Abstract
Background
The COVID-19 pandemic is presumably having an impact on the consumption of psychoactive substances. Social distancing and lockdown measures may particularly affect the use of “party drugs” (e.g., stimulants, dissociatives, and GHB/GBL) through the absence of typical use settings. We aimed to analyse the use patterns of those substances and underlying motivations before and during the pandemic.
Methods
A subsample of 1,231 users of stimulants (amphetamine, methamphetamine, MDMA/ecstasy, cocaine), dissociative drugs (ketamine, dextromethorphan, PCP), and GHB/GBL was assessed from 30th April to 4th August 2020 as part of the Corona Drug Survey, a cross-sectional international online survey in five languages that included a total of 5,049 participants. The reported use of distinct substances and the underlying motivations were ascertained before (retrospectively) and during the pandemic. Furthermore, associations between drug use as a coping mechanism, pandemic-related stressors, and substance use were examined.
Results
Regarding the reported frequency of use during the pandemic, 48.0–64.8% of the sample ceased or decreased, 11.9–25.5% maintained, and 23.6–29.1% increased their consumption. MDMA/ecstasy showed the strongest decrease and GHB/GBL and dissociatives the highest increase. Participants reported that price, quality, and supply were mostly unaffected by the pandemic. The most common motivations before and during the pandemic were mood-related factors, such as a desire to feel exhilarated, euphoric, high, or buzzed. The relevance of social purposes and mood-related motivators declined during the pandemic, whereas dealing with boredom increased. Overall, 16.4–35.6% perceived drug use as helpful for dealing with pandemic-related stressors, which were associated with an increased consumption frequency.
Conclusion
The early stage of the COVID-19 pandemic was associated with major changes in the use of “party drugs”. Those who increased their level of drug use and perceived it as a coping strategy in particular might be targeted with adaptive preventive and therapeutic measures.
Keywords: Corona, Substance use, Ketamine, Amphetamine, Cocaine, MDMA
Introduction
The spread of the Coronavirus SARS-CoV-2 which causes the disease COVID-19 led to an unprecedented worldwide pandemic. The influence of the pandemic on substance use was already anticipated at the beginning of the COVID-19 pandemic, and warnings of an increase in use were issued (World Health Organization, 2020). Furthermore, differences were expected between the consumption of alcohol, cannabis, different “party drugs”, and other substances (EMCDDA, 2020; World Health Organization, 2020). The rather loosely defined term of “party drugs” often refers to stimulant, mood-enhancing, and euphoriant substances that are commonly consumed in recreational “party” settings (e.g., nightclubs, festivals, raves). Stimulants (e.g., amphetamine, methamphetamine, 3,4-methylenedioxymethamphetamine [MDMA/ecstasy], cocaine), dissociatives (e.g., ketamine, dextromethorphan, phencyclidine [PCP]), and ɣ-hydroxybutyrate (GHB)/ɣ-butyrolactone (GBL) are frequently grouped into this category (Betzler et al., 2019; Edland-Gryt, Sandberg, & Pedersen, 2017; Palamar, Acosta, Le, Cleland, & Nelson, 2019; Reinstadler et al., 2021). Unlike the other substances included in this study, of which the effects are well known, GHB/GBL is a comparatively new substance, has a dose-dependent stimulant or sedative effect and is prevalent in party settings (Betzler et al., 2019). Alcohol and cannabis are often consumed in recreational settings as well, but they are not included in the narrower definition of party drugs. Whereas, on average, increases in the consumption of alcohol and cannabis were anticipated and confirmed, research into the use of typical party drugs during the pandemic is lacking and an overall decrease was conjectured due to the relative absence of parties and other recreational events (EMCDDA, 2020; Winstock et al., 2020b).
During the COVID-19 lockdown in spring 2020, wastewater analyses provided insight into objectively measured changes in the consumption of psychoactive substances at the community level (EMCDDA, 2020; Reinstadler et al., 2021): compared to pre-pandemic levels, the markers decreased substantially for MDMA (−28%), amphetamine (−23%), and cocaine (−6% to −25%) in Austria, the Netherlands, and Spain. The markers for methamphetamine were more than doubled in Austria (Reinstadler et al., 2021). Finland and Norway recorded increases in amphetamine and GHB (EMCDDA, 2020).
Quantitative online surveys with subjective self-rating assessments mostly replicated these findings. A large survey during the first three months of the pandemic in Europe revealed that almost half (46%) of the 7,352 participants that formerly used illegal drugs reported no or less drug consumption during the early pandemic (EMCDDA, 2020). Nevertheless, about 30% used the same amount, and 25% even increased their drug use. The use of party drugs in particular decreased according to the international Global Drug Survey (Winstock et al., 2020a; Winstock et al., 2020b). In contrast, alcohol and cannabis showed inverse patterns, with a larger number of increases than reductions and the percentage of risky drinking particulary increased (Institute of Alcohol Studies, 2020).
Changes in the use of psychoactive substances can be influenced by various pandemic-related factors (EMCDDA, 2020). Firstly, the measures intended to contain the spread of the virus, such as the stipulations for social distancing and the temporary closure of bars, clubs, gatherings, festivals, and other events, massively limited the opportunity to use drugs in social, recreational settings (EMCDDA, 2020; Palamar, Le, & Acosta, 2020). This seems to have particularly affected substances commonly used in this context, such as MDMA and cocaine (EMCDDA, 2020; Palamar et al., 2020). Secondly, disruptions in drug markets – from production to retail level – may have reduced the availability of several substances (EMCDDA, 2020; UNODC, 2020). Thirdly, unemployment rates skyrocketed, and the pandemic posed massive financial and/or mental distress to the majority of people, which, in turn, is known to be associated with elevated substance use (UNODC, 2020; Vanderbruggen et al., 2020). Furthermore, the pandemic-caused economic downturn has the potential to lead to financial shortages and, therefore, either a reduction in drug use or a shift towards less costly licit substances (EMCDDA, 2020) or cheaper and potentially more harmful illegal substances (similar to findings after the financial crisis of 2008) (UNODC, 2020). An example is the shift to the enhanced use of methamphetamine as a substitute for amphetamine and cocaine during the COVID-19 lockdown in Austria (Reinstadler et al., 2021) and Italy (UNODC, 2020).
Recreational occasional users tended to reduce their use of alcohol (Chodkiewicz, Talarowska, Miniszewska, Nawrocka, & Bilinski, 2020; Sidor & Rzymski, 2020; Sun et al., 2020) and cannabis (EMCDDA, 2020) during the pandemic, whereas regular/heavy users tended to increase their amount of consumption. Older age was associated with more frequent use of cocaine and MDMA in a US-partygoer sample (Palamar et al., 2020), whereas a more pronounced consumption of illegal substances (Wainwright et al., 2020) was associated with younger age in studies from Belgium and the US.
Besides the amount of drug use, the consumption contexts changed; solitary use particularly increased (Dumas, Ellis, & Litt, 2020; Palamar & Acosta, 2020). Consuming alone constitutes a potential risk behaviour, as well as behaviours facilitating virus transmission and increasing the probability for severe disease outcomes (Dietze & Peacock, 2020; Harris, 2020; Jacka, Phipps, & Marshall, 2020; Marski, Meaiki, & Shanouda, 2020; Melamed, Hauck, Buckley, Selby, & Mulsant, 2020). Furthermore, the use of illegal substances was, as a risk factor, cross-sectionally and prospectively associated with stronger pandemic-related anxiety and fears (Bendau et al., 2020; Petzold et al., 2020).
The substantial increases in the consumption of alcohol, cannabis, and prescription benzodiazepines (37%) were particularly explained by the attempt to maladaptively cope with anxiety, depression, isolation, and loneliness (Bartel, Sherry, & Stewart, 2020; Rolland et al., 2020; Winstock et al., 2020a; Winstock et al., 2020b). Mental health issues were a risk factor for the increase in cannabis use as a maladaptive coping strategy (Winstock et al., 2020b) and higher levels of anxiety and psychological distress (Bendau et al., 2021). Regarding the use of specific “party drugs” as maladaptive coping mechanisms, evidence is lacking.
The findings of a partial increase in substance use, especially alcohol, are congruent with results from previous epidemics and pandemics, crises, and disasters, such as hurricanes (Kishore, 2008; Ma & Smith, 2017), the global financial crisis in 2008 (Dietze & Peacock, 2020; UNODC, 2020), and major terrorist attacks (Gargano, Nguyen, DiGrande, & Brackbill, 2016; Rehm et al., 2020). However, the COVID-19 pandemic is, in many ways, a unique and unparalleled crisis, as it can be considered a worldwide, rapidly developing disaster with unknown scale and impact on multiple dimensions of physical and mental health (Dietze & Peacock, 2020). In light of the large-scale restrictions and enormous economic, social and political consequences of the pandemic, previous events are limited in their transferability and predictive power (Dietze & Peacock, 2020). Therefore, it is important to examine the changes and differences in several illegal substances and their associations with the underlying motivations for drug use and the pandemic-related circumstances beyond existing research. This is particularly relevant for identifying vulnerable populations and addressing them with adaptive preventive and therapeutic measures.
Previous research hardly differentiates between different stimulants and other illegal substances and is mostly limited to smaller regional samples (Dietze & Peacock, 2020; Palamar et al., 2020). Most existing studies focus on relative changes and do not ascertain the absolute frequencies of substance use before and during the pandemic (EMCDDA, 2020; Sutherland et al., 2020). Furthermore, a comprehensive analysis of motivational factors, pandemic-related strains, and their associations with the use of “party drugs” is lacking. Our study aims to address these knowledge gaps. For this purpose, we conducted a detailed systematic analysis of the reported frequency and underlying motivations of the use of stimulants (amphetamine, methamphetamine, MDMA/ecstasy, cocaine), dissociatives (ketamine, PCP), and GHB/GBL in a large international sample. Furthermore, we examined exploratory associations between drug use as a coping mechanism, pandemic-related stressors, and substance use.
Methods
Design, eligibility criteria, and recruitment
The cross-sectional study data were collected as part of the international online-based Corona Drug Survey with a non-probability self-selected convenience sample of 5,049 participants. The study was online from 30 April (when 3,110,995 cases of COVID-19 infections worldwide, including 225,258 deaths, had been confirmed) to 4 August 2020 (23,755,191 confirmed cases, including 821,143 deaths) (World Health Organization, 2021).
The survey was carried out online on the secure web-based platform SoSci Survey (Leiner, 2019a). Recruitment was done on an international level via articles in online magazines, advertisement on several webpages and social media, electronic postings, and e-mail announcements. Interposed with the link to the survey was the project landing page, which provided detailed information about the survey. All participants gave written informed consent prior to completing the survey, and participation was fully anonymous and voluntary. It was kindly requested that all items be answered, but not mandatory (to avoid frustration and drop-outs resulting from obligatory/forced answers). All answers were based on self-rating/self-report. The study was approved by the ethics committee of the Charité – Universitätsmedizin Berlin, Germany (EA1/109/20).
The aim of the umbrella project was to investigate how the consumption of psychoactive substances (alcohol, nicotine, cannabis, benzodiazepines, cocaine, amphetamine, methamphetamine, MDMA/ecstasy, GHB/GBL, dissociatives, psychedelics, opioids, and new psychoactive substances) had changed in the context of the COVID-19 pandemic. The survey was available in five languages (English, German, Spanish, Italian, Korean). The inclusion criteria were the ability to complete the survey in one of those languages, the minimum age of 18 years, and the consumption of at least one of the above-named psychoactive substances in 2019 or 2020.
The present analysis focuses on stimulants (amphetamine, methamphetamine, MDMA)/ecstasy, cocaine), dissociatives (ketamine, dextromethorphan, PCP), and GHB/GBL. Participants that reported the use of one of those substances in 2020 or 2019 and provided further information about the usage frequency were included in the analysis.
Assessment
Sociodemographic and pandemic-related information
The survey contained questions about sociodemographic information, such as age, gender, country of origin, country of current residence, educational level, and work-related situation before and during the pandemic. Furthermore, we examined how much the participants and their environments were affected by pandemic measures. The degree of limitation in social contact and other restrictions, work-related consequences as well as states of quarantine, and whether the individual had tested (positive) for SARS-CoV-2 were recorded. Moreover, subjective worries and concerns, as well as the self-efficacy to deal with the situation and adherence to preventive measures were obtained. A change in psychopathologic strain during the pandemic compared to the pre-pandemic state was assessed with a slightly modified version of the self-rating Symptom Checklist short version-9 (SCL-K-9) (Prinz et al., 2013). The 5-point Likert scale for rating the severity of each of the nine items was modified to directly assess how much more or less (in comparison to before the pandemic) the individual was bothered or distressed over the past seven days by several psychopathological symptoms (from −2 “much less” to 2 “much more”).
Motivation and frequency of the use of stimulants, dissociatives, and GHB/GBL
The frequency of use before (retrospectively) and during the COVID-19 pandemic (in the last four weeks) was reported on an ordinal-scaled, seven-point format from “never” (0) to “daily” (6) for each substance separately. Furthermore, for the substances that were reportedly consumed, the contextual factors of drug use (where, with whom, aspects of quality, price, and supply constraints), and underlying motivations for drug use were examined retrospectively for the state before the pandemic and for the current situation during the last four weeks. Motivational aspects were assessed with 17 items based on Boys, Marsden, and Strang (2001) and Betzler et al. (2019) in five dimensions (changing mood, physical effects, social purposes, facilitate activity, modify effects of other substances). Furthermore, it was assessed whether the users experienced those substances as helpful in dealing with the pandemic in general and particularly with regard to social isolation.
Data analysis
A total of 17,444 clicks on the survey questionnaire has been recorded. Only participants that had consumed at least one of the included substances in 2019 or 2020 and reported the frequency of its use before and during the pandemic have been included in the analysis (N = 5,049). Furthermore, datasets were excluded if they exhibited more than 40 missing answers, completed less than 10 pages (where the substance-related section of the survey started), showed obvious discrepancies (e.g., mutually exclusive responses) or exceeded the recommended cut-off of the relative speed index (2.0) (Leiner, 2019b); this procedure reduced the sample from 5,049 to 4,915 participants.
All analyses were carried out with IBM SPSS Statistics Version 26. Missing data were handled by listwise deletion (Little's MCAR test was not significant and the data may be assumed to be missing completely at random). Descriptive statistics provided the core of the analysis. Due to the ordinal-scaled indication of the frequency of use, partly small subgroups and the rather exploratory focus of the analysis, we used non-parametric tests for inferential analyses. We applied Kruskal-Wallis Tests to examine gender differences (independent variable; female, male, non-binary/diverse/other) with regard to the changes in the consumption frequency (dependent variable; peri-pandemic minus pre-pandemic frequency) for each substance. Spearman's rank correlations were used to test for associations of changes of the frequency of substance use with age for each substance. We did not examine other demographic characteristics (e.g., educational level, family status, etc.) with regard to changes in consumption frequency because we expected that the implications of those characteristics vary substantially between different countries and therefore the results would be neither very informative nor interpretable. To analyse changes in the motives (relative proportions) of substance use from before to during the pandemic, we applied McNemar tests besides the descriptive examination. Furthermore, we carried out spearman's rank correlations (with statistical control for the pre-pandemic frequency of drug use) to test correlations of the extent to which one perceived substance use as helpful for coping with the pandemic and the changes in the frequency of use for each substance. In the next step, we divided the sample into two groups (those who perceived substance use as not helpful for coping with the pandemic vs those evaluating it as slightly, moderately, very or extremely helpful) and calculated Spearman's rank correlations of the extent of pandemic stressors with the ordinal-scaled frequency of substance use during the pandemic for each of the two groups and each substance separately. We did not adjust for demographic characteristics or other potential confounding / effect modifying variables because neither the associations between the frequency of use and age nor gender differences were significant for the majority of included substances. Furthermore, the applied non-parametric tests complicate the inclusion of any confounding variables. Due to the descriptive and exploratory focus of the analysis we did not account for multiple testing. For all analyses, the significance level was set to 0.05 (two-tailed).
Results
Sample characteristics
Of the original adjusted sample of N = 4,915 participants (after applying the exclusion criteria described in the data analysis section), 31.1% (n = 1,529) reported having used cocaine in 2020 or 2019. This makes cocaine the most frequent “party drug” in our sub-sample. It is followed by MDMA/ecstasy, which was consumed by 26.7% (n = 1,313) of the sample, amphetamine and/or methamphetamine (19.6%; n = 963), and dissociatives (e.g., ketamine; 15.3%; n = 753). GHB/GBL was the rarest substance with 3.2% (n = 155) users. We included only participants in further analyses that gave detailed information regarding at least one stimulant or dissociative drug or GHB/GBL (cocaine: 16.2%, n = 795; MDMA/ecstasy: 15.4%, n = 756; dissociatives: 8.1%, n = 398; amphetamine: 7.5%, n = 369; methamphetamine: 1.8%, n = 89; GHB/GBL: 1.1%, n = 55); the final study sample thus comprised N = 1231 individuals.
The final sample consisted of 53.2% (n = 655) male, 43.4% (n = 534) female, and 1.9% (n = 24) non-binary/diverse identifying individuals; 18 participants did not specify their gender. The mean age was 27.95 years (SD = 8.26; Range: 18–69). In our sample, 2.8% (n = 35) of the participants had no school degree, 9.3% (n = 114) an intermediate or lower secondary school degree, 34.2% (n = 420) an upper secondary school degree, 42.5% (n = 523) a university degree, and 11.3% (n = 139) a completed apprenticeship. A majority of 80.4% of the individuals (n = 990) reported that they have no children. The participants lived in 45 different countries: 55.8% of the sample (n = 687) resided in Europe, 24.3% (n = 299) in South America, 15.5% (n = 191) in North America, 2.3% (n = 28) in Africa, 1.6% (n = 20) in Asia, and 0.5% (n = 6) in Australia.
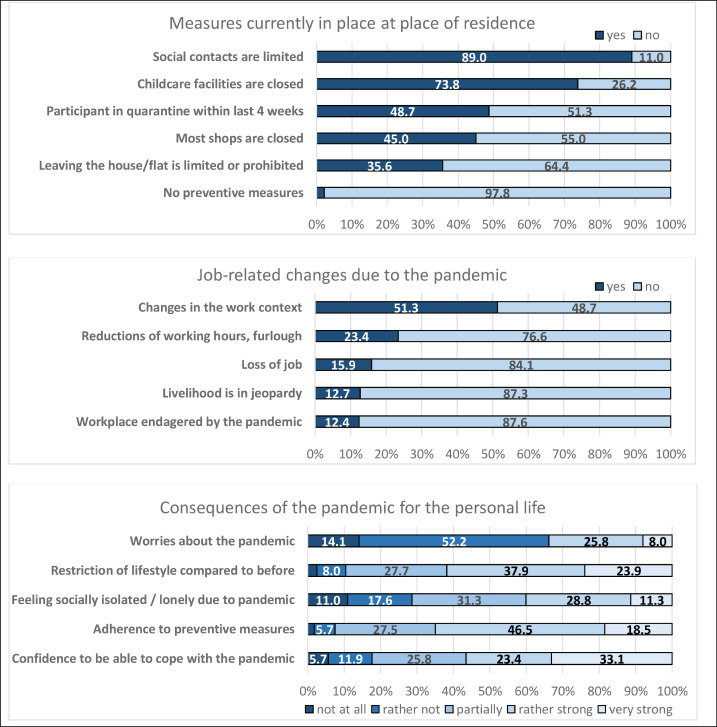
Pandemic-related situation during data collection
Fig. 1 gives an overview of the pandemic-related consequences for the participants. The vast majority reported restrictions such as limitations in social contacts, about one half experienced work-related changes, one third expressed worries about the pandemic, and the majority reported that they adhered to preventive measures.
Fig. 1.
Overview of the consequences related to the COVID-19 pandemic for the participants (N = 1,321).
The average difference score of the modified SCL-9 was M = 0.40 (SD = 0.66) with a range from −2 to 2. This indicates that, on average, the mental strain was not or only slightly increased during the pandemic compared to before. Nevertheless, some participants felt much less strain in all nine SCL items, whereas others perceived much more strain.
Frequency of substance use before and during the pandemic
Almost half of the participants (45.3%, n = 558) had consumed only one type of stimulant, dissociative, or GHB/GBL in 2019 and/or 2020; 25.0% (n = 308) had used two, 16.9% (n = 208) three, and 12.7% (n = 157) four or more different substances.
Table 1 shows the frequency of drug use before and during the COVID-19 pandemic. Large parts of the sample used drugs rather occasionally (less than one time per month) before the pandemic. During the pandemic, the majority never used drugs in the last four weeks or approximately once. Between 48.0% (amphetamine) and 64.8% (MDMA) of the participants decreased the consumption of those specific substances, whereas about one quarter reported increased drug use. The reported consumption of GHB/GBL and dissociatives in particular increased by a substantial percentage (each 29.1%). MDMA showed comparatively the smallest percentage of constant substance use (11.9%), whereas amphetamine displayed the most prominent (25.5%).
Table 1.
Reported frequency of drug use before and during the COVID-19 pandemic (N = 1,321).
| Amphetamine (n = 369) | Metamphetamine (n = 89) | MDMA /Ecstasy (n = 756) | GHB/GBL (n = 55) | Cocaine (n = 795) | Dissociative drugs (n = 398) | ||
|---|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | ||
| Before the pandemic | never (0) | 14 (3.8) | 8 (9.0) | 37 (4.9) | 8 (14.5) | 50 (6.3) | 28 (7.0) |
| <1x per month (1) | 130 35.2) | 38 (42.7) | 489 (64.7) | 28 (50.9) | 355 (44.7) | 207 (52.0) | |
| ∼1x per month (2) | 56 (15.2) | 5 (5.6) | 125 (16.5) | 6 (10.9) | 134 (16.9) | 57 (14.3) | |
| 2–4x per month (3) | 102 (27.6) | 14 (15.7) | 96(12.7) | 7 (12.7) | 153 (19.2) | 77 (19.3) | |
| 2–3x per week (4) | 34 (9.2) | 7 (7.9) | 5 (0.7) | 4 (7.3) | 62 (7.8) | 16 (4.0) | |
| 4–6x per week (5) | 12 (3.3) | 2 (2.2) | 3 (0.4) | 0 (0.0) | 18 (2.3) | 11 (2.8) | |
| Daily (6) | 21 (5.7) | 15 (16.9) | 1 (0.1) | 2 (3.6) | 23 (2.9) | 2 (0.5) | |
| During the pandemic (in the last 4 weeks) | never in 4weeks (1) | 138 (37.4) | 44 (49.4) | 487 (64.4) | 32 (58.2) | 410 (51.6) | 202 (50.6) |
| <1x per month (1) | 83(22.5) | 18 (20.2) | 198 (26.2) | 14 (25.2) | 159 (20.0) | 86 (21.6) | |
| ∼1x per month (2) | 85 (23.0) | 12 (13.5) | 64 (8.5) | 4 (7.3) | 146 (18.4) | 74 (18.5) | |
| 2–4x per month (3) | 34 (9.2) | 9 (10.1) | 5 (0.7) | 1 (1.8) | 51 (6.4) | 24 (6.0) | |
| 2–3x per week (4) | 11 (3.0) | 0 (0.0) | 1 (0.1) | 3 (5.5) | 12 (1.5) | 7 (1.8) | |
| 4–6x per week (5) Daily (6) | 18 (4.9) | 6 (6.7) | 1 (0.1) | 1 (1.8) | 17 (2.1) | 6 (1.5) | |
| Difference (during minus pre-pandemic) | Decrease | 117 (48.0) | 47 (52.8) | 490 (64.8) | 31 (56.4) | 431 (54.2) | 210 (52.8) |
| Unchanged | 94 (25.5) | 21 (23.6) | 90 (11.9) | 8 (14.5) | 152 (19.1) | 72 (18.1) | |
| Increase | 98 (26.5) | 21 (23.6) | 176 (23.3) | 16 (29.1) | 212 (26.7) | 116 (29.1) | |
| Modal | −1 | −1 | −1 | −1 | −1 | −1 | |
| Median | 0 | −1 | −1 | −1 | −1 | −1 | |
| M | −0.41 | −0.83 | −0.59 | −0.44 | −0.55 | −0.32 | |
| SD | 1.57 | 2.05 | 1.29 | 1.50 | 1.69 | 1.51 | |
| Min.; Max. | −6; 6 | −6; 3 | −5; 4 | −6; 2 | −6; 5 | −5; 6 | |
| Most common context | Before pandemic | Club: 318 (85.7) | At home: 64 (70.3) | Club: 643 (85.1) | Club: 34 (61.8) | Club: 639 (79.9) | At home: 284 (70.8) |
| During pandemic | At home: 196 (84.8) | At home: 33 (73.3) | At home: 214 (79.6) | At home: 20 (87.0) | At home: 294 (76.4) | At home: 172 (87.3) | |
| Price | Decrease | 16 (4.7) | 7 (8.1) | 12 (1.9) | 1 (1.9) | 20 (2.9) | 4 (1.2) |
| Unchanged | 299 (88.2) | 63 (73.3) | 520 (80.6) | 41 (78.8) | 498 (72.2) | 287 (82.5) | |
| Increase | 24 (7.1) | 16 (18.6) | 103 (17.5) | 10 (19.2) | 172 (25.0) | 57 (4.6) | |
| Quality | Decrease | 35 (10.4) | 10 (11.7) | 56 (8.7) | 2 (3.9) | 147 (21.5) | 28 (8.1) |
| Unchanged | 288 (85.0) | 65 (76.5) | 554 (86.7) | 48 (94.1) | 498 (72.7) | 303 (87.3) | |
| Increase | 16 (4.7) | 10 (11.8) | 29 (4.6) | 1 (2.0) | 40 (5.9) | 16 (4.6) | |
| Delivery / supply constraint | Decrease | 9 (4.0) | 6 (10.6) | 19 (5.4) | 1 (3.8) | 18 (4.2) | 40 (19.6) |
| Unchanged | 193 (85.8) | 43 (75.4) | 266 (75.6) | 19 (73.1) | 312 (74.3) | 153 (75.0) | |
| Increase | 23 (10.2) | 8 (14.1) | 57 (18.0) | 6 (23.0) | 90 (21.5) | 11 (5.4) |
Note. During the pandemic, “never in the last 4 weeks” is treated equivalent with “<1x per month”. Difference scores are calculated by the pandemic minus the pre-pandemic frequency; negative values thus indicate a decrease in the frequency of drug use and positive values an increase.
The most frequently reported location of drug use changed across substances from “in the club” before the pandemic to “at home” during the pandemic – except for methamphetamine and dissociatives, where the most frequently reported consumption context was “at home” even before the pandemic. The majority reported no substantial changes in price, quality, or supply constraints due to the pandemic. The largest change was evident for cocaine with regard to an increase in the price (reported by 25% of the users) and a decrease in quality (reported by 21.5%).
Except for MDMA (Kruskal-Wallis Test: χ²(2) = 12.784, p = .002) there were no significant gender differences evident with regard to the changes in the consumption frequency (all p ≥ 0.171). Non-binary individuals showed on average an increased frequency of MDMA use, whereas male and female participants in contrast reported a decrease. For cocaine (rS = 0.208; p < 0.001) and dissociatives (rS = 0.194; p < 0.001), age was positively associated with a relative increase of substance use; the other substance groups showed an insignificant trend in the same direction (all p ≥ 0.055).
Motivation for substance use before and during the pandemic
Table 2 descriptively displays different motivational aspects for drug use before and during the COVID-19 pandemic. For both time periods, across substances, the most commonly reported motivation was “to feel exhilarated and euphoric”, followed by “just to get high or buzzed”. Furthermore, “staying awake” was a frequent reason for amphetamine, methamphetamine, MDMA, and cocaine use, whereas “relaxing” was a common motivation for GHB and dissociatives. The relative number of users who reported social purposes (e.g., to enjoy the company of friends; to be more self-confident in social situations), physical effects (e.g., staying awake), and mood change (e.g., to feel exhilarated and euphoric) as motivators decreased from before to during the pandemic. In contrast, dealing with boredom increased substantially as a reason for substance use during the pandemic. Furthermore, in participants who reported using GHB, an increase in using this substance to “feel better when sad or in a bad mood” and “escape from a problem” was evident – however, it should be taken into account that this finding is based on a very few individuals.
Table 2.
Motivation for the use of stimulants and dissociatives before and during the COVID-19 pandemic (N = 1,321).
| What do you expect from the immediate effect | Amphetamine |
Metamphetamine |
MDMA/Exctasy |
GHB/GBL |
Cocaine |
Dissociative drugs |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Before (n = 355) | During (n = 231) | Before (n = 81) | During (n = 45) | Before (n = 719) | During (n = 269) | Before (n = 47) | During (n = 23) | Before (n = 745) | During (n = 385) | Before (n = 370) | During (n = 197) | |
| I take it to… | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) |
|
Changing mood … feel better when I'm sad or in a bad mood … escape from a problem … relax … feel exhilarated and euphoric … just to get high or buzzed |
73 (21.0)* 47 (13.5) 61 (17.2)* 236 (66.5) 190 (53.5) |
55 (23.8)* 37 (16.0) 41 (17.7)* 146 (63.2) 115 (49.8) |
35 (43.2)* 25 (30.9)* 28 (34.6)* 57 (70.4)* 51 (63.0)* |
15 (33.3)* 11 (24.4)* 12 (26.7)* 26 (57.8)* 23 (51.1)* |
126 (17.5)* 85(11.8)* 238 (33.1)* 606 (84.3)* 471 (65.5)* |
46 (17.1)* 36 (13.4)* 87 (32.3)* 190 (70.6)* 156 (58.0)* |
4 (8.5) 3 (6.4) 21 (44.7)* 36 (76.6)* 37 (78.7)* |
6 (26.1) 6 (26.1) 10 (43.1)* 15 (65.2)* 19 (82.6)* |
204 (27.4)* 147 (19.7)* 178 (23.9)* 554 (74.4)* 469 (63.0)* |
106 (27.5)* 67 (17.4)* 103 (26.8)* 241 (62.6)* 207 (53.8)* |
86 (23.2)* 79 (21.4)* 207 (55.9)* 225 (60.8)* 275 (74.3)* |
51 (25.9)* 51 (25.9)* 110 (55.8)* 103 (52.3)* 130 (66.0)* |
|
Physical effects … enhance my sexual feelings or for pleasure … stay awake … sleep … lose weight |
80 (23.0)* 295 (84.8)* 1 (0.3) 61 (17.5)* |
44 (19.0)* 164 (71.0)* 1 (0.4) 38 (16.5)* |
26 (32.1)* 52 (64.2)* 5 (6.2) 24 (29.6)* |
13(28.9)* 17 (37.8)* 3 (6.7) 7 (15.6)* |
242 (33.7)* 198 (27.5)* 16 (2.2) 40 (5.6)* |
64 (23.8)* 32 (11.9)* 7 (2.6) 14 (5.2)* |
31 (66.0)* 5 (10.6) 7 (14.9) 3 (6.4) |
14 (60.9)* 3 (13.0) 5 (21.7) 2 (8.7) |
205 (27.5)* 455 (61.1)* 26 (3.5)* 71 (9.5)* |
83 (21.6)* 145 (37.7)* 10 (2.6)* 35 (9.1)* |
58 (15.7)* 31 (8.4)* 60 (16.2)* 17 (4.6)* |
26 (13.2)* 10 (5.1)* 27 (13.7)* 5 (2.5)* |
|
Social purposes … enjoy the company of my friends … to put myself in other people's shoes … be more self-confident in social situations … ease my anxiety |
125 (35.9)* 17 (4.9) 116 (32.7)* 45 (12.9)* |
75 (32.5)* 11 (4.8) 66 (28.6)* 34 (14.7)* |
32 (39.5)* 8 (9.9)* 27 (33.3)* 22 (27.2)* |
7 (15.6)* 0 (0.0)* 11 (24.4)* 11 (24.4)* |
380 (52.9)* 113 (15.7)* 228 (31.7)* 120 (16.7)* |
107 (39.8)* 36 (13.4)* 43 (16.0)* 33 (12.3)* |
19 (40.4)* 5 (10.6) 16 (34.0)* 11 (23.4)* |
10 (43.5)* 3 (13.0) 6 (26.1)* 5 (21.7)* |
338 (45.4)* 38 (5.1)* 274 (26.8)* 130 (17.4)* |
130 (33.8)* 12 (3.1)* 79 (20.5)* 48(12.5)* |
139 (37.6)* 35 (5.9)* 52 (14.1)* 71 (19.2)* |
58 (29.4)* 16 (7.6)* 18 (9.1)* 46 (23.4)* |
|
Facilitate activity … concentrate while studying or working … more efficient in everyday activities … deal with boredom |
107 (30.7)* 107 (30.7)* 85 (24.4) |
66 (28.9)* 82 (35.5)* 79 (34.2) |
33 (40.7)* 44 (54.3)* 34 (42.0)* |
13 (28.9)* 17 (37.8)* 18 (40.0)* |
0 (0.0) 29 (4.0)* 124 (17.2)* |
0 (0.0) 9 (3.3)* 67 (24.9)* |
2 (4.3) 3 (6.4) 17 (36.2) |
1 (4.3) 1 (4.3) 12 (52.2) |
126 (16.9)* 132 (17.7)* 205 (27.5)* |
46 (11.9)* 61 (15.8)* 137 (35.6)* |
16 (4.3)* 17 (4.6) 111 (30.0)* |
6 (3.0)* 10 (5.1) 82 (41.6)* |
| Modify effects of other substances | 93 (26.7)* | 52 (22.8)* | 28 (34.6)* | 11 (24.4)* | 212 (29.5)* | 64 (23.8)* | 17 (36.2)* | 6 (26.1)* | 220 (29.5)* | 91 (23.6)* | 145 (39.2)* | 56 (28.4)* |
Note. Choosing multiple options was possible. Bold font marks a relative decrease of at least 5% and underlined font a relative increase of at least 5% of the percentage which reported this source of motivation. Asterisks (*) indicate a significant difference (p ≤ 0.05) between the relative frequencies before and during the pandemic according to McNemar Tests.
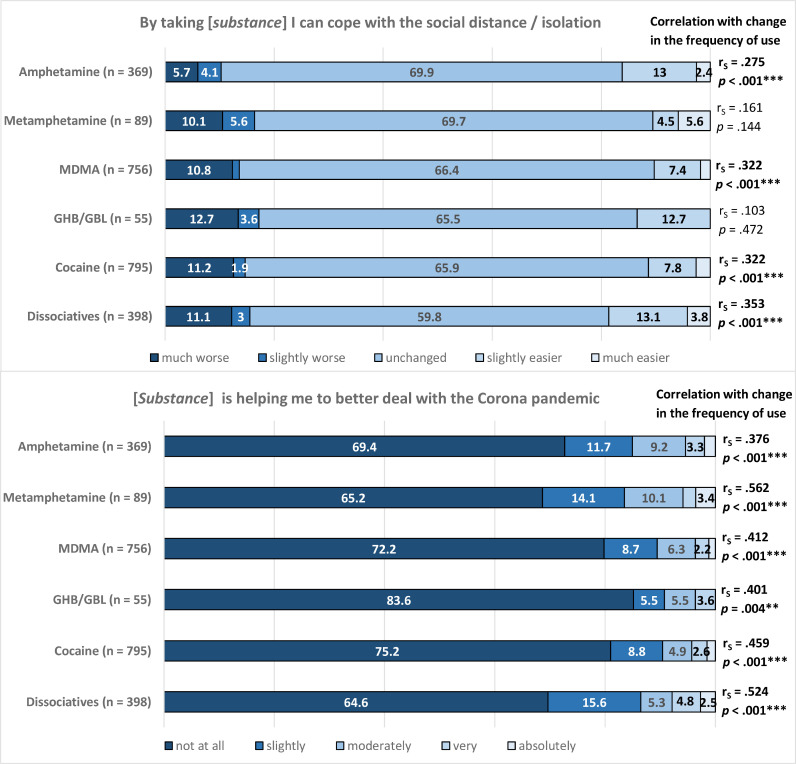
Fig. 2 shows to what extent the participants evaluated drug use as a “coping strategy” that helped to deal with social isolation and the COVID-19 pandemic in general. The majority (64.4% [methamphetamine] to 83.6% [GHB/GBL]) perceived substance use as not supportive in dealing with the pandemic. The ability to deal with social isolation seemed relatively unaffected by drug use for large percentages of the participants (59.8% [dissociatives] to 69.9% [amphetamine]).
Fig. 2.
Drug use as a “coping strategy” and its association with changes in the amount of use.
Note. The bars present percentages. The right column displays partial non-parametric Spearman rank correlation coefficients of the extent of drug use as a coping strategy with the difference in frequency (controlled for baseline frequency of substance use). Significance levels: *** p < 0.001, ** p < 0.01, * p < 0.05.
The extent to which individuals perceived substance use as helpful in general and particularly as a coping strategy regarding isolation was significantly positively correlated with an increased frequency of substance use from before to during the pandemic for almost all examined substances (except isolation in users of methamphetamine and GHB due to small group sizes).
Association with pandemic-related stressors and mechanisms
Table 3 shows the moderation of the associations of pandemic-related stressors with substance use during the pandemic by the perception of drugs as a coping strategy. For users of amphetamine, stronger pandemic-related restrictions, strains, and concerns were associated with significantly less frequent drug use when they evaluated those substances as not helpful in dealing with the pandemic. In contrast, users that perceived drug use as helpful showed weaker associations or even positive trends. The same pattern was visible for cocaine use, whereas the patterns for the other substance groups were less consistent.
Table 3.
Associations with pandemic-related stressors and mechanisms with the consumption frequency during the pandemic – grouped by the evaluation of drug use as helpful coping strategy vs. not helpful.
| Amphetamine | Metamphe-tamine | MDMA/Ecstasy | GHB/GBL | Cocaine | Dissociative drugs | |||
|---|---|---|---|---|---|---|---|---|
| Pandemic stressors | Helpful to cope? | rS (p) df | (n = 369) | (n = 89) | (n = 756) | (n = 55) | (n = 795) | (n = 398) |
| SCL-9 | Not helpful | −0.019 (0.829) 124 | .011 (0.950) 37 | .037 (0.518) 300 | .230 (0.248) 27 | −0.186 (0.001⁎⁎⁎) 337 | .194 (0.020*) 143 | |
| Helpful | .044 (0.762) 50 | .096 (0.075) 18 | .081 (0.461) 86 | .433 (0.467) 5 | .141 (0.193) 87 | −0.119 (0.335) 68 | ||
| Corona Concern | Not helpful | −0.179 (0.004⁎⁎) 256 | .042 (0.753) 58 | −0.051 (0.238) 546 | .052 (0.732) 46 | −0.152 (<0.001⁎⁎⁎) 598 | −0.048 (0.446) 257 | |
| Helpful | −005 (0.965) 97 | −0.119 (0.553) 27 | −0.103 (0.228) 139 | −0.038 (0.929) 8 | −0.127 (0.133) 141 | −0.078 (0.411) 112 | ||
| Life restricted | Not helpful | −0.271 (<0.001⁎⁎⁎) 256 | −0.079 (0.558) 58 | −0.102 (0.017*) 546 | −0.040 (0.792) 46 | −0.215 (<0.001⁎⁎⁎) 598 | −0.122 (0.050*) 257 | |
| Helpful | −0.047 (0.647) 97 | −0.319 (0.044*) 27 | −0.026 (0.760) 139 | −0.050 (0.906) 8 | .001 (0.991) 141 | −0.011 (0.911) 112 | ||
| Isolation | Not helpful | −0.183 (0.003⁎⁎) 256 | .057 (0.673) 58 | −0.056 (0.128) 546 | .286 (0.054) 46 | −0.149 (<0.001⁎⁎⁎) 598 | −0.029 (0.641) 257 | |
| Helpful | .090 (0.382) 97 | −0.003 (0.989) 27 | .099 (0.244) 139 | −0.237 (0.572) 8 | −0.066 (0.434) 141 | −0.012 (0.903) 112 |
Note. Non-parametric Spearman rank correlations. Grouped by “not helpful at all” vs. “slightly + moderately + very + absolutely helpful” in dealing with the pandemic. SCL-9 = Modified 9-item self-rating Symptom Checklist short version. Significance levels: *** p < 0.001, ** p < 0.01, * p < 0.05. Due to the descriptive character of this analysis, we neither accounted for multiple testing, nor compared correlations by inferential statistics.
Discussion
Summary and interpretation of the results
In our study sample, a large percentage of individuals decreased the frequency of or ceased drug use during the pandemic, but a substantial part maintained or even increased the levels of consumption. The majority of active users before and during the pandemic consisted of occasional users that consumed the various substances from a few times per year up to a few times per month. The percentages of reported consumption reduction were higher than in the Global Drug Survey sample with 55,811 participants from May to June 2020 (Winstock et al., 2020b): MDMA (our survey: 65 vs Global Drug Survey: 41%), cocaine (54 vs 38%), amphetamine (48 vs 35%), and dissociatives/ketamine (53 vs 34%). Simultaneously, the percentages of increases were also slightly higher in our sample: cocaine (27 vs 21%), MDMA (23 vs 13%) and dissociatives/ketamine (29 vs 21%). Those differences might arise, for instance, from methodological factors, the broader time period of assessment in our survey, and regional divergences. In specific populations, e.g., electronic dance music partygoers, that typically show a high prevalence of recreational drug use, the reduction rates of cocaine (79%) and MDMA (71%) were even higher than in our sample (Palamar et al., 2020).
In summary, our results fit the assumption that the use of stimulants, dissociatives, and GHB/GBL is typically context-dependent. Thus, the frequency of their use shows, on average, a downturn that parallels the restrictions on recreational settings (EMCDDA, 2020; Palamar et al., 2020). This is furthermore underlined by the finding that for MDMA, GHB, cocaine, and amphetamine, clubs were the most common place of substance use before the pandemic. Not surprisingly, in light of the stay-at-home measures, the largest percentages reported “at home” as the most frequent location during the pandemic. As MDMA is the most typical “party drug” with almost no use in daily life (Edland-Gryt et al., 2017), it is reasonable that MDMA showed the lowest frequencies and the strongest reduction compared to other substances in our and other studies (EMCDDA, 2020).
Those assumptions are supported by the findings of other studies: according to the self-reports of users, the main reasons for less consumption of “party drugs” were fewer occasions (MDMA: 87.2%, cocaine: 80.5%), less contact with the usual partners with whom one consumes (MDMA: 63.5%, cocaine: 70.0%), and not liking to use the drug at home (46.0%, 46.3%), respectively during the pandemic (36.6%, 42.3%) (EMCDDA, 2020; Winstock et al., 2020a). Difficulties in the availability of those substances (17.8%, 23.4%) or the affordability (5.5%, 23.4%) played a subordinate role (Palamar et al., 2020; Winstock et al., 2020a).
The examination of factors that are associated with differences in the frequency of substance use is particularly important. Therefore, in our study, we analysed patterns in the underlying motivations for the use of stimulants, dissociatives, and GHB/GBL before and during the pandemic. While the relative proportion of several motivations (e.g., “relaxing”) remained somewhat stable, the clearest reduction is evident in motivators that are associated with social/recreational settings, such as social purposes and a desire to change the mood to an exhilarated and euphoric, high or buzzed state. The most prominent increase was in using stimulants and dissociatives to deal with boredom. This is in line with European and international findings where boredom as well as reducing anxiety were common reasons for using drugs during the pandemic (EMCDDA, 2020; Winstock et al., 2020a). In a Belgian study, the loss of daily structures, a lack of social contacts, loneliness, a rewarding function, and conviviality were furthermore reported as reasons for peri-pandemic substance use (Vanderbruggen et al., 2020).
Our observation that the reported price and quality increased or decreased in some cases but otherwise remained relatively stable for the different substances is consistent with the findings of Palamar et al. (2020) and EMCDDA and Europol (2020). Disruptions in the drug supply seemed very heterogeneous in several studies, with strong differences between geographical regions and substances (Giommoni, 2020), but on average, the drug supply was mostly robust against pandemic-related circumstances (EMCDDA & Europol, 2020; UNODC, 2020). It might be possible that tangible interruptions would become more apparent with a longer persistence of the pandemic and could not be captured by data collected during the early pandemic. Nevertheless, our findings indicate lower effects of the pandemic on the drug market than those reported in the Global Drug Survey (Winstock et al., 2020a; Winstock et al., 2020b) and may be an indicator that changes in drug use in our sample were not primarily driven by reduced access or changes in quality or prices. Congruent with the findings from Palamar et al. (2020), older age – at least for cocaine and dissociatives – was associated with lower odds for a reduction in the use of those substances.
Considering the small number of users, attention should be paid to the relative elevation in maladaptive coping motivation (escaping from problems and negative emotions) and a large percentage (29.1%) of increased use frequency in users of GHB/GBL. This is particularly important in light of the increased wastewater concentrations of GHB/GBL in Finland and Norway and its rising prevalence in Germany (Betzler et al., 2021; Betzler, Heinz, & Köhler, 2016), as well as the high risk of overdose and addiction potential, which often include severe complications in withdrawal attempts (EMCDDA, 2020; Kamal et al., 2017).
Large percentages of the participants evaluated the use of stimulants, dissociatives, and GHB/GBL as not helpful in dealing with the pandemic in general or with the social distance and isolation. The more drug use was perceived as a helpful coping strategy, the higher one's relative level of substance use during the pandemic was on average. This represents drug use as a maladaptive self-medication/coping strategy, which is particularly relevant with regard to the multiple negative effects of the pandemic (such as unemployment, loneliness, worrying, and worse mental health) that increase the mental burden and pressure for alleviation (Dietze & Peacock, 2020; EMCDDA, 2020).
Furthermore, we examined the moderating role of perceiving drugs as coping mechanisms on the associations of pandemic-related consequences and strains with the frequency of substance use during the pandemic. Overall, the patterns were mixed, but for amphetamine and cocaine, we found a moderating effect of drug use as a coping mechanism. For instance, isolation was negatively correlated with amphetamine use for individuals that did not perceive it as helpful in coping, whereas the association was positive for those who evaluated it as helpful. These findings may help to understand the contradictory results of previous research: for example, social isolation, in some studies, was associated with a higher risk for substance use to reduce negative emotions (Copeland, Fisher, Moody, & Feinberg, 2018; Palamar et al., 2020), whereas in others, isolation was associated with reduced drug use because of fewer peer ties (Kobus & Henry, 2010). In light of our findings, it might be relevant to analyse the subjective evaluation of the function of substance use to predict whether isolation results in higher use due to self-medication purposes or in reduced consumption due to fewer opportunities and less peer ties.
In summary, the pandemic is multifaceted and associated with multiple consequences which have resulted in simultaneous increases and decreases in the use of stimulants, dissociatives, and GHB/GBL. Those who increase their level of drug use and perceive it as a coping strategy for dealing with the multiple challenges of the pandemic in particular may need consideration and mitigation (EMCDDA, 2020). Our survey was carried out during a phase of relative relaxation of infection numbers of the 1st wave and preventive restrictions in most countries, and it can be expected that the problematic role of drug use to deal with the pandemic grows in parallel to the increasing duration and severity of the pandemic. Furthermore, it is possible that problematic shifts persist beyond the end of the pandemic, which emphasizes the relevance of addressing them now with adaptive educational and preventive measures (Dietze & Peacock, 2020), first, with regard to potentially harmful use patterns, and second, to minimize the risk of transmission and severe outcomes of COVID-19 in drug users (Dietze & Peacock, 2020; Jacka et al., 2020; Sutherland et al., 2020). For example, online preventive and therapeutic harm reduction interventions (e.g., similar to programmes regarding alcohol misuse (Kaal et al., 2020; Ornell et al., 2020)) could be used.
Limitations and future research
Besides its strengths, our study has some limitations. Our sample is a self-selected convenience sample. The average of the participants was relatively young and well-educated, some groups may not be adequately represented, and media- and/or drug-affine individuals, as well as those with better access to the internet, might have had a higher probability of taking part. This reduces the generalizability of the results. Furthermore, it cannot be ruled out that demographic characteristics or other confounding variables influence and modify the results.
Most changes in drug use are assumably directly or indirectly influenced by national confinement measures (EMCDDA, 2020). Due to variations in the infection rates and the timing and severity of those measures between different geographical regions and other differences, e.g., in the countries’ economic and social stability, the comparability and generalizability of the results are limited (EMCDDA, 2020; Giommoni, 2020). Furthermore, the distinct substances as well as the different users represent a very heterogenous group that is not unboundedly generalizable for all users of stimulants, dissociatives, and GHB/GBL. In addition, the majority of our sample seem to be rather recreational, sporadic users which may create a bias with respect to pathological heavy users and/or polytoxic drug use.
All answers rely on online self-reports, and the information regarding the use before the pandemic was retrospectively obtained and not actually assessed before the pandemic. This increases the risk for memory and answer biases and the possible presence of purposefully wrong responses cannot be ruled out entirely. Due to the rare use of GHB and methamphetamine, the groups of those users were small, which reduced the informative value of group comparisons. Due to the focus on stimulants, dissociatives, and GHB, as well as the design of our study, we did not analyse a potential shift to other substances such as alcohol or cannabis or interactions between different substances. Furthermore, approximately half of the participants were “polydrug users” (used two or more different substances); as a result, direct comparisons are only possible on the substance level but not on the user level. Our study relies on cross-sectional data, which does not allow any causal conclusions; future longitudinal studies are needed to map courses over time.
Most analyses of this study provide a rather descriptive and exploratory way of examination to take into account these limitations and to build a solid base for future studies and analyses.
Conclusion
In our large international sample of users of stimulants, dissociatives, and GHB/GBL, substantially higher percentages of individuals decreased or ceased than maintained or increased the frequency of use. This reflects that those substances seem to be linked to recreational “party” occasions for large percentages of our sample, and therefore their use decreased in parallel to the interruption of those events due to the pandemic. Nevertheless, it is important to differentiate between different substances, use frequencies, and underlying motivations rather than grouping them all together. Those who increased the use of substances during the pandemic (e.g., to cope with the burdensome circumstances) may need particular consideration.
Our study contributes to the examination of the impact of the pandemic on the patterns of use of psychoactive substances and related harms. Future studies should complement this through research and monitoring – particularly with regard to high-risk users (who may be underrepresented in our sample) that exhibit symptoms of harmful use or dependence (Dietze & Peacock, 2020; EMCDDA, 2020). Those measures need to be interconnected with the provision and availability of health services and aspects of clinical practice and drug policy (Wisse, Burke-Shyne, Chang, & Southwell, 2021; Zolopa et al., 2021). In the short and long term, with respect to the further progress of the pandemic and implications after the pandemic, potentially harmful use patterns need attention and further research. Supervision, prevention, and education on different dimensions, as well as the provision of professional support to deal with difficulties on personal, social, or economic levels, are of high relevance – both during and after the pandemic (Helbig et al., 2019; Wisse et al., 2021; Zolopa et al., 2021).
Ethics
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Declarations of Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Bartel S.J., Sherry S.B., Stewart S.H. Self-isolation: A significant contributor to cannabis use during the COVID-19 pandemic. Substance Abuse. 2020;41(4):409–412. doi: 10.1080/08897077.2020.1823550. [DOI] [PubMed] [Google Scholar]
- Bendau A., Kunas S.L., Wyka S., Petzold M.B., Plag J., Asselmann E., et al. Longitudinal changes of anxiety and depressive symptoms during the COVID-19 pandemic in Germany: The role of pre-existing anxiety, depressive, and other mental disorders. Journal of Anxiety Disorders. 2021;79 doi: 10.1016/j.janxdis.2021.102377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bendau A., Plag J., Kunas S., Wyka S., Ströhle A., Petzold M.B. Longitudinal changes in anxiety and psychological distress, and associated risk and protective factors during the first three months of the COVID-19 pandemic in Germany. Brain and Behavior. 2020;11(2):e01964. doi: 10.1002/brb3.1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betzler F., Ernst F., Helbig J., Viohl L., Roediger L., Meister S., et al. Substance use and prevention programs in Berlin's party scene: Results of the SuPrA-study. European Addiction Research. 2019;25(6):283–292. doi: 10.1159/000501310. [DOI] [PubMed] [Google Scholar]
- Betzler F., Heinz A., Köhler S. Synthetische Drogen – wichtige und neue Substanzen im Überblick [Synthetic Drugs - An overview of important and newly emerging substances] Fortschritte der Neurologie-Psychiatrie. 2016;84(11):690–698. doi: 10.1055/s-0042-117507. [DOI] [PubMed] [Google Scholar]
- Betzler F., Helbig J., Viohl L., Ernst F., Roediger L., Gutwinski S., et al. Drug checking and its potential impact on substance use. European Addiction Research. 2021;27(1):25–32. doi: 10.1159/000507049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boys A., Marsden J., Strang J. Understanding reasons for drug use amongst young people: A functional perspective. Health Education Research. 2001;16(4):457–469. doi: 10.1093/her/16.4.457. [DOI] [PubMed] [Google Scholar]
- Chodkiewicz J., Talarowska M., Miniszewska J., Nawrocka N., Bilinski P. Alcohol consumption reported during the COVID-19 pandemic: The initial stage. International Journal of Environmental Research and Public Health. 2020;17(13) doi: 10.3390/ijerph17134677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland M., Fisher J.C., Moody J., Feinberg M.E. Different kinds of lonely: Dimensions of isolation and substance use in adolescence. Journal of Youth and Adolescence. 2018;47(8):1755–1770. doi: 10.1007/s10964-018-0860-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dietze P.M., Peacock A. Illicit drug use and harms in Australia in the context of COVID-19 and associated restrictions: Anticipated consequences and initial responses. Drug and Alcohol Review. 2020;39(4):297–300. doi: 10.1111/dar.13079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumas T.M., Ellis W., Litt D.M. What does adolescent substance use look like during the COVID-19 pandemic? Examining changes in frequency, social contexts, and pandemic-related predictors. The Journal of Adolescent Health. 2020;67(3):354–361. doi: 10.1016/j.jadohealth.2020.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edland-Gryt M., Sandberg S., Pedersen W. From ecstasy to MDMA: Recreational drug use, symbolic boundaries, and drug trends. International Journal of Drug Policy. 2017;50:1–8. doi: 10.1016/j.drugpo.2017.07.030. [DOI] [PubMed] [Google Scholar]
- EMCDDA, & Europol (2020). EU Drug Markets: Impact of COVID-19.
- EMCDDA (2020). Impact of COVID-19 on patterns of drug use and drug-related harms in Europe.
- Gargano L.M., Nguyen A., DiGrande L., Brackbill R.M. Mental health status of World Trade Center tower survivors compared to other survivors a decade after the September 11, 2001 terrorist attacks. American Journal of Industrial Medicine. 2016;59(9):742–751. doi: 10.1002/ajim.22636. [DOI] [PubMed] [Google Scholar]
- Giommoni L. Why we should all be more careful in drawing conclusions about how COVID-19 is changing drug markets. International Journal of Drug Policy. 2020;83 doi: 10.1016/j.drugpo.2020.102834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris M. An urgent impetus for action: Safe inhalation interventions to reduce COVID-19 transmission and fatality risk among people who smoke crack cocaine in the United Kingdom. International Journal of Drug Policy. 2020;83 doi: 10.1016/j.drugpo.2020.102829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helbig J., Ernst F., Viohl L., Roediger L., Köhler S., Ströhle A., et al. Präventionsansätze zur Reduktion von Konsumrisiken in der Berliner Partyszene [Harm Reduction and Preventive Measures in Berlin's Party Scene] Psychiatrische Praxis. 2019;46(8):445–450. doi: 10.1055/a-0992-6904. [DOI] [PubMed] [Google Scholar]
- Institute of Alcohol Studies (2020). Alcohol consumption during the Covid-19 lockdown in the UK (FINAL).docx. Retrieved from http://www.ias.org.uk/uploads/pdf/IAS%20reports/sb28062020.pdf.
- Jacka B.P., Phipps E., Marshall B.D.L. Drug use during a pandemic: Convergent risk of novel coronavirus and invasive bacterial and viral infections among people who use drugs. International Journal of Drug Policy. 2020;83 doi: 10.1016/j.drugpo.2020.102895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaal E., Schaub M.P., Wenger A., Ülesoo T., Blankers M., Haug S., et al. Testing the efficacy of a minimal-guidance online self-help intervention for alcohol misuse in Estonia: Study protocol of a randomized controlled trial. BMC Public Health. 2020;20(1):790. doi: 10.1186/s12889-020-08791-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamal R.M., van Noorden M.S., Wannet W., Beurmanjer H., Dijkstra B.A.G., Schellekens A. Pharmacological treatment in γ-hydroxybutyrate (GHB) and γ-butyrolactone (GBL) dependence: Detoxification and relapse prevention. CNS Drugs. 2017;31(1):51–64. doi: 10.1007/s40263-016-0402-z. [DOI] [PubMed] [Google Scholar]
- Kishore (2008). Kishore2008_DisasterMedicineArticle.
- Kobus K., Henry D.B. Interplay of network position and peer substance use in early adolescent cigarette, alcohol, and marijuana use. The Journal of Early Adolescence. 2010;30(2):225–245. doi: 10.1177/0272431609333300. [DOI] [Google Scholar]
- Leiner D.J. München: Sosci survey GmbH. 2019. SoSci survey (version 3.1. 06)[computer software] [Google Scholar]
- Leiner D.J. Advance online publication; 2019. Too fast, too straight, too weird: Non-reactive indicators for meaningless data in internet surveys. [DOI] [Google Scholar]
- Ma C., Smith T.E. Increased alcohol use after Hurricane Ike: The roles of perceived social cohesion and social control. Social Science & Medicine. 2017;190(1982):29–37. doi: 10.1016/j.socscimed.2017.08.014. [DOI] [PubMed] [Google Scholar]
- Marski K., Meaiki A., Shanouda M. Levamisole-adulterated cocaine poses a concern during the COVID-19 pandemic. Journal of Addictive Diseases. 2020;38(4):580–581. doi: 10.1080/10550887.2020.1800890. [DOI] [PubMed] [Google Scholar]
- Melamed O.C., Hauck T.S., Buckley L., Selby P., Mulsant B.H. Covid-19 and persons with substance use disorders: Inequities and mitigation strategies. Substance Abuse. 2020;41(3):286–291. doi: 10.1080/08897077.2020.1784363. [DOI] [PubMed] [Google Scholar]
- Ornell F., Moura H.F., Scherer J.N., Pechansky F., Kessler F.H.P., von Diemen L. The COVID-19 pandemic and its impact on substance use: Implications for prevention and treatment. Psychiatry Research. 2020;289 doi: 10.1016/j.psychres.2020.113096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar J.J., Acosta P. Virtual raves and happy hours during COVID-19: New drug use contexts for electronic dance music partygoers. International Journal of Drug Policy. 2020;93 doi: 10.1016/j.drugpo.2020.102904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar J.J., Acosta P., Le A., Cleland C.M., Nelson L.S. Adverse drug-related effects among electronic dance music party attendees. International Journal of Drug Policy. 2019;73:81–87. doi: 10.1016/j.drugpo.2019.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar J.J., Le A., Acosta P. Shifts in drug use behavior among electronic dance music partygoers in New York during COVID-19 social distancing. Substance Use & Misuse. 2020;56(2):1–7. doi: 10.1080/10826084.2020.1857408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petzold M.B., Bendau A., Plag J., Pyrkosch L., Mascarell Maricic L., Betzler F., et al. Risk, resilience, psychological distress, and anxiety at the beginning of the COVID-19 pandemic in Germany. Brain and Behavior. 2020;10(9):e01745. doi: 10.1002/brb3.1745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prinz U., Nutzinger D.O., Schulz H., Petermann F., Braukhaus C., Andreas S. Comparative psychometric analyses of the SCL-90-R and its short versions in patients with affective disorders. BMC Psychiatry. 2013;13:104. doi: 10.1186/1471-244X-13-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J., Kilian C., Ferreira-Borges C., Jernigan D., Monteiro M., Parry C.D.H., et al. Alcohol use in times of the COVID 19: Implications for monitoring and policy. Drug and Alcohol Review. 2020;39(4):301–304. doi: 10.1111/dar.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinstadler V., Ausweger V., Grabher A.-.L., Kreidl M., Huber S., Grander J., et al. Monitoring drug consumption in Innsbruck during coronavirus disease 2019 (COVID-19) lockdown by wastewater analysis. The Science of the Total Environment. 2021;757 doi: 10.1016/j.scitotenv.2020.144006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rolland B., Haesebaert F., Zante E., Benyamina A., Haesebaert J., Franck N. Global Changes and factors of increase in caloric/salty food intake, screen use, and substance use during the early COVID-19 containment phase in the general population in France: Survey study. JMIR Public Health and Surveillance. 2020;6(3):e19630. doi: 10.2196/19630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sidor A., Rzymski P. Dietary Choices and habits during COVID-19 lockdown: Experience from Poland. Nutrients. 2020;12(6) doi: 10.3390/nu12061657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Y., Li Y., Bao Y., Meng S., Sun Y., Schumann G., et al. Brief Report: Increased addictive internet and substance use behavior during the COVID-19 pandemic in China. The American Journal on Addictions. 2020;29(4):268–270. doi: 10.1111/ajad.13066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutherland, R., Baillie, G., Memedovic, S., Hammoud, M., Barratt, M., Bruno, R. et al. (2020). Key findings from the ‘Australians’ drug use: Adapting to Pandemic Threats (ADAPT)’ study. 10.26190/5EFBEF7C8D821. [DOI]
- UNODC (2020). Research Brief: COVID-19 and the drug supply chain: From production and trafficking to use.
- Vanderbruggen N., Matthys F., van Laere S., Zeeuws D., Santermans L., van den Ameele S., et al. Self-reported alcohol, tobacco, and cannabis use during COVID-19 lockdown measures: Results from a web-based survey. European Addiction Research. 2020;26(6):309–315. doi: 10.1159/000510822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wainwright J.J., Mikre M., Whitley P., Dawson E., Huskey A., Lukowiak A., et al. Analysis of drug test results before and after the US declaration of a national emergency concerning the COVID-19 outbreak. Journal of the American Medical Association. 2020;324(16):1674–1677. doi: 10.1001/jama.2020.17694. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winstock, A. R., Davies, E. L., Gilchrist, G., Zhuparris, A., Ferris, J. A., Maier, L. J. et al. (2020a). Global drug survey: Special edition on COVID-19. Interim report global.
- Winstock, A. R., Zhuparris, A., Gilchrist, G., Davies, E. L., Puljevic, C., Potts, L. et al. (2020b). Global drug survey - Special edition on COVID-19. Key findings report: Executive summary.
- Wisse E., Burke-Shyne N., Chang J., Southwell M. Covid-19 and people who use drugs; seizing opportunity in times of chaos. International Journal of Drug Policy. 2021;90 doi: 10.1016/j.drugpo.2020.103097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . 2020. Mental health and psychosocial considerations during the COVID-19 outbreak 19MARCH2020_marissa.docx.https://www.who.int/docs/default-source/coronaviruse/mental-health-considerations.pdf Geneva Retrieved from. [Google Scholar]
- World Health Organization . 2021. WHO coronavirus disease (COVID-19) dashboard. Retrieved from https://covid19.who.int/ [PubMed] [Google Scholar]
- Zolopa C., Hoj S., Bruneau J., Meeson J.-.S., Minoyan N., Raynault M.-.F., et al. A rapid review of the impacts of “Big Events” on risks, harms, and service delivery among people who use drugs: Implications for responding to COVID-19. International Journal of Drug Policy. 2021;92 doi: 10.1016/j.drugpo.2021.103127. [DOI] [PMC free article] [PubMed] [Google Scholar]