Abstract
Background
Women with ovarian cancer have been shown to be at significant risk of malnutrition with incidence rates described as being between 28% to 67%. Nutrition interventions may improve clinical outcomes positively, nutritional status or quality of life measures in this patient group.
Objectives
This review was conducted to assess the effects of nutrition interventions during the perioperative period for women with ovarian cancer.
Search methods
Electronic searches were conducted of the Cochrane Gynaecological Cancer Group Specialised Register, the Cochrane Central Register of Controlled Trials (CENTRAL 2012, Issue 7), Medline (1946 to July week 4 2012), Embase (1980 to 2012 week 31), DARE (to 7th August 2012) AMED (1985 to April 2012), BNI (1992 to April 2012), CINAHL (to April 2012). We also searched trials databases, conference proceedings and related citation lists. Reference listings were handsearched. No restrictions were applied on language or date.
Selection criteria
Randomised controlled trials (RCTs) in which women 18 years and over with any stage of ovarian cancer, including recurrent cancer, were in the perioperative phase of treatment and received any type of nutrition intervention.
Data collection and analysis
Titles and abstracts were screened by two review authors with study selection discussed by a team. Pairs of review authors worked independently on data collection and compared findings.
Main results
A total of 4092 titles were screened and 14 full text reports reviewed; a single small study met the inclusion criteria. In the included RCT, 40 women (35 with ovarian cancer) had extensive elective surgery including bowel resection for treatment of gynaecological malignancy. Randomisation was made to either early oral feeding (oral fluids in the first 24 hours, solid foods on the following day) or to a 'traditional' feeding regimen where oral fluids and foods were delayed until there was evidence of bowel function. Most women in the early feeding group (14/18) were able to resume eating solid food one day after surgery. This resulted in a significantly shorter hospital stay with no increase in postoperative complications or change in quality of life measures in comparison with the women on the 'traditional' feeding regimen. The incidence of nausea and vomiting during the postoperative stay was similar in both groups and was noted in slightly more than half of the women. Overall survival was evaluated until 30 days following discharge from hospital; in this period, there was one death of a woman who had been in the 'traditional oral feeding' group, cause of death was not noted. We assessed risk of bias and found no high risk of bias was identified in the methodology and reporting of the included study, although there was an increased risk of bias due to the small size of the study in which not all of the women had ovarian cancer.
Authors' conclusions
Although women with ovarian cancer have been shown to be at risk of malnutrition, there is a lack of evidence derived from RCTs evaluating the identification, assessment and treatment of malnutrition during the perioperative phase of treatment. There is evidence from one small study that some women with ovarian cancer undergoing surgery with associated bowel resection may safely commence oral fluids within 24 hours of surgery and solid foods on the following day. Further research is required, including a RCT, to generate guidance concerning the treatment of malnutrition in this patient group.
Plain language summary
Nutrition for women who are having surgery for ovarian cancer
Women who have ovarian cancer, (a cancer which develops in the two organs (ovaries) that produce eggs in women) are more likely to have difficulties with food and with eating a nourishing diet in comparison to women with other types of gynaecological cancers. One reason may be because the symptoms of ovarian cancer can be difficult to recognise. Women may have a lack of interest in food, feel full, feel sick or have a painful or swollen abdomen. Some women become thinner in parts of their bodies while becoming bigger around their abdomen due to an abnormal build up of fluid or large tumours. There may be no change in body weight or weight may increase, this can make it difficult to know which women are developing problems due to a poor food intake.
Women who are unable to eat and drink well are at risk of becoming malnourished and may then have more complications from the treatments for ovarian cancer than women who are not malnourished. It is recommended that people who are having difficulties with eating and drinking should be identified and helped when they receive hospital care. Currently, there is no agreed method for finding and treating nutritional problems for women with ovarian cancer.
In this review, the authors looked for studies (randomised controlled trials (RCTs)) from around the world to find out how women with ovarian cancer were assessed to see if they were eating and drinking well and what help they may be given with nutrition before or after surgery. A lack of information was found on this topic.
One RCT was found where a small group of women (40 including 35 with ovarian cancer) requiring extensive elective surgery for gynaecological cancer including surgery to the gut, were able to restart eating normal foods on the day after surgery. They were able to leave hospital earlier and did not have more complications in the month after surgery than women who were not allowed to resume eating normal foods until at least three days after the operation.
More studies are needed to confirm whether restarting normal eating one day after surgery can be recommended for women having surgery for ovarian cancer. More research is needed to provide information about how to identify and treat problems of malnutrition in women with ovarian cancer.
Background
Description of the condition
Based on worldwide statistics, ovarian cancer is the seventh most frequent cancer for both incidence and mortality with age‐standardised rates (ASR) respectively of 6.3 and 3.8 per 100,000 women. Within these rates is significant geographical variation with an ASR of incidence of 9.3 per 100,000 in more developed regions and 4.9 per 100,000 in less developed regions of the world (GLOBOCAN 2008). Approximately 90% of ovarian cancers originate in the epithelial (or surface) layers of the ovary; other types of ovarian cancer can occur in the sex cord‐stroma (inner structure of the ovary) and in the germ cells (where the eggs develop).
The presenting symptoms of ovarian cancer are often of a non‐specific nature such as abdominal pain, abdominal bloating, changes in bowel habit, extreme fatigue or back pain and may be attributed to other reasons. As a consequence, patients may often be found to have advanced disease at the time of diagnosis. The treatment and prognosis of ovarian cancer are indicated by the staging of the disease classified using the International Federation of Gynecology and Obstetrics (FIGO) system (Benedet 2000). Staging may be evaluated from ultrasound, computerised tomography (CT) or other scanning techniques or from the finding of malignant cells in ascites (abnormal fluid collection in the abdomen); staging is confirmed when surgery occurs. The surgical treatment of ovarian cancer diagnosed at an early stage entails the removal of one or both ovaries and the uterus, depending on the extent of the disease and the need to preserve fertility. Where abnormal tissue is more widespread, for example in other pelvic organs, cytoreductive surgery is used with the aim of surgically removing all visible tumour tissue (optimal cytoreduction). If optimal cytoreductive surgery cannot be undertaken as a primary treatment, due to the presence of disease at inaccessible sites or poor performance status, chemotherapy may be commenced (neoadjuvant chemotherapy), prior to subsequent surgical reduction of the tumour (interval debulking) (Tangitgamol 2010). Surgical intervention may also be indicated where intestinal obstruction occurs as a complication of the disease.
Causes of malnutrition and weight loss in people with cancer have been described and these may include: tumour‐induced anorexia; catabolic effects of the tumour; abnormal metabolism of nutrients; physical obstruction of the gastrointestinal tract by a tumour; reduced food intake as a side effect of radiotherapy or chemotherapy and diminished intake due to pain, anxiety or depression (Henry 2011). Specifically in ovarian cancer, common presenting symptoms include abdominal discomfort or pain, abdominal distension, nausea, dyspepsia, early satiety and constipation (Brooks 1994). In one UK study, more than 50% of 35 women recruited were reported to have a visibly distended abdomen due to ascites or ovarian mass (Balogun 2011).These factors are liable to influence food intake and consequently nutritional status within this patient group. Malnutrition in association with ovarian cancer has been identified as a problem for many years particularly in women with advanced cancer (FIGO stages III and IV) (Tunca 1983). Within a group of 33 women with ovarian cancer requiring an operation for a bowel obstruction, 75% were identified as having severe nutritional deprivation (Larson 1989).
A variety of methods have been used to identify malnutrition. Subjective global assessment (SGA) is a method of evaluating nutrition status combining weight change, diet history and physical examination. In a Brazilian study of women with gynaecological cancers, SGA identified malnutrition in four out of 14 (28%) women with ovarian cancer (Zorlini 2008), while the same method found 50% of 132 women with ovarian cancer in a US study were malnourished (Gupta 2008). In Australia, using the patient‐generated SGA (PG‐SGA), malnutrition was identified in two‐thirds of 48 women with ovarian cancer in comparison with 12% of women with other gynaecological cancers. The mean body mass index (BMI) of the malnourished women (27.4 kg/m2) indicated that some women were overweight although their mean BMI was significantly lower than the mean BMI of well‐nourished patients. Therefore, it was noted that the use of BMI and weight alone would not be sufficient to detect malnutrition in this patient group (Laky 2008).
Evidence of malnutrition in women with ovarian cancer has been related to outcomes from surgery. When surgery has been required for intestinal obstruction, poor nutritional status (identified either by weight loss, low serum albumin or low lymphocyte count) was a factor that significantly correlated with poor surgical outcome (Krebs 1983), poor postoperative survival (Clarke‐Pearson 1988) and an increased incidence of postoperative infectious complications (Donato 1992). In a study of older women (aged 75 years or over) with ovarian and primary peritoneal cancer, serum albumin was used as a surrogate measure for nutritional status and was significantly associated with lower rates of optimal cytoreduction. Women with sub‐optimal cytoreductive surgery had a lower median survival time in comparison with the women who underwent optimal cytoreduction (17 months versus 62 months) (Alphs 2006). Although serum albumin may reflect chronic protein deficiency, it is also an indicator of acute clinical stress, hydration status, liver dysfunction and inflammation, so requires careful evaluation. In a study where prealbumin was used as a nutrition assessment marker, a significant relationship was shown between low serum prealbumin and the risk of complications after primary radical cytoreductive surgery for ovarian cancer, with significantly greater risk of blood loss, morbidity and mortality where serum prealbumin was lower than 10 mg/dL (Geisler 2007).
Current guidelines recommend the use of nutrition screening in hospital to identify individuals at risk of malnutrition. Identification of patients found to be malnourished or at risk of malnutrition should be linked to further assessment and implementation of an appropriate nutrition care plan, which may include nutrition support (ASPEN 2011; Kondrup 2003; NICE 2006). Women with ovarian cancer may have co‐existing excess weight or obesity with or without ascites, therefore appropriate screening and assessment methods are required to ensure that malnutrition is identified and treated.
Description of the intervention
In this context, nutrition interventions include nutrition screening, nutrition assessment or nutrition advice, which may be combined with nutrition support (additional or alternative provision of nutrients), with the intention to improve or maintain nutrient intake. Nutrition support may be provided as supplementary foods and drinks, fortified foods or oral nutrition supplements; also nutrition formulations given by tube into the gastrointestinal tract (enteral feeding) or given by infusion intravenously (parenteral feeding or PN). Nutrition support may compensate in part or in full for inadequate food consumption. In this review, nutrition interventions do not include the use of nutrition formulations given routinely in 'Enhanced Recovery after Surgery (ERAS)' programmes, which have been recently reviewed in the context of gynaecological oncology (Lv 2010). Nutrition interventions may occur at any stage in the perioperative period with the intention to identify, prevent or treat malnutrition. It is important that the risk of adverse effects associated with the provision of nutrition support are considered. Risks associated with nutrition support interventions may range from minor effects such as taste dislike or nausea to life‐threatening effects such as PN catheter‐related sepsis.
How the intervention might work
Nutrition screening and assessment may identify women at risk of malnutrition and enable nutrition support to be implemented. Nutrition support may improve the nutrient intake of women undergoing surgical intervention for the investigation or treatment of ovarian cancer or associated complications. The nutrition intervention may prevent further nutritional losses at a time of increased metabolic requirements due to the stresses of surgery and the requirement for postoperative wound healing.
Nutrition interventions may improve quality of life (QoL) as perceived by the patient. In other patient groups undergoing radiotherapy for cancer treatment, randomised controlled trials (RCTs) have shown that nutrition counselling improved nutrition intake, nutritional status and QoL (Ravasco 2005; Ravasco 2005a).
Nutrition interventions may reduce the length of hospital stay. Malnutrition has been identified as a factor contributing to prolonged length of stay following surgery for gynaecological cancer (Laky 2010).
Nutrition interventions may affect clinical outcome by reducing postoperative complications. Parenteral nutrition has been successfully used to raise prealbumin levels above 10 mg/dL in women with ovarian cancer; this reduced the incidence of surgical complications, which occurred in women when prealbumin levels were lower than 10 mg/dL. Prealbumin levels were subsequently used to determine the prescription of nutritional support and the timing of surgical intervention (Geisler 2007).
Women who are unable to eat due to ovarian cancer‐related intestinal obstruction can be given nutrients by an alternative route (PN) either pre‐ or perioperatively (Rubin 1989). Nutrition support techniques may be used as an alternative to normal food intake where gastroparesis has occurred as a side effect of cytoreductive surgery in ovarian cancer (Caprino 2006).
The identification of malnutrition may provide useful prognostic information. Mean survival time has been shown to be longer in well‐nourished women than in malnourished women with similar cancer staging (Gupta 2008). Nutrition status can improve. Some women with ovarian cancer identified as being malnourished at diagnosis, were subsequently noted to be nourished three months later and they had a median survival time similar to that of women who were identified as well nourished both at diagnosis and at three months. Nutritional interventions may have contributed to improved nutritional status (Gupta 2010).
Why it is important to do this review
Malnutrition has been shown to be a significant risk in women with ovarian cancer and therefore requires purposeful identification and treatment. Nutrition interventions may positively improve clinical outcomes, nutritional status or QoL measures in women with ovarian cancer. There is a need to develop practical guidance on the use of nutrition interventions derived from a systematic review of high quality studies undertaken in this patient group.
Objectives
Primary objective
To assess the effects of nutrition interventions in the perioperative period for women with ovarian cancer.
Secondary objectives
To evaluate whether the effects are modified by nutritional status at baseline or by type of nutrition intervention.
Methods
Criteria for considering studies for this review
Types of studies
Only RCTs were included.
Types of participants
Adult women (aged 18 years and over) in the perioperative phase of surgical treatment for ovarian cancer. Although the perioperative period may be considered to extend from the time when the patient is admitted to hospital for surgery until they are discharged, the term can also cover the period of time in which a patient is prepared physically (and psychologically) for surgery (i.e. from the time that surgery is planned as a treatment for ovarian cancer). The latter broader time period was considered for inclusion. Studies could include surgery at any stage in the treatment of ovarian cancer including recurrent cancer.
If studies included patients with cancer other than ovarian cancer, such as other gynaecological cancers, we only included studies where all patients were being surgically treated for cancer and where at least 75% of participants were women with ovarian cancer. No studies were found where information was reported by separate types of cancer and where data on ovarian cancer only could be extracted.
Types of interventions
We examined trials where any type of nutrition interventions was provided at any stage in the perioperative period where surgery was used as a treatment for ovarian cancer. Nutrition interventions were defined as any of the following: nutrition screening/assessment, nutrition counselling/advice, supplementary foods or drinks, fortified foods, oral nutrition supplements, enteral or parenteral feeds. Nutrition support would include a mixture of nitrogen and non‐nitrogen energy with vitamins and minerals and be either supplementary to the usual food and drink provision or be the sole source of nourishment. Nutrition interventions were considered in comparison with no nutrition intervention or were comparisons of alternative types of nutrition intervention.
Types of outcome measures
Primary outcomes
Overall survival (OS) recorded up to five years.
Length of hospital stay.
Secondary outcomes
Infective and non‐infective complications that occurred subsequent to the surgery including haemorrhage, sepsis, wound breakdown, anastomatic leak, bowel obstruction, paralytic ileus, pulmonary embolism and deep vein thrombosis, chest infection and urinary infection. Complications were included in relation to the route of access (line infection, nasogastric tube misplacement) or in relation to the substrate (such as metabolic abnormalities). Details about whether complications were recorded prospectively or retrospectively and how they were defined were noted.
Nutrition measures including nutrient intake, anthropometry (physical measures of the body), subjective global assessment (SGA) or other validated nutrition assessment tools or minor complications related to the nutrition including nausea, vomiting or diarrhoea.
Functional measures such as change in performance status, hand grip strength or sit‐to‐stand time.
QoL measures including patient‐reported outcomes.
Biochemical measures of nutritional status (blood tests), e.g. prealbumin, transferrin, retinol‐binding protein, urinary nitrogen balance.
Search methods for identification of studies
Electronic searches
The following electronic databases were searched:
the Cochrane Gynaecological Cancer Group Specialised Register, the Cochrane Central Register of Controlled Trials (CENTRAL 2012, Issue 7) and DARE (2012, Issue 3) (Appendix 1),
Medline (1946 to July week 4 2012) (Appendix 2, Appendix 2)
Embase (1980 to 2012 week 31) (Appendix 3),
AMED (1985 to April 2012), BNI (1992 to April 2012), CINAHL (1981 to April 2012)
All relevant articles were identified on PubMed and using the ‘related articles’ feature, a further search was carried out for newly published articles. Papers in all languages were sought and translations were carried out as necessary.
Searching other resources
Unpublished and grey literature
Metaregister (http://www.controlled-trials.com/rct), Physicians Data query (http://nci.nih.gov), http://www.clinicaltrials.gov and http://www.cancer.gov/clinicaltrials were searched for ongoing trials. An ongoing trial that had not been published was identified; we approached the principal investigator to ask for information concerning the protocol and likely date of publication of results. Conference proceedings and abstracts were searched through ZETOC (http://zetoc.mimas.ac.uk) and WorldCat Dissertations.
Handsearching
Handsearching was undertaken of the citation lists of included studies and a previous systematic review to identify further relevant trials.
Data collection and analysis
Selection of studies
All titles and abstracts retrieved by electronic searching were examined by two review authors to determine relevance and eligibility. Papers that did not meet the eligibility criteria were excluded. When there was insufficient information to make a decision based on the abstract and title, the full article was obtained in order to make a decision. Two review authors independently reviewed relevant references and discussed with the team of review authors to ensure they met the eligibility criteria. The reasons for exclusion of studies were documented.
Data extraction and management
A data collection form devised for the study to facilitate data collection from the included studies was piloted and modified. Data extraction was undertaken by review authors (JC, VLD, LK, LJL) independently with discrepancies discussed. The following information was recorded:
authorship, year of publication, country of origin and source of funding;
patient details, number of participants, age, inclusion and exclusion criteria;
cancer diagnosis including staging if indicated, type of surgery used, details of prior chemotherapy;
details of nutrition status of women including BMI, the proportion of malnourished women (and definition of malnutrition);
details of nutrition intervention (including type of food or nutrition support product, route of intervention, time period of intervention and quantity delivered);
details of primary and secondary outcomes including the time points when these were collected and reported.
Data on outcomes were extracted:
For dichotomous outcomes, we examined the number of women in each treatment arm who experienced the outcome of interest and the number of women assessed at endpoint, in order to estimate a risk ratio (RR).
For continuous outcomes, we recorded the final value and standard deviation (SD) of the outcome of interest and the number of women assessed at endpoint in each treatment arm at the end of follow‐up, in order to estimate the mean difference (MD) between treatment arms and its standard error.
All data extracted were relevant to an intention‐to‐treat analysis, in which participants were analysed in the groups to which they were assigned.
Assessment of risk of bias in included studies
The risk of bias in included studies was assessed using The Cochrane Collaboration's tool (Higgins 2011). This included assessment of:
-
selection bias:
random sequence generation;
allocation concealment;
-
performance bias:
blinding of participants and personnel (women and treatment providers) ‐ although blinding may not have been possible due to the nature of the interventions;
-
detection bias:
blinding of outcome assessment;
-
attrition bias:
-
incomplete outcome data: the proportion of participants whose outcomes were not reported at the end of the study was noted; a level of loss to follow‐up for each outcome was coded as:
low risk of bias, if fewer than 20% of women were lost to follow‐up and reasons for loss to follow‐up were similar in both treatment arms;
high risk of bias, if more than 20% of women were lost to follow‐up or reasons for loss to follow‐up differed between treatment arms;
unclear risk of bias, if loss to follow‐up was not reported;
-
-
reporting bias:
selective reporting of outcomes
other possible sources of bias.
The 'Risk of bias' tool was independently applied and differences resolved by discussion. Results were summarised in a 'Risk of bias' summary. Results of meta‐analyses in future updates of the review will be interpreted in light of the findings with respect to risk of bias.
Measures of treatment effect
The following measures of the effect of treatment were used: for dichotomous outcomes RR was used and for continuous outcomes the MD between treatment arms.
Dealing with missing data
If missing data were identified, it had been planned to contact study authors to seek relevant information. There was no imputation of missing data for any outcome.
Sensitivity analysis
Sensitivity analyses were planned to be performed, excluding studies at high risk of bias
Results
Description of studies
Results of the search
The results of the search are summarised in Figure 1. Following the initial review of titles and abstracts and after handsearching, it was noted that the search strategy had not been sufficiently broad to identify all available studies in this area, in some studies, patients with ovarian cancer were categorised as having 'gynaecological cancer'. The title search was therefore repeated to include the broader term of 'gynaecological cancer', when a further 2642 titles were examined for relevance. A total of 4092 titles were therefore screened. Fourteen papers were examined in detail to determine relevance where this could not be determined from the abstract. Thirteen studies were excluded as they did not meet the criteria of the protocol, one study met the protocol criteria and was included.
1.
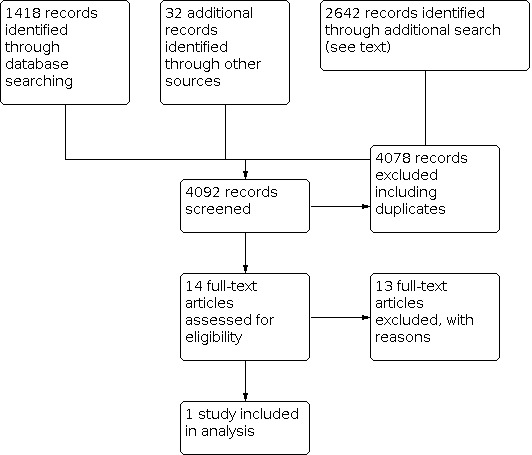
Study flow diagram.
Included studies
See Characteristics of included studies. In this RCT (Minig 2009a) a comparison was made of postoperative feeding regimens for women who were undergoing intestinal resection in conjunction with surgery for gynaecological malignancy; 88% of the women had ovarian cancer (n = 35); FIGO staging was not reported. This was a single‐centre trial conducted in Milan, Italy with the aim of investigating the feasibility of early postoperative oral feeding in this patient group and evaluating whether this would result in a reduced length of hospital stay. Baseline characteristics of the women in the two comparison groups were similar; the median age of the women in the intervention and the control group was 54 and 58 years respectively. The nutritional intervention included nutritional assessment prior to surgery using a standardised subjective global assessment questionnaire that classified women as well nourished, moderately nourished or severely malnourished. This assessment was used to determine eligibility for the trial and women who were found to be severely malnourished were excluded. Postoperatively, the nutritional intervention comprised an early oral feeding (EOF) regimen in comparison with a "traditional" oral feeding regime (TOF) where nourishment was withheld until normal bowel function resumed, evidenced by bowel sounds and passage of flatus.
Excluded studies
See Characteristics of excluded studies. All of the excluded studies included some women with ovarian cancer. One RCT examined the provision of oral and parenteral nutrition supplementation in women with advanced ovarian cancer undergoing chemotherapy, however, the chemotherapy was given after the surgical phase of treatment rather than prior to surgery (Nuutinen 1982). The use of postoperative parenteral nutrition for women with advanced ovarian cancer was studied in a group of women in comparison with a similar group of women who did not receive parenteral nutrition, but the trial was excluded as there was no reported evidence of randomisation (Tan 2002). Two studies, which were not RCTs, examined early postoperative feeding as part of a new clinical pathway and compared data from the prospective trials with data extracted retrospectively on earlier patients (Gerardi 2008; Marx 2006). Four RCTs examining early postoperative oral feeding in contrast to traditional postoperative regimens in women undergoing major abdominal gynaecological surgery were not included, as the study groups included women with benign disease in addition to women with malignant disease and there was an insufficient proportion of women with ovarian cancer (Pearl 1998; Pearl 2002; Schilder 1997; Steed 2002). The effects of early postoperative feeding were also observed in three RCTs including only women with gynaecological cancer, the proportion of women with ovarian cancer ranged from 18% to 58%, this was lower than the protocol inclusion rate of 75% (Cutillo 1999; Feng 2008; Minig 2009b). An earlier RCT included an intervention group who were given postoperative elemental feeding via jejunostomy tube. Although all the women in the study had gynaecological malignancies, only half had ovarian cancer (Spirtos 1988). More recently perioperative enteral feeding using standard and immune‐enhancing feeds was compared in an RCT of women with gynaecological cancers; this trial included 32% of patients with ovarian cancer (Celik 2009).
Risk of bias in included studies
See Risk of bias in included studies.
In the included study (seeCharacteristics of included studies), a web‐based randomisation system was used (TENALEA 2013) where patient details were entered prior to the randomisation. Allocation to groups was made after surgery was completed and when it had been verified that no intraoperative exclusion criteria had occurred (exclusions were: if total or anterior pelvic exenteration had occurred or if intestinal bowel resection had not been performed). No information was reported concerning whether those who cared for the women, measured outcomes and analysed the data were aware of which intervention the women were receiving; due to the nature of the intervention, blinding may not have been possible. Postoperative exclusion from the trial was to occur if intensive care unit (ICU) admission equalled or exceeded 24 hours, or if the malignancy was found to be non‐gynaecological. Eleven of 51 women (22%) were excluded from the trial postoperatively, with similar numbers and reasons in both study groups. It is reported that these women received the intervention, although it is unclear for what length of time. Post‐randomisation exclusion may have increased the risk of bias and raises the possibility that the intervention may be associated with an outcome that resulted in exclusion from the trial. As the nutrition intervention is a supportive therapy rather than a primary treatment, the welfare of the patient undergoing prolonged ICU admission may not be compatible with the continuing administration of the intervention.
The authors reported both their primary and secondary end‐points. Although it was noted that there was a significant difference in estimated blood loss (EBL), which was greater in the group receiving the traditional feeding regimen compared with those receiving early oral feeding, the authors state that EBL did not have a significant impact on length of hospital stay. FIGO stage was also reported as not being associated with length of hospital stay but details of FIGO staging were not reported. Although subjective global assessment score was evaluated, it was not reported so it is unclear if there were differences in nutritional status between the comparison groups.
Other potential sources of bias
There is a potential risk of bias associated with the small size of the study. The women in the study were carefully selected for inclusion in the RCT; although they all had gynaecological cancer, not all of them had ovarian cancer.
Effects of interventions
In the included study, most women in the early intervention group (78%, n = 14) were able to consume drinks within 24 hours of surgery and solid food one day after surgery, this was at least two days prior to those in the traditional feeding group. The primary outcome of the study was length of stay which was significantly shorter in the EOF group (9.1 ± 4.5 (mean days ± SD) compared to 6.9 ± 2.6 ). After adjustment for postoperative complications, the mean reduction in stay was 1.7 days. Overall survival was evaluated until 30 days following discharge from hospital. In this period, there was one death of a woman who had been in the group receiving traditional oral feeding (TOF), cause of death was not noted. The incidence of postoperative complications did not differ statistically between the groups, 44% of the patients in the EOF group had complications, none of which were infectious complications; in the TOF group, complications occurred in 55% of the patients of which a quarter had infectious complications. No complications were reported to result from the nutrition intervention. The incidence of nausea and vomiting during the postoperative stay was similar in both groups and was noted in slightly more than half of the women. Scores were similar between the two groups on the two health‐related quality of life questionnaires used at 30 days after hospital discharge and overall postoperative satisfaction was noted to be similar in both groups. Half of the women in the TOF group reported a wish to eat sooner than was allowed by the protocol. Nutrient intake, anthropometric measures, functional and biochemical measures were not evaluated as outcomes in this study.
Discussion
Summary of main results
Results from the included study showed evidence that a small group of women with ovarian cancer who were undergoing surgery including intestinal resection could tolerate an early introduction of oral fluids and foods postoperatively, and that this resulted in a reduced length of hospital stay and no difference in postoperative complication rates in comparison with women who had a traditional postoperative feeding regimen. One of the strengths of the study was that alternative feeding regimens were the only aspects of the perioperative management of the patients that differed between the randomised groups.
Overall completeness and applicability of evidence
The most striking observation from this review concerns the absence of information on this topic. While it has been reported that the incidence of malnutrition in women with ovarian cancer may vary between 28% (Zorlini 2008) and 67% (Laky 2008) and may extend to 75% where there is associated bowel obstruction (Larson 1989), there are currently no published RCTs specifically addressing the treatment of malnutrition in women with ovarian cancer or investigating the use of nutrition assessment linked to preoperative nutritional interventions in this patient group. This situation will be partly addressed by a trial currently underway where randomisation to early postoperative enteral feeding is being trialled in women identified as being at nutritional risk (Characteristics of ongoing studies). The included study is of limited applicability to women with ovarian cancer, as the 35 women in the study with ovarian cancer were all undergoing surgery that included intestinal resection.
Quality of the evidence
Results from the included study indicate that women with ovarian cancer who are undergoing surgery with associated intestinal resection may be able to manage selected fluids within 24 hours of operation and solid foods on the following day. The small number of women with gynaecological cancer (n = 40) included in the study was calculated on the basis of demonstrating a significant difference in the length of hospital stay in relation to the feeding regimens. There was no reported quantification of the amount of foods consumed, information concerning the use of intravenous fluids or measurement of nutrition outcomes. The study was conducted in a single centre and therefore may not be generalisable. Additionally, there were several reasons why women were not eligible for the trial, including women with significant other presenting conditions including an ASA (American Society of Anesthesiologists) score of four or more, severe concomitant medical condition, metabolic disease such as type 1 diabetes, infection or intestinal obstruction. Women were also excluded if found to be severely malnourished, although this was reported to be determined only on the criteria of recent weight loss greater than 10%, an assessment which may not be applicable to women with ovarian cancer; within this study, 42% of the women (n = 17) were noted to have ascites, which may disguise significant weight loss. There is no evidence from the included trial that can be applied to women who have ovarian cancer in association with these exclusion criteria or who require surgery without intestinal resection.
Potential biases in the review process
We undertook to minimise bias in this review by the breadth of our search for relevant papers including handsearching and by repeating the electronic searches when it became evident that some studies, which included patients with ovarian cancer, were categorised as having 'gynaecological cancer'. Titles, abstracts and papers were all reviewed by at least two review authors. Bias in the review process may have been influenced by the decision to exclude studies where fewer than 75% of included patients had ovarian cancer in an attempt to secure information relevant to women with ovarian cancer. It became evident from our data selection process that most studies relevant to this topic include women with differing types of gynaecological cancer or where groups of women may have either a benign or malignant tumour and that data are not reported separately for differing types of disease. Although malnutrition has been noted in association with other types of gynaecological cancer, it is most prevalent in association with ovarian cancer and therefore, data were sought that was specific to women with ovarian cancer. If we had lowered the inclusion rate selected to include studies where a majority of the women in a mixed study (more than 50%) had ovarian cancer, this would only have resulted in the inclusion of one additional study.
Agreements and disagreements with other studies or reviews
Our review concurs with a recent systematic review which was unable to identify any RCTs that evaluated the use of nutrition supplementation or nutrition counselling in women with ovarian cancer (Balogun 2012). A Cochrane systematic review on the topic of early versus delayed oral fluids and food after major abdominal gynaecologic surgery included three studies including some patients undergoing surgery for ovarian cancer (Charoenkwan 2007). The conclusion of Charoenkwan 2007 was that early feeding after major abdominal gynaecologic surgery was safe even though associated with an increased risk of nausea, and that early feeding was associated with a reduced length of hospital stay.
Authors' conclusions
Implications for practice.
There is limited evidence from one small randomised controlled trial (RCT) that some women with ovarian cancer undergoing surgery, including bowel resection, may manage to commence oral fluids within 24 hours of surgery and may manage to eat normal foods on the following day without increasing the risk of postoperative complications.
Implications for research.
Women with ovarian cancer may be at risk of malnutrition but there is an absence of research concerning the identification and treatment of malnutrition in this patient group. Studies are needed which examine whether nutrition interventions such as good quality nutrition counselling with or without the use of oral supplements following diagnosis and before and during the perioperative period may be efficacious in improving nutrition status, treatment outcomes and quality of life for women with ovarian cancer. Particular effort should be given to identifying, supporting and treating women identified as being most at risk of malnutrition.
Further analysis of data from RCTs, which include large sub‐groups of women with ovarian cancer (such as RCTs where women with other types of gynaecological cancer are also included), could provide more information concerning the effect of nutrition interventions specific to this population group.
Replication of the early feeding intervention in a further RCT and with the inclusion of women who may have additional co‐morbidities will confirm whether early oral fluids and foods should be recommended as standard practice for women with ovarian cancer undergoing surgery either with or without bowel surgery.
What's new
| Date | Event | Description |
|---|---|---|
| 5 January 2022 | Amended | No longer for update as any future update will require the development of a new protocol reflecting current Cochrane methodological criteria. |
History
Protocol first published: Issue 4, 2012 Review first published: Issue 9, 2013
Acknowledgements
We thank Chris Williams and Jo Morrison for clinical and editorial advice, Jane Hayes for designing the search strategy and Gail Quinn and Clare Jess for their contribution to the editorial process. We additionally thank Janice Lui for study translation. Dr Sorrel Burden was supported by a Post Doctoral Fellowship Grant from Macmillan Cancer Support.
The National Institute for Health Research (NIHR) is the largest single funder of the Cochrane Gynaecological Cancer Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the NIHR, NHS or the Department of Health.
Appendices
Appendix 1. CENTRAL/DARE search strategy
CENTRAL/DARE
#1 MeSH descriptor Perioperative Care explode all trees #2 MeSH descriptor Perioperative Period explode all trees #3 peri‐operative or perioperative #4 MeSH descriptor Surgical Procedures, Operative explode all trees #5 Any MeSH descriptor with qualifier: SU #6 surg* or operat* or procedure* #7 (#1 OR #2 OR #3 OR #4 OR #5 OR #6) #8 MeSH descriptor Nutrition Therapy explode all trees #9 MeSH descriptor Nutrition Disorders explode all trees #10 MeSH descriptor Nutritional Status, this term only #11 MeSH descriptor Nutrition Assessment, this term only #12 MeSH descriptor Cachexia, this term only #13 weight or underweight or cachexi* or malnutrition #14 nutrition* or nutrient* or macronutrient* or micronutrient* or immunonutrition or immunonutrition #15 MeSH descriptor Foodexplode all trees #16 food* or feed* or supplement* or vitamin* or mineral* or protein* or fat* or carbohydrate* or calorie* or energy #17 MeSH descriptor Dietexplode all trees #18 Any MeSH descriptor with qualifier: DH #19 diet* #20 MeSH descriptor Fish Oils explode all trees #21 MeSH descriptor Amino Acids explode all trees #22 amino acid* or fatty acid* or fish oil* or omega 3 or glutamin* or arginine or novel substrate* or nitrogen #23 MeSH descriptor Feeding Methods explode all trees #24 enteral or parenteral of PN or TPN or naso‐gastric or nasogastric or gastrostomy or jejunostomy #25 (#8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24) #26 MeSH descriptor Genital Neoplasms, Female explode all trees #27 MeSH descriptor Ovarian Neoplasms explode all trees #28 (gynaecologic* or gynecologic* or ovar*) near/5 (cancer* or tumor* or tumour* or malignan* or carcinoma* or adenocarcinoma*) #29 (#26 OR #27 OR #28) #30 (#7 AND #25 AND #29)
Appendix 2. Medline search strategy
Medline Ovid
1 exp Perioperative Care/ 2 exp Perioperative Period/ 3 (peri‐operative or perioperative).mp. 4 exp Surgical Procedures, Operative/ 5 surgery.fs. 6 (surg* or operat* or procedure*).mp. 7 1 or 2 or 3 or 4 or 5 or 6 8 exp Nutrition Therapy/ 9 exp Nutrition Disorders/ 10 Nutritional Status/ 11 Nutrition Assessment/ 12 Cachexia/ 13 (weight or underweight or cachexi* or malnutrition).mp. 14 (nutrition* or nutrient* or macronutrient* or micronutrient* or immunonutrition or immuno‐nutrition).mp. 15 exp Food/ 16 (food* or feed* or supplement* or vitamin* or mineral* or protein* or fat* or carbohydrate* or calorie* or energy).mp. 17 exp Diet/ 18 diet therapy.fs. 19 diet*.mp. 20 exp Fish Oils/ 21 exp Amino Acids/ 22 (amino acid* or fatty acid* or fish oil* or omega 3 or glutamin* or arginine or novel substrate* or nitrogen).mp. 23 exp Feeding Methods/ 24 (enteral or parenteral or TPN or naso‐gastric or nasogastric or gastrostomy or jejunostomy).mp. 25 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 26 exp Genital Neoplasms, Female/ 27 exp Ovarian Neoplasms/ 28 ((gynaecologic* or gynecologic* or ovar*) adj5 (cancer* or tumor* or tumour* or malignan* or carcinoma* or adenocarcinoma*)).mp. 29 26 or 27 or 28 30 randomized controlled trial.pt. 31 controlled clinical trial.pt. 32 randomized.ab. 33 placebo.ab. 34 clinical trials as topic.sh. 35 randomly.ab. 36 trial.ti. 37 30 or 31 or 32 or 33 or 34 or 35 or 36 38 7 and 25 and 29 and 37~ 39 exp animals/ not humans.sh. 40 38 not 39
key: mp=protocol supplementary concept, rare disease supplementary concept, title, original title, abstract, name of substance word, subject heading word, unique identifier pt=publication type ab=abstract sh=subject heading fs=floating subheading
Appendix 3. Embase search strategy
1 perioperative period/ 2 (peri‐operative or perioperative).mp. 3 exp surgery/ 4 su.fs. 5 (surg* or operat* or procedure*).mp. 6 1 or 2 or 3 or 4 or 5 7 exp diet therapy/ 8 exp nutritional disorder/ 9 exp nutritional status/ 10 nutritional assessment/ 11 cachexia/ 12 (weight or underweight or cachexi* or malnutrition).mp. 13 (nutrition* or nutrient* or macronutrient* or micronutrient* or immunonutrition or immuno‐nutrition).mp. 14 exp Food/ 15 (food* or feed* or supplement* or vitamin* or mineral* or protein* or fat* or carbohydrate* or calorie* or energy).mp. 16 exp diet/ 17 diet*.mp. 18 fish oil/ 19 exp amino acid/ 20 (amino acid* or fatty acid* or fish oil* or omega 3 or glutamin* or arginine or novel substrate* or nitrogen).mp. 21 exp food intake/ 22 (enteral or parenteral or PN or TPN or naso‐gastric or nasogastric or gastrostomy or jejunostomy).mp. 23 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 24 exp female genital tract tumor/ 25 exp ovary tumor/ 26 ((gynaecologic* or gynecologic* or ovar*) adj5 (cancer* or tumor* or tumour* or malignan* or carcinoma* or adenocarcinoma*)).mp. 27 24 or 25 or 26 28 crossover procedure/ 29 double‐blind procedure/ 30 randomized controlled trial/ 31 single‐blind procedure/ 32 random*.mp. 33 factorial*.mp. 34 (crossover* or cross over* or cross‐over*).mp. 35 placebo*.mp. 36 (double* adj blind*).mp. 37 (singl* adj blind*).mp. 38 assign*.mp. 39 allocat*.mp. 40 volunteer*.mp. 41 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 42 6 and 23 and 27 and 41 43 (exp Animal/ or Nonhuman/ or exp Animal Experiment/) not Human/ 44 42 not 43
[mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Minig 2009a.
| Study characteristics | ||
| Methods | Randomised controlled trial | |
| Participants | Women aged 18 to 75 with preoperative diagnosis of gynaecological malignancy undergoing laparotomy with associated intestinal resection, at the European Institute of Oncology, Milan, Italy between 2007 to 2008. 18/22 women in the intervention group had ovarian cancer (82%) in comparison with 17/18 women (94%) in the control group. Other women in the study had either cancer of the endometrium or fallopian tube; FIGO staging was not reported. The median age of the women in the intervention group was 54 and in the control group was 58 (not significantly different). Sixty‐two per cent of the women had undergone previous unspecified surgery while a smaller number (17%) had been given preoperative chemotherapy in the preceding six months. The women in the study underwent a variety of surgical procedures, the most frequent of which included rectosigmoid (large bowel) resection (75% of women), 70% had hysterectomy (removal of womb) and/or adnexectomy (removal of fallopian tubes and/or ovaries) and the same number had omentectomy (removal of the abdominal lining). Upper abdominal surgery occurred in 38% of the women, there were no significant differences between the intervention and control group in the types of surgery that occurred, in the median operative time or in intraoperative complications, which occurred in 35% of the patients. Perioperative care was standardised during the study and included preoperative bowel preparation, naso‐gastric tube insertion for the duration of surgery and pharmacological regimes for pain, nausea and vomiting. Discharge from hospital occurred when regular diet had been tolerated for at least 24 hours with the resumption of bowel function and when normal clinical measures and physical examination were satisfactory. | |
| Interventions | Nutrition status was evaluated using subjective global assessment and a standardised questionnaire to categorise women as well nourished, moderately nourished or severely malnourished, patients categorised as severely malnourished were excluded from the trial. Postoperatively, early oral feeding (EOF) was compared with a "traditional" postoperative feeding regimen (TOF). Patients in the EOF were offered liquids (mineral water, tea, chamomile infusion or apple juice) during the first 24 hours postoperatively; after 24 hours, if liquids were well tolerated, the women commenced on a regular diet of beef, chicken or fish for the duration of hospital stay. Patients allocated to the TOF regimen remained 'nil by mouth' until there was evidence of bowel sounds and passage of flatus, after which, if they did not have nausea and emesis, they were switched to an oral liquid diet for 24 hours, provided this was well tolerated, they were placed on a semi‐solid diet for a further 24 hours and again if this was well tolerated, they were then prescribed the regular diet. | |
| Outcomes | The primary outcome was length of hospital stay. Other outcome measures examined were recovery of intestinal activity, intensity of abdominal pain, presence of nausea and vomiting, postoperative complications, analgesic and antiemetic drug requirements, patient satisfaction level and QoL (assessed by standard questionnaires EORTC QLQ‐C30 and EORTC QLQ‐OV28). Following discharge from hospital, outcomes continued to be assessed with weekly telephone calls for the subsequent 30 days. | |
| Notes | Exclusions preoperatively were for any of: infection, intestinal obstruction, severe malnutrition, ASA score ≥ 4 or planned pelvic exenteration; postoperative exclusion from the study was made if admission to ICU ≥ 24 hours or if the malignancy was found to be non‐gynaecologic. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer web‐based randomisation (TENALEA 2013). |
| Allocation concealment (selection bias) | Low risk | Web‐based randomisation was used prior to commencement of intervention. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | More than 20% of patients (22%) were randomised but then excluded from the trial and the analysis, however post‐intervention exclusion was for pre‐determined reasons (admission to ICU for ≥ 24 hours, non‐gynaecologic malignancy). |
| Selective reporting (reporting bias) | Unclear risk | Primary and secondary end‐points were reported. Trial protocol was not seen. |
| Other bias | Low risk | Although there was an significant imbalance in the groups for estimated blood loss (EBL) and FIGO stage and volume of ascites were not reported, the authors report that these factors did not have a significant impact on either nutritional group in terms of length of hospital stay. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to assess risk of bias. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to assess risk of bias. |
ASA: American Society of Anesthesiologists FIGO: Federation of Gynecology and Obstetrics ICU: intensive care unit QoL: quality of life
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Celik 2009 | Fewer than 75% of the women in this RCT had ovarian cancer (32%). The study is a comparison of two types of enteral feeding given perioperatively to women with gynaecological malignancies. |
| Cutillo 1999 | Fewer than 75% of the women in this RCT had ovarian cancer (48%). The study examined early postoperative oral feeding in comparison with nasogastric decompression and delayed feeding in women who had major surgery for gynaecological cancer. |
| Feng 2008 | Fewer than 75% of the women in this RCT had ovarian cancer (18%). This study evaluated the introduction of a semi‐liquid diet in comparison with clear fluids, 6 hours after major abdominal surgery for gynaecological cancer. |
| Gerardi 2008 | Not a RCT (prospective and retrospective comparison). The study is an evaluation of a clinical pathway which included rapid diet advancement following cytoreductive surgery with intestinal resection. |
| Marx 2006 | Not a RCT (prospective and retrospective comparison). The study evaluated the introduction of a multi‐modal rehabilitation programme including early oral feeding in comparison with conventional care in women undergoing surgery for ovarian cancer. |
| Minig 2009b | Fewer than 75% of the women in this RCT had ovarian cancer (58%). This study compared early oral feeding and traditional oral feeding in women following major abdominal surgery for gynaecological cancer. |
| Nuutinen 1982 | RCT was not undertaken in the perioperative phase of treatment for ovarian cancer. A study of nutrition support during chemotherapy for gynaecological cancer. |
| Pearl 1998 | Fewer than 100% of the women in this RCT had cancer (75%) Fewer than 75% of the women in this RCT had ovarian cancer (32%). This study compared the early introduction of a liquid diet in comparison with delayed postoperative feeding in women undergoing gynaecological intra‐abdominal surgery. |
| Pearl 2002 | Fewer than 100% of the women in this RCT had cancer (79%) Fewer than 75% of the women in this RCT had ovarian cancer (33%). This study compared the effect of introducing a normal diet in comparison with clear liquids one day after intraabdominal gynaecological surgery. |
| Schilder 1997 | Fewer than 100% of the women in this RCT were diagnosed with cancer (55%). An evaluation of early postoperative oral feeding in women following major gynaecological surgery. |
| Spirtos 1988 | Fewer than 75% of the women in this RCT had ovarian cancer (49%). An evaluation of postoperative feeding of an elemental diet via jejunostomy tube in comparison with a control group given IV fluids. |
| Steed 2002 | Fewer than 100% of the women in this RCT were diagnosed with cancer (58%). This study examined early postoperative oral feeding in comparison with delayed feeding in 96 women undergoing major abdominal gynaecological cancer. |
| Tan 2002 | No indication in the text (translated from Chinese) that randomisation had been used to allocate the women to the intervention and control groups. |
IV: intravenous RCT: randomised controlled trial
Characteristics of ongoing studies [ordered by study ID]
QCGC OPEN study.
| Study name | Post‐operative enteral nutrition in patients with epithelial ovarian cancer (OPEN) |
| Methods | Interventional randomised controlled trial |
| Participants | Women aged over 18 undergoing planned cytoreductive surgery for ovarian, primary peritoneal or fallopian tube cancer who have been identified as having signs of moderate or severe malnutrition using the Patient‐Generated Subjective Global Assessment method.. |
| Interventions | Women will be randomised to commence enteral (tube) feeding directly into the small bowel, commencing 4 hours postoperatively, after 24 hours feeds will be gradually increased to an individualised goal rate, this will be in addition to standard post‐surgery care. Women randomised to standard postoperative diet will be given intravenous fluids and increasing oral diet as tolerated. |
| Outcomes | Length of stay in hospital and related costings, length of stay in intensive care unit or high dependency unit, Quality of life measured preoperatively, 6 weeks after surgery and following the 3rd course of postoperative chemotherapy, use of inotropic medication to support blood pressure and kidney function, using standardised questionnaire, intravenous treatment requirements, treatment‐related adverse events, delay and dose reductions of chemotherapy administered postoperatively. |
| Starting date | February 2009 |
| Contact information | Dana Middleton, Queensland Centre for Gynaecological Cancer, Level 6 Ned Hanlon Building, Royal Brisbane and Women's Hospital, Herston Qld 4029, Australia Email: dana_middleton@health.qld.gov.au |
| Progress of study | Currently recruiting |
| Notes | ClinicalTrials.gov Identification: NCT00850772 |
Differences between protocol and review
Some minor clarification of methods was made at the request of reviewers which did not affect how the present review was undertaken but would be incorporated into future updates of this review. Due to time constraints, some tasks were undertaken by different authors than originally planned. As only one study was identified for inclusion, it was not necessary to use some statistical analysis as detailed in the protocol. If we had obtained further studies, then the following elements of the protocol would have been used and these will be incorporated in future updates as appropriate
Assessment of heterogeneity
We planned to assess heterogeneity between studies by visual inspection of forest plots, by estimation of the percentage heterogeneity between trials that could not be ascribed to sampling variation (Higgins 2003), by a formal statistical test of the significance of the heterogeneity (Deeks 2001) and, if possible, by subgroup analyses (Subgroup analysis and investigation of heterogeneity). If there was evidence of substantial heterogeneity, we planned to investigate and report the possible reasons for this.
Assessment of reporting biases
We intended to examine funnel plots corresponding to meta‐analysis of the primary outcome to assess the potential for small‐study effects such as publication bias. If these plots suggested that treatment effects were not sampled from a symmetric distribution, as assumed by the random‐effects model, we would have performed further meta‐analyses using fixed‐effect models.
Data synthesis
If sufficient, clinically similar studies were available, their results would have been pooled in meta‐analyses.
For time‐to‐event data, we planned to pool hazard ratios (HRs) using the generic inverse variance facility of RevMan 5.
For any dichotomous outcomes, the RR would have been calculated for each study and these were then to be pooled.
For continuous outcomes, we planned to pool the mean differences between the treatment arms at the end of follow‐up if all trials measured the outcome on the same scale, otherwise standardised mean differences would have been used.
If any trials had multiple treatment groups, the ‘shared’ comparison group would have been divided into the number of treatment groups and comparisons between each treatment group and the split comparison group would have been treated as an independent comparison.
We planned to use random‐effects models with inverse variance weighting for all meta‐analyses (DerSimonian 1986) if data allowed.
If possible, studies making different comparisons would have been synthesised using the methods of Bucher 1997.
Subgroup analysis and investigation of heterogeneity
We planned to undertake subgroup analysis on studies if data allowed grouping the trials by:
malnourished versus non‐malnourished; trials conducted before and after 1990 (since when there have been significant developments in artificial feeding and nutrition support);
factors such as age, stage, type of intervention, length of follow‐up, adjusted/unadjusted analysis were planned to be considered in the interpretation of any heterogeneity.
Contributions of authors
The protocol and review was drafted by HAB who also co‐ordinated the review and undertook data entry. CH provided specialist advice that the focus of the review should be on women with ovarian cancer and provided a clinical perspective to the review and to the interpretation of data. JC was involved in designing the review, screening search results and screening retrieved papers for eligibility, VLD was involved in designing the review, screening retrieved papers, extracting data from papers and appraising the quality of papers. LK was involved in designing the review, screening retrieved papers for eligibility, liaison with the interpreter, extracting data from papers and appraising the quality of papers, LJL was involved in designing the review, screening retrieved papers for eligibility, the design of data extraction forms, liaison with the interpreter, extracting data from papers and appraising the quality of papers, AJW was involved in the design of the review and the design of data extraction forms. SB supervised HAB, conceived and initiated the review to examine the nutritional requirements of patients with gynaecological cancer, screened retrieved papers and provided methodological perspective to the review. All authors reviewed both the draft protocol and draft review, which was subsequently amended to reflect their comments.
Sources of support
Internal sources
This work was supported by the NIHR Manchester Biomedical Research Centre, UK
External sources
No sources of support provided
Declarations of interest
None known.
Edited (no change to conclusions)
References
References to studies included in this review
Minig 2009a {published data only}
- Minig L, Biffi R, Zanagnolo V, Attanasio A, Beltrami C, Bocciolone L, et al. Early oral versus "traditional" postoperative feeding in gynecologic oncology patients undergoing intestinal resection: a randomized controlled trial. Annals of Surgical Oncology 2009;16(6):1660-8. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Celik 2009 {published data only}
- Celik JB, Gezginc K, Ozcelik K, Celik C. The role of immunonutrition in gynecologic oncologic surgery. European Journal of Gynaecological Oncology 2009;30(4):418-21. [PMID: ] [PubMed] [Google Scholar]
Cutillo 1999 {published data only}
- Cutillo G, Maneschi F, Franchi M, Giannice R, Scambia G, Benedetti-Panici P. Early feeding compared with nasogastric decompression after major oncologic gynecologic surgery: a randomized study. Obstetrics and Gynecology 1999;93(1):41-5. [PMID: ] [DOI] [PubMed] [Google Scholar]
Feng 2008 {published data only}
- Feng S, Chen L, Wang G, Chen A, Qiu Y. Early oral intake after intra-abdominal gynecological oncology surgery. Cancer Nursing 2008;31(3):209-13. [PMID: ] [DOI] [PubMed] [Google Scholar]
Gerardi 2008 {published data only}
- Gerardi MA, Santillan A, Meisner B, Zahurak ML, Diaz Montes TP, Giuntoli RL 2nd, et al. A clinical pathway for patients undergoing primary cytoreductive surgery with rectosigmoid colectomy for advanced ovarian and primary peritoneal cancers. Gynecologic Oncology 2008;108(2):282-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
Marx 2006 {published data only}
- Marx C, Rasmussen T, Jakobsen DH, Ottosen C, Lundvall L, Ottesen B, et al. The effect of accelerated rehabilitation on recovery after surgery for ovarian malignancy. Acta Obstetricia et Gynecologica Scandinavica 2006;85(4):488-92. [PMID: ] [DOI] [PubMed] [Google Scholar]
Minig 2009b {published data only}
- Minig L, Biffi R, Zanagnolo V, Attanasio A, Beltrami C, Bocciolone L, et al. Reduction of postoperative complication rate with the use of early oral feeding in gynecologic oncologic patients undergoing a major surgery: a randomized controlled trial. Annals of Surgical Oncology 2009;16(11):3101-10. [PMID: ] [DOI] [PubMed] [Google Scholar]
Nuutinen 1982 {published data only}
- Nuutinen LS, Kauppila A, Ryhänen, Niinimäki A, Kivinen S, Saarela M, et al. Intensified nutrition as an adjunct to cytotoxic chemotherapy in gynaecological cancer patients. Clinical Oncology 1982;8:107-12. [PubMed] [Google Scholar]
Pearl 1998 {published data only}
- Pearl ML, Valea FA, Fischer M, Mahler L, Chalas E. A randomized controlled trial of early postoperative feeding in gynecologic oncology patients undergoing intra-abdominal surgery. Obstetrics and Gynecology 1998;92(1):94-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Pearl 2002 {published data only}
- Pearl ML, Frandina M, Mahler L, Valea FA, DiSilvestro PA, Chalas E. A randomized controlled trial of a regular diet as the first meal in gynecologic oncology patients undergoing intraabdominal surgery. Obstetrics and Gynecology 2002;100(2):230-4. [PMID: ] [DOI] [PubMed] [Google Scholar]
Schilder 1997 {published data only}
- Schilder JM, Hurteau JA, Look KY, Moore DH, Raff G, Stehman FB, et al. A prospective controlled trial of early postoperative oral intake following major abdominal gynecologic surgery. Gynecologic Oncology 1997;67(3):235-40. [PMID: ] [DOI] [PubMed] [Google Scholar]
Spirtos 1988 {published data only}
- Spirtos NM, Ballon SC. Needle catheter jejunostomy: a controlled, prospective, randomized trial in patients with gynecologic malignancy. American Journal of Obstetrics and Gynecology 1988;158(6 Pt 1):1285-90. [PMID: ] [DOI] [PubMed] [Google Scholar]
Steed 2002 {published data only}
- Steed HL, Capstick V, Flood C, Schepansky A, Schulz J, Mayes DC. A randomized controlled trial of early versus "traditional" postoperative oral intake after major abdominal gynecologic surgery. American Journal of Obstetrics and Gynecology 2002;186(5):861-5. [PMID: ] [DOI] [PubMed] [Google Scholar]
Tan 2002 {published data only}
- Tan WH, Wu J, Tai S, Che JH, Chi Q. The use of parenteral nutrition in postoperative patients with advanced ovarian cancer [(Published in Chinese)]. Parenteral & Enteral Nutrition 2002;9(4):218-20. [Google Scholar]
References to ongoing studies
QCGC OPEN study {published data only}
- Queensland Centre for Gynaecological Cancer (QCGC). Post-operative Enteral Nutrition in Patients with Epithelial Ovarian Cancer (OPEN). ClinicalTrials.gov identifier: NCT00850772.
Additional references
Alphs 2006
- Alphs HH, Zahurak ML, Bristow RE, Diaz-Montes TP. Predictors of surgical outcome and survival among elderly women diagnosed with ovarian and primary peritoneal cancer. Gynecologic Oncology 2006;103(3):1048-53. [DOI] [PubMed] [Google Scholar]
ASPEN 2011
- Mueller C, Compher C, Ellen DM and the American Society for Parenteral and Enteral Nutrition. A.S.P.E.N. clinical guidelines: nutrition screening, assessment and intervention in adults. Journal of Parenteral and Enteral Nutrition 2011;35:16-24. [DOI] [PubMed] [Google Scholar]
Balogun 2011
- Balogun N, Forbes A, Widschwendter M, Lanceley A. Changes in nutritional status of women diagnosed and treated for ovarian cancer. In: Proceedings American Institute for Cancer Research annual research meeting on food, nutrition, physical activity and cancer; 2011 Nov 3-4; Washington, DC. 2011.
Balogun 2012
- Balogun N, Forbes A, Widschwendter M, Lanceley A. Noninvasive nutritional management of ovarian cancer patients: beyond intestinal obstruction. International Journal of Gynecological Cancer 2012;22(6):1089-95. [PMID: ] [DOI] [PubMed] [Google Scholar]
Benedet 2000
- Benedet JL, Bender H, Jones H 3rd, Ngan HY, Pecorelli S. FIGO staging classifications and clinical practice guidelines in the management of gynecologic cancers. FIGO Committee on Gynecologic Oncology. International Journal of Gynaecology and Obstetrics 2000;70(2):209-62. [PubMed] [Google Scholar]
Brooks 1994
- Brooks SE. Preoperative evaluation of patients with suspected ovarian cancer. Gynecologic Oncology 1994;55:S80-S90. [DOI] [PubMed] [Google Scholar]
Bucher 1997
- Bucher HC, Guyatt GH, Griffith LE, Walter SD. The results of direct and indirect treatment comparisons in meta-analysis of randomized controlled trials. Journal of Clinical Epidemiology 1997;50(6):683-91. [DOI] [PubMed] [Google Scholar]
Caprino 2006
- Caprino P, Fagotti A, Missere M, Fanfani F, Scambia G. Severe prolonged gastroparesis after cytoreductive surgery in an advanced ovarian cancer patient. International Journal of Gynecological Cancer 2006;16(5):1936-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Charoenkwan 2007
- Charoenkwan K, Phillipson G, Vutyavanich T. Early versus delayed oral fluids and food for reducing complications after major abdominal gynaecologic surgery. Cochrane Database of Systematic Reviews 2007, Issue 4. Art. No: CD004508. [DOI: 10.1002/14651858.CD004508.pub3] [CD004508] [DOI] [PubMed] [Google Scholar]
Clarke‐Pearson 1988
- Clarke-Pearson DL, DeLong ER, Chin N, Rice R, Creasman WT. Intestinal obstruction in patients with ovarian cancer. Variables associated with surgical complications and survival. Archives of Surgery 1988;123(1):42-5. [PMID: ] [DOI] [PubMed] [Google Scholar]
Deeks 2001
- Deeks JJ, Altman DG, Bradburn MJ. Statistical methods for examining heterogeneity and combining results from several studies in meta-analysis. In: Egger M, Davey Smith G, Altman DG, editors(s). Systematic Reviews in Health Care: Meta-Analysis in Context. 2nd edition. London: BMJ Publication Group, 2001:285-312. [Google Scholar]
DerSimonian 1986
- DerSimonian R, Laird N. Meta-analysis in clinical trials. Controlled Clinical Trials 1986;7:177-88. [DOI] [PubMed] [Google Scholar]
Donato 1992
- Donato D, Angelides A, Irani H, Penalver M, Averette H. Infectious complications after gastrointestinal surgery in patients with ovarian carcinoma and malignant ascites. Gynecologic Oncology 1992;44(1):40-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
EORTC QLQ‐C30
- Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. Journal of the National Cancer Institute 1993;85(5):365-76. [PMID: ] [DOI] [PubMed] [Google Scholar]
EORTC QLQ‐OV28
- Greimel E, Bottomley A, Cull A, Waldenstrom AC, Arraras J, Chauvenet L, et al. An international field study of the reliability and validity of a disease-specific questionnaire module (the QLQ-OV28) in assessing the quality of life of patients with ovarian cancer. European Journal of Cancer (Oxford, England : 1990) 2003;39(10):1402-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Geisler 2007
- Geisler JP, Linnemeier GC, Thomas AJ, Manahan KJ. Nutritional assessment using prealbumin as an objective criterion to determine whom should not undergo primary radical cytoreductive surgery for ovarian cancer. Gynecologic Oncology 2007;106(1):128-31. [PMID: ] [DOI] [PubMed] [Google Scholar]
GLOBOCAN 2008
- Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. GLOBOCAN 2008, cancer Incidence and Mortality Worldwide: IARC CancerBase No. 10 [Internet]. Lyon, France: International Agency for Research on Cancer; 2010. Available from: http://globocan.iarc.fr (accessed 2nd July 2013).
Gupta 2008
- Gupta D, Lammersfeld CA, Vashi PG, Dahlk SL, Lis CG. Can subjective global assessment of nutritional status predict survival in ovarian cancer? Journal of Ovarian Research 2008;1(1):5. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gupta 2010
- Gupta D, Lis CG, Vashi PG, Lammersfeld CA. Impact of improved nutritional status on survival in ovarian cancer. Supportive Care in Cancer 2010;18(3):373-81. [PMID: ] [DOI] [PubMed] [Google Scholar]
Henry 2011
- Henry C. Effect of malnutrition on cancer patients. In: Shaw C, editors(s). Nutrition and Cancer. Wiley-Blackwell, 2011:45-82. [Google Scholar]
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane-handbook.org.
Kondrup 2003
- Kondrup J, Allison SP, Elia M, Vellas B, Plauth M. ESPEN guidelines for nutrition screening 2002. Clinical Nutrition 2003;22(4):415-21. [DOI] [PubMed] [Google Scholar]
Krebs 1983
- Krebs HB, Goplerud DR. Surgical management of bowel obstruction in advanced ovarian carcinoma. Obstetrics and Gynecology 1983;61(3):327-30. [PMID: ] [PubMed] [Google Scholar]
Laky 2008
- Laky B, Janda M, Cleghorn G, Obermair A. Comparison of different nutritional assessments and body-composition measurements in detecting malnutrition among gynecologic cancer patients. American Journal of Clinical Nutrition 2008;87(6):1678-85. [PMID: ] [DOI] [PubMed] [Google Scholar]
Laky 2010
- Laky B, Janda M, Kondalsamy-Chennakesavan S, Cleghorn G, Obermair A. Pretreatment malnutrition and quality of life - association with prolonged length of hospital stay among patients with gynecological cancer: a cohort study. BioMed Central Cancer 2010;10:232. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Larson 1989
- Larson JE, Podczaski ES, Manetta A, Whitney CW, Mortel R. Bowel obstruction in patients with ovarian carcinoma: analysis of prognostic factors. Gynecologic Oncology 1989;35(1):61-5. [PMID: ] [DOI] [PubMed] [Google Scholar]
Lv 2010
- Lv D, Wang X, Shi G. Perioperative enhanced recovery programmes for gynaecological cancer patients. Cochrane Database of Systematic Reviews 2010, Issue 6. Art. No: CD008239. [DOI: 10.1002/14651858.CD008239.pub2] [DOI] [PubMed] [Google Scholar]
NICE 2006
- National Collaborating Centre for Acute Care. Nutrition support in adults: oral nutrition support, enteral tube feeding and parenteral nutrition. National Collaborating Centre for Acute Care, London. Available from http://www.nice.org.uk/CG32 February 2006. [Commissioned by the National Institute for Clinical Excellence Available from www.rcseng.ac.uk] [PubMed]
Ravasco 2005
- Ravasco P, Monteiro-Grillo I, Vidal PM, Camilo ME. Dietary counselling improves patient outcomes: a prospective, randomized, controlled trial in colorectal cancer patients undergoing radiotherapy. Journal of Clinical Oncology 2005;23(7):1431-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Ravasco 2005a
- Ravasco P, Monteiro-Grillo I, Marques Vidal P, Camilo ME. Impact of nutrition on outcome: a prospective randomized controlled trial in patients with head and neck cancer undergoing radiotherapy. Head & Neck 2005;27(8):659-68. [PMID: ] [DOI] [PubMed] [Google Scholar]
Rubin 1989
- Rubin SC, Hoskins WJ, Benjamin I, Lewis JL Jr. Palliative surgery for intestinal obstruction in advanced ovarian cancer. Gynecologic Oncology 1989;34(1):16-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Tangitgamol 2010
- Tangjitgamol S, Manusirivithaya S, Laopaiboon M, Lumbiganon P, Bryant A. Interval debulking surgery for advanced epithelial ovarian cancer. Cochrane Database of Systematic Reviews 2010, Issue 10. Art. No: CD006014. [DOI: 10.1002/14651858.CD006014.pub5] [DOI] [PubMed] [Google Scholar]
TENALEA 2013
- Trans European Network for Clinical Trials Services. https://nl.tenalea.net/amc/ALEA (accessed 2nd July 2013).
Tunca 1983
- Tunca JC. Nutritional evaluation of gynecologic cancer patients during initial diagnosis of their disease. American Journal of Obstetrics and Gynecology 1983;147(8):893-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
Zorlini 2008
- Zorlini R, Akemi Abe Cairo A, Salete Costa Gurgel M. Nutritional status of patients with gynecologic and breast cancer. Nutricion Hospitalaria 2008;23(6):577-83. [PMID: ] [PubMed] [Google Scholar]


