Healthcare workers (HCWs) in the United Kingdom (UK) have been prioritised in the SARS-CoV-2 vaccination agenda, including the ongoing booster programme.1 We previously reported that 23% of 11,584 HCWs who completed the baseline UK-REACH (UK Research study into Ethnicity And Covid-19 outcomes in Healthcare workers) cohort study questionnaire2 were hesitant about receiving a SARS-CoV-2 vaccine between 4th December 2020 and 28th February 2021. Vaccine hesitancy was more likely amongst certain ethnic minority groups and was associated with lower trust in employing healthcare organisations and in vaccines themselves. HCWs who were hesitant also reported concerns about vaccine safety and side effects, especially given the speed of vaccine development and roll-out, and expressed a desire to delay vaccination until more people had been vaccinated. As the vaccine programme progresses these concerns may lessen,3 however, the latest NHS England data show that around 15% of HCWs in some areas remain unvaccinated.4 To increase vaccine confidence and uptake for first, second and booster doses, we need to understand which HCWs are more likely to remain hesitant and why. This is particularly critical given the recent announcement that SARS-CoV-2 vaccination will be a mandatory requirement for UK HCWs from spring 2022.5 This leaves limited time to encourage HCWs to accept vaccination voluntarily, thereby lessening the potential deleterious effects of mandatory vaccination on staff morale and workforce retention.
Here, we report the persistence of hesitancy for first and second vaccine doses among UK HCWs, and the factors that predict persistent hesitancy. We analysed longitudinal data from the baseline and first follow-up UK-REACH questionnaire, the latter administered between 21st April and 28th June 2021 (53.1% of participants who completed the first questionnaire completed the follow-up). Our sample comprised UK HCWs who i) had completed both UK-REACH questionnaires, ii) reported being hesitant at baseline and iii) reported an incomplete SARS-CoV-2 vaccine schedule at baseline. Our outcome measure was remaining SARS-CoV-2 vaccine hesitant at follow-up. Participants were coded as remaining hesitant if they indicated hesitancy about their second dose at follow-up (if they had had a first dose at baseline) or for their first or second dose at follow-up (if they had had no doses at baseline). We constructed a logistic regression model to identify factors associated with remaining hesitant. We selected variables based on their association with vaccine hesitancy in our previous work and, to ensure results were relevant to policy, on which we felt employing healthcare trusts were likely to have data. The base model consisted of age, sex, ethnicity, job role and flu vaccination history (variables derived as previously6) on complete cases. To this model we then added variables representing i) trusted vaccine information sources; ii) information advocating against vaccination; iii) beliefs about the importance of vaccination and how well informed a participant felt about vaccines, to investigate their effect on persistent hesitancy.
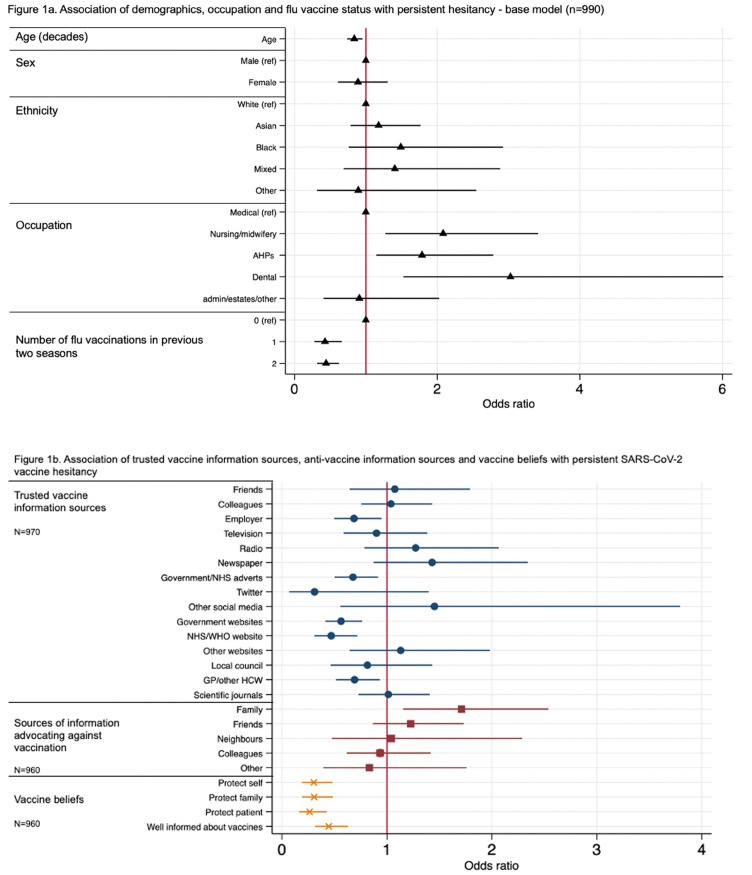
Results are shown in Fig 1a [n=990, n=275 (27.7%) remained hesitant] and Fig 1b (n=960 to 970). HCWs in nursing/midwifery roles (aOR 2.00, 95%CI 1.20 – 3.28), allied health professionals (including pharmacists, healthcare scientists, ambulance workers and those in optical roles; 1.79, 1.15 – 2.80) and dental roles (3.02, 1.53 – 6.01) were more likely to remain hesitant than those in medical roles. Those who had taken up influenza vaccination in the previous seasons were less likely to remain SARS-CoV-2 vaccine hesitant (0.43, 0.28 – 0.66 [for one influenza vaccination in previous two seasons], 0.45, 0.32 – 0.62 [for influenza vaccine uptake in both seasons]). Older HCWs were less likely to remain hesitant. There were no significant differences in risk of persistent hesitancy by sex or ethnic group.
Figure 1.
(a) shows the adjusted odds ratios for the association of covariates with an outcome of persistent SARS-CoV-2 vaccine hesitancy (adjusted for age, sex, ethnicity, occupation and flu vaccination status). Note that the allied health professionals category includes pharmacists, healthcare scientists, ambulance workers and those in optical roles and the nursing/midwifery category includes healthcare assistants and nursing associates. AHP – allied health professional, Ref – reference category. (b) shows the adjusted odds ratios for the association of i) trusted vaccine information sources, ii) sources of information advocating against vaccination and iii) vaccine beliefs with persistent SARS-CoV-2 vaccine hesitancy. These are adjusted for the variables in the base model. GP – general practitioner, NHS – National Health Service, WHO – World Health Organisation.
HCWs who reported trusting vaccine information sourced from their employer (0.69, 0.50 – 0.95), Government/NHS adverts (0.68, 0.50 – 0.92), official websites (0.56, 0.41 – 0.76 [Government website], 0.47, 0.31 – 0.72[NHS/WHO website]), and their own GP/HCW (0.69, 0.51 – 0.93) were less likely to remain hesitant than those that did not trust these sources. Those that had been advised not to take the SARS-CoV-2 vaccine by their family were more likely to remain hesitant than those who had not (1.71, 1.15 – 2.54). HCWs who indicated that they agreed with statements regarding the importance of vaccines in protecting themselves (0.30, 0.19 – 0.48), their families (0.31, 0.19 – 0.49) and patients under their care (0.26, 0.16 – 0.43) were less likely to remain hesitant than those that indicated they did not agree with these statements. Those who indicated they felt well informed about SARS-CoV-2 vaccination were also less likely to remain hesitant (0.45, 0.32 – 0.63) than those who did not report feeling well informed.
A significant minority of HCWs in our sample were still experiencing vaccine hesitancy at follow up. In our previous work we highlighted trust (in employer, healthcare organisations and the Government) as a critical factor in predicting vaccine hesitancy.6 The results of the current analysis demonstrate that trust in these institutions is also important in determining whether hesitancy is likely to persist. Building trust amongst groups who are more likely to experience vaccine hesitancy may therefore represent a strategy of enhancing vaccine uptake. Importantly, we also demonstrate that having had family members advocate against vaccination increases the risk of persistent SARS-CoV-2 vaccine hesitancy. This highlights the importance of not only targeting interventions for improving vaccine uptake at HCWs, but also working to share messaging in their communities about the risks and benefits of vaccines to address concerns. Furthermore, our results indicate that any messaging designed to improve vaccine uptake and aimed at HCWs should emphasise the importance of vaccination for protection of HCWs, their families and their patients.
In summary, we have identified factors that might influence changes in vaccine hesitancy which should directly inform interventions aimed at improving vaccine uptake in HCWs and the wider community.
Acknowledgments
Funding
UK-REACH is supported by a grant from the MRC-UK Research and Innovation (MR/V027549/1) and the Department of Health and Social Care through the National Institute for Health Research (NIHR) rapid response panel to tackle COVID-19. Core funding was also provided by NIHR Biomedical Research Centres. KW is funded through an NIHR Career Development Fellowship (CDF-2017-10-008). LBN is supported by an Academy of Medical Sciences Springboard Award (SBF005\1047). ALG was funded by internal fellowships at the University of Leicester from the Wellcome Trust Institutional Strategic Support Fund (204801/Z/16/Z) and the BHF Accelerator Award (AA/18/3/ 34220). C.J. held a Medical Research Council Clinical Research Training Fellowship (MR/P00167X/1). MDT holds a Wellcome Trust Investigator Award (WT 202849/Z/ 16/Z) and an NIHR Senior Investigator Award. KK is supported by the National Institute for Health Research (NIHR) Applied Research Collaboration East Midlands (ARC EM). KK and MP are supported by the NIHR Leicester Biomedical Research Centre (BRC). MP is supported by a NIHR Development and Skills Enhancement Award. This work is carried out with the support of BREATHE - The Health Data Research Hub for Respiratory Health [MC_PC_19004] in partnership with SAIL Databank. BREATHE is funded through the UK Research and Innovation Industrial Strategy Challenge Fund and delivered through Health Data Research UK.
Acknowledgements
We would like to thank all the participants who take part in this study when the NHS is under immense pressure. We wish to acknowledge the Professional Expert Panel group (Amir Burney, Association of Pakistani Physicians of Northern Europe; Tiffanie Harrison; London North West University Healthcare NHS Trust; Ahmed Hashim, Sudanese Doctors Association; Sandra Kazembe, University Hospitals Leicester NHS Trust; Susie M. Lagrata (Co-chair), Filipino Nurses Association, UK & University College London Hospitals NHS Foundation Trust; Satheesh Mathew, British Association of Physicians of Indian Origin; Juliette Mutuyimana, Kingston Hospitals NHS Trust; Padmasayee Papineni (Co-chair), London North West University Healthcare NHS Trust; Tatiana Monteiro, University Hospitals Leicester NHS Trust), the UK-REACH Stakeholder Group 7, the Study Steering Committee, Serco, as well as the following people and organisations for their support in setting up the study from the regulatory bodies: Kerrin Clapton and Andrew Ledgard (General Medical Council), Caroline Kenny (Nursing and Midwifery Council), David Teeman and Lisa Bainbridge (General Dental Council), My Phan (General Pharmaceutical Council), Angharad Jones (General Optical Council), Mark Neale (Pharmaceutical Society of Northern Ireland) and the The Health and Care Professions Council.
We would also like to acknowledge the following trusts and sites who recruited participants to the study: Affinity Care, Berkshire Healthcare NHS Trust, Birmingham and Solihull NHS Foundation Trust, Birmingham Community Healthcare NHS Foundation Trust, Black Country Community Healthcare NHS Foundation Trust, Bridgewater Community Healthcare NHS Trust, Central London Community Healthcare NHS Trust, Chesterfield Royal Hospital NHS Foundation Trust, County Durham and Darlington Foundation Trust, Derbyshire Healthcare NHS Foundation Trust, Lancashire Teaching Hospitals NHS Foundation Trust, Lewisham and Greenwich NHS Trust, London Ambulance NHS Trust, Northern Borders, Northumbria Healthcare NHS Foundation Trust, Nottinghamshire Healthcare NHS Foundation Trust, Royal Brompton and Harefield NHS trust, Royal Free NHS Foundation Trust, Sheffield Teaching Hospitals NHS Foundation Trust, South Central Ambulance Service NHS Trust, South Tees NHS Foundation Trust, St George's University Hospital NHS Foundation Trust, Sussex Community NHS Foundation Trust, University Hospitals Coventry and Warwickshire NHS Trust, University Hospitals of Leicester NHS Trust, University Hospitals Southampton NHS Foundation Trust, Walsall Healthcare NHS Trust and Yeovil District Hospital NHS Foundation Trust.
Contributors
MP conceived of the idea and led the application for funding with input from MT, KK, KW, LN, SC, LG, ALG and CJ. The questionnaire were designed by KW, MP, ICM, CMel, CJ, ALG, LN, AG and CAM. Online consent and questionnaire tools were developed by LB. CAM and KW wrote the first draft of the manuscript with input from MP, DP and JN. All authors contributed to and approved the submitted manuscript.
Declaration of interest
KK is Director of the University of Leicester Centre for Black Minority Ethnic Health, Trustee of the South Asian Health Foundation, Chair of the Ethnicity Subgroup of the UK Government Scientific Advisory Group for Emergencies (SAGE). SC is Deputy Medical Director of the General Medical Council, UK Honorary Professor, University of Leicester. MP reports grants from Sanofi, grants and personal fees from Gilead Sciences and personal fees from QIAGEN, outside the submitted work. KW, ICM, CAM, LBN, ALG, CM, LB, AG, CJ, MDT, JN, DP and LJG have no competing interests to declare.
References
- 1.England PH. JCVI issues updated advice on COVID-19 booster vaccination. 2021. https://www.gov.uk/government/news/jcvi-issues-updated-advice-on-covid-19-booster-vaccination (accessed 07/10/2021 2021).
- 2.Woolf K, Melbourne C, Bryant L, et al. Protocol: The United Kingdom Research study into Ethnicity And COVID-19 outcomes in Healthcare workers (UK-REACH): protocol for a prospective longitudinal cohort study of healthcare and ancillary workers in UK healthcare settings. BMJ Open. 2021;11(9) doi: 10.1136/bmjopen-2021-050647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Halbrook M, Gadoth A, Martin-Blais R, et al. Longitudinal assessment of COVID-19 vaccine acceptance and uptake among frontline medical workers in Los Angeles, California. Clinical Infectious Diseases. 2021 doi: 10.1093/cid/ciab614. [DOI] [PubMed] [Google Scholar]
- 4.NHS England. COVID-19 weekly announced vaccinations 04 November 2021. 2021. https://www.england.nhs.uk/statistics/statistical-work-areas/covid-19-vaccinations/(accessed 9th November 2021).
- 5.BBC News. Covid-19: Vaccines to be compulsory for frontline NHS staff in England. 2021. https://www.bbc.co.uk/news/health-59215282 (accessed 9th November 2021).
- 6.Woolf K, McManus IC, Martin CA, et al. Ethnic differences in SARS-CoV-2 vaccine hesitancy in United Kingdom healthcare workers: Results from the UK-REACH prospective nationwide cohort study. The Lancet Regional Health - Europe. 2021 doi: 10.1016/j.lanepe.2021.100180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Woolf K, Melbourne C, Bryant L, et al. The United Kingdom Research study into Ethnicity And COVID-19 outcomes in Healthcare workers (UK-REACH): Protocol for a prospective longitudinal cohort study of healthcare and ancillary workers in UK healthcare settings. medRxiv. 2021 doi: 10.1136/bmjopen-2021-050647. 2021.02.23.21251975. [DOI] [PMC free article] [PubMed] [Google Scholar]