Abstract
Objective:
To characterize the indications, timing, barriers, and perceived value of rehabilitation currently provided for individuals with moderate or severe traumatic brain injury (TBI) admitted to the intensive care unit (ICU) based on the perspectives of providers who work in the ICU setting.
Participants:
Members (n = 66) of the Neurocritical Care Society and the American Congress of Rehabilitation Medicine.
Design:
An anonymous electronic survey of the timing of rehabilitation for patients with TBI in the ICU.
Main Measures:
Questions asked about type and timing of rehabilitation in the ICU, extent of family involvement, participation of physiatrists in patient care, and barriers to early rehabilitation.
Results:
Sixty-six respondents who reported caring for patients with TBI in the ICU completed the survey; 98% recommended rehabilitative care while patients were in the ICU. Common reasons to wait for the initiation of physical therapy and occupational therapy were normalization of intracranial pressure (86% and 89%) and hemodynamic stability (66% and 69%).
Conclusions:
The majority of providers caring for patients with TBI in the ICU support rehabilitation efforts, typically after a patient is extubated, intracranial pressure has normalized, and the patient is hemodynamically stable. Our findings describe current practice; future studies can be designed to determine optimal timing, intensity, and patient selection for early rehabilitation.
Keywords: brain injury recovery, critical care practice, rehabilitation, traumatic brain injury
Traumatic Brain Injury (TBI) affects 2.8 million people in the United States each year and is a leading cause of disability1; prevalence of disability following TBI is between 3.2 and 5.3 million people in the United States. Although some moderate and severe TBI survivors live with significant long-term physical, cognitive, and psychological disabilities postinjury, many have good functional recoveries following prolonged rehabilitation.2,3 After moderate or severe TBI, adults are usually initially admitted to an intensive care unit (ICU). Most patients in the ICU eventually need extensive rehabilitation, as those with critical illness are at risk of severe and prolonged neuromuscular complications.4 Following TBI, many neuro-ICUs engage brain injury rehabilitation specialists (physiatrists, neurologists, and therapists) for physical, occupational, cognitive, and speech rehabilitation.
Evidence to inform rehabilitation practices for patients with TBI admitted to the ICU has largely been extrapolated from the broader critical care literature. In medical ICUs, rehabilitation of patients who are mechanically ventilated reduces ICU and hospital length of stay and delirium.4 In children, early rehabilitation following TBI resulted in shorter and more efficient rehabilitation periods following ICU discharge.5 Use of a mobility protocol in critically ill patients with cardiothoracic surgery produced clinically significant reductions in hospital length of stay, ICU days, ICU readmission rates, and pressure ulcer prevalence.6 However, recent data from patients with an ischemic stroke suggested that early mobilization is associated with worse long-term outcomes.7 Subjects in the intervention arm of this study were mobilized within 24 hours of stroke, and it is possible that the early time frame may have contributed to the discouraging results. A similarly defined time frame for early rehabilitation has not been established within the TBI literature. Families of patients with TBI likely require attention as well, as one study suggested that posttraumatic stress disorder and depression at 3 months are higher in family members of patients with TBI compared with critically ill patients with other diagnoses.8 We surveyed practitioners of 2 medical societies who commonly care for individuals with TBI about current rehabilitation practices and ascertained how clinical status affects current practice.
METHODS
We conducted an anonymous electronic survey using REDcap (Research Electronic Data Capture) through the Neurocritical Care Society (NCS) and the American Congress of Rehabilitation Medicine (ACRM), designated by the local institutional review board as nonhuman subject research.9 Questions asked about the timing of rehabilitation in the ICU, the extent of family involvement, participation of physiatrists in patient care, and the barriers to early rehabilitation. The survey was piloted within the group of neurointensivists and physiatrists at our institution to obtain feedback regarding the question content, wording of the items, need for additional items, and ease of use of the survey. A link to the final survey (see Table 1) was posted via an e-mailed newsletter to the ACRM in July 2016 and was posted to the NCS Web site from July 2016 until November 2017. Using NCS and ACRM membership listservs, 2 e-mail reminders were sent to each group. At the time the survey was launched, there were approximately 2400 members of the NCS and 2000 members of the ACRM, although it is unknown what proportion care for patients with TBI in the ICU setting. No incentives were offered to those who completed the survey, and responses remained anonymous.
TABLE 1.
Survey questions
| Questions | Responses, n (%, 95% CI) |
|---|---|
|
| |
| 1. Do you take care of or consult on patients with traumatic brain injury in the ICU? |
Yes 66 (68%, 58.23%–76.5%) No 31 (32%, 23.5%–41.8%) |
| 2. What is your current level of training? |
Resident 3 (4.5%, 0.5%–9.5%) Fellow 5 (7.6%, 1.2%–14%) Attending 27 (40.9%, 30.2%–51.6%) APP 8 (12.1%, 4.2%–20%) Nurse 6 (9.1%, 2.2%–16%) PT 6 (9.1%, 2.2%–16%) OT 5 (7.6%, 1.2%–14%) Speech 5 (7.6%, 1.2%–14%) Other 1 (1.5%, 1.4%–4.4%) |
| 3. Do you ever recommend rehabilitation care (defined as physical therapy, occupational therapy, or speech therapy) in the ICU for patients with TBI? |
Yes 61 (98.4%, 98.35%–98.45%) No 1 (1.6%, 1.5%–4.7%) |
| 4. Do you ever involve a physiatrist in the care of patients with TBI in your ICU? |
Always 9 (13.6%, 5.3%–21.9%) Usually 24 (36.4%, 24.8%–35.6%) Sometimes 16 (24.2%, 13.9%–34.5%) Rarely 9 (13.6%, 5.3%–21.9%) Never 8 (12.1%, 4.4%–20%) |
| 5. Who is involved in the decision in your ICU when patients with TBI have rehabilitation care initiated? |
Trauma 43 (66%, 54%–76.5%) NCC 55 (84.6%, 74%–91.4%) Neurosurgery 51 (78.5%, 67%–86.7%) Neurology 24 (36.9%, 26.2%–49%) PM&R 33 (50.8%, 38.9%–62.5%) PT 39 (60%, 38.9%–62.5%) OT 35 (53.8%, 41.9%–65.4%) Speech therapy 29 (44.6%, 33.2%–56.7%) Other 2 (3.1%, 0.9%–10.6%) |
| 6. When does rehabilitation begin in your institution? Is it based on (time, milestones since injury, or different depending on type of rehabilitation)? |
Time since injury 7 (10.6%, 5.2%–20.3%) Once milestones met 25 (37.9%, 27.2%–49.9%) Different, based on type 34 (51.5%, 39.7%–63.2%) |
| 7. If milestones were answered, what milestones do you use to decide when to initiate physical therapy (defined as assessment by the physical therapist followed by recommendations for motor skills, including passive range of movement)? |
No further surgical procedures 10 (22.7%, 12.8%–37%) ICP normalized 36 (81.8%, 68%–90.5%) Afebrile 6 (13.6%, 6.4%–26.7%) Off vasopressors 16 (36.4%, 23.8%–51.1%) Intracranial monitors removed 15 (34.1%, 22%–49%) Extubated 9 (20.5%, 11.2%–34.5%) After trach if needed 6 (13.6%, 6.4%–26.7%) HD stable 32 (72.7%, 58.2%–83.7%) Unchanged neurologic examination 7 (15.9%, 7.9%–29.4%) Other 4 (9.1%, 3.6%–21.2%) |
| 8. If you answered “milestones” above, please indicate which milestones are necessary before speech therapy is started. Please check all that apply. |
No further surgical procedures 4 (10.8%, 4.3%–24.7%) ICP normalized 19 (51.4%, 35.9%–66.6%) Afebrile 2 (5.4%, 1.5%–17.7%) Off vasopressors 6 (16.2%, 7.7%–31.1%) ICP monitors removed 11 (29.7%, 17.5%–45.8%) Extubated 26 (70.3%, 54.2%–82.5%) Post trach 15 (40.5%, 26.4%–56.5%) HD stable table 16 (43.2%, 28.7%–59.1%) Unchanged neurologic examination 2 (5.4%, 1.5%–17.7%) Other 6 (16.2%, 6.8%–32.7%) |
| 9. If you answered “milestones” above, please indicate which milestones are necessary before occupational therapy is started. Please check all that apply. |
No further surgical procedures 7 (20%, 10%–35.9%) ICP normalized 32 (91.4%, 75.8%–97.7%) Afebrile 5 (14.3%, 6.3%–29.4%) Off vasopressors 16 (45.7%, 30.5%–61.9% ICP monitors out 16 (45.7%, 30.5%–61.8%) Extubated 12 (34.3%, 20.8%–50.9%) After trach 7 (20%, 10%–35.9%) HD stable table 27 (77.1%, 61%–88%) Unchanged neurologic examination 5 (14.3%, 6.3%–29.3%) Other 0 (0%; 0%–9.9%) |
| 10. To what extent are patients’ families involved in the decision as to when therapy is started in the ICU? |
Always 10 (15.6%, 8.7%–16.4%) Usually 6 (9.4%, 4.4%–19%) Sometimes 16 (25%, 16%–36.8%) Rarely 25 (39.1%, 28.1%–51.3%) Never 7 (11%, 5.4%–20.9%) |
| 11. Some people say that “acute” therapies such as range of movement, strengthening, ambulation, neurostimulation, or other acute therapies are useful prior to more formalized rehabilitation. Please share your thoughts on initiating these therapies in the ICU, and the barriers that may exist in your institution. | See Table 2 |
Abbreviations: APP, advanced practice provider; CI, confidence interval; HD, hemodynamically; ICP, intracranial pressure; ICU, intensive care unit; NCC, neurocritical care; OT, occupational therapist; PM&R, physical medicine and rehabilitation; PT, physical therapist; TBI, traumatic brain injury.
Potential respondents were first asked whether they cared for patients with TBI in the ICU. Only those who answered yes were given the opportunity to complete the survey. The survey items in Table 1 consisted of a series of both open-ended and closed-ended questions. Closed-ended questions were analyzed using descriptive statistics. One open-ended question was analyzed using content analysis (Q11, Table 1). Early rehabilitation was defined in the survey as, “acute therapies such as range of movement, strengthening, ambulation, neurostimulation, or other acute therapies prior to more formalized rehabilitation.” The initial coding scheme for this item was developed based on the content of responses by a neurointensivist (N.K.) and a neurocritical care nurse practitioner (K.R.). The responses were read multiple times to identify themes. After discussion, a coding frame was developed and responses were coded by both N.K. and K.R. independently. If new codes emerged the coding frame was changed, and responses were recoded according to the new structure. Toward the end of the study, no new themes emerged, suggesting that the major themes had been identified.10 Codes were organized into themes, and Cohen’s κ was calculated to determine agreement. A structured codebook was developed and applied to the responses.
RESULTS
Of 97 people who followed the survey link, the 66 (68%) who cared for patients with TBI in the ICU were invited to complete the entire survey. These included 27 attending physicians, 8 advanced practice providers (ie, nurse practitioners and physician assistants), 16 therapists (occupational, speech, and physical therapy), 6 nurses, 5 physicians in neurocritical care fellowship, 3 residents, and 1 other. Respondents represented several regions of the United States (northeast, southeast, midwest, and west). Of all respondents, 98% recommended rehabilitative care while patients with TBI were in the ICU.
Although 98% of respondents recommended rehabilitative care while individuals are still in their ICU course, views about the timing of rehabilitation differed. Only 11% of respondents based the decision to start rehabilitation on the amount of time since the injury had occurred; 38% based this decision on patient milestones that needed to be met, and others stated that it depended on the type of rehabilitation in question (52%). The most common milestones to meet for initiation of physical therapy were normalization of intracranial pressure (ICP) (82%) and hemodynamic stability (73%); the same milestones were required for initiation of occupational therapy (91% and 77%, respectively). The variation of milestones that needed to be met before starting physical therapy is described further in Figure 1. Speech therapy was typically recommended after extubation (70%) and normalization of ICP (51%).
Figure 1.
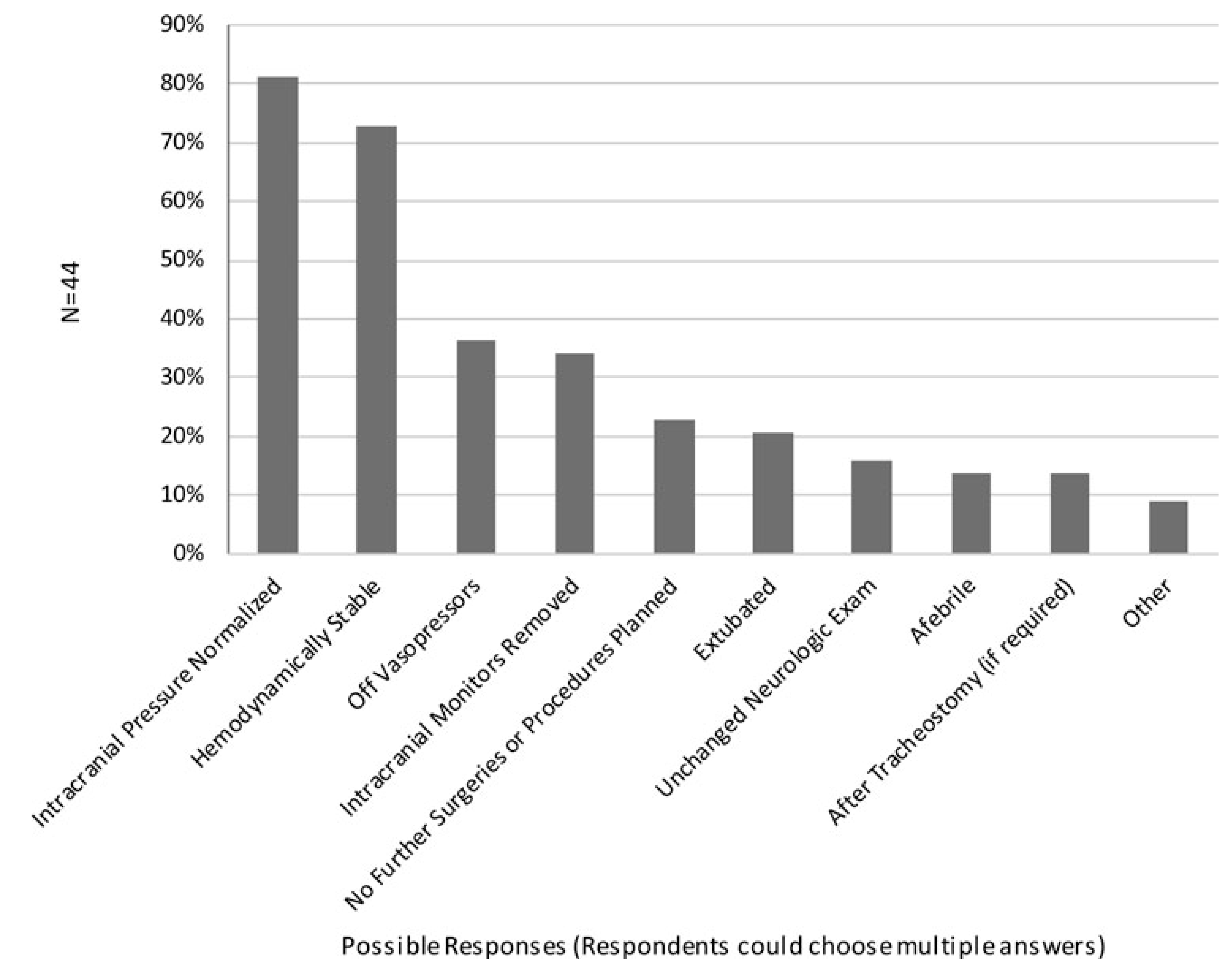
Milestones to starting physical therapy.
Physiatrists were always involved in the care of the patient in the ICU in 14% of cases, usually in 36% of cases, sometimes in 24%, rarely in 14%, and never in 12% of cases. Of those who engaged physiatry, they were involved at various time points after admission, but mostly during the acute hospitalization period: 13% at the time of admission, 70% during the hospitalization, 14% at the time of discharge or to facilitate additional discharge planning, and 44% stated “other.”
The decision to start rehabilitation in the ICU is made by many different teams of practitioners. The neurocritical care team was involved in this decision more than any other specialty (85% of the time). Other specialties that contributed to this decision included neurosurgery (79%), trauma surgery (66%), physical therapy (60%), occupational therapy (54%), speech therapy (45%), physiatry (51%), and neurology (37%). Overall, families were involved in the decision to start therapy “rarely” in 39% of cases, “always” in 16%, “usually” in 9%, “sometimes” in 25%, and “never” in 11%.
Our last question explored opinions about and barriers to early rehabilitation, which fell into 3 main themes: provider barriers, patient barriers, and organizational barriers. Within these 3 themes, there were a total of 13 codes (see Table 2). Cohen’s κ for this coding scheme was 0.95. The most frequently cited barrier to rehabilitation in our qualitative analysis was limited resources. Example responses of this included, “Daily PT/OT is rarely performed due to short staffed therapists and RN high ratios cause time constraints,” “Barriers are largely volume. Supply versus demand. The demand is always for patients to be ‘cleared’ prior to discharge or for SLP (speech therapy) deciding about NPO status/tube placement, again so the discharge can proceed. Other demand for PT is the ortho hips/knee surgeries are also high priority,” or “Daily PT/OT is rarely performed due to short staffed therapists and RN high ratios. Rehab in the acute phase is extremely beneficial—even if it’s just range of motion for comatose patients.”
TABLE 2.
Brief description of codes
| Code | Description | n (%, 95% CI) |
|---|---|---|
|
| ||
| Codes describing values of early rehabilitation | ||
| PROPONENT | Participants may describe a general appreciation of early PT/OT without going into specific reasons for why they feel that way. | 21 (24%, 16.6%–34.5%) |
| BENEFICIAL | Describes any of the benefits, where they either cite evidence or personal experience of good outcomes w/early rehab. | 9 (10.5%, 5.6%–18.7%) |
| FAMILY | Describes reasons families benefit, and reasons (nonmedical) that patients benefit when rehab is started in the ICU. | 8 (9.3%, 4.8%–17.3%) |
| EDUCATE | Providers agree in the value of PT/OT, but also go one step beyond agreeing to demonstrate a need to educate others on its value. | 3 (3.5%, 1.2%–9.8%) |
| Provider barriers | ||
| SKILLSET | Describes reasons that rehab is held because someone just does not know why and how to do it. | 4 (4.7%, 1.8%–11.4%) |
| UNWILLING | The facility may have abundant resources, and skilled staff, but if there is not willingness by the staff to perform PT/OT, it does not get done. | 3 (3.5%, 1.2%–9.8%) |
| BIASES | Institutional, cultural, national, and/or learned biases about TBI or rehab may inhibit effective early PT/OT. | 3 (3.5%, 1.2%–9.8%) |
| UNINVOLVED | Describing a general attitude that someone has about the role of therapists; that someone else should be in charge of organizing and making sure of follow-through. | 2.5 (2.9%, 1.2%–10.6%) |
| Patient barriers | ||
| STEPWISE APPROACH | Describes specific patient safety concerns. Used to describe very specific ICU scenarios that take place and prevent rehab. | 10.5 (12.2%, 7.3%–22.2%) |
| Organizational barriers | ||
| RESOURCES | Describes reasons that the rehab would be done otherwise, but not enough time/money/people who are willing to do it. | 12 (14%, 8.2%–22.8%) |
| SUGGESTIONS | Describes a suggestion that we can do to improve the use of rehab. Use for system level. | 8 (9.3%, 4.8%–17.3%) |
| INSURANCE | Providers may be limited in the care they provide to patients simply related to what insurance may pay. | 1 (1.2%, 0.2%–6.2%) |
| LEADERSHIP | An important aspect to the success of rehabilitation programs is a leadership structure that hires and compels physicians, nurses, and therapists to ensure patients’ rehab needs are met. | 1 (1.2%, 0.2%–6.2%) |
Abbreviations: CI, confidence interval; ICU, intensive care unit; OT, occupational therapist; PT, physical therapist.
DISCUSSION
In this mixed-methods study describing practice patterns and barriers to rehabilitation of patients with moderate and severe TBI in the ICU, we found that practitioners caring for this patient population were nearly all proponents of rehabilitation in the ICU; that they face numerous barriers to instituting early rehabilitation; and that they support a milestone-driven approach to initiating rehabilitation. Most barriers remain unexplored for individuals who have sustained a TBI, but fell into 3 major categories: provider, patient, and organizational characteristics. The most frequently cited barrier to rehabilitation in our qualitative analysis was limited resources. The general critical care literature suggests that an initial increased need for resources of PT/OT and other consultation services required for rehabilitation is offset by reduced delirium, higher levels of functional mobility, and decreased ICU and hospital length of stay.11
In our qualitative analysis, patient safety concerns were described as the second most common barrier to rehabilitation. Data related to safety of early rehabilitation in the neurocritical care patient population are limited. In children, early rehabilitation in the ICU following TBI resulted in shorter and more efficient rehabilitation periods following ICU discharge, and early passive range of movement did not result in increased ICP.5,12 In ischemic stroke, however, data from A Very Early Rehabilitation Trial (AVERT) demonstrated harm with early (within 24 hours) mobilization.7 In our survey, respondents preferred using a milestone approach rather than predefined period to guide rehabilitation in the ICU. It is yet unknown whether the risks of rehabilitation early in an ICU course may outweigh the benefits, and this decision may need to be made on a case-by-case basis. Early mobility is likely favorable as long as a patient is medically stable, which is congruent with practice patterns identified in this survey. Our findings do not provide specific insight into the safety of early rehabilitation but rather characterize current practice.
We emphasize the preliminary nature of our report and note that much research is needed regarding early rehabilitation of individuals with TBI in the ICU. Specifically, 3 research needs regarding rehabilitation in patients with TBI in the ICU include (1) determining the optimal timing for rehabilitation, (2) determining the safety of rehabilitation in the ICU, and (3) determining the efficacy of ICU rehabilitation regarding what types and frequency of rehabilitation may be best depending on type and severity of injury, other injuries and comorbidities, and the need for invasive monitoring. In addition, as this line of research moves forward, it will be important to determine how these goals can be achieved while factoring in varying types of practitioners, hospital practice settings, and years in practice.
Our survey further revealed that multiple specialties play a role in the decision to start rehabilitation. Although this may be institution-dependent, research in nonneurologically injured patient populations suggests that a protocolized approach implemented by those on the “front line” of care, coupled with mandatory electronic mobilization orders, may be most effective.11,13–17 Such protocols need to be multidisciplinary, involving therapists, technicians, physicians, nurses, nursing assistants, and respiratory therapists if an ICU rehabilitation protocol or program is to be successful.11
Limitations
Although a wide breadth of geographic areas and specialties is represented in our survey, we had an overall relatively low response rate. An additional limitation was the fact that we did not link responses to the specialty of respondents, with both neurocritical care and physical medicine and rehabilitation physician specialties being represented. Although 98% endorsed rehabilitation in the ICU for individuals with TBI, this may not reflect universal support for early rehabilitation in this patient population since our respondents were all practitioners who cared for patients with TBI in the ICU. Our study was not designed to determine differences in perceptions between different clinicians. Our data should be considered informative of current practice, not definitive.
CONCLUSION
We demonstrated consensus among respondents on the recommendation for early rehabilitative care following TBI, typically after a patient is extubated, ICP has normalized, and the patient is hemodynamically stable. To generate evidence-based guidance to inform rehabilitation practices for individuals with TBI admitted to the ICU, prospective studies are warranted to evaluate the merits of these provider-reported rehabilitation initiation criteria and harms of barriers to rehabilitation.
Footnotes
The authors declare no conflicts of interest.
Contributor Information
Natalie Kreitzer, Department of Emergency Medicine, University of Cincinnati, Ohio; Department of Neurology and Rehabilitation Medicine, University of Cincinnati, Ohio.
Kelly Rath, Department of Neurology and Rehabilitation Medicine, University of Cincinnati, Ohio; University of Cincinnati College of Nursing, Ohio.
Brad G. Kurowski, Department of Pediatrics, University of Cincinnati, Ohio.
Tamilyn Bakas, University of Cincinnati College of Nursing, Ohio.
Kim Hart, Department of Emergency Medicine, University of Cincinnati, Ohio.
Christopher J. Lindsell, Department of Biostatistics, Vanderbilt University Medical Center, Nashville, Tennessee.
Opeolu Adeoye, Department of Emergency Medicine, University of Cincinnati, Ohio; Department of Neurology and Rehabilitation Medicine, University of Cincinnati, Ohio; Department of and Neurosurgery, University of Cincinnati, Ohio.
REFERENCES
- 1.Rutland-Brown W, Langlois JA, Thomas KE, Xi YL. Incidence of traumatic brain injury in the United States, 2003. J Head Trauma Rehabil. 2006;21(6):544–548. [DOI] [PubMed] [Google Scholar]
- 2.Zaloshnja E, Miller T, Langlois JA, Selassie AW. Prevalence of long-term disability from traumatic brain injury in the civilian population of the United States, 2005. J Head Trauma Rehabil. 2008;23(6):394–400. [DOI] [PubMed] [Google Scholar]
- 3.Thurman DJ, Alverson C, Dunn KA, Guerrero J, Sniezek JE. Traumatic brain injury in the United States: a public health perspective. J Head Trauma Rehabil. 1999;14(6):602–615. [DOI] [PubMed] [Google Scholar]
- 4.Needham DM. Mobilizing patients in the intensive care unit: improving neuromuscular weakness and physical function. JAMA. 2008;300(14):1685–1690. [DOI] [PubMed] [Google Scholar]
- 5.Tepas JJ 3rd, Leaphart CL, Pieper P, et al. The effect of delay in rehabilitation on outcome of severe traumatic brain injury. J Pediatr Surg. 2009;44(2):368–372. [DOI] [PubMed] [Google Scholar]
- 6.Floyd S, Craig SW, Topley D, Tullmann D. Evaluation of a progressive mobility protocol in postoperative cardiothoracic surgical patients. Dimens Crit Care Nurs. 2016;35(5):277–282. [DOI] [PubMed] [Google Scholar]
- 7.AVERT Trial Collaboration group. Efficacy and safety of very early mobilisation within 24h of stroke onset (AVERT): a randomised controlled trial. Lancet. 2015;386(9988):46–55. [DOI] [PubMed] [Google Scholar]
- 8.Warren AM, Rainey EE, Weddle RJ, Bennett M, Roden-Foreman K, Foreman ML. The intensive care unit experience: psychological impact on family members of patients with and without traumatic brain injury. Rehabil Psychol. 2016;61(2):179–185. [DOI] [PubMed] [Google Scholar]
- 9.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guest G, MacQueen KM, Namey EE. Applied Thematic Analysis. Thousand Oaks, CA: Sage; 2011. [Google Scholar]
- 11.Needham DM, Korupolu R, Zanni JM, et al. Early physical medicine and rehabilitation for patients with acute respiratory failure: a quality improvement project. Arch Phys Med Rehabil. 2010;91(4):536–542. [DOI] [PubMed] [Google Scholar]
- 12.Roth C, Stitz H, Kalhout A, Kleffmann J, Deinsberger W, Ferbert A. Effect of early physiotherapy on intracranial pressure and cerebral perfusion pressure. Neurocritical Care. 2013;18(1):33–38. [DOI] [PubMed] [Google Scholar]
- 13.Hopkins RO, Spuhler VJ, Thomsen GE. Transforming ICU culture to facilitate early mobility. Crit Care Clin. 2007;23(1):81–96. [DOI] [PubMed] [Google Scholar]
- 14.Thomsen GE, Snow GL, Rodriguez L, Hopkins RO. Patients with respiratory failure increase ambulation after transfer to an intensive care unit where early activity is a priority. Crit Care Med. 2008;36(4):1119–1124. [DOI] [PubMed] [Google Scholar]
- 15.Dinglas VD, Colantuoni E, Ciesla N, Mendez-Tellez PA, Shanholtz C, Needham DM. Occupational therapy for patients with acute lung injury: factors associated with time to first intervention in the intensive care unit. Am J Occup Ther. 2013;67(3):355–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morris PE, Goad A, Thompson C, et al. Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Crit Care Med. 2008;36(8):2238–2243. [DOI] [PubMed] [Google Scholar]
- 17.Hildreth AN, Enniss T, Martin RS, et al. Surgical intensive care unit mobility is increased after institution of a computerized mobility order set and intensive care unit mobility protocol: a prospective cohort analysis. Am Surg. 2010;76(8):818–822. [PubMed] [Google Scholar]


