Abstract
Background
This study examined the extent to which the network structure of anxiety and depression among adolescents identified during the peak of the COVID-19 pandemic could be cross-validated in a sample of adolescents assessed after the COVID-19 peak.
Methods
Two cross-sectional surveys were conducted between February 20 and 27, 2020 and between April 11 and 19, 2020, respectively. Depressive and anxiety symptoms were assessed using the 20-item Center for Epidemiological Studies-Depression and 7-item Generalized Anxiety Disorder, respectively. Anxiety-depression networks of the first and second assessments were estimated separately using a sparse Graphical Gaussian Model combined with the graphical least absolute shrinkage and selection operator method. A Network Comparison Test was conducted to assess differences between the two networks.
Results
The most central symptoms in the first and second survey networks were Depressed affect and Nervousness. Compared with connections in the first survey network, connections in the second survey network analysis between Relax-Nervousness–Depressed affect–Interpersonal problems (diff, contrast: second survey–first survey. diff=-0.04, P = 0.04; diff=-0.03, P = 0.03; diff=-0.03, P = 0.04), and Irritability–Somatic complaints (diff=-0.04, P = 0.02) were weaker while connections of Somatic complaints-Nervousness (diff=0.05, P<0.001), Somatic complaints–Depressed affect (diff=0.03, P = 0.009), and Irritability–Control worry–Restlessness (diff=0.02, P = 0.03; diff=0.05, P = 0.02) were stronger.
Conclusions
Depressed affect emerged as a robust central symptom and bridge symptom across Anxiety-Depression networks. Considering the negative impact of depression and anxiety on daily life, timely interventions targeting depressed affect should be implemented to reduce the co-occurrence of anxious and depressive symptoms among adolescents during the COVID-19 pandemic.
Keywords: Adolescent, Depression, Anxiety, COVID-19, Network analysis
1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic is a global health emergency (Eurosurveillance Editorial Team., 2020; Mattila et al., 2021). As of early 2021, COVID-19 has spread to more than 200 countries and territories, with more than 100 million confirmed cases (WorldoMeters, 2021). To control rapid transmission, a range of strategies has been implemented and includes mass lockdowns, home quarantines and school closures, all of which could have a negative impact on mental health of certain subpopulations including adolescents and their families (Ghosh, 2020; Golberstein et al., 2020; Guessoum et al., 2020; Zhu et al., 2020). Previous studies found depressive and anxiety symptoms were common in adolescents during the COVID-19 pandemic (Qi et al., 2020; Zhou et al., 2020a, 2020b). Although they are found in separate diagnostic categories (Zbozinek et al., 2012), depression and anxiety often occur together, particularly in children and adolescents (Melton et al., 2016), in part, because they have some causes in common. Considering the co-occurrence of depression and anxiety in different populations during the COVID-19 pandemic as well as exploring the pattern and relationship between anxious and depressive symptoms during different phases of pandemics may aid in explaining their negative impact on daily life and functional outcomes, developing effective preventive measures, and facilitating timely treatments.
In traditional approaches to understanding the psychopathology of depression and anxiety, symptoms are secondary to an underlying common cause (Borsboom, 2008; Schmittmann et al., 2013). For instance, depression causes dysphoric feelings, insomnia symptoms and impaired cognition in a manner similar to infections as a cause of fever. However, many studies have found that individual symptoms of a particular psychiatric diagnosis may be related to different risk factors or causes (Fried, 2015; Fried and Nesse, 2014; Kapur et al., 2012; Mamun et al., 2020; Wasserman et al., 2021). Furthermore, differences between individual symptoms and their associations with typical symptoms of other syndromes are not usually emphasized in traditional theories of psychopathology (Beard et al., 2016; Contreras et al., 2019).
Network analysis is a new approach to investigating complex, dynamic relationships between individual psychiatric symptoms (Fisher et al., 2017). This method is based on the premise that a particular psychiatric disorder is an interacting cluster of symptoms (Jones et al., 2019), and emphasis on understanding the strength and nature of associations among symptoms (Beard et al., 2016; Rouquette et al., 2018). In network analysis, nodes reflect psychiatric symptoms and edges between nodes reflect relationships between symptoms, including the activation spread from one symptom to other symptoms through the network (Borsboom, 2017; Rouquette et al., 2018). Nodes can also function as bridge symptoms that transfer symptom activation from one disorder to another disorder. Therefore, network analysis has utility in elucidating connection patterns between individual psychiatric symptoms and also between psychiatric disorders (Borsboom and Cramer, 2013).
Several past network analysis studies have examined the comorbidity of depression and anxiety. For example, one such study on generalized anxiety disorder and major depressive disorder found that fatigue, restlessness and sleep disturbances were key symptoms associated with the comorbid depression and anxiety (Cramer et al., 2010). Another study that examined the association between anxiety as measured by the 7-item Generalized Anxiety Disorder Scale (GAD-7) and depression as measured by the Patient Health Questionnaire-9 (PHQ-9), found that sad mood and worry were the most prominent central symptoms (i.e., those are most highly connected to other symptoms) in a large psychiatric sample (Beard et al., 2016).
Some network analysis studies have been conducted during the COVID-19 pandemic. A study examining changes of depressive and anxiety symptoms between the COVID-19 outbreak peak and its aftermath among Chinese adults (Wang et al., 2020) indicated symptoms of restlessness and an inability to relax had high centrality during the outbreak but gradually remitted after the peak. Furthermore, symptoms of irritability and loss of energy were bridge symptoms (i.e., symptoms that connect one psychiatric syndrome/disorder to another and may be important as targets of treatments intended to reduce or prevent comorbid problems) after the pandemic peak. However, because clinical features of depression and anxiety can be quite different between adolescents and adults (Nardi et al., 2013; Pyramid Healthcare, 2018; Rice et al., 2019), there is no clear basis for assuming findings of network analyses in adults during the COVID-19 pandemic are also applicable to adolescents who experience these symptoms. Furthermore, it is not clear whether network findings based on only one assessment are replicable or can be generalized over time or within other samples drawn from the same population. Toward addressing this limitation, cross-validation procedures designed to evaluate the stability of initial network models across two samples are one strategy that can be incorporated to clarify more versus less stable features of models generated in network analysis studies.
In sum, although network analysis has aided in elucidating links between psychiatric symptoms in adult samples, little is known about trajectories of individual depressive and anxiety symptoms among adolescents. Therefore, we conducted this study to characterize depressive and anxiety symptom clusters using network analysis and explored the extent to which a network model generated in one large adolescent sample during the COVID-19 outbreak peak could be replicated within another large adolescent sample shortly after the peak.
2. Methods
2.1. Settings and participants
Two national, cross-sectional surveys were undertaken by the National Clinical Research Center for Mental Disorders, China. The first survey was conducted between February 20 and 27 (peak of the COVID-19 outbreak) during which adolescents were required to stay at home due to nationwide lockdown measures (Peng et al., 2020; Sanchez-Caballero et al., 2020). The second survey was conducted between April 11 and 19, 2020 after the COVID-19 outbreak peak had remitted and during which schools in some provinces in China reopened (Xinhuanet, 2020). To reduce the risk of contagion, face-to-face interviews were not adopted. Following other studies (Liu et al., 2020b; Wang et al., 2020), data were collected through the WeChat-based QuestionnaireStar application using a snowball sampling method. WeChat is a widely used social communication application with 1.2 billion users in China, and is employed in most secondary schools nationwide for the online teaching. To be eligible for the research, participants were to be: (1) secondary school students aged between 11 and 20 years and (2) living in China during the COVID-19 outbreak. All participants and their guardians were required to provide written informed consent. This study was approved by the Medical Ethical Committee of Beijing Anding Hospital, Capital Medical University, China.
2.2. Measurements
Depressive symptoms were assessed with the self-report Center for Epidemiological Studies Depression Scale (CES-D) (Radloff, 1977); the CES-D has 20 items covering four clusters of symptoms: depressed affect (items 3, 6, 9, 10, 14, 17 and 18), positive affect (items 4, 8, 12 and 16), somatic complaints (items 1, 2, 5, 7, 11, 13 and 20), and interpersonal problems (items 15 and 19) (Nguyen et al., 2004; Radloff, 1977). Each item is scored from 0 (not at all) to 3 (a lot); total scores range from 0 to 60, with higher scores indicating more severe depressive symptoms. The Chinese version of the CES-D has satisfactory psychometric properties and has been widely used in adolescents (Guo et al., 2016; Sun et al., 2017; Zhou et al., 2020a).
Anxiety symptoms were measured using the 7-item self-report Generalized Anxiety Disorder Scale (GAD-7) (Spitzer et al., 2006). Each item is scored from 0 (not at all) to 3 (nearly every day). Total scores range from 0 to 21 and higher total scores indicate more severe anxiety symptoms. The Chinese version of GAD-7 has been validated with satisfactory psychometric properties in Chinese samples (He et al., 2010; Tong et al., 2016). Item content of the two scales is listed in Table S1.
2.3. Network estimation
Network analyses were conducted using bootnet (Epskamp et al., 2018a) and qgraph (Epskamp et al., 2012) packages in the R program (version 3.6.3). In network parlance, symptoms were nodes, while correlations between individual symptoms were edges (Beard et al., 2016; Wang et al., 2020). In this study, 11 nodes/symptoms were included: (1) 4 clusters of depressive symptoms (depressive nodes) as measured by the CES-D (i.e., Depressed, Positive, Somatic, and Interpersonal) and (2) 7 anxiety symptoms (anxiety nodes) as measured by the GAD-7 (i.e., Nervousness, Control Worry, Worry A Lot, Relax, Restlessness, Irritability, and Afraid). Pearson correlation analyses were used to estimate strengths of association between nodes, with thicker edges indicating stronger relationships.
To examine relationships between symptoms within networks during the COVID-19 outbreak, network models from the two surveys were estimated separately using sparse Graphical Gaussian Models (GGM) combined with a graphical least absolute shrinkage and selection operator (LASSO) method (Friedman et al., 2008); model selection was based on the Extended Bayesian Information Criterion (EBIC) (Chen and Chen, 2008). The GGM method was applied to construct network models. However, the approach can produce a large number of spurious edges due to latent variables (Epskamp et al., 2018b; Montazeri et al., 2020). To reduce the number of spurious edges and improve interpretability of results, network models were regularized using LASSO, a well-established algorithm for regularization that reduces weak associations to zero by removing them from models as potentially “false positive” edges (Epskamp et al., 2018a; Friedman et al., 2008; Heeren et al., 2018). EBIC is a widely used approach to model selection based on a tuning parameter (Epskamp, 2016; van Borkulo et al., 2015) that is usually set between 0 and 0.5. If the tuning parameter is close to 0.5, EBIC generates a simple model containing fewer edges; in contrast, if the tuning parameter is close to 0, EBIC generates a model with more edges (Epskamp et al., 2018a; Heeren et al., 2018). Following previous studies (Beard et al., 2016; Wang et al., 2020), the ‘estimateNetwork’ function in bootnet (Epskamp et al., 2018a) was used, with ‘EBICglasso’ as the default method and 0.5 as the default tuning parameter.
To assess the importance of each node in the network, centrality indices including Strength, Betweenness and Closeness were calculated (Borgatti, 2005; Freeman, 1978; Opsahl et al., 2010; Pan and Liu, 2020), using the ‘centralityPlot’ function in qgraph package (Epskamp et al., 2012) and normalized (z-scored) values were plotted for each node. Strength is the sum of absolute edge weights of all direct connections between a specific node and other nodes, reflecting the importance of an individual symptom in the network. Betweenness represents the frequency of a node that lies on all the shortest paths between other nodes, reflecting the importance of a symptom as a “connecter” to other symptoms. Closeness refers to the reciprocal of the sum of the shortest path distance of a specific node to all other nodes in a network, indicating the strength of a symptom's indirect connections to other symptoms (Dalege et al., 2017; Wang et al., 2020). Furthermore, to identify individual symptoms that act as pathways in links between depressive and anxious symptoms, bridge centrality indices (e.g., bridge strength, bridge closeness, and bridge betweenness) were measured using the ‘bridge’ function in networktools (Jones, 2021). Bridge centrality measures the importance of a node in linking its network to other networks (Jones et al., 2019; Wang et al., 2020).
2.4. Estimation of network stability
Following previous studies (Beard et al., 2016; Belvederi Murri et al., 2020; Wang et al., 2020), the accuracy and stability of networks were tested using R package bootnet (Epskamp et al., 2018a). First, to estimate the accuracy of edge weights, non-parametric bootstrapping (1000 replicates, 8 cores) was performed to compute 95% confidence intervals (CI) of edge values. Second, bootstrapped difference tests were used to determine significant differences between edge weights and node strengths. Finally, to determine the stability of centrality indices, case-dropping subset bootstrapping (1000 replicates, 8 cores) was performed to compute correlation stability coefficients (CS). A host of correlation values was calculated between centrality indices in the original sample and subset centrality based on different subsets of original samples (e.g., 95% of the sample, 80%, 70%, …, 25%) (Epskamp et al., 2018a; Hevey, 2018). CS represents the maximum proportion of cases that can be dropped from the original sample; for instance, with a 95% probability, correlation coefficients between centrality indices in the original networks and centrality indices in case-subset networks should reach at least 0.7 (default) (Epskamp et al., 2018a). The CS should not be lower than 0.25, and is recommended to be above 0.5 (Epskamp et al., 2018a).
2.5. Comparison of networks between the first and the second surveys
To assess differences between first versus second surveys, a Network Comparison Test (NCT) was conducted via the R package NetworkComparisonTest (van Borkulo et al., 2017). NCT is a two-tailed permutation method to test differences between two networks based on several invariance measures (i.e., global strength, network structure, and edge strength) (Dalege et al., 2017; van Borkulo et al., 2017). In this procedure, NCTs were run 1000 times and mean differences in global strength (the sum of absolute edge weights of the two networks were compared (Opsahl et al., 2010)). In addition, significant differences between two networks were estimated separately using a P<0.05 (two-tailed) level of significance.
2.6. Sensitivity analyses
In order to test the robustness of results across samples, a sensitivity analysis was conducted by repeating the network analyses after excluding data from those who participated in both surveys (n = 6719) from the second survey sample (i.e., group sampled after the COVID-19 peak had remitted).
3. Results
3.1. Participants
A total of 20,158 adolescents from mainland China was included in the final analysis; 9,553 adolescents participated in the first survey, with a mean age of 15.11 1.94 years. In the second survey, 10,605 adolescents completed the assessment; their mean age was 15.44 1.74 years. Table 1 shows the basic demographic characteristics of participants in each sample.
Table 1.
Demographic characteristics of survey samples.
| First Survey (N = 9553) | Second Survey (N = 10,605) | Second Survey1 (N = 3886) | ||||
|---|---|---|---|---|---|---|
| Age (mean, SD) | 15.11 | 1.94 | 15.44 | 1.74 | 15.79 | 1.60 |
| Female (n,%) | 4977 | 52.10 | 5708 | 53.80 | 2132 | 54.9 |
| Junior secondary school | 5459 | 57.10 | 4656 | 43.90 | 1262 | 32.5 |
| CES-D (mean, SD) | ||||||
| Depressed affect | 4.62 | 4.53 | 5.76 | 5.01 | 6.42 | 5.02 |
| Positive affect | 3.00 | 2.85 | 3.49 | 3.01 | 3.81 | 3.01 |
| Somatic complaints | 5.43 | 4.27 | 6.89 | 4.68 | 7.65 | 4.58 |
| Interpersonal problems | 1.01 | 1.48 | 1.23 | 1.56 | 1.41 | 1.60 |
| GAD total score (mean, SD) | 2.28 | 3.54 | 3.46 | 4.34 | 3.98 | 4.46 |
Note: 1 Based on a sensitivity analysis of the independent subgroup that completed only the second survey. CES-D, Center for Epidemiological Studies Depression Scale; GAD-7, 7-item Generalized Anxiety Disorder Scale. SD, standard deviation.
3.2. Network structures
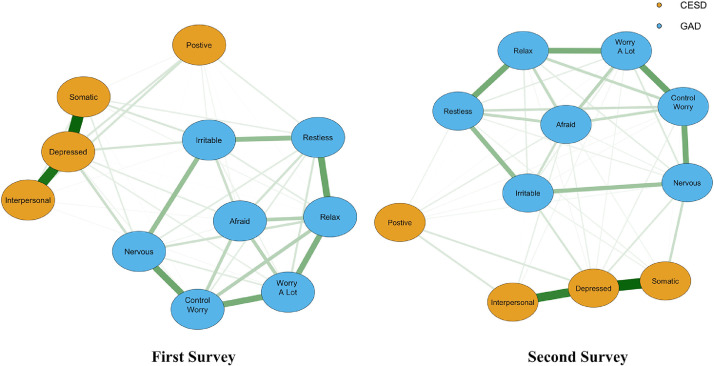
As shown in Fig. 1 , the first survey network (during the COVID-19 outbreak peak) of 11 nodes revealed that 48 of 55 edges were estimated to be above zero. Similarly, the second survey network (after the outbreak peak) of 11 nodes indicated 47 of 55 edges were estimated to be above zero. In both the first and second sample networks, the strongest edges between nodes of depression were for Depressed affect and Somatic complaints as well as Depressive affect and Interpersonal problems while the two strongest edges between nodes of anxiety were for (1) Relax and Restlessness, and (2) Nervousness and Control Worry. Bootstrapped confidence intervals for the edges (Figure S1) and correlation matrices (Table S2 and S3) are shown in Supplementary materials.
Fig. 1.
Symptom network of depressive and anxiety symptoms among adolescents during different stages of the COVID-19 outbreak. The first survey was conducted between February 20 and 27 (during the COVID-19 outbreak). The second survey was conducted between April 11 and 19 (after the COVID-19 outbreak). In the diagram symptom nodes with stronger connections are closer to each other. The orange nodes denote the CES-D factors; the blue nodes denote the GAD-7 items. The dark green lines represent positive correlations. The edge thickness represents the strength of the association between symptom nodes.
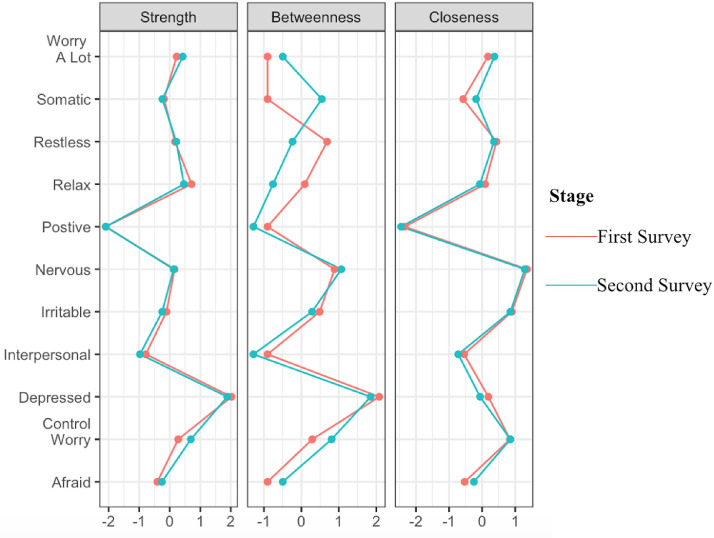
Fig. 2 shows centrality indices of all nodes as measured in the two surveys. Regarding closeness centrality in the first survey network, Nervousness was the strongest symptom connected with other nodes on the shortest path, followed by Irritability and Control Worry. Strength centrality data suggested that Depressed affect was the most central symptom, followed by anxiety symptoms of Relax and Control worry. Analyses of betweenness centrality identified Depressed affect as the node that most frequently lying on the shortest path between other nodes, followed by Nervousness, Restlessness and Irritability.
Fig. 2.
Centrality measures of all symptoms within the network at different stages of the COVID-19 outbreak. The figure shows centrality measures (i.e., strength, betweenness, and closeness) of all symptoms within the network (z-scores).
Similarly, in the second survey network, Nervousness was cross-validated as the node with the highest closeness centrality, followed by Irritability and Control Worry. Depressed affect was the node with the highest strength centrality, followed by Control worry and Relax. Replicating the initial network model, Depressed affect also had the highest betweenness centrality, followed by Nervousness; however, unlike the initial network model, Control worry had the highest betweenness centrality. Bridge centrality indices underscored Depressed affect as the node with the highest bridge strength and bridge betweenness while Nervousness had the highest bridge closeness across networks representing adolescent samples assessed during two stages of the COVID-19 outbreak (Figure S2).
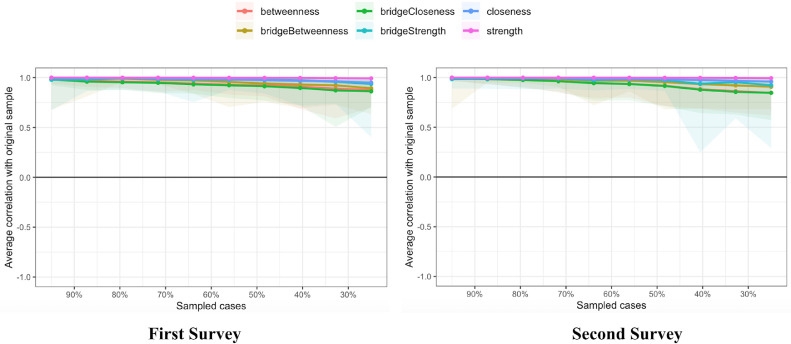
3.3. Network accuracy and stability
As shown in Fig. 3 , results of case-dropping subset bootstrapping indicated the strength, betweenness, closeness, bridge strength, bridge betweenness, and bridge closeness remained stable under various analysis conditions. CS coefficients for strength, betweenness and closeness were 0.75 in the first survey; 0.75, 0.67 and 0.75, respectively in the second survey. CS coefficients for bridge strength, bridge betweenness and bridge closeness were 0.75, 0.67 and 0.75, respectively in the first survey; 0.75, 0,67 and 0.59, respectively in the second survey.
Fig. 3.
Stability of centrality indices by case dropping subset bootstrap. The x-axis represents the percentage of cases of original sample used at each step. The y-axis represents the average of correlations between the centrality indices from the original network and the centrality indices from the networks that were re-estimated after dropping increasing percentages of cases. Each line indicates the correlations of betweenness, strength, closeness, bridge betweenness, bridge strength, and bridge closeness, while areas indicate 95% CI.
Bootstrapped 95% CIs for edges at different stages of the COVID-19 outbreak were narrow and edge values were significantly higher than zero, indicating that the edges were stable (Figure S1). The bootstrapped difference test revealed that most of the edge weights and node strengths had statistically significant differences from one another in individual comparisons (Figure S3 and S4).
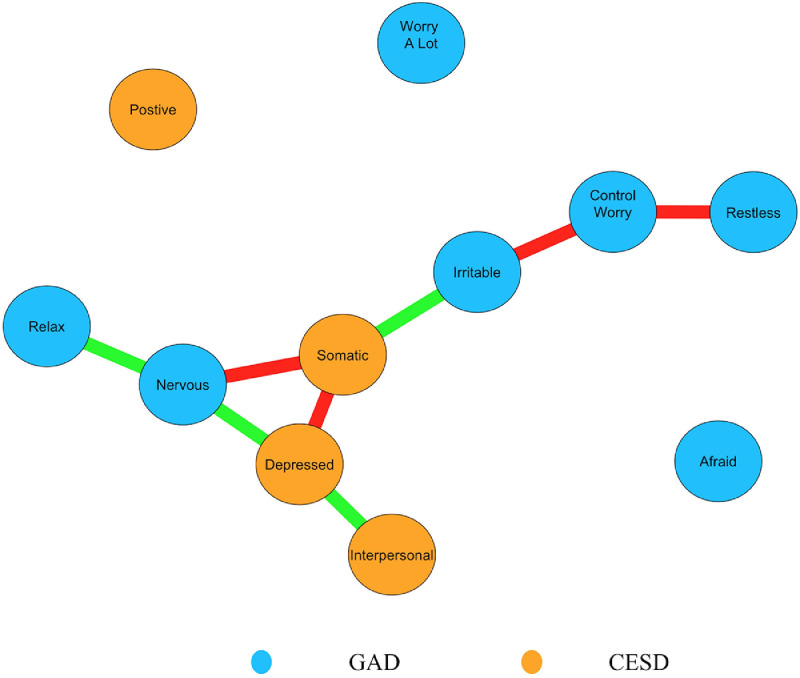
3.4. Network comparisons
Comparisons of the first versus the second surveys networks based on NCT results showed a significant difference in global strength (S = 0.09, P<0.001), but not network structure (M = 0.05, P = 0.22). Compared with the first survey network, the second survey network showed edge weight decreases for Relax- Nervousness – Depressed affect – Interpersonal problems (diff, contrast: second survey – first survey. diff=−0.04, P = 0.04; diff=−0.03, P = 0.03; diff=−0.03, P = 0.04), and Irritability – Somatic complaints (diff=−0.04, P = 0.02). Conversely, the second survey network revealed comparatively increased edge weights for Somatic complaints - Nervousness (diff=0.05, P<0.001), Somatic complaints – Depressed affect (diff=0.03, P = 0.009), and Irritability – Control worry – Restlessness (diff=0.02, P = 0.03; diff=0.05, P = 0.02) (Fig. 4 ).
Fig. 4.
Significant different edge between the two stages of the COVID-19 outbreak. The blue nodes denote the GAD-7 items, and the orange nodes denote the CES-D factors. Compared with the first survey, the second survey network showed the edge weights of Relax- Nervousness - Depressed affect - Interpersonal problems, and Irritability - Somatic complaint were significant decreased (light green lines). In contrast, Somatic complaint- Nervous, Somatic complaint - Depressed affect, and Irritability - Control worry - Restlessness were significant increased (red lines).
3.5. Sensitivity analysis
After excluding adolescents who completed both surveys from the second survey (i.e., those who joined both the first and second surveys), 9,553 adolescents from the first survey and 3,886 adolescents from the second survey were included in the sensitivity analysis. Replicating primary results based on the original sample, the strongest edges between nodes of depression in the second survey network (N = 3,886) were the connections of Depressed affect with Somatic complaints and Interpersonal problems, while the two strongest edges between nodes of anxiety were connections between Relax and Restlessness, and between Nervousness and Control Worry (Figure S5). Depressed affect had the strongest strength centrality and betweenness centrality; Nervousness had the highest closeness centrality (Figure S6). Further, compared with the network based on the first survey, the network based on the independent sample that completed only the second survey showed edge weight decreases for Restlessness – Interpersonal problems – Depressed affect (diff=−0.03, P = 0.008; diff=−0.05, P = 0.001), and Irritability – Somatic complaints (diff=−0.05, P = 0.03). Conversely, the edge weight of Irritability – Control worry (diff=0.06, P = 0.002) increased in the network based on the sample that completed only the second survey (Figure S7).
4. Discussion
Although numerous network studies have documented relations between psychiatric symptoms within a single sample or time point during the COVID-19 outbreak, it is not clear whether observed models are replicable across two samples drawn from the same population and assessed during different phases of the pandemic. To the best of our knowledge, this was the first network analysis study to investigate the stability of depressive and anxious symptom networks using cross-validation procedures within national samples of adolescents during different stages of the COVID-19 outbreak. In general, network structures were stable across samples assessed during and shortly following the COVID-19 outbreak peak, suggesting that symptom relations observed in the initial network model are similar across Chinese adolescent samples assessed during different pandemic phases.
Depressed affect emerged as the most prominent central and bridge symptom for adolescents across survey networks during and following the COVID-19 outbreak peak in China. These results are consistent with previous network analysis findings showing that depressed affect is also the central node in depression networks of adults (Fried et al., 2016; van Borkulo et al., 2015). Still other network analysis research on depression and anxiety during the pandemic also found that Depressed affect was the central symptom in nursing students (Bai et al., 2021) and the general population (Hoffart et al., 2021). Depressed affect is a hallmark characteristic of depression (Beard et al., 2016) that refers to a cluster of negative mood experiences such as sadness, feeling “blue”, depressed mood, fear, loneliness, crying spells, and perceptions of the self as a failure (Danhauer et al., 2013). Due to the COVID-19 outbreak peak, adolescents in China could not pursue many routine activities outside of the home such as schooling, social communications and physical activities; presumably disrupted routines and isolation increased the likelihood of depression in this group (Courtney et al., 2020; Liu et al., 2020a). Furthermore, extended homestays due to long-term quarantine measures during the pandemic, may have contributed to loneliness, increased stress, and fear that could increase risk for negative mood experiences such as depression and anxiety (Courtney et al., 2020; Guessoum et al., 2020; Qi et al., 2020). Previous studies have found that depressive affect is the common risk factor underlying comorbid emotional disorders including depression and anxiety (Conway et al., 2017; Mineka et al., 1998; Naragon-Gainey et al., 2016; Prenoveau et al., 2010). Such evidence may help to could account for depressed affect as the most prominent symptom linking depressive and anxious symptoms across two samples in this study.
Also underscoring the replicability of observed network model relations across different samples of Chinese adolescents, Depressed affect had its strongest associations with other depression nodes reflecting somatic complaints and interpersonal problems across both surveys during the COVID-19 outbreak. Select past studies have found that both depressed affect and stressful events are associated with somatic symptoms (Bohman et al., 2018; Firat et al., 2018), while other studies have indicated depressed affect is also directly related to interpersonal problems (Majd Ara et al., 2017; Rice et al., 2017; Schwartz-Mette and Smith, 2018). In tandem with more severe depressed affect, adolescents might suffer from more frequent physical complaints, lower self-efficacy and reduced life contentment during the COVID-19 pandemic (Yun et al., 2021). Notwithstanding this evidence from other samples, the pandemic has resulted in increased restrictions related to engaging in routine physical activities and higher than typical levels of social isolation. Hence, these disruptions to daily life brought about by the COVID-19 pandemic may have contributed to more pronounced connections of depressed affect with somatic complaints and interpersonal problems across two different assessments of adolescents in this study.
The symptom of Nervousness presented high closeness and bridge closeness in both survey symptom networks, a finding that suggests Nervousness is more likely to affect and/or be affected by changes in other symptoms. Nervousness and anxiety are common among adolescents due to frequent exposure to negative events and feelings of insecurity (Kılınçel et al., 2021; Qi et al., 2020; Zhou et al., 2020b). This finding aligns with other recent China-based findings (Bai et al., 2021) identifying Nervousness as a bridge symptom between depression and anxiety during the COVID-19 pandemic among nursing students. Furthermore, connections between (1) Nervousness and Control Worry, and (2) Relax and Restlessness were relatively strong in both the first and second survey networks. Interactions between Nervousness and Control worries as well as contradictory experiences of Relaxation and Restlessness might have been strengthened among adolescents due to the widespread uncertainty and unpredictability resulting from the pandemic (Durodie, 2020; Orgilés et al., 2020).
Although the most prominent central symptoms, bridge symptoms and edges of the initial network model were cross-validated across samples and pandemic phases, select findings were not replicated across the samples. Specifically, connections of Relax – Nervousness – Depressed affect – Interpersonal problems, and Irritability – Somatic complaints were weaker in network model of the second sample. In addition, connections of Restlessness– Interpersonal problems– Depressed affect, and Irritability – Somatic complaints had significantly weaker connections in the second survey when the sensitivity analysis was run on the participant subgroup that had completed only the second survey (N = 3,886), As such, linkages of mood, communication and physical problems within anxiety-depression network models may be less stable or generalizable across pandemic phases and/or different groups of Chinese adolescents. It is not clear why these facets of the initial network model were less replicable. One hypothesis may be that changes in pandemic conditions contributed to changes in these relations. To elaborate, during the initial COVID-19 outbreak, many adolescents experienced heavy academic burdens and psychological distress, both of which had a negative impact on their physical and mental health in tandem with increased physical and social isolation (Jiao et al., 2020; Qi et al., 2020; Zhou et al., 2020b). After the peak of the COVID-19 outbreak, lockdown and quarantine measures were gradually lifted in most areas and schools reopened; these shifts toward regular routines may have may have contributed to more attenuated connections between these nodes within the symptom network following the pandemic peak (Fancourt et al., 2020; Lu et al., 2020; Wang et al., 2020).
Other relations from the initial network model that were not cross-validated included stronger connections between nodes of Depressed affect - Somatic complaints - Nervousness, and Irritability – Control worry – Restlessness observed in the network model generated for the second assessment of adolescents. Furthermore, the connection of Irritability – Control worry was significantly stronger for the second survey based on the sensitivity analysis of participants who completed only the second survey. Although it is not clear why these associations were not consistent in the post-peak survey sample, it should be noted that quarantine measures can have a lingering long-term negative impact on experiences of stress. For instance, following the COVID-19 outbreak peak, many adolescents had to re-establish rapport with teachers and classmates, adapt to the transition from online to classroom teaching, cope with heavy academic demands related to the end of an academic year, and live with the uncertainty of possible future waves of COVID-19 (Lee, 2020; Singh et al., 2020; Tasso et al., 2021); these adjustments could contribute to the persistence or increased connectivity between these nodes.
In relation to treatment implications, high overall depression and anxiety levels, highly consistent central symptoms, reliable bridge symptoms and stable connections between select nodes across anxiety-depression network models of two different evaluations of Chinese adolescents underscored the importance of monitoring adolescents’ long-term mental health across different phases of the COVID-19 pandemic as well as the potential utility of targeting particular symptoms, most notably in interventions tailored for the overall population of adolescents. Drawing upon recommendations from other network analysis research (Beard et al., 2016; Fried et al., 2016), the cross-validation of depressed affect both as a central symptom and a bridge symptom across both assessment samples suggests that interventions targeting experiences of sadness, depressed mood, nervousness, loneliness, and physical activity may be particularly beneficial in reducing distress and potential comorbidity of anxiety and depression among adolescents during different pandemic phases. For example, Cognitive Behavioral Therapy (CBT) strategies such as behavioral activation and cognitive restructuring may aid in reducing depressed affect and help to explain the efficacy of very brief CBT as an approach to reducing to depression in this population (Bjorgvinsson et al., 2014).
Strengths of this study included its use of a cross-validation approach to identify the most reliable features of anxiety-depression networks across two assessments of large national samples of adolescents, assessments at different phases of a pandemic, and use of network analysis to elucidate the nature and strength of associations between depressive and anxious symptoms of adolescents. In addition, the sensitivity analysis demonstrated that most of the main findings were robust and stable across independent samples of adolescents evaluated during different phases of the COVID-19 pandemic. The results may be useful in encouraging researchers and clinicians to consider the significance of individual symptoms of depression and anxiety across groups of adolescents drawn from the same population as well as their interrelations while questioning the assumption that all symptoms have an equal impact in the expression of these disturbances.
The main limitations should also be noted. First, data for each sample were cross-sectional in nature so they offered single snapshots of symptom networks for particular groups of adolescents at particular points during a pandemic rather than dynamic changes within a single group over different phases of the pandemic. Although our research helped to highlight anxiety-depression network features that are important across different groups of Chinese adolescents and stages of the COVID-19 pandemic, longitudinal extensions following adolescents over more extended periods are needed to evaluate whether and how the structure of adolescent depression-anxiety symptom networks may evolve over time within a single group of adolescents. Second, because results were based on self-report scales, replications based on interviewer-rated scales would be useful in bolstering the validity of results. Third, although most of the main results were replicated across two national samples, random selection was not employed to recruit participants, in part, because pandemic conditions did not allow for offline recruitment strategies. As such, findings may not be entirely representative of the adolescent population of China. Finally, it is not clear whether results from this survey generalize to adolescents in other countries or non-pandemic eras. This limitation provides another foundation for extensions.
In conclusion, network analyses of central and bridge symptoms of depression and anxiety found relatively stable structures of depressive and anxious symptoms across two evaluations of large national adolescent samples assessed during and after the peak of the COVID-19 outbreak in China. In addition, select relations between symptoms were not cross-validated across the two assessments, suggesting that some features of the network models are less stable and do not extend as well to the overall study population and/or different pandemic phases. The findings suggested that effective interventions targeting depressed affect in particular during both phases of the pandemic could be helpful reducing co-occurring depressive and anxious symptoms among Chinese adolescents.
Role of funding
The study was supported by the National Natural Science Foundation of China (81901368), Beijing Hospitals Authority Clinical medicine Development of Special Funding Support (ZYLX202128); the Beijing Municipal Administration of Hospitals Incubating Program (PX2020072) and the Beijing Hospitals Authority Clinical Medicine Development of special funding support (XMLX202128).
Author contributions
Study design: Rui Liu, Ling Zhang, Yu-Tao Xiang. Data collection, analysis and interpretation: Xu Chen, Han Qi, Rui Liu, Yuan Feng, Teris Cheung, Hui Lei. Drafting of the manuscript: Rui Liu, Han Qi, Zhaohui Su, Yu-Tao Xiang. Critical revision of the manuscript: Todd Jackson. Approval of the final version for publication: all co-authors.
Declaration of Competing Interest
The authors have no conflicts of interest to declare.
Acknowledgements
None.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2021.12.137.
Appendix. Supplementary materials
References
- Bai W., Xi H.T., Zhu Q., Ji M., Zhang H., Yang B.X., Cai H., Liu R., Zhao Y.J., Chen L., Ge Z.M., Wang Z., Han L., Chen P., Liu S., Cheung T., Tang Y.L., Jackson T., An F., Xiang Y.T. Network analysis of anxiety and depressive symptoms among nursing students during the COVID-19 pandemic. J. Affect. Disord. 2021;294:753–760. doi: 10.1016/j.jad.2021.07.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beard C., Millner A.J., Forgeard M.J., Fried E.I., Hsu K.J., Treadway M.T., Leonard C.V., Kertz S.J., Björgvinsson T. Network analysis of depression and anxiety symptom relationships in a psychiatric sample. Psychol. Med. 2016;46:3359–3369. doi: 10.1017/S0033291716002300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belvederi Murri M., Amore M., Respino M., Alexopoulos G.S. The symptom network structure of depressive symptoms in late-life: results from a European population study. Mol. Psychiatry. 2020;25:1447–1456. doi: 10.1038/s41380-018-0232-0. [DOI] [PubMed] [Google Scholar]
- Bjorgvinsson T., Kertz S.J., Bigda-Peyton J.S., Rosmarin D.H., Aderka I.M., Neuhaus E.C. Effectiveness of cognitive behavior therapy for severe mood disorders in an acute psychiatric naturalistic setting: a benchmarking study. Cogn. Behav. Ther. 2014;43:209–220. doi: 10.1080/16506073.2014.901988. [DOI] [PubMed] [Google Scholar]
- Bohman H., Laftman S.B., Cleland N., Lundberg M., Paaren A., Jonsson U. Somatic symptoms in adolescence as a predictor of severe mental illness in adulthood: a long-term community-based follow-up study. Child Adolesc. Psychiatry Ment. Health. 2018;12:42. doi: 10.1186/s13034-018-0245-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borgatti S.P. Centrality and network flow. Soc. Netw. 2005;27:55–71. [Google Scholar]
- Borsboom D. Psychometric perspectives on diagnostic systems. J. Clin. Psychol. 2008;64:1089–1108. doi: 10.1002/jclp.20503. [DOI] [PubMed] [Google Scholar]
- Borsboom D. A network theory of mental disorders. World Psychiatry. 2017;16:5–13. doi: 10.1002/wps.20375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom D., Cramer A.O. Network analysis: an integrative approach to the structure of psychopathology. Annu. Rev. Clin. Psychol. 2013;9:91–121. doi: 10.1146/annurev-clinpsy-050212-185608. [DOI] [PubMed] [Google Scholar]
- Chen J., Chen Z. Extended Bayesian information criteria for model selection with large model spaces. Biometrika. 2008;95:759–771. [Google Scholar]
- Contreras A., Nieto I., Valiente C., Espinosa R., Vazquez C. The study of psychopathology from the network analysis perspective: a systematic review. Psychother. 2019;88:71–83. doi: 10.1159/000497425. [DOI] [PubMed] [Google Scholar]
- Conway C.C., Zinbarg R.E., Mineka S., Craske M.G. Core dimensions of anxiety and depression change independently during adolescence. J. Abnorm. Psychol. 2017;126:160–172. doi: 10.1037/abn0000222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtney D., Watson P., Battaglia M., Mulsant B.H., Szatmari P. COVID-19 impacts on child and youth anxiety and depression: challenges and opportunities. Can. J. Psychiatry. 2020;65:688–691. doi: 10.1177/0706743720935646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cramer A.O., Waldorp L.J., Van Der Maas H.L., Borsboom D. Comorbidity: a network perspective. Behav. Brain Sci. 2010;33:137. doi: 10.1017/S0140525X09991567. [DOI] [PubMed] [Google Scholar]
- Dalege J., Borsboom D., van Harreveld F., van der Maas H.L.J. Network analysis on attitudes: a brief tutorial. Soc. Psychol. Personal. Sci. 2017;8:528–537. doi: 10.1177/1948550617709827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danhauer S.C., Legault C., Bandos H., Kidwell K., Costantino J., Vaughan L., Avis N.E., Rapp S., Coker L.H., Naughton M., Naylor C., Terracciano A., Shumaker S. Positive and negative affect, depression, and cognitive processes in the Cognition in the Study of Tamoxifen and Raloxifene (Co-STAR) Trial. Neuropsychol. Dev. Cogn. B Aging Neuropsychol. Cogn. 2013;20:532–552. doi: 10.1080/13825585.2012.747671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durodie B. Handling uncertainty and ambiguity in the COVID-19 pandemic. Psychol. Trauma. 2020;12:S61–S62. doi: 10.1037/tra0000713. [DOI] [PubMed] [Google Scholar]
- Epskamp, S., 2016. Regularized Gaussian psychological networks: brief report on the performance of extended BIC model selection. arXiv:1606.05771.
- Epskamp S., Borsboom D., Fried E.I. Estimating psychological networks and their accuracy: a tutorial paper. Behav. Res. Method. 2018;50:195–212. doi: 10.3758/s13428-017-0862-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S., Cramer A.O., Waldorp L.J., Schmittmann V.D., Borsboom D. qgraph: network visualizations of relationships in psychometric data. J. Stat. Softw. 2012;48:1–18. [Google Scholar]
- Epskamp S., Waldorp L.J., Mõttus R., Borsboom D. The Gaussian graphical model in cross-sectional and time-series data. Multivariate Behav. Res. 2018;53:453–480. doi: 10.1080/00273171.2018.1454823. [DOI] [PubMed] [Google Scholar]
- Eurosurveillance Editorial Team Note from the editors: world Health Organization declares novel coronavirus (2019-nCoV) sixth public health emergency of international concern. Eurosurveillance. 2020;25 doi: 10.2807/1560-7917.ES.2020.25.5.200131e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fancourt D., Steptoe A., Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(20)30482-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Firat S., Gul H., Sertcelik M., Gul A., Gurel Y., Kilic B.G. The relationship between problematic smartphone use and psychiatric symptoms among adolescents who applied to psychiatry clinics. Psychiatry Res. 2018;270:97–103. doi: 10.1016/j.psychres.2018.09.015. [DOI] [PubMed] [Google Scholar]
- Fisher A.J., Reeves J.W., Lawyer G., Medaglia J.D., Rubel J.A. Exploring the idiographic dynamics of mood and anxiety via network analysis. J. Abnorm. Psychol. 2017;126:1044–1056. doi: 10.1037/abn0000311. [DOI] [PubMed] [Google Scholar]
- Freeman L.C. Centrality in social networks conceptual clarification. Soc. Netw. 1978;1:215–239. [Google Scholar]
- Fried E.I. Problematic assumptions have slowed down depression research: why symptoms, not syndromes are the way forward. Front. Psychol. 2015;6:309. doi: 10.3389/fpsyg.2015.00309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried E.I., Epskamp S., Nesse R.M., Tuerlinckx F., Borsboom D. What are 'good' depression symptoms? Comparing the centrality of DSM and non-DSM symptoms of depression in a network analysis. J. Affect. Disord. 2016;189:314–320. doi: 10.1016/j.jad.2015.09.005. [DOI] [PubMed] [Google Scholar]
- Fried E.I., Nesse R.M. The impact of individual depressive symptoms on impairment of psychosocial functioning. PLoS One. 2014;9:e90311. doi: 10.1371/journal.pone.0090311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman J., Hastie T., Tibshirani R. Sparse inverse covariance estimation with the graphical lasso. Biostatistics. 2008;9:432–441. doi: 10.1093/biostatistics/kxm045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghosh A. COVID-19 pandemic and an early career mental health researcher from a low and middle income country: is there any light at the end of the tunnel? Asia-Pacific Psychiatry. 2020;12:e12424. doi: 10.1111/appy.12424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golberstein E., Wen H., Miller B.F. Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatr. 2020;174:819–820. doi: 10.1001/jamapediatrics.2020.1456. [DOI] [PubMed] [Google Scholar]
- Guessoum S.B., Lachal J., Radjack R., Carretier E., Minassian S., Benoit L., Moro M.R. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 2020;291 doi: 10.1016/j.psychres.2020.113264. -113264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo L., Xu Y., Deng J., Huang J., Huang G., Gao X., Wu H., Pan S., Zhang W.-.H., Lu C. Association between nonmedical use of prescription drugs and suicidal behavior among adolescents. JAMA Pediatr. 2016;170:971–978. doi: 10.1001/jamapediatrics.2016.1802. [DOI] [PubMed] [Google Scholar]
- He X., Li C., Qian J., Cui H.S., Wu W. Reliability and validity of a generalized anxiety scale in general hospital outpatients. Shanghai Arch. Psychiatry. 2010;22:200–203. [Google Scholar]
- Heeren A., Jones P.J., McNally R.J. Mapping network connectivity among symptoms of social anxiety and comorbid depression in people with social anxiety disorder. J. Affect. Disord. 2018;228:75–82. doi: 10.1016/j.jad.2017.12.003. [DOI] [PubMed] [Google Scholar]
- Hevey D. Network analysis: a brief overview and tutorial. Health Psychol. Behav. Med. 2018;6:301–328. doi: 10.1080/21642850.2018.1521283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffart A., Johnson S.U., Ebrahimi O.V. The network of stress-related states and depression and anxiety symptoms during the COVID-19 lockdown. J. Affect. Disord. 2021;294:671–678. doi: 10.1016/j.jad.2021.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiao W.Y., Wang L.N., Liu J., Fang S.F., Jiao F.Y., Pettoello-Mantovani M., Somekh E. Behavioral and Emotional Disorders in Children during the COVID-19 Epidemic. J. Pediatr. 2020;221:264–266. doi: 10.1016/j.jpeds.2020.03.013. e261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones, P., 2021. Networktools: Tools for identifying important nodes in networks. R package version 1.4.1. Retrieved from https://CRAN.R-project.org/package=networktools.
- Jones P.J., Ma R., McNally R.J. Bridge centrality: a network approach to understanding comorbidity. Multivariate Behav. Res. 2019:1–15. doi: 10.1080/00273171.2019.1614898. [DOI] [PubMed] [Google Scholar]
- Kapur S., Phillips A.G., Insel T.R. Why has it taken so long for biological psychiatry to develop clinical tests and what to do about it? Mol. Psychiatry. 2012;17:1174–1179. doi: 10.1038/mp.2012.105. [DOI] [PubMed] [Google Scholar]
- Kılınçel Ş., Kılınçel O., Muratdağı G., Aydın A., Usta M.B. Factors affecting the anxiety levels of adolescents in home-quarantine during COVID-19 pandemic in Turkey. Asia-Pacific Psychiatry. 2021;13:e12406. doi: 10.1111/appy.12406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J. Mental health effects of school closures during COVID-19. Lancet Child. Adolesc. Health. 2020;4:421. doi: 10.1016/S2352-4642(20)30109-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J.J., Bao Y., Huang X., Shi J., Lu L. Mental health considerations for children quarantined because of COVID-19. Lancet Child. Adolesc. Health. 2020;4:347–349. doi: 10.1016/S2352-4642(20)30096-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S., Yang L., Zhang C., Xiang Y.-.T., Liu Z., Hu S., Zhang B. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e17–e18. doi: 10.1016/S2215-0366(20)30077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu P., Li X., Lu L., Zhang Y. The psychological states of people after Wuhan eased the lockdown. PLoS One. 2020;15 doi: 10.1371/journal.pone.0241173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Majd Ara E., Talepasand S., Rezaei A.M. A structural model of depression based on interpersonal relationships: the mediating role of coping strategies and loneliness. Noro Psikiyatr Ars. 2017;54:125–130. doi: 10.5152/npa.2017.12711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mamun M.A., Hossain M.S., Moonajilin M.S., Masud M.T., Misti J.M., Griffiths M.D. Does loneliness, self-esteem and psychological distress correlate with problematic internet use? A Bangladeshi survey study. Asia-Pacific Psychiatry. 2020;12:e12386. doi: 10.1111/appy.12386. [DOI] [PubMed] [Google Scholar]
- Mattila E., Peltokoski J., Neva M.H., Kaunonen M., Helminen M., Parkkila .A..-K. COVID-19: anxiety among hospital staff and associated factors. Ann. Med. 2021;53:237–246. doi: 10.1080/07853890.2020.1862905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melton T.H., Croarkin P.E., Strawn J.R., McClintock S.M. Comorbid anxiety and depressive symptoms in children and adolescents: a systematic review and analysis. J. Psychiatr. Pract. 2016;22:84–98. doi: 10.1097/PRA.0000000000000132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mineka S., Watson D., Clark L.A. Comorbidity of anxiety and unipolar mood disorders. Annu. Rev. Psychol. 1998;49:377–412. doi: 10.1146/annurev.psych.49.1.377. [DOI] [PubMed] [Google Scholar]
- Montazeri F., de Bildt A., Dekker V., Anderson G.M. Network analysis of behaviors in the depression and Autism Realms: inter-relationships and clinical implications. J. Autism Dev. Disord. 2020;50:1580–1595. doi: 10.1007/s10803-019-03914-4. [DOI] [PubMed] [Google Scholar]
- Naragon-Gainey K., Prenoveau J.M., Brown T.A., Zinbarg R.E. A comparison and integration of structural models of depression and anxiety in a clinical sample: support for and validation of the tri-level model. J. Abnorm. Psychol. 2016;125:853–867. doi: 10.1037/abn0000197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nardi B., Francesconi G., Catena-Dell'osso M., Bellantuono C. Adolescent depression: clinical features and therapeutic strategies. Eur. Rev. Med. Pharmacol. Sci. 2013;17:1546–1551. [PubMed] [Google Scholar]
- Nguyen H.T., Kitner-Triolo M., Evans M.K., Zonderman A.B. Factorial invariance of the CES-D in low socioeconomic status African Americans compared with a nationally representative sample. Psychiatry Res. 2004;126:177–187. doi: 10.1016/j.psychres.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Opsahl T., Agneessens F., Skvoretz J. Node centrality in weighted networks: generalizing degree and shortest paths. Soc. Netw. 2010;32:245–251. [Google Scholar]
- Orgilés M., Morales A., Delvecchio E., Mazzeschi C., Espada J.P. Immediate psychological effects of the COVID-19 quarantine in youth from Italy and Spain. Front. Psychol. 2020:11. doi: 10.3389/fpsyg.2020.579038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan H., Liu Q. Difference of depression between widowed and non-widowed older people in China: a network analysis approach. J. Affect. Disord. 2020 doi: 10.1016/j.jad.2020.11.058. [DOI] [PubMed] [Google Scholar]
- Peng Y., Pei C., Zheng Y., Wang J., Zhang K., Zheng Z., Zhu P. A cross-sectional survey of knowledge, attitude and practice associated with COVID-19 among undergraduate students in China. BMC Public Health. 2020;20:1292. doi: 10.1186/s12889-020-09392-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prenoveau J.M., Zinbarg R.E., Craske M.G., Mineka S., Griffith J.W., Epstein A.M. Testing a hierarchical model of anxiety and depression in adolescents: a tri-level model. J. Anxiety Disord. 2010;24:334–344. doi: 10.1016/j.janxdis.2010.01.006. [DOI] [PubMed] [Google Scholar]
- Pyramid Healthcare, 2018. Anxiety: how is it Different for Kids and Adults? https://www.pyramidhealthcarepa.com/anxiety-kids-adults/ (access October 16, 2018).
- Qi H., Liu R., Chen X., Yuan X.F., Li Y.Q., Huang H.H., Zheng Y., Wang G. Prevalence of anxiety and associated factors for Chinese adolescents during the COVID-19 outbreak. Psychiatry Clin. Neurosci. 2020;74:555–557. doi: 10.1111/pcn.13102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff L.S. The CES-D scale: a self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977;1:385–401. [Google Scholar]
- Rice F., Eyre O., Riglin L., Potter R. Adolescent depression and the treatment gap. Lancet Psychiatry. 2017;4:86–87. doi: 10.1016/S2215-0366(17)30004-4. [DOI] [PubMed] [Google Scholar]
- Rice F., Riglin L., Lomax T., Souter E., Potter R., Smith D.J., Thapar A.K., Thapar A. Adolescent and adult differences in major depression symptom profiles. J. Affect. Disord. 2019;243:175–181. doi: 10.1016/j.jad.2018.09.015. [DOI] [PubMed] [Google Scholar]
- Rouquette A., Pingault J.B., Fried E.I., Orri M., Falissard B., Kossakowski J.J., Vitaro F., Tremblay R., Cote S.M., Borsboom D. Emotional and behavioral symptom network structure in elementary school girls and association with anxiety disorders and depression in adolescence and early adulthood: a network analysis. JAMA Psychiatry. 2018;75:1173–1181. doi: 10.1001/jamapsychiatry.2018.2119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez-Caballero S., Selles M.A., Peydro M.A., Perez-Bernabeu E. An efficient COVID-19 prediction model validated with the cases of China, Italy and Spain: total or partial lockdowns? J. Clin. Med. 2020;9 doi: 10.3390/jcm9051547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmittmann V.D., Cramer A.O., Waldorp L.J., Epskamp S., Kievit R.A., Borsboom D. Deconstructing the construct: a network perspective on psychological phenomena. New Idea. Psychol. 2013;31:43–53. [Google Scholar]
- Schwartz-Mette R.A., Smith R.L. When does co-rumination facilitate depression contagion in adolescent friendships? Investigating intrapersonal and interpersonal factors. J. Clin. Child. Adolesc. Psychol. 2018;47:912–924. doi: 10.1080/15374416.2016.1197837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh S., Roy D., Sinha K., Parveen S., Sharma G., Joshi G. Impact of COVID-19 and lockdown on mental health of children and adolescents: a narrative review with recommendations. Psychiatry Res. 2020;293 doi: 10.1016/j.psychres.2020.113429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Sun X.Y., Li Y.X., Yu C.Q., Li L.M. Reliability and validity of depression scales of Chinese version: a systematic review (in Chinese) J. Chin. Epidemiol. 2017;38:110–116. doi: 10.3760/cma.j.issn.0254-6450.2017.01.021. [DOI] [PubMed] [Google Scholar]
- Tasso A.F., Hisli Sahin N., San Roman G.J. COVID-19 disruption on college students: academic and socioemotional implications. Psychol. Trauma. 2021;13:9–15. doi: 10.1037/tra0000996. [DOI] [PubMed] [Google Scholar]
- Tong X., An D., McGonigal A., Park S.P., Zhou D. Validation of the Generalized Anxiety Disorder-7 (GAD-7) among Chinese people with epilepsy. Epilepsy Res. 2016;120:31–36. doi: 10.1016/j.eplepsyres.2015.11.019. [DOI] [PubMed] [Google Scholar]
- van Borkulo C., Boschloo L., Borsboom D., Penninx B.W., Waldorp L.J., Schoevers R.A. Association of symptom network structure with the course of [corrected] depression. JAMA Psychiatry. 2015;72:1219–1226. doi: 10.1001/jamapsychiatry.2015.2079. [DOI] [PubMed] [Google Scholar]
- van Borkulo, C., Boschloo, L., Kossakowski, J., Tio, P., Schoevers, R., Borsboom, D., Waldorp, L., 2017. Comparing network structures on three aspects: A permutation test. Manuscript submitted for publication (preprint). Retrieved from https://www.researchgate.net/publication/314750838_Comparing_network_structures_on_three_aspects_A_permutation_test?channel=doi?linkld=58c55ef145851538eb8af8a9&showFulltext=true. [DOI] [PubMed]
- Wang Y., Hu Z., Feng Y., Wilson A., Chen R. Changes in network centrality of psychopathology symptoms between the COVID-19 outbreak and after peak. Mol. Psychiatry. 2020:1–10. doi: 10.1038/s41380-020-00881-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wasserman D., Carli V., Iosue M., Javed A., Herrman H. Suicide prevention in childhood and adolescence: a narrative review of current knowledge on risk and protective factors and effectiveness of interventions. Asia-Pacific Psychiatry. 2021;13:e12452. doi: 10.1111/appy.12452. [DOI] [PubMed] [Google Scholar]
- WorldoMeters, 2021. COVID-19 CORONAVIRUS PANDEMIC. https://www.worldometers.info/coronavirus/ (access February 15, 2021).
- Xinhuanet, 2020. China says its COVID-19 peak is over. http://www.xinhuanet.com/english/2020-03/12/c_138870547.htm (access March 12, 2020).
- Yun J.Y., Kim J.W., Myung S.J., Yoon H.B., Moon S.H., Ryu H., Yim J.J. Impact of COVID-19 on lifestyle, personal attitudes, and mental health among Korean medical students: network analysis of associated patterns. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.702092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zbozinek T.D., Rose R.D., Wolitzky-Taylor K.B., Sherbourne C., Sullivan G., Stein M.B., Roy-Byrne P.P., Craske M.G. Diagnostic overlap of generalized anxiety disorder and major depressive disorder in a primary care sample. Depress. Anxiety. 2012;29:1065–1071. doi: 10.1002/da.22026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou J., Yuan X., Qi H., Liu R., Li Y., Huang H., Chen X., Wang G. Prevalence of depression and its correlative factors among female adolescents in China during the coronavirus disease 2019 outbreak. Global Health. 2020;16:69. doi: 10.1186/s12992-020-00601-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou S.J., Zhang L.G., Wang L.L., Guo Z.C., Wang J.Q., Chen J.C., Liu M., Chen X., Chen J.X. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child Adolesc. Psychiatry. 2020;29:749–758. doi: 10.1007/s00787-020-01541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu S., Wu Y., Zhu C.Y., Hong W.C., Yu Z.X., Chen Z.K., Chen Z.L., Jiang D.G., Wang Y.G. The immediate mental health impacts of the COVID-19 pandemic among people with or without quarantine managements. Brain Behav. Immun. 2020;87:56–58. doi: 10.1016/j.bbi.2020.04.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.