based foods during follow-up.22 However, many of the patients in these cohorts had allergic symptoms with mammal product consumption persisting for years. We also do not have data related to subsequent tick bites and resensitization, although 3 patients presented to the Louisville, KY clinic for this reason after data analysis. Future prospective research should use molecular methods to determine the mechanism of remission in patients treated with this method.
Conclusion
Ninety-six percent of patients with available outcome data had complete remission of AGS mammalian product allergy after SAAT treatment lasting months to years. No adverse reactions were noted as a result of the auricular acupuncture. This alternative medicine approach to AGS management should be further studied in prospective trials with firm laboratory confirmation both before and after the procedure. This low-risk treatment shows promise in treating a medical condition that causes distress in an increasing number of patients.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
No funding was received for this article.
References
- 1. Molaei G, Little EAH, Williams SC, Stafford KC. Bracing for the worst—Range expansion of the lone star tick in the Northeastern United States. N Engl J Med. 2019;381(23):2189–2192. [DOI] [PubMed] [Google Scholar]
- 2. Paules CI, Marston HD, Bloom ME, Fauci AS. Tickborne diseases—Confronting a growing threat. N Engl J Med. 2018;379(8):701–703. [DOI] [PubMed] [Google Scholar]
- 3. Fischer J, Huynh HN, Hebsaker J, Forchhammer S, Yazdi AS. Prevalence and impact of type I sensitization to alpha-gal in patients consulting an allergy unit. Int Arch Allergy Immunol. 2020;181(2):119–127. [DOI] [PubMed] [Google Scholar]
- 4. Rowane M, Valencia R, Stewart-Bates B, Casselman J, Hostoffer R Jr. No bull: A case of alpha-gal syndrome associated with buffalo meat sensitivity. Allergy Rhinol (Providence). 2019;10:2152656719893366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. de la Fuente J, Cabezas-Cruz A, Pacheco I. Alpha-gal syndrome: challenges to understanding sensitization and clinical reactions to alpha-gal. Expert Rev Mol Diagn. 2020;20(9):905–911. [DOI] [PubMed] [Google Scholar]
- 6. Platts-Mills TAE, Li RC, Keshavarz B, Smith AR, Wilson JM. Diagnosis and management of patients with the alpha-gal syndrome. J Allergy Clin Immunol Pract. 2020;8(1):15.e1–23.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Oleson TD, Kroening RJ, Bresler DE. An experimental evaluation of auricular diagnosis: the somatotopic mapping or musculoskeletal pain at ear acupuncture points. Pain. 1980;8(2):217–229. [DOI] [PubMed] [Google Scholar]
- 8. Hou PW, Hsu HC, Lin YW, Tang NY, Cheng CY, Hsieh CL. The history, mechanism, and clinical application of auricular therapy in Traditional Chinese Medicine. Evid Based Complement Alternat Med. 2015;2015:495684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Soliman N. A comparison study of the effectiveness of SAAT (Soliman's Auricular Allergy Treatment) approach and Nogier's allergy treatment technique. Med Acupunct. 2014;26(3):167–172. [Google Scholar]
- 10. Hilger C, Fischer J, Wolbing F, Biedermann T. Role and mechanism of galactose-alpha-1,3-galactose in the elicitation of delayed anaphylactic reactions to red meat. Curr Allergy Asthma Rep. 2019;19(1):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. van Nunen SA. Tick-induced allergies: mammalian meat allergy and tick anaphylaxis. Med J Aust. 2018;208(7):316–321. [DOI] [PubMed] [Google Scholar]
- 12. Kiewiet MBG, Apostolovic D, Starkhammar M, Grundstrom J, Hamsten C, van Hage M. Clinical and serological characterization of the alpha-gal syndrome-importance of atopy for symptom severity in a European cohort. J Allergy Clin Immunol Pract. 2020;8(6):2027.e2–2034.e2. [DOI] [PubMed] [Google Scholar]
- 13. Martin-Lazaro J, Nunez-Orjales R, Gonzalez-Guzman LA, Gonzalez MT, Boquete M, Carballada F. Galactose-alpha-1,3-galactose (alpha-gal) allergy: first pediatric case in a series of patients in Spain. Allergol Immunopathol (Madr). 2020;48(3):251–258. [DOI] [PubMed] [Google Scholar]
- 14. Yucel E, Sipahi Cimen S, Varol S, Suleyman A, Ozdemir C, Tamay ZU. Red meat desensitization in a child with delayed anaphylaxis due to alpha-Gal allergy. Pediatr Allergy Immunol. 2019;30(7):771–773. [DOI] [PubMed] [Google Scholar]
- 15. Chinuki Y, Morita E. Alpha-Gal-containing biologics and anaphylaxis. Allergol Int. 2019;68(3):296–300. [DOI] [PubMed] [Google Scholar]
- 16. Li J, Fulton RB, O'Connell R, Jang HS, Fernando SL. Specific-IgE to galactose-alpha-1,3-galactose (alpha-gal) has limited utility in diagnosing meat allergy in a tick-endemic population. Ann Allergy Asthma Immunol. 2018;121(4):509–511. [DOI] [PubMed] [Google Scholar]
- 17. Commins SP. Diagnosis & management of alpha-gal syndrome: lessons from 2,500 patients. Expert Rev Clin Immunol. 2020:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Crispell G, Commins SP, Archer-Hartman SA, et al. . Discovery of alpha-gal-containing antigens in North American tick species believed to induce red meat allergy. Front Immunol. 2019;10:1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Park Y, Kim D, Boorgula GD, et al. . Alpha-gal and cross-reactive carbohydrate determinants in the N-glycans of salivary glands in the lone star tick, Amblyomma americanum. Vaccines (Basel). 2020;8(1):18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mabelane T, Basera W, Botha M, Thomas HF, Ramjith J, Levin ME. Predictive values of alpha-gal IgE levels and alpha-gal IgE: Total IgE ratio and oral food challenge-proven meat allergy in a population with a high prevalence of reported red meat allergy. Pediatr Allergy Immunol. 2018;29(8):841–849. [DOI] [PubMed] [Google Scholar]
- 21. Liebell D. Effect of Soliman Auricular Allergy Treatment (SAAT) on IgE-mediated reactions due to exposure to mammalian meat oligosaccharide, galactose-α-1,3-galactose. Am J Biomed Life Sci. 2020;8(5):189–197. [Google Scholar]
- 22. Young I, Prematunge C, Pussegoda K, Corrin T, Waddell L. Tick exposures and alpha-gal syndrome: A systematic review of the evidence. Ticks Tick Borne Dis. 2021;12(3):101674. [DOI] [PubMed] [Google Scholar]