In this issue,1 Kremer and colleagues add to the epidemiological evidence demonstrating differences in the association of blood pressure and mortality across frailty or functional status.2, 3 In a cohort of 1,170 community-dwelling older adults in southern Germany enrolled in the Activity and Function in the Elderly in Ulm (ActiFE Ulm) Study, they found the lowest risk of mortality among non-frail participants was observed at systolic blood pressure of approximately 130 mmHg, consistent with many guideline recommendations. In contrast, among frail older adults, the risk of death decreased with higher systolic blood pressure, with the lowest risk occurring in those with systolic blood pressure 160 mmHg or higher. These patterns were consistent after adjustment for potential confounders as well as excluding deaths in the first year after blood pressure assessment; to account for the fact that blood pressure often declines near the end of life.4 About half of their study population would have met inclusion criteria for the Systolic Blood Pressure Intervention Trial (SPRINT), and the authors did not find evidence of effect modification by frailty status in this subpopulation. This finding is consistent with SPRINT, which did not observe evidence of effect modification of intensive blood pressure lowering by frailty status.5
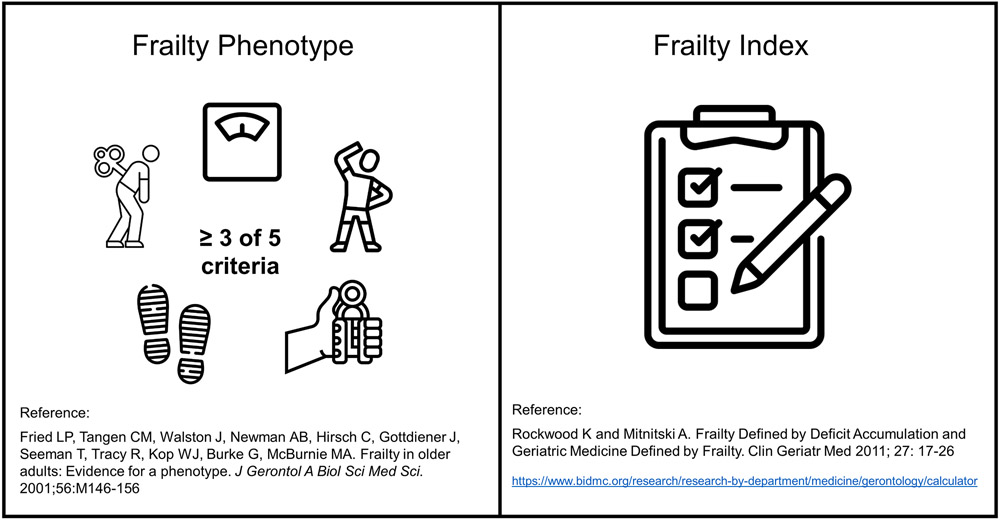
As the authors note, measurement of frailty remains elusive. The conceptual definition, lack of physiologic reserve and vulnerability to stressors, remains challenging to measure in practice. The physical frailty phenotype remains among the most popular, and is generally assessed by grip strength, gait speed, low physical activity, self-reported exhaustion, and unintended weight loss.6 (Figure) A strength of this measure of frailty is that the measure is distinct from comorbidity and disability.6 However, not all of these components are accessible in all studies. The frailty index, often described as a “deficit accumulation” method is a complementary measure of frailty that uses available measures of deficits including physical and cognitive function, comorbidities, and psychosocial health.7 (Figure) This method was applied in the ActiFE Ulm study. A benefit of this method is that it can be applied across a variety of studies and does not require the same standardized methods. A limitation is that it may capture elements of poor health not unique to the clinical syndrome of frailty, including cardiovascular risk factors. Additionally, although the present study, ActiFE Ulm, and SPRINT both used these deficit accumulation frailty indices, they did not comprise the same data elements and were tailored to the availability of measures in these studies.8, 9
Figure:
The Frailty Phenotype and the Frailty Index are the two major tools to assess frailty
The study by Kremer and colleagues complements existing literature demonstrating that the relationship between blood pressure and mortality differs by the presence of frailty. This is often termed “effect modification” where the effect of an exposure, such as blood pressure, varies across the level of some subgroup, such as frailty. Moreover, the present study shows lack of effect modification, or no difference in the relationship between blood pressure and mortality by frailty, when the study population is limited to those meeting the SPRINT inclusion criteria. However, this finding should be interpreted with caution, since the sample size among those meeting SPRINT eligibility criteria was less than half of the study population, and thus statistical power may be limited. Nonetheless, this is consistent with SPRINT and Hypertension in the Very Elderly Trial (HYVET), both of which trials found no differences of blood pressure lowering treatment across levels the frailty index.5, 10 This suggests that whether or not a difference in the relationship between blood pressure and mortality is present may be influenced by the characteristics of participants included in the study.
There are important differences between observational studies of lower blood pressure and randomized controlled trials of blood pressure lowering. A key difference is that measured and unmeasured confounders are asymptotically balanced across treatment groups in randomized controlled trials. Statistical adjustment is used to account for any imbalance in observational studies, but residual and unmeasured confounding are common. This can lead to an apparent increase in risk associated with treatment (confounding by indication) or benefit (healthy user bias) depending on the characteristics of those with lower blood pressures. The ability to balance confounders through randomization is the reason why randomized controlled trials are cited as the strongest form of evidence for causal effects.
However, another less well recognized difference between observational studies and randomized controlled trials is the difference in the populations included. Randomized controlled trials often employ inclusion and exclusion criteria to ensure that study participants are able to complete the study protocol and are not subject to undue risks, but these criteria often exclude patients who are the sickest. Inclusion criteria also frequently select for participants at higher risk of the study outcomes. Differences in the selection of those participants included in randomized controlled trials can lead to lack of external validity and poor generalizability. In the presence of subgroup differences, the population-level causal effects in trials will not extend to populations without the same distribution of the subgroups. Furthermore, if a subset of patients (i.e. the sickest and frailest) are underrepresented or excluded from trials, then effect modification will be either underpowered or absent in the trial populations. In the present study, the prevalence of frailty was 17.0% in the subpopulation meeting SPRINT criteria, and 25.4% in the population who did not meet SPRINT criteria, which highlights the impact that inclusion criteria can have on the prevalence of frailty. Finally, older adults with limited life expectancy may not live long enough to experience the benefit from the intervention of interest.11
There is a growing body of evidence that demonstrates the lack of representation in the study populations of trials compared to observational studies and real world patients. The recent Strategy of Blood Pressure Intervention in the Elderly Hypertensive Patients (STEP) trial of intensive blood pressure control in older patients in China did not find a reduction in mortality12 and all-cause mortality rates in both arms were 0.5% per year compared to 2.2% in SPRINT, and 3.1% in the present study. We previously demonstrated that SPRINT and the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trials are representative of less than one-third of the target population for the 2017 American College of Cardiology/American Heart Association guideline for high blood pressure.13 Among older adults, those with multiple chronic conditions and limited life expectancy, both of which overlap with frailty, were most likely to be excluded.14 Participants in HYVET were healthier and had fewer comorbidities than most community-dwelling octogenarians.15 None of the aforementioned trials included individuals residing in long-term care settings. Although these trials showed clear benefit of blood pressure lowering in some older adults, whether these findings should be extended to all older adults, particularly those with limited life expectancy, remains uncertain.
In summary, the results from Kremer and colleagues suggest that frail older adults with multiple chronic conditions may benefit from higher blood pressures. This population has been underrepresented or excluded from clinical trials, leaving clinicians and patients with limited evidence to guide decision-making. We recommend a patient-centered approach that considers patient preferences, cardiovascular risk, competing risks, and time to benefit in this population. At least one guideline has been developed specifically to guide targets in this population.16 Moreover, we advocate for the need to continue to expand trial criteria to include those who have been underrepresented in previous studies. Pragmatic trials may help fill this important gap. In the meantime, high quality observational study data coupled with rigorous epidemiological and statistical methods may help inform the balance of risks and benefits in this population.
Footnotes
Disclosure: none
References:
- 1.Kremer KM, Braisch U, Rothenbacher D, Denkinger M, Dallmeier D. Systolic blood pressure and mortality in community-dwelling older adults: Frailty as an effect modifier. Hypertension. 2021. in press [DOI] [PubMed] [Google Scholar]
- 2.Odden MC, Beilby PR, Peralta CA. Blood pressure in older adults: The importance of frailty. Curr Hypertens Rep. 2015;17:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu C, Smit E, Peralta CA, Sarathy H, Odden MC. Functional status modifies the association of blood pressure with death in elders: Health and retirement study. J Am Geriatr Soc. 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ravindrarajah R, Hazra NC, Hamada S, Charlton J, Jackson SHD, Dregan A, Gulliford MC. Systolic blood pressure trajectory, frailty, and all-cause mortality >80 years of age: Cohort study using electronic health records. Circulation. 2017;135:2357–2368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Williamson JD, Supiano MA, Applegate WB, Berlowitz DR, Campbell RC, Chertow GM, Fine LJ, Haley WE, Hawfield AT, Ix JH, Kitzman DW, Kostis JB, Krousel-Wood MA, Launer LJ, Oparil S, Rodriguez CJ, Roumie CL, Shorr RI, Sink KM, Wadley VG, Whelton PK, Whittle J, Woolard NF, Wright JT Jr., Pajewski NM, Group SR. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged >/=75 years: A randomized clinical trial. JAMA. 2016;315:2673–2682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA. Frailty in older adults: Evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146–156 [DOI] [PubMed] [Google Scholar]
- 7.Rockwood K, Mitnitski A. Frailty defined by deficit accumulation and geriatric medicine defined by frailty. Clin Geriatr Med. 2011;27:17–26 [DOI] [PubMed] [Google Scholar]
- 8.Dallmeier D, Braisch U, Rapp K, Klenk J, Rothenbacher D, Denkinger M, Acti FESG. Frailty index and sex-specific 6-year mortality in community-dwelling older people: The actife study. J Gerontol A Biol Sci Med Sci. 2020;75:366–373 [DOI] [PubMed] [Google Scholar]
- 9.Pajewski NM, Williamson JD, Applegate WB, Berlowitz DR, Bolin LP, Chertow GM, Krousel-Wood MA, Lopez-Barrera N, Powell JR, Roumie CL, Still C, Sink KM, Tang R, Wright CB, Supiano MA, Group SSR. Characterizing frailty status in the systolic blood pressure intervention trial. J Gerontol A Biol Sci Med Sci. 2016;71:649–655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Warwick J, Falaschetti E, Rockwood K, Mitnitski A, Thijs L, Beckett N, Bulpitt C, Peters R. No evidence that frailty modifies the positive impact of antihypertensive treatment in very elderly people: An investigation of the impact of frailty upon treatment effect in the hypertension in the very elderly trial (hyvet) study, a double-blind, placebo-controlled study of antihypertensives in people with hypertension aged 80 and over. BMC Med. 2015;13:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Krishnaswami A, Peterson ED, Goyal P, Kim DH, Rich MW, Lee SJ. Time to benefit and harm of intensive blood pressure treatment: Insights from sprint. Eur Heart J Qual Care Clin Outcomes. 2021;7:e1–e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang W, Zhang S, Deng Y, Wu S, Ren J, Sun G, Yang J, Jiang Y, Xu X, Wang TD, Chen Y, Li Y, Yao L, Li D, Wang L, Shen X, Yin X, Liu W, Zhou X, Zhu B, Guo Z, Liu H, Chen X, Feng Y, Tian G, Gao X, Kario K, Cai J, Group SS. Trial of intensive blood-pressure control in older patients with hypertension. N Engl J Med. 2021;385:1268–1279 [DOI] [PubMed] [Google Scholar]
- 13.Anderson TS, Odden M, Penko J, Kazi DS, Bellows BK, Bibbins-Domingo K. Generalizability of clinical trials supporting the 2017 american college of cardiology/american heart association blood pressure guideline. JAMA Intern Med. 2020;180:795–797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Anderson TS, Odden MC, Penko J, Kazi DS, Bellows BK, Bibbins-Domingo K. Characteristics of populations excluded from clinical trials supporting intensive blood pressure control guidelines. J Am Heart Assoc. 2021;10:e019707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Odden MC, Peralta CA, Covinsky KE. Walking speed is a useful marker of frailty in older persons--reply. JAMA Intern Med. 2013;173:325–326 [DOI] [PubMed] [Google Scholar]
- 16.Mallery LH, Allen M, Fleming I, Kelly K, Bowles S, Duncan J, Moorhouse P. Promoting higher blood pressure targets for frail older adults: A consensus guideline from canada. Cleve Clin J Med. 2014;81:427–437 [DOI] [PubMed] [Google Scholar]