Abstract
The COVID-19 pandemic caused the suspension at all levels of the Catalan FIT-based CRC screening program on March 12, 2020. Screening invitations to FIT were resumed on September 1, 2020. We aimed to assess the short-term impact of the pandemic and describe strategies implemented to minimize harm by the disruption of the FIT-based CRC screening in the Metropolitan Area of Barcelona. We analyzed participation rate, colonoscopy adherence, time intervals to colonoscopy, detection rates, and advanced-stage cancers in 2019 and 2020. To identify perceived distress levels during the suspension of the screening we conducted a phone interview. As a result of the suspension, 43% of the individuals due for screening did not receive their invitation by December 31, 2020. A percent decrease of 5.1% in participation and of 8.9% in colonoscopy adherence among invitees between January–March was observed, with a recovery to 2019 levels when the screening activities were restarted. The time interval between a positive test to colonoscopy was longer in 2020 than in 2019. A decrease in advanced neoplasia rate and an increase in later stages of CRC were also observed. Individuals with a positive test did not report higher levels of perceived distress compared to those with a negative test. Although the disruption of screening had a temporary impact on participation and colonoscopy adherence, timing delay continues and a large backlog in the invitation of the target population remains. Thus, it is critical to implement strategies to minimize the long-term effects.
Keywords: COVID-19, Coronavirus, Colorectal cancer, Screening, Colonoscopy, Fecal immunochemical test
1. Background
The Director-General of the World Health Organization (WHO) on March 11, 2020, declared the novel coronavirus disease 2019 (COVID-19) as a global pandemic (WHO, 2020). In Catalonia (Spain), after the first confirmed case at the end of February 2020, the rapid spread of the COVID-19 pandemic struck the health system capacity (Updated SARS-CoV-2 data, n.d.). One of the health services most severely impacted by COVID-19 was cancer screening. Similar to most European countries hit by the COVID-19 pandemic (Puricelli Perin et al., 2021), the FIT-based CRC screening program in Catalonia was suspended at all levels on March 12, 2020. Due to the relocation of professionals from endoscopy units to care for people infected with the coronavirus, the sending of invitations to FIT screening was suspended, but also the deferral of diagnostic colonoscopies among individuals with a positive FIT result and further adjournment of those invitees with an incomplete FIT screening.
The potential effects of a screening disruption can be immediate, mid-, or long-term. Among short-term screening outcomes that may be affected are a decrease in participation to FIT and adherence to diagnostic colonoscopy. Some recent studies have shown decreases of 3.5 to 4 percentage points in FIT screening participation and larger decreases to diagnostic colonoscopy acceptance after a positive FIT result due to the first wave of COVID-19 (Cheng et al., 2021; Kortlever et al., 2021). Whereas different levels of perceived distress exist during different steps of a FIT-based CRC screening (Vermeer et al., 2020), the suspension of the screening may have increased distress of individuals because of the diagnostic delay.
Furthermore, medium to long-term potential effects of COVID-19-related disruptions to CRC screening is its impact on CRC incidence and mortality (de Jonge et al., 2021). Limiting time between a positive FIT result and colonoscopy completion is essential to reduce both the incidence of CRC and the stage at diagnosis (Ricciardiello et al., 2021; Forbes et al., 2021). In this study, we aimed to assess the short-term impact of COVID-19 on participation, colonoscopy adherence, time delays, detection rates, stage distribution of CRC, and perceived distress levels in a FIT-based CRC screening hub in the Metropolitan Area of Barcelona. We also described strategies implemented to minimize harm by the disruption of screening.
2. Methods
2.1. Setting and screening procedure
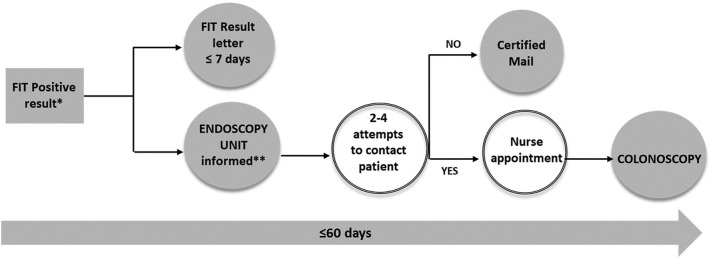
In 2000, Catalonia launched a stool-based CRC screening program among women and men aged 50–69 years, and currently, ten coordinating hubs provide screening services in the entire Catalan territory. The CRC screening hub of the Catalan Institute of Oncology is one of the largest hubs in Catalonia, covering a target population of approximately 495,000 men and women aged 50–69 years in the Metropolitan Area of Barcelona. An invitation letter is sent biennially to pick up and complete a FIT kit at a collaborating pharmacy. A cutoff of 20 μg Hb/g feces is used to determine positivity on the FIT, and those with a positive test result are referred for diagnostic colonoscopy. Participants with a negative FIT result receive a recommendation letter for biennial screening while individuals with a positive FIT receive a result letter within 7 days. In parallel, endoscopic units of reference hospitals are informed about individuals with a positive FIT result through the CRC screening computer system. Nurses contact participants up to four times by phone for a pre-colonoscopy interview, where the participant's risks are assessed, and instructions are given for colonoscopy bowel preparation. When a participant cannot be contacted, a registered letter is sent with a recommendation for a diagnostic colonoscopy (Supplementary Fig. 1).
Supplementary Fig. 1.
Algorithm of the procedure from detection of a positive FIT result to performance of diagnostic colonoscopy. * Registry of FIT-positive participants with real-time updates; ** Risks and bowel preparation explained.
On March 12, 2020, invitations to FIT screening in the Metropolitan Area of Barcelona were paused, and on March 16, 2020, diagnostic colonoscopies from the screening process were discontinued.
2.2. Strategies to minimize harm due to disruption of the CRC screening program
Three strategies were implemented to minimize the diagnostic delay impact, to prompt participation among those whose screening was incomplete, and to reduce the backlog due to the suspension.
To minimize the diagnostic delay impact, when endoscopic activity was resumed in early May, individuals with a FIT result of 160 μg Hb/g feces and higher were prioritized to schedule colonoscopy, followed by results between 80 and 160 μg Hb/g feces (Crespo et al., 2020).
To prompt participation among individuals whose screening was incomplete, an SMS reminder strategy was implemented at the end of July 2020, when FIT kit pick-up and delivery at community pharmacies resumed. SMS reminders to complete and return the kit at the pharmacy (to those who had already picked it up before the suspension of the program) and SMS reminders for participation (to those who had not yet picked up the FIT when the program was paused) were sent if a mobile phone number was registered.
To reduce the screening activity of endoscopic units by 25% and eventually reduce the backlog of invitations to screening, the positivity threshold was increased from 20 μg Hb/g feces to 31 μg Hb/g feces on September 1, 2020, as the COVID-19 pandemic was still going on.
2.3. Outcomes
We used the data from the Information System for Monitoring CRC Screening from 2019 and 2020. The following outcomes were calculated: proportion of invitees, participation rate, colonoscopy adherence rate, CRC, advanced adenoma, and advanced neoplasia detection rate, the proportion of Advanced- CRC, time to diagnostic colonoscopy, and perceived distress levels.
The proportion of invitees was the number of invitations sent out among the total number of planned invitations. The participation rate was measured as the number of individuals with a FIT result divided by the total invitees. Colonoscopy adherence rate was calculated as the number of individuals with a colonoscopy result divided by the total number of individuals with a positive FIT result. CRC, advanced adenoma, and advanced neoplasia detection rates were calculated as the number of CRC, advanced adenoma, or advanced neoplasia per 1000 participants, respectively. We calculated the proportion of CRC advanced stage as the number of CRC in stages III and IV among the total number of CRC detected. The time to diagnostic colonoscopy was the interval in days between the FIT-positive result date and colonoscopy performance date.
Perceived distress was measured with the Spanish version of the Perceived Stress Scale-10 (PSS-10) as used by Remor (2006). A PSS-10 total score from 0 to 40 was obtained by summing all 10 items. Higher scores indicate a higher level of perceived distress. To calculate distress from the PSS-10 scale, we excluded observations with any missing values, and therefore we performed a sensitivity analysis to test the robustness of the results under a reasonable worst-case scenario. Distress levels were recoded into two categories based on the second tertile within the control group; that is scores under or equal to 13 or above 13. In addition, this cutoff was consistent with other studies that classified low self-perceived stress scores ranging from 0 to 13 and moderate/high self-perceived stress scores ranging from 14 to 40 (NH Department of Administrative Services, 2020; Perera et al., 2017).
2.4. Data analysis
Participation, colonoscopy adherence, and detection rates with 95% confidence intervals (CIs) were calculated for individuals invited throughout 2020, from January to March 2020, and from September to December 2020 and were compared with data from 2019 (January to March, September to December and overall rates). Time-to-event analysis was conducted from the FIT result date and the first colonoscopy scheduled date. Time to diagnostic colonoscopy was described using Kaplan-Meier estimates, and differences between invitation periods of 2019 and 2020 were compared using the log-rank test. Univariable and multivariable logistic regression models were used to examine factors associated with higher levels of perceived distress (> 13), and odds ratios (ORs) and their 95% confidence intervals (CIs) were reported. Finally, a descriptive analysis to assess the impact of recovery strategies (SMS) on participation was performed.
The statistical analysis was performed using Stata 15 (StataCorp. 2017. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC).
3. Results
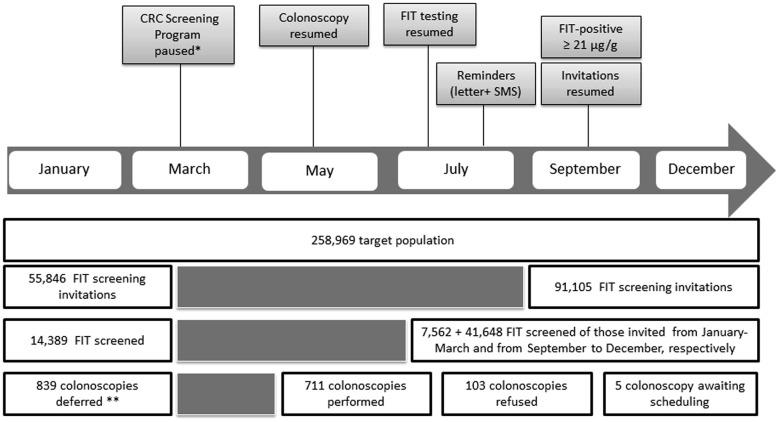
Due to the first wave of the COVID-19 pandemic, 43% (111,000 / 258,969) of the target population for CRC screening in 2020, were not invited by December 31, 2020. Between January 1 and March 12, 2020, 14,389 out of 55,846 individuals invited had completed FIT kit screening before the suspension (25.8%), and from the resumption to the end of 2020, a further total of 7562 individuals completed a FIT kit (13.5%). At the time of the pause, 839 participants with a positive FIT result had their colonoscopy deferred (Fig. 1 ).
Fig. 1.
Flowchart of CRC screening in the Metropolitan Area of Barcelona at the onset of the COVID-19 pandemic.
* Registry of FIT-positive participants with real-time updates; ** Risks and bowel preparation explained.
To prompt participation during the recovery period, we sent an SMS reminder to 34,063 individuals with a mobile phone number registered in our database (82.2% of individuals whose screening was incomplete). Around 90% of SMSs reminders were successfully delivered (n = 30,597) and participation reached 19.7% (95% CI: 19.3–20.2). Participation among who did not received SMS (n = 7394) was 14.3% (95% CI, 13.6–15.0).
The participation rate declined by 5.1% between January and March 2020 but it increased significantly, higher than expected, from September to December in comparison with the global participation of 2019.
Colonoscopy adherence rates between January and March 2020 dropped by 8.9% as compared to 2019 but they returned to normal levels after the suspension.
Among individuals with a FIT positive result, the 90th percentile time to colonoscopy was 155 days compared to 57 days in 2019. After the suspension, the 90th percentile time to colonoscopy was longer than 60 days (standard time).
Between January and March 2020, the advanced neoplasia detection rate was as expected. However, with the restart of screening and the increased FIT positivity threshold, the detection rate dropped to 15.2‰ (Table 1 ).
Table 1.
Main screening outcomes of CRC screening before and after the disruption of the CRC screening program in the Metropolitan Area of Barcelona.
| 2020 |
2019 |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Screening outcome |
January–March |
September–December |
Global |
January–March |
September–December |
Global |
||||||
| N | % (95% CI) | N | % (95% CI) | N | % (95% CI) | N | % (95% CI) | N | % (95% CI) | N | % (95% CI) | |
| Participation to FIT | 55,846 | 39.3 (38.9–39.7) | 91,105 | 45.7 (45.4–46) | 147,969 | 43.6 (43.3–43.8) | 68,115 | 43.5 (43.1–43.8) | 94,730 | 41.5 (41.2–41.9) | 244,531 | 41.4 (41.2–41.6) |
| Adherence to colonoscopy | 1054 | 81.4 (78.9–83.7) | 1633 | 88 (86.3–89.5) | 2719 | 87.8 (86.5–89) | 1485 | 89 (87.3–90.6) | 1988 | 88.9 (87.5–90.3) | 5140 | 89.3 (88.4–90.2) |
| CRC detection rate (‰) | 22,275 | 0.99 (0.6–1.5) | 41,648 | 1.5 (1.2–1.9) | 64,447 | 1.3 (1.1–1.6) | 29,653 | 1.8 (1.3–2.3) | 39,347 | 1.5 (1.1–1.9) | 101,418 | 1.5 (1.3–1.8) |
| Advanced adenoma detection rate (‰) | 22,275 | 16.3 (14.6–18) | 41,648 | 13.7 (12.6–14.8) | 64,447 | 14.7 (13.8–15.7) | 29,653 | 18.6 (17.1–20.3) | 39,347 | 18.6 (16.3–18.9) | 101,418 | 18.3 (17.5–19.1) |
| Advanced neoplasia detection rate (‰) | 22,275 | 17.2 (15.3–19.5) | 41,648 | 15.2 (13.8–16.8) | 64,447 | 16 (14.8–17.3) | 29,653 | 20.4 (18.4–22.6) | 39,347 | 19.1 (17.4–20.8) | 101,418 | 19.8 (18.8–20.9) |
N values refer to the denominator of the screening outcomes: screening invitations, individuals with a positive FIT, and screenees.
The absolute number of screen-detected cancers in 2020 was lower compared to those detected in 2019 (85 and 156, respectively). The stage distribution of screen-detected cancers changed in 2020, the proportion of advanced-stage CRC (III and IV) increased by 13% (from 38.5% in 2019 to 43.5% in 2020) (Table 2 ).
Table 2.
Stage distribution of CRC detected in the screening program of the Metropolitan Area of Barcelona. 2019–2020.
| 2020 |
2019 |
|
|---|---|---|
| N (%) | N (%) | |
| Early-stage | ||
| I | 28 (32.9) | 69 (44.2) |
| II | 13 (15.3) | 17 (10.9) |
| Advanced stage | ||
| III | 30 (35.3) | 52 (33.3) |
| IV | 7 (8.2) | 8 (5.1) |
| Unknown | 7 (8.2) | 10 (6.4) |
| Total CRC | 85 | 156 |
Fig. 2 shows the Kaplan-Meier curves for time to colonoscopy in 2019 and 2020. Time to colonoscopy was significantly longer in 2020 compared with the previous year (p < 0.001).
Fig. 2.
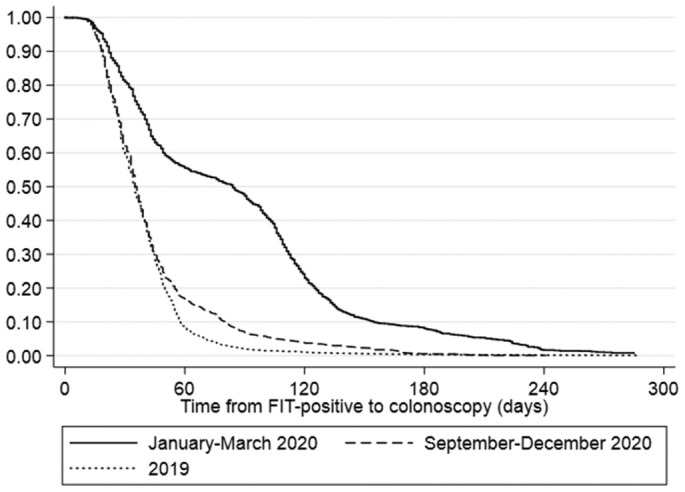
Time to the performance of colonoscopy by invitation period of 2020 and 2019.
*Invitations, FIT Distribution, and colonoscopies; **N = 20 non referred to colonoscopy.
A total of 448 individuals were interviewed by phone, 310 individuals with a positive FIT result who performed colonoscopy between June and September 2020, and 219 individuals with a negative FIT result (control group) (Supplementary methods). Individuals with a positive FIT result did not report higher levels of perceived distress as compared to those with a negative FIT result. Irrespective of FIT result, having poorer emotional well-being during the COVID-19 pandemic, and having more perceived CRC risk compared to same-aged persons were associated with increased levels of perceived distress among participants in a CRC screening program in the context of the COVID-19 pandemic (Table 3 and Supplementary Table 1).
Table 3.
Factors associated with high levels of perceived distress in participants of CRC screening during the first wave of the COVID-19 pandemic.
| Perceived distress level |
|||||
|---|---|---|---|---|---|
| Low (≤13) |
Moderate/high (>13) |
aORa |
95%CI |
p |
|
| n (%) | n (%) | ||||
| FIT screening result | |||||
| Negative | 140 (53.2) | 63 (46) | 1 | ||
| Positive | 123 (46.8) | 74 (54) | 1.34 | 0.88–2.04 | 0.17 |
| Sex | |||||
| Men | 133 (50.6) | 55 (40.1) | 1 | ||
| Women | 130 (49.4) | 82 (59.9) | 1.60 | 1.05–2.46 | 0.03 |
| DS index (0−100) | |||||
| 1st tertile | 36 (13.7) | 19 (13.9) | 1 | ||
| 2nd tertile | 120 (45.6) | 56 (40.9) | 0.87 | 0.44–1.63 | 0.57 |
| 3rd tertile | 107 (40.7) | 62 (45.3) | 0.98 | 0.57–2.06 | |
| Age | |||||
| 50–59 years | 123 (46.8) | 69 (50.4) | 1 | ||
| 60–69 years | 140 (53.2) | 68 (49.6) | 0.84 | 0.55–1.29 | 0.42 |
| Marital status | |||||
| Married | 204 (77.9) | 96 (70.1) | 1 | ||
| Not married | 58 (22.1) | 41 (29.9) | 1.39 | 0.87–2.24 | 0.17 |
| Work status affected by COVID-19 | |||||
| No | 213 (81) | 115 (83.9) | 1 | ||
| Yes | 50 (19) | 22 (16.1) | 0.74 | 0.42–1.3 | 0.30 |
| Personal/nearby COVID-19 diagnosis | |||||
| No | 152 (58.2) | 80 (58.4) | 1 | ||
| Yes | 109 (41.8) | 57 (41.6) | 1 | 0.65–1.52 | 0.99 |
| FIT result meaning | |||||
| Definitely no CRC/very unlikely | 130 (53.7) | 50 (39.4) | 1 | ||
| Unlikely | 83 (34.3) | 51 (40.2) | 1.70 | 1.04–2.76 | 0.04 |
| Likely/certain | 29 (12) | 26 (20.5) | 2.26 | 1.2–4.23 | |
| Comparative perceived CRC risk | |||||
| About the same | 196 (78.1) | 91 (68.9) | 1 | 0.02 | |
| Higher | 25 (10) | 30 (22.7) | 2.44 | 1.35–4.41 | |
| Lower | 30 (12) | 11 (8.3) | 0.79 | 0.38–1.64 | |
| Emotional well-being affected by COVID-19 | |||||
| Not at all/only a little | 145 (55.3) | 39 (28.7) | 1 | ||
| To some extent | 95 (36.3) | 66 (48.5) | 2.51 | 1.55–4.05 | 0.00 |
| Rather much/very much | 22 (8.4) | 31 (22.8) | 4.90 | 2.53–9.49 | |
Minimal adjusted model by sex, age, and DS index; after adjusting the model by sex, age, DS index, and variables with p < 0.1 variables associated with psychological distress were emotional well-being affected by COVID-19 (not at all/only a little: Reference category; to some extent: aOR: 2.42; 95%CI: 1.43–4.12; rather much/very much: aOR: 5.79; 95%CI: 2.79–12.02) and comparative perceived CRC risk (about the same: Reference category; higher: aOR: 2.52; 95%CI: 1.28–4.96; lower: aOR: 0.81; 95%CI: 0.35–1.88); 48 individuals excluded (32 among the FIT positive and 16 among the FIT negative) because of 1 or more missing values in the PSS.
4. Discussion
The analysis of the short-term effects of the COVID-19 pandemic on a large FIT-based CRC screening hub in Catalonia showed that 43% of the individuals due for screening did not receive their invitation by December 31, 2020, leading to a screening backlog of 5 months. We observed a temporary decrease in participation and adherence to colonoscopy. No differences in distress levels were found in individuals with a positive test compared to those with a negative test, although the timeline to colonoscopy after a positive FIT result was longer than the previous year. Finally, a decrease in the advanced neoplasia rate was observed along with an increase in advanced stages of CRC.
The decrease in participation of invitees during the first quarter of 2020 in our screening hub is in line with recently published results by Cheng et al. (2021), Kortlever et al. (2021). Contrary to these studies, participation after the screening suspension was significantly higher than in the previous year. We strongly believe that the COVID-19 pandemic has triggered an awareness increase to participate in the program, although further research is needed as participation in our program is increasing annually. In addition, the COVID-19 era has brought an opportunity to demonstrate the effectiveness of implementing m-health strategies such as SMS reminders to boost cancer screening participation. In this sense, our findings show for individuals whose screening was incomplete due to program suspension and who received an SMS reminder, participation was about 5 percentage points higher than in individuals where SMS could not be sent or delivered because the mobile phone number was not provided, or the SMS failed.
A major concern from our study is the decrease observed in colonoscopy adherence rates among individuals invited during the first quarter of 2020 when compared to the previous year. Individuals with a positive FIT result have a high risk of advanced neoplasm; therefore, a decrease in diagnostic colonoscopy adherence can result in worse health outcomes (D'Andrea et al., 2020; Lee and Miller, 2018). Fear of contracting COVID-19 in health care settings has been widely reported; specifically, in the context of screening, previous studies have shown that 50% of colonoscopies after a positive FIT result were refused because of fear of contracting COVID-19 during the first wave (Cheng et al., 2021). We are unable to determine whether the decrease in colonoscopy adherence was due to the endoscopic units (fewer attempts to locate patients) and/or was due to the individuals' fear of being infected by the COVID.
As expected, the time to colonoscopy among FIT-positive individuals affected by the pause of the program was more than two times longer than usual. When resuming colonoscopies in May, we established a prioritization criterion stratified by fecal hemoglobin concentration levels, which is strongly associated with the likelihood of having advanced neoplasm at colonoscopy. To safeguard the capacity of the endoscopy units during the next outbreaks of COVID-19 and eventually to reduce the backlog in screening invitations, the advisory committee of the Catalan FIT-based CRC screening program increased the FIT cutoff point to 31 μg Hb/g feces, thus decreasing the number of screening colonoscopies by 25%. Consequently, the advanced neoplasia rate decreased by 23% after screening suspension.
Our findings show that in comparison to individuals with a negative FIT result, individuals with a positive FIT result did not report increased levels of perceived distress preceding colonoscopy. Among all interviewees, the levels of distress were higher in those individuals whose emotional well-being was greatly interfered with the COVID-19 the pandemic, illustrating the associated fear and the competing health risks during the first wave. Previous studies have shown increased distress levels after a positive FIT result and before a confirmatory diagnostic procedure (Vermeer et al., 2020; Denters et al., 2013). Denters et al. reported that the overall level of distress was highest shortly after having been informed about a positive test result and just before undergoing the colonoscopy it was significantly lower (Denters et al., 2013). Therefore, it is imperative to guarantee that the time between procedures is as short as possible (Vermeer et al., 2020; Denters et al., 2013).
The main challenge of this study was how to examine differences in screening outcomes, comparing observed data in 2020 with the expected number in a situation without COVID-19. We compared outcomes from 2020 with 2019 considering the same period (January–March and September–December). We also compared observed rates with overall rates from 2019 because we think they are more comparable to 2020. Screening invitations are sent according to primary health care areas (territorial divisions through which primary health care services are organized) and there are differences in screening results by geographical areas. Despite using overall rates as the comparison data, we cannot rule out some sort of bias, resulting in either an underestimation or an overestimation of the differences in participation, colonoscopy adherence, and detection rates.
Regarding the perceived distress, we only considered individuals with a scheduled colonoscopy in June–September 2020. We cannot rule out that individuals who refused to undergo colonoscopy had a higher level of psychological distress than their counterparts who agreed to receive a colonoscopy. If any, the effect size would be small.
Four out of ten individuals due for screening did not receive their invitation by the end of 2020. For those, around 45,500 individuals would have completed the FIT at home, of which 5.1% would have had a FIT-positive screening, and around 3.8% of those will have CRC. This equates to 88 undiagnosed CRC cases due to the screening pause. Additionally, more than 943 people will have advanced adenomas undetected, with a 2.6 to 4.2% (Brenner et al., 2007) annually transition to CRC if not removed. To minimize the long-term impact of the COVID-19 pandemic on CRC screening, strategies should be implemented to reduce the screening backlog while considering endoscopic capacity constraints. A range of strategies is possible, from skipping one screening round for those affected by the pause to implementing catch-up. In the latter case, it would be important to shorten recovery time as much as possible, for instance, by increasing the FIT positivity threshold (de Jonge et al., 2021; Dekker et al., 2020; Morrison, 2021). To maximize diagnostic yield with limited endoscopic capacity, we could also consider prioritizing colonoscopies after a FIT positive result rather than post-polypectomy surveillance colonoscopies due to their greater benefits (Greuter et al., 2017).
The efforts of the COVID-19 and Cancer Global Modelling Consortium (ccgmc.org) to simulate different scenarios of recovery strategies for cancer screening are noteworthy. However, real-world data could be useful to validate the calibrated models in different settings to facilitate decision-makers to choose the best recovery strategy for their screening programs.
5. Conclusions
The COVID-19 pandemic has strongly impacted the functioning of our CRC screening hub, resulting in a large backlog of the target population to be invited. In the short term, we have observed a decrease in advanced neoplasia rate and an increase in later stages of CRC. Thus, it is critical to implement recovery strategies to minimize the long-term effects.
Ethics approval and consent to participate
The Colorectal Cancer Screening Program in Catalonia follows Public Health laws and the Organic Law on Data Protection (Regulation (EU) 2016/679, 2016). The screening program accomplishes the specific protocol based on the existing guidelines (Consell Assessor del Programa, 2015). The study of the impact of COVID-19 on perceived distress in CRC screening participants, including the consent procedure, was approved by the Ethics Committees of the University Bellvitge Hospital (approval number PR236/20). All participants provided verbal informed consent, which was noted by the trained interviewer before starting the survey. The study was performed following Good Clinical Practice and the Declaration of Helsinki.
The following are the supplementary data related to this article.
Characteristics of individuals interviewed during the first wave of the COVID-19 pandemic according to FIT result
Supplementary material 1
Supplementary material 2
Funding
None.
Availability of data and material
Data, analytic methods, and study materials available under request.
CRediT authorship contribution statement
Nuria Vives: Conceptualization, Data curation, Formal analysis, Methodology, Supervision, Writing – original draft, Writing – review & editing. Gemma Binefa: Conceptualization, Methodology, Writing – review & editing. Carmen Vidal: Conceptualization, Methodology, Writing – review & editing. Núria Milà: Conceptualization, Methodology, Writing – review & editing. Rafael Muñoz: Investigation. Virtudes Guardiola: Investigation. Olga Rial: Investigation. Montse Garcia: Conceptualization, Formal analysis, Methodology, Supervision, Writing – original draft, Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Brenner H., Hoffmeister M., Stegmaier C., et al. Risk of progression of advanced adenomas to colorectal cancer by age and sex: estimates based on 840 149 screening colonoscopies. Gut. 2007;56:1585–1589. doi: 10.1136/gut.2007.122739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng S.Y., Chen C.F., He H.C., et al. Impact of COVID-19 pandemic on fecal immunochemical test screening uptake and compliance to diagnostic colonoscopy. J. Gastroenterol. Hepatol. 2021;36:1614–1619. doi: 10.1111/jgh.15325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Consell Assessor del Programa . Departament de Salut. Generalitat de Catalunya; Catalonia: 2015. de detecció precoç de càncer de còlon i recte de Catalunya del Pla Director D’oncologia. [Organizational and operational guidelines in the Catalan Program for Early Detection of Colorectal Cancer] [Google Scholar]
- Crespo J., Andrade R., Alberca de las Parras F., et al. Resumption of activity in gastroenterology departments. Recommendations by SEPD, AEEH, GETECCU, and AEG. Gastroenterol. Hepatol. 2020;43:332–347. doi: 10.1016/j.gastrohep.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Andrea E., Ahnen D.J., Sussman D.A., et al. Quantifying the impact of adherence to screening strategies on colorectal cancer incidence and mortality. Cancer Med. 2020;9:824–836. doi: 10.1002/cam4.2735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Jonge L., Worthington J., van Wifferen F., et al. Impact of the COVID-19 pandemic on fecal immunochemical test-based colorectal cancer screening programs in Australia, Canada, and the Netherlands: a comparative modeling study. Lancet Gastroenterol. Hepatol. 2021;6:304–314. doi: 10.1016/S2468-1253(21)00003-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dekker E., Chiu H.M., Lansdorp-Vogelaar I., et al. Colorectal cancer screening in the novel coronavirus disease-2019 era. Gastroenterology. 2020;159:1998–2003. doi: 10.1053/j.gastro.2020.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denters M.J., Deutekom M., Essink-Bot M.L., et al. FIT false-positives in colorectal cancer screening experience psychological distress up to 6 weeks after colonoscopy. Support Care Cancer. 2013;21:2809–2815. doi: 10.1007/s00520-013-1867-7. [DOI] [PubMed] [Google Scholar]
- Forbes N., Hilsden R.J., Martel M., et al. Association between time to colonoscopy after positive fecal testing and colorectal cancer outcomes: a systematic review. Clin. Gastroenterol. Hepatol. 2021;19:1344–1354. doi: 10.1016/j.cgh.2020.09.048. e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greuter M.J.E., De Klerk C.M., Meijer G.A., et al. Screening for colorectal cancer with fecal immunochemical testing with and without post polypectomy surveillance colonoscopy: a cost-effectiveness analysis. Ann. Intern. Med. 2017;167:544–554. doi: 10.7326/M16-2891. [DOI] [PubMed] [Google Scholar]
- Kortlever T.L., de Jonge L., Wisse P.H.A., et al. The national FIT-based colorectal cancer screening program in the Netherlands during the COVID-19 pandemic. Prev. Med. (Baltim.) 2021;151 doi: 10.1016/j.ypmed.2021.106643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S., Miller A. Factors influencing participation in fecal occult blood testing to screen for colorectal cancer in Australia: a scoping review protocol. JBI Database Syst. Rev. Implement. Rep. 2018;16:57–62. doi: 10.11124/JBISRIR-2017-003392. [DOI] [PubMed] [Google Scholar]
- Morrison D.S. Recovering cancer screening in the pandemic: strategies and their impacts. Br. J. Cancer. 2021;124 doi: 10.1038/s41416-021-01264-6. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NH Department of Administrative Services NH Department of Administrative Services Perceived Stress Scale. 2020. https://das.nh.gov/wellness/docs/percievedstressscale.pdf accessed 16 April 2021.
- Perera M.J., Brintz C.E., Birnbaum-Weitzman O., et al. Factor structure of the perceived stress scale-10 (PSS) across English and Spanish language responders in the HCHS/SOL sociocultural ancillary study. Psychol. Assess. 2017;29:320–328. doi: 10.1037/pas0000336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puricelli Perin D.M., Elfström K.M., Bulliard J.L., et al. Early assessment of the first wave of the COVID-19 pandemic on cancer screening services: the International Cancer Screening Network COVID-19 survey. Prev. Med. (Baltim.) 2021;151 doi: 10.1016/j.ypmed.2021.106642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Regulation (EU) 2016/679 of the European Parliament and of the council of 27 April 2016 on the protection of natural persons about the processing of personal data and on the free movement of such data, and repealing Directive 95/46/EC. Luxemburgo. 2016. https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=OJ:L:2016:119:TOC accessed 31 July 2020.
- Remor E. Psychometric properties of a European Spanish version of the Perceived Stress Scale (PSS) Span. J. Psychol. 2006;9:86–93. doi: 10.1017/s1138741600006004. [DOI] [PubMed] [Google Scholar]
- Ricciardiello L., Ferrari C., Cameletti M., et al. Impact of SARS-CoV-2 pandemic on colorectal cancer screening delay: effect on stage shift and increased mortality. Clin. Gastroenterol. Hepatol. 2021;19:1410–1417.e9. doi: 10.1016/j.cgh.2020.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Updated SARS-CoV-2 data Catalan Agency for Health Quality and Evaluation (AQuAS) https://aquas.gencat.cat/ca/actualitat/ultimes-dades-coronavirus accessed 20 January 2021.
- Vermeer N.C.A., van der Valk M.J.M., Snijders H.S., et al. Psychological distress and quality of life following positive fecal occult blood testing in colorectal cancer screening. Psychooncology. 2020 doi: 10.1002/pon.5381. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO Director-General's opening remarks at the media briefing on COVID-19 - 11. March 2020. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 accessed 20 January 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Characteristics of individuals interviewed during the first wave of the COVID-19 pandemic according to FIT result
Supplementary material 1
Supplementary material 2
Data Availability Statement
Data, analytic methods, and study materials available under request.