Abstract
Background
Unintended pregnancy among adolescents represents an important public health challenge in high‐income countries, as well as middle‐ and low‐income countries. Numerous prevention strategies such as health education, skills‐building and improving accessibility to contraceptives have been employed by countries across the world, in an effort to address this problem. However, there is uncertainty regarding the effects of these interventions, hence the need to review the evidence‐base.
Objectives
To assess the effects of primary prevention interventions (school‐based, community/home‐based, clinic‐based, and faith‐based) on unintended pregnancies among adolescents.
Search methods
We searched all relevant studies regardless of language or publication status up to November 2015. We searched the Cochrane Fertility Regulation Group Specialised trial register, The Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2015 Issue 11), MEDLINE, EMBASE, LILACS, Social Science Citation Index and Science Citation Index, Dissertations Abstracts Online, The Gray Literature Network, HealthStar, PsycINFO, CINAHL and POPLINE and the reference lists of articles.
Selection criteria
We included both individual and cluster randomised controlled trials (RCTs) evaluating any interventions that aimed to increase knowledge and attitudes relating to risk of unintended pregnancies, promote delay in the initiation of sexual intercourse and encourage consistent use of birth control methods to reduce unintended pregnancies in adolescents aged 10 years to 19 years.
Data collection and analysis
Two authors independently assessed trial eligibility and risk of bias, and extracted data. Where appropriate, binary outcomes were pooled using a random‐effects model with a 95% confidence interval (Cl). Where appropriate, we combined data in meta‐analyses and assessed the quality of the evidence using the GRADE approach.
Main results
We included 53 RCTs that enrolled 105,368 adolescents. Participants were ethnically diverse. Eighteen studies randomised individuals, 32 randomised clusters (schools (20), classrooms (6), and communities/neighbourhoods (6). Three studies were mixed (individually and cluster randomised). The length of follow up varied from three months to seven years with more than 12 months being the most common duration. Four trials were conducted in low‐ and middle‐ income countries, and all others were conducted in high‐income countries.
Multiple interventions
Results showed that multiple interventions (combination of educational and contraceptive‐promoting interventions) lowered the risk of unintended pregnancy among adolescents significantly (RR 0.66, 95% CI 0.50 to 0.87; 4 individual RCTs, 1905 participants, moderate quality evidence. However, this reduction was not statistically significant from cluster RCTs. Evidence on the possible effects of interventions on secondary outcomes (initiation of sexual intercourse, use of birth control methods, abortion, childbirth, sexually transmitted diseases) was not conclusive.
Methodological strengths included a relatively large sample size and statistical control for baseline differences, while limitations included lack of biological outcomes, possible self‐report bias, analysis neglecting clustered randomisation and the use of different statistical tests in reporting outcomes.
Educational interventions
Educational interventions were unlikely to significantly delay the initiation of sexual intercourse among adolescents compared to controls (RR 0.95, 95% CI 0.71 to 1.27; 2 studies, 672 participants, low quality evidence).
Educational interventions significantly increased reported condom use at last sex in adolescents compared to controls who did not receive the intervention (RR 1.18, 95% CI 1.06 to 1.32; 2 studies, 1431 participants, moderate quality evidence).
However, it is not clear if the educational interventions had any effect on unintended pregnancy as this was not reported by any of the included studies.
Contraceptive‐promoting interventions
For adolescents who received contraceptive‐promoting interventions, there was little or no difference in the risk of unintended first pregnancy compared to controls (RR 1.01, 95% CI 0.81 to 1.26; 2 studies, 3,440 participants, moderate quality evidence).
The use of hormonal contraceptives was significantly higher in adolescents in the intervention group compared to those in the control group (RR 2.22, 95% CI 1.07 to 4.62; 2 studies, 3,091 participants, high quality evidence)
Authors' conclusions
A combination of educational and contraceptive‐promoting interventions appears to reduce unintended pregnancy among adolescents. Evidence for programme effects on biological measures is limited. The variability in study populations, interventions and outcomes of included trials, and the paucity of studies directly comparing different interventions preclude a definitive conclusion regarding which type of intervention is most effective
Plain language summary
Interventions for preventing unintended pregnancy among adolescents
Interventions for preventing unintended pregnancy include any activity (health education or counselling only, health education plus skills‐building, health education plus contraception education, contraception education and distribution, faith‐based group or individual counselling) designed to increase adolescents' knowledge and attitudes relating to risk of unintended pregnancies; promote delay in initiation of sexual intercourse; encourage consistent use of birth control methods and reduce unintended pregnancies.
This review included 53 randomised controlled trials comparing these interventions to various control groups (mostly usual standard sex education offered by schools). The search for trials was not limited by country, though most of the included trials were conducted in high‐income countries, with just four trials in middle‐ and low‐income countries, mainly representing the lower socio‐economic groups. Interventions were administered in schools, community centres, healthcare facilities and homes. Meta‐analysis was performed for studies where it was possible to extract data.
Only interventions involving a combination of education and contraception promotion (multiple interventions) was seen to significantly reduce unintended pregnancy over the medium‐term and long‐term follow‐up period. Results for behavioural (secondary) outcomes were inconsistent across trials.
Limitations of this review include reliance on programme participants to report their behaviours accurately and methodological weaknesses in the trials.
Summary of findings
Background
The World Health Organization defines adolescents as individuals between 10 years and 19 years of age (WHO 1980). Adolescence is a period of transition, growth, exploration and opportunities. During this phase of life, adolescents experience physical and sexual maturation and tend to develop an increased interest in sex, with attendant risks of unintended pregnancies, health risks associated with early childbearing, abortion outcomes, and sexually transmitted infections, including HIV/AIDS.
Adolescents who have an unintended pregnancy face a number of challenges, including abandonment by their partners, inability to complete school education (which ultimately limits their future social and economic opportunities), and increased adverse pregnancy outcomes (Henshaw 2000; Koniak‐Griffin 2001; Kosunen 2002; Moore 1993; Phipps 2002;, Upchurch 1990).
Description of the condition
Unintended pregnancy among adolescents is a common public health problem in industrialised, middle‐ or low‐income countries (WHO 1995). The number of unintended pregnancies is reported to be on the decline in the US, with the Office of Adolescent Health reporting a 10% drop from 2012 to 2013, and more than a 50% drop between 1991 and 2013 (Hamilton 2014). The same decline was seen across all racial groups but some disparities remain: Black and Hispanic teens make up a large proportion of teen births in the US (Hamilton 2014). The same trend is reported in most countries (World Bank 2014): in sub‐Saharan Africa, there was a decline in the fertility rate among adolescents from 134 live births per 1000 in 2000 to 115 live births per 1000 in 2010, although these rates are still high when compared to the world standard; in India, adolescent pregnancies constitute 19% of total fertility (Mehra 2004) but this rate has been declining with 77 live births per 1000 in 2010 as compared to 109 live births per 1000 in 2000; and an Israeli study estimated the incidence of teenage pregnancy in Israel to be 32 live births per 1000 adolescent girls (Sikron 2003).
Repeat pregnancies among adolescents are also common and are associated with increased risks of adverse maternal and child health outcomes (Nelson 1990). Unintended pregnancy is not only costly to the teenagers and their families, it is also a huge financial burden to the state, borne by taxpayers in high‐income nations. It was estimated that spending on medicaid‐subsidised medical care related to unintended pregnancy totals more than USD 12 billion annually (Thomas 2009). These costs include welfare support for mothers experiencing financial difficulties, implementation of programmes (educational and skills training) to empower mothers to gain financial independence, and lost tax revenues arising from reduced employability and earnings (Burt 1986; Haveman 1997; Maynard 1996; Rich‐Edwards 2002 ).
Adolescent mothers are more likely to perform poorly in school, come from low socio‐economic homes and a less advantageous environment; and be themselves children of mothers with limited school education and a history of unintended teenage pregnancies (Elfebein 2003). Children born to adolescent mothers are more likely to have low birth weight, and become victims of physical neglect and abuse (Elfebein 2003), more likely to end up as school‐dropouts like their mothers, or engage in delinquent behaviours (Monea 2011).
Description of the intervention
On account of the short‐ and long‐term consequences of unintended pregnancies for the adolescent, their families and society at large (Burt 1990; Trussell 1997), government public health programmes, bilateral agencies and non‐governmental organisations (NGOs) have implemented (and continue to implement) various interventions to address the problem, using a variety of approaches.
Such interventions include:
curriculum‐based sex and STD/HIV education programmes (Safer Choices (Coyle 2001), Becoming a Responsible Teen (St. Lawrence 2005), All for You (Coyle 2006));
abstinence‐alone programmes (Postponing Sexual Involvement (Kirby 1997b), Sex can Wait (Denny 2006));
comprehensive programmes ‐ a combination of multiple components (Sexual Health and Relationships (SHARE) (Henderson 2007), RIPPLE (Stephenson 2004), Children's Aid Society‐Carrera program (Philliber 2002));
sex and STD/HIV education programmes for parents and teens (Keepin' it R.E.A.L (Dilorio 2006), REAL Men (Dilorio 2007));
interactive video‐based and computer‐based interventions (DeLamater 2000, Downs 2004);
clinical protocol and one‐on‐one programmes, which include advance promotion and provision of emergency contraceptives (Raine 2000; Raymond 2006);
clinic‐based programmes (Lindberg 2006), promotion of clinic appointments and supportive activities (Danielson 1990, Orr 1996);
youth development programmes (service learning such as the Reach for health service learning program (O'Donnell 2003), Teen Outreach Program (TOP) (Philliber 1992); and
vocational education (Summer Training and Education Program (STEP) (Grossman 1992).
How the intervention might work
Interventions that are designed to reduce teen pregnancy appear to be most effective when a multifaceted approach is used, as the problem is multiple determined and multidimensional. The interventions should not only focus on sexual factors and related consequences, they should also include non‐sexual factors such as skills training, and personal development. Further, stakeholders including pregnant teens, parents, the health sector, schools and churches should work together to devise programmes that are practical, evidence based, culturally appropriate and acceptable to the target population.
Some interventions focus primarily on changing the psychosocial risk and protective factors that involve sexuality. One such is Safer Choices (Coyle 2001) which improves teens’ knowledge about the risks and consequences of pregnancy and STDs, values and attitudes regarding sex, perceptions of peer norms about sex and contraception, self‐efficacy (ability to say ‘no’ to unwanted sex), consistent use of contraception including condoms, and their intentions regarding sexual behaviours. Some interventions promote abstinence only (Denny 2006), and others add a comprehensive, health‐education approach wherein safer sexual practices are also included (Jemmott 1998). Sex and STD/HIV education programmes for parents and teens seek to improve parent/child communication regarding sexual health and sexuality, and promote connectedness (Dilorio 2006). Clinic protocols and one‐on‐one programmes promote practices that provide advance supplies of emergency contraceptives to high risk adolescents (Lindberg 2006; Orr 1996), as well as providing health counselling for young men (Danielson 1990).
Other interventions, such as youth development endeavours, focus on non‐sexual factors, which aim to engender positive values in adolescents, inspire hope for the future, improve performance in school and bolster family relationships. They also aim to reduce risky behaviours such substance abuse and violence; promote service‐learning programmes which provide supervised voluntary community‐service opportunities, as well as mentoring opportunities on skills‐building (O'Donnell 2003, Philliber 1992). Some make use of trained peer educators to conduct the health‐education sessions serving as mentors or role models in achieving sustained behavioural changes (Borgia 2005).
Experts suggest that in order to reduce teenage pregnancies, interventions should be designed to address multiple sexual and non‐sexual antecedents that correlate with adolescent sexuality, and which may be related to the adolescents, their families, schools, communities and cultural factors ‐ notably religion (Kirby 2002a). Interventions should also include publicly‐financed mass media campaigns and expanding government‐subsidised family‐planning services (Thomas 2012).
With regard to cultural factors, while one Israeli study showed that the incidence of pregnancy was three times higher among Muslims than among Jews (Sikron 2003), another showed that women with no religious affiliation had the highest unintended pregnancy rate compared to women with religious affiliation, and that these women were also most likely to end the pregnancy by abortion (Finer 2006). This raises questions about the possible impact of faith‐based interventions, which tend to start early and are often sustained for long periods at the home and community levels. In some communities, premarital or extra‐marital sex, whether in young or older people, is seen by the larger society as a violation of morality. Most moral codes and laws that prescribe acceptable conducts of sexual relationships have their origin in major religions.
Why it is important to do this review
Evaluation studies of specific interventions as well as reviews and meta‐analyses of the effects of current strategies show discrepant evidence of effectiveness (DiCenso 2002, Fullerton 1997, Maness 2013). For example, a review of 73 studies reported that four intervention programmes resulted in delay in initiation of sexual intercourse, increased condom and contraceptive use, and reduced unintended teenage pregnancy (Kirby 2002b). The interventions identified as being effective in that review were sex and HIV education curricula; one‐on‐one clinician‐patient protocols in healthcare settings; service learning programmes; and intensive youth development programmes (Kirby 2002b).
Another systematic review of randomised controlled trials showed that several primary prevention measures did not delay the initiation of sexual intercourse nor reduce the number of pregnancies among adolescents (DiCenso 2002, Maness 2013). As this review demonstrated, a small number of programmes actually led to an increase in the number of pregnancies among partners of male participants of abstinence programmes (DiCenso 2002). One author had attributed the small decline in the level of adolescent pregnancy in the US to a decrease in sexual activity and an increase in contraceptive use, especially long‐term contraceptive injectables and implants (Pettinato 2003), fear of contracting HIV/AIDS, health education programmes, a changing moral climate, new contraceptives, and improved economic climate (Klerman 2002).
It is possible that discrepancies in results of existing reviews and meta‐analyses may partly be explained by design flaws in the evaluation of studies and reviews. For example, most reviews included non‐randomised and observational studies; most were limited in scope through their exclusion of unpublished studies; very few included rigorous statistical analysis, and some were based on surveys (Franklin 1997).
This calls for rigorous reviews to more clearly elucidate the effects of these interventions, taking cognizance of the complex and multi‐factorial nature of adolescent sexuality and pregnancy.
Moreover, most of the reviews were limited to industrialised nations (DiCenso 2002), and thus could not account for any influences of social, cultural, and economic factors in diverse populations. Such reviews have limited value to bilateral agencies and international NGOs working in the field of adolescent health promotion. In light of this, the Cochrane systematic approach was used to limit bias (systematic errors) and reduce chance effects, thereby providing more reliable results upon which to draw conclusions and make rational and evidence‐based recommendations (Antman 1992; Oxman 1993). This review draws from the expertise and resources already developed within Cochrane in general and Cochrane Fertility Regulation in particular.
In this review, we assessed and summarised the effects that adolescent pregnancy prevention interventions have on: [i] adolescents' knowledge and attitudes relating to risks of unintended pregnancies, [ii] delay in initiation of sexual intercourse, [iii] consistent use of birth control methods, and [iv] reduction in unintended pregnancies. To reduce publication bias (Cook 1993, Dickersin 1990), we considered all published and unpublished randomised controlled studies that assessed the effectiveness of interventions to reduce unintended pregnancy among adolescents, written in any language. Studies conducted in both high‐income and middle‐ and low‐income countries were also considered (WHO 1995). This body of evidence will help to elucidate what works, and what does not in the efforts to reduce unintended pregnancies among adolescents, and thus help to justify the use of scarce resources, train public health professionals, and facilitate the design of interventions that are effective.
Objectives
To assess the effects of primary prevention interventions (school‐based, community/home‐based, clinic‐based, and faith‐based) on unintended pregnancies among adolescents.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials, including cluster randomised trials where the unit of randomisation is the household, community, youth centre, school, classroom, health facility, or faith‐based institution.
Types of participants
Male and female adolescents aged 10 years to 19 years
Types of interventions
Any activity (either health education or counselling only, health education plus skills‐building, health education plus contraception‐education, contraception education and distribution, faith‐based group or individual counselling) designed to increase adolescents' knowledge and attitudes about the risk of unintended pregnancies, promote delay in initiation of sexual intercourse, encourage consistent use of birth control methods, and reduce unintended pregnancies. Where our search strategy identified studies that were not specifically designed to influence adolescent pregnancy, but were later reported to influence any of our primary or secondary outcomes, we included such studies if they met the other eligibility criteria.
We categorised interventions as follows.
Educational interventions: health education, HIV/STD education, community services, counselling only, health education plus skills‐building, faith‐based group or individual counselling.
Contraceptive‐promoting interventions: contraception‐education with or without contraceptive distribution.
Multiple interventions: combination of educational interventions with contraceptive‐promotion interventions.
Control: no additional activity/intervention to existing conventional population‐wide activities.
Types of outcome measures
Primary outcomes
Unintended pregnancy.
Secondary outcomes
Reported changes in knowledge and attitudes about the risk of unintended pregnancies.
Initiation of sexual intercourse.
Use of birth control methods
Abortion.
Childbirth.
Morbidity related to pregnancy, abortion or childbirth.
Mortality related to pregnancy, abortion or childbirth.
Sexually transmitted infections (including HIV).
Search methods for identification of studies
See: Cochrane Fertility Regulation methods used in reviews.
We did not impose any language restrictions, and sought translations where necessary. We did not impose any restrictions on journal of publication and used no country names or other geographical terms in the search. Full search strategies are shown below (Appendix 1).
Electronic searches
We searched all relevant studies regardless of language or publication status (published, unpublished, in press, and in progress).
We searched the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library) online; Issue 11 November 2015.
The Cochrane Fertility Regulation Trials Search Co‐ordinator helped us to search the Group's specialised trial register (Code: SR‐FERTILREG).
We searched the following electronic databases: MEDLINE (1966 to November 2015), EMBASE (1980 to November 2015), Dissertations Abstracts Online (http://library.dialog.com/bluesheets/html/bl0035.html), The Gray Literature Network (http://www.osti.gov/graylit/), HealthStar, PsycINFO, CINAHL and POPLINE for randomised controlled trials using the Cochrane Fertility Regulation search strategy (Helmerhorst 2004).
We searched LILACS (La Literatura Latinoamericana y del Caribe de Informacion en Ciencias de la Salud) database 2015 (www.bireme.br; accessed November 2015) and the Social Science Citation Index and Science Citation Index (1981 to November 2015).
We searched the Specialist Health Promotion Register (Social Science Research Unit (SSRU), Institute of Education, University of London at: http://eppi.ioe.ac.uk; June 2005)
For search terms, see Appendix 1.
Searching other resources
In addition, we contacted individual researchers, national and international research institutes/centres and organisations (including non‐governmental organisations) working in the field of adolescent reproductive health in order to obtain information on unpublished and on‐going trials. To ensure that no relevant studies were left out, we read through the list of references in each identified study in order to follow up on articles that may have qualified for inclusion in the review.
Data collection and analysis
One hundred and forty‐two (142) potentially relevant studies were identified of which 53 studies met the inclusion criteria and two are awaiting data extraction (Studies awaiting classification) pending the collection of complete data from the study authors.
Selection of studies
Two authors (CO and EE) independently applied the inclusion criteria to all identified studies and made decisions on which studies to include. The studies were initially checked for duplicates and relevance to the review by looking at the titles and abstracts. Where it was not possible to exclude a publication by looking at the title or the abstract, the full paper was retrieved. Differences were resolved by discussion and consultation with a third author (MM, HE or JE) when in doubt. The results section of each publication was blinded during screening to minimise bias. There were no language preferences in the search or the selection of articles.
Data extraction and management
Two authors (CO and EE) undertook data extraction using a standard data extraction form. We extracted the following data from each study that qualified for inclusion in the review.
Methods: the nature of concealment of allocation to study or control group (whether adequate, unclear, inadequate, or not done), study duration, type of trial, provider and outcome assessor blinding, extent of drop‐outs and cross‐overs, co‐interventions, other potential confounders, and any validity criteria that were used.
Participants: study setting (including country, state, region, community) and unit of randomisation (schools, households, communities, faith‐based institutions), age, gender, race/ethnicity, and other socio‐demographic characteristics of participants.
Interventions: nature of the intervention delivered to the study and control groups, and how it was delivered; timing and duration, and length of follow‐up.
Outcome measures and results: differences between intervention and control groups in terms of unintended pregnancy (first pregnancy), reported knowledge and attitudes about the risk of unintended pregnancies, initiation of sexual intercourse, use of birth control methods, abortion, childbirth, morbidity related to pregnancy, abortion or childbirth, and mortality related to pregnancy, abortion or childbirth.
Missing data: missing data arose from two sources, participant attrition and missing statistics.
Assessment of risk of bias in included studies
We assessed the methodological quality of included studies using standard methods for randomised controlled trials as described in the Cochrane Handbook for Systematic Reviews of Interventions Version 5.1 (Higgins 2011a).
We considered six parameters: generation of allocation sequence, concealment of allocation sequence, blinding, incomplete outcome data, selective outcome reporting and other sources of bias.
-
Generation of allocation sequence:
Yes ‐ if the method described was suitable to prevent selection bias (such as computer‐generated random numbers, table of random numbers or drawing lots);
Unclear ‐ if the method was not described but trial was described as "randomised"; and
No ‐ if sequences could be related to prognosis (case record number, date of birth, day, month, or year of admission).
-
Concealment of allocation:
Yes ‐ if there was evidence that the authors took proper measures to conceal allocation through, for example, centralised randomisation or use of serially‐numbered, opaque, sealed envelopes;
Unclear ‐ if the authors either did not report an allocation concealment scheme at all, or reported an approach that is unclear;
No ‐ if concealment of allocation was inadequate (such as alternation or reference to participant identification numbers or dates of birth).
-
Blinding:
Yes ‐ if there was evidence of no blinding and outcomes were unlikely to be influenced by lack of blinding, or blinding of participants and key study personnel was ensured and unlikely that blinding was broken, or outcome assessment was blinded and the non‐blinding of others was unlikely to introduce bias;
Unclear ‐ insufficient information or outcome not addressed;
No ‐ no blinding and outcome likely to be influenced by lack of blinding or blinding carried out but likely to be broken.
-
Incomplete outcome data:
Yes ‐ if there is evidence that there are no missing outcome data, or reason for missing outcome data unlikely to be related to true outcome, or missing outcome data balanced in numbers across intervention groups and with similar reasons across groups, or for dichotomous outcome data, the proportion of missing outcomes compared with observed event risk not enough to have a clinically‐relevant impact on the intervention effect estimate, or for continuous outcome data, plausible effect size (difference in means or standardised difference in means) among missing outcomes not enough to have a clinically‐relevant impact on observed effect size, or missing data have been imputed using appropriate methods;
Unclear ‐ insufficient reporting of attrition/exclusions to permit judgement of ‘Yes’ or ‘No’ (e.g. number randomised not stated, no reasons for missing data provided) or outcome not addressed;
No ‐ reason for missing outcome data likely to be related to true outcome, with either imbalance in numbers or reasons for missing data across intervention groups or for dichotomous outcome data, the proportion of missing outcomes compared with observed event risk enough to induce clinically‐relevant bias in intervention effect estimate, or for continuous outcome data, plausible effect size (difference in means or standardised difference in means) among missing outcomes enough to induce clinically relevant bias in observed effect size, or ‘as‐treated’ analysis done with substantial departure of the intervention received from that assigned at randomisation, or potentially inappropriate application of simple imputation.
-
Selective outcome reporting:
Yes ‐ if there is evidence that all of the study’s pre‐specified (primary and secondary) outcomes that are of interest in the review have been reported as stated in the protocol, or it is clear that the published reports include all expected outcomes, including those that were pre‐specified in the absence of the protocol;
Unclear ‐ insufficient information to permit judgement of ‘Yes’ or ‘No’;
No ‐ not all of the study’s pre‐specified primary outcomes have been reported; or one or more primary outcomes is reported using measurements, analysis methods or subsets of the data (e.g. sub scales) that were not pre‐specified, or one or more reported primary outcomes were not pre‐specified, or one or more outcomes of interest in the review are reported incompletely so that they cannot be entered in a meta‐analysis, or the study report fails to include results for a key outcome that would be expected to have been reported for such a study.
-
Other sources of bias:
Yes ‐ if study is free of other sources of bias;
Unclear ‐ insufficient information to assess if an important risk of bias exists or insufficient rationale or evidence that an identified problem will introduce bias;
No ‐ has extreme baseline imbalance or claimed to have been fraudulent or stopped early due to some data‐dependent process (including a formal ‐ stopping rule) or potential source of bias related to the specific study design used.
Measures of treatment effect
We performed data entry and analysis in Review Manager (RevMan) version 5.3 (RevMan 2014). For meta‐analysis of categorical variables we calculated Relative Risk (RR) or Peto's Odds Ratio (OR) with 95% confidence interval (Cl). For meta‐analysis of continuous variables we calculated mean differences (MD).
Unit of analysis issues
Cluster randomised trials
Only cluster‐randomised trials for which adjustment had been made for design effect were included in the meta‐analyses. Where possible, we corrected for design effects using standard procedures (Rao 1992). Before entering the results of cluster‐randomised studies into RevMan, we transformed outcome data according to the procedure in the Cochrane Handbook for Systematic Reviews of Interventions ( Adam 2004; Deeks 2011), dividing the number of events and number of participants by the design effect [1 + (1 ‐ m) * r]. We used the details provided by each study (total n and number of clusters) to calculate the average cluster size (m). Since most of the trials did not provide the intra cluster correlation coefficient, we adopted a fairly reliable intra cluster correlation coefficient of 0.02 which had been used in a similar systematic review (DiCenso 2002).
Trials with multiple groups
Eleven studies had multiple groups ( Dilorio 2006; Downs 2004; Herceg‐Brown 1986; Jemmott 1998; Jemmott 2005; Markham 2012; Morberg 1998;, Norton 2012; O'Donnell 1999; Raine 2005, Walker 2006, ). For studies included in the meta‐analyses (Dilorio 2006; Herceg‐Brown 1986; Jemmott 1998; Morberg 1998; Raine 2005), we combined all relevant experimental intervention groups in the studies into a single group. The same was done for the control groups as recommended by the Cochrane Handbook for Systematic Reviews of Interventions, Section 16.5.4 .(Higgins 2011b) For studies with multiple follow‐up points, we used data from the last time points.
Dealing with missing data
Missing data arose from participant attrition and missing statistics.
Where possible, we extracted data by allocation intervention, irrespective of compliance with the allocated intervention, in order to allow an 'intention‐to‐treat' analysis, as this minimizes bias (Hollis, 1999); otherwise we performed an 'as‐treated' analysis. We included these variables in a meta‐analysis using Review Manager (RevMan) 5.3 for the outcomes selected above (RevMan 2014). We conducted sensitivity analyses to investigate attrition as a source of heterogeneity and possible bias.
Where statistics were missing (numbers of participants per group, attrition rates, percentage affected for each outcome), we contacted primary study authors to supply the information. Where the information was unavailable due to data loss or non‐response, we reported the available results as stated in the trial report in the Additional table (Table 5).
1. Studies that Could not be included in meta‐analysis.
| Intervention | Outcome | Study ID | Number Assessed | Case affected | Control affected | Test Statistics | 95% CI | p‐value |
| Educational intervention | Pregnancy | Mitchell‐DiCenso 1997 | 1701 | ‐ | ‐ | OR: 0.97 | 0.93 to 1.0 | 0.04 |
| Initiation of intercourse | Clark 2005 | 156 | ‐ | ‐ | Beta: 1.604 and SE: 1.00 | ‐ | < 0.11 | |
| Aarons 2000 (females) | 139 | Adj. OR: 1.88 | 1.02 to 3.47 | 0.04 | ||||
| Aarons 2000 (males) | 123 | Adj. OR: 1.18 | 0.61 to 2.29 | 0.62 | ||||
| Perskin 2015 | 1079 | ‐ | ‐ | OR: 1.00 | 0.70 to 1.41 | |||
| Changes in knowledge and attitudes about the risk of unintended pregnancy | Blake 2001 | 351 | 92.9% | 91.8% | ns | |||
| Use of birth control at last sex | Mitchell‐DiCenso 1997 (females) | 109 | 42.2% | 46.7% | OR: 1.03 | 1.00 to 1.07 | 0.03 | |
| Mitchell‐DiCenso 1997 (males) | 214 | 39.3% | 35.9% | OR: 1.06 | 1.02 to 1.77 | 0.005 | ||
| Aarons 2000 (females) | 135 | Adj. OR: 3.39 | 1.16 to 9.95 | 0.025 | ||||
| Aarons 2000 (males) | 125 | Adj. OR: 1.53 | 0.55 yo 4.26 | 0.42 | ||||
| Use of condom at last sex | Okonofua 2003 | 1896 | 39.1% | 31.9% | OR: 1.41 | 1.12 to 1.77 | ‐ | |
| Clark 2005 | 221 | 77% | 73% | |||||
| Unprotected intercourse in the past 3 monthsa | Kogan 2012 | 502 | Beta: ‐0.375 and SE: 0.32 | >0.05 | ||||
| Ever had sex without condoms | Dilorio 2007 | Mean: 0.23 | Mean: 0.57 | ‐0.61 to ‐0.06 | 0.03 | |||
| Multiple interventions | Pregnancy | Coyle 2006 | 308 | ‐ | ‐ | OR; 0.84 | ‐ | 0.61 |
| Diclemente 2004 | 460 | ‐ | ‐ | OR: 0.53 | 0.27 to 1.03 | 0.06 | ||
| Stephenson 2004b | 1172 | 2.3% | 3.3% | ‐ | ‐ | 0.07 | ||
| Kirby 2004 | 2145 | ‐ | ‐ | OR: 1.34 | 0.98 to 1.84 | 0.07 | ||
| Coyle 2006 | 417 | ‐ | ‐ | OR: 0.77 | 0.49 to 1.23 | 0.28 | ||
| Smith 1994 | 95 | ‐ | ‐ | ‐ | ‐ | < 0.05 | ||
| O'Donnell 2002 | 195 | 6.8% | 18.5% | |||||
| Morrison‐Beedy 2013 | 323 | B=‐.823 OR: 0.44 |
0.009 | |||||
| Allen 1997 | 560 | ‐ | ‐ | OR: 0.41 | ‐ | ‐ | ||
| Initiation of sexual intercourse (mixed gender) | Coyle 2006 | 94 | ‐ | ‐ | OR: 1.23 | 0.51 to 2.97 | 0.65 | |
| Smith 1994 | 95 | .Mean: 1.19 | .Mean: 2.74 | |||||
| Basen‐Engquist 2001 | 8326 | ‐ | ‐ | OR: 1.03 | 0.88 to 1.21 | 0.69 | ||
| Markham 2012 | 627 | AOR:0.65 | 0.54,0.77 | <.01 | ||||
| O'Donnell 2002 | 195 | 40.1% | 66.1% | OR: 0.39 | 0.20 to 0.76 | 0.005 | ||
| Markham 2012 | 735 | AOR:0.82 | 0.51,1.34 | >0.05 | ||||
| Coyle 1999 | 2565 | OR:1.13 SE: 0.24 |
0.71 to 1.82 | 0.60 | ||||
| Initiation of sexual intercourse (male) | Coyle 2004 | 1412 | 19.3% | 27.7% | model R2: 0.118 | ‐ | 0.02 | |
| Kirby 2004 | 809 | ‐ | ‐ | OR: 1.08 | 0.80 to 1.46 | 0.63 | ||
| Stephenson 2004 | 8156 | 32.7% | 31.1% | OR: 0.90 | 0.65 to 1.23 | 0.35 | ||
| Eisen 1990 | 408 | 36% | 44% | ‐ | ‐ | ‐ | ||
| Initiation of sexual intercourse (female) | Coyle 2004 | 1417 | 20.3% | 22.1% | model R2: 0.145 | ‐ | 0.53 | |
| Kirby 2004 | 1220 | ‐ | ‐ | OR: 0.88 | 0.59 to 1.31 | 0.54 | ||
| Stephenson 2004 | 8156 | 34.7% | 40.8% | OR: 0.80 | 0.66 to 0.97 | 0.008 | ||
| Eisen 1990 | 480 | 27% | 22% | ‐ | ‐ | ‐ | ||
| Use of condoms at last sex | Kirby 2004 | 2145 | ‐ | ‐ | OR: 1.38 | 1.06 to 1.79 | 0.02 | |
| Coyle 2006 | 359 | ‐ | ‐ | OR: 1.00 | 0.49 to 1.23 | 0.99 | ||
| Diclemente 2004 | 460 | ‐ | ‐ | OR: 3.94 | 2.58 to 6.03 | < .001 | ||
| Downs 2004 | 258 | ‐ | ‐ | OR: 2.13 | ‐ | 0.15 | ||
| Norton 2012 | 198 | OR: 0.93 | ‐0.75,0.62 | 0.85 | ||||
| Coyle 1999 | 1018 | OR:191 SE:0.27 |
1.13 to 3.21 | 0.02 | ||||
| Childbirth | Henderson 2007 | 4196 | 300/1000 | 274/1000 | OR: 14.6 | 0.32 | ||
| Abortion | Henderson 2007 | 4196 | 127/1000 | 112/1000 | OR: 26.4 | 0.40 | ||
| Consistent condom use at 12 months | Sieving 2011 | 253 | Mean: 0.96 (116/126) | Mean: 0.66 (81/127) | ARR:145 | 1.26 to 1.67 | 0.00 | |
| Consistent condom use at 24 months | Sieving 2011 | 204 | Mean:1.53 | Mean: 0.93 | ARR: 1.57 | 1.28,1.94 | ||
| Consistent hormonal contraceptive use at 12 months | Sieving 2011 | 253 | Mean: 4.27 (74/126) | Mean: 2.91 (51/127) | ARR:1.46 | 1.13 to 1.89 | 0.00 | |
| Consistent hormonal contraceptive use at 24 months | Sieving 2011 | 203 | Mean: 3.29 | Mean: 2.34 | ARR: 1.30 | 1.06,1.58 | ||
| Minnis 2014 | 162 | OR:0.42 | 0.12 | |||||
| Use of condoms at first sex | Coyle 1999 | 285 | OR:0.68 SE:0.48 |
0.26 to 1.75 | 0.42 | |||
| Protected against pregnancy at last sex | Coyle 1999 | 998 | OR:1.62 SE:0.22 |
1.05 to 2.50 | 0.03 | |||
| Sexually Transmitted Infections | Morrison‐Beedy 2013 | 323 | B=‐0.067 OR: ‐0.94 |
0.77 | ||||
| Jemmott 2005c | Mean:10.5 SE: 2.9 |
Mean:18.2 SE:2.8 |
0.05 | |||||
|
Baird 2010: The following listed outcomes were reported. However, the method of reporting made difficult to extract correct estimates. 1. Pregnancy School girls and dropouts among the treatment group are 1.1 percentage points less likely to have become pregnant over the past year. Not statistically significant. 2. Onset of sexual intercourse There was a 46.6% reduction in the onset of sexual activity among initial dropouts (P < 0.01) and a 31.3% reduction in the onset of sexual activity among initial schoolgirls (P = 0.112). 3.Condom use The intervention had no impact on self‐reported condom use. | ||||||||
a ‐ Binary outcome (did unprotected intercourse occur or not?)
b ‐ Study (Stephenson 2008) same as Stephenson 2004, but with an extended follow up (7yrs)
c ‐ Data comparing skills‐based intervention versus health‐promotion intervention
Analyses assessing impact on delay of sexual initiation excluded individuals who reported any type of sexual intercourse at baseline
Analyses assessing impact on other on sexual behaviours are limited to individuals that are sexually active
ns ‐ non‐significant
Assessment of heterogeneity
We assessed data sets for heterogeneity by visual assessment of forest plots and chi2 tests for heterogeneity with a 10% level of statistical significance, and applied the I2 statistic with a value of 50% or higher denoting significant levels of heterogeneity.
Assessment of reporting biases
Since asymmetry of funnel plots may result from publication bias, heterogeneity, or poor methodological quality (Sterne 2011), we planned to examine funnel plots using Review Manager 5.3 but found an insufficient number of trials to do this.
Data synthesis
We used a fixed‐effects model (FEM) for data synthesis and a random‐effects model (REM) for cases where we detected heterogeneity, and considered it appropriate to still perform meta‐analysis.
Subgroup analysis and investigation of heterogeneity
We sub‐grouped the use of birth control into 'condom use at last sex', 'consistent condom use', 'contraceptive use at last sex', 'consistent contraceptive use' and 'use of hormonal contraceptive'. We found insufficient data to conduct sub‐group analysis of homosexual and heterosexual intercourse. We excluded quasi‐experimental studies (controlled before‐and‐after, and interrupted time series) as this was cumbersome and would have delayed the update of this review.
Sensitivity analysis
We conducted sensitivity analysis of the primary outcome (unintended pregnancy) including and excluding trials with high attrition rates (> 20%). The number of trials that used adequate allocation concealment was insufficient to allow for sensitivity analysis to assess the possible influence of high risk of bias in trials that did not apply allocation concealment.
Results
Description of studies
Results of the search
We found 142 studies, of which we included 53 and excluded 87 , with two awaiting assessment (Characteristics of studies awaiting classification); we have approached the primary authors of these papers for relevant additional information.
Included studies
All the studies were randomised controlled trials. Eighteen of the studies randomised individuals, 32 randomised clusters (schools (20), classrooms (6), and communities/neighbourhoods such as community‐based organisations and social networks (6). Three studies were mixed (individually and cluster randomised) (Allen 1997; Eisen 1990; Kirby 1997b). The length of follow up varied from three months to seven years, with greater than 12 months being the most common duration.
Participants
A total of 105,368 participants were included in all the included studies. The number of participants per study varied greatly (Characteristics of included studies). Most of the studies confined inclusion of participants to specific age requirements, others restricted inclusion based on specific school grade levels (varying between 6th grade to 12th grade). The age of participants in the included studies ranged from 9 years to 19 years, except for seven studies which included participants aged 9 years to 24 years: Baird 2010, 13 years to 22 years; Mba 2007, 10 years to 20 years; Minnis 2014, 16 years to 21 years; Okonofua 2003, 14 years to 20 years; Raine 2005, 15 years to 24 years (mean 19.9); Raymond 2006, 14 years to 24 years; and Shrier 2001, 13 years to 22 years (median 17). For these studies, more than 75% of the participants were within the stipulated age limit of 10 years to 19 years. Sixteen studies included participants who were sexually active (Baird 2010; Bonell 2013; Diclemente 2004; Downs 2004; Jemmott 2005, Jemmott 2010; Kogan 2012; Markham 2012; Mba 2007; Minnis 2014; Morrison‐Beedy 2013; Norton 2012; O'Donnell 1999; Raine 2005; Raymond 2006; Sieving 2011); one study recruited adolescent mothers < 18 years at time of delivery living with their mothers (Black 2006); three studies recruited dyads (adolescents and their guardian) (Dilorio 2006; Dilorio 2007; Guilamo‐Ramos 2011b). Most studies included male and female participants. Eighteen studies included female participants only (Allen 1997; Baird 2010; Black 2006; Bonell 2013; Cabezon 2005; Diclemente 2004; Downs 2004; Ferguson 1998; Guilamo‐Ramos 2011b; Henderson 2007; Herceg‐Brown 1986; Howard 1990; Jemmott 2005; Morrison‐Beedy 2013; Raine 2005; Raymond 2006; , Shrier 2001; Sieving 2011) and one, male participants only (Dilorio 2007).
Setting
Four trials were conducted in low‐ and middle‐income countries (Baird 2010; Fawole 1999; Mba 2007; Okonofua 2003), and all others were conducted in high‐income countries: United States of America (41), England (2), Scotland (2), Canada (1), Italy (1) and Mexico (2). Most of the studies were conducted in schools. Other sites included hospitals or family planning health agencies, neighbourhoods/communities and clubs.
Interventions
Educational interventions
Six studies compared an educational interventions to a standard school curriculum (control): Aarons 2000; Blake 2001; Clark 2005; Dilorio 2007 (parent‐based educational intervention); Mitchell‐DiCenso 1997; and Perskin 2015 (computer‐based sexual health education). Three studies compared the intervention to regular health promotion classes or no control intervention (Kogan 2012; Mba 2007; Okonofua 2003). One study offered the same intervention to the two groups but with different instructors (peers or teachers) (Borgia 2005). Another study compared a parent‐based intervention based on social cognitive theory (intervention 1) and a life skills programme based on problem behaviour theory (intervention 2) versus a one‐hour HIV‐prevention session (control) (Dilorio 2006);
Contraceptive‐promoting interventions
Two studies compared the effect of improving access to contraception. Raine 2005 had two intervention groups (pharmacy access and advance provision of contraceptives) and a control (clinic access, as needed); Raymond 2006 compared increased access to contraceptives (unlimited free supply) versus standard access (as needed, at usual cost). Another study compared contraception education to usual school sex education (Graham 2002).
Multiple interventions (educational and contraceptive‐promoting interventions)
Twelve studies compared a combination of educational interventions and contraceptive‐promoting interventions with standard school curriculum (sex or HIV/AIDS education) (Basen‐Engquist 2001; Coyle 1999; Coyle 2004; Coyle 2006; Eisen 1990; Fawole 1999; Henderson 2007; Howard 1990; Kirby 1997a; Kirby 2004; Shrier 2001; Wight 2002). Sieving 2011 compared multiple interventions linked to clinical services versus usual clinical service only for 17 months and 24 months, and Bonell 2013 compared weekly three‐hour sessions over 18 weeks to 20 weeks in pre‐school nurseries developing parenting, self‐awareness and confidence versus health promotion only . Three studies added community youth services to their intervention versus the following control groups: regular health curriculum (Allen 1997) and standard class curriculum (O'Donnell 1999; O'Donnell 2002).
Four studies compared multiple interventions with health promotional interventions unrelated to sexual behaviour, or no intervention for the control groups (Cabezon 2005; Diclemente 2004; Morrison‐Beedy 2013; Villarruel 2006 ). One study offered written materials on the lessons covered in the intervention programme to the control group (Smith 1994).
Nine studies compared more than one intervention (multiple intervention groups). Jemmott 1998 had two interventions, one with an emphasis on abstinence versus one with an emphasis on the use of contraceptives, compared to a health promotion control. Jemmott 2005 compared the same intervention (informative versus skills‐based (practical) versus health promotion (control). Kirby 1997b compared an adult‐led intervention versus a youth‐led intervention (each with the same contents) compared to the standard sex curriculum. Markham 2012 compared risk avoidance (abstinence until marriage) versus risk reduction (with the emphasis on abstinence until older) versus a control of regular health classes. Morberg 1998 compared a four‐week intervention over three years in one intervention group and a 12‐week intervention over one year in the other, versus the usual school curriculum. Walker 2006 used the same intervention for both intervention groups but one emphasised the use of condoms and the other emphasised access to condoms and emergency contraceptives, versus biology‐based sex education.. . . Two studies compared three intervention groups with different aims. Jemmott 2010 compared three different levels of training: enhanced training (intervention package, two days' training plus hands‐on training/practice); standard training (intervention package plus two days' training); and manual only (intervention package provided to participants but no training) compared to non‐sexual‐related health promotion intervention (control). Norton 2012 compared the promotion of condom use to prevent an unplanned pregnancy (pregnancy intervention), STI (STI intervention), and HIV (HIV intervention), versus standard health services received by students. . Herceg‐Brown 1986 had two intervention groups, regular clinic services plus 50 minutes of family or individualised counselling services on sex and contraceptive education for six weeks known as the 'Family support group', versus regular clinic services plus staff support through two to six telephone calls four to six weeks after the initial clinic visit, known as the 'Periodic support group', versus regular clinic services.
One study, Downs 2004 had one intervention and two control groups. The same information was provided to the control groups as to the intervention group, however they differed in their mode of administration (interactive video versus book form or brochure for the controls). Another study, Guilamo‐Ramos 2011b evaluated a parent‐based intervention (health education and skills‐building); parents and their adolescent children participated in the intervention, versus standard health promotion for nine months.
Two studies offered some form of incentive to the intervention group; Minnis 2014 combined conditional cash transfers (CCT) as an incentive for completing educational, reproductive health and life skills sessions; while Baird 2010 provided CCT (an incentive for schoolgirls and dropouts to stay in school or return to school respectively), with the aim of reducing certain sexual behaviours.
One study offered peer‐led multiple interventions versus usual teacher‐led sex education (Stephenson 2004), while another compared same intervention administered by peer counsellors compared to adult staff (Ferguson 1998).
One study compared the intervention with an alternative youth programme (recreational activities, art & crafts) (Philliber 2002).
Black 2006 aimed to prevent a second unintended pregnancy. The intervention involved a home‐mentoring programme (home visits every week until the infant's first birthday, approximately 19 visits) compared to a no‐intervention control ().
Outcomes
Twenty studies assessed and reported on unintended pregnancy (Allen 1997; Bonell 2013; Cabezon 2005; Coyle 2006; Diclemente 2004; Ferguson 1998; Herceg‐Brown 1986; Howard 1990; , Kirby 1997a; Kirby 1997b; Kirby 2004; Mitchell‐DiCenso 1997; Morrison‐Beedy 2013; O'Donnell 2002; Philliber 2002; , Raine 2005; Raymond 2006; Smith 1994; Stephenson 2004; Wight 2002 , , , , ) and one study reported second unintended pregnancy (Black 2006). Other outcomes reported were initiation of intercourse, consistent use of contraceptives or condoms, use of contraceptives or condoms at last sex, use of hormonal contraceptives, knowledge about the risk of pregnancy, abstinence, sexually transmitted diseases, childbirth and abortion.
Most studies reported outcomes on the change in knowledge of STD, HIV, AIDS, condom and contraceptive use, as well as intentions to use condoms, contraceptives or have sex. However, these were not part of the outcomes assessed in this review and therefore were not reported.
Excluded studies
Eighty‐four studies were excluded; forty‐six studies, though randomised studies were excluded for one or more of the following reasons: none of the desired outcomes was measured, participants were either pregnant or couples, more than 25% of the participants were above the required age range, the study did not use the desired intervention, there was no formal control group, had no protocol, and the stated method of randomisation was not adequate. The remaining studies (38) were not randomised controlled studies (Characteristics of excluded studies).
No ongoing studies were found.
Risk of bias in included studies
1.
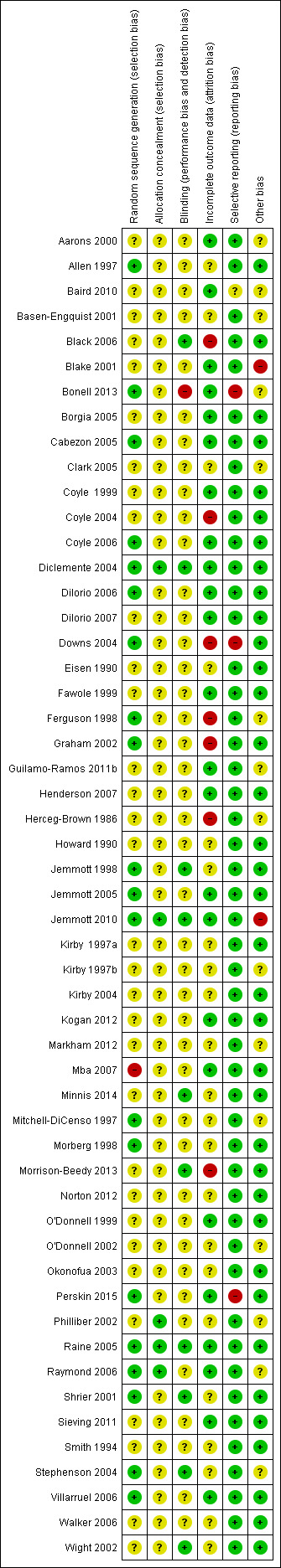
Risk of bias summary: review authors' judgments about each risk of bias item for each included study.
2.
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Allocation
Generation of allocation sequence: ten studies used a computer‐generated allocation sequence (Bonell 2013; Dilorio 2006; Graham 2002; Jemmott 1998; Jemmott 2005; Jemmott 2010; Raine 2005; Raymond 2006; Stephenson 2004; Villarruel 2006), four used a table of random numbers (Diclemente 2004; Downs 2004; Mitchell‐DiCenso 1997, Shrier 2001), one used simple balloting (Cabezon 2005), two used coin toss technique (Allen 1997; Ferguson 1998). Two trials used restricted randomisation involving multiple steps (Coyle 2004, Coyle 2006), and two other studies used block randomisation (Morberg 1998; Philliber 2002,). One trial reported use of "balanced randomisation" (Wight 2002) but gave no details to explain the procedure, and another one used quarterly marking period within school (Blake 2001). One study used a modified "multi‐attribute randomization method", providing no further details (Perskin 2015). The remaining studies (29) had insufficient or no information on the randomisation generation method, and used terms such as "assigned at random" or "randomly assigned", leaving us uncertain whether the trial results were vulnerable to selection bias.
Allocation concealment: four studies reported adequate allocation concealment that used sealed, opaque envelopes (Diclemente 2004; Philliber 2002; Raine 2005; Raymond 2006). The remaining studies did not provide information on concealment of allocation.
Baseline differences can be increased by inadequate and clustered randomisation sequences. Out of the 53 trials, 17 reported at least one significant group difference at baseline (Aarons 2000; Allen 1997; Basen‐Engquist 2001; Coyle 2004; Coyle 2006; Dilorio 2006; Jemmott 1998; Jemmott 2005; Jemmott 2010; Kirby 1997b; Markham 2012; Mitchell‐DiCenso 1997; Morberg 1998; Okonofua 2003; Raymond 2006; Smith 1994 ) and each one of these trials controlled for baseline differences in analyses. One study Mba 2007, did not test for baseline differences between groups.
Three trials did not report a clear statement of baseline differences between groups (Dilorio 2007; Ferguson 1998; Henderson 2007) but controlled for these differences in their analyses. One trial used a significance level of P < 0.01 for these calculations (Kirby 1997a), and two reported baseline differences only for sexual behaviours (Clark 2005; O'Donnell 2002).
Blinding
For most of the trials, staff (assessors and administrators) were not blinded to group assignment, as every trial utilised written self‐reported questionnaires, although assessor blinding was reported in eight studies (Black 2006; Bonell 2013; Diclemente 2004; Jemmott 1998; Raine 2005; Shrier 2001; Stephenson 2004; Wight 2002 ). Two studies blinded participants and interviewers (Jemmott 2010; Minnis 2014). For one study, the condition was unknown to participant and facilitators until groups were filled and facilitators assigned (Morrison‐Beedy 2013) and for another, the condition was unknown only to participants until after baseline assessment (Perskin 2015). Blinding was not reported in the remaining 42 studies. The impossibility of blinding intervention staff may have given rise to performance bias.
Contamination or 'exchange of information' of the control group might have occurred as the intervention and control groups sometimes attended different programmes at the same site. This is more likely to be present in trials that randomised participants by individual or classroom, rather than by entire community centre, school or neighbourhood. This, however, leads to bias in the findings in the direction of no effect rather than in the direction of significance.
Incomplete outcome data
Attrition rates at final follow‐up ranged from 0.5% (Henderson 2007) to 58% (Coyle 2006). Five studies did not clearly explain/state the numbers of individuals lost to follow up (Baird 2010; Basen‐Engquist 2001; Blake 2001; Howard 1990; Norton 2012). Eighteen trials reported overall attrition rates that exceeded 20% at final follow up (Borgia 2005; Clark 2005; Coyle 2004; Coyle 2006; Dilorio 2007; Eisen 1990; Jemmott 2010; Kirby 1997a; Kirby 2004; Markham 2012; Mitchell‐DiCenso 1997; Morberg 1998; O'Donnell 2002; Philliber 2002; Shrier 2001; ,Smith 1994; Stephenson 2004; Walker 2006 , . ).
Most trials conducted a modified intention‐to‐treat analysis (whereby all students were included in the analysis regardless of number of sessions attended as long as they provided baseline and follow‐up data). Outcomes such as pregnancy, use of condoms, contraceptive and sexually transmitted diseases were analysed using the number who initiated sex or were already sexually active as the sample size (denominator). Coyle 2004 made use of a rich‐imputation model based on baseline peer norms, group, time, ethnicity, and group‐by‐time interaction to account for dropouts. O'Donnell 2002 conducted several sets of analyses according to different principles: not reporting results according to original dropouts.
Studies with outcomes that could not be included in the meta analysis are reported in Table 5.
Selective reporting
Apart from the primary outcome, most included studies reported a range of outcomes (sexual behaviour), using different recall periods and grouping outcomes such as initiation of intercourse at three months and six months, and use of condoms at last sex, thus suggesting no standard set of outcomes for evaluation, preventing a comprehensive meta‐analysis.
Results were also analysed based on subgroups of participants, for example, measuring initiation of intercourse among virgins and non‐virgins at baseline. However, more often, sexual initiation was often assessed only among participants who reported never having had sexual intercourse at baseline.
Few studies reported at least one outcome separately by gender without providing overall summaries of effect (Aarons 2000; Coyle 2004; O'Donnell 2002).
Due to missing information such as numbers of participants per trial arm and percentages for dichotomous outcomes, meta‐analysis could not be carried out for some studies (data presented in Table 5).
The lack of statistical controls for cluster‐randomised data, is a limitation for this study. While most cluster randomised studies controlled for clustering in their analyses, some did not (Aarons 2000; Allen 1997; Fawole 1999; Kirby 1997a), suggesting that studies which did not report statistical methods for dealing with clustered data analysed their results on an individual level.
Few studies attempted to control for the occurrence of a Type I error which is likely to occur when different outcomes are analysed; Allen 1997 and Raine 2005 used a Bonferroni correction when considering the significance of statistical tests, and Coyle 2004 stated it use though the method was not specified.
Other potential sources of bias
Limitations of self‐report and behavioural outcome data
Most of the studies made use of self‐reported data which is an inevitable source of bias for studies evaluating sexual behaviours (as there is the tendency for respondents to agree with statements associated with healthier behaviours or attitudes). However, the veracity of the self‐reported behaviours was improved by privacy and confidentiality in most studies.
Heterogeneity in programme design and implementation across trials
A major source of bias in this review is a high degree of heterogeneity in the ways programmes were designed and implemented across trials. This can be seen in some of the meta‐analyses carried out. Our inclusion criteria specified that we would accept interventions that aimed to prevent unintended pregnancy while promoting safer‐sex strategies such as condom use or contraceptive use but it is unclear how much emphasis was put on these goals. An example is Eisen 1990 that offered almost the same intervention to both groups differing only in the level of emphasis and duration of the intervention, or studies offering same intervention but administered differently such as peer‐counsellor facilitators versus adult staff (Ferguson 1998) and Downs 2004, interactive video versus book form or brochure of the same intervention.
Finding relevant trials
Though the search for relevant trials was comprehensive, it is likely that relevant trials may have been omitted from this review, if the specified search terms were not mentioned in the title and abstracts but most likely due to inability to assess all unpublished trials.
Underreporting of implementation data
Inadequate description of programme design and implementation made the assessment of heterogeneity challenging. Differences in the way that programmes were designed, delivered, and taken up may have made the studies too heterogeneous to permit comparisons across trials; however, these differences are difficult to determine from the available data and could have influenced the meta‐analyses. Few studies reported strategies to monitor and promote the extent to which programmes were delivered by facilitators and taken up by participants as planned. Such strategies include take‐home assignments, keeping attendance records, conducting interviews with programme staff and participants, bringing in independent raters (Morrison‐Beedy 2013), conducting exit interviews with participants, and communication with participants by phone (Herceg‐Brown 1986, Dilorio 2006). One study regularly trained all programme staff, visiting each site regularly (Philliber 2002). Though these strategies were put in place, most trials rarely stated the extent of implementation fidelity. One study Morberg 1998, reported difficulties for community‐based programme activities to convey programme messages related to sexual behaviour due to vocal opposition; at one programme site, a member of the community opposition group attended every programme session related to sexual behaviour, potentially affecting programme delivery.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4
for the main comparison.
| Contraceptive‐promoting interventions (individual RCTs) | |||||
| Patient or population: Male and female adolescents aged 10 years to 19 years Setting: All settings Intervention: Contraceptive‐ promoting interventions Comparison: No additional activity/intervention to existing conventional population‐wide activities | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | |
| Risk with No intervention/standard curriculum | Risk with Contraception Intervention | ||||
| Unintended pregnancy follow up: range 6 months to 12 months | Study population | RR 1.01 (0.81 to 1.26) | 3440 (2 RCTs) | ⊕⊕⊕⊝ MODERATE 1 | |
| 83 per 1000 | 84 per 1000 (67 to 105) | ||||
| Moderate | |||||
| 85 per 1000 | 86 per 1000 (69 to 107) | ||||
| Use of birth control methods (condom use in last sex) follow up: range 6 months to 12 months | Study population | RR 0.95 (0.87 to 1.04) | 3091 (2 RCTs) | ⊕⊕⊕⊕ HIGH | |
| 367 per 1000 | 348 per 1000 (319 to 381) | ||||
| Moderate | |||||
| 312 per 1000 | 296 per 1000 (271 to 324) | ||||
| Use of birth control methods (hormonal contraceptives) follow up: range 6 months to 12 months | Study population | RR 2.22 (1.07 to 4.62) | 3091 (2 RCTs) | ⊕⊕⊕⊕ HIGH | |
| 165 per 1000 | 365 per 1000 (176 to 760) | ||||
| Moderate | |||||
| 131 per 1000 | 292 per 1000 (141 to 607) | ||||
| Sexually Transmitted Diseases follow up: range 6 months to 12 months | Study population | RR 0.92 (0.75 to 1.13) | 3440 (2 RCTs) | ⊕⊕⊕⊕ HIGH | |
| 103 per 1000 | 95 per 1000 (77 to 117) | ||||
| Moderate | |||||
| 98 per 1000 | 90 per 1000 (73 to 111) | ||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; OR: Odds ratio; | |||||
| GRADE Working Group grades of evidence High quality: We are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect Very low quality: We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect | |||||
1 Downgraded by 1 for imprecision: confidence interval fail to appreciable harm and included the null value
2.
| Educational interventions (cluster RCTs) | |||||
| Patient or population: Male and female adolescents aged 10 years to 19 years Setting: All settings Intervention: Educational interventions Comparison: No additional activity/intervention to existing conventional population‐wide activities | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | |
| Risk with No intervention/Standard curriculum | Risk with Educational intervention | ||||
| Use of birth control methods (condom use at last sex) follow up: range 5 months to 24 months | Study population | RR 1.18 (1.06 to 1.32) | 1431 (2 RCTs) | ⊕⊕⊕⊝ MODERATE 1 | |
| 261 per 1000 | 308 per 1000 (277 to 345) | ||||
| Moderate | |||||
| 534 per 1000 | 630 per 1000 (566 to 704) | ||||
| Initiation of sexual intercourse (mixed gender) follow up: range 12 months to 24 months | Study population | RR 0.95 (0.71 to 1.27) | 672 (2 RCTs) | ⊕⊕⊝⊝ LOW 1 2 | |
| 227 per 1000 | 215 per 1000 (161 to 288) | ||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; OR: Odds ratio; | |||||
| GRADE Working Group grades of evidence High quality: We are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect Very low quality: We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect | |||||
1 Several risk of bias assessment were unclear (not provided in the text)
2 Low number of events and confidence interval includes the null value
3.
| Multiple interventions (cluster RCTs) | |||||
| Patient or population: Male and female adolescents aged 10 years to 19 years Setting: All settings Intervention: Multiple interventions Comparison: No additional activity/intervention to existing conventional population‐wide activities | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | |
| Risk with No Intervention/Standard curriculum | Risk with Multiple interventions | ||||
| Unintended pregnancy follow up: range 3 months to 48 months | Study population | RR 0.50 (0.23 to 1.09) | 3149 (5 RCTs) | ⊕⊕⊝⊝ LOW 1 2 3 | |
| 67 per 1000 | 33 per 1000 (15 to 73) | ||||
| Moderate | |||||
| 25 per 1000 | 13 per 1000 (6 to 27) | ||||
| Initiation of sexual intercourse (mixed gender) follow up: range 3 months to 36 months | Study population | RR 0.84 (0.68 to 1.04) | 8608 (7 RCTs) | ⊕⊝⊝⊝ VERY LOW 1 4 5 | |
| 253 per 1000 | 212 per 1000 (172 to 263) | ||||
| Moderate | |||||
| 212 per 1000 | 178 per 1000 (144 to 220) | ||||
| Use of birth control methods (condom use at last sex) follow up: range 6 months to 17 months | Study population | RR 1.01 (0.93 to 1.09) | 2620 (4 RCTs) | ⊕⊕⊕⊝ MODERATE 1 6 | |
| 585 per 1000 | 591 per 1000 (544 to 637) | ||||
| Moderate | |||||
| 565 per 1000 | 570 per 1000 (525 to 615) | ||||
| Use of birth control methods (consistent condom use) follow up: range 6 months to 36 months | Study population | RR 1.95 (0.70 to 5.44) | 826 (3 RCTs) | ⊕⊕⊝⊝ LOW 1 7 | |
| 353 per 1000 | 689 per 1000 (247 to 1000) | ||||
| Moderate | |||||
| 133 per 1000 | 259 per 1000 (93 to 722) | ||||
| Use of birth control methods (hormonal contraceptives) follow up: range 16 months to 24 months | Study population | RR 1.01 (0.72 to 1.43) | 3987 (3 RCTs) | ⊕⊝⊝⊝ VERY LOW 1 5 7 | |
| 244 per 1000 | 246 per 1000 (176 to 349) | ||||
| Moderate | |||||
| 251 per 1000 | 254 per 1000 (181 to 360) | ||||
| Sexually Transmitted Diseases follow up: range 6 months to 17 months | Study population | RR 0.76 (0.27 to 2.14) | 420 (2 RCTs) | ⊕⊕⊝⊝ LOW 1 8 | |
| 37 per 1000 | 28 per 1000 (10 to 80) | ||||
| Moderate | |||||
| 31 per 1000 | 24 per 1000 (8 to 66) | ||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; OR: Odds ratio; | |||||
| GRADE Working Group grades of evidence High quality: We are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect Very low quality: We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect | |||||
1 Downgraded by 1 for risk of bias; several assessments were unclear due to no information provided. Such potential limitations are likely to lower confidence in the estimate of effect
2 Downgraded by 1 for imprecision; low number of events, confidence interval includes appreciable benefit and null value
3 Heterogeneity could be explained (difference in comparison intervention and length of follow up)
4 Downgraded by 1 for imprecision: confidence interval includes appreciable benefit
5 Downgraded by 1 for inconsistency: unexplained large variations in effect
6 Confidence interval includes the null value, however, the sample size and number of events are fairly large and confidence interval is relatively narrow
7 Downgraded by 1 for imprecision: confidence interval includes appreciable benefit and harm
8 Downgraded by 1 for imprecision; low number of events, confidence interval includes appreciable benefit and harm
4.
| Multiple interventions ( individual RCTs) | |||||
| Patient or population: Male and female adolescents aged 10 years to 9 years Setting: All settings Intervention: Multiple interventions Comparison: No additional activity/intervention to existing conventional population‐wide activities | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | |
| Risk with No Intervention/Standard curriculum | Risk with Multiple interventions | ||||
| Unintended pregnancy follow up: range 12 months to 36 months | Study population | RR 0.66 (0.50 to 0.87) | 1905 (4 RCTs) | ⊕⊕⊕⊝ MODERATE 1 | |
| 116 per 1000 | 76 per 1000 (58 to 101) | ||||
| Moderate | |||||
| 149 per 1000 | 98 per 1000 (74 to 129) | ||||
| Initiation of sexual intercourse (mixed gender) follow up: range 9 months to 36 months | Study population | RR 0.99 (0.74 to 1.32) | 1796 (4 RCTs) | ⊕⊕⊕⊝ MODERATE 1 | |
| 410 per 1000 | 406 per 1000 (304 to 542) | ||||
| Moderate | |||||
| 236 per 1000 | 234 per 1000 (175 to 312) | ||||
| Use of birth control methods (condom use in last sex) follow up: range 12 months to 24 months | Study population | RR 1.00 (0.95 to 1.06) | 796 (3 RCTs) | ⊕⊕⊕⊝ MODERATE 1 6 | |
| 840 per 1000 | 840 per 1000 (798 to 891) | ||||
| Moderate | |||||
| 837 per 1000 | 837 per 1000 (795 to 887) | ||||
| Use of birth control methods (consistent condom use) follow up: range 12 months to 24 months | Study population | RR 1.21 (0.95 to 1.54) | 1681 (5 RCTs) | ⊕⊕⊝⊝ LOW 1 5 6 | |
| 353 per 1000 | 427 per 1000 (335 to 544) | ||||
| Moderate | |||||
| 476 per 1000 | 575 per 1000 (452 to 732) | ||||
| Sexually Transmitted Diseases follow up: mean 12 months |
Study population | RR 0.89 (0.65 to 1.22) | 699 (2 RCTs) | ⊕⊝⊝⊝ VERY LOW 1 5 8 | |
| 191 per 1000 | 170 per 1000 (124 to 233) | ||||
| Moderate | |||||
| 270 per 1000 | 241 per 1000 (176 to 330) | ||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; OR: Odds ratio; | |||||
| GRADE Working Group grades of evidence High quality: We are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect Very low quality: We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect | |||||
1 Downgraded by 1 for risk of bias; several assessments were unclear due to no information provided. Such potential limitations are likely to lower confidence in the estimate of effect
2 Downgraded by 1 for imprecision; low number of events, confidence interval includes appreciable benefit and null value
3 Heterogeneity could be explained (difference in comparison intervention and length of follow up)
4 Downgraded by 1 for imprecision: confidence interval includes appreciable benefit
5 Downgraded by 1 for inconsistency: unexplained large variations in effect
6 Confidence interval includes the null value, however, the sample size and number of events are fairly large and confidence interval is relatively narrow
7 Downgraded by 1 for imprecision: confidence interval includes appreciable benefit and harm
8 Downgraded by 1 for imprecision; low number of events, confidence interval includes appreciable benefit and harm
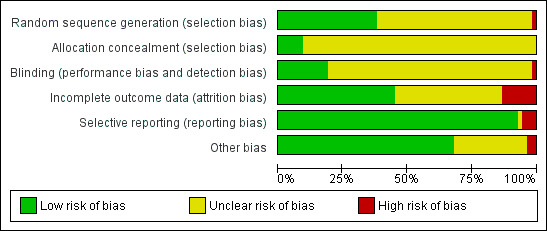
MULTIPLE INTERVENTIONS
Unintended pregnancy
Four individually randomised trials (Bonell 2013; Herceg‐Brown 1986; Morrison‐Beedy 2013; Philliber 2002), showed that risk of unintended pregnancy was significantly lower among participants that received multiple interventions compared with the control group; (RR 0.66, 95% CI 0.50 to 0.87; 4 studies; 1905 participants, Analysis 1.1).
1.1. Analysis.
Comparison 1 Multiple interventions, Outcome 1 Unintended pregnancy [individually randomised trials].
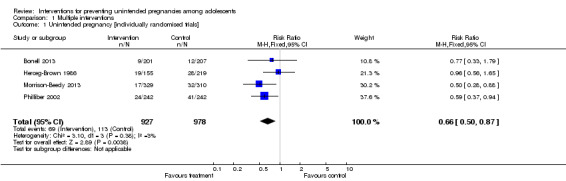
Five cluster trials (Cabezon 2005; Ferguson 1998; Howard 1990; Kirby 1997b; Wight 2002) that adjusted for design effect showed a 50% reduction in the risk of unintended pregnancy in the intervention group compared to the control group, although the difference was not statistically significant ((RR 0.50, 95% CI 0.23 to 1.09; 5 studies, 3149 participants, Analysis 1.2). However sensitivity analysis excluding trials with high attrition rates showed that the risk of unintended pregnancy was significantly lower in the intervention than control groups ((RR 0.20, 95% CI 0.10 to 0.39; 2 studies, 497 participants, Analysis 2.1). In addition, an analysis that combined cluster‐randomized trials (adjusted for design effect) with individually randomised trials (Bonell 2013; Cabezon 2005; Ferguson 1998; Herceg‐Brown 1986; Morrison‐Beedy 2013 ) showed significantly lower risk of unintended pregnancy in the intervention group compared to control (RR 0.53, 95% CI 0.39 to 0.72; 5 studies,1918 participants,Analysis 2.3 ). This sensitivity analysis showed a persistence of statistical heterogeneity with I2 statistic of 77% (Analysis 2.3).
1.2. Analysis.
Comparison 1 Multiple interventions, Outcome 2 Unintended pregnancy [cluster‐randomised trials].
2.1. Analysis.
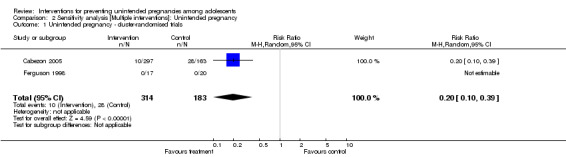
Comparison 2 Sensitivity analysis [Multiple interventions]: Unintended pregnancy, Outcome 1 Unintended pregnancy ‐ cluster‐randomi sed trials .
2.3. Analysis.
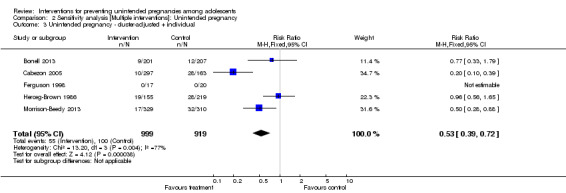
Comparison 2 Sensitivity analysis [Multiple interventions]: Unintended pregnancy, Outcome 3 Unintended pregnancy ‐ cluster‐adjusted + individual .
Table 5 shows trials with insufficient data for inclusion in meta‐analyses. Based on trial authors' conclusions, two of the trials reported results in favour of the intervention groups suggesting that the intervention reduced the risk of unintended pregnancy (Morrison‐Beedy 2013; Smith 1994).
Initiation of sexual intercourse
Four individually randomised trials (Guilamo‐Ramos 2011b; Jemmott 1998Philliber 2002; Villarruel 2006) reporting initiation of intercourse among a mixed gender sample showed no significant difference between participants in the intervention and control groups with respect to time of initiation of sexual intercourse (during the intervention or in the follow up period) (RR 0.99, 95% CI 0.74 to 1.32; 4 studies, 1796 participants, Analysis 1.3).
1.3. Analysis.
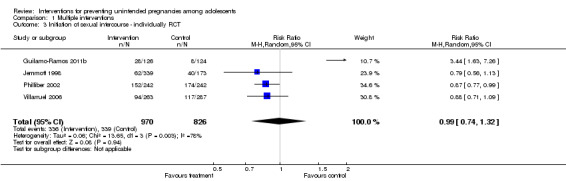
Comparison 1 Multiple interventions, Outcome 3 Initiation of sexual intercourse ‐ individually RCT.
Seven cluster randomised studies (Fawole 1999; Ferguson 1998; Howard 1990; Kirby 1997a; Morberg 1998; O'Donnell 1999; Wight 2002) that merged male and female participants showed no statistically significant difference in effects between intervention and control groups (RR 0.84, 95% CI 0.68 to 1.04; 7 studies, 8608 participants, Analysis 1.4).
1.4. Analysis.
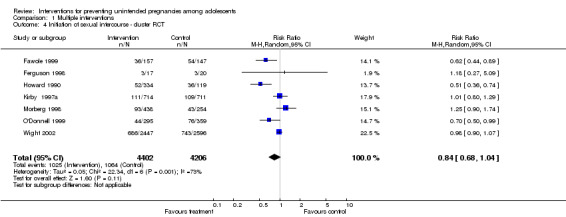
Comparison 1 Multiple interventions, Outcome 4 Initiation of sexual intercourse ‐ cluster RCT.
Sensitivity analysis excluding trials with high attrition rates also showed no statistically significant difference in effects in three individual randomised trials (Guilamo‐Ramos 2011b; Jemmott 1998; Villarruel 2006) (RR: 1.18, 95% Cl 0.67 to 2.09) and four cluster randomised trials (Fawole 1999; Ferguson 1998; Morberg 1998; O'Donnell 1999) (RR 0.84, 95% CI 0.57 to 1.25). Meta‐analysis including cluster‐randomized trials (adjusted for design effects) and individually randomised trials also showed no statistically significant difference in effects between intervention and control groups (RR 0.88, 95% CI 0.74 to 1.05, Analysis 3.3).
3.3. Analysis.
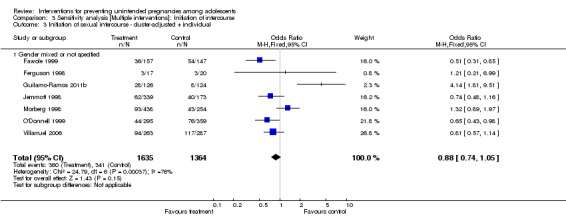
Comparison 3 Sensitivity analysis [Multiple interventions]: Initiation of intercourse, Outcome 3 Initiation of sexual intercourse ‐ cluster‐adjusted + individual.
The summary of results of 8 trials (Basen‐Engquist 2001; Coyle 2004; Coyle 2006; Eisen 1990; Kirby 2004; Markham 2012; Smith 1994; Stephenson 2004) that reported this outcome but had insufficient data to meta‐analyse has been presented in Table 5. One trial (Markham 2012) with mixed gender participants, reported significantly lower risk of initiation of sexual intercourse in the intervention group compared to the control group.Two trials reporting effects among male participants (Coyle 2004; Eisen 1990) concluded that participants who had multiple interventions were less likely to initiate intercourse during the period of follow‐up in comparison to the control arm. One trial (Stephenson 2004) which reported initiation of sexual intercourse in female participants, also showed significant effects in favour of the intervention.
Use of birth control methods
a) Condom use at last sex
Three individually randomised trials (Bonell 2013; Philliber 2002; Shrier 2001) showed no difference between intervention and control groups with respect to condom use at last sex (RR 1.00, 95% CI 0.95 to 1.06; 3 studies, 796 participants, Analysis 1.5)
1.5. Analysis.
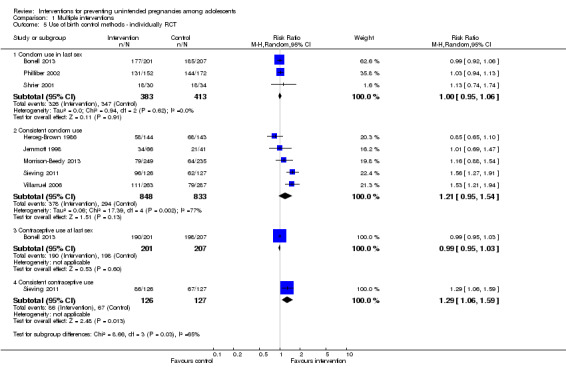
Comparison 1 Multiple interventions, Outcome 5 Use of birth control methods ‐ individually RCT.
Four cluster‐randomised trials (Fawole 1999; Jemmott 2010; Kirby 1997a; Walker 2006) reported condom use at last sex showed no statistically significant differences between intervention and control groups (RR: 1.01, 95% CI 0.93 to 1.09; 4 studies, 2620 participants, Analysis 1.6).
1.6. Analysis.
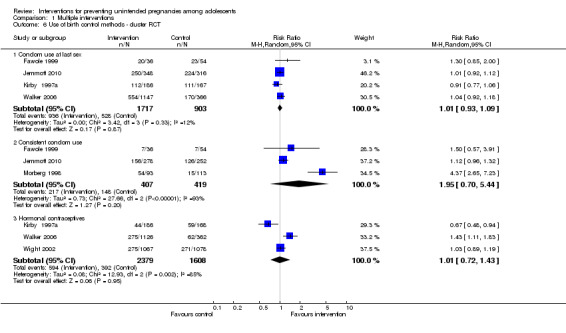
Comparison 1 Multiple interventions, Outcome 6 Use of birth control methods ‐ cluster RCT.
b) Consistent condom use (in prior 90 days and more)
Five individually randomised trials (Herceg‐Brown 1986; Jemmott 1998; Morrison‐Beedy 2013; Sieving 2011; Villarruel 2006) which reported consistent condom use, similarly showed no statistically significant differences between intervention and control groups (RR 1.21, 95% CI 0.95 to 1.54; 5 studies, 1681 participants, Analysis 1.5)
Three cluster‐randomised trials (Ferguson 1998; Jemmott 2010; Morberg 1998) reported consistent condom use in at least the preceding 90 days. There however was no statistically significant difference between intervention and control groups (RR 1.95, 95% CI 0.70 to 5.44; 3 studies, 826 participants, Analysis 1.6). There was also a significantly high level of heterogeneity (I2= 93%).
c) Contraceptive use at last sex
One individually randomised trial (Bonell 2013) reported no significant difference in the risk of contraceptive use at the last sex between intervention and control groups (RR 0.99, 95% CI 0.95 to 1.03; 1 study, 408 participants, Analysis 1.5).
d) Consistent contraceptive use at 24 months
Another individually randomised trial (Sieving 2011) reported consistent contraceptive use up to 24 months post‐intervention. However, there was no significant difference between the intervention and control groups (RR 1.29, 95% CI 1.06 to 1.59; 1 study, 253 participants, Analysis 1.5).
e) Hormonal contraceptive use
Three cluster‐randomised trials (Kirby 1997a; Walker 2006; Wight 2002) which reported hormonal contraceptive use showed no difference between intervention and control groups (RR 1.01, 95% CI 0.72 to 1.43; 3 studies, 3987 participants, I2= 85%, Analysis 1.6)
Sexually Transmitted Diseases (STD)
Two individually randomised controlled trials (Morrison‐Beedy 2013; Shrier 2001) measured STD reporting in the intervention group (61/359) compared with the control group (65/340) (RR 0.89, 95% CI 0.65 to 1.22; 2 studies, 699 participants, Analysis 1.7).
1.7. Analysis.
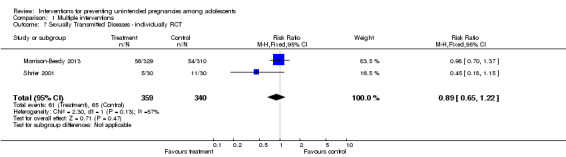
Comparison 1 Multiple interventions, Outcome 7 Sexually Transmitted Diseases ‐ individually RCT.
Two cluster RCTs (Fawole 1999; Kirby 1997b) measured STD reporting in the intervention group (6/205) compared with the control group (8/215) (RR 0.72, 95% Cl 0.26 to 2.02, Analysis 1.8). Neither the individual nor cluster randomised trials showed statistically significant effects.
1.8. Analysis.
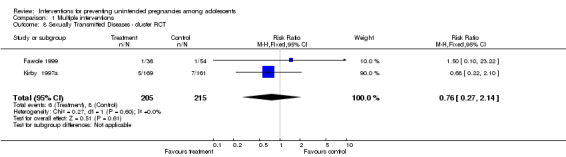
Comparison 1 Multiple interventions, Outcome 8 Sexually Transmitted Diseases ‐ cluster RCT.
Childbirth
One cluster randomised trial (Stephenson 2004) reported that relatively fewer participants in the intervention group (178/2529) than in the control group (237/2247) had experienced childbirth during the period of observation; the difference was statistically significant (RR 0.64, 95% CI 0.52 to 0.79; 1 study, 4776 participants, Analysis 1.9)
1.9. Analysis.
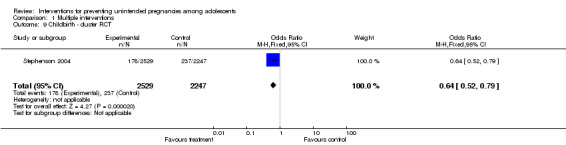
Comparison 1 Multiple interventions, Outcome 9 Childbirth ‐ cluster RCT.
One individually randomised study (Philliber 2002) reported that relatively fewer participants in the intervention group (10/242) than in the control group (15/242) had experienced childbirth during the period of observation; the difference was, however, not statistically significant (RR 0.67, 95% Cl 0.31 to 1.45, 1 study, 484 participants, Analysis 1.10).
1.10. Analysis.
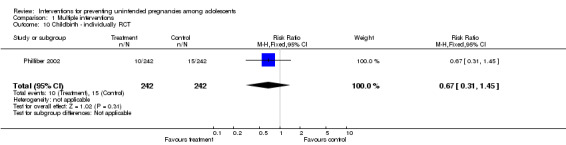
Comparison 1 Multiple interventions, Outcome 10 Childbirth ‐ individually RCT.
Second unintended pregnancy
One study (Black 2006) reported a lower risk of second unintended pregnancy in the intervention group (8/70) compared to the control group; the difference in effect approached statistical significance (19/79) (RR: 0.48, 95% Cl 0.22 to 1.02; 1 study, 149 participants, Analysis 1.11).
1.11. Analysis.
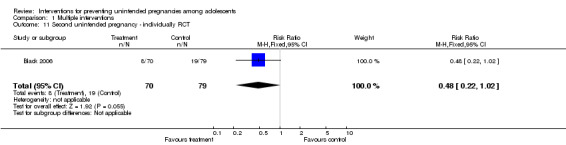
Comparison 1 Multiple interventions, Outcome 11 Second unintended pregnancy ‐ individually RCT.
Abortion
One cluster randomised trial (Stephenson 2004) reported no statistically significant difference in the incidence of abortion between participants in the intervention group and the control group (RR 0.93, 95% CI 0.72 to 1.21; 1 study, 4776 participants, Analysis 1.12)
1.12. Analysis.
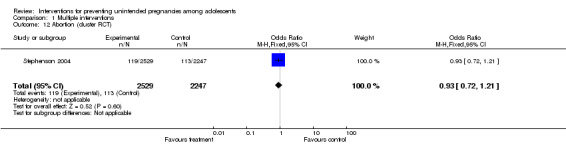
Comparison 1 Multiple interventions, Outcome 12 Abortion (cluster RCT).
EDUCATIONAL INTERVENTIONS
Initiation of sexual intercourse
Two cluster RCTs (Clark 2005; Dilorio 2006) of an educational intervention showed no statistically significant difference in the proportion of participants that initiated sexual intercourse during follow‐up in the intervention group and control (RR 0.95, 95% Cl 0.71 to 1.27, Analysis 4.1).
4.1. Analysis.
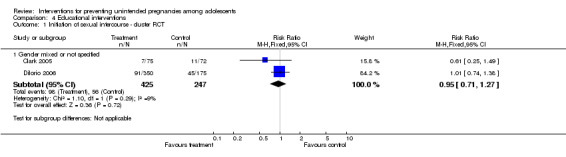
Comparison 4 Educational interventions , Outcome 1 Initiation of sexual intercourse ‐ cluster RCT.
Condom use at last sex
Two cluster RCTs (Borgia 2005, Dilorio 2006) showed that condom use at last sex was statistically significantly higher in the intervention group (258/704) than control group (190/727) (RR 1.18, Cl 1.06 to 1.32, Analysis 4.2).
4.2. Analysis.
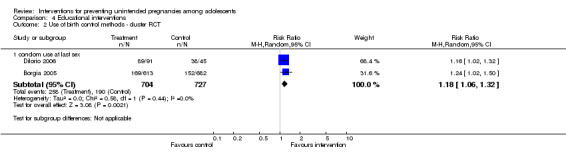
Comparison 4 Educational interventions , Outcome 2 Use of birth control methods ‐ cluster RCT.
Use of contraceptives
One study (Mba 2007) reported a significant increase in the use of contraceptives in the intervention group (35/180) compared to control group (14/180) (RR 2.50, 95% CI 1.39 to 4.48; 1 study, 360 participants, Analysis 4.3).
4.3. Analysis.
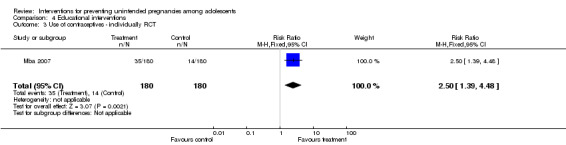
Comparison 4 Educational interventions , Outcome 3 Use of contraceptives ‐ individually RCT.
Changes in knowledge and attitudes about the risk of unintended pregnancies
Only one study (Blake 2001) clearly reported the above outcome by assessing change in knowledge on the risks of pregnancy at first intercourse and found no significant difference between intervention and control groups (see Table 5).
CONTRACEPTIVE‐PROMOTING INTERVENTIONS
Unintended pregnancy
Two individually randomised trials (Raine 2005, Raymond 2006) (3440 participants) showed no statistically significant difference in risk of unintended pregnancy between the intervention group (133/1572) and control (155/1868) (RR 1.01, 95% CI 0.81 to 1.26, Analysis 5.1).
5.1. Analysis.
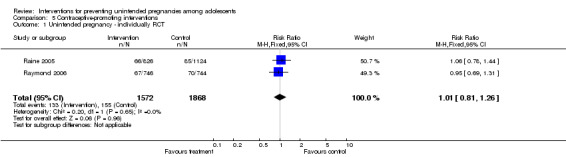
Comparison 5 Contraceptive‐promoting interventions, Outcome 1 Unintended pregnancy ‐ individually RCT.
Initiation of Sexual Intercourse
One cluster RCT (Graham 2002) measured initiation of sexual intercourse. The result showed no statistically significant difference in effect between intervention and control, neither for male participants (RR 1.02, 95% Cl 0.87 to 1.21; 1560 participants) nor female (RR 0.89, 95% Cl 0.76 to 1.04; 1446 participants, Analysis 5.2).
5.2. Analysis.
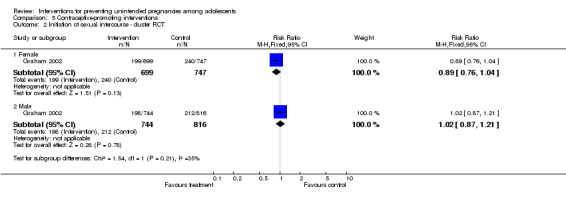
Comparison 5 Contraceptive‐promoting interventions, Outcome 2 Initiation of sexual intercourse ‐ cluster RCT.
Use of birth control
See Analysis 5.3 and Analysis 5.4
5.3. Analysis.
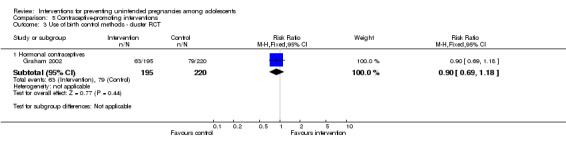
Comparison 5 Contraceptive‐promoting interventions, Outcome 3 Use of birth control methods ‐ cluster RCT.
5.4. Analysis.
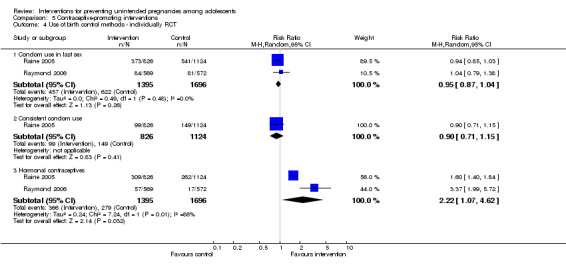
Comparison 5 Contraceptive‐promoting interventions, Outcome 4 Use of birth control methods ‐ individually RCT.
a) Condom use at last sex
Two individual RCTs (Raine 2005, Raymond 2006) of contraceptive‐promoting interventions showed no statistically significant difference in condom use at last sex between intervention group (457/1395) and control group (622/1696) (RR 0.94, 95% Cl 0.87 to 1.04).
b) Consistent condom use
One individual RCT (Raine 2005) measured the consistent use of condoms in sexual intercourse; the result showed no statistically significant difference between intervention group (99/826) and control group (149/1124) (RR 0.90, 95% Cl 0.71 to 1.15).
c) Hormonal contraceptive use
Two individual RCTs (Raine 2005, Raymond 2006) showed that the rate of hormonal contraceptive use was significantly higher in the intervention group (366/1395) than in the control group (279/1696) (RR 2.22, 95% Cl 1.07 to 4.62). The analysis showed a statistically significant heterogeneity (I2 = 86%).
One cluster RCT (Graham 2002) found no statistically significant difference in use of emergency contraceptives between the intervention group (63/195) and control (79/220) (RR 0.90, 95% Cl 0.69 to 1.18, Analysis 5.3).
Sexually Transmitted Diseases (STD)
Two individual RCTs (Raine 2005, Raymond 2006) of contraceptive‐promoting interventions showed no statistically significant difference in risk of sexually transmitted diseases between the intervention group (143/1572) and control group (193/1868) (RR: 0.92, 95% Cl 0.75 to 1.13, Analysis 5.5).
5.5. Analysis.
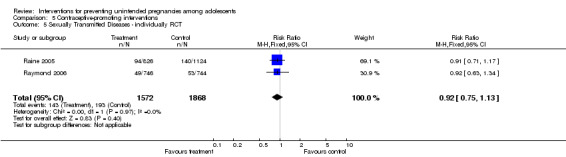
Comparison 5 Contraceptive‐promoting interventions, Outcome 5 Sexually Transmitted Diseases ‐ individually RCT.
Discussion
Summary of main results
Limited information suggests that programmes that involve concurrent application of multiple interventions (educational, skill building and contraception promotion) can reduce rates of unintended pregnancies in adolescents. Reviews done by Kirby 2002c; Manlove 2002; National Research Council (NRC 1987) have also highlighted the need for multiple strategies to address this public health challenge. Sensitivity analyses including trials with lower risk of bias showed that more cases of unintended pregnancy were reported in the control group than those that received multiple preventive interventions. Promoting the use of contraceptive measures alone did not appear to reduce the risk of unintended pregnancy. There was insufficient data to show whether education as a single intervention would reduce the risk of unintended pregnancy.
The possible effects of these preventive interventions on secondary outcomes such as time of initiation of sexual intercourse, risk of sexually transmitted infections and use of contraceptive measures like condoms and pills were not conclusively determined because of insufficient data and variation in methods of reporting.
Overall completeness and applicability of evidence
External validity
Some of the limitations of this review include the relatively small data sets available for the main outcomes of interest, and the likelihood of incomplete reporting of such outcomes as abortion, which have the potential to affect the rate of unintended pregnancy reported.
Furthermore, most of the trials were conducted in high‐income countries, thus this may limit the applicability of the results in middle‐ or low‐income countries.
Another limitation is the small number of studies with a true control group (without any intervention capable of reducing the incidence of unintended pregnancy). Because most of the trial settings already had community‐wide interventions (primarily in schools) aimed at improving adolescent sexual behaviours, it was difficult to find trials that had a control arm that was totally devoid of any form of educational intervention. The situation is likely to be different in low‐income countries, where such interventions may not be as widespread, making it more feasible to set up trials with true control arms.
Evidence in the practice context
The evidence provided in this review shows that concurrent application of preventive interventions such as education, skills‐building and contraception promotion could lower the incidence of unintended pregnancies in adolescents but the fact that most of the trials were conducted in industrialised countries (especially the USA) and among the lower socio‐economic populations, raises issues about applicability. The socio‐cultural context as well as cost implications of these interventions should be considered in efforts to introduce such measures in low‐income countries. Many low‐ and middle‐income countries may lack the infrastructure and resources to successfully implement these interventions. Trials in such resource‐poor settings would be needed to address some of these contextual and location‐specific issues.
Summaries for stakeholders
Application of the findings of this review should be approached with caution given the methodological deficiencies of included trials, the substantial heterogeneity across trials in the ways programmes were delivered and the frequent omission of methodological details and implementation information from primary trial reports.
Quality of the evidence
We assessed the quality of the evidence using the GRADE approach (Schünemann 2011) and have presented it in four ’Summary of findings’ tables (Table 1; Table 2; Table 3; Table 4). We assessed the evidence for the following outcomes: reduction of unintended pregnancy; reduction in the initiation of sexual intercourse; and increase in the use of birth controls (condoms or hormonal contraceptives, or both) for the different groups of interventions.
Unintended Pregnancy
We considered the evidence for a reduction in unintended pregnancies to be moderate quality, and low quality for both the contraceptive‐promoting interventions (downgraded for imprecision) and for multiple interventions (downgraded for risk of bias (ROB), imprecision and inconsistency) (Table 1; Table 3).
Contraceptive‐promoting intervention
The evidence for the following outcomes, condom use at last sex, use of hormonal contraceptives and reduction in sexually transmitted diseases was considered high quality (Table 1).
Educational interventions
Evidence for the reduction in the initiation of intercourse was considered low quality (downgraded for ROB and imprecision); while evidence for use of condom at last sex was considered moderate quality (downgraded for ROB only). (Table 2)
Multiple interventions
Evidence for studies that employed multiple interventions was grouped into individual and cluster randomised controlled trials (Table 3; Table 4). For Individual RCTs, evidence for reduction in initiation of intercourse and condom use at last sex was considered moderate quality (downgraded for ROB only); evidence for consistent use of condoms and reduction in sexually transmitted diseases was considered low quality (downgraded for ROB and inconsistency) and very low quality (downgraded for ROB, inconsistency and imprecision) respectively. Evidence from cluster RCTs was considered moderate quality (downgraded for ROB only) for condom use at last sex, low quality (downgraded for ROB and imprecision) for consistent condom use and reduction in sexually transmitted diseases; and very low quality (downgraded for ROB, imprecision and inconsistency) for reduction in initiation of intercourse and use of hormonal contraception.
Overall, the studies had several important strengths: most had large sample sizes, long‐term follow‐up, described the development of data collection instruments, used techniques to promote the validity of self‐reported data, controlled for baseline differences in statistical analyses, and reported the causes and possible impacts of attrition.
Methodological quality was sometimes difficult to judge due to incomplete reporting of key methodological features and it was often difficult to obtain additional information by contacting the trial authors due to data loss and non‐response. Weaknesses include the underreporting of key methodological features; few of the trials specified the procedures used for assigning participants, or concealed allocation, blinded outcome assessors or separated programme facilitators between the intervention and control groups.
Five studies reported adequate allocation concealment using sealed, opaque envelopes (Diclemente 2004; Jemmott 2010; Raine 2005; Raymond 2006; Philliber 2002 ). The remaining studies did not provide information on concealment of allocation.
Assessor blinding was reported in 11 studies (Black 2006; Bonell 2013; Diclemente 2004; Jemmott 1998; Jemmott 2010; Minnis 2014; Morrison‐Beedy 2013; Raine 2005; Shrier 2001; Wight 2002, ) and not in the remaining 42 studies.
Thirty‐four studies had insufficient or no information on randomisation generation method and used terms such as "assigned at random" or "randomly assigned".
Attrition at last follow‐up
Sixteen studies included more than 90% of randomised participants in the analysis (defined in the review methods as adequate), thirty‐seven had greater than 10% attrition and accounted for less than 90% of randomised participants in the data analysis (inadequate), and two studies did not mention number of participants lost to follow up. The percentage loss to follow up ranged from 0.5% to 48%.
Missing data
Commonly missing data across studies included the number of participants per trial arm at baseline and follow‐up, means and standard deviations for continuous outcomes, percentages for dichotomous outcomes, effect sizes, and attrition analyses.
Unit of analysis problems
Of the thirty‐four trials that used cluster randomisation, 26 controlled for clustering in analyses and eight did not (Aarons 2000; Allen 1997; Cabezon 2005; Fawole 1999; Ferguson 1998, Howard 1990; Kirby 1997a; Morberg 1998). While one study (Kirby 1997a) explained that using individuals as the unit of analysis gave no significant results thus no need for adjusting for clusters. These studies are potentially vulnerable to bias due to incorrect analysis and could result in one or more statistically significant effect occurring by chance.
Limitations of outcome measures:
All outcome data in this review are vulnerable to self‐report bias except for pregnancy and STDs in the following studies: Jemmott 1998; Raine 2005; Raymond 2006. These studies used biological outcomes which are better indicators for pregnancy and STDs. Self‐reported behavioural outcomes unavoidably introduce self‐report bias. Most behavioural outcomes were reported in subgroups and varied greatly such as initiation of intercourse ("last sex", "sex in the last three months", "sex among virgins"). Follow‐up periods also varied greatly. Likewise the use of contraceptives; while some studies used the term "contraceptive", others differentiated it into condom use, hormonal contraceptives, pills. The reporting of sub‐groups also varied. The results of this review highlight the need for a standardised set of outcome measures with explicit definitions, consistent follow‐up times and recall periods to enable comparisons across primary trials. Long‐term follow‐up data are also particularly relevant for studies of unintended pregnancy and sexual behaviour, although these studies tend to lose large numbers of study participants to follow up. One study (Guilamo‐Ramos 2011b), reported "had vaginal intercourse" as one of its outcomes but did not indicate if individuals analysed excluded those who reported any sexual intercourse.
Potential biases in the review process
There are several potential biases in the review process. Our search strategy, though exhaustive may have not been enough to identify all potentially important unpublished data, thus the review is not without publication bias. Several randomised controlled trials that we included did not measure unintended pregnancy which is the primary outcome in this review.
While assessing trials for inclusion, we might have omitted trials that aimed at preventing unintended pregnancy as they may not have included any of the search terms in their title or abstract. We hope to correct this in future updates.
Another source of bias is our inability to obtain relevant missing data, including methodological characteristics and outcome data leading to the exclusion of a number of trials from the meta‐analysis. Twenty studies were included in the meta‐analysis, of which the majority had various methodological limitations capable of increasing the risk of bias and definitely compromising the strength of evidence.
We encountered some difficulty finding a reliable intra‐class correlation coefficient (ICC) when computing the design effect for cluster randomised trials. Using the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011c), we were able to run a sensitivity analysis for some of the data that provided enough information to calculate average cluster size using a range of possible ICC values. This could have affected the significance of results for isolated pair‐wise comparisons in the direction of insignificance.
Agreements and disagreements with other studies or reviews
Evidence about the prevention of unintended pregnancy in adolescence differed from a previous systematic review carried out (DiCenso 2002) as this reported that the interventions had no effect on the incidence of unintended pregnancy. The review did not include the recent trials, which reported a reduction in the incidence of unintended pregnancy in the intervention group (Cabezon 2005; Philliber 2002). Outcomes such as the initiation of sexual intercourse and contraceptive use showed no significant difference between intervention and control irrespective of intervention, a finding consistent with the previous review.
Authors' conclusions
Implications for practice.
The results of this review suggest that the concurrent use of interventions such as education, skills‐building and contraception promotion reduces the risk of unintended pregnancy in adolescents but offers little evidence about the effect of each of these interventions offered alone. Overall, the evidence remains inconclusive, and could not be the basis for recommending the use or discontinuation of any of these interventions where they are already in use.
Implications for research.
The trials included in this review reported outcomes in different ways and were largely based in industrialised countries. There is a need to develop a uniform approach to reporting outcomes in these types of trials to make for comparability across studies and geographical context. More trials need to be conducted in low income countries to provide a balance of evidence with regard to the obvious disparities in socio‐cultural and economic situations.
What's new
| Date | Event | Description |
|---|---|---|
| 23 November 2015 | New search has been performed | A search of the Cochrane Fertility Regulation Specialised trial register, CENTRAL (The Cochrane Library) and other electronic resources identified 41 potentially eligible trials. Twelve of these trials were included in the updated review. |
| 23 November 2015 | New citation required but conclusions have not changed | New included trials added to meta‐analysis and minor changes made throughout the review |
History
Protocol first published: Issue 2, 2005 Review first published: Issue 4, 2009
| Date | Event | Description |
|---|---|---|
| 21 July 2008 | Amended | converted to new review format |
Acknowledgements
The support of the Australasian Cochrane Centre in providing the grant for this review is gratefully acknowledged. Professor Alba DiCenso is gratefully acknowledged for providing technical guidance.
Appendices
Appendix 1. Search Strategy
#1explode CONTRACEPTION
#2CONTRACEPTION‐BEHAVIOR
#3contracept*
#4adolescent
#5teenage
#6teenager
#7teens
#8explode FAMILY‐PLANNING
#9family planning or planned parenthood or birth control
#10birth regulat* or population regulat* or fertility regulat* or birth spacing
#11population control or fertility control or reproduct* control
#12pregnan* near (prevent* or interrupt* or terminat*)
#13birth control clinic
#14sex education
#15primary prevention
#16school
#17POPULATION‐CONTROL
#18FAMILY‐PLANNING‐POLICY
#19explode CONTRACEPTIVE‐DEVICES
#20intrauterine device* or intra‐uterine device* or IUD* or TCu380a or CuT‐200 or Gynefix
#21barrier method* or condom* or vaginal sponge* or cervical cap*
#22explode REPRODUCTIVE‐CONTROL‐AGENTS
#23ovulat* near (suppress* or inhibit* or prevent*)
#24ABORTION‐APPLICANTS
#25explode ABORTION‐INDUCED
#26abortion or abortifacient*or termination or morning after pill or RU‐486 or Yuzpe
#27explode STERILIZATION‐SEXUAL
#28(female or woman or women or male or man or men) near sterili*
#29vasectom*
#30SEXUAL‐ABSTINENCE
#31periodic* abstinen* or sexual* abstinen* or coitus interruptus. We included the following search terms to identify additional reports on educational interventions that the above strategy may omit:
#32 (counsel* or debrief* or educat* or teach*). We scrutinized college studies to identify groups that fulfilled the review inclusion criteria.
Data and analyses
Comparison 1. Multiple interventions.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Unintended pregnancy [individually randomised trials] | 4 | 1905 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.50, 0.87] |
| 2 Unintended pregnancy [cluster‐randomised trials] | 5 | 3149 | Risk Ratio (M‐H, Random, 95% CI) | 0.50 [0.23, 1.09] |
| 3 Initiation of sexual intercourse ‐ individually RCT | 4 | 1796 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.74, 1.32] |
| 4 Initiation of sexual intercourse ‐ cluster RCT | 7 | 8608 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.68, 1.04] |
| 5 Use of birth control methods ‐ individually RCT | 8 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.1 Condom use in last sex | 3 | 796 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.95, 1.06] |
| 5.2 Consistent condom use | 5 | 1681 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.95, 1.54] |
| 5.3 Contraceptive use at last sex | 1 | 408 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.95, 1.03] |
| 5.4 Consistent contraceptive use | 1 | 253 | Risk Ratio (M‐H, Random, 95% CI) | 1.29 [1.06, 1.59] |
| 6 Use of birth control methods ‐ cluster RCT | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 6.1 Condom use at last sex | 4 | 2620 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.93, 1.09] |
| 6.2 Consistent condom use | 3 | 826 | Risk Ratio (M‐H, Random, 95% CI) | 1.95 [0.70, 5.44] |
| 6.3 Hormonal contraceptives | 3 | 3987 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.72, 1.43] |
| 7 Sexually Transmitted Diseases ‐ individually RCT | 2 | 699 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.65, 1.22] |
| 8 Sexually Transmitted Diseases ‐ cluster RCT | 2 | 420 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.27, 2.14] |
| 9 Childbirth ‐ cluster RCT | 1 | 4776 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.52, 0.79] |
| 10 Childbirth ‐ individually RCT | 1 | 484 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.31, 1.45] |
| 11 Second unintended pregnancy ‐ individually RCT | 1 | 149 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.22, 1.02] |
| 12 Abortion (cluster RCT) | 1 | 4776 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.72, 1.21] |
Comparison 2. Sensitivity analysis [Multiple interventions]: Unintended pregnancy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Unintended pregnancy ‐ cluster‐randomi sed trials | 2 | 497 | Risk Ratio (M‐H, Random, 95% CI) | 0.20 [0.10, 0.39] |
| 2 Unintended pregnancy ‐ individually‐randomi sed trials | 3 | 1421 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.46, 1.00] |
| 3 Unintended pregnancy ‐ cluster‐adjusted + individual | 5 | 1918 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.39, 0.72] |
2.2. Analysis.
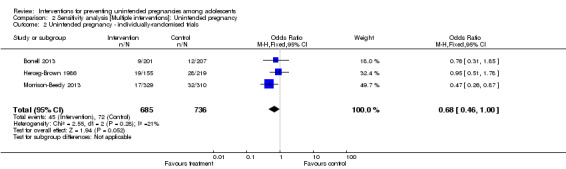
Comparison 2 Sensitivity analysis [Multiple interventions]: Unintended pregnancy, Outcome 2 Unintended pregnancy ‐ individually‐randomi sed trials .
Comparison 3. Sensitivity analysis [Multiple interventions]: Initiation of intercourse.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Initiation of sexual intercourse ‐ individually RCT | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 Gender mixed or not specified | 3 | 1312 | Risk Ratio (M‐H, Random, 95% CI) | 1.18 [0.67, 2.09] |
| 2 Initiation of sexual intercourse ‐ cluster RCT | 4 | 1687 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.57, 1.25] |
| 2.1 Gender mixed or not specified | 4 | 1687 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.57, 1.25] |
| 3 Initiation of sexual intercourse ‐ cluster‐adjusted + individual | 7 | 2999 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.74, 1.05] |
| 3.1 Gender mixed or not specified | 7 | 2999 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.74, 1.05] |
3.1. Analysis.
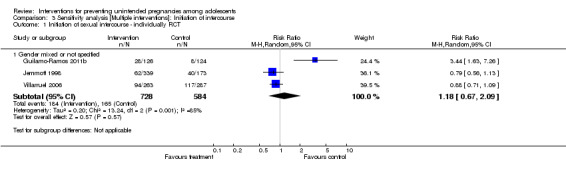
Comparison 3 Sensitivity analysis [Multiple interventions]: Initiation of intercourse, Outcome 1 Initiation of sexual intercourse ‐ individually RCT.
3.2. Analysis.
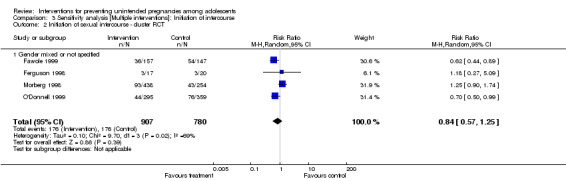
Comparison 3 Sensitivity analysis [Multiple interventions]: Initiation of intercourse, Outcome 2 Initiation of sexual intercourse ‐ cluster RCT.
Comparison 4. Educational interventions.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Initiation of sexual intercourse ‐ cluster RCT | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Gender mixed or not specified | 2 | 672 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.71, 1.27] |
| 2 Use of birth control methods ‐ cluster RCT | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 condom use at last sex | 2 | 1431 | Risk Ratio (M‐H, Random, 95% CI) | 1.18 [1.06, 1.32] |
| 3 Use of contraceptives ‐ individually RCT | 1 | 360 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.5 [1.39, 4.48] |
Comparison 5. Contraceptive‐promoting interventions.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Unintended pregnancy ‐ individually RCT | 2 | 3440 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.81, 1.26] |
| 2 Initiation of sexual intercourse ‐ cluster RCT | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Female | 1 | 1446 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.76, 1.04] |
| 2.2 Male | 1 | 1560 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.87, 1.21] |
| 3 Use of birth control methods ‐ cluster RCT | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 Hormonal contraceptives | 1 | 415 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.69, 1.18] |
| 4 Use of birth control methods ‐ individually RCT | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 Condom use in last sex | 2 | 3091 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.87, 1.04] |
| 4.2 Consistent condom use | 1 | 1950 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.71, 1.15] |
| 4.3 Hormonal contraceptives | 2 | 3091 | Risk Ratio (M‐H, Random, 95% CI) | 2.22 [1.07, 4.62] |
| 5 Sexually Transmitted Diseases ‐ individually RCT | 2 | 3440 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.75, 1.13] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Aarons 2000.
| Methods | Cluster‐randomis ed controlled study; method of generating allocation sequence not mentioned in the paper Unit of randomis ation: schools | |
| Participants | 582 students who enrolled in the 7th grade at the beginning of the study; enrolled in the 8th grade at the beginning of the 1996/1997 session; capable of reading and comprehending the questionnaire in English or Spanish; not truant or suspended during the trial; mean age of 12.8 years; 52% female and 48% male; 84% African American, 13% Hispanic, 2% other, low socio‐economic status | |
| Interventions | Intervention: t hree 45‐ minute reproductive health education classes by health professionals, five 45‐ minute sessions on postponing sexual involvement by peer leaders in 10th and 11th grades, health risk assessment questionnaire Control: conventional education programme |
|
| Outcomes | Initiation of intercourse (age at initiation), use of birth control/condoms at last sex | |
| Notes | Duration of follow up: 15 months. Loss to follow up: 19% |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method used for allocation sequence generation not provided |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were reported |
| Other bias | Unclear risk | Did not control for cluster randomi sation during the analysis |
Allen 1997.
| Methods | Randomis ed controlled trial. Randomis ation was done at two levels; student (75% of sample) by picking names out of a hat or choosing every other name on an alphabetis ed list, and classroom (25% of sample) by a coin toss | |
| Participants | 695 students from 25 sites in the United States, 9th grade to 12th grade, mean age of 15.8 years, 85% female and 15% male; 67% African American, 19% White, 11% Hispanic and 3% other | |
| Interventions | Intervention: 20 hours per year of supervised community volunteer services and one hour per week of classroom‐ based discussion of service experiences, future life options, developmental tasks of adolescents and sex education Control: standard curriculum offerings |
|
| Outcomes | Unintended pregnancy (women only) | |
| Notes | Duration of follow up: nine months Loss to follow up: 7.0% lost to follow up (5.3% among experimental students and 8.4% among control students) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Picking names out of a hat (for individual) or coin toss (for classrooms) |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information provided on this domain |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Three sites were excluded from analysis. Higher attrition rate in the control groups. There were some differences between students lost and those retained in that students lost were more likely to have had or caused a prior pregnancy, been suspended, be younger and be male. |
| Selective reporting (reporting bias) | Low risk | Pre‐specifed outcomes were reported |
| Other bias | Low risk | The study appears to be free from other bias |
Baird 2010.
| Methods | Cluster ‐ randomis ed controlled trial; randomis ation was done using Enumeration Areas (EAs). | |
| Participants | Young women aged 12 years to 22 years and not married | |
| Interventions | Intervention: conditional cash transfer (CCT) as an incentive for school girls and young women to stay or return to school Control: no CCT provided |
|
| Outcomes | Pregnancy, sexual behaviour (onset of sexual activity, number of sexual partners in the past 12 months, condom use, frequency of sexual activity) | |
| Notes | Duration of follow up: 12 months | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Information on this domain was not provided |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rate was low and balanced across treatment and control groups |
| Selective reporting (reporting bias) | Unclear risk | Outcomes to be measured were not clearly listed in the methods |
| Other bias | Unclear risk | Baseline differences between dropouts and school girls (dropouts were older, less literate and more likely to have started childbearing) |
Basen‐Engquist 2001.
| Methods | Cluster‐randomis ed controlled study. Method of generating allocation sequence not mentioned in the paper Unit of randomis ation: schools |
|
| Participants | 7614, 8319 and 9489 9 (at baseline, 19 and 31 months); grade 9 to 12 students in schools in California and Texas, 47% male, 53% female, 18% African American, 17% Asian, 33% Hispanic, 27% White, 5% other | |
| Interventions | Intervention: 20 sessions of health education, skills‐ building, contraceptive education, social norms and peer education, parent education, community linkages Control: standard knowledge‐ based curriculum on contraception, HIV and other STDs |
|
| Outcomes | Initiation of intercourse, contraception use | |
| Notes | Duration of follow up: 31 months Loss to follow up: not clear |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation sequence generation not stated |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information on attrition/exclusion to permit judgement as number of participants in the study increased with each follow up. |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were reported |
| Other bias | Unclear risk | The sampling methods for including students not clear |
Black 2006.
| Methods | Randomis ed controlled study. Method of allocation sequence not mentioned. Unit of randomis ation: individual | |
| Participants | 181 adolescent mothers in urban hospitals who were living with their mother, 13.5 years to 17.9 years at delivery, first‐time delivery, Black, no history of drugs, infants should be 37 weeks and birth weight of > 2500 g with no congenital problems, chronic illnesses, or disabilities. | |
| Interventions | Intervention: home mentoring programme (home visits every week until infant's first birthday, approximately 19 visits) Control: no intervention |
|
| Outcomes | Second unintended pregnancy | |
| Notes | Duration of follow up: 24 months Loss to follow up: 18% Evaluators were blinded to intervention status |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation sequence generation not stated |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Evaluators only |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Only participants with both baseline and 24‐months' data were included in the analysis. |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were reported |
| Other bias | Low risk | The study appears to be free from other bias |
Blake 2001.
| Methods | Cluster‐randomis ed controlled study. Quarterly marking period within schools was used to generate allocation sequence Unit of randomis ation: schools |
|
| Participants | 351 8th grade students in Rochester, New York living in middle class suburban communities, 48% female and 52% male. 85% were white and non‐Hispanic. | |
| Interventions | Intervention: enhanced intervention; five one‐hour sessions on standard school‐ based curriculum ( health education; skills‐ building; abstinence; communication skills) plus five parent‐child homework assignments on sexuality and sexual behaviour led by trained youth leaders Control: standard school‐ based curriculum only |
|
| Outcomes | Initiation of intercourse, knowledge on the risk of pregnancy | |
| Notes | Duration of follow up: seven weeks. No mention of loss to follow up | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quarterly marking period within schools |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Only those who completed pre‐test and post‐test questionnaires were analys ed at baseline and end of the study. Analysis adjusted for clusters |
| Selective reporting (reporting bias) | Low risk | Pre‐stated outcomes were reported |
| Other bias | High risk | Selection bias as the proportion of students who had completed no assignments was higher among Black and Hi spanic adolescents than among non‐Hispanic White students (43% vs 18%; P < 0.05); higher among male than female students (27% vs 9%; P < 0.01) and was higher among adolescents who reported recent sexual intercourse than among those who did not (63% vs 17%; P < 0.001) |
Bonell 2013.
| Methods | Matched‐pair individual‐allocation randomi sed trial. | |
| Participants | Girls aged 13 years to 15 years | |
| Interventions | Intervention: weekly three‐hour sessions in pre‐school nuseries to develop awareness of the responsibility involved in parenting, self‐awareness and confidence to reduce risk of teenage pregnancy, other issues addressed include self‐esteem and sense of control, emotional literacy and social skills, teenage sex, sexual health and consequences of unplanned pregnancy Control: not stated |
|
| Outcomes | Last sex without contraception in the last three months, more than one episode of sex without contraception in the last three months, new pregnancy since baseline, last sex without condom in the last three months, more than one episode of sex without condom in the last three months | |
| Notes | Duration of follow up: 22 weeks and 12 months Loss to follow up; 9% |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐ generated random number |
| Allocation concealment (selection bias) | Unclear risk | Children: Our Ultimate Investment (COUI) and school staff were blinded to allocation; however, neither intervention teachers, nor girls nor analyst were blinded to allocation status |
| Blinding (performance bias and detection bias) All outcomes | High risk | Teachers and girls were not blinded to allocation status |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Few number of participants lost to follow up; intention‐ to‐ treat analysis was employed |
| Selective reporting (reporting bias) | High risk | Pregnancy was based on self‐reporting |
| Other bias | Unclear risk | The study appears to be free from other bias |
Borgia 2005.
| Methods | Cluster‐randomis ed controlled study. Method of allocation concealment not mentioned. Unit of randomization: schools |
|
| Participants | 1295 students from 18 high schools in Rome, 51% male, 49% female, mean age 18.3 years | |
| Interventions | Intervention: HIV/AIDS education and skills‐ building by peer Control: same intervention by teachers |
|
| Outcomes | Consistent condom use | |
| Notes | Duration of follow up: 5 months Loss to follow up: 20% for peer‐led group and 27% teacher‐led group |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation sequence generation not stated |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Trial authors stated they used an intention‐to‐treat analysis, whereby classes which did not perform the interventions were included in the outcome evaluation. Analysis adjusted for clusters |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
Cabezon 2005.
| Methods | Cluster‐randomis ed controlled trial. Classrooms were randomised by blindly, taking letters of the class from a bag (simple balloting) Unit of randomis ation: classrooms |
|
| Participants | 1259 9th grade female students in San Bernardo, Chile, aged 15 years to 16 years, White Hispanic, who had initiated high school in 1997 and 1998. | |
| Interventions | Intervention: one 45‐ minute class per week for a year on health education, contraceptive education, skills‐ building and abstinence Control: no intervention |
|
| Outcomes | Unintended pregnancy | |
| Notes | Duration of follow up: 4 years Loss to follow up: 19% |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Simple balloting (blindly taking letters from a bag) |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Per‐ protocol analysis was carried out but missing outcome data balanced in numbers across intervention groups with similar reasons for missing data across groups (change of residence and financial problems) |
| Selective reporting (reporting bias) | Low risk | Stated outcomes were measured |
| Other bias | Low risk | The study appears to be free from other bias |
Clark 2005.
| Methods | Cluster‐randomis ed controlled study. Method of allocation sequence not mentioned Unit of randomis ation: class |
|
| Participants | 211 African American 7th grade students, 11 years to 14 years of age, 55% male, 45% female, low income | |
| Interventions | Intervention: 10 sessions (once or twice per week for six weeks) on skills‐ building and career mentoring Control: standard health curriculum |
|
| Outcomes | Initiation of intercourse | |
| Notes | Duration of follow up: 1 year Loss to follow up: 26% |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation sequence generation not stated |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Only participant, the provided baseline, and end of study information were included in the one‐ year follow‐ up analysis |
| Selective reporting (reporting bias) | Low risk | Stated outcome reported |
| Other bias | Unclear risk | The study appears to be free from other sources of bias |
Coyle 1999.
| Methods | Cluster‐randomis ed controlled study. Method of allocation sequence not mentioned in this study Unit of randomis ation: schools |
|
| Participants | 3869 9th grade students from 20 urban high schools in Texas and California, mean age 15 years, 53% female and 47% male; 31% White, 27% Hispanic, 18% Asian or Pacific Islanders, 16% African‐American, < 1% African Indian, 7% other | |
| Interventions | Intervention: 20 sessions on health education, skills‐ building, contraceptive education, parent education, community linkages Control: standard knowledge‐ based HIV‐ prevention curriculum |
|
| Outcomes | Initiation of intercourse, use of contraceptive at last sex | |
| Notes | Duration of follow up: 7 months Loss to follow up: 3% |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Whereas only those with data at baseline and at follow up were included in the analysis, there were no differences in the sexual behaviours between those lost to follow up and those who remained in the study across groups. |
| Selective reporting (reporting bias) | Low risk | Stated outcomes reported |
| Other bias | Low risk | Appears to be free from other bias |
Coyle 2004.
| Methods | Randomis ed controlled study. Method of generating allocation sequence not mentioned in the paper Unit of randomis ation: schools |
|
| Participants | 2829 6th grade students with an average age of 11.5 years from 19 schools in Northern California; 50% female and 50% male; 5.2% African American, 15.9% Asian, 59.3% Hispanic 16.5% White and 3.1% Other. | |
| Interventions | Intervention: 20‐ session curriculum ( five lessons in 6th grade on skills‐ building in non‐sexual situations, eight lessons in 7th grade on determining personal limits in intercourse, understanding consequences of unplanned sexual intercourse (including pregnancy and STD), skills‐ building, seven lessons in 8th grade on contraception education, HIV‐infected speaker and refusal skills in dating) Control: standard curriculum |
|
| Outcomes | Initiation of intercourse | |
| Notes | Duration of follow up: 36 months; lost to follow up: 36% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation sequence generation not stated |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High attrition rate among participants |
| Selective reporting (reporting bias) | Low risk | Pre‐stated outcomes reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
Coyle 2006.
| Methods | Cluster‐randomi sed controlled study. Method of generation of allocation was done using restricted randomi sation into matched sets. Unit of randomi sation: schools |
|
| Participants | 988 students, 14 years to 18 years or older, in community day schools located in four urban counties in Northern California, 63% male, 37% female, 27% African American, 15% Asian American, 30% Hispanic, 12% White, 16% other | |
| Interventions | Intervention: 14 sessions (26 hrs) on HIV/STDs/ pregnancy education, skills‐ building, risks related to sexual behaviour, contraception education and service learning activities ( five visits to volunteer sites) Control: usual curriculum |
|
| Outcomes | Unintended pregnancy, initiation of intercourse, use of contraceptives and condoms at last sex | |
| Notes | Duration of follow up: 18 months Loss to follow up: 58% |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Restricted randomis ation into matched set |
| Allocation concealment (selection bias) | Unclear risk | No information provided on this domain |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All students were included in the analysis regardless of programme dose. No statistically significant difference was found in the rates of attrition across groups |
| Selective reporting (reporting bias) | Low risk | All expected/stated outcomes reported |
| Other bias | Low risk | The study seems to be free from other bias |
Diclemente 2004.
| Methods | Randomis ed controlled study. Table of random numbers was used to generate allocation sequence. Unit of randomi sation: individual | |
| Participants | 522 female participants between the ages of 14 years to 18 years in four community health agencies in southern United States, African American, reporting vaginal intercourse in the preceding six months. | |
| Interventions | Intervention: four‐hour interactive group sessions on ethnic and gender pride, health/HIV education, skills‐ building and contraception education Control: four‐hour interactive group sessions on general health promotion condition (exercise and nutrition) |
|
| Outcomes | Unintended pregnancy, consistent condom use and sexually transmitted disease | |
| Notes | Duration of follow up: 12 months. Loss to follow up: 12% (12.7% for intervention and 11.1% for the control). Assessors were blinded to participants' condition assignments. Allocation concealed in opaque envelopes | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Table of random numbers |
| Allocation concealment (selection bias) | Low risk | Use of sealed opaque envelopes |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Assessors were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Participants were analys ed in their groups irrespective of number of sessions attended. Missing outcome data balanced in numbers with similar reasons for missing data across groups |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
Dilorio 2006.
| Methods | Randomis ed controlled study. Computer‐generated random numbers used to generate allocation sequence. Unit of randomi sation: sites | |
| Participants | 582 adolescents from a community‐ based organi sation and their mothers, 11 years to 14 years, 60% male, 40% female, 98% African American | |
| Interventions | Intervention 1: seven sessions ( two hours) over 14 weeks ( four sessions for mother and adolescents together) on HIV education, communication skills, take‐ home activities and sexual decision making, consequences of early sexual intercourse Intervention 2: stress reduction exercise and specific type of at‐risk behaviours including early sexual intercourse, take‐ home assignments and community service (mothers and adolescents attended the first and last sessions together) Control: mothers and adolescents had a one‐hour HIV prevention session |
|
| Outcomes | Condom use at last sex among participants who have ever had sex | |
| Notes | Duration of follow up: 24months. Loss to follow up: 10% |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Trial authors stated the use of intention‐ to‐ treat analysis; for the use of condoms, only respondents who indicated being sexually active were included in the analysis |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
Dilorio 2007.
| Methods | Randomis ed controlled study. Method for generating allocation sequence not mentioned in the paper Unit of randomi sation: sites |
|
| Participants | 277 adolescent boys from seven sites in Atlanta, 11 years to 14 years, 96% African American | |
| Interventions | Intervention: seven two‐hour sessions, 6th session for fathers of participants only, and the last session for both on communication, parental monitoring and relationship with peers, HIV/AIDS education Control: seven sessions on nutrition and exercise |
|
| Outcomes | Ever had sex without a condom among participants who have ever had sex Ever had sex among all participants | |
| Notes | Duration of follow up: 12 months Loss to follow up: 20% |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method on allocation sequence generation not stated |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intent‐to‐treat analysis carried out. |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
Downs 2004.
| Methods | Randomis ed controlled study. Table of random numbers was used to generate the allocation sequence. Unit of randomis ation: individuals | |
| Participants | 300 female part icipants from four urban Pittsburgh area healthcare sites, who were aged 14 years to 18 years and had reported heterosexual vaginal sexual activity in the previous six months, 75% were African American, 15% Whites and 10% other or mixed race | |
| Interventions | Intervention: interactive video intervention on reproductive health/STD education, skills‐ building and contraceptive education delivered for 30 minutes at baseline and 15 minutes on each follow up visit Control 1: content‐matched control (same intervention in a book form) Control 2: topic‐matched control (same intervention using commercially available brochures) |
|
| Outcomes | Unintended pregnancy, use of condoms, sexually transmitted disease | |
| Notes | Duration of follow up: 6 months Loss to follow up: 14% Individuals were randomised to one of the three groups ( interactive video intervention, content‐matched control and topic‐matched control) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Table of random numbers |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Only participants who provided data at six months were included in the analysis |
| Selective reporting (reporting bias) | High risk | Pre‐specifed outcomes reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
Eisen 1990.
| Methods | Randomis ed controlled multicentre study. Method used to generate allocation sequence not mentioned in the paper Unit of randomi sation: individual and classroom |
|
| Participants | 1444 8th to 9th grade students from six family planning agencies and one school in Texas and California; mean age 15.5 years; 52% female, 48% male; 15% White, 24% African‐American, 53% Hispanic and 8% Asian | |
| Interventions | Intervention: 12 hours to 15 hours on health education (reproductive biology), skills‐ building, contraceptive/STD education Control: usual sex education programmes which varied among sites |
|
| Outcomes | Initiation of intercourse, consistent use of contraceptives | |
| Notes | Duration of follow up: one year Loss to follow up: 39% Randomis ation was done individually or by classroom units (71% by classroom and 29% by individual) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation sequence generation not stated |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to assess this domain |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
Fawole 1999.
| Methods | Cluster‐randomis ed controlled trial. Method used to generate allocation not mentioned in the paper. Unit of randomi sation: classrooms | |
| Participants | 450 students from 11 mixed‐sex public schools in Ibadan, Nigeria; mostly Yoruba; 55.2% female, 44.9% male. Low socioeconomic status | |
| Interventions | Intervention: six weekly (each lasted between two hours and six hours) of AIDS/HIV education, health education and contraceptive education Control: standard curriculum |
|
| Outcomes | Initiation of intercourse, use of condoms at last sex, consistent use of condom, sexually transmitted disease | |
| Notes | Duration of follow up: 6 months Loss to follow up: 3.8% |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation sequence generation not stated |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Participants lost to follow up were less than 5% of the total participants included in the study |
| Selective reporting (reporting bias) | Low risk | all pre‐specified outcomes were reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
Ferguson 1998.
| Methods | Cluster‐randomis ed controlled study. Coin toss technique was used to generate allocation sequence Unit of randomis ation: neighbourhood | |
| Participants | 63 female African American students aged 12 years to 16 years who completed the Camp Horizon Adolescent Pregnancy Prevention Program, residing in one of the four public housing developments in Charlottesville, Virginia, not currently pregnant, had never given birth, 5th grade to 10th grade, low income | |
| Interventions | Intervention: two hours per week for eight weeks on health education, skills ‐building, contraceptive education, abstinence, ethnic/cultural values, family options, career counselling by peer counsellors Control: same interventions taught by usual adult staff | |
| Outcomes | Unintended pregnancy, initiation of intercourse, use of contraceptive at last sex | |
| Notes | Duration of follow up: 3 months. Loss to follow up: 17% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Tossing a coin |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Imbalance in numbers los t to follow up across intervention groups and reasons not stated. Per‐protocol analysis done with substantial departure from one of the groups |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were reported |
| Other bias | Unclear risk | Baseline differences not reported |
Graham 2002.
| Methods | Cluster‐randomi sed controlled study. Computer‐ generated random numbers used to generate allocation sequence. Unit of randomis ation: schools | |
| Participants | 3794 adolescents from secondary schools in Avon, UK , 14 years to 15 years, 52% male, 48% female | |
| Interventions | Intervention: contraception (emergency contraceptives) education Control: usual sex education |
|
| Outcomes | Use of contraceptives, initiation of intercourse | |
| Notes | Duration of follow up: 6 months Loss to follow up: 18% |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐ generated random numbers |
| Allocation concealment (selection bias) | Unclear risk | No information provided on this domain |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition rate > 10% |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
Guilamo‐Ramos 2011b.
| Methods | Randomis ed controlled trial. Dyads (mothers and their adolescents) were randomly assigned. Method of randomis ation was not stated | |
| Participants | 2016 adolescents aged 11 years to 14 years, either African American or Hispanic, and accompanied to the clinic by a resident mother | |
| Interventions | Intervention: mothers met with a social work interventionist for 30 minutes and were then given a packet containing reference materials and family activities (teaching parent effective communication and parenting strategies for reducing sexual risk, communication aids) to implement with their daughter at home. They also received two booster calls as a reminder to implement materials. Control: mothers met with their adolescent's healthcare provider only at the clinic |
|
| Outcomes | Vaginal sexual intercourse, frequency of sexual intercourse in the past 30 days and oral sex | |
| Notes | Duration of follow up: 9 months loss to follow up: 5.4% |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Information on this domain was not provided |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | High retention rate (98.6%) |
| Selective reporting (reporting bias) | Low risk | Reported stated outcome |
| Other bias | Unclear risk | There was no way of assessing if mothers did implement the intervention at home |
Henderson 2007.
| Methods | Cluster‐randomis ed controlled study. Method used to generate allocation sequence not mentioned in the paper. Unit of randomis ation: schools | |
| Participants | 4196 female students in secondary schools in Scotland, 13 years to 15 years, | |
| Interventions | Intervention: SHARE (20 session package: 10 for 3rd year and 10 for 4th years of secondary school respectively) on health/sex education, skills‐ building, contraceptive education primarily through the use of interactive video. Control: conventional sex education |
|
| Outcomes | Childbirth and abortion | |
| Notes | Duration of follow up: 4.5 years Loss to follow up: 0.5% One of the control schools demonstrated how to handle condoms (one of the lesson included in the intervention group). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Information on this domain was not provided |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Minimal participants lost to follow up (0.5%) |
| Selective reporting (reporting bias) | Low risk | Primary outcomes reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
Herceg‐Brown 1986.
| Methods | Randomis ed controlled study. Method used to generate allocation sequence was not mentioned in the paper. Unit of randomis ation:i Individual | |
| Participants | 417 female adolescents aged 12 years to 17 years from nine family planning clinics in Philadelphia, making their first visit to the clinics, residing in the area and with a family member. 53% African American, 47% White | |
| Interventions | Intervention 1: Family Support Group ( regular clinic services plus 50 minutes of family or individualis ed counselling services on sex and contraceptive education for six weeks) Intervention 2: Periodic Support Group ( regular clinic services plus staff supports through two to six telephone calls four to six weeks after initial clinic visit, to monitor teenage adjustment to the contraceptive received at the clinic) Control Group A and B: regular clinic services |
|
| Outcomes | Unintended pregnancy and consistent use of contraceptives | |
| Notes | Duration of follow up: 15 months. Loss to follow up: 14% |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Allocation sequence generation not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) All outcomes | High risk | The number of people assessed in each group was not clearly stated |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes were reported |
| Other bias | Unclear risk | High rate of non‐compliance among participants randomis ed to the intervention |
Howard 1990.
| Methods | Cluster‐randomi sed controlled study. Method used to generate allocation sequence not mentioned in the paper Unit of randomis ation: schools | |
| Participants | 536 low‐ income minority students from 53 schools in Atlanta, 99% Black, 8th grade to 9th grade | |
| Interventions | Intervention: five sessions on health/STD education, skills‐ building, contraceptive education (first four sessions given fairly close together ‐ four classroom periods in a week or one each week for four weeks; the fifth session given one to three months later) Control: existing human sexuality programme | |
| Outcomes | Unintended pregnancy, initiation of intercourse | |
| Notes | Duration of follow up: 2 years Loss to follow up: no mention | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation sequence generation not stated |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
Jemmott 1998.
| Methods | Randomis ed controlled study. Computer‐ generated random number was used to generate the allocation sequence Unit of randomis ation: individual |
|
| Participants | 659 African American students in 6th to 7th grade from three middle schools serving low‐income African American communities in Philadelphia, PA.; mean age of 11.8 years; 53% female and 47% male. | |
| Interventions | Intervention 1: eight 1‐hour modules over two consecutive Saturdays on abstinence HIV intervention (health education, skills‐ building, contraception education with emphasis on abstinence) Intervention 2: eight 1‐hour modules over two consecutive Saturdays on safer sex HIV intervention (health education, skills‐ building, abstinence with emphasis on the use of contraceptives) Control: health issues unrelated to sexual behaviour Each intervention consisted of eight 1‐hour modules divided equally over two consecutive Saturdays |
|
| Outcomes | Initiation of intercourse, consistent condom use ( sexual intercourse in past three months among all participants) | |
| Notes | Duration of follow up: 12 months Loss to follow up: 7.4% Individuals were randomly allocated to one of the three conditions (abstinence HIV intervention, safer sex HIV intervention and control) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐ generated random numbers |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Proctors were blinded to participants' intervention group |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Per‐protocol analys es were carried out, included only patient present at the end of the study regardless of the number of intervention sessions attended |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes were reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
Jemmott 2005.
| Methods | Cluster‐randomis ed controlled study. Computer‐generated random numbers were used to generate allocation sequence. Unit of randomis ation: schools | |
| Participants | 682 sexually experienced adolescent girls of a children's hospital, mean age 15.5 years, 68% African American, 32% Hispanic, low income | |
| Interventions | Intervention 1: HIV/STD education, contraceptive education Intervention 2: skills‐ building, HIV/STD education, contraceptive education Control: health promotion intervention |
|
| Outcomes | Sexually transmitted diseases | |
| Notes | Duration of follow up: 12 months Loss to follow up: 11.4% |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐ generated random numbers |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition was low (11.4%) and did not differ by condition |
| Selective reporting (reporting bias) | Low risk | Pre‐stated outcomes reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
Jemmott 2010.
| Methods | Cluster‐ randomi sed controlled trial using blocked (4 to 8 in size) computer‐generated random number sequences; unit of randomis ation: community‐ based organis ations (CBOs) in a 2 x 3 factorial design to the HIV/STD risk‐reduction intervention or control and to one of the three levels of facilitator training (manual only, standard training and enhanced training) | |
| Participants | 1707 adolescents aged 13 years to 18 years who read, wrote and spoke English with written parental or guardian consent in English or Spanish. Over 80% of the participants w ere Black or African American and half of the participants were female | |
| Interventions | Intervention: six 50‐ minute modules of developmentally appropriate interactive activities, films, small group discussions, experimental exercises and role‐play activities. Information provided included the aetiology, detection, transmission, prevention and possibilities of asymptomatic infection, attitudes toward condom use, skill and self‐efficacy in using condoms. It also teaches abstinence as the most effective way to prevent STDs Manual only: intervention package and no training Standard training: intervention package and two days' training Enhanced training: intervention package, two days' standard training and practice implementation of the intervention with group of adolescents Control: health promotion which focused on reducing behaviours linked to risk for heart disease, hypertension, lung disease and cancer |
|
| Outcomes | Self‐reported consistent condom use in the previous three months, proportion of condom‐protected sex, frequency of sex in the past three months, condom use at most recent sex | |
| Notes | Duration of follow up: 3, 6 and 12 months; analysis on condoms and contraceptives were limited to those who were sexually active loss to follow up: 21.3% |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number sequence |
| Allocation concealment (selection bias) | Low risk | Facilitators were not aware of which group were in the follow‐up sample and participants were blinded to intervention prior to enrolment |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Data collectors were blind to the participant's intervention |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were reported |
| Other bias | High risk | Selection bias likely with respect to high decline from CBOs that support abstinence |
Kirby 1997a.
| Methods | Cluster‐randomised controlled trial. Method used to generate allocation sequence not mentioned in the paper. Unit of randomis ation: classrooms | |
| Participants | 1657 7th grade students from six schools in California, mean age of 12.3 years; 54% female and 46% male; 64% Hispanic, 13% Asian, 9% African American, 5% non‐ Hispanic , low socio‐economic status | |
| Interventions | Intervention: eight sessions for two weeks on health education, skills ‐building, contraceptive education, risks and consequences of teen sex and community resources Control: standard curriculum |
|
| Outcomes | Unintended pregnancy, initiation of intercourse, use of condoms at last sex, sexually transmitted diseases | |
| Notes | Duration of follow up: 17 months; loss to follow up: 23% Subset of patients was assessed for certain outcomes such as initiation of intercourse (only students who had never had sex at pre‐test were analys ed); likewise pregnancy and Sexually Transmitted Diseases (STD) (included in the analysis only students who had never been pregnant or never had an STD respectively) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided. Authors simply stated "randomly assigned" |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | High attrition |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes were reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
Kirby 1997b.
| Methods | Randomis ed controlled study. Method of allocation sequence not mentioned in this paper Unit of randomi sation: schools, agency, classroom, individual |
|
| Participants | 10,600 youths in 7th grade and 8th grade (mean age of 12.8 years) from schools and community‐based organi sations in California; 58% female and 42% male; 31% Hispanic, 38% White, 9% African‐American | |
| Interventions | Intervention 1: adult‐led intervention ( five sessions, 45‐50 minutes in length, delivered in classrooms or small group settings on health education, skills‐ building, contraceptive education) in addition to the available standard sexuality curriculum, taught by adults Intervention 2: youth‐led intervention (same intervention taught by peers) Control: standard sexuality curriculum |
|
| Outcomes | Unintended pregnancy, initiation of intercourse, use of condoms, use of hormonal contraceptive, sexually transmitted diseases | |
| Notes | Duration of follow up: 17 months Loss to follow up: 17% Five randomis ations were reported (random assignment by classroom to adult‐led intervention, by classroom to youth‐led intervention, by school to adult‐led intervention, by individual to adult‐led intervention, and control) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation sequence generation not stated |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | High attrition rate |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported |
| Other bias | Unclear risk | The study appears to be free from other sources of bias |
Kirby 2004.
| Methods | Cluster‐randomis ed controlled study. Method used to generate allocation sequence not mentioned in the paper. Unit of randomis ation: schools | |
| Participants | 3869 9th grade students from 20 urban high schools in Texas and California who completed the baseline survey in autumn 1993 and officially enrolled at first follow up (spring 1994), mean age 15 years, 53% female and 47% male; 30% White, 27% Hispanic, 18% Asian or Pacific Islanders, 17% Black and 7% other Exclusion: students who left the school during the 1993 to 1994 school year |
|
| Interventions | Intervention: 20 sessions on health education, skills‐ building, contraceptive education, community linkages Control: standard knowledge‐ based HIV prevention curriculum |
|
| Outcomes | Initiation of intercourse, use of contraceptive at last sex | |
| Notes | Duration of follow up: 31 months Loss to follow up: 21% |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation sequence generation not stated |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Analysis was carried out on the number of students' observations for each outcomes. |
| Selective reporting (reporting bias) | Low risk | Pre‐stated outcomes we re reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
Kogan 2012.
| Methods | Randomis ed controlled study; families were randomly assigned | |
| Participants | 506 African Americans aged 16 years, with 51% female | |
| Interventions | Intervention: Strong African American Families Teen (SAAF‐T) programme: a family‐ centred intervention made up of five sessions on optimal parenting, preparation for life after high school, content on sexual health, and an optional condom skills unit Control: family‐ centred intervention but designed to promote healthful behaviours (good nutrition, exercise, and informed consumer behaviour) |
|
| Outcomes | Unprotected intercourse in the past three months, condom efficacy | |
| Notes | Duration of follow up: 5 and 22 months Loss to follow up: 5% |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation not stated |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low attrition rate |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
Markham 2012.
| Methods | Three‐ armed randomis ed controlled trial, schools were randomis ed using a multi‐attribute randomis ation protocol | |
| Participants | 1258 students; 75% of students were classified as economically disadvantaged, 59.8% female, 39.3% African American and 48.4% Hispanic with a mean age of 12.6 years | |
| Interventions | Intervention 1 (Risk Avoidance): interactive skills‐training exercises, peer role model videos, emphasis ed interactions between personal, environmental and behavioral influences, beliefs and normative beliefs. it also included homework to facilitate parent‐child communication, incorporating elements of character development and future orientation. It was framed to reinforce abstinence‐until‐marriage beliefs Intervention 2 (Risk Reduction): contained similar activities as Risk Avoidance but reinforced abstinence‐until‐older beliefs. In addition, it promoted self‐resect and responsibility, activities addressing knowledge and self‐efficacy regarding condom and contraceptive use Control: regular health classes offered by the respective schools |
|
| Outcomes | Sexual initiation (for virgins only), unprotected sex at last vaginal intercourse, frequency of sex in the past three months, frequency of sex without a condom in the past three months, number of lifetime sexual partners, number of sexual partners in the past three months | |
| Notes | Duration of follow up: 16 and 26 months Loss to follow up: 25%. In addition, 75 students were excluded because of missing or inconsistent responses |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of randomi sation not clearly explained |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Sample sizes for each outcome varied due to missing data |
| Selective reporting (reporting bias) | Low risk | Pre‐stated outcomes reported |
| Other bias | Unclear risk | The presence of baseline imbalances in demographics and sexual behaviour between conditions |
Mba 2007.
| Methods | Randomis ed controlled study. Unit of randomisation: individuals; method of randomis ation was not stated | |
| Participants | 360 students aged 10 years to 20 years, all African | |
| Interventions | Intervention: reproductive health education on STDs, HIV/AIDS and family planning Control: no education or intervention |
|
| Outcomes | Correct knowledge about STD (control measures), HIV/AIDS (transmission and cure) and family planning (methods and usage) | |
| Notes | Duration of follow up: 6 weeks Loss to follow up: None |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Schools were selected using a basket method of random sampling, while students were selected using a systematic sampling method (every ninth student on the school register) |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Due to the short duration in follow up, no participants were lost and there were no missing outcome data |
| Selective reporting (reporting bias) | Low risk | All stated outcomes were reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
Minnis 2014.
| Methods | Cluster‐ randomis ed study; social networks were randomi sed; method of randomis ation not stated but both participants and research interviewers were blinded to the assignment | |
| Participants | 162 youths , male and female, aged 16 years to 21 years (median age 16.8) who were Hispanic, residing in San Francisco, spoke English or Spanish, were not pregnant or parenting | |
| Interventions | Intervention: eight life skills sessions (communication and relationship‐ building skills) promoting sexual health with a focus on STI and unintended pregnancy prevention and early childbearing norms; job training, reproductive health wellness (such as clinic visit), cash payment to youth on completion of a given activity Control: standard community services |
|
| Outcomes | Childbearing expectations, STIs, contraceptive self‐efficacy and motivation | |
| Notes | Duration of follow up: 6 months loss to follow up: 8% |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Information on this domain was not provided |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Both participants and research interviewers were blinded to the assignment |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition rate < 10%, baseline differences between participants adherent to the intervention compared to those who did not participate or participated minimally with regards to risky behaviours (lower proportion had ever had sex (< 0.01), gang‐affiliated close friends (< 0.05) and used alcohol frequently (< 0.01) |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
Mitchell‐DiCenso 1997.
| Methods | Cluster‐ randomised controlled trial. Table of random numbers was used to generate allocation sequence Unit of randomis ation: schools |
|
| Participants | 3289 students in Grades 7 and 8 in 21 schools in Hamilton, Ontario‐Canada; mean age 12.6 years, 52% female, 48% male, most White Exclusion: non‐consent by parent or students; planning to move out of the area in the next few weeks; unable to speak or understand English, severe learning disabilities, reached 17th birthday, attendance at a private or separate school |
|
| Interventions | Intervention: ten 1‐hour sessions on health education and skills building, media and peer pressure, parenting, teenage pregnancy and responsibility in relationships Control: conventional sex education |
|
| Outcomes | Unintended pregnancy, initiation of intercourse, use of contraceptives | |
| Notes | Duration of follow up: 4 years Loss to follow up: 44% During the study, 10 students transferred from the control to the experimental school and one student from an experimental to a control school |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Table of random numbers |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | High rate of attrition by the fourth year with close to half the participants lost to follow up. Analysis for each outcome included only student who responded to that outcome |
| Selective reporting (reporting bias) | Low risk | Pre‐stated outcomes were reported |
| Other bias | Unclear risk | Contamination of intervention groups as students who completed Grade 8 moved on to high schools that drew students from a variety of schools, thereby bringing together experimental and control group students |
Morberg 1998.
| Methods | Cluster‐randomised controlled study. Block randomi sation was used to generate allocation sequence. Unit of randomis ation: s chools | |
| Participants | 2483 6th grade students in 21 middle schools in small cities and towns in Wisconsin; by 9th grade, participants included 48% male, 52% female, 96% White, 4% other | |
| Interventions | Intervention 1: age‐ appropriate: taught four weeks each year over three years in grade 6, 7 and 8: on social situations, refusal skills (skills‐ building), parental values, media, parent relationship, contraception education, risks, responsibility and sexuality Intervention 2: intensive; taught as a 12‐ week block in grade 7: same programme Control: usual curriculum |
|
| Outcomes | Initiation of intercourse, use of condoms | |
| Notes | Duration of follow up: 3 years Loss to follow up: 20% Students were randomised into one of three interventions ( control, age ‐ appropriate intervention or intensive intervention. One of the seven schools dropped out of the intensive intervention (n = 590), data from these are excluded |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomis ation design nested within two self‐selected treatment options |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No statistical difference between interventions in attrition by 9th grade (p = 0.21). But high percentage of participants were lost to follow up in the 10th grade (32%) and underrepresented the intensive subjects. Individuals were used as the unit of analysis even though clusters were randomised |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
Morrison‐Beedy 2013.
| Methods | Randomis ed controlled trial, individual was randomi sed by block randomi sation, research assistant was blinded to conditions | |
| Participants | 738 girls aged 15 years to 19 years, unmarried, not pregnant, not given birth within the past three months, sexually active within the past three months; predominantly low income, 69% African American | |
| Interventions | Intervention: four weekly, 120‐ minute sessions and two 90‐ minute booster sessions at three months and six months post‐intervention. It provided HIV information, motivation to reduce risky behaviour, interpersonal and self‐management and communication skills facilitating sexual risk reduction and condom use Control: general health promotion (nutrition, breast health, anger management) with the same number of sessions and led by the same facilitators |
|
| Outcomes | Frequency of sexual behaviour, protected vaginal sex, number of sexual partners, abstinence | |
| Notes | Duration of follow up: 3 months, 6 months and 12 months Loss to follow up: approx 14% |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Block randomi sation of participants, but method of block randomi sation not stated |
| Allocation concealment (selection bias) | Unclear risk | No information on this domain was provided |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Condition was known only to the project director until each group was filled and facilitators assigned. Also, pregnancy and STI was confirmed by testing |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition rate: 14%; Girls lost to follow up were older and may have been at more risk of the outcomes |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
Norton 2012.
| Methods | Randomi sed controlled trial; method of randomis ation not stated | |
| Participants | 198 college students that were at least 18 years of age, heterosexual, engaged in sexual intercourse at least once during the past three months; 70% females, 85% White and 15% non‐ White | |
| Interventions | Intervention: it includes information and myths, attitudes and social norms, teaching skills and building self‐efficacy regarding increasing condom use and safer sexual behaviour. with an exclusive focus on preventing unplanned pregnancy (Intervention A), STI (Intervention B) or HIV infection (Intervention C). Control: standard healthcare services received by students in college settings |
|
| Outcomes | Condom use, including percentage, frequency and use at last sex; number of unprotected vaginal intercourse | |
| Notes | Duration of follow up: 4 weeks and 8 weeks; for certain outcomes, the different interventions were collapsed as one | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of randomis ation not stated |
| Allocation concealment (selection bias) | Unclear risk | No information on this domain was provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information on this domain was provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition rates were not reported |
| Selective reporting (reporting bias) | Low risk | All stated outcomes w ere reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
O'Donnell 1999.
| Methods | Cluster‐ randomis ed controlled trial. Classrooms within the intervention school were randomly assigned | |
| Participants | 1061 minority students, 7th & 8th graders, 79.2% African American, 47.2% male and 15.9% Hispanic, high‐risk health profile, high‐risk academic profile, with limited access to resources | |
| Interventions | Intervention: the intervention was split into two; the regular community youth service (CYS) classroom curriculum (40 lessons in 7th grade and 34 lessons in 8th grade on risk related to early and unprotected sex, violence, substance use, healthy development and sexuality) and CYS classroom curriculum enhanced by participation. In the latter, participants engaged in three hours per week community placement performing a variety of tasks associated with social skills and behaviours, assisting or observing doctors, recreation groups etc Control: intervention not explained |
|
| Outcomes | Initiation of sex (virgins at baseline), recent sex in the last three months, use of protection during the most recent intercourse | |
| Notes | Duration of follow up: 6 months loss to follow up: 8.3% |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of randomi sation was not stated |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low loss to follow up (< 10%) |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
O'Donnell 2002.
| Methods | Cluster‐randomis ed controlled study. Method used to generate allocation sequence not stated. Unit of randomis ation: classrooms | |
| Participants | 225 7th grade students from 18 classrooms attending a public middle school in New York, 71% non‐Hispanic African‐American, 26% Hispanic, low socio‐economic status | |
| Interventions | Intervention: thr ee hours per week Community Youth Service (CYS) plus classroom curriculum (40 lessons in 7th grade and 34 lessons in 8th grade on risk related to early and unprotected sex, violence, substance use, healthy development and sexuality) Control: standard classroom curriculum |
|
| Outcomes | Pregnancy among all participants not reporting pregnancy at baseline Ever had sex among all participants | |
| Notes | Duration of follow up: 4 years Loss to follow up: 23% After year 1 of the programme, the school expanded the CYS component to more students resulting in 32 students transferring into the intervention group and 16 transferring to the control group because CYS did not fit their schedules. Analyses were divided into youths receiving two programme years, youths receiving one programme year (i.e. those who transferred in or out after year 1), and no‐exposure controls. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation sequence generation not stated |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Irrespective of the crossover of participants between intervention and control groups, analysis retained participants in their previous randomised group |
| Selective reporting (reporting bias) | Low risk | Pre‐specifed outcomes were reported |
| Other bias | Unclear risk | Crossover of students between groups could have contaminated the different groups. |
Okonofua 2003.
| Methods | Cluster‐randomised controlled study. Method used to generate allocation sequences not mentioned. Unit of randomis ation: schools | |
| Participants | 1896 students in secondary schools in Benin, Nigeria, 14 years to 20 years, 53% female, 47% male, 33% Ishan, 36% Bini, 5% Yoruba, 10% Ibo, 16% other | |
| Interventions | Health education, peer education on STD, individual or group counselling by trained peer educators, training of health providers on STD diagnosis and treatment around the intervention schools Control: no intervention |
|
| Outcomes | Use of condoms | |
| Notes | Duration of follow up: 10 months Loss to follow up: 1% |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation sequence generation not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain was not provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Individuals were used as the unit of analysis even though clusters (classrooms) were randomised. All participants lost to follow up were from the control group and per‐protocol analysis used |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
Perskin 2015.
| Methods | Two‐arm nested randomis ation design. Randomi sation was carried out using a Multi‐attribute randomi sation method. Unit of randomi sation: s chools | |
| Participants | 1571 female participants with mean age of 14.3 years (standard deviation = 0.59), and was 59% female, 74% Hispanic, 17% African‐American, and 9% other race/ethnicity. Close to 20% of students reported ever engaging in any type of sex (vaginal, oral, or anal) | |
| Interventions | Intervention: computer‐based sexual health education, animated scenario with modelling and skills practices, peer‐modelling videos, quizzes, virtual role‐playing activities to stimulate student skills practice in real‐world situation, healthy/unhealthy dating relationship, anatomy of reproduction, social, emotional, physical consequences of sex, communication skills, internet communication safety, causes of teen pregnancies and STIs, knowledge and skills of condoms and contraception use and condom negotiation Control: state‐approved school health education |
|
| Outcomes | Delayed initiation of any sexual activity, sexual behaviours such as use of condoms in the past three months and last sex, number of partners at different time points, knowledge of STIs and condoms, and beliefs (psychosocial measures) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Multi‐attribute randomi sation method |
| Allocation concealment (selection bias) | Unclear risk | Method not stated but it was stated that "participants were blinded to condition during allocation" |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain was not provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rate approx. 10%, which was similar across groups |
| Selective reporting (reporting bias) | High risk | Primary outcome was reported. However, most of the secondary pre‐specified outcomes such as condom use at last sex or in the last three months were not reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
Philliber 2002.
| Methods | Randomis ed controlled study. Unit of randomi sation: individual | |
| Participants | 484 teenagers in New York not currently pregnant or a parent, 13 years to 15 years, 55% female, 45% male, 56% Black, 42% Hispanic, 2% other | |
| Interventions | Intervention: job clubs, academic skills, family and life sexuality education, developing personal art skills, recreational activities, group/individual counselling, contraceptive education, medical care ( five days per week for a school year) Control: alternative youth programme (recreational activities, homework help, art and crafts) |
|
| Outcomes | Unintended pregnancy, childbirth, initiation of intercourse, use of condoms at last sex | |
| Notes | Duration of follow up: 3 years Loss to follow up: 21% Allocation concealment by the use of opaque envelopes |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of randomis ation not stated |
| Allocation concealment (selection bias) | Low risk | Use of opaque envelopes |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain not provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Analysis was based on number of participants present at the end of the three ‐year follow up (high attrition rate) |
| Selective reporting (reporting bias) | Low risk | Pre‐specfied outcomes reported |
| Other bias | Unclear risk | Possible contamination (exchange of information) between groups, since both programmes were conducted at the same site |
Raine 2005.
| Methods | Randomis ed controlled study. Computer‐generated randomi sation sequence was used. Unit of randomi sation: individual |
|
| Participants | 2117 women attending four California clinics providing family planning services, who were not desiring pregnancy, 15 years to 24 years (mean 19.9), spoke English or Spanish, had sexual intercourse in the past six months, using long‐ term hormonal contraception or requesting EC, 20% Hispanic, 15% Black, 31% White, 22% Asian, 12% Other | |
| Interventions | intervention 1: pharmacy access group (instructions for obtaining levonorgestrel Intervention 2: (provision of three packets of levonorgestrel EC and its dosage) Control: clinic access (instructions to return to the clinic for EC, if needed) |
|
| Outcomes | Unintended pregnancy, contraceptive use (consistent condom use, use of hormonal contraceptives, use of condom at last sex), sexually transmitted diseases | |
| Notes | Duration of follow up: 6 months Loss to follow up: 8% Single blinding ( research staff only) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐ generated numbers |
| Allocation concealment (selection bias) | Low risk | Sealed, sequential numbered boxes identical in appearance were used to conceal allocation |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Research staff only |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Use of a Modified intention‐to treat where only participants who completed follow‐up in their respective randomised group were analys ed. Attrition analysis showed no difference in characteristics of women lost to follow up. |
| Selective reporting (reporting bias) | Low risk | All stated outcomes in the method section were reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
Raymond 2006.
| Methods | Randomis ed controlled study. Computer‐ generated random numbers were used in allocation sequence. Unit of randomis ation: individuals | |
| Participants | 1490 sexually active women not desiring pregnancy, 14 years to 24 years, 13% Hispanic, 70% White, 21% non‐ White | |
| Interventions | Intervention: contraception distribution ( two packages of pills dispensed in advance with unlimited resupply at no charge) Control: contraceptive distribution (pills dispensed when needed at usual charge) |
|
| Outcomes | Unintended pregnancy, sexually transmitted diseases | |
| Notes | Duration of follow up: 1 year Loss to follow up: < 7% |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐ generated number |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain not provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised participants were included in the analysis |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcome reported |
| Other bias | Unclear risk | Higher proportion of people in the increased access group had a sexually transmitted disease which may lead to increased use of condoms |
Shrier 2001.
| Methods | Randomis ed controlled trial. Table of random numbers was used to generate allocation sequence. Unit of randomis ation: individuals | |
| Participants | 123 female participants between the ages of 13 years to 22 years (median 17.2) with cervicitis or pelvic inflammatory disease in urban children's hospital, adolescent clinic and inpatient service in Boston, 49% non‐Hispanic Black, 18% Hispanic, 14% Non‐Hispanic White, 17% other Exclusion: p atient had treatment of STDs between laboratory confirmation; patient pregnant at treatment visit; patient already exposed to intervention through pilot study |
|
| Interventions | Intervention: watch a seven ‐minute videotape featuring contraception education (condoms), contraception distribution, individual counselling on risk perception, STD education, pregnancy prevention and consequences of unprotected sex and a booster session at one , three and six months. Control: standard STD education and contraceptive education and distribution |
|
| Outcomes | Sexually transmitted diseases | |
| Notes | Duration of follow up: 12 months Loss to follow up: 48% Assessors were blinded to participant allocation |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Table of random numbers |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain not provided |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Assessors only |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | High attrition rates of over 20% though it did not differ between the intervention and control groups. As‐treated analysis was done with substantial loss‐ to‐ follow‐ up of participants across groups. |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported |
| Other bias | Low risk | Study appears to be free from other sources of bias |
Sieving 2011.
| Methods | Randomis ed controlled trial. Individuals were randomi sed to the intervention or control but the method of randomi sation was not stated. | |
| Participants | 253 girls aged between 13 years to 17 years, racially mixed ; American Indian, Asian, Hispanic, White/European, mixed and Black/African/African American. Black/African/African American made up over 40% of the population | |
| Interventions | Intervention: one‐on‐one case management addressing the following issues: emotional skills, healthy relationships, responsible sexual behaviours, positive family, school and community involvement and the peer leadership components which provided hands‐on skills‐ building experiences; plus usual clinic services Control: usual clinic services |
|
| Outcomes | Contraceptive use (condom, hormonal and dual method) consistency with most recent sex partner, number of sex partners in the past six months | |
| Notes | Duration of follow up: ,12 & 24 months, intention‐to‐treat design Loss to follow up: 5.5% and 6.7% at 12 and 24 months respectively |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of randomis ation not stated |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain not provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain not provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rate was low (< 10%) |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes not provided |
| Other bias | Low risk | The study seems to be free from other sources of bias |
Smith 1994.
| Methods | Randomis ed controlled study. Method used to generate allocation sequence not mentioned in the paper. Unit of randomis ation: individuals | |
| Participants | 120 9th grade students from the 1989 class of freshmen at a high school in Queens, New York. Mean age 15.1 years; 74.2% female and 25.8% male; 43.3% African American, 30.8% West Indian, 22.5% Hispanic and 3.3% other | |
| Interventions | Intervention: one session per week for 14 weeks on health/STD education, skills‐ building, contraceptive education and individual counselling on career mentorship Control: written materials on contraception and decision making pertaining to sexual‐ and fertility‐ related risk‐taking behaviour |
|
| Outcomes | Initiation of intercourse ( absolute sexual frequency ‐ instances of completed sexual activity during past two months, among all participants) | |
| Notes | Duration of follow up: six months. Loss to follow up: 21% |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of allocation sequence generation not stated |
| Allocation concealment (selection bias) | Unclear risk | No information provided on this domain |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information provided on this domain |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Per‐protocol analysis was done with substantial departure of the intervention received from that assigned at randomis ation |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
Stephenson 2004.
| Methods | Cluster‐randomis ed controlled study. Schools were randomised within strata, using a computer‐generated sequence of allocation of block size ten. Unit of randomis ation: schools | |
| Participants | 8766 pupils in 29 schools in central and southern England, aged 13 years to 14 years; over 9000 pupils | |
| Interventions | Intervention: Three 1‐hour sessions on sexual communication and relationships, contraceptive education (condoms) (pressure role play on declining sex or insisting on the use of condoms), HIV/STD education (transmission and treatment) taught by peer leaders (16 years to 17years) Control: usual teacher‐led sex education |
|
| Outcomes | Unintended pregnancy, heterosexual intercourse at age 16 years, use of contraceptives (at first and last sex), use of condoms, abortion and livebirth at age 20 years, self‐reported STD | |
| Notes | Duration of follow up: 18 months and 54 months Loss to follow up: 14% and > 40% at 18 months and 54 months respectively Data on abortion and livebirth are included in data & analysis, while others are reported in additional tables |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated sequence of allocation of block size ten |
| Allocation concealment (selection bias) | Unclear risk | No information provided on this domain |
| Blinding (performance bias and detection bias) All outcomes | Low risk | While blinding of participants/facilitators to allocation was not possible, matching of outcomes to sources was blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | All participants who experienced the outcome at baseline and who completed at least one follow‐up questionnaire were included in the analysis for the primary outcome (initiation of intercourse). High attrition rate at 54 months but intention ‐to‐ treat was employed for primary outcomes (childbirth and abortion by 20 years) at the second follow up |
| Selective reporting (reporting bias) | Low risk | Expected outcomes and those pre‐specified in the methods were reported |
| Other bias | Unclear risk | It is not known for sure if there was no contamination between pupils in the different groups |
Villarruel 2006.
| Methods | Randomised controlled study. Computer‐generated random numbers used to generate allocation sequence Unit of randomi sation: individuals |
|
| Participants | 656 8th grade to 11th grade students in Northeast Philadelphia schools and community‐ based organis ations, aged 13 years to 18 years, 45% male, 55% female, 85.4% Hispanic | |
| Interventions | Intervention: six 50‐minute modules on Health/HIV education, skills‐ building, contraceptive education Control: health promotion education |
|
| Outcomes | Initiation of intercourse in the past t hree months, consistent condom use in the past three months, | |
| Notes | Duration of follow up: 12 months Loss to follow up: 13% 103 students were excluded from the analysis because they were non‐ Hispanic |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐ generated numbers |
| Allocation concealment (selection bias) | Unclear risk | No information provided on this domain |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information provided on this domain |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Analyse s were conducted using an intention‐to‐treat approach in which participants were analy sed in their original randomised groups regardless of the number of sessions attended |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes were reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
Walker 2006.
| Methods | Cluster‐randomis ed controlled study. Method used to generate allocation sequence not mentioned in the paper. Unit of randomi sation: schools | |
| Participants | 10,954 10th grade to 12th grade high school students in Morelos, 15 years to 18 years, 48% male, 52% female | |
| Interventions | Intervention 1: HIV education, skills‐ building, cultural values, contraceptive promotion ( condoms). Intervention 2: HIV education, skills‐ building, cultural values plus contraceptive education (EC plus condoms and their access). Control: biology‐ based sex education |
|
| Outcomes | Initiation of intercourse, use of condom at last sex, use of hormonal contraceptive | |
| Notes | Duration of follow up: 16 months Loss to follow up: 33.3% Two of the intervention schools were included in the control group because they did not teach the intervention course |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The statement "randomly assigned" was said but the method of allocation generation was not stated. |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain not provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Information on this domain not provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Per‐protocol analysis was done. But analysis took the cluster sample design into account. |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes not provided |
| Other bias | Low risk | The study appears to be free from other sources of bias |
Wight 2002.
| Methods | Cluster‐randomis ed controlled study. Method used to generate allocation sequence not mentioned. Unit of randomi sation: schools | |
| Participants | 7616 pupils from 25 secondary schools in east Scotland, 13 years to 15 years, 50% male, 50% female | |
| Interventions | Intervention: SHARE (20‐ session package: 10 for 3rd years and 10 for 4th years of secondary school respectively) on health/sex education, skills ‐building, contraceptive education primarily through the use of interactive video Control: conventional sex education |
|
| Outcomes | Unintended pregnancy, initiation of intercourse, use of condoms at last sex | |
| Notes | Duration of follow up: 2 years Loss to follow up: 31% Single blinding ( assessors) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of randomis ation was not stated |
| Allocation concealment (selection bias) | Unclear risk | Information on this domain not provided |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Assessors only |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Outcomes were analy sed based on the number of participants at the end of the two ‐year follow up. |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported |
| Other bias | Low risk | The study appears to be free from other sources of bias |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Agha 2002 | Did not measure any of the desired outcomes |
| Amin 2004 | Randomi sed controlled trial but participants were pregnant or parenting teens |
| Antunes 2002 | Participants above the required age range |
| Barlow 2006 | Had none of the required interventions |
| Barnet 2009 | Secondary prevention of adolescent pregnancy |
| Barnet 2010 | Unintended repeat pregnancies assessed |
| Bonell 2005 | No specified intervention |
| Bouris 2010 | Non‐randomis ed controlled trial |
| Boyer 2005 | Participants above the required age range |
| Brinkman 2010 | Published protocol |
| Brown 2011 | Control group received an intervention aimed at promoting contraceptive usage |
| Buston 2007 | Non‐randomis ed controlled trial |
| Cagampang 1997 | Non‐randomis ed controlled trial |
| Chesney 2003 | Non‐randomis ed controlled trial |
| Chung‐Park 2008 | Participants aged 18 years to 32 years (above required age range) |
| Cowan 2008 | Reported information on baseline characteristics only |
| Crosby 2005 | None of the desired outcomes was measured |
| Danielson 1990 | Quasi‐experimental study |
| Decat 2014 | C ross‐sectional st udy |
| Di 2004 | None of the desired outcomes was measured |
| Diclemente 2001 | Non‐randomis ed controlled study |
| Doniger 2001 | Non‐randomis ed controlled study |
| Dycus 1990 | Non‐randomis ed controlled study |
| East 2003 | Non‐randomis ed controlled study |
| Eisen 1985 | Non‐randomis ed controlled study |
| Eisen 1987 | Non‐randomis ed controlled study |
| El‐Bassel 2003 | Participants were above the required age range |
| Ferguson 1998 | Quasi‐randomis ed controlled study |
| Fitzgerald 2002 | Non‐randomis ed controlled study |
| Gallegos 2008 | Did not measure any of the desired outcomes |
| Garbers 2012 | Participants above the required age and different outcomes measured |
| Gaughran 2014 | Non‐randomis ed controlled trial |
| Guilamo‐Ramos 2011a | No control group |
| Harvey 2004 | Randomis ed controlled trial but participants included couples only |
| Havens 1997 | Unintended repeat pregnancies assessed |
| Howard 1990 | Non‐randomi sed controlled trial |
| Hutchinson 2003 | None of the desired outcomes was measured |
| James 2005 | Participant above the required age range |
| Jay 1984 | Did not measure any of the desired outcomes |
| Jennings 2014 | Non‐randomis ed controlled trial |
| Jewkes 2006 | Participants above the required age range |
| Kaljee 2005 | None of the desired outcomes was measured |
| Kamali 2002 | Age range above the required range |
| Katz 2011 | Unintended repeat pregnancies assessed |
| Kirby 2002a | A Review |
| Kirby 2002c | Non‐randomis ed controlled trial |
| Kuroki 2008 | An epidemiological study |
| Kyrychenko 2006 | Non‐randomis ed controlled study |
| Legardy 2005 | Participants' age range was above the required range |
| Liberman 2000 | Non‐randomis ed controlled study |
| Magnani 2005 | Non‐randomis ed controlled trial |
| Martiniuk 2003 | Study did not measure any of the desired outcomes |
| Matteson 2006 | No intervention |
| McBride 2000 | Method of randomis ation not adequate |
| Metcalf 2005 | Participants were above the required age range |
| Mitchell 2014 | Non‐randomis ed controlled trial |
| O'Donnell 2005 | None of the desired outcomes was measured |
| Ochiogu 2011 | Non‐randomis ed controlled trial |
| Olsen 1991 | Not a randomis ed controlled trial |
| Padian 2007 | Participants above the required age range |
| Peipert 2008 | Participants above the required age range |
| Peipert 2011 | Participants above the required age range |
| Peipert 2012 | Not a randomis ed controlled trial |
| Peragallo 2005 | Participants above the required age range |
| Peterson 2007 | Participants above the required age range |
| Proude 2004 | Participants above the required age range |
| Rickert 2007 | Participants above the required age range |
| Robin 2004 | A review |
| Schreiber 2010 | Unintended repeat pregnancies assessed |
| Schwarz 2008 | Participants above the required age range |
| Secura 2014 | Non‐randomis ed controlled trial |
| Shuey 1999 | A quasi‐randomis ed study |
| Sieving 2012 | Non‐randomis ed controlled trial |
| Silva 2002 | A review |
| Stout 1989 | A review |
| Thato 2008 | Quasi‐experimental design |
| Thomas 2000 | A review |
| Thomas 2004 | Non‐randomis ed controlled trial |
| Tingle 2002 | Non‐randomis ed controlled trial |
| Van 1985 | Study included participants greater than the age limit and it was not clearly stated what percentage was within the accepted age range |
| Van Devanter 2002 | Participants were not within the age limit |
| Wiggins 2009 | Case‐control study |
| Yoo 2004 | Non‐randomis ed study |
| Zabin 1986 | Non‐randomis ed study |
| Zabin 1988 | Non‐randomis ed study |
| Zimmerman 2008 | Quasi‐experimental study |
Characteristics of studies awaiting assessment [ordered by study ID]
Murray 2015.
| Methods | Multi‐center, clinic‐based, randomised controlled trial |
| Participants | Female, aged 14 years to 19 years |
| Interventions | Seventeen Days (theory‐based interactive video intervention) |
| Outcomes | Unintended pregnancy and STIs |
| Notes | Full paper pending |
Shafii 2014.
| Methods | Randomised controlled study |
| Participants | Male and female (14 years to 24 years) |
| Interventions | Interactive computer‐based intervention |
| Outcomes | STIs, unintended pregnancy, number of partners, rate of unprotected vaginal sex (without condoms) and rate of unprotected vaginal sex (without contraceptive) |
| Notes | Full paper pending |
Differences between protocol and review
We included five trials that had a small percentage of participants aged 19 years to 24 years (outside the age limit stipulated in the protocol). However, the ages of most of the study population (more than 75%) in each of these four trials were within the age limit stipulated in the review protocol (10 years to 19 years).
We excluded all quasi experimental and cross‐over trials as this was cumbersome and would have prolonged the completion of this review.
Methodological quality of included studies was assessed using the 'Risk of bias tool' outlined in the Cochrane Handbook for Systematic Reviews of Interventions Version 5.1 (Higgins 2011a) and no longer by the method outlined in the 2004 Cochrane Reviewers' Handbook (Clark 2004) as previously stated.
Contributions of authors
JE conceived the review; JE, MM, AM contributed to the design and drafting of the protocol. JE and MM co‐ordinated the review, CO, EE, HE undertook searches of electronic databases (CENTRAL, PubMed, EMBASE, LILACS), carried out the email search for unpublished literature, and organised the retrieval of papers. CO, EE and HE screened for included studies while CO and EE extracted and entered data on trial results into RevMan 5.3. MM and CO interpreted the data and prepared the first draft of the complete review. All authors contributed to the drafting and editing of the review. JM and MM secured funding for the review. CO prepared the 'Summary of findings' tables
Sources of support
Internal sources
University of Calabar, Calabar, Nigeria.
External sources
-
Australian Cochrane Centre, Australia.
Provided the fund for this review
Mel and Enid Zuckerman College of Public Health, University of Arizona, Tucson, USA.
Nigeria branch of the South Africa Cochrane Centre, Nigeria.
Declarations of interest
Chioma Oringanje: none Martin M Meremikwu: none Hokehe Eko: none Ekpereonne Esu: none Anne Meremikwu: none John E Ehir: none
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Aarons 2000 {published data only}
- Aarons SJ, Jenkins RR, Raine TR, El‐Khorazaty MN, Woodward KM, Williams RL. Postponing sexual intercourse among urban junior high school students ‐ a randomized controlled evaluation. Journal of Adolescent Health 2000;27:236‐47. [DOI] [PubMed] [Google Scholar]
Allen 1997 {published data only}
- Allen JP, Phillber S, Herring S, Kupermine GP. Preventing teen pregnancy and academic failure; experimental evaluation of a developmentally based approach. Child Development 1997;64(4):729‐42. [Google Scholar]
Baird 2010 {published data only}
- Baird S, Chirwa E, McIntosh C, Özler B. The short‐term impacts of a schooling conditional cash transfer program on the sexual behavior of young women. Health Economics 2010;19:55‐68. [DOI] [PubMed] [Google Scholar]
Basen‐Engquist 2001 {published data only}
- Basen‐Engquist K, Coyle KK, Parcel GS, Kirby D, Banspach SW, Carvajal SC, et al. Schoolwide effects of a multi‐component HIV, STD, and pregnancy prevention program for high school students. Health Education & Behaviour 2001;28(2):166‐85. [DOI] [PubMed] [Google Scholar]
Black 2006 {published data only}
- Black MM, Bentley ME, Papas MA, Oberlander S, Teti LO, McNary S, et al. Delaying second births among adolescent mothers: a randomized, controlled trial of a home‐based mentoring program. Pediatrics 2006;118:1087‐99. [DOI] [PubMed] [Google Scholar]
Blake 2001 {published data only}
- Blake SM, Simkin L, Ledsky R, Perkins C, Calabrese JM. Effects of a parent‐child communications intervention on young adolescents' risk for early onset of sexual intercourse. Family Planning Perspectives 2001;33(2):52‐61. [PubMed] [Google Scholar]
Bonell 2013 {published data only}
- Bonell C, Maisey R, Speight S, Purdon S, Keogh P, Wollny I, et al. Randomized controlled trial of ‘teens and toddlers’: a teenage pregnancy prevention intervention combining youth development and voluntary service in a nursery. Journal of Adolescence 2013;36:859‐70. [DOI] [PubMed] [Google Scholar]
Borgia 2005 {published data only}
- Borgia P, Marinacci C, Schiifano P, Perruci CA. Is peer education the best approach for HIV prevention in school? Findings from a randomized controlled trial. Journal of Adolescent Health 2005;36:508‐16. [DOI] [PubMed] [Google Scholar]
Cabezon 2005 {published data only}
- Cabezon C, Vigil P, Rojas I, Leiva ME, Riquelme R, Aranda W, et al. Adolescent pregnancy prevention: an abstinence‐centred randomized controlled intervention in a Chilean public high school. Journal of Adolescent Health 2005;36:64‐9. [DOI] [PubMed] [Google Scholar]
Clark 2005 {published data only}
- Clark LF, Miller KS, Nagy SS, Avery J, Roth DL, Liddon N, et al. Adult identity mentoring: reducing sexual risk for African American seventh grade students. Journal of Adolescent Health 2005;37:337‐47. [DOI] [PubMed] [Google Scholar]
Coyle 1999 {published data only}
- Coyle KK, Basen‐Engquist KM, Kirby DB, Parcey GS, Banspach SW, Collins JL, et al. Safer Choices: Long‐term impact of a multi‐component school‐based HIV, other STD and pregnancy program‐a randomized controlled trial. Unpublished data 1999.
Coyle 2004 {published data only}
- Coyle KK, Kirby DB, Marin BV, Gomez CA, Gregorich SE. Draw the line/respect the line: a randomized trial of a middle school intervention to reduce sexual risk behaviors. American Journal of Public Health 2004;94:843‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Coyle 2006 {published data only}
- Coyle KK, Kirby DB, Robin LE, Banspach SW, Baulmer E, Glassman JR. ALL4YOU! A randomized trial of an HIV, other STDs, and pregnancy prevention intervention for alternative school students. AIDS Education and Prevention 2006;18(3):187‐203. [DOI] [PubMed] [Google Scholar]
Diclemente 2004 {published data only}
- Diclemente RJ, Wingood GM, Harrington KF, Lang DL, Davies SL, Hook EW, et al. Efficacy of an HIV prevention intervention for African American girls. JAMA 2004;292(2):171‐9. [DOI] [PubMed] [Google Scholar]
Dilorio 2006 {published data only}
- Dilorio C, Resnicow K, McCarty F, De AK, Dudley WN, Wang DT, et al. Keepin' it R.E.A.L! Results of a Mother‐Adolescent HIV prevention program. Nursing Research 2006;55(1):43‐51. [DOI] [PubMed] [Google Scholar]
Dilorio 2007 {published data only}
- Dilorio C, McCarty F, Resnicow K, Lehr S, Denzmore P. REAL Men: A group‐randomized trial of an HIV prevention intervention for adolescent boys. American Journal of Public Health 2007;97:1084‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Downs 2004 {published data only}
- Downs JS, Murray PJ, Bruine de Bruin W, Penrose J, Palmgren C, Fischhoff B. Interactive video behaviour intervention to reduce adolescent females' STD risk: a randomized controlled trial. Social Science & Medicine 2004;59:1561‐72. [DOI] [PubMed] [Google Scholar]
Eisen 1990 {published data only}
- Eisen M, Zellman GL, McAlister AL. Evaluating the impact of a theory‐based sexuality and contraceptive education program. Family Planning Perspectives 1990;22(6):261‐71. [PubMed] [Google Scholar]
Fawole 1999 {published data only}
- Fawole IO, Azuzu MC, Oduntan SO, Brieger WR. A school‐based AIDS education programme for secondary school students in Nigeria: a review of effectiveness. Health Education Research Theory & Practice 1999;14(5):675‐83. [DOI] [PubMed] [Google Scholar]
Ferguson 1998 {published data only}
- Ferguson SL. Peer counselling in a culturally specific adolescent pregnancy prevention program. Journal of Health Care for the Poor and Underserved 1998;9(3):323‐33. [DOI] [PubMed] [Google Scholar]
Graham 2002 {published data only}
- Graham A, Moore L, Sharp D, Diamond I. Improving teenagers' knowledge of emergency contraception: cluster randomized controlled trial of a teacher led intervention. BMJ 2002;324:1179‐85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Guilamo‐Ramos 2011b {published data only}
- Guilamo‐Ramos V, Bouris A, Jaccard J, Gonzalez B, McCoy W, Aranda D. A parent‐based intervention to reduce sexual risk behavior in early adolescence: building alliances between physicians, social workers, and parents. Journal of Adolescent Health 2011;48:159‐63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Henderson 2007 {published data only}
- Henderson M, Wight D, Raab GM, Abraham C, Parkes, Scott S, et al. Impact of a theoretically based sex education programme (SHARE) delivered by teachers on NHS registered conceptions and terminations: final results of cluster randomised trial. BMJ 2007;334:133‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Herceg‐Brown 1986 {published data only}
- Herceg‐Brown R, Furstenberg FF, Shea J, Harris KM. Supporting teenager's use of contraceptives: a comparison of clinic services. Family Planning Perspectives 1986;18(9):61‐6. [PubMed] [Google Scholar]
Howard 1990 {published data only}
- Howard M, McCabe JB. Helping teenagers postpone sexual involvement. Family Planning Perspectives 1990;22(1):21‐7. [PubMed] [Google Scholar]
Jemmott 1998 {published data only}
- Jemmott JB, Jemmott LS, Fong GT. Abstinence and safer sex HIV risk‐reduction interventions for African American adolescents. JAMA 1998;279(19):1259‐536. [DOI] [PubMed] [Google Scholar]
Jemmott 2005 {published data only}
- Jemmott JB, Jemmott LS, Braverman PK, Fong GT. HIV/STD risk reduction interventions for African American and Latino adolescent girls at an adolescent medicine clinic. Archives of Pediatrics and Adolescent Medicine 2005;159:440‐9. [DOI] [PubMed] [Google Scholar]
Jemmott 2010 {published data only}
- Jemmott JB, Jemmott LS, Fong GT, Morales KH. Effectiveness of an HIV/STD risk‐reduction intervention for adolescents when implemented by community‐based organizations: a cluster‐randomized controlled trial. American Journal of Public Health 2010;100(4):720‐26. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kirby 1997a {published data only}
- Kirby D, Korpi M, Adivi M, Weissman J. An impact evaluation of project SNAPP: an AIDS and pregnancy prevention middle school program. AIDS Education and Prevention 1997;9(suppl 1):44‐61. [PubMed] [Google Scholar]
Kirby 1997b {published data only}
- Kirby D, Korpi M, Barth RP, Cagampang HH. The impact of the postponing sexual involvement curriculum among youths in California. Family planning perspectives 1997;29:100‐8. [PubMed] [Google Scholar]
Kirby 2004 {published data only}
- Kirby DB, Baumler E, Coyle KK, Basen‐Engquist K, Parcel GS, Harrist R, et al. The "Safer Choices" Intervention: Its Impact on the Sexual Behaviours of Different Subgroups of High School Students. Journal of Adolescent Health 2004;35:442‐52. [DOI] [PubMed] [Google Scholar]
Kogan 2012 {published data only}
- Kogan SM, Yu T, Brody GH, Chen Y, DiClemente RJ, Wingood GM, et al. Integrating condom skills into family‐centered prevention: efficacy of the Strong African American Families – teen program. Journal of Adolescent Health 2012;51(2):164‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Markham 2012 {published data only}
- Markham CM, Tortolero SR, Peskin MF, Shegog R, Thiel M, Baumler ER, et al. Sexual risk avoidance and sexual risk reduction interventions for middle school youth: a randomized controlled trial. Journal of Adolescent Health 2012;50:279–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mba 2007 {published data only}
- Mba CI, Obi SN, Ozumba BC. The impact of health education on reproductive health knowledge among adolescents in a rural Nigerian community. Journal of Obstetrics and Gynaecology 2007;27(5):513‐17. [DOI] [PubMed] [Google Scholar]
Minnis 2014 {published data only}
- Minnis AM, vanDommelen‐Gonzalez E, Luecke E, Dow W, Bautista‐Arredondo S, Padian NS. Yo puedo ‐ a conditional cash transfer and life skills intervention to promote adolescent sexual health: results of a randomized feasibility study in San Francisco. Journal of Adolescent Health 2014;55(1):85‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mitchell‐DiCenso 1997 {published data only}
- Mitchell‐DiCenso A, Thomas BH, Devlin MC, Goldsmith CH, Willan A, Singer J, et al. Evaluation of an education program to prevent adolescent pregnancy. Health Education and Behaviour 1997;24(3):300‐12. [DOI] [PubMed] [Google Scholar]
Morberg 1998 {published data only}
- Morberg DP, Piper DL. The health for life project: sexual risk behaviour outcomes. AIDS Education and Prevention 1998;10(2):128‐48. [PubMed] [Google Scholar]
Morrison‐Beedy 2013 {published data only}
- Morrison‐Beedy D, Jones SH, Xia Y, Tu X, Crean HF, Carey MP. Reducing sexual risk behavior in adolescent girls: results from a randomized controlled trial. Journal of Adolescent Health 2013;52(3):314‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Norton 2012 {published data only}
- Norton WE, Jeffrey D. Fisher JD, Rivet Amico K, Dovidio JF, Johnson BT. Relative efficacy of a pregnancy, sexually transmitted infection, or human immunodeficiency virus prevention–focused intervention on changing sexual risk behavior among young adults. Journal of American College Health 2012;60(8):574‐82. [DOI] [PubMed] [Google Scholar]
O'Donnell 1999 {published data only}
- O'Donnell L, Stueve A, Doval AS, Duran R, Haber D, Atnafou R, et al. The Effectiveness of the Reach for Health Community Youth Service Learning Program in Reducing Early and Unprotected Sex Among Urban Middle School Students. American Journal of Public Health 1999;89(2):176‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
O'Donnell 2002 {published data only}
- O'Donnell L, Stueve A, O'Donnell C, Duran R, Doval AS, Wilson RF, et al. Long‐term reductions in sexual initiation and sexual activity among urban middle schoolers in the reach for Health Service learning program. Journal of Adolescent Health 2002;31:93‐100. [DOI] [PubMed] [Google Scholar]
Okonofua 2003 {published data only}
- Okonofua FE, Coplan P, Collins S, Oronsaye F, Ogunsakin D, Ogonor JT, et al. Impact of an intervention to improve treatment‐seeking behaviour and prevent sexually transmitted diseases among Nigerian youths. International Journal of Infectious Diseases 2003;7:61‐73. [DOI] [PubMed] [Google Scholar]
Perskin 2015 {published data only}
- Peskin MF, Shegog R, Markham CM, Thiel M, Baumler ER, Addy RC, et al. Efficacy of It's your Game‐Tech: a computer‐based sexual health education program for middle school youth. Journal of Adolescent Health 2015;56:515‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Philliber 2002 {published data only}
- Philliber S, Kaye JW, Herlings S, West E. Preventing pregnancy and improving health care access among teenagers: an evaluation of the children's aid society‐Carrera program. Perspectives on sexual and reproductive health 2002;34(5):244‐51. [PubMed] [Google Scholar]
Raine 2005 {published data only}
- Raine TR, Harper CC, Rocca CH, Fisher R, Padian N, Klausner JD, et al. Direct access to emergency contraception through pharmacies and effect on unintended pregnancy and STIs. JAMA 2005;293:54‐62. [DOI] [PubMed] [Google Scholar]
Raymond 2006 {published data only}
- Raymond EG, Stewart F, Weaver M, Monteith C, Pol B. Impact of increased access to emergency contraceptive pills. Obstetrics and Gynecology 2006;108(5):1098‐106. [DOI] [PubMed] [Google Scholar]
Shrier 2001 {published data only}
- Shrier LA, Ancheta R, Goodman E, Chiou VM, Lyden MR, Emans SJ. Randomized controlled trial of a safer sex intervention for high‐risk adolescent girls. Archives of Pediatrics and Adolescent Medicine 2001;155:73‐9. [DOI] [PubMed] [Google Scholar]
Sieving 2011 {published and unpublished data}
- Sieving RE, McMorris BJ, Beckman KJ, Pettingell SL, Secor‐Turner M, Kugler K, et al. Prime Time: 12‐month sexual health outcomes of a clinic‐based intervention to prevent pregnancy risk behaviors. Journal of Adolescent Health 2011;49(2):172‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sieving RE, McRee A, McMorris BJ, Beckman KJ, Pettingell SL, Bearinger LH, et al. Sexual Health Outcomes at 24 months for a Clinic‐Linked Intervention to Prevent Pregnancy Risk Behaviors. JAMA Pediatric 2013;167(4):333‐340. [DOI] [PMC free article] [PubMed] [Google Scholar]
Smith 1994 {published data only}
- Smith MAB. Teen incentives program: evaluation of a health promotion model for adolescent pregnancy prevention. Journal of Health Education 1994;25(1):24‐9. [DOI] [PubMed] [Google Scholar]
Stephenson 2004 {published data only}
- Stephenson JM, Strange V, Allen E, Copas A, Johnson A, Bonell C, et al. The long‐term effects of a peer‐led sex education programme (RIPPLE): a cluster randomised trial in schools in England. PLoS Medicine 2008;5(11):e224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephenson JM, Strange V, Oakley A, Copas A, Allen E, Babiker. Pupil‐led sex education in England (RIPPLE study): cluster randomised intervention trial. Lancet 2004;364:338‐46. [DOI] [PubMed] [Google Scholar]
Villarruel 2006 {published data only}
- Villarruel AM, Jemmott JB, Jemmott LS. A randomized controlled trial testing an HIV prevention intervention for Latino youth. Arch Pediatr Adolesc Med 2006;160:772‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Walker 2006 {published data only}
- Walker D, Gutierrez JP, Torres P, Bertozzi SM. HIV prevention in Mexico schools; prospective randomized evaluation of intervention. BMJ 2006;332:1189‐94. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wight 2002 {published data only}
- Wight D, Raab GM, Henderson M, Abraham C, Buston K, Hart G, et al. Limits of teacher delivered sex education: interim behavioural outcomes from randomized trial. BMJ 2002;324:1430‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Agha 2002 {published data only}
- Agha S. An evaluation of the effectiveness of a peer sexual health intervention among secondary‐school students in Zambia. AIDS 2002;14(4):269‐81. [DOI] [PubMed] [Google Scholar]
Amin 2004 {published data only}
- Amin R, Sato T. Impact of a school‐based comprehensive program for pregnant teens on their contraceptive use, future contraceptive intention, and desire for more children. Journal of Community Health Nursing 2004;21(1):39‐47. [DOI] [PubMed] [Google Scholar]
Antunes 2002 {published data only}
- Antunes MC, Peres CA, Paiva V, Stall R, Hearst N. Differences in AIDS prevention among young men and women of public schools in Brazil. Revista de Saúde Pública 2002;36(4 suppl):88‐95. [PubMed] [Google Scholar]
Barlow 2006 {published data only}
- Barlow A, Varipatis‐Baker E, Speakman K, Ginsburg G, Friberg I, Goklish N, et al. Home‐visiting intervention to improve child care among American Indian adolescent mothers. Archives of Pediatrics and Adolescent Medicine 2006;160:1101‐7. [DOI] [PubMed] [Google Scholar]
Barnet 2009 {published data only}
- Barnet B, Liu J, DeVoe M, Duggan AK, Gold MA, Pecukonis E. Motivational intervention to reduce rapid subsequent births to adolescent mothers: a community‐based randomized trial. Annals of Family Medicine 2009;7(5):436‐45. [DOI] [PMC free article] [PubMed] [Google Scholar]
Barnet 2010 {published data only}
- Barnet B, Rapp T, DeVoe M, Mullins CD. Cost‐effectiveness of a motivational intervention to reduce rapid repeated childbearing in high‐risk adolescent mothers: a rebirth of economic and policy considerations. Archives of Pediatrics and Adolescent Medicine 2010;164(4):370‐6. [DOI] [PubMed] [Google Scholar]
Bonell 2005 {published data only}
- Bonell C, Allen E, Strange V, Copas A, Oakley A, Stephenson J, et al. The effect of dislike of school on risk of teenage pregnancy: testing of hypotheses using longitudinal data from a randomized trial of sex education. Journal of Epidemiology and Community Health 2005;59:223‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bouris 2010 {published data only}
- Bouris A, Guilamo‐Ramos V, Jaccard J, McCoy W, Aranda D, Pickard A, et al. The feasibility of a clinic‐based parent intervention to prevent HIV, sexually transmitted infections, and unintended pregnancies among latino and African American adolescents. AIDS Patient Care STDS 2010;24(6):381‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Boyer 2005 {published data only}
- Boyer CB, Shafer M, Shaffer RA, Brodine SK, Pollack LM, Betsinger K, et al. Evaluation of a cognitive ‐ behavioural, group, randomized controlled intervention trial to prevent sexually transmitted infections and unintended pregnancies in young women. Preventive Medicine 2005;40:420‐31. [DOI] [PubMed] [Google Scholar]
Brinkman 2010 {published data only}
- Brinkman SA, Johnson SE, Lawrence D, Codde JP, Hart MB, Straton JAY, et al. Study protocol for the evaluation of an Infant Simulator based program delivered in schools: a pragmatic cluster randomised controlled trial. Trials 2010;11(1):100. [DOI] [PMC free article] [PubMed] [Google Scholar]
Brown 2011 {published data only}
- Brown KE, Hurst KM, Arden MA. Improving adolescent contraceptive use: evaluation of a theory‐driven classroom‐based intervention. Psychology, Health & Medicine 2011;16(2):141‐55. [DOI] [PubMed] [Google Scholar]
Buston 2007 {published data only}
- Buston K, Williamson L, Hart G. Young women under 16 years with experience of sexual intercourse: who became pregnant?. Journal of Epidemiology and Community Health 2007;61:221‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cagampang 1997 {published data only}
- Cagampang HH, Barth RP, Korpi M, Kirby D. Education now and babies later (ENABL): life history of a campaign to postpone sexual involvement. Family Planning Perspectives 1997;29:109‐14. [PubMed] [Google Scholar]
Chesney 2003 {published data only}
- Chesney MA, Koblin BA, Barresi PJ, Husnik MJ, Celum CL, Colfax G, et al. An individually tailored intervention for HIV prevention: baseline data from the EXPLORe study. American Journal of Public Health 2003;93:933‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chung‐Park 2008 {published data only}
- Chung‐Park MS. Evaluation of a pregnancy prevention programme using the Contraceptive Behavior Change model. Journal of Advanced Nursing 2008;61(1):81‐91. [DOI] [PubMed] [Google Scholar]
Cowan 2008 {published data only}
- Cowan FM, Pascoe SJS, Langhaug LF, Dirawo J, Chidiya S, Jaffar S, et al. The Regai Dzive Shiri Project: a cluster randomised controlled trial to determine the effectiveness of a multi‐component community‐based HIV prevention intervention for rural youth in Zimbabwe – study design and baseline results. Tropical Medicine and International Health 2008;13(10):1235‐44. [DOI] [PubMed] [Google Scholar]
Crosby 2005 {published data only}
- Crosby RA, DiClemente RJ, Wingwood GM, Salazar LF, Rose E, Levine D, et al. Condom failure among adolescents: Implications for STD prevention. Journal of Adolescent Health 2005;36:534‐6. [DOI] [PubMed] [Google Scholar]
Danielson 1990 {published data only}
- Danielson R, Marcy S, Plunkett A, Wiest W, Greenlick MR. Reproductive health counselling for young men: what does it do?. Family Planning Perspectives 1990;22(3):115‐22. [PubMed] [Google Scholar]
Decat 2014 {published data only}
- Decat P, Meyer S, Jaruseviciene L, Orozco M, Ibarra M, Segura Z, et al. Sexual onset and contraceptive use among adolescents from poor neighbourhoods in Managua, Nicaragua. The European Journal of Contraception and Reproductive Health Care 2014;20(2):1‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Di 2004 {published data only}
- Noia J, Schinke SP, Pena JB, Schwinn TM. Evaluation of a brief computer‐mediated intervention to reduce HIV risk among early adolescent females. Journal of Adolescent Health 2004;35(1):62‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Diclemente 2001 {published data only}
- Diclemente RJ, Wingwood GM, Crosby R, Cobb BK, Harrington K, Davies SL. Parent‐adolescent communication and sexual risk behaviours among African American adolescent females. The Journal of Pediatrics 2001;32(2):407‐12. [DOI] [PubMed] [Google Scholar]
Doniger 2001 {published data only}
- Doniger AS, Adams E, Utter CA, Riley JS. Impact evaluation of the "Not Me, Not Now" abstinence‐oriented, adolescent pregnancy prevention communications program, Monroe County, New York. Journal of Health Communications 2001;6:45‐60. [DOI] [PubMed] [Google Scholar]
Dycus 1990 {published data only}
- Dycus S, Costner G. Healthy early‐adolescent development (11‐13 years olds): Implementing a human sexuality. Elementary School Guidance & Counselling 1990;25(1):46‐54. [Google Scholar]
East 2003 {published data only}
- East P, Kiernan E, Chavez G. An evaluation of California's adolescent sibling pregnancy prevention program. Perspectives on Sexual and Reproductive Health 2003;35(2):62‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Eisen 1985 {published data only}
- Eisen M, Zellman GL, McAlister AL. A health belief model approach to adolescents' fertility control: some pilot program findings. Health Education Quarterly 1985;12(2):185‐210. [DOI] [PubMed] [Google Scholar]
Eisen 1987 {published data only}
- Eisen M, Zellman GL. Changes in incidence of sexual intercourse of unmarried teenagers following a community‐based sex education program. The Journal of Sex Research 1987;23(4):527‐44. [Google Scholar]
El‐Bassel 2003 {published data only}
- El‐Bassel N, Witte SS, Guilbert L, Wu E, Chang M, Hill J, et al. The efficacy of a relationship‐based HIV/STD prevention program for heterosexual couples. American Journal of Public Health 2003;93:963‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ferguson 1998 {published data only}
- Ferguson SL. Peer counselling in a culturally specific adolescent pregnancy prevention program. Journal of Health Care for the Poor and Underserved 1998;9(3):323‐33. [DOI] [PubMed] [Google Scholar]
Fitzgerald 2002 {published data only}
- Fitzgerald SM, Jordan TR, Yoo LM, Hart R. Effectiveness of the responsible social values program for 6th grade students in one rural school district. Psychological Reports 2002;91:1129‐32. [DOI] [PubMed] [Google Scholar]
Gallegos 2008 {published data only}
- Gallegos EC, Villarruel AM, Loveland‐Cherry C, Ronis DL, Zhou Y. Intervention to reduce adolescents sexual risk behaviours: a randomized controlled trial. Salud Publica Mexico 2008;50:59‐66. [DOI] [PubMed] [Google Scholar]
Garbers 2012 {published data only}
- Garbers S, Meserve A, Kottke M, Hatcher R, Ventura A, Chiasson MA. Randomized controlled trial of a computer‐based module to improve contraceptive method choice. Contraception 2012;86(4):383‐90. [DOI] [PubMed] [Google Scholar]
Gaughran 2014 {published data only}
- Gaughran M, Asgary RJ. On‐site comprehensive curriculum to teach reproductive health to female adolescents in Kenya. Womens Health 2014;23(4):358‐64. [DOI] [PubMed] [Google Scholar]
Guilamo‐Ramos 2011a {published data only}
- Guilamo‐Ramos V, Jaccard J, Dittus P, Bouris A, Gonzalez B, Casillas E, et al. A comparative study of interventions for delaying the initiation of sexual intercourse among Latino and Black youth. Perspectives on Sexual and Reproductive Health 2011;43(4):247‐54. [DOI] [PubMed] [Google Scholar]
Harvey 2004 {published data only}
- Harvey SM, Henderson JT, Thorburn S, Casillas A, Mendez L, Cervantes R. A randomized study of a pregnancy and disease prevention intervention for Hispanic couples. Perspectives on Sexual and Reproductive Health 2004;36(4):162‐9. [DOI] [PubMed] [Google Scholar]
Havens 1997 {published data only}
- Havens KK, Wagstaff DA, Mercer PA, Longeway K, Gutman M. Lessons learned from a mentoring program for teenage mothers. Wisconsin Medical Journal 1997;96(9):38‐43. [PubMed] [Google Scholar]
Howard 1990 {published data only}
- Howard M, McCabe JB. Helping teenagers postpone sexual involvement. Family Planning Perspectives 1990;22(1):21‐7. [PubMed] [Google Scholar]
Hutchinson 2003 {published data only}
- Hutchinson MK, Jemmott JB, Jemmott LS, Braverman P, Fong GT. Role of a mother‐daughter sexual risk communication in reducing sexual risk behaviours among urban adolescent females: a prospective study. Journal of Adolescent Health 2003;33:98‐107. [DOI] [PubMed] [Google Scholar]
James 2005 {published data only}
- James S, Reddy PS, Ruiter RAC, Taylor M, Jinabhai CC, Empelen P, et al. The effects of a systematically developed photo‐novella on knowledge, attitudes, communication and behavioural intention with respect to sexually transmitted infections among secondary school learners in South Africa. Health Promotion International 2005;20(2):157‐65. [DOI] [PubMed] [Google Scholar]
Jay 1984 {published data only}
- Jay MS, DuRant RH, Shoffitt T, Linder CW, Litt IF. Effect of peer counselors on adolescent compliance in use of oral contraceptive. Pediatrics 1984;73(2):126‐31. [PubMed] [Google Scholar]
Jennings 2014 {published data only}
- Jennings JM, Howard S, Perotte CL. Effects of a school‐based sexuality education program on peer educators: the Teen PEP model. Health Education Research 2014;29(2):319‐29. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jewkes 2006 {published data only}
- Jewkes R, Nduna M, Levin J, Jama N, Dunkle K, Khuzwayo N, et al. A cluster randomized controlled trial to determine the effectiveness of stepping stones in preventing HIV infections and promoting safer sex sexual behaviours amongst youth in the rural Eastern Cape, South Africa: trial design, methods and baseline findings. Tropical Medicine and International Health 2006;11(1):3‐16. [DOI] [PubMed] [Google Scholar]
Kaljee 2005 {published data only}
- Kaljee LM, Genberg B, Riel R, Cole M, Tho le H, Thoa le TK, et al. Effectiveness of a theory‐based risk reduction HIV prevention program for Vietnamese adolescents. AIDS education and prevention 2005;17(3):185‐99. [DOI] [PubMed] [Google Scholar]
Kamali 2002 {published data only}
- Kamali A, Kinsman J, Nalweyiso N, Mitchell K, Kanyesigye E, Kengeya‐Kayondo JF, et al. A community randomized controlled trial to investigate impact of improved STD management and behavioural interventions on HIV incidence in rural Masaka, Uganda: trial design, methods and baseline findings. Tropical Medicine and International Health 2002;7(12):1053‐63. [DOI] [PubMed] [Google Scholar]
Katz 2011 {published data only}
- Katz KS, Rodan M, Milligan R, Tan S, Courtney L, Gantz M, et al. Efficacy of a randomized cell phone‐based counseling intervention in postponing subsequent pregnancy among teen mothers. Maternal and Child Health Journal 2011;15 Suppl 1:S42‐53. [DOI] [PubMed] [Google Scholar]
Kirby 2002a {published data only}
- Kirby D. Effective approaches to reducing adolescent unprotected sex, pregnancy and childbearing. The Journal of Sex Research 2002;39(1):51‐7. [DOI] [PubMed] [Google Scholar]
Kirby 2002c {published data only}
- Kirby D. The impact of schools and school programs upon adolescent sexual behaviour. The Journal of Sex Research 2002;39(1):27‐33. [DOI] [PubMed] [Google Scholar]
Kuroki 2008 {published data only}
- Kuroki LM, Allsworth JE, Redding CA, Blume JD, Peipert JF. Is a previous unplanned pregnancy a risk factor for a subsequent unplanned pregnancy?. American Journal of Obstetrics and Gynecology 2008;199:517.e1‐517.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kyrychenko 2006 {published data only}
- Kyrychenko P, Kohler C, Sathiakumar N. Evaluation of a school‐based HIV/AIDS educational intervention in Ukraine. Journal of Adolescent Health 2006;39:900‐7. [DOI] [PubMed] [Google Scholar]
Legardy 2005 {published data only}
- Legardy JK, Macaluso M, Artz L, Brill I. Do participants' characteristics influence the effectiveness of behavioural intervention? Promoting condom use of women. Sexually Transmitted Diseases 2005;32(1):665‐71. [DOI] [PubMed] [Google Scholar]
Liberman 2000 {published data only}
- Liberman LD, Gray H, Wier M, Fiorentino R, Maloney P. Long‐term outcomes of an abstinence‐based small‐group pregnancy prevention program in New York City schools. Family Planning Perspectives 2000;32(5):237‐45. [PubMed] [Google Scholar]
Magnani 2005 {published data only}
- Magnani R, MacIntyre K, Karim AM, Brown L, Hutchinson P. The impact of life skills education on adolescent sexual risk behaviours in KwaZulu‐Natal, South Africa. Journal of Adolescent Health 2005;36:289‐304. [DOI] [PubMed] [Google Scholar]
Martiniuk 2003 {published data only}
- Martiniuk ALC, O'Connor KS, King WD. A cluster randomized trial of sex education programme in Belize, Central America. International Journal of Epidemiology 2003;32:131‐6. [DOI] [PubMed] [Google Scholar]
Matteson 2006 {published data only}
- Matteson KA, Peipert JF, Allsworth J, Phipps MG, Redding CA. Unplanned pregnancy. Does past experience influenced use of a contraceptive method?. Obstetrics & Gynecology 2006;107(1):121‐7. [DOI] [PubMed] [Google Scholar]
McBride 2000 {published data only}
- McBride D, Glenapp A. Using randomized designs to evaluate client‐centered programs to prevent adolescent pregnancy. Family Planning Perspectives 2000;32(5):227‐35. [PubMed] [Google Scholar]
Metcalf 2005 {published data only}
- Metcalf CA, Malotte CK, Douglas JM, Paul SM, Dillon BA, Cross H, et al. Efficacy of a booster counselling session 6 months after HIV testing and counselling. A randomized controlled trial (RESPECT‐2). Sexually Transmitted Diseases 2005;32(2):123‐9. [DOI] [PubMed] [Google Scholar]
Mitchell 2014 {published data only}
- Mitchell EM, Heumann S, Araujo A, Adesse L, Halpern CT. Brazilian adolescents' knowledge and beliefs about abortion methods: a school‐based internet inquiry. BMC Women's Health 2014;14:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
O'Donnell 2005 {published data only}
- O'Donnell L, Stueve A, Agranick G, Wilson‐Simmons R, Duran R, Jeanbaptistie V. Saving sex for later: an evaluation of a parent education intervention. Perspectives on Sexual and Reproductive Health 2005;37(4):166‐73. [DOI] [PubMed] [Google Scholar]
Ochiogu 2011 {published data only}
- Ochiogu IN, Miettola J, Ilika AL, Vaskilampi T. Impact of timing of sex education on teenage pregnancy in Nigeria: cross‐sectional survey of secondary school students. Journal of Community Health 2011;36(3):375‐80. [DOI] [PubMed] [Google Scholar]
Olsen 1991 {published data only}
- Olsen JA, Weed SE. The effects of three abstinence sex education programs on student attitudes toward sexual activity. Adolescence 1991;26(103):631‐42. [PubMed] [Google Scholar]
Padian 2007 {published data only}
- Padian NS, Straten A, Ramjee G, Chipato T, Bruyn G, Blanchard K, et al. Diaphragm and lubricant gel for prevention of HIV acquisition in Southern African women: a randomized controlled trial. Lancet 2007;370:251‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]
Peipert 2008 {published data only}
- Peipert JF, Redding CA, BLume JD, Allsworth JE, Matteson KA, Lozowski F, et al. Tailored intervention to increase dual‐contraceptive method use: a randomized trial to reduce unintended pregnancies and sexually transmitted infections. American Journal of Obstetrics and Gynecology 2008;198:630.e1‐630.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Peipert 2011 {published data only}
- Peipert JF, Zhao Q, Meints L, Peipert BJ, Redding CA, Allsworth JE. Adherence to dual‐method contraceptive use. Contraception 2011;84(3):252‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Peipert 2012 {published data only}
- Peipert JF, Madden T, Allsworth JE, Secura GM. Preventing unintended pregnancies by providing no‐cost contraception. Obstetrics & Gynecology 2012;120(6):1291‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Peragallo 2005 {published data only}
- Peragallo N, Deforge B, O'Campo P, Lee SM, Kim YJ, Cianelli R, et al. A randomized clinical trial of an HIV‐Risk reduction intervention among low income Latina women. Nursing research 2005;54(2):108‐18. [DOI] [PubMed] [Google Scholar]
Peterson 2007 {published data only}
- Peterson R, Albright J, Garrett JM, Curtis KM. Pregnancy and STD prevention counselling using an adaptation of motivational interviewing: a randomized controlled trial. Perspectives on Sexual and Reproductive Health 2007;39(1):21‐8. [DOI] [PubMed] [Google Scholar]
Proude 2004 {published data only}
- Proude EM, D'Este C, Ward JE. Randomized trial in family practice of a brief intervention to reduce STI risk in young adults. Family Practice 2004;21(5):537‐44. [DOI] [PubMed] [Google Scholar]
Rickert 2007 {published data only}
- Rickert VI, TIezzi L, Lipshutz J, Leon J, Vaughan RD, Westhoff C. Depo Now: preventing unintended pregnancies among adolescent and young adults. Journal of Adolescent Health 2007;40:22‐8. [DOI] [PubMed] [Google Scholar]
Robin 2004 {published data only}
- Robin L, Dittus P, Whitaker D, Crosby R, Ethier K, Mezoff J, et al. Behavioural interventions to reduce incidence of HIV, STD and pregnancy among adolescents: a decade in review. Journal of Adolescent Health 2004;34:3‐26. [DOI] [PubMed] [Google Scholar]
Schreiber 2010 {published data only}
- Schreiber CA, Ratcliffe SJ, Barnhart KT. A randomized controlled trial of the effect of advanced supply of emergency contraception in postpartum teens: a feasibility study. Contraception 2010;81(5):435‐40. [DOI] [PubMed] [Google Scholar]
Schwarz 2008 {published data only}
- Schwarz EB, Gerbert B, Gonzales R. Computer‐assisted provision of emergency contraception a randomized controlled trial. Journal of General and Internal Medicine 2008;23(6):794‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Secura 2014 {published data only}
- Secura GM. Adams T, Buckel CM, Zhao QH, Peipert JF. Change in sexual behavior with provision of no‐cost contraception. Obstetrics and Gynecology 2014;123(4):771‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shuey 1999 {published data only}
- Shuey DA, Babishangire BB, Ominat S, Bagarukayo H. Increased sexual abstinence among in‐school adolescents as a result of school health education in Soroti district, Uganda. Health Education Research 1999;14(3):411‐9. [DOI] [PubMed] [Google Scholar]
Sieving 2012 {published data only}
- Sieving RE, Bernat DH, Resnick MD, Oliphant J, Pettingell S, Plowman S, et al. A clinic‐based youth development program to reduce sexual risk behaviors among adolescent girls: prime time pilot study. Health Promotion Practice 2012;13(4):462‐71. [DOI] [PubMed] [Google Scholar]
Silva 2002 {published data only}
- Silva M. The effectiveness of school‐based sex education programs in the promotion of abstinent behaviour: a meta‐analysis. Health Education Research 2002;17(4):471‐81. [DOI] [PubMed] [Google Scholar]
Stout 1989 {published data only}
- Stout JW, Rivara FP. Schools and sex education: does it work?. Pediatrics 1989;83(3):375‐9. [PubMed] [Google Scholar]
Thato 2008 {published data only}
- Thato 2008, Jenkins RA, Dusitsin N. Effects of the culturally‐sensitive comprehensive sex education programme among Thai secondary school students. Journal of Advanced Nursing 2008;62(4):457‐69. [DOI] [PubMed] [Google Scholar]
Thomas 2000 {published data only}
- Thomas MH. Abstinence‐based programs for prevention of adolescent pregnancies. Journal of Adolescent Health 2000;26:5‐17. [DOI] [PubMed] [Google Scholar]
Thomas 2004 {published data only}
- Thomas DV, Looney SW. Effectiveness of a comprehensive psychoeducation intervention with pregnant and parenting adolescents: a pilot study. Journal of Child and Adolescent Psychiatric Nursing 2004;17(2):66‐77. [DOI] [PubMed] [Google Scholar]
Tingle 2002 {published data only}
- Tingle LR. Evaluation of the North Carolina "Baby Think it Over" Project. (Research Paper). Journal of School Health 2002;75(5):178(6). [DOI] [PubMed] [Google Scholar]
Van 1985 {published data only}
- Van D, Leslie J. Use of nurse‐client contracting to reduce risk of unintended pregnancy in an adolescent population. The American Public Health Association Annual Meeting 1985.
Van Devanter 2002 {published data only}
- Devanter N, Gonzales V, Merzel C, Parikh NS, Celantano D, Greenberg J. Effect of an STD/HIV behavioural intervention on women's use of the female condom. American Journal of Public Health 2002;92:109‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wiggins 2009 {published data only}
- Wiggins M, Bonell C, Sawtell M, Austerberry H, Burchett H, Allen E, et al. Health outcomes of youth development programme in England: prospective matched comparison study. BMJ 2009;339:b2534. [DOI] [PMC free article] [PubMed] [Google Scholar]
Yoo 2004 {published data only}
- Yoo S, Johnson CC, Rice J, Manuel P. A qualitative evaluation of the Students of Service (SOS) program for sexual abstinence in Louisiana. Journal of School Health 2004;74(8):329‐34. [DOI] [PubMed] [Google Scholar]
Zabin 1986 {published data only}
- Zabin LS, Hirsch MB, Smith EA, Streett R, Hardy JB. Evaluation of a pregnancy prevention program for urban teenagers. Family Planning Perspectives 1986;183(3):119‐26. [PubMed] [Google Scholar]
Zabin 1988 {published data only}
- Zabin LS, Hirsch MB, Smith EA, Smith M, Emerson MR, King TM, et al. The Baltimore pregnancy prevention program for urban teenagers: II. what did it cost?. Family Planning Perspectives 1988;20(4):188‐92. [PubMed] [Google Scholar]
Zimmerman 2008 {published data only}
- Zimmerman RS, Cupp PK, Donohew L, Sionean CK, Feist‐Price S, Helme D. Effects of a school‐based, theory‐driven HIV and Pregnancy prevention curriculum . Perspectives on Sexual and Reproductive Health 2008;40(1):42‐51. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Murray 2015 {published data only}
- Murray PJ, Ashcraft AM, Downs J. Can you get an STI from a virgin? The answer might surprise you: Intervention improves knowledge about sexual risk perception. Journal of Pediatric Adolescent Gynecology (Poster Abstracts) 2015; Vol. 28:e41‐e78.
Shafii 2014 {published data only}
- Shafii T, Benson SK, Morrison DM, Hughes JP, Golden MR, Holmes KK. Results from ekiss (electronic kiosk intervention for safer‐sex): A pilot randomized controlled trial to test an interactive computer‐based intervention for sexual health in adolescents and young adults. Journal of Adolescent Health 2014;54(2 Suppl. 1):S10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Adam 2004
- Adams G, Gulliford MC, Ukoumunne OC, Eldridge S, Chinn S, Campbell MJ. Patterns of intra‐cluster correlation from primary care research to inform study design and analysis. Journal of Clinical Epidemiology 2004;57:785‐94. [DOI] [PubMed] [Google Scholar]
Antman 1992
- Antman EM, Lau J, Kupelnick B, Mostellar F, Chalmers TC. A comparison of results of meta‐analyses of randomized control trials and recommendations of clinical experts. Journal of the American Medical Association 1992;268:240‐8. [PubMed] [Google Scholar]
Burt 1986
- Burt MR. Estimating the public cost of teenage childbearing. Family Planning Perspective 1986;18:221‐6. [PubMed] [Google Scholar]
Burt 1990
- Burt MR. Public cost and policy implications of teenage childbearing. Adv Adolescent Mental Health 1990;4:265‐80. [PubMed] [Google Scholar]
Clark 2004
- Clark M, Oxman MD. Cochrane Reviewers' Handbook. The Cochrane Library [database on disk and CDROM]. Oxford, 2004, issue 3.
Cook 1993
- Cook DJ, Guyatt GH, Ryan G, Clifton J, Buckingham L, Willan A, et al. Should unpublished data be included in meta‐analyses? Current convictions and controversies. JAMA 1993;269:2749‐53. [PubMed] [Google Scholar]
Coyle 2001
- Coyle KK, Basen‐Enquist KM, Kirby DB, Parcel GS, Banspach SW, Collins JL, et al. Safer choices: reducing teen pregnancy, HIV and STDs. Public Health Reports 2001;1(16):82‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Deeks 2011
- Deeks JJ, Higgins JPT, Altman DG (editors). Chapter 9: Analysing data and undertaking meta‐analyses. In: Higgins JPT, Green S (editors).Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
DeLamater 2000
- Delamater J, Wagstaff DA, Havens KK. The impact of a culturally appropriate STD/AIDS education intervention on black male adolescents' sexual and condom use behaviour. Health Education and Behaviour 2000;27(4):453‐69. [DOI] [PubMed] [Google Scholar]
Denny 2006
- Denny G, Young M. An evaluation of an abstinence‐only sex education curriculum: an 18‐months follow‐up. Journal of School Health 2006;76(8):414‐22. [DOI] [PubMed] [Google Scholar]
DiCenso 2002
- DiCenso A, Guyatt G, Willan A, Griffith L. Interventions to reduce unintended pregnancies among adolescents: systematic review of randomized controlled trials. BMJ 2002;342:1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dickersin 1990
- Dickersin K. The existence of publication bias and risk factors for its occurrence. JAMA 1990;263:1385‐9. [PubMed] [Google Scholar]
Elfebein 2003
- Elfebein DS, Felice ME. Adolescent pregnancy. Pediatric Clinics of North America 2003;50(4):781‐800. [DOI] [PubMed] [Google Scholar]
Finer 2006
- Finer LB, Zolna MR. Unintended pregnancy in the United States: incidence and disparities. Contraception 2006;84(5):478–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Franklin 1997
- Franklin C, Grant D, Corcoran J, Miller P, Bultman L. Effectiveness of prevention programs for adolescent pregnancy: a meta‐analysis. Journal of Marriage and Family 1997;59:551‐67. [Google Scholar]
Fullerton 1997
- Fullerton D, Dickson R, Eastwood AJ, Sheldon TA. Preventing unintended teenage pregnancies and reducing their adverse effects. Quality in Health Care 1997;6(2):102‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Grossman 1992 [Computer program]
- Grossman JB, Sipe CL. Summer training and Education Program (STEP): Report on long‐term impacts. Philadelphia: Public/Private Ventures, 1992.
Hamilton 2014
- Hamilton BE, Martin JA, Osterman MJK, Curtin SC. Birth: Preliminary Data for 2013 National Vital Statistics Reports. Vol. 63, Hyattsville, Maryland: National Center for Health Statistics., May 29, 2014. [Google Scholar]
Haveman 1997
- Haveman RH, Wolfe B, Peterson E. Children of early childbearers as young adults. In: In R.A. Maynard editor(s). Kids having kids: economic costs and social consequences of teen pregnancy. New York: The Robin Hood Foundation, 1997. [Google Scholar]
Helmerhorst 2004
- Helmerhorst F, Helmerhorst A. Cochrane Fertility Regulation Group. In: The Cochrane Library, Issue 3, 2004. Chichester, UK: John Wiley & Sons, Ltd.
Henshaw 2000
- Henshaw SK, Feivelson DJ. Teenage abortion and pregnancy statistics by state. Family Planning Perspectives 2000;32(6):272‐80. [PubMed] [Google Scholar]
Higgins 2011a
- Higgins JPT, Altman DG, Sterne JAC (editors). Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S (editors).Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Higgins 2011b
- Higgins JPT, Deeks JJ, Altman DG (editors). Chapter 16: Special topics in statistics. In: Higgins JPT, Green S (editors), Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Higgins 2011c
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011.. Available from www.cochrane‐handbook.org.
Hollis, 1999
- Hollis S, Campbell F. What is meant by intention‐to‐treat analysis?. BMJ 1999;319:670‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kirby 2002b
- Kirby D. Antecedents of adolescent initiation of sex, contraceptive use, and pregnancy. American Journal of Health Behavior 2002;26(6):473‐85. [DOI] [PubMed] [Google Scholar]
Klerman 2002
- Klerman LV. Adolescent pregnancy in the United States. International Journal of Adolescent Medical Health 2002;14(2):91‐6. [DOI] [PubMed] [Google Scholar]
Koniak‐Griffin 2001
- Koniak‐Griffin D, Turner‐Pluta C. Health risks and psychosocial outcomes of early childbearing: a review of the literature. Journal of Perinatal and Neonatal Nursing 2001;15(2):1‐17. [DOI] [PubMed] [Google Scholar]
Kosunen 2002
- Kosunen EA, Vikat A, Gissler M, Rimpela. Teenage pregnancies and abortions in Finland in the 1990s. Scandinavian Journal of Public Health 2002;30(4):300‐5. [DOI] [PubMed] [Google Scholar]
Lindberg 2006
- Lindberg LD, Frost JJ, Sten C, Dailard C. Provision of contraceptive and related services by publicly funded family planning clinics. Perspectives on Sexual and Reproductive Health 2006;38(3):139‐47. [DOI] [PubMed] [Google Scholar]
Maness 2013
- Maness SB, Buhi ER. A systematic review of pregnancy prevention programs for minority youth in the US: a critical analysis and recommendations for improvement. Journal of Health Disparities Research and Practice 2013;6(2):91‐106. [Google Scholar]
Manlove 2002
- Manlove J, Terry‐Humen E, Papillo RA, Franzentta K, Williams S, Ryan S. Preventing teenage pregnancy, childbearing and STDs [What the Research Shows]. Child Trends Research Brief 2002.
Maynard 1996
- Maynard RA. Kids having kids: A Robin Hood Foundation special report on the costs of adolescent childbearing. New York: Robin Hood Foundation, 1996. [Google Scholar]
Mehra 2004
- Mehra S, Agrawal D. Adolescent health determinants for pregnancy and child health outcomes among the urban poor. Indian Journal of Pediatrics 2004;41(2):137‐45. [PubMed] [Google Scholar]
Monea 2011
- Monea E, Thomas A. The high cost of unintended pregnancy. CCF Briefs #45 July 2011.
Moore 1993
- Moore KA, Myers DE, Morrison DR, Winquist Nord C, Brown B, Edmonston B. Age at first childbirth and later poverty. Journal of Research on Adolescence 1993;3:393‐422. [DOI] [PubMed] [Google Scholar]
Nelson 1990
- Nelson PB. Repeat pregnancy among adolescent mothers: a review of the literature. Journal of the National Black Nurses Association 1990;4(1):28‐34. [PubMed] [Google Scholar]
NRC 1987
- National Research Council. Risking the future: adolescent sexuality, pregnancy, and childbearing. Cheryl D. Hayes. Washington DC: National Academy Press, 1987. [PubMed] [Google Scholar]
O'Donnell 2003 [Computer program]
- O'Donnell L, Doval A.S, Duran R, Haber D, Atnafou R, Piessens P, et al. Reach for health: a school sponsored community youth service intervention for middle school students.. Los Altos, CA:Sociometrics, 2003.
Orr 1996
- Orr DP, Langefeid CD, Katz BP, Caine VA. Behavioural intervention to increase condom use among high‐risk female adolescents. Journal of Pediatrics 1996;128(2):288‐95. [DOI] [PubMed] [Google Scholar]
Oxman 1993
- Oxman AD, Guyatt GH. The science of reviewing research. Annals of the New York Academy of Science 1993;703:125‐33. [DOI] [PubMed] [Google Scholar]
Pettinato 2003
- Pettinato A, Emans SJ. New contraceptive methods: update 2003. Current Opinion in Pediatrics 2003;15(4):362‐9. [DOI] [PubMed] [Google Scholar]
Philliber 1992
- Philliber S, Allen JP. Life options and community service: teen outreach program [Miller BC, Card JJ, Paikoff RL and Peteson JL (Eds)]. Prevention adolescent pregnancy. Newburg Park, CA: Sage Publications, 1992:139‐155. [Google Scholar]
Phipps 2002
- Phipps MG, Blume JD, DeMonner SM. Young maternal age associated with increased risk of post‐neonatal death. Obstetrics and Gynecology 2002;100(3):481‐6. [DOI] [PubMed] [Google Scholar]
Raine 2000
- Raine T, Harper C, Leon K, Darney P. Emergency contraception: advance provision in a young, high‐risk clinic population. Obstetrics and Gynecology 2000;96(1):1‐7. [DOI] [PubMed] [Google Scholar]
Rao 1992
- Rao JN, Scott AJ. A simple method for analysis of clustered binary data. Biometrics 1992;48(2):577‐85. [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rich‐Edwards 2002
- Rich‐Edwards J. Teen pregnancy is not a public health crisis in the United States: it is time we made it one. International Journal of Epidemiology 2002;31:555‐6. [DOI] [PubMed] [Google Scholar]
Schünemann 2011
- Schünemann HJ, Oxman AD, Vist GE, Higgins JPT, Deeks JJ, Glasziou P, et al. Chapter 12: Interpreting results and drawing conclusions. In: Higgins JPT, Green S (editors), Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Sikron 2003
- Sikron F, Wilf‐Miron R, Israeli A. Adolescent pregnancy in Israel: methodology for rate estimation and analysis of characteristics and trends. Harefuah 2003;142(2):131‐6. [PubMed] [Google Scholar]
St. Lawrence 2005
- St. Lawrence JS. Becoming a responsible teen: an HIV risk‐reduction program for adolescents. Scott valley, CA: ETR Associates 2005.
Sterne 2011
- Sterne JAC, Egger M, Moher D (editors). Chapter 10: Addressing reporting biases. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Intervention. Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Thomas 2009
- Thomas A, Monea E. FamilyScape: a simulation model of family formation. The Brookings Institution, Washington, D.C. 2009.
Thomas 2012
- Thomas A. Policy solutions for preventing unplanned pregnancy. Center on Children and Families at Brookings (CCF) Briefs March 2012.
Trussell 1997
- Trussell J, Koenig J, Stewart F, Darroch JE. Medical care cost savings from adolescent contraceptive use. Family Planning Perspectives 1997;29(6):248‐55, 295. [PubMed] [Google Scholar]
Upchurch 1990
- Upchurch DM, McCarthy JL. The timing of first birth and high school completion. American Sociological Review 1990;55:224‐34. [Google Scholar]
WHO 1980
- World Health Organization. Regional Working Group on health needs of adolescents: final report. WHO Document ICP/MCH/005. Manila: World Organization, Regional Office for the Western Pacific, 1980.
WHO 1995
- World Health Organization. World Health Report, 1995 ‐ Closing the gap. Geneva: World Health Organization, 1995.
World Bank 2014
- The World Bank. Adolescent fertility rate (births per 1000 women ages 15‐19). United Nations Population Division, World Population Prospects. The 2010 Revision 2011.


