Abstract
BACKGROUND
Aging is accompanied by an overall dysregulation of many dynamic physiologic processes including those related to blood pressure (BP). While year-to-year BP variability is associated with cardiovascular events and mortality, no studies have examined this trend with more frequent BP assessments. Our study objective is to take the next step to examine week-to-week BP dynamics—pattern, variability, and complexity—before death.
METHODS
Using a retrospective study design, we assessed BP dynamics in the 6 months before death in long-term nursing home residents between 1 October 2006 and 30 September 2017. Variability was characterized using SD and mean squared error after adjusting for diurnal variations. Complexity (i.e., amount of novel information in a trend) was examined using Shannon’s entropy (bits). Generalized linear models were used to examine factors associated with overall BP variability.
RESULTS
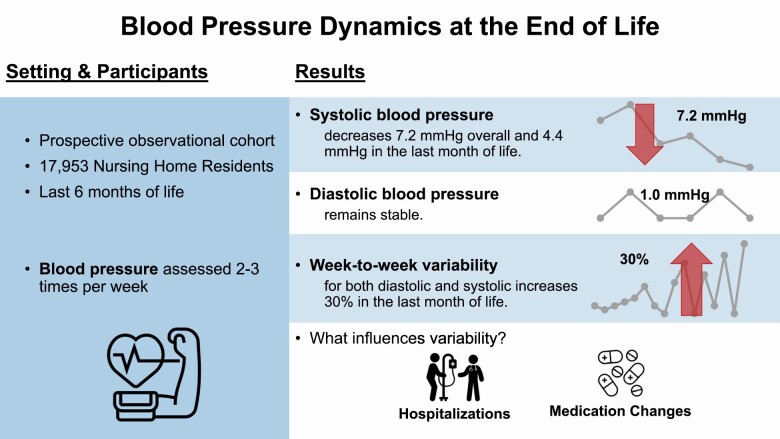
We identified 17,953 nursing home residents (98.0% male, 82.5% White, mean age 80.2 years, and mean BP 125.7/68.6 mm Hg). Despite a slight trend of decreasing systolic week-to-week BP over time (delta = 7.2 mm Hg), week-to-week complexity did not change in the 6 months before death (delta = 0.02 bits). Average weekly BP variability was stable until the last 3–4 weeks of life, at which point variability increased by 30% for both systolic and diastolic BP. Factors associated with BP variability include average weekly systolic/diastolic BP, days in the nursing home, days in the hospital, and changes to antihypertensive medications.
CONCLUSIONS
Week-to-week BP variability increases substantially in the last month of life, but complexity does not change. Changes in care patterns may drive the increase in BP variability as one approaches death.
Keywords: blood pressure, dynamics, hypertension, mortality, nursing home
Graphical Abstract
Graphical Abstract.
Blood pressure (BP) is a complex dynamic system in the human body that can be described not only by a trajectory but also by the variability and complexity its trajectory. Exploring this dynamic data system may provide complementary information to the static, one-time BP measurements that are more commonly used in research. Several studies have reported a decrease in year-to-year BP before death, with the steepest decline in the last 2 years of life, independent of age, hypertension, and medication use.1 Moreover, others have reported an association of greater year-to-year BP variability with cardiovascular events and/or death.2–7 Unfortunately, most studies to date only evaluate year-to-year or visit-to-visit variability and thus do not capture the granular week-to-week changes in BP before death. A better understanding of the dynamics of BP before death could shed light on the physiologic process of dying. Moreover, BP dynamics could serve as a prognostic marker to guide treatment-decision making among those with limited life expectancy.
The study of dynamic data systems is the study of changes in a system, or a group of interrelated and interacting data points, due to multilevel interactions.8 In contrast to static data elements, dynamic data systems are complex, nonlinear, time-varying, and require repeated measures data, so they are less often studied and described in medical research.9 Of the studies that have examined BP as a dynamic data system, some have found that BP dynamics may lose complexity with aging.10–12 Heart rate is another example of a dynamic data system that has been explored in this manner. In critical care research, heart rate variability has routinely been associated with impending cardiovascular events.13
To understand BP as a dynamic data system, we first need to describe the patterns of BP in terms of both variability and complexity.14,15 Variability, the more commonly examined dynamic data characteristic, is the range of values a data point may take on. It can be measured in terms of SD or coefficients of variation, but it is often best captured by mean squared error (MSE). The MSE measures variation around a fitted linear or nonlinear regression line, thus removing any variation due to the data’s trend alone.
The other measure used to describe a dynamic data system, complexity, is essentially a measure of information content or, conversely, the uncertainty or randomness in the data series.16 Complexity can be used to describe self-similarity, nonlinearity, temporal changes, and interdependency in a dynamic data system.17 Shannon’s entropy is 1 measure of complexity that attempts to capture complexity within a data series. Shannon’s entropy assumes that an event’s information content is a function of the probability of that event, –log2(P), where P is the probability of the event.18 The complexity of a data system can then be summarized as the average entropy contribution of each event in a data series. Understanding both variability and complexity is integral to fully describe the data as a dynamic system.14,15
In the present study, we describe the week-to-week trajectory, variability, and complexity of inpatient BP measurements among older nursing home residents 6 months before death. We use data from nearly 18,000 residents in an open cohort study of Veterans Health Administration (VHA) nursing homes in the United States. BP is assessed multiple times per week in this population and thus provides more granularity than the visit-to-visit and year-to-year BP assessments, which have historically been used. Our primary objective is to describe BP as a dynamic data system in older people nearing death. Our secondary objective is to examine patient characteristics associated with BP variability before death.
METHODS
Study design and study population
This study was reviewed and approved by the Stanford Institutional Review Board with a waiver of informed consent. Our study population includes patients receiving care at a VHA community living center between 1 October 2007 and 30 September 2017. Community living centers are VHA nursing homes that provide 24-hour skilled nursing care, access to VHA social services, and access to VHA geriatric evaluation and management. Patients were included if they died during or within 6 months of their nursing home stay. Patients were excluded from the study if they died within 90 days of their nursing home admission, had a short-term stay at the nursing home (<90 days), were less than 65 years old at the time of admission, used hospice care before their nursing home stay, or had fewer than 5 BP assessments during their stay.
Data sources and variables
All data were obtained from the VHA Corporate Data Warehouse (CDW). The CDW is the national repository for VHA electronic healthcare records and includes all aspects of care recorded during a patient’s nursing home stay. The CDW Inpatient domain was used to identify nursing home admissions. The CDW Patient domain was used to determine patient age, gender, race, and ethnicity at the time of admission. Patient comorbidities were assessed by querying the CDW Inpatient and Outpatient domain for relevant diagnoses 1 year before the nursing home admission date. Evidence of palliative care consults, hospice care, or acute care stays at a VA hospital during the nursing home stay were also obtained from the CDW Inpatient and Outpatient domains. Hypertensive medication usage during the nursing home stay was obtained from the CDW Bar-Coded Medication Administration domain, which captures all medication administered during the nursing home stay or any acute care stay at a VA hospital. Hypertensive medications were categorized by type the dose was standardized to examine BP variability by medication type, number of administrations per day, and standardized dose.
Systolic and diastolic BP assessments during the nursing home stay or acute VHA hospital stays were obtained from the CDW Vital Signs domain. All BP data were obtained from administrative data sources and thus we are unable to ensure systematic collection of BPs both across time and across nursing homes. Descriptive statistics about the frequency and timing of BP assessment are included in the Supplementary Materials online.
Measures of variability and complexity were calculated both (i) overall, for the entire 6 months preceding death, and (ii) weekly, for each week in the 6 months preceding death. Variability and complexity were not calculated for patients with 2 or fewer BP assessments during a given week.
Variability.
BP variability before death was calculated using 2 methods: (i) SD and (ii) MSE. SD is most commonly used to describe BP variability in the literature. However, the SD may overestimate week-to-week BP variability leading up to death because of the known decreasing trend in BP in a person before death.
Because of this trend and potential confounding by daily and seasonal variation, we also calculated an adjusted MSE to assess variability independent of the known trend and BP level. The MSE was calculated using a generalized linear model with generalized estimating equations to account for the clustering of BP measurements within a patient. For the adjusted MSE, we also included the timing of day, day of week, and month of year that the BP measurement was taken as covariates in the generalized linear model. Time to death in weeks was included as a categorical term to allow for nonlinear trends in BP over time. Fixed effects for the hour of the day, day of the week, and month of the year were also included to account for variation due to environmental stimuli. The MSE for each patient was calculated by squaring the residuals from the model, averaging the squared residuals, and then taking the square root.
Complexity.
Shannon’s entropy [H(x)] was used to describe BP complexity before death. In information theory, entropy is a measure of the level of uncertainty for each event/outcome (i.e., BP) in a series of data, such as a series of BP measures. The level of uncertainty for each event is assumed to be a function of the probability of that event’s outcome, defined as –log2(P), where P is the probability of the event’s outcome over all possible outcomes. Shannon’s entropy combines the entropy measures of all measures in a data series to estimate the average level of uncertainly for all events in the data series, or the complexity of the data series. For example, a pattern of ABBBBBA has less uncertainty in the possible outcome (A or B) and thus a lower complexity than a pattern of ABCDEFG where possible outcomes include A, B, C, D, E, F, and G. Recent literature has noted that Shannon’s entropy can provide complementary value to the P value and confidence intervals, as it measures the extent to which the observed data are unexpected.18
The formula for determining Shannon’s entropy of a data series is as follows:
Shannon’s entropy is measured in bits and ranges from 0 to infinity, with 0 indicating an event that is fully known or perfectly predictable.16 The larger the value, the more complex the data series.
Statistical analyses
Missingness, distributions, and frequencies of all variables were examined before beginning bivariate analyses. The majority of variables were deemed to have a normal distribution, and, for consistency in reporting, we use means to describe all continuous variables. Week-to-week BP variability and complexity in the 6 months before death was plotted across time.19
Generalized linear models with generalized estimating equations to account for clustering within individual and nursing home facility were used to examine factors associated with week-to-week BP variability, as measured by MSE. The unit of analysis for these models was patient-week allowing us to adjust for changes in medication type and dosage over the study time period. Unadjusted and adjusted associations between covariates and BP variability were estimated and plotted as a forest plot. Adjusted estimates were determined from a fully adjusted generalized linear model with all covariates included. All analyses were conducted in SAS Enterprise Guide v7.1. The ggplot2 R package was used to plot BP complexity and variability over time.19
RESULTS
Population characteristics
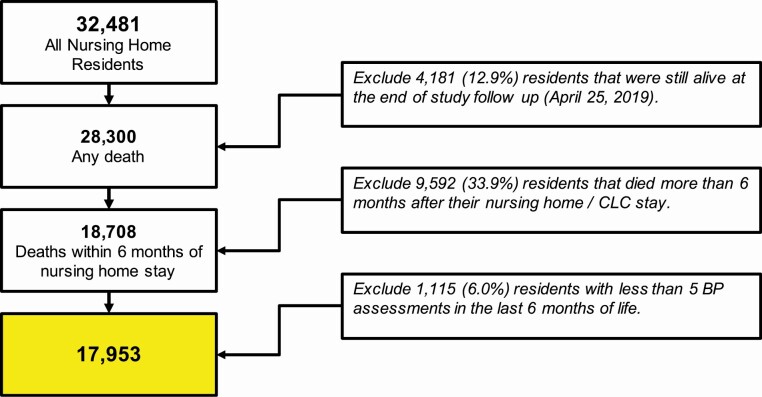
We identified 17,953 patients receiving care at a VHA nursing home during our 10-year study period (Figure 1). Most patients were male (98.0%), White (82.5%), an average of 80.2 years old when they were admitted, and stayed an average of 495.6 days (median = 275.0 days) in the nursing home. Hypertension was the most common comorbidity observed (77.4%), followed by dementia (48.4%), coronary heart disease (42.6%), and diabetes (40.2%). In the 6 months before death, 82.5% of patients had evidence of hypertensive medication use (Table 1).
Figure 1.
CONSORT flow diagram for study population.
Table 1.
Characteristics of long-term VA nursing home patients who died during a nursing home stay between 1 October 2006 and 30 September 2017 (n = 17,953)
| N | % | Mean | (SD) | Median | (Q1–Q3) | |
|---|---|---|---|---|---|---|
| Patient demographics | ||||||
| Age at admission, years | 17,953 | 80.2 | (8.2) | 81 | (74–87) | |
| Gender, n (%) | ||||||
| Male | 17,589 | 98.0% | ||||
| Female | 364 | 2.0% | ||||
| Race, n (%) | ||||||
| White | 13,566 | 82.5% | ||||
| Black | 2,429 | 14.8% | ||||
| Asian | 237 | 1.4% | ||||
| American Indian | 75 | 0.5% | ||||
| Multiple races | 147 | 0.9% | ||||
| Hispanic ethnicity, n (%) | ||||||
| No | 17,284 | 96.3% | ||||
| Yes | 669 | 3.7% | ||||
| Healthcare utilization | ||||||
| Length of nursing home stay, days | 17,953 | 476.8 | (534.2) | 275 | (157–619) | |
| End-of-life hospitalizations, n (%) | ||||||
| None | 14,204 | 79.1% | ||||
| 1 | 3,193 | 17.8% | ||||
| More than 1 | 556 | 3.1% | ||||
| Days in acute care, days | 17,953 | 8.4 | (15.7) | 0 | (0–11) | |
| Any hospice care, n (%) | 220 | 1.2% | ||||
| Palliative care consultations, n (%) | 5,987 | 33.4% | ||||
| Comorbidities at admission | ||||||
| Charlson Comorbidity Index | 17,953 | 4.9 | (3.3) | 4 | (2–7) | |
| Hypertension, n (%) | 13,890 | 77.4% | ||||
| Dementia, n (%) | 8,693 | 48.4% | ||||
| Coronary heart disease, n (%) | 7,641 | 42.6% | ||||
| Diabetes, n (%) | 7,215 | 40.2% | ||||
| Depression, n (%) | 6,761 | 37.7% | ||||
| Any malignancy, n (%) | 6,369 | 35.5% | ||||
| Heart failure, n (%) | 6,115 | 34.1% | ||||
| Cerebrovascular disease, n (%) | 5,772 | 32.2% | ||||
| Renal failure, n (%) | 5,257 | 29.3% | ||||
| Osteoarthritis, n (%) | 5,047 | 28.1% | ||||
| Atrial fibrillation, n (%) | 4,824 | 26.9% | ||||
| Peripheral vascular disease, n (%) | 4,597 | 25.6% | ||||
| Acute kidney injury, n (%) | 3,754 | 20.9% | ||||
| Metastatic cancer, n (%) | 2,409 | 13.4% | ||||
| Chronic obstructive pulmonary disease, n (%) | 1,726 | 9.6% | ||||
| Medication use before death | ||||||
| Hypertensive medications, n (%) | 14,806 | 82.5% | ||||
| Percentage (%) of days covered* | 77.2 | (30.8) | 93.5 | (66.6–98.4) | ||
| No. of hypertensive medications | 3.1 | (1.9) | 3 | (2–4) |
Abbreviation: Q1–Q3, interquartile range.
aPercentage (%) of days covered is defined as the proportion of days in the 6 months prior to death that the patient received at least 1 hypertension medication.
Patients had an average of 132.3 BP assessments (median = 96 assessments; interquartile range = 38–192) in the 6 months before death with an average of 1 assessment every 70.3 hours (SD: 107.2 hours). Twenty-five percent (25%) of patients had at least 1 assessment every 16.6 hours (Supplementary Figure S1 online).
BP dynamics before death
The average systolic BP was 125.7 mm Hg in the 6 months before death, and the average diastolic BP was 68.6 mm Hg (Table 2). Variability across the 6 months was similar when measured by either SD or MSE. Over the entire 6 months before death, a patient’s systolic BP varied by roughly 16 mm Hg, or 13% of the mean (SD: 16.2 mm Hg, MSE: 16.0 mm Hg). Similarly, a patient’s diastolic BP varied by roughly 9 mm Hg, also 13% of the mean (SD: 9.5 mm Hg, MSE: 9.4 mm Hg, Table 2). Week-to-week BP complexity averaged 5.0 bits (SD: 0.9 bits, 18% of the mean) for systolic BP and 4.6 bits (SD: 0.7 bits, 15% of the mean) for diastolic BP.
Table 2.
Overall summary of systolic and diastolic blood pressure in the 6 months before death among patients residing in a VA nursing home between 1 October 2006 and 30 September 2017 (n = 17,953)
| Mean | (SD) | Median | (Q1–Q3) | Range | |
|---|---|---|---|---|---|
| Systolic blood pressure (n = 2,458,841) | |||||
| Per individuala, mm Hg | 125.7 | (13.3) | 125.1 | (116.3–134.4) | (80.7–191.7) |
| Shannon entropy (bits) | 5.0 | (0.9) | 5.3 | (4.7–5.6) | (0.9–6.9) |
| Variation | |||||
| SD | 16.2 | (4.3) | 15.8 | (13.2–18.8) | (2.0–44.1) |
| Adjusted MSEb | 16.0 | (4.2) | 15.5 | (13.1–18.4) | (2.4–41.8) |
| Diastolic blood pressure (n = 2,456,225) | |||||
| Per individuala, mm Hg | 68.6 | (6.8) | 68.4 | (64.0–72.9) | (37.4–99.6) |
| Shannon entropy (bits) | 4.6 | (0.7) | 4.7 | (4.3–5.0) | (1.4–6.3) |
| Variation | |||||
| SD | 9.5 | (2.3) | 9.3 | (8.0–10.8) | (1.5–30.1) |
| Adjusted MSEb | 9.4 | (2.2) | 9.2 | (7.9–10.7) | (1.8–28.4) |
Abbreviations: MSE = mean squared error; Q1–Q3 = interquartile range.
aOverall average for a patient.
bAdjusted for time of day, day of week, and month of year with a random effect for person.
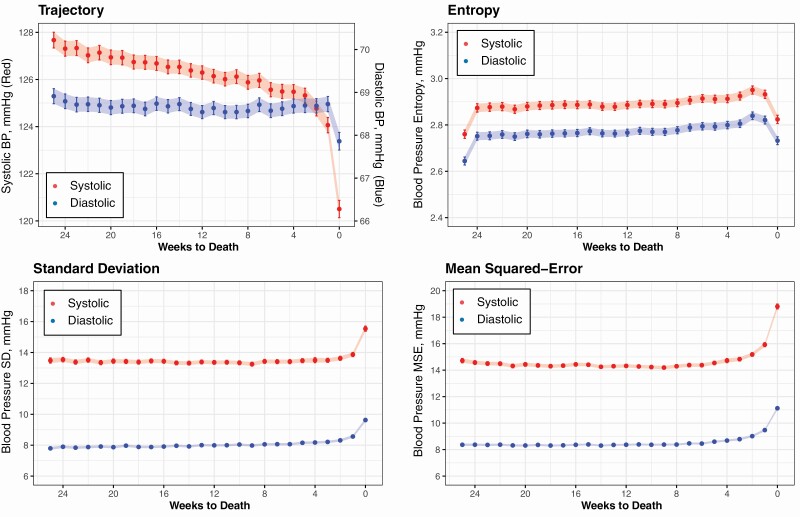
Systolic BP decreased in the 6 months before death from an average of 127.7 mm Hg at baseline to 120.5 mm Hg at death (6.2 mm Hg, P < 0.001, Figure 2). The most remarkable change occurred in the last week of life when the average systolic BP decreased from 125.1 mm Hg the week before to 120.5 mm Hg (4.4 mm Hg, P < 0.001). In contrast, diastolic remained relatively stable in the last 6 months of life (68.9 mm Hg at baseline vs. 67.9 mm Hg in the last week of life). Despite this trend of decreasing systolic BP, both systolic and diastolic BP complexity changed very little in the 6 months before death, with an average increase in Shannon’s entropy of only 0.02 bits (0.4%) each week for both systolic and diastolic BP (P < 0.001, Figure 2).
Figure 2.
Week-to-week blood pressure complexity and variability in the 6 months before death. Each point represents the mean value across all patients for that time interval. Error bars and ribbon widths represent the 95% confidence interval around the mean value.
As measured by weekly MSE and SD, BP variability was also relatively stable until the last 3–4 weeks of life, at which point variability increases, with the largest change occurring in the last week of life (Figure 2). The average weekly systolic MSE was 14.4 mm Hg and remained stable until the last 3 weeks of life. In the last week of life, average systolic MSE increases to 18.8 mm Hg, a 30.3% increase over baseline (4.4 mm Hg, P < 0.001). Findings were similar for diastolic MSE, which increased from 8.3 mm Hg at baseline to 11.1 mm Hg in the last week before death (2.8 mm Hg, 33.7%, P < 0.001). A similar trend was seen when variability was measured by weekly SD (Figure 2).
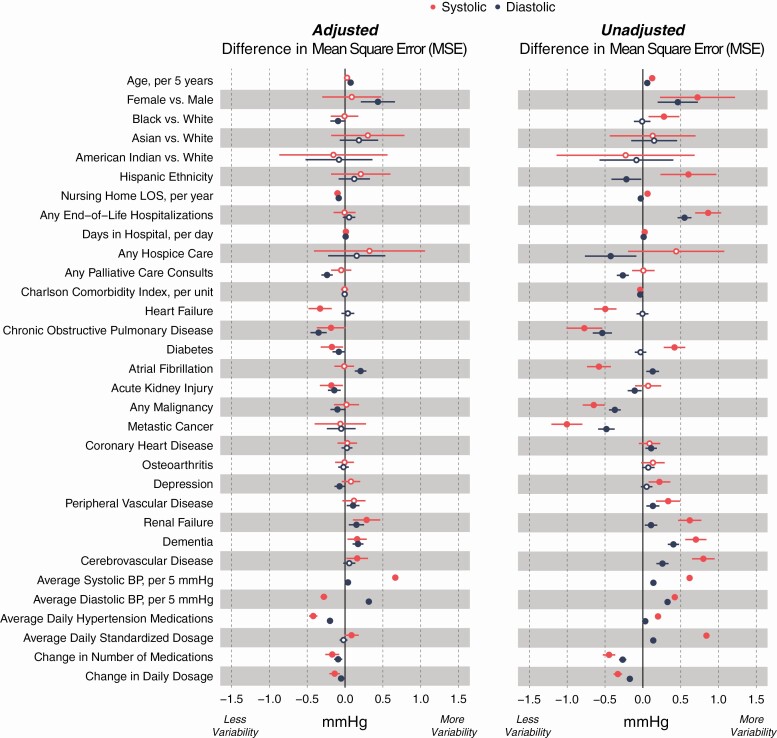
Outside of average weekly systolic BP, no factor we included explained more than a 0.5 mm Hg change in BP, or a change of more than 3% of the overall MSE (Figure 3). In our final model, systolic BP variability was positively associated with average weekly systolic BP but negatively correlated with average weekly diastolic BP. In contrast, diastolic BP variability is positively correlated with both systolic and diastolic BP. Factors most strongly associated with increased variability included days in acute care, dementia, renal failure, and increased average systolic BP. In contrast, longer time in the nursing home, palliative care consults, chronic obstructive pulmonary disease, diabetes, acute kidney injury, more daily antihypertensive drugs, and changes in antihypertensive drugs and doses were associated with decreased BP variability, both systolic and diastolic, in the 6 months before death. Heart failure was only associated with reduced systolic BP variability, and atrial fibrillation was associated with increased diastolic BP variability. Average diastolic BP was positively associated with diastolic BP variability but negatively associated with systolic BP variability (Figure 3). Variability in BP by antihypertensive drug type is presented in Supplementary Materials online.
Figure 3.
Factors associated with week-to-week blood pressure (BP) variability in the 6 months before death. Week-to-week variability is defined as root mean squared error (MSE). Estimates of change are adjusted using a fully adjusted model and generalized estimating equations to account for clustering of weekly estimates within patients and clustering of patients within nursing home. Hypertensive medication type was also included in the model and is presented in Supplementary Figure S2 online. Bars represent 95% confidence intervals. Solid circles represent P < 0.05.
DISCUSSION
Our goal was to describe both the variability and complexity of BP in older adults near the end of life. We found that despite a steady and gradual decrease in BP before death, BP complexity in the last 6 months of life is relatively stable. In addition, variability remains stable until the last few weeks of life, during which both systolic and diastolic BP variability increase by as much as 30%. These findings further describe the complex association between BP and mortality in older populations.
Our findings extend upon the current peer-reviewed literature examining the dynamics of BP in older adults. To date, our understanding of BP complexity is limited. Lipsitz and colleagues have performed the majority of research on BP complexity.10–12 They have repeatedly found that older patients tend to have less complex BP patterns over short time intervals (i.e., 6–60 minutes). Their research concludes that “normal aging is associated with a generalized loss of complexity in the dynamics of the cardiovascular control system.” 10 In contrast, our study examined changes in complexity over a much longer time (6 months), with less frequent BP assessments (1 every 3 days), and was limited to an end-of-life population. We found no noticeable change in complexity in the last 6 months of life (0.4%). Our findings suggest that the loss of complexity identified by Lipsitz may either be a gradual decrease over years or only identified at a granular level when BP is measured on a short-term, minute-by-minute basis. Moreover, these findings also support the hypothesis that aging and dying processes represent different phenomena as Lipsitz’s research examines the process of aging, whereas our research is more representative of the dying process. Others have demonstrated that there are unique physiologic signatures to these 2 processes.20 This can be difficult to untangle since frequent BP monitoring is invasive and/or bothersome and rarely implemented for long periods; thus, the feasibility of capturing large-scale data on BP complexity at the end of life is limited.
We also found that BP variability changes drastically in the last 3 weeks of life. This finding extends upon prior research in the general population suggesting an association between greater BP variability and death, adverse cardiovascular events, or other critical events that may precede death.2,5,6,21–23 We found that BP variability increases by 30% in the last 3 weeks of life. While we were able to identify some factors associated with this variability in the 6 months before death, most of the factors we examined only explained a small proportion of variability (3% or less). Of those, greater variability was associated with end-of-life hospitalizations, hospice care, and medication changes suggesting that the complexity of care patterns associated with the process of dying may be driving variability rather than intrinsic factors.
To date, most studies of BP variability examine only 1 measure of variability. SD is the most common measure used, but other BP variability estimates include the standardized residuals, coefficient of variation, and variation independent of the mean.24 One important strength of our study is the ability to compare BP variability as measured by SD, which includes variability due to a trend, to BP variability as measured by the MSE, which adjusts for variability due to an overall trend or secular changes. While the MSE weights outliers more heavily, we ultimately found very little difference between BP variability when measured by SD or MSE.
Taken as a whole, our findings of the week-to-week dynamics of BP before death can provide important insights into the biology of aging and dying processes.2,3,7,24 Over time, there are many age-related structural changes to the vasculature of a human body. These structural changes lead to increased arterial stiffness, resulting in increased systolic BP and decreasing diastolic BP as individuals age.25,26 In contrast, the dying process is often accompanied by, and perhaps a result of, a terminal decline in organ function or other critical events preceding death, which may also drive the steep drop in BP and increase in variability that we observed near death. Further exploration of BP dynamics at the end of life could provide insight into treatment-decision making among those with limited life expectancy.
As with all studies, our study is not void of limitations. While interpreting our findings, it is important to keep in mind that this is an observational study of the Veteran population. Our results are heavily weighted toward males (98.0%) who are White (82.5%) with multiple comorbidities. Also, while the observational study design allows us to examine a large study sample in a nationwide population, we could not intervene with a standardized BP measurement protocol. Not only does this likely lead to more variation, but it also impedes our ability to distinguish routine BP measurements from those taken for other purposes. While we do not think this affected our estimates of mean BP and patterns over time, it does mean that our estimates of variability are likely inflated. Finally, studies of death may only be conducted retrospectively. Thus, although our findings are hypothesis-generating regarding the biology of aging and dying, they cannot be used to inform clinical care of nursing home residents. In addition, there is also the possibility that the observed increase in BP variability in the last week may be due to an acute decline in secondary to a critical event leading to death.
To conclude, this is the most extensive analysis to examine intraindividual week-to-week BP dynamics leading up to death. We found a decline in systolic BP in the last week of life that was not accompanied by an increase in complexity. Further, the apparent increase in both systolic and diastolic BP variability at the end of life may be driven by increasingly complex care patterns, such as hospitalizations and medication changes, as one approaches death. Future research on the dynamics of BP at the end of life may lend insight into the complex biology of the aging and dying processes.
Supplementary Material
FUNDING
This research was funded by the National Institute on Aging (R56AG055576, RF1AG062568, K24AG049057, K24AG066998). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
DISCLOSURE
Dr Peralta serves as the Chief Medical Officer for Cricket Health, Inc. Dr Odden serves as a consultant for Cricket Health, Inc.
REFERENCES
- 1. Delgado J, Bowman K, Ble A, Masoli J, Han Y, Henley W, Welsh S, Kuchel GA, Ferrucci L, Melzer D. Blood pressure trajectories in the 20 years before death. JAMA Intern Med 2018; 178:93–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wu C, Shlipak MG, Stawski RS, Peralta CA, Psaty BM, Harris TB, Satterfield S, Shiroma EJ, Newman AB, Odden MC; Health ABC Study . Visit-to-visit blood pressure variability and mortality and cardiovascular outcomes among older adults: the health, aging, and body composition study. Am J Hypertens 2017; 30:151–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Diaz KM, Tanner RM, Falzon L, Levitan EB, Reynolds K, Shimbo D, Muntner P. Visit-to-visit variability of blood pressure and cardiovascular disease and all-cause mortality: a systematic review and meta-analysis. Hypertension 2014; 64:965–982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Suchy-Dicey AM, Wallace ER, Mitchell SV, Aguilar M, Gottesman RF, Rice K, Kronmal R, Psaty BM, Longstreth WT Jr. Blood pressure variability and the risk of all-cause mortality, incident myocardial infarction, and incident stroke in the cardiovascular health study. Am J Hypertens 2013; 26:1210–1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hossain M, Ooi WL, Lipsitz LA. Intra-individual postural blood pressure variability and stroke in elderly nursing home residents. J Clin Epidemiol 2001; 54:488–494. [DOI] [PubMed] [Google Scholar]
- 6. Mehlum MH, Liestøl K, Kjeldsen SE, Julius S, Hua TA, Rothwell PM, Mancia G, Parati G, Weber MA, Berge E. Blood pressure variability and risk of cardiovascular events and death in patients with hypertension and different baseline risks. Eur Heart J 2018; 39:2243–2251. [DOI] [PubMed] [Google Scholar]
- 7. Wang J, Shi X, Ma C, Zheng H, Xiao J, Bian H, Ma Z, Gong L. Visit-to-visit blood pressure variability is a risk factor for all-cause mortality and cardiovascular disease: a systematic review and meta-analysis. J Hypertens 2017; 35:10–17. [DOI] [PubMed] [Google Scholar]
- 8. Connell JP, DiMercurio A, Corbetta D. Dynamic systems theory. In: Vonk J, Shackelford T (eds), Encyclopedia of Animal Cognition and Behavior. Springer International Publishing: Cham, 2017, pp. 1–8. [Google Scholar]
- 9. Boker SM, Wenger MJ.. Data Analytic Techniques for Dynamical Systems. Routledge Taylor & Francis Group: London; 2012. [Google Scholar]
- 10. Lipsitz LA. Age-related changes in the “complexity” of cardiovascular dynamics: a potential marker of vulnerability to disease. Chaos 1995; 5:102–109. [DOI] [PubMed] [Google Scholar]
- 11. Lipsitz LA. Dynamics of stability: the physiologic basis of functional health and frailty. J Gerontol A Biol Sci Med Sci 2002; 57:B115–B125. [DOI] [PubMed] [Google Scholar]
- 12. Lipsitz LA. Physiological complexity, aging, and the path to frailty. Sci Aging Knowledge Environ 2004; 2004:pe16. [DOI] [PubMed] [Google Scholar]
- 13. Rajendra Acharya U, Paul Joseph K, Kannathal N, Lim CM, Suri JS. Heart rate variability: a review. Med Biol Eng Comput 2006; 44:1031–1051. [DOI] [PubMed] [Google Scholar]
- 14. Goldberger AL, Peng CK, Lipsitz LA. What is physiologic complexity and how does it change with aging and disease? Neurobiol Aging 2002; 23:23–26. [DOI] [PubMed] [Google Scholar]
- 15. Valenza G, Citi L, Garcia RG, Taylor JN, Toschi N, Barbieri R. Complexity variability assessment of nonlinear time-varying cardiovascular control. Sci Rep 2017; 7:42779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Shannon CE. A mathematical theory of communication. Bell Syst Tech J 1948; 27:379–423. [Google Scholar]
- 17. Seely AJ, Macklem PT. Complex systems and the technology of variability analysis. Crit Care 2004; 8:R367–R384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Cole SR, Edwards JK, Greenland S. Surprise! Am J Epidemiol 2021; 190:191–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wickham H. Ggplot2: Elegant Graphics for Data Analysis. 2nd ed. 2016 edition. Springer: New York, NY, 2016. [Google Scholar]
- 20. Diehr P, Williamson J, Burke GL, Psaty BM. The aging and dying processes and the health of older adults. J Clin Epidemiol 2002; 55:269–278. [DOI] [PubMed] [Google Scholar]
- 21. Parati G, Ochoa JE, Lombardi C, Bilo G. Assessment and management of blood-pressure variability. Nat Rev Cardiol 2013; 10:143–155. [DOI] [PubMed] [Google Scholar]
- 22. Mancia G. Short- and long-term blood pressure variability: present and future. Hypertension 2012; 60:512–517. [DOI] [PubMed] [Google Scholar]
- 23. Parati G, Ochoa JE, Lombardi C, Bilo G. Blood pressure variability: assessment, predictive value, and potential as a therapeutic target. Curr Hypertens Rep 2015; 17:537. [DOI] [PubMed] [Google Scholar]
- 24. Stevens SL, Wood S, Koshiaris C, Law K, Glasziou P, Stevens RJ, McManus RJ. Blood pressure variability and cardiovascular disease: systematic review and meta-analysis. BMJ 2016; 354:i4098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Harvey A, Montezano AC, Touyz RM. Vascular biology of ageing-Implications in hypertension. J Mol Cell Cardiol 2015; 83:112–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Cheng S, Xanthakis V, Sullivan LM, Vasan RS. Blood pressure tracking over the adult life course: patterns and correlates in the Framingham heart study. Hypertension 2012; 60:1393–1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.