Abstract
Background
Ileal Crohn’s disease (CD) complicated by intraabdominal abscess, phlegmon, fistula, and/or microperforation is commonly treated with antibiotics, bowel rest, and percutaneous drainage followed by interval ileocolic resection (ICR). This “cool off” strategy is intended to facilitate the safe completion of a one-stage resection using a minimally invasive approach and minimize perioperative complications. There is limited data evaluating the benefits of delayed versus early resection.
Methods
A retrospective review of a prospectively maintained inflammatory bowel disease (IBD) database at a tertiary center was queried from 2013–2020 to identify patients who underwent ICR for complicated ileal CD confirmed on preoperative imaging. ICR cohorts were classified as early (≤ 7 days) vs delayed (> 7 days) based on the interval from diagnostic imaging to surgery. Operative approach and 30-day postoperative morbidity were analyzed.
Results
Out of 474 patients who underwent ICR over the 7-year period, 112 patients had complicated ileal CD including 99 patients (88%) with intraabdominal abscess. Early ICR was performed in 52 patients (46%) at a median of 3 days (IQR 2, 5) from diagnostic imaging. Delayed ICR was performed in 60 patients (54%) following a median “cool off” period of 23 days of non-operative treatment (IQR 14, 44), including preoperative percutaneous abscess drainage in 17 patients (28%). A higher proportion of patients with intraabdominal abscess underwent delayed vs early ICR (57% vs 43%, p = 0.19). Overall, there were no significant differences in the rate of laparoscopy (96% vs 90%), conversion to open surgery (12% vs 17%), rates of extended bowel resection (8% vs 13%), additional concurrent procedures (44% vs 52%), or fecal diversion (10% vs 2%) in the early vs delayed ICR groups. The median postoperative length of stay was 5 days in both groups with an overall 25% vs 17% (p = 0.39) 30-day postoperative complication rate and a 6% vs 5% 30-day readmission rate in early vs delayed ICR groups, respectively. Overall median follow-up time was 14.3 months (IQR 1.2, 24.1) with no difference in the rate of subsequent CD-related intestinal resection (4% vs 5%) between the two groups.
Conclusions
In this contemporary series, at a high-volume tertiary referral center, a “cool off” delayed resectional approach was not found to reduce perioperative complications in patients undergoing ICR for complicated ileal Crohn’s disease. Laparoscopic ICR can be performed within one week of diagnosis with low rates of conversion and postoperative complications.
Keywords: Crohn’s disease, Abscess, Ileocolic resection, Drainage, Complications, Laparoscopy
Crohn’s disease (CD) is a chronic inflammatory disease characterized by transmural inflammation of the bowel wall which can result in intestinal perforation and intraabdominal sepsis. Up to 20% of patients with CD will develop an intraabdominal abscess, which is associated with a more severe disease course [1–3]. Intraabdominal abscess is a common indication for surgery in CD and accounts for 7–25% of operations performed [4]. In recent years, non-operative management has emerged as the first-line treatment of intraabdominal abscess complicating ileal CD. Management traditionally consists of antibiotics with or without percutaneous drainage in order to avoid surgery entirely or as a bridge to surgery once inflammation has improved in order to facilitate a more limited resection and reduce the need for fecal diversion [5, 6]. Studies have shown varying success of non-operative management, with abscess resolution ranging 14–85%, with many patients ultimately requiring surgical resection [7]. Additionally, surgery after failed non-operative management is associated with longer hospitalization and need for additional surgery [8–10]. Even with complete resolution of an abscess, surgical resection is often unavoidable, as penetrating CD often co-exists with fibrostenotic CD which itself may require surgical resection due to recurrent obstructive symptoms.
An alternative to delayed surgical management of complicated CD is early operative management following initial diagnosis. The primary concerns with immediate surgical resection in patients with ileal CD complicated by intraabdominal abscess are the potentially increased risks of open surgery or conversion to laparotomy and higher rates of fecal diversion and postoperative septic complications, the latter shown to occur in up to 40% of patients undergoing immediate surgery [11–16]. However, as medical treatments for CD continue to improve and minimally invasive surgery becomes more widely adopted in the management of complicated CD, the role of initial non-operative and delayed resection vs early up-front resection of complicated ileal CD needs reappraisal [17]. The aim of this study was to investigate the outcomes of patients undergoing early vs delayed surgical resection for complicated ileal CD at a high-volume tertiary referral center. Our hypothesis is that patients undergoing early resection have equivalent outcomes compared to those undergoing delayed resection, particularly focusing on rates of laparoscopy, conversion, stoma formation, and postoperative complications.
Materials and methods
An IRB-approved retrospective analysis of a prospectively maintained IBD database supplemented by individual chart review was performed to identify patients who underwent ileocolic resection for complicated ileal CD between 2013 and 2020 at a high-volume tertiary referral center. This study was reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.
Complicated ileal CD was defined as terminal ileitis with one or more of the following findings on diagnostic imaging: intraabdominal abscess, extraluminal fluid collection, phlegmon, enteroenteric or enterocolic fistula, and/or microperforation. Intraabdominal abscesses included all abscess subtypes, including mesenteric, psoas, and interloop abscesses. Microperforation was defined as contained perforation in the absence of an intraabdominal abscess. Patients with no radiologic evidence of complicated ileal CD preoperatively and found to have complicated disease intraoperatively were excluded. Additionally, patients presenting with septic shock or evidence of uncontained bowel perforation on imaging were also excluded. Patients were categorized as either undergoing early ICR (≤ 7 days from diagnostic imaging to surgery) or delayed ICR (> 7 days post imaging) following a trial of non-operative management. Non-operative management consisted of antibiotics with or without percutaneous abscess drainage.
Patient demographics, preoperative laboratory values, perioperative use of immunosuppressants, operative details, and postoperative outcomes were recorded. Surgical technique for ICR was standardized at our institution and was performed laparoscopically whenever feasible as determined by the operating surgeon, including in patients with previous laparotomies. Briefly, laparoscopic ICR at our institution consists of right colon mobilization followed by exteriorization of the ileocolic specimen through a 4–6 cm incision. Mesenteric vessels are divided followed by extracorporeal side-to-side functional end-to-end anastomosis. Additional concurrent procedures were performed based on the extent of disease and included takedown of enteric fistulae, stricturoplasty, and additional non-contiguous small bowel resection. A diverting ileostomy was performed when determined by the operating surgeon as necessary for control of intraabdominal sepsis and operative drains were placed according to surgeon preference. Ileocolic anastomoses were performed extracorporeally in a side-to-side fashion and were hand-sewn or stapled. Conversion to open surgery was defined as an unplanned midline incision or extension of the planned extraction site. The extent of ileal resection was obtained from the pathology report and defined as the length of terminal ileum resected. Extended bowel resection was defined as additional colonic resection beyond that of a standard ICR (i.e., right hemicolectomy) and was performed as needed in order to achieve macroscopically negative margins. Subsequent surgery was defined as any additional CD-related intestinal resection (repeat ICR or small bowel resection) following index surgery, excluding stoma creation or reversal.
The primary outcome in this study was the rate of complications within 30 days of ICR. Postoperative complications were classified according to the Clavien–Dindo classification system and identified through review of the electronic medical record and cross-referenced with our institutional NSQIP database, with final grading confirmed by a board-certified colorectal surgeon [18]. Grade III or IV complications were considered major complications.
Data were collected and analyzed using Statistical Package for Social Science (SPSS) version 24 (IBM, Armonk, NY). Categorical variables were compared using the Pearson’s Chi-square test or the Fisher exact test and continuous variables were compared using Student’s t-test or Mann–Whitney U test. Hypothesis testing was performed at 5% level of significance.
Results
A total of 474 consecutive patients underwent ICR for ileal CD between February 2013 and June 2020; of these, 112 patients had complicated disease on prior imaging in either the outpatient or inpatient setting. All surgeries were performed at a single institution by 11 surgeons. Overall, 99 patients (88%) presented to the primary institution and 13 patients (12%) were transferred following an initial median length of stay of 4 days (IQR 3, 8) at another institution. Preoperative imaging demonstrated an intraabdominal abscess in 99 patients (88%), phlegmon in 34 patients (30%), fistula in 52 patients (46%), and/or microperforation in 7 patients (6%) (Table 1).
Table 1.
Patient demographics, imaging characteristics, operative characteristics, and postoperative outcomes
| Overall (n = 112) |
Early resection (n = 52) |
Delayed resection (n = 60) |
p value | |
|---|---|---|---|---|
| Patient and disease characteristics | ||||
| Male (%) | 68 (61) | 32 (62) | 36 (60) | 1.00 |
| Age (median [IQR]) | 26 [22, 32] | 26 [22, 30] | 27 [22, 33] | 0.35 |
| BMI (median [IQR]) | 22.1 [19.6, 25.1] | 22.4 [19.0, 27.0] | 21.8 [19.7, 24.5] | 0.54 |
| ASA ≥ 3 (%) | 44 (39) | 22 (42) | 22 (37) | 0.68 |
| Smoker (%) | 8 (7) | 5 (10) | 3 (5) | 0.56 |
| Duration of CD, months (median [IQR]) | 6.0 [1.0, 12.0] | 7.0 [1.0, 12.8] | 6.0 [1.0, 11.0] | 0.62 |
| History of prior ICR (%) | 18 (16) | 10 (19) | 8 (13) | 0.56 |
| Perioperative steroids (%) | 18 (16) | 7 (14) | 11 (18) | 0.66 |
| Perioperative biologics (%) | 64 (57) | 31 (60) | 33 (55) | 0.76 |
| WBC, × 103/µL (median [IQR]) | 8.3 [6.4, 10.8] | 8.3 [6.1, 11.1] | 8.2 [6.6, 10.3] | 0.92 |
| Albumin, g/dL (median [IQR]) | 3.1 [2.8, 3.5] | 3.0 [2.8, 3.4] | 3.2 [2.9, 3.6] | 0.10 |
| Imaging characteristics | ||||
| Abscess | 99 (88) | 43 (83) | 56 (93) | 0.15 |
| Abscess size, cm (median [IQR]) | 3.5 [2.5, 4.9] | 0.17 | ||
| Phlegmon | 34 (30) | 16 (31) | 18 (30) | 1.00 |
| Fistula | 52 (46) | 27 (52) | 25 (42) | 0.37 |
| Microperforation | 7 (6) | 5 (10) | 2 (3) | 0.34 |
| Percutaneous abscess drainage (%) | 18 (16) | 1 (2) | 17 (28) | < 0.001 |
| Operative characteristics | ||||
| Time from imaging to surgery, days (median [IQR]) | 9 [3, 25] | 3 [2, 5] | 23 [14, 44] | < 0.001 |
| Laparoscopic approach (%) | 104 (93) | 50 (96) | 54 (90) | 0.37 |
| Conversion (%) | 15 (14) | 6 (12) | 9 (17) | 0.69 |
| Extended ICR (%) | 12 (11) | 4 (8) | 8 (13) | 0.51 |
| Concurrent procedures (%) | 54 (48) | 23 (44) | 31 (52) | 0.55 |
| Fistula takedown | 35 (31) | 11 (21) | 24 (40) | 0.05 |
| Small bowel resection | 16 (14) | 7 (14) | 9 (15) | 1.00 |
| Colectomy | 11 (10) | 6 (12) | 5 (8) | 0.80 |
| Stricturoplasty | 5 (5) | 4 (8) | 1 (2) | 0.28 |
| Diverting stoma (%) | 6 (5) | 5 (10) | 1 (2) | 0.15 |
| Duration, minutes (median [IQR]) | 128 [109, 168] | 125 [112, 162] | 138 [106, 179] | 0.70 |
| Blood loss, mL (median [IQR]) | 75 [50, 150] | 75 [50, 150] | 75 [50, 150] | 0.70 |
| Length of ileal resection, cm (median [IQR]) | 22.4 [16.0, 38.0] | 24.0 [17.0, 46.5] | 22.0 [15.0, 33.0] | 0.35 |
| Postoperative outcomes | ||||
| Length of stay, days (median [IQR]) | 5 [4, 7] | 5 [4, 7] | 5 [4, 7] | 0.66 |
| Any complication (%) | 23 (21) | 13 (25) | 10 (17) | 0.39 |
| Intraabdominal abscess | 5 (5) | 2 (4) | 3 (5) | 1.00 |
| Ileus | 12 (11) | 8 (15) | 4 (7) | 0.14 |
| Superficial surgical site infection | 2 (2) | 1 (2) | 1 (2) | 1.00 |
| Venous thromboembolism | 2 (2) | 2 (4) | 0 (0) | 0.21 |
| Major complication (%) | 4 (4) | 2 (4) | 2 (3) | 1.00 |
| 30-day readmission (%) | 6 (5) | 3 (6) | 3 (5) | 1.00 |
| Follow-up, months (median [IQR]) | 14.3 [1.2, 24.1] | 14.4 [1.0, 26.7] | 14.3 [1.5, 23.7] | 0.84 |
| Subsequent surgerya (%) | 5 (5) | 2 (4) | 3 (5) | 1.00 |
Statistics presented as Median (IQR) or N (%)
aSubsequent surgery: ileocolic resection (n = 4), small bowel resection (n = 1)
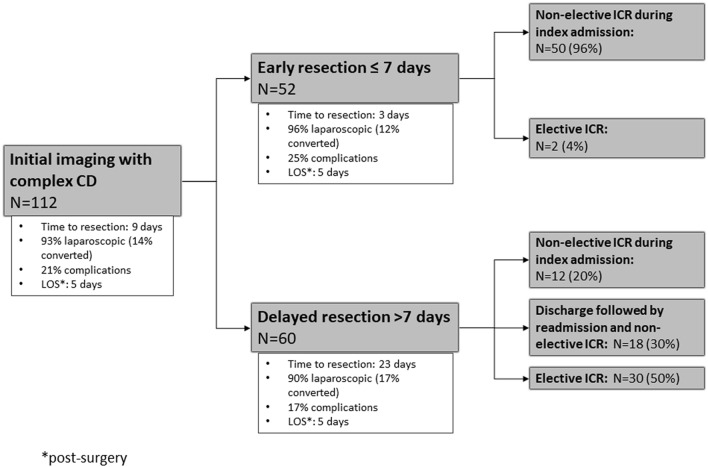
Early ICR was performed in 52 patients (46%) with a median interval of 3 days (IQR 2, 5) between imaging and surgery (Fig. 1). Among early ICR patients, preoperative imaging revealed an intraabdominal abscess in 43 (83%), phlegmon in 16 (31%), fistula in 27 (52%), and microperforation in 5 patients (10%). Two patients (4%) were treated in the outpatient setting with oral antibiotics followed by elective resection. All other 50 patients underwent surgery during index admission. One patient underwent preoperative percutaneous drainage of an intraabdominal abscess followed by ICR 4 days later.
Fig. 1.
Overall management and outcomes of patients with complicated ileal CD
Delayed ICR was performed in 60 patients (54%) at a median interval of 23 days (IQR 14, 44) from imaging. Preoperative imaging demonstrated an intraabdominal abscess in 56 patients (93%), of which 17 patients (30%) underwent preoperative percutaneous abscess drainage at a median of 2 days (IQR 0, 6) following diagnostic imaging. Of the 60 patients undergoing delayed ICR, 15 (25%) were managed entirely in the outpatient setting with oral antibiotics after imaging demonstrated complicated ileal CD, while 15 (25%) underwent elective surgery after discharge from initial inpatient management. The other patients in the delayed cohort underwent non-elective surgery; surgery was performed during the index admission in 12 patients (20%), and non-electively during a readmission in 18 patients (30%).
When comparing early vs delayed ICR cohorts, there were no significant differences in age, sex, BMI, or preoperative laboratory values (Table 1). No significant differences in duration of CD, prior ICR, or use of biologics or systemic steroids within 30 days of surgery were noted between these cohorts. Although these groups did not differ significantly with regards to preoperative imaging findings, the delayed ICR cohort did have a higher proportion of patients with abscess (93% vs 83%, p = 0.15) and the early ICR group had a higher proportion of patients with microperforation (10% vs 3%, p = 0.34).
Overall, laparoscopic ICR was performed in 93% of patients, with no difference between the early vs delayed groups (96% vs 90%) (Table 1). The overall conversion rate to open surgery was 14%, with no significant difference between groups (16% vs 12%, p = 0.69). Operative time was not significantly different between early and delayed groups (125 vs 138 min, p = 0.70). Relative to early ICR, a higher proportion of patients in the delayed group underwent extended resections (13% vs 8%, p = 0.51) and concurrent procedures (52% vs 44%, p = 0.55), although these differences did not reach statistical significance. The overall rate of fecal diversion was 5% and although the rate was higher among those undergoing early ICR, the difference was not significant (10% vs 2%, p = 0.15).
The overall 30-day postoperative complication rate following ICR in this cohort of complicated ileal CD was 21% (Table 1). A higher rate of postoperative complications was noted in the early vs delayed ICR group (25% vs 17%, p = 0.39) although these differences were not statistically significant. The rate of major complications (Clavien–Dindo grade ≥ 3) (4% vs 3%, p = 1.00) and postoperative intraabdominal abscess (4% vs 5%, p = 1.00) did not differ significantly between the early vs delayed ICR groups, respectively. Minor complications included ileus, superficial surgical site infections, and venous thromboembolism (Table 1). There were no significant differences in the rate of minor complications between groups. No incidence of anastomotic leakage or 30-day reoperations were observed in either group. Median length of stay after surgery was 5 days in both groups with no significant difference in the rates of readmission (6% vs 5%, p = 1.00). At a median follow-up of 14.3 months (IQR 1.2, 24.1), 5 patients (5%) underwent additional intestinal resection related to CD, including repeat ICR (n = 4) and SBR (n = 1).
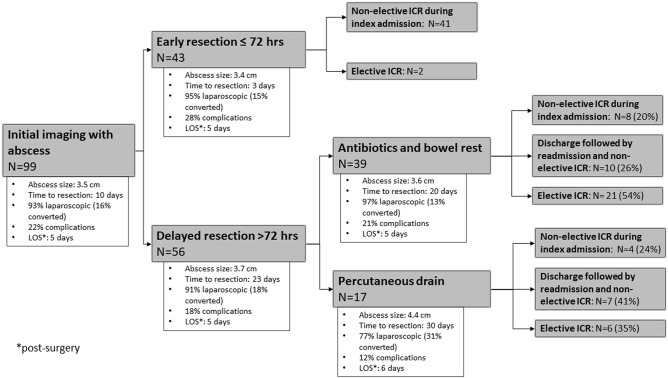
The group of patients presenting with ileal CD complicated by intraabdominal abscess was considered specifically (n = 99) (Table 2). In this group, 43 patients underwent early and 56 underwent delayed ICR, with no significant differences in preoperative characteristics. Again, there were no significant differences in frequency of laparoscopic approach, conversion to laparotomy, rate of diverting stoma, or rate of overall complications between early and late groups. Of patients with abscesses, 18 (18%) underwent percutaneous abscess drainage after a median of 1.5 days from diagnostic imaging, followed by ICR a median of 29 days following initial imaging (IQR 21, 40) (Fig. 2). Median abscess size was 4.4 cm vs 3.5 cm in those who did vs those who did not undergo drainage (p = 0.01). Six patients (33%) that underwent percutaneous abscess drainage were successfully discharged and subsequently underwent delayed elective ICR. Finally, among those with abscesses, the group undergoing early surgery (n = 43) was compared to the groups undergoing delayed ICR with drainage (n = 17) or without drainage (n = 39) (Table 3). A laparoscopic approach was performed in a significantly lower proportion of patients who underwent delayed ICR with preoperative drainage compared to both those who underwent early ICR or delayed ICR without drainage (77% vs 95% vs 97%, p = 0.01), but there were no other significant differences in outcomes.
Table 2.
Patient demographics, imaging characteristics, operative characteristics, and postoperative outcomes in patients who presented with abscess (n = 99)
| Overall (n = 99) |
Early resection (n = 43) |
Delayed resection (n = 56) |
p value | |
|---|---|---|---|---|
| Patient and disease characteristics | ||||
| Male (%) | 60 (61) | 28 (65) | 32 (57) | 0.55 |
| Age (median [IQR]) | 27 [22, 32] | 25 [22, 30] | 28 [22, 34] | 0.23 |
| BMI (median [IQR]) | 22.0 [19.6, 25.0] | 22.5 [19.6, 27.1] | 21.6 [19.6, 24.3] | 0.32 |
| ASA ≥ 3 (%) | 37 (37) | 17 (40) | 20 (36) | 0.86 |
| Smoker (%) | 7 (7) | 4 (9) | 3 (5) | 0.46 |
| Duration of CD, months (median [IQR]) | 7.0 [1.0, 12.0] | 7.0 [1.5, 12.5] | 6.0 [1.0, 12.0] | 0.71 |
| History of prior ICR (%) | 16 (16.2) | 8 (18.6) | 8 (14.3) | 0.76 |
| Perioperative steroids (%) | 17 (17.2) | 6 (14.0) | 11 (19.6) | 0.64 |
| Perioperative biologics (%) | 55 (55.6) | 24 (55.8) | 31 (55.4) | 1.00 |
| WBC, × 103/µL (median [IQR]) | 8.3 [6.4, 10.6] | 8.3 [6.2, 11.1] | 8.2 [6.5, 10.3] | 0.88 |
| Albumin, g/dL (median [IQR]) | 3.1 [2.8, 3.5] | 3.1 [2.8, 3.4] | 3.2 [2.9, 3.6] | 0.18 |
| Imaging characteristics | ||||
| Abscess size, cm (median [IQR]) | 3.5 [2.5, 4.9] | 3.4 [2.0, 4.8] | 3.7 [2.7, 4.9] | 0.17 |
| Phlegmon | 24 (24) | 10 (23) | 14 (25) | 1.00 |
| Fistula | 45 (46) | 22 (51) | 23 (41) | 0.43 |
| Time from imaging to drainage (median [IQR]) | 1.5 [0.0, 6.0] | 1.0 | 2.0 [0.0, 6.0] | 0.77 |
| Time from drainage to surgery, days (median [IQR]) | 22 [11, 40] | 4 | 22 [14, 40] | 0.12 |
| Operative characteristics | ||||
| Time from imaging to surgery, days (median [IQR]) | 10 [4, 26] | 3 [2, 5] | 23 [13, 44] | < 0.001 |
| Laparoscopic approach (%) | 92 (93) | 41 (95) | 51 (91) | 0.70 |
| Conversion (%) | 15 (16) | 6 (15) | 9 (18) | 0.92 |
| Concurrent procedures (%) | 48 (49) | 19 (44) | 29 (52) | 0.58 |
| Diverting stoma (%) | 6 (6) | 5 (12) | 1 (2) | 0.08 |
| Duration, minutes (median [IQR]) | 129 [108, 168] | 127 [112, 160] | 133 [106, 176] | 0.90 |
| Blood loss, mL (median [IQR]) | 75 [50, 150] | 75 [50, 150] | 75 [50, 100] | 0.45 |
| Length of ileal resection, cm (median [IQR]) | 22.2 [15.0, 39.3] | 25.0 [17.0, 48.0] | 22.0 [15.0, 36.0] | 0.51 |
| Postoperative outcomes | ||||
| Length of stay, days (median [IQR]) | 5 [4, 7] | 5 [5, 7] | 5 [4, 7] | 0.47 |
| Any complication (%) | 22 (22) | 12 (28) | 10 (18) | 0.34 |
| Intraabdominal abscess | 4 (4) | 1 (2) | 3 (5) | 0.63 |
| Major complication (%) | 3 (3) | 1 (2) | 2 (4) | 1.00 |
| 30-day readmission (%) | 6 (6) | 3 (7) | 3 (5) | 1.00 |
| Follow-up, months (median [IQR]) | 14.6 [1.3, 24.9] | 14.6 [0.7, 26.8] | 14.6 [2.8, 24.0] | 0.89 |
| Subsequent surgerya (%) | 5 (5) | 2 (5) | 3 (5) | 1.00 |
Statistics presented as Median (IQR) or N (%)
aSubsequent surgery: ileocolic resection (n = 4), small bowel resection (n = 1)
Fig. 2.
Overall management and outcomes of patients with intraabdominal abscess
Table 3.
Patients with abscess and drainage
| Early resection (n = 43) |
Delayed resection (n = 39) |
Delayed resection + PAD (n = 17) |
p value | |
|---|---|---|---|---|
| Patient and disease characteristics | ||||
| Male (%) | 28 (65) | 22 (56) | 10 (59) | 0.71 |
| Age (median [IQR]) | 25 [22, 30] | 28 [22, 34] | 28 [22, 34] | 0.38 |
| BMI (median [IQR]) | 22.5 [19.6, 27.1] | 21.6 [19.3, 23.6] | 23.3 [18.6, 25.3] | 0.53 |
| ASA ≥ 3 (%) | 17 (40) | 13 (33) | 7 (41) | 0.79 |
| Smoker (%) | 4 (9) | 2 (5) | 1 (6) | 0.75 |
| Duration of CD, months (median [IQR]) | 7.0 [1.5, 12.5] | 5.5 [0.5, 11.8] | 7.0 [1.0, 15.0] | 0.96 |
| History of prior ICR (%) | 8 (19) | 6 (15) | 2 (12) | 0.80 |
| Perioperative steroids (%) | 6 (14) | 7 (18) | 4 (24) | 0.67 |
| Perioperative biologics (%) | 24 (56) | 21 (54) | 10 (59) | 0.94 |
| WBC, × 103/µL (median [IQR]) | 8.3 [6.2, 11.1] | 8.3 [6.4, 10.3] | 8.1 [7.2, 10.8] | 0.35 |
| Albumin, g/dL (median [IQR]) | 3.1 [2.8, 3.4] | 3.2 [2.8, 3.6] | 3.2 [2.9, 3.4] | 0.31 |
| Imaging characteristics (%) | ||||
| Abscess size, cm (median [IQR]) | 3.4 [2.0, 4.8] | 3.6 [2.5, 4.4] | 4.4 [3.2, 7.4] | 0.02 |
| Phlegmon | 10 (23) | 14 (36) | 0 (0) | 0.02 |
| Fistula | 22 (51) | 14 (36) | 9 (53) | 0.30 |
| Time from drainage to surgery, days (median [IQR]) | – | 22 [14, 40] | 0.30 | |
| Operative characteristics | ||||
| Time from imaging to surgery, days (median [IQR]) | 3 [2, 5] | 20 [12, 45] | 30 [21, 48] | < 0.001 |
| Laparoscopic approach (%) | 41 (95) | 38 (97) | 13 (77) | 0.01 |
| Conversion (%) | 6 (15) | 5 (13) | 4 (31) | 0.31 |
| Concurrent procedures (%) | 19 (44) | 20 (51) | 9 (53) | 0.75 |
| Diverting stoma (%) | 5 (12) | 1 (3) | 0 (0) | 0.12 |
| Duration, minutes (median [IQR]) | 127 [112, 160] | 138 [104, 168] | 117 [107, 206] | 0.95 |
| Blood loss, mL (median [IQR]) | 75 [50, 150] | 63 [48, 100] | 100 [38, 150] | 0.12 |
| Length of ileal resection, cm (median [IQR]) | 25.0 [17.0, 48.0] | 21.2 [14.3, 37.0] | 22.0 [16.0, 34.5] | 0.75 |
| Postoperative outcomes | ||||
| Length of stay, days (median [IQR]) | 5 [5, 7] | 5 [4, 6] | 6 [5, 7] | 0.58 |
| Any complication (%) | 12 (28) | 8 (21) | 2 (12) | 0.38 |
| Intraabdominal abscess | 1 (2) | 2 (5) | 1 (6) | 0.74 |
| Major complication (%) | 1 (2) | 1 (3) | 1 (6) | 0.75 |
| 30-day readmission (%) | 3 (7) | 2 (5) | 1 (6) | 0.94 |
Statistics presented as Median (IQR) or N (%)
Discussion
The current study explores the impact of the timing of surgical resection on morbidity and other perioperative outcomes in patients undergoing ileocolic resection for complicated ileal CD. This study highlights that when performed by experienced surgeons, early ileocolic resection (within 7 days of initial imaging) for complicated ileal CD in selected patients is safe and feasible with a low rate of major postoperative morbidity. The study also demonstrates that these cases can be successfully performed laparoscopically with an acceptable rate of conversion. Although early resection may increase the risk of fecal diversion and minor postoperative complications as compared to delayed management, this must be balanced against the challenges and duration of initial non-operative management.
The purported goals of delayed resection for complicated ileal CD are to reduce operative risks and facilitate an elective and minimally invasive approach [6, 8, 13]. In recent years, minimally invasive surgery has become the preferred operative approach for patients with uncomplicated ileal CD and has been shown to have a number of benefits when compared to open surgery, including earlier return of bowel function, decreased postoperative pain, and shorter hospitalization [17]. However, it is unclear that this delayed approach truly benefits patients in terms of improving postoperative outcomes, and surgeons must consider the risks of initial non-operative management, which include ongoing symptoms, readmissions, and procedures prior to definitive surgical management. The retrospective nature of this study makes it impossible to provide data with regard to patient quality of life with early vs. delayed surgery, and these data are also lacking in the surgical literature, indicating a need for further research in this area. However, within our study, only half of patients initially managed non-operatively (delayed resection) were effectively “bridged” to elective surgical management, with the remainder undergoing non-elective surgery during the index admission or subsequent readmission, suggesting that many patients have ongoing symptoms that may decrease perceived quality of life.
This study highlights that laparoscopic ICR for ileal CD complicated by abscess, phlegmon, fistula and/or microperforation can be safely performed early (i.e., within 7 days of presentation) without significant increased risk of conversion or major postoperative complications. Overall, 93% of all complicated ileal CD cases in our study were approached laparoscopically with a 14% conversion rate, with no significant differences between the early and delayed cohorts. Our findings are consistent with a 2016 retrospective study by Kristo et al. that reported a 10% conversion rate among 133 patients undergoing laparoscopic resection for penetrating CD which notably included a smaller cohort of patients with intraabdominal abscess (32%) [17]. Additionally, although the rate of fecal diversion appeared higher in the early ICR cohort, this difference was not significant and the overall fecal diversion rate in our study was only 5%. This contrasts with the 49% rate reported by Sangster et al. in a retrospective study of ICR outcomes in 47 patients with penetrating ileocolic Crohn’s disease and intraabdominal abscess [16] and the 39% rate reported by Goyer et al. among 54 patients with complicated CD who underwent laparoscopic ICR [15]. From the results of our current study, early ICR in complicated ileal CD may be associated with increased postoperative morbidity; however, these were mostly minor complications.
The group with intraabdominal abscess merits specific consideration, particularly patients who undergo abscess drainage to facilitate delayed surgical management. Although some studies suggest that surgery can be avoided following percutaneous drainage, the success rate of abscess resolution varies widely, patients often require multiple drainage procedures, and not all abscesses are amenable to drainage [6, 9, 10, 19, 20]. In the current study, patients who underwent drainage and delayed resection were rarely “bridged” to elective surgery (35%) and less likely to undergo a laparoscopic approach compared to either the cohort managed with early resection or delayed resection without drainage (77% vs. 95% and 97%, respectively, p = 0.01). Rates of postoperative complications and stoma formation were lower in the delayed group, although these differences were not significant. The potentially increased risk of diverting ileostomy in the setting of early surgical intervention deserves further study, given that impact on quality of life and need for a second surgery to reverse are non-trivial. It is important to note that our results indicate that larger abscesses were more frequently managed with percutaneous drainage and delayed resection, which is consistent with anecdotal reports of how our surgeons choose to manage these patients. This group may be at higher risk of adverse outcomes, regardless of operative approach, and this management choice may bias the results of the current study. Thus, the optimal management of large abscesses (≥ 4.0 cm) merits further consideration.
There are several limitations and biases inherent to this retrospective study. The decision to perform an early or delayed resection was at the discretion of the operating surgeon, and the selection of 7 days as the cutoff for considering an operation to be early vs. delayed was arbitrary. Additional factors may have affected the timing of surgery, such as patient preference, weekday vs weekend presentation, and decisions made at another institution prior to transfer. While the delayed and early resection groups appear similar in terms of baseline characteristics and operative risk, there may be differences that are not considered which bias the results. In particular, the retrospective nature of this study makes it difficult to study exact details of nutritional status and perioperative medical management, although serum albumin and overall rates of preoperative steroid and biologic use were used as surrogates. Furthermore, we only included patients who ultimately underwent a surgical resection; there may be patients with abscess who were managed non-operatively and went on to avoid surgery entirely. This group must be considered when weighing the risks and benefits of an early operative approach. Additionally, we acknowledge the overall low incidence of complications, which means that we are underpowered to detect small differences given our sample size. Finally, this study was performed at a single center specializing in IBD with surgeons who are very experienced with laparoscopy and, as a result, its findings may not be generalizable to non-specialized centers.
Overall, our study results suggest that early laparoscopic ICR in hemodynamically stable patients presenting with complicated ileal CD is appropriate without a need for a “cool off” period or percutaneous drainage, when performed by experienced surgeons. The potentially increased risk of stoma formation and perioperative morbidity with this strategy, albeit minor, should be discussed with patients and balanced against the risk of a protracted and potentially more symptomatic course incurred by delaying surgery. While drainage may be preferable for larger abscesses, it does not significantly reduce the rate of postoperative complications, conversion or fecal diversion rates, and it only successfully “bridges” a minority of patients to elective surgery.
Conclusion
This contemporary series on the timing of surgical resection for complicated ileal CD demonstrates that early laparoscopic ICR is safe and feasible in select patients with complicated ileal CD. When performed by experienced laparoscopic surgeons, early ICR was not associated with increased risk of conversion to open surgery, major postoperative complications, or need for fecal diversion compared to a delayed resection. Overall, only half of patients who underwent a delayed surgical approach were successfully “bridged” to an elective resection. Early surgical resection may reduce the need for prolonged antibiotics or repeat drainage procedures, which may be preferable for some patients, but further study is needed to examine quality of life metrics in the setting of early versus delayed surgery to determine the most appropriate management approach.
Declarations
Disclosures
Patricia Sylla is a consultant for Ethicon, Medtronic, and Olympus. Randolph Steinhagen has received payment for expert testimony. Daniel Peyser, Heather Carmichael, Adrienne Dean, Vanessa Baratta, Anthony D’Andrea, Gurpawan Kang, Deepika Bhasin, Alexander Greenstein, and Sergey Khaitov have no conflicts of interest or financial ties to disclose.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Greenstein AJ, Lachman P, Sachar DB, Springhorn J, Heimann T, Janowitz HD, Aufses AH., Jr Perforating and non-perforating indications for repeated operations in Crohn's disease: evidence for two clinical forms. Gut. 1988;29(5):588–592. doi: 10.1136/gut.29.5.588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yamaguchi A, Matsui T, Sakurai T, Ueki T, Nakabayashi S, Yao T, Futami K, Arima S, Ono H. The clinical characteristics and outcome of intraabdominal abscess in Crohn's disease. J Gastroenterol. 2004;39(5):441–448. doi: 10.1007/s00535-003-1317-2. [DOI] [PubMed] [Google Scholar]
- 3.Niewiadomski O, Studd C, Hair C, Wilson J, Ding NS, Heerasing N, Ting A, McNeill J, Knight R, Santamaria J, Prewett E, Dabkowski P, Dowling D, Alexander S, Allen B, Popp B, Connell W, Desmond P, Bell S. Prospective population-based cohort of inflammatory bowel disease in the biologics era: disease course and predictors of severity. J Gastroenterol Hepatol. 2015;30(9):1346–1353. doi: 10.1111/jgh.12967. [DOI] [PubMed] [Google Scholar]
- 4.Goldstone RN, Steinhagen RM. Abdominal emergencies in inflammatory bowel disease. Surg Clin N Am. 2019;99(6):1141–1150. doi: 10.1016/j.suc.2019.08.007. [DOI] [PubMed] [Google Scholar]
- 5.Pfefferkorn MD, Marshalleck FE, Saeed SA, Splawski JB, Linden BC, Weston BF. NASPGHAN clinical report on the evaluation and treatment of pediatric patients with internal penetrating Crohn disease: intraabdominal abscess with and without fistula. J Pediatr Gastroenterol Nutr. 2013;57(3):394–400. doi: 10.1097/MPG.0b013e31829ef850. [DOI] [PubMed] [Google Scholar]
- 6.de Groof EJ, Carbonnel F, Buskens CJ, Bemelman WA. Abdominal abscess in Crohn's disease: multidisciplinary management. Dig Dis. 2014;32(Suppl 1):103–109. doi: 10.1159/000367859. [DOI] [PubMed] [Google Scholar]
- 7.Clancy C, Boland T, Deasy J, McNamara D, Burke JP. A meta-analysis of percutaneous drainage versus surgery as the initial treatment of Crohn's disease-related intra-abdominal abscess. J Crohns Colitis. 2016;10(2):202–208. doi: 10.1093/ecco-jcc/jjv198. [DOI] [PubMed] [Google Scholar]
- 8.Nguyen DL, Sandborn WJ, Loftus EV, Jr, Larson DW, Fletcher JG, Becker B, Mandrekar J, Harmsen WS, Bruining DH. Similar outcomes of surgical and medical treatment of intra-abdominal abscesses in patients with Crohn's disease. Clin Gastroenterol Hepatol. 2012;10(4):400–404. doi: 10.1016/j.cgh.2011.11.023. [DOI] [PubMed] [Google Scholar]
- 9.Perl D, Waljee AK, Bishu S, Higgins PDR, Wasnik AP, Stidham RW. Imaging features associated with failure of nonoperative management of intraabdominal abscesses in Crohn disease. Inflamm Bowel Dis. 2019;25(12):1939–1944. doi: 10.1093/ibd/izz069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lobatón T, Guardiola J, Rodriguez-Moranta F, Millán-Scheiding M, Peñalva M, De Oca J, Biondo S. Comparison of the long-term outcome of two therapeutic strategies for the management of abdominal abscess complicating Crohn's disease: percutaneous drainage or immediate surgical treatment. Colorectal Dis. 2013;15(10):1267–1272. doi: 10.1111/codi.12419. [DOI] [PubMed] [Google Scholar]
- 11.Alves A, Panis Y, Bouhnik Y, Pocard M, Vicaut E, Valleur P. Risk factors for intra-abdominal septic complications after a first ileocecal resection for Crohn’s disease: a multivariate analysis in 161 consecutive patients. Dis Colon Rectum. 2007;50:331–336. doi: 10.1007/s10350-006-0782-0. [DOI] [PubMed] [Google Scholar]
- 12.Müller-Wille R, Iesalnieks I, Dornia C, Ott C, Jung EM, Friedrich C, Schill G, Hoffstetter P, Zorger N, Schreyer AG. Influence of percutaneous abscess drainage on severe postoperative septic complications in patients with Crohn’s disease. Int J Colorectal Dis. 2011;26:769–774. doi: 10.1007/s00384-011-1135-6. [DOI] [PubMed] [Google Scholar]
- 13.Xie Y, Zhu W, Li N, Li J. The outcome of initial percutaneous drainage versus surgical drainage for intra-abdominal abscesses in Crohn’s disease. Int J Colorectal Dis. 2012;27:199–206. doi: 10.1007/s00384-011-1338-x. [DOI] [PubMed] [Google Scholar]
- 14.Mino JS, Gandhi NS, Stocchi LL, Baker ME, Liu X, Remzi FH, Monteiro R, Vogel JD. Preoperative risk factors and radiographic findings predictive of laparoscopic conversion to open procedures in Crohn's disease. J Gastrointest Surg. 2015;19(6):1007–1014. doi: 10.1007/s11605-015-2802-7. [DOI] [PubMed] [Google Scholar]
- 15.Goyer P, Alves A, Bretagnol F, Bouhnik Y, Valleur P, Panis Y. Impact of complex Crohn's disease on the outcome of laparoscopic ileocecal resection: a comparative clinical study in 124 patients. Dis Colon Rectum. 2009;52(2):205–210. doi: 10.1007/DCR.0b013e31819c9c08. [DOI] [PubMed] [Google Scholar]
- 16.Sangster W, Berg AS, Choi CS, Connelly TM, Chesnut CH, 3rd, Koltun WA, Stewart DB., Sr Outcomes of early ileocolectomy after percutaneous drainage for perforated ileocolic Crohn's disease. Am J Surg. 2016;212(4):728–734. doi: 10.1016/j.amjsurg.2016.01.044. [DOI] [PubMed] [Google Scholar]
- 17.Kristo I, Stift A, Argeny S, Mittlböck M, Riss S. Minimal-invasive approach for penetrating Crohn's disease is not associated with increased complications. Surg Endosc. 2016;30(12):5239–5244. doi: 10.1007/s00464-016-4871-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bermejo F, Garrido E, Chaparro M, Gordillo J, Mañosa M, Algaba A, López-Sanromán A, Gisbert JP, García-Planella E, Guerra I, Domènech E. Efficacy of different therapeutic options for spontaneous abdominal abscesses in Crohn's disease: are antibiotics enough? Inflamm Bowel Dis. 2012;18(8):1509–1514. doi: 10.1002/ibd.21865. [DOI] [PubMed] [Google Scholar]
- 20.Garcia JC, Persky SE, Bonis PA, Topazian M. Abscesses in Crohn's disease: outcome of medical versus surgical treatment. J Clin Gastroenterol. 2001;32(5):409–412. doi: 10.1097/00004836-200105000-00010. [DOI] [PubMed] [Google Scholar]