Abstract
The COVID-19 pandemic in the U.S. has been largely monitored using death certificates containing reference to COVID-19. However, prior analyses reveal that a significant percentage of excess deaths associated with the pandemic were not directly assigned to COVID-19. In this study, we estimated a generalized linear model of expected mortality based on historical trends in deaths by county of residence between 2011 and 2019. We used the results of the model to generate estimates of excess mortality and excess deaths not assigned to COVID-19 in 2020 for 1470 county sets in the U.S. representing 3138 counties. Across the country, we estimated that 438,386 excess deaths occurred in 2020, among which 87.5% were assigned to COVID-19. Some regions (Mideast, Great Lakes, New England, and Far West) reported the most excess deaths in large central metros, whereas other regions (Southwest, Southeast, Plains, and Rocky Mountains) reported the highest excess mortality in nonmetro areas. The proportion assigned to COVID-19 was lowest in large central metro areas (79.3%). Regionally, the proportion of excess deaths assigned to COVID-19 was lowest in the Southeast (81.6%), Southwest (82.6%), Far West (83.7%), and Rocky Mountains (86.7%). Across the regions, the number of excess deaths exceeded the number of directly assigned COVID-19 deaths in most counties. The exception to this pattern occurred in New England, which reported more directly assigned COVID-19 deaths than excess deaths in metro and nonmetro areas. Many county sets had substantial numbers of excess deaths that were not accounted for in direct COVID-19 death counts. Estimates of excess mortality at the local level can inform the allocation of resources to areas most impacted by the pandemic and contribute to positive behavior feedback loops, such as increases in mask-wearing and vaccine uptake.
Keywords: COVID-19, Excess deaths, Mortality, Geographic inequalities, Counties
Highlights
-
•
438,386 excess deaths occurred in 2020, among which 87.5% were assigned to COVID-19.
-
•
There was substantial heterogeneity in excess death rates across counties.
-
•
The mortality impact of the Covid-19 pandemic was effectively hidden in many counties.
-
•
The percent of excess deaths assigned to COVID-19 was lowest in the South and West.
-
•
New England uniquely reported more direct COVID-19 deaths than excess deaths.
1. Introduction
Estimates of excess deaths are critical for tracking the direct and indirect effects of the COVID-19 pandemic and for developing equitable policy responses (Leon et al., 2020). Provisional estimates from the Center for Disease Control and Prevention (CDC) indicate that between 545,600 and 660,200 excess deaths occurred in the United States from January 26, 2020 to February 27, 2021 (Rossen et al., 2021). The CDC further estimates that between 75 and 88% of excess deaths were directly assigned to COVID-19 on death certificates (Rossen et al., 2021). Other prior estimates of excess mortality have also found significant discrepancies between direct COVID-19 deaths and excess mortality (Rossen et al., 2021; Stokes et al., 2021a; Weinberger et al., 2020; Woolf et al., 2020). Weinberger et al. found that 95,235 deaths were assigned to COVID-19 between March 1 and May 30, 2020 and that 122,300 excess deaths occurred, meaning that 78% of excess deaths were assigned to COVID-19 (Weinberger et al., 2020). Woolf et al. identified that 72.4% of excess deaths were assigned to COVID-19 from March 1, 2020 to January 2, 2021 (Woolf et al., 2020).
Excess deaths not assigned to COVID-19 may reflect a variety of factors, including COVID-19 deaths that were ascribed to other causes of death due to limited testing (Kiang et al., 2020), indirect deaths caused by interruptions in the provision of health care services (Friedman et al., 2021; Hartnett et al., 2020), or indirect deaths caused by the broader social and economic consequences of the pandemic (Egede & Walker, 2020; Faust et al., 2021; Matthay et al., 2021). At the state-level, the proportion of excess deaths not assigned to COVID-19 has been shown to vary significantly, suggesting that attribution of deaths to COVID-19 may not be uniform across the country (Woolf et al., 2020). For example, there were more COVID-19 deaths than excess deaths in the state of Massachusetts, whereas only 35.9% of excess deaths were assigned to COVID-19 in the state of Alaska (Woolf et al., 2020).
Estimation of excess mortality at the local level may be valuable for several reasons. First, prior studies have found that the proportion of excess deaths not assigned to COVID-19 differed significantly by county-level sociodemographic and health care factors (Stokes et al., 2021a, 2021b). Second, deaths are registered at the county-level (Curtin et al., 2019; Institute of Medicine, 2003; Stokes et al., 2021c). Thus, it is reasonable to assume that administrative differences may exist between counties in the processing of deaths. Third, county-level data may be helpful for appreciating the full burden of the COVID-19 pandemic in an area and informing community and policy interventions. Fourth, providing accurate data to residents could result in a positive behavioral feedback loop, encouraging protective actions such as wearing masks and pursuing vaccination (Gutierrez, Rubli, & Tavares, 2021).
The objective of the present study is to generate estimates of excess mortality at the local level and examine geographic variation in excess mortality and the proportion of excess deaths not assigned to COVID-19. Examining excess deaths across local areas has the potential to identify jurisdictions that have been especially hard hit by the COVID-19 pandemic and whose excess mortality has been hidden. Such estimates can be used to inform pandemic preparedness and response at the county, state, and national levels.
2. Methods
2.1. Data
We used provisional data from the National Center for Health Statistics (NCHS) on COVID-19 mortality and all-cause mortality by county of residence from January 1 to December 31, 2020 reported by June 3, 2021. We used data with a twenty-two week lag (December 31, 2020 to June 3, 2021) to improve the completeness of data, since prior analysis of provisional NCHS vital statistics reveal low completeness within the month following a death but more than 75 percent completeness after eight-weeks (Spencer & Ahmad, 2016).
COVID-19 deaths were identified using the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) code U07.1 and included deaths assigned to COVID-19 as the underlying cause as well as deaths in which COVID-19 was reported as a cause that contributed to death on the death certificate. Prior reports indicate that COVID-19 was assigned as the underlying cause on death certificates in 92% of deaths that NCHS attributed to COVID-19 (National Center for Health Statistics, 2021).
For our historical comparison period, we used CDC Wonder data on all-cause mortality by county of residence from 2011 to 2019. To compute death rates, we used data on estimated midyear populations from the U.S. Census Bureau for the years 2011 through 2020. For counties with between 1 and 9 all-cause or COVID-19 deaths in 2020 or fewer than 10 all-cause deaths in a particular year between 2011 and 2019, NCHS censored the exact number of deaths, so we used a value of 5.
To assess geographic patterns in mortality, we classified counties into 4 metropolitan‐nonmetropolitan categories and also examined patterns by Bureau of Economic Analysis (BEA) Regions (Appendix C). (Elo et al., 2019) We then stratified the regions by metropolitan‐nonmetropolitan categories to yield 32 distinct geographic units.
To provide precise estimates reflecting each county area, we aggregated small counties according to the United States Census Bureau's County Sets classification. Counties with a population of 50,000 or more stood alone, and smaller groups of counties were combined to form sets with a total population exceeding 50,000. Counties within these sets were contiguous and did not cross state borders. Our data included 3138 counties with reported all-cause mortality for 2011–2020. This translated into a final analytic sample of 1470 county sets.
The present investigation relied on de-identified publicly available data and was therefore exempted from review by the Boston University Medical Center Institutional Review Board. Analyses were conducted using R, version 3.6.3 (R Project for Statistical Computing). Additional details about the data along with programming code for replicating the analyses are available from the linked GitHub repository.
2.2. General model for county-level mortality
To generate a prediction of expected mortality in 2020, we estimated a statistical model of mortality using historical mortality data from 2011 to 2019. Specifically, we modeled mortality at the county set-year level using a quasi-poisson generalized linear model (QP-GLM) of the following form (Cameron & Trivedi, 2013; McCullagh & Nelder, 1989) (Appendix B):
Here, Yit denoted the number of all-cause deaths divided by the population of county set i in year t. In the exponent, we included a county set-specific intercept term, ⍺, which captured latent characteristics of each county set that may be correlated with mortality beyond the county-level variability in COVID-19 deaths and the proportion of excess deaths assigned to COVID-19. We included one lag of the dependent variable, Yt-1, to capture potential serial correlation in mortality. We included a time trend, t, and allowed the time trend to vary across county sets according to ꞵi. Davies et al. and Barnard et al. used a similar approach to modeling excess mortality in England (Barnard et al., 2021; Davies et al., 2021).
We used the model estimates described above to compute fitted values of total deaths and the death rate per 100,000 person-years for each county set and year from 2011 to 2020. We selected 2011 as the first year in our sample by comparing the predictive performance of our baseline Poisson GLM on 2019 mortality using different starting windows from 2009 to 2015.
2.3. Excess deaths
We defined excess deaths as the difference between the number of predicted all-cause deaths in 2020 and the number of observed all-cause deaths in 2020. For each county set in our sample, we produced an excess death rate for 2020 as well as a ratio of observed to expected deaths.
2.4. Excess deaths not assigned to COVID-19
We defined excess deaths not assigned to COVID-19 as the difference between the number of excess deaths and the number of observed directly assigned COVID-19 deaths in 2020. Next, we defined the proportion of excess deaths assigned to COVID-19 as the ratio of the direct COVID-19 death rate to the excess death rate.
3. Results
Across 1470 county-sets in the U.S. representing 3138 counties, we estimated that 438,386 excess deaths occurred in 2020. All-cause mortality was higher in most county sets in 2020 compared to predictions based on years 2011 through 2019, leading to substantial estimates of excess mortality (Appendix Fig. A1). For most county sets, excess mortality exceeded directly assigned COVID-19 mortality. Across all county sets, 87.5% of excess deaths were assigned to COVID-19, indicating that 12.5% of excess deaths were not assigned to COVID-19.
Table 1 presents summary statistics for excess mortality and excess deaths not assigned to COVID-19 across metropolitan-nonmetropolitan categories and BEA regions. Excess death rates were highest in nonmetro areas (150.7 deaths per 100,000 residents) and large metro areas (148.4 deaths per 100,000 residents) compared to small or medium metro areas (121.7 deaths per 100,000 residents) and large fringe metros (113.9 deaths per 100,000 residents). Across BEA regions, excess mortality was highest in the Mideast (188.6 deaths per 100,000 residents), Great Lakes (145.8 deaths per 100,000 residents), and Southwest (142.9 deaths per 100,000 regions) regions. Some regions (Mideast, Great Lakes, New England, and Far West) reported more excess deaths in large central metros compared to nonmetro areas. In contrast, the other regions (Southwest, Southeast, Plains, and Rocky Mountains) reported higher excess mortality in nonmetro areas compared to large central metros (Appendix Fig. A2).
Table 1.
Excess mortality and direct COVID-19 mortality by metropolitan-nonmetropolitan status and BEA region.
| Geography | Expected |
Observed |
Observed/ |
Excess |
Excess |
COVID-19 |
COVID-19 to |
N |
|---|---|---|---|---|---|---|---|---|
| Deaths | Deaths | Expected | Deaths | Per 100,000 | Deaths | Excess Ratio (%) | ||
| All | 2,943,562 | 3,381,948 | 1.15 | 438,386 | 132.4 | 383,607 | 87.5 | 1470 |
| By Metro-Nonmetro Status | ||||||||
| Lg central metro | 742,272 | 892,036 | 1.20 | 149,764 | 148.4 | 118,797 | 79.3 | 66 |
| Lg fringe metro | 684,649 | 779,034 | 1.14 | 94,385 | 113.9 | 90,102 | 95.5 | 268 |
| Md/Sm metro | 917,391 | 1,034,423 | 1.13 | 117,032 | 121.7 | 103,881 | 88.8 | 474 |
| Nonmetro | 599,250 | 676,455 | 1.13 | 77,205 | 150.7 | 70,827 | 91.7 | 662 |
| By BEA Region | ||||||||
| Far West | 419,406 | 470,729 | 1.12 | 51,323 | 89.7 | 42,937 | 83.7 | 105 |
| Great Lakes | 465,525 | 534,115 | 1.15 | 68,590 | 145.8 | 60,378 | 88.0 | 253 |
| Mideast | 439,691 | 532,077 | 1.21 | 92,386 | 188.6 | 83,457 | 90.3 | 145 |
| New England | 138,457 | 153,761 | 1.11 | 15,304 | 102.5 | 19,706 | 128.8 | 50 |
| Plains | 202,900 | 231,515 | 1.14 | 28,615 | 132.7 | 27,297 | 95.4 | 172 |
| Rocky Mountain | 91,453 | 102,808 | 1.12 | 11,355 | 90.0 | 9847 | 86.7 | 67 |
| Southeast | 849,893 | 959,353 | 1.13 | 109,460 | 127.5 | 89,318 | 81.6 | 520 |
| Southwest | 336,239 | 397,590 | 1.18 | 61,351 | 142.9 | 50,667 | 82.6 | 158 |
| Far West | ||||||||
| Lg central metro | 204,753 | 237,522 | 1.16 | 32,769 | 106.6 | 26,042 | 79.5 | 11 |
| Lg fringe metro | 63,188 | 69,674 | 1.10 | 6486 | 74.2 | 5444 | 83.9 | 14 |
| Md/Sm metro | 117,005 | 127,899 | 1.09 | 10,894 | 75.0 | 9915 | 91.0 | 47 |
| Nonmetro | 34,460 | 35,634 | 1.03 | 1174 | 36.9 | 1536 | 130.8 | 33 |
| Great Lakes | ||||||||
| Lg central metro | 115,547 | 138,880 | 1.20 | 23,333 | 181.7 | 17,988 | 77.1 | 8 |
| Lg fringe metro | 110,574 | 126,187 | 1.14 | 15,613 | 125.1 | 14,084 | 90.2 | 50 |
| Md/Sm metro | 129,980 | 146,656 | 1.13 | 16,676 | 133.2 | 15,300 | 91.7 | 73 |
| Nonmetro | 109,424 | 122,392 | 1.12 | 12,968 | 141.1 | 13,006 | 100.3 | 122 |
| Mideast | ||||||||
| Lg central metro | 124,426 | 169,593 | 1.36 | 45,167 | 279.9 | 35,932 | 79.6 | 14 |
| Lg fringe metro | 180,531 | 212,735 | 1.18 | 32,204 | 158.1 | 32,551 | 101.1 | 47 |
| Md/Sm metro | 101,069 | 112,919 | 1.12 | 11,850 | 123.3 | 11,965 | 101.0 | 51 |
| Nonmetro | 33,664 | 36,830 | 1.09 | 3166 | 110.5 | 3009 | 95.0 | 33 |
| New England | ||||||||
| Lg central metro | 13,156 | 15,962 | 1.21 | 2806 | 164.3 | 3031 | 108.0 | 2 |
| Lg fringe metro | 53,540 | 59,926 | 1.12 | 6386 | 105.4 | 8748 | 137.0 | 13 |
| Md/Sm metro | 47,293 | 52,826 | 1.12 | 5533 | 109.8 | 6854 | 123.9 | 14 |
| Nonmetro | 24,468 | 25,047 | 1.02 | 579 | 27.1 | 1073 | 185.4 | 21 |
| Plains | ||||||||
| Lg central metro | 23,236 | 27,015 | 1.16 | 3779 | 133.1 | 3097 | 82.0 | 4 |
| Lg fringe metro | 37,735 | 42,207 | 1.12 | 4472 | 99.2 | 4545 | 101.6 | 20 |
| Md/Sm metro | 52,465 | 59,792 | 1.14 | 7327 | 118.3 | 6678 | 91.1 | 38 |
| Nonmetro | 89,463 | 102,501 | 1.15 | 13,038 | 162.4 | 12,977 | 99.5 | 110 |
| Rocky Mountain | ||||||||
| Lg central metro | 11,820 | 13,645 | 1.15 | 1825 | 95.0 | 1399 | 76.6 | 2 |
| Lg fringe metro | 14,487 | 16,901 | 1.17 | 2414 | 104.9 | 1934 | 80.1 | 6 |
| Md/Sm metro | 40,629 | 44,706 | 1.10 | 4077 | 72.6 | 3956 | 97.0 | 23 |
| Nonmetro | 24,517 | 27,556 | 1.12 | 3039 | 109.4 | 2558 | 84.2 | 36 |
| Southeast | ||||||||
| Lg central metro | 122,205 | 140,196 | 1.15 | 17,991 | 117.3 | 14,008 | 77.9 | 17 |
| Lg fringe metro | 177,621 | 198,856 | 1.12 | 21,235 | 98.5 | 17,984 | 84.7 | 93 |
| Md/Sm metro | 339,726 | 379,750 | 1.12 | 40,024 | 124.2 | 32,469 | 81.1 | 185 |
| Nonmetro | 210,341 | 240,551 | 1.14 | 30,210 | 180.7 | 24,857 | 82.3 | 225 |
| Southwest | ||||||||
| Lg central metro | 127,130 | 149,223 | 1.17 | 22,093 | 113.9 | 17,300 | 78.3 | 8 |
| Lg fringe metro | 46,973 | 52,548 | 1.12 | 5575 | 81.8 | 4812 | 86.3 | 25 |
| Md/Sm metro | 89,224 | 109,875 | 1.23 | 20,651 | 198.6 | 16,744 | 81.1 | 43 |
| Nonmetro | 72,912 | 85,944 | 1.18 | 13,032 | 206.0 | 11,811 | 90.6 | 82 |
Notes: Aggregated results by various geographic regions. Aggregate rates are computed by summing actual and predicted counts over counties in a particular region and dividing by the summed population. Note that this is equivalent to the population-weighted means of the county-level rates. COVID-19 deaths refer to deaths that appeared as either an underlying or contributing cause on the death certificate.
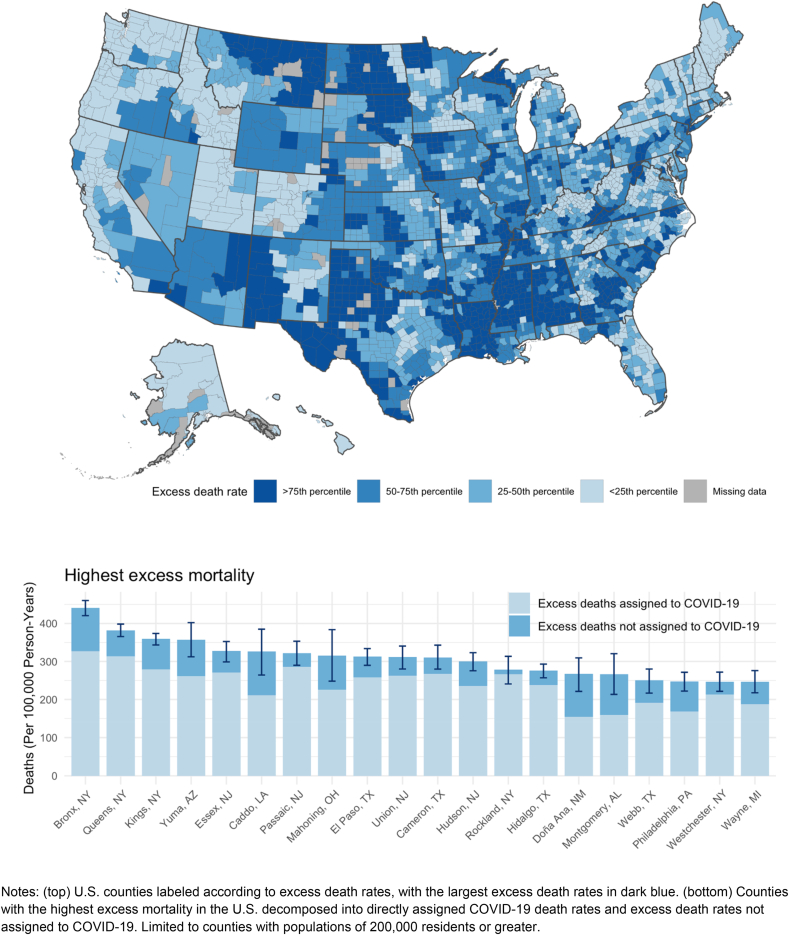
Fig. 1 is a map of excess death rates in the U.S. This figure highlights the geographic dispersion of the COVID-19 pandemic. The figure also identifies specific county sets with the highest excess mortality such as Bronx and Queens, New York. Appendix Table A1 presents summary statistics on excess mortality for each state.
Fig. 1.
Excess mortality rates across U.S. Counties.
Notes: (top) U.S. counties labeled according to excess death rates, with the largest excess death rates in dark blue. (bottom) Counties with the highest excess mortality in the U.S. decomposed into directly assigned COVID-19 death rates and excess death rates not assigned to COVID-19. Limited to counties with populations of 200,000 residents or greater.
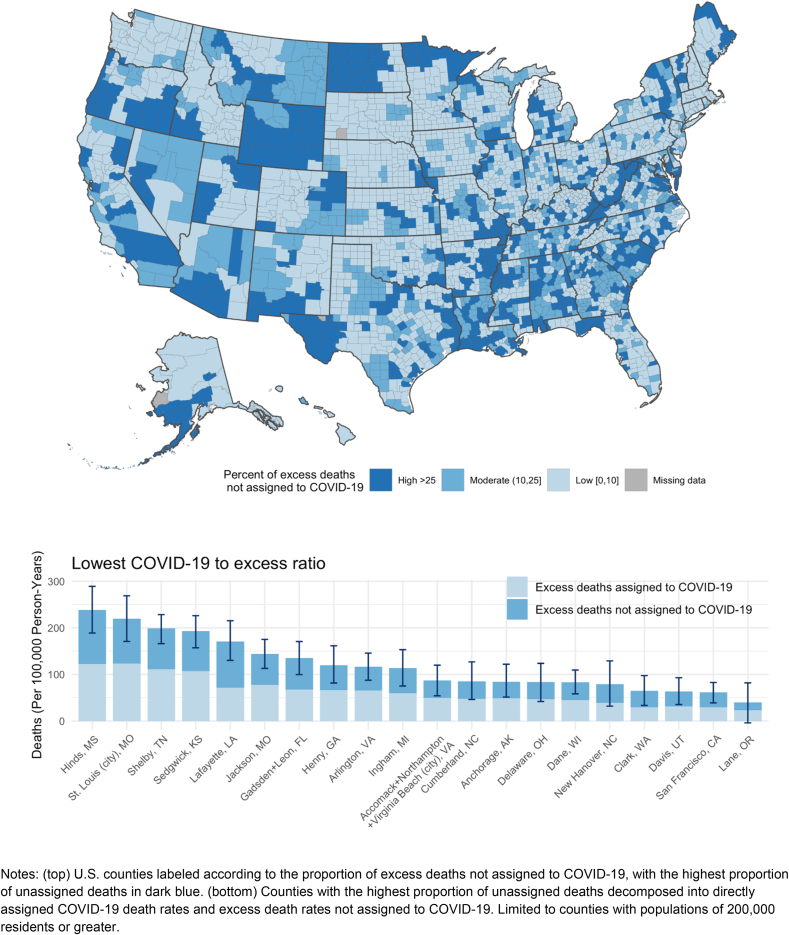
There was also significant variation in the proportion of excess deaths assigned to COVID-19 across county sets in the U.S. Across the country, 91.2 million U.S. residents lived in counties where less than 75% of excess deaths were assigned to COVID-19 (Appendix Table A2). On average, Table 1 shows that assignment of excess deaths to COVID-19 was lowest in large central metro areas (79.3%) compared to medium or small metros (88.8%), nonmetro areas (91.7%) and large fringe metros (95.5%). Regionally, the proportion of excess deaths assigned to COVID-19 was lowest in the Southeast (81.6%), Southwest (82.6%), Far West (83.7%), and Rocky Mountains (85.2%).
Fig. 2 is a map of the proportion of excess deaths not assigned to COVID-19 across counties in the U.S., labeling counties as having high, moderate, or low proportions of unassigned deaths. The figure also identifies county sets with the lowest proportion of excess deaths assigned to COVID-19. These counties are disproportionately in southern regions.
Fig. 2.
Proportion of excess deaths not assigned to COVID-19 across U.S. Counties.
Notes: (top) U.S. counties labeled according to the proportion of excess deaths not assigned to COVID-19, with the highest proportion of unassigned deaths in dark blue. (bottom) Counties with the highest proportion of unassigned deaths decomposed into directly assigned COVID-19 death rates and excess death rates not assigned to COVID-19. Limited to counties with populations of 200,000 residents or greater.
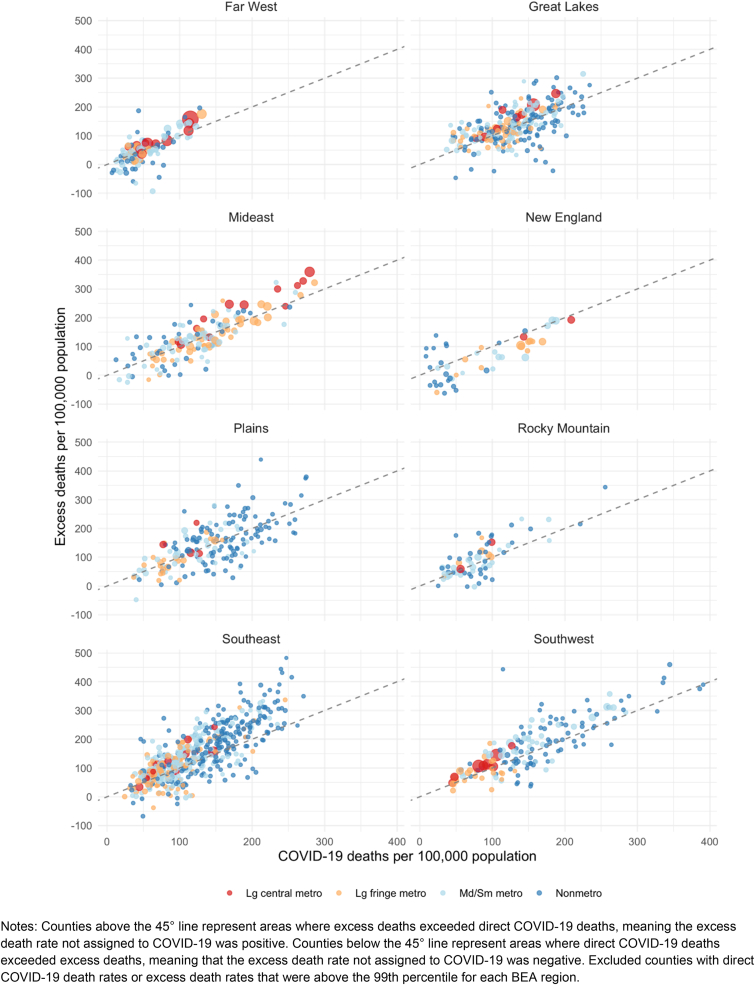
Fig. 3 plots excess death rates against directly assigned COVID-19 death rates for each county set in each BEA region. In these plots, counties above the 45-degree line represent county sets where excess deaths exceeded directly assigned COVID-19 deaths, meaning that excess deaths not assigned to COVID-19 occurred in these areas. In all regions except New England, most county sets had excess deaths not assigned to COVID-19. In New England, 185.4% were assigned to COVID-19 in nonmetro areas, 137.0% in large fringe metro areas, 123.9% in medium or small metros, and 108.0% in large central metro areas (Appendix Fig. A2). Two types of county sets emerged among those with negative excess death rates not assigned to COVID-19: (1) nonmetro counties with low direct COVID-19 death rates where excess death rates were negative, and (2) metro counties with positive excess death rates and substantial numbers of direct COVID-19 deaths that exceeded the number of excess deaths.
Fig. 3.
Plots of Excess Death Rates vs. Direct COVID-19 Death Rates by BEA Region.
Notes: Counties above the 45° line represent areas where excess deaths exceeded direct COVID-19 deaths, meaning the excess death rate not assigned to COVID-19 was positive. Counties below the 45° line represent areas where direct COVID-19 deaths exceeded excess deaths, meaning that the excess death rate not assigned to COVID-19 was negative. Excluded counties with direct COVID-19 death rates or excess death rates that were above the 99th percentile for each BEA region.
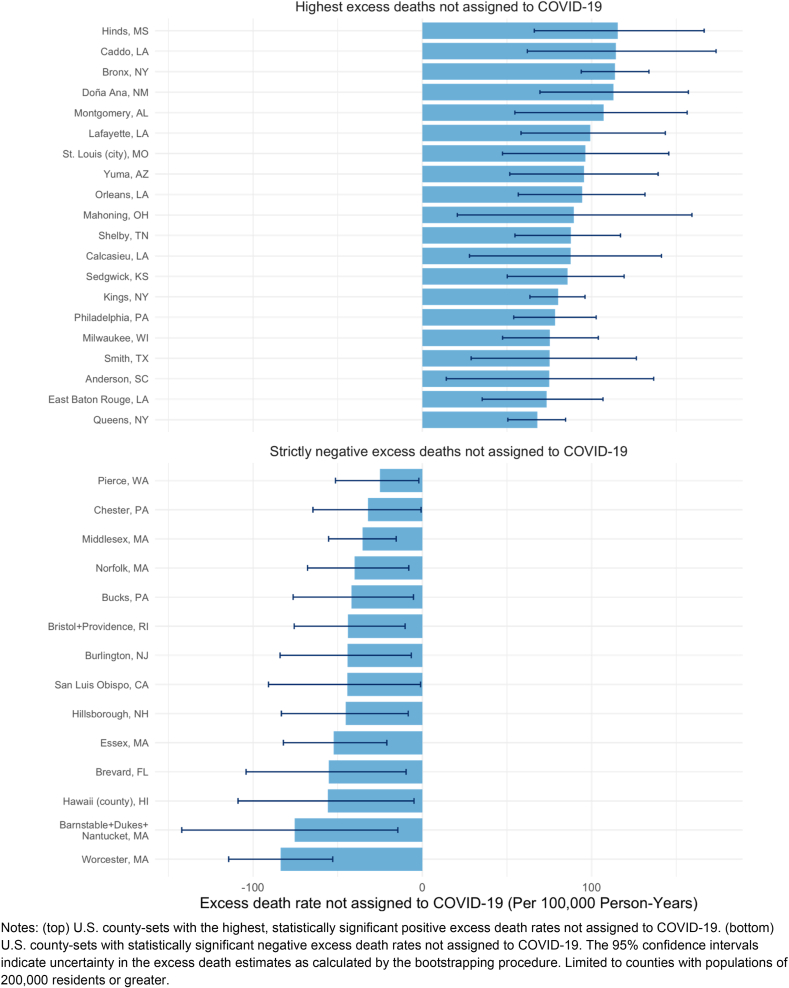
Fig. 4 decomposes excess death rates for county sets with the highest excess death rates not assigned to COVID-19 and the most negative excess death rates not assigned to COVID-19. Counties with large, negative excess mortality not assigned to COVID-19 were mostly in the New England region. Appendix Figs. A3 and A4 display a time series of observed death rates from 2011 to 2019 and a comparison of the 2020 predicted death rate and the 2020 expected death rate for large county sets across the U.S.
Fig. 4.
U.S. Counties with the highest excess death rates not assigned to COVID-19 and statistically significant negative excess death rates not assigned to COVID-19.
Notes: (top) U.S. county-sets with the highest, statistically significant positive excess death rates not assigned to COVID-19. (bottom) U.S. county-sets with statistically significant negative excess death rates not assigned to COVID-19. The 95% confidence intervals indicate uncertainty in the excess death estimates as calculated by the bootstrapping procedure. Limited to counties with populations of 200,000 residents or greater.
Only 48 county sets, representing less than 2% of the U.S. population (5.5 million residents) experienced negative excess mortality (observed mortality was less than expected). Among these county sets, none had statistically significant negative excess death rates. Appendix Table D1 provides estimates of excess death rates and their uncertainty intervals for 1470 county sets across the U.S.
4. Discussion
In this study, we produced county set level estimates of excess mortality and the proportion of excess deaths not assigned to COVID-19 and examined geographic variation in mortality across the United States. In total, we estimated that 438,386 total excess deaths occurred in 2020, of which 87.5% were assigned to COVID-19. This number is similar to the 458,000 excess deaths estimated by Islam et al.(Islam et al., 2021). Variation in estimates of excess deaths is partly a function of differences in the historical time period used to predict the expected number of deaths. A recent analysis by Woolf et al. used trends from 2014 to 2019 to estimate 522,368 excess deaths between March 1, 2020, and January 2, 2021 (Woolf et al., 2020). Using data from 1999 to 2020 and a cubic model, Glei identified 402,743 excess deaths in 2020 (Glei, 2021). Ahmad et al. found an increase of 503,976 deaths between 2019 and 2020 without controlling for recent mortality trends (Ahmad, 2021). As noted above, we chose the period used in our model (2011 through 2019) based on experimentation to determine which period was most successful in predicting deaths in 2019.
Our study reveals substantial heterogeneity in excess deaths and the proportion of excess deaths not assigned to COVID-19 across counties, which are the administrative unit for death registration. This result highlights the value of local-area estimates of excess mortality as state and national-estimates mask significant variability.
There are several potential explanations for the discrepancy between excess mortality and directly assigned COVID-19 mortality observed in this study. One explanation is that the gap reflects underreporting of COVID-19 deaths. Especially early in the pandemic, testing was severely limited. Underreporting may have also related to a lack of awareness of the clinical manifestations of COVID-19 as well as various social, health care, and political factors (Boukhris et al., 2020; Stokes et al., 2021a, 2021b). The gaps may also be explained by the indirect effects of the pandemic on mortality levels. Indirect effects could relate to interruptions or delays in health care or the broader social and economic upheaval caused by the pandemic, including loss of employment, social isolation and loneliness, and other factors (Lange et al., 2020; Wolfson & Leung, 2020; Wu, 2020). Wolfson et al. found that food insecurity has increased substantially during the COVID-19 pandemic, which could contribute to a range of health concerns (Wolfson & Leung, 2020). Lange et al. identified a 42% decline in emergency department visits during the early pandemic, suggesting that life-threatening health conditions may have gone untreated and resulted in indirect deaths (Lange et al., 2020). Wu argued that social isolation and loneliness were major risk factors for older adults during the pandemic and may have contributed to poor physical health status, including mortality (Wu, 2020). NCHS data suggest that approximately 19,000 more deaths from unintentional injuries occurred in 2020 than in 2019 (Ahmad, 2021).
We also observed numerous counties in which the direct COVID-19 death rate exceeded our estimates of excess mortality, especially in New England. A similar pattern was observed internationally, with countries such as New Zealand and Taiwan having few direct COVID-19 deaths and negative excess mortality while countries such as Luxembourg, France, Belgium, and Costa Rica had positive excess mortality but their direct COVID-19 death rates exceeded their excess death rates (Sanmarchi et al., 2021). This finding could have occurred for several reasons. First, increases in mortality in 2020 due to COVID-19 may have been offset by declines in deaths from other causes (e.g. influenza, traffic deaths, and suicide) (Ahmad, 2021; Olsen et al., 2020; Yasin et al., 2021). Shelter-in-place policies may have also been associated with reductions in non-natural deaths (Catalano et al., 2021). Several of the counties with negative excess death rates not assigned to COVID-19 stood out as economically privileged areas that may have been isolated from the pandemic through an ability to work-from-home and avoid household crowding. It is also possible that medical certifiers in some counties over-assigned COVID-19 to death certificates. Differences could also relate to how directly assigned COVID-19 deaths were counted by NCHS. In about 8% of cases, COVID-19 was listed as something other than the underlying cause (National Center for Health Statistics, 2021). Frailty selection may have also occurred if deaths from COVID-19 occurred among individuals who were likely to die from other causes. Finally, non-linear trends in mortality over recent years may have biased our estimate of expected mortality, affecting our estimate of excess deaths.
Accurate county-level assessments of excess mortality are an important addition to existing research on excess mortality at the state and national level. County-level estimates of excess mortality may enable researchers to examine geographic variation in excess mortality and leverage variation in sociodemographic, health, and structural factors to examine inequities. They may also be relevant to local public health departments and play an important role in motivating individual and community responses, including mask wearing and vaccine uptake. Our study indicates that direct COVID-19 death rates have been less accurate measures of excess mortality in areas such as the Southeast and Rocky Mountain regions, which are also areas that are experiencing slower vaccine uptake (U.S. Department of Health & Human Services, 2021).
4.1. Limitations
This analysis had several limitations. First, the present study used cumulative data for all of 2020, and thus, it was not possible to examine changes in excess mortality over time. Examining trends in excess mortality using small-area data is a priority for future research. Second, an important caveat of this study is that age structure differs across counties. Since COVID-19 mortality is more common in older populations, some of the patterns observed across counties may simply reflect differences in age structure. Thus, an important future direction is to age standardize county-level estimates when age-specific mortality data become available. Indirect age standardization procedures could be used in the absence of county-level age-specific death rates. Demographic and socioeconomic variables could also be included in future versions of the model as explanatory variables. Third, the provisional county-level mortality files released by the NCHS did not include information on cause of death, and therefore it was not possible to disentangle the sources of excess deaths in 2020. Decomposing excess deaths by cause of death will be critical to understanding why some counties have a higher fraction of deaths unassigned to COVID-19 than others and the extent to which the discrepancies are explained by COVID-19 death undercounts versus indirect pandemic effects. Finally, the data used in the present study are provisional in nature and may be subject to further corrections by the NCHS.
5. Conclusion
In conclusion, the present study builds on prior work by extending estimates of excess mortality and excess deaths not assigned to COVID-19 to US county sets. The added geographic detail of these estimates compared to prior studies may facilitate research on the causes and consequences of the COVID-19 pandemic on population health and provide useful data for local area health policy and planning. Estimates of excess mortality at the local level can also inform the allocation of resources to areas most impacted by the pandemic and contribute to positive protective behavior feedback loops, such as increases in mask-wearing and vaccine uptake. In doing so, they can inform the response to the COVID-19 pandemic and to any future pandemics that the country may face.
The present investigation relied on de-identified publicly available data and was therefore exempted from review by the Boston University Medical Center Institutional Review Board.
Funding disclosure
The Robert Wood Johnson Foundation supported the research reported in this publication (Grant #77521).
Disclosure and Acknowledgements
The authors would like to thank Robert N. Anderson and Farida B. Ahmad from the National Center for Health Statistics, Katherine Hempstead from the Robert Wood Johnson Foundation (RWJF), and Abe Dunn from the Bureau of Economic Analysis (BEA) for their input and technical support. Dr. Stokes gratefully acknowledges financial support from the RWJF. The authors would also like to thank Elif Coskun for her editorial assistance during the preparation of the manuscript. The views expressed in this paper are those of the authors and not necessarily the views of RWJF, the U.S. Bureau of Economic Analysis, or the U.S. Department of Commerce.
Access to data/code for replication
Additional details about the data along with programming code for replicating the analyses of the present study can be accessed at the following GitHub repository: https://github.com/Mortality-Surv-and-Reporting-Proj/county-level-estimates-of-excess-mortality.
Authorship contribution statement
Calvin A. Ackley: Conceptualization, Methodology, Formal Analysis, Writing – Original Draft, Visualization. Dielle J. Lundberg: Conceptualization, Data Curation, Writing – Original Draft. Lei Ma: Conceptualization, Methodology, Formal Analysis, Visualization. Irma T. Elo: Conceptualization, Methodology, Writing – Review & Editing. Samuel H. Preston: Conceptualization, Methodology, Writing – Review & Editing. Andrew C. Stokes: Conceptualization, Methodology, Writing – Original Draft, Visualization, Supervision, Project Administration, Funding Acquisition.
Declaration of competing interest
A. C. Stokes reported receiving grants from Johnson & Johnson, Inc. and Swiss Re outside the submitted work. No other disclosures were reported.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2021.101021.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Ahmad F.B. Provisional mortality data — United States, 2020. MMWR Morb Mortal Wkly Rep. 2021:70. doi: 10.15585/mmwr.mm7014e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnard S., Chiavenna C., Fox S., et al. Methods for modelling excess mortality across England during the COVID-19 pandemic. Stat Methods Med Res. Published online October. 2021;23 doi: 10.1177/09622802211046384. 09622802211046384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boukhris M., Hillani A., Moroni F., et al. Cardiovascular implications of the COVID-19 pandemic: A global perspective. Canadian Journal of Cardiology. 2020;36(7):1068–1080. doi: 10.1016/j.cjca.2020.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron A.C., Trivedi P.K. Cambridge University Press; 2013. Econometric society monographs: Regression analysis of count data series number 30. [DOI] [Google Scholar]
- Catalano R, Maria Glymour M, Chen Y-H, Bibbins-Domingo K. Sheltering in place and the likelihood of nonnatural death. American Journal of Epidemiology. Published online 2021. doi:10.1093/aje/kwab062. [DOI] [PMC free article] [PubMed]
- Davies B., Parkes B.L., Bennett J., et al. Community factors and excess mortality in first wave of the COVID-19 pandemic in England. Nature Communications. 2021;12(1):3755. doi: 10.1038/s41467-021-23935-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egede L.E., Walker R.J. Structural racism, social risk factors, and Covid-19 - a dangerous convergence for Black Americans. New England Journal of Medicine. 2020;383(12):e77. doi: 10.1056/NEJMp2023616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elo I.T., Hendi A.S., Ho J.Y., Vierboom Y.C., Preston S.H. Trends in non-hispanic white mortality in the United States by metropolitan-nonmetropolitan status and region, 1990-2016. Population and Development Review. 2019;45(3):549–583. doi: 10.1111/padr.12249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faust J.S., Du C., Mayes K.D., et al. Mortality from drug overdoses, homicides, unintentional injuries, motor vehicle crashes, and suicides during the pandemic, March-August 2020. JAMA. 2021;326(1):84–86. doi: 10.1001/jama.2021.8012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman A.B., Barfield D., David G., et al. Delayed emergencies: The composition and magnitude of non-respiratory emergency department visits during the COVID-19 pandemic. J Am Coll Emerg Physicians Open. 2021;2(1) doi: 10.1002/emp2.12349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtin SC, Tolson GC, Arias E, Anderson RN. Funeral directors' handbook on death registration and fetal death reporting : 2019 revision. Published online March 2019. https://www.cdc.gov/nchs/data/nvss/handbook/2019-Funeral-Directors-Handbook-508.pdf.
- Gutierrez E, Rubli A, Tavares T. Information and behavioral responses during a pandemic: Evidence from delays in COVID-19 death reports. Journal of Development Economics. 2021 doi: 10.2139/ssrn.3645317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartnett K.P., Kite-Powell A., DeVies J., et al. Impact of the COVID-19 pandemic on emergency department visits - United States, January 1, 2019-may 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23):699–704. doi: 10.15585/mmwr.mm6923e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine . The National Academies Press; 2003. Medicolegal death investigation system: Workshop summary. [PubMed] [Google Scholar]
- Islam N., Shkolnikov V.M., Acosta R.J., et al. Excess deaths associated with covid-19 pandemic in 2020: Age and sex disaggregated time series analysis in 29 high income countries. BMJ. 2021;373:n1137. doi: 10.1136/bmj.n1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiang M.V., Irizarry R.A., Buckee C.O., Balsari S. Every body counts: Measuring mortality from the COVID-19 pandemic. Annals of Internal Medicine. 2020;173(12):1004–1007. doi: 10.7326/M20-3100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lange S.J., Ritchey M.D., Goodman A.B., et al. Potential indirect effects of the COVID-19 pandemic on use of emergency departments for acute life-threatening conditions — United States, January–may 2020. MMWR Morbidity and Mortality Weekly Report. 2020;69(25):795–800. doi: 10.15585/mmwr.mm6925e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leon D.A., Shkolnikov V.M., Smeeth L., Magnus P., Pechholdová M., Jarvis C.I. COVID-19: A need for real-time monitoring of weekly excess deaths. Lancet. 2020;395(10234) doi: 10.1016/S0140-6736(20)30933-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthay E.C., Duchowny K.A., Riley A.R., Galea S. Projected all-cause deaths attributable to COVID-19-related unemployment in the United States. American Journal of Public Health. 2021;111(4):696–699. doi: 10.2105/AJPH.2020.306095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics Provisional death counts for Coronavirus Disease (COVID-19) technical notes. 2021. https://www.cdc.gov/nchs/nvss/vsrr/covid19/tech_notes.htm Published January 19.
- Olsen S.J., Azziz-Baumgartner E., Budd A.P., et al. Decreased influenza activity during the COVID-19 pandemic — United States, Australia, Chile, and South Africa, 2020. MMWR Morbidity and Mortality Weekly Report. 2020;69(37):1305–1309. doi: 10.15585/mmwr.mm6937a6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossen L.M., Branum A.M., Ahmad F.B., Sutton P.D., Anderson R.N. Notes from the field: Update on excess deaths associated with the COVID-19 pandemic - United States, January 26, 2020-February 27, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(15):570–571. doi: 10.15585/mmwr.mm7015a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanmarchi F., Golinelli D., Lenzi J., et al. Exploring the gap between excess mortality and COVID-19 deaths in 67 countries. JAMA Network Open. 2021;4(7) doi: 10.1001/jamanetworkopen.2021.17359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spencer M.R., Ahmad F. Timeliness of death certificate data for mortality surveillance and provisional estimates. National Vital Statistics Rapid Release. 2016;1 [Google Scholar]
- Stokes A.C., Lundberg D.J., Bor J., Bibbins-Domingo K. Excess deaths during the COVID-19 pandemic: Implications for US death investigation systems. American Journal of Public Health. 2021;111(S2):S53–S54. doi: 10.2105/AJPH.2021.306331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCullagh P., Nelder J.A. Generalized linear models. 2nd edition. Chapman and Hall. Published online; London: 1989. [Google Scholar]
- Glei DA. The US midlife mortality crisis continues: Increased death rates from causes other than COVID-19 during 2020. medRxiv. Published online July 26, 2021. doi:10.1101/2021.05.17.21257241.
- Stokes AC, Lundberg DJ, Bor J, Elo IT, Hempstead K, Preston SH. Association of Health Care Factors With Excess Deaths Not Assigned to COVID-19 in the US. JAMA Netw Open. 2021;4(9):e2125287. doi: 10.1001/jamanetworkopen.2021.25287. https://scholar.google.com/scholar?q=Stokes%20AC,%20Lundberg%20DJ,%20Bor%20J,%20Elo%20IT,%20Hempstead%20K,%20Preston%20SH.%20Association%20of%20health%20care%20factors%20with%20excess%20deaths%20not%20assigned%20to%20COVID-19.%20JAMA%20Network%20Open;%20Forthcoming.%20Published%20online%202021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stokes A.C., Lundberg D.J., Elo I.T., Hempstead K., Bor J., Preston S.H. COVID-19 and excess mortality in the United States: A county-level analysis. PLoS Medicine. 2021;18(5) doi: 10.1371/journal.pmed.1003571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health & Human Services . 2021. ASPE Predictions of Vaccine Hesitancy for COVID-19 Vaccines by Geographic and Sociodemographic Features.https://aspe.hhs.gov/pdf-report/vaccine-hesitancy Published April 6. [Google Scholar]
- Weinberger D.M., Chen J., Cohen T., et al. Estimation of excess deaths associated with the COVID-19 pandemic in the United States, March to may 2020. JAMA Internal Medicine. 2020;180(10):1336–1344. doi: 10.1001/jamainternmed.2020.3391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfson J.A., Leung C.W. Food insecurity and COVID-19: Disparities in early effects for US adults. Nutrients. 2020;12(6) doi: 10.3390/nu12061648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolf SH, Chapman DA, Sabo RT, Zimmerman EB. Excess deaths from COVID-19 and other causes in the US, March 1, 2020, to January 2, 2021. JAMA. Published online April 2, 2021. doi:10.1001/jama.2021.5199. [DOI] [PMC free article] [PubMed]
- Wu B. Social isolation and loneliness among older adults in the context of COVID-19: A global challenge. Glob Health Res Policy. 2020;5:27. doi: 10.1186/s41256-020-00154-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yasin Y.J., Grivna M., Abu-Zidan F.M. Global impact of COVID-19 pandemic on road traffic collisions. World Journal of Emergency Surgery. 2021;16(1):51. doi: 10.1186/s13017-021-00395-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.