Abstract
Summary
This study examines the difference in length of stay and total hospital charge by income quartile in hip fracture patients. The length of stay increased in lower income groups, while total charge demonstrated a U-shaped relationship, with the highest charges in the highest and lowest income quartiles.
Introduction
Socioeconomic factors have an impact on outcomes in hip fracture patients. This study aims to determine if there is a difference in hospital length of stay (LOS) and total hospital charge between income quartiles in hospitalized hip fracture patients.
Methods
National Inpatient Sample (NIS) data from 2016 to 2018 was used to determine differences in LOS, total charge, and other demographic/clinical outcomes by income quartile in patients hospitalized for hip fracture. Multivariate regressions were performed for both LOS and total hospital charge to determine variable impact and significance.
Results
There were 860,045 hip fracture patients were included this study. With 222,625 in the lowest income quartile, 234,215 in the second, 215,270 in the third, and 190,395 in the highest income quartile. LOS decreased with increase in income quartile. Total charge was highest in the highest quartile, while it was lowest in the middle two-quartiles. Comorbidities with the largest magnitude of effect on both LOS and total charge were lung disease, kidney disease, and heart disease. Time to surgery post-admission also had a large effect on both outcomes of interest.
Conclusion
The results demonstrate that income quartile has an effect on both hospital LOS and total charge. This may be the result of differences in demographics and other clinical variables between quartiles and increased comorbidities in lower income levels. The overall summation of these socioeconomic, demographic, and medical factors affecting patients in lower income levels may result in worse outcomes following hip fracture.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00198-021-06260-3.
Keywords: Length of stay, Hospital charges, Outcomes, Hip fracture, NIS database
Introduction
Fractures of the hip are one of the most common orthopedic conditions requiring hospitalization and are a significant public health concern. This is especially true in the ageing and elderly population, which experiences significant morbidity and mortality due to this injury [1, 2]. Between 2000 and 2009, the lowest hip fracture rate in white women, the demographic group with the highest incidence of hip fracture, was still as high as 975.2 per 100,000 women [3]. It is projected that by the year 2050, the worldwide number of hip fractures will reach 4.5–6.26 million, from 1.26 to 1.66 million in 1990 [4, 5]. While reports of age-standardized incidence differ between different areas of the world, the prevalence is increasing steadily worldwide due to the ageing population [2]. Hip fractures contribute significantly to healthcare costs, and it is projected that by the year 2040, they will contribute $9.8 billion to US healthcare spending [1]. Thus, it is essential to identify and properly manage the economic aspects of caring for those hip fracture patients.
Healthcare inequality has become a major topic of discussion in recent years in the USA as more light has been shed on issues that were traditionally not discussed or investigated. Social factors including socioeconomic status, race, education level, marital status, payer type, area of residence, smoking status, and alcohol use have been studied and may have a significant impact on incidence and treatment outcomes in hip fracture patients [6–11]. The impact of these social determinants could be a contributing cause to increased healthcare spending. One indicator of this inequality of healthcare could be differences in hospital length of stay (LOS) and total hospital charge following hip fracture, as this is the most common fracture requiring inpatient treatment [12, 13].
Hospital length of stay is a key performance indicator for hospitals and may impact both patient outcomes and healthcare spending [14, 15]. Increased LOS brings increased costs both for patients and hospitals. Increasing charges to patients would intuitively be a positive for hospitals as businesses. However, reimbursement to hospitals by insurance is rarely equal to what is being charged for treating patients [16]. Thus, it benefits both the country as a whole as well as individual hospitals to reduce LOS and costs for patients with hip fractures. Increased LOS can also be associated with increased mortality in hospitalized patients [14]. Reducing unnecessarily long hospitalizations could lead to both decreased spending and decreased patient mortality. While there are studies examining LOS and influencing factors following hip fracture [17, 18], to our knowledge, there are no studies examining differences in LOS of hip fracture patients by income level. Income level is one of the key contributors of a person’s socioeconomic status and impacts many other social factors including insurance payer and area/type of residence, among others. This study aims to determine if there is a difference in LOS and total hospital charge by income level for patients hospitalized with hip fractures and seeks to examine differences in LOS and cost between different surgical interventions, payer status, and comorbidities in hip fracture patients.
Materials and methods
The discharge data from the National Inpatient Sample (NIS), Healthcare Cost and Utilization Project (HCUP), Agency for Healthcare Research and Quality from 2016 to 2018 was utilized for this study. The NIS is the largest publicly available all-payer inpatient healthcare database. It is designed to produce US regional and national estimates of inpatient utilization, access, charges, quality, and outcomes. It uses inpatient and discharge data from hospitals in 47 states and the District of Colombia representing 20% of US hospitals weighted to be representative of 97% of the US population. Data includes patient demographics, hospital demographics, hospital LOS, diagnoses, procedures, comorbidities, complications, mortality, and discharge destination [19]. At the time of this study, data from 2018 were the most up to date available for analysis. We used data from 2016 to 2018 based on the ability to use ICD-10 codes. The study was determined as non-human subject research project by the institutional review board.
Participants
The primary outcomes of interest were LOS and total charge for patients hospitalized with traumatic hip fracture, stratified by income quartiles. We included data from patients aged 18 and older hospitalized with hip fracture, diagnosed based on the ICD-10 codes S72.0, S72.1, and S72.2 and subgroups identifying traumatic fractures of the proximal end of the femur, and who underwent total hip arthroplasty (THA), hemiarthroplasty, or internal fixation. The full list of ICD-10 codes included can be seen in Supplemental Table 1. Only initial encounters for traumatic hip fracture and patients treated surgically were included. Patient encounters due to post-surgery complications including periprosthetic fracture, malunion, or nonunion, as well as non-traumatic fracture, were excluded. Patients treated non-operatively or via external fixation were excluded as well.
Baseline demographic and clinical information, hospital demographics, comorbidities, treatment, and discharge disposition data were collected and compared by income quartiles. Comorbidities included were heart disease, hyperlipidemia, hypertension, diabetes mellitus, lung disease, liver disease, kidney disease, peripheral vascular disease, cerebrovascular disease, cancer, dementia, and obesity (body mass index equal or greater than 30). Data for comorbid conditions was extracted via ICD-10 codes, a full list of which can be seen in Supplemental Table 1.
Outcomes
The primary outcomes of interest in this study were hospital LOS and total hospital charge. Data for both of these outcomes was extracted for each patient meeting inclusion criteria from the NIS database.
Identifying income
Income quartile is available for all inpatient stays recorded in the NIS. Income quartile was characterized based on the median income of the patient’s ZIP code, with quartile one being the lowest income and quartile four being the highest. The median income by ZIP code present in the NIS is derived from ZIP code-demographic data obtained from Claritas™ using five-digit ZIP codes.
Statistical analysis
Characteristics of hip fracture patients were described by income quartile, including total number, gender, age, race, hospital type at which they were treated, payer, discharge disposition, treatment received, time to first procedure after admission, mortality, and presence of comorbidities. Chi-square and ANOVA were used to evaluate differences in characteristics by income quartile for categorical and continuous variables, respectively. The association between income quartile and outcomes (LOS and total hospital charges) was evaluated using linear regression, using survey procedures to account for the NIS sampling scheme. The level of significance was set at 0.05, and all analyses were performed using SAS v. 9.4.Because the dataset obtained from the NIS is weighted, stepwise regression was unable to be performed. A univariate analysis of all variable for their effect on both outcomes of interest was first performed. All significant and clinically relevant variables were then inputted into the multivariate analysis. The model with the highest r2 value was then identified and used for final analysis.
Results
Full NIS data from 2016 to 2018 was first obtained. This was then filtered using ICD-10 CM codes S72.0, S72.1, and S72.2 and subgroups identifying initial encounters for traumatic fractures of the proximal end of the femur in order to avoid encounters due to post-surgery complications including periprosthetic fracture, malunion, or nonunion, as well as non-traumatic fracture. Once this was obtained, the results were then further filtered to patients treated operatively via THA, hemiarthroplasty, or internal fixation. The full list of codes used to identify our analytical sample can be seen in Supplemental Table 1.
Table 1 contains baseline patient demographic and clinical data for the study cohort by income quartile. In total there were 860,045 hip fracture patients included with 222,625 in the lowest income quartile; 234,215 in quartile two; 215,270 in quartile three; and 190,395 in the highest income quartile. The cohort contained 582,555 females in total (67.7%). The average age was 79.95 (SE 0.06) in quartile one, 77.54 (SE 0.06) in quartile two, 77.98 (SE 0.06) in quartile three, and 79.02 (SE 0.06) in quartile four. In general, there was a significant difference in most of the variables by income quartile. Further specific baseline data can be seen in Table 1.
Table 1.
Baseline demographic information and clinical and cost outcomes for patients hospitalized with hip fracture from 2016–2018 divided by patient income quartile
| Variable | Total | Income quartile one | Income quartile two | Income quartile three | Income quartile four | p value | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Number | Quartile % | Number | Quartile % | Number | Quartile % | Number | Quartile % | |||
| Total number of patients | 860,045 | 222,625 | 234,215 | 215,270 | 190,395 | * | ||||
| Gender (female) | 582,555 | 147,245 | 66.14 | 158,355 | 67.61 | 146,840 | 68.07 | 130,475 | 68.53 | < .0001 |
| Mortality | 13,440 | 3,610 | 1.62 | 3,880 | 1.66 | 3,295 | 1.53 | 2,655 | 1.39 | 0.0100 |
| Days from admission to procedure ** | 1.21 | 0.01 | 1.14 | 0.01 | 1.15 | 0.01 | 1.11 | 0.01 | < .0001 | |
| Age ** | 79.95 | 0.06 | 77.54 | 0.06 | 77.98 | 0.06 | 79.02 | 0.06 | < .0001 | |
| Age groups | < .0001 | |||||||||
| Less than 65 | 122,830 | 38,895 | 17.47 | 33,325 | 14.23 | 28,890 | 13.39 | 21,720 | 11.41 | |
| 65 to 79 | 269,190 | 74,110 | 33.29 | 74,035 | 31.61 | 65,740 | 30.47 | 55,305 | 29.05 | |
| 80 and over | 471,025 | 109,620 | 49.24 | 126,855 | 54.16 | 120,640 | 55.92 | 113,910 | 59.83 | |
| Race | < .0001 | |||||||||
| White | 715,070 | 171,385 | 76.98 | 198,340 | 84.68 | 183,100 | 84.88 | 162,245 | 85.21 | |
| Black | 38,730 | 21,180 | 9.51 | 7,935 | 3.39 | 5,825 | 2.70 | 3,790 | 1.99 | |
| Hispanic | 48,125 | 17,440 | 7.83 | 11,936 | 5.10 | 10,765 | 4.99 | 7,985 | 4.19 | |
| Asian/Pacific Islander | 15,160 | 2,050 | 0.92 | 2,485 | 1.06 | 3,915 | 1.81 | 6,710 | 3.52 | |
| Native American | 3,050 | 1,570 | 0.71 | 810 | 0.35 | 375 | 0.17 | 295 | 0.15 | |
| Others | 16,435 | 3,785 | 1.70 | 3,540 | 1.51 | 3,790 | 1.76 | 5,320 | 2.79 | |
| Hospital type | < .0001 | |||||||||
| Urban teaching | 533,560 | 125,880 | 56.54 | 133,040 | 56.80 | 140,140 | 64.96 | 134,500 | 70.64 | |
| Urban non-teaching | 232,605 | 51,065 | 22.94 | 64,145 | 27.39 | 63,265 | 29.33 | 54,130 | 28.43 | |
| Rural | 96,880 | 45,380 | 20.38 | 37,030 | 15.81 | 11,865 | 5.50 | 2,305 | 1.21 | |
| Obesity (BMI > 30) | 44,865 | 12,110 | 5.44 | 12,925 | 5.52 | 11,365 | 5.27 | 8,465 | 4.45 | < .0001 |
| Diabetes mellitus | 199,865 | 57,975 | 26.04 | 55,285 | 23.60 | 48,695 | 22.57 | 37,910 | 19.91 | < .0001 |
| Heart disease | 461,815 | 117,415 | 52.74 | 125,420 | 53.55 | 115,930 | 53.74 | 103,320 | 54.27 | < .0001 |
| Lung disease | 267,595 | 73,195 | 32.88 | 74,465 | 31.79 | 65,545 | 30.38 | 54,390 | 28.57 | < .0001 |
| Kidney disease | 238,665 | 62,180 | 27.93 | 64,385 | 27.49 | 59,810 | 27.73 | 52,290 | 27.46 | 0.2546 |
| Liver disease | 26,885 | 8,105 | 3.64 | 6,995 | 2.99 | 6,630 | 3.07 | 5,155 | 2.71 | < .0001 |
| Peripheral vascular disease | 52,460 | 12,710 | 5.71 | 13,475 | 5.75 | 13,410 | 6.22 | 12,865 | 6.76 | < .0001 |
| Hyperlipidemia | 357,370 | 85,415 | 38.37 | 96,060 | 41.01 | 91,675 | 42.50 | 84,220 | 44.23 | < .0001 |
| Hypertension | 422,585 | 110,835 | 49.79 | 115,555 | 49.34 | 104,050 | 48.23 | 92,145 | 48.40 | < .0001 |
| Cancer | 37,665 | 8,765 | 3.94 | 9,950 | 4.25 | 9,625 | 4.46 | 9,325 | 4.90 | < .0001 |
| Dementia | 223,465 | 54,880 | 24.65 | 59,755 | 25.51 | 55,830 | 25.88 | 53,000 | 27.84 | < .0001 |
| Cerebrovascular disease | 51,205 | 13,925 | 6.25 | 13,675 | 5.84 | 12,505 | 5.80 | 11,100 | 5.83 | 0.0108 |
| Alcohol abuse | 18,310 | 5,645 | 2.54 | 5,040 | 2.15 | 4,200 | 1.95 | 3,245 | 1.70 | < .0001 |
| Tobacco use | 7,535 | 2,685 | 1.21 | 2,255 | 0.96 | 1,645 | 0.76 | 950 | 0.50 | < .0001 |
| Payer | < .0001 | |||||||||
| Medicare | 708,770 | 177,995 | 79.95 | 193,230 | 82.50 | 178,150 | 82.58 | 159,395 | 83.72 | |
| Medicaid | 33,565 | 13,230 | 5.94 | 9,210 | 3.93 | 6,905 | 3.20 | 4,220 | 2.22 | |
| Private, including HMO | 87,305 | 20,040 | 9.00 | 22,530 | 9.62 | 22,950 | 10.64 | 21,785 | 11.44 | |
| Self-pay | 11,980 | 4,475 | 2.01 | 3,165 | 1.35 | 2,465 | 1.14 | 1,875 | 0.98 | |
| No charge | 935 | 385 | 0.17 | 275 | 0.12 | 170 | 0.08 | 105 | 0.06 | |
| Others | 19,465 | 6,140 | 2.76 | 5,395 | 2.30 | 4,475 | 2.07 | 3,455 | 1.81 | |
| Discharge disposition | ||||||||||
| Routine | 66,250 | 19,625 | 8.82 | 17,990 | 7.68 | 15,975 | 7.41 | 12,660 | 6.65 | |
| Transfer, short-term hospital | 7,530 | 2,000 | 0.90 | 2,150 | 0.92 | 1,690 | 0.78 | 1,690 | 0.89 | |
| Other transfers | 686,835 | 174,325 | 78.30 | 187,315 | 79.98 | 172,440 | 79.94 | 152,755 | 80.23 | |
| Home healthcare | 86,325 | 22,435 | 10.08 | 22,295 | 9.52 | 21,045 | 9.76 | 20,550 | 10.79 | |
| Against medical advice | 2,165 | 550 | 0.25 | 400 | 0.17 | 735 | 0.34 | 480 | 0.25 | |
| Died in hospital | 13,440 | 3,610 | 1.62 | 3,880 | 1.66 | 3,295 | 1.53 | 2,655 | 1.39 | |
| Treatment | ||||||||||
| Total hip arthroplasty | 56,125 | 12,920 | 5.80 | 14,900 | 6.36 | 14,460 | 6.70 | 13,845 | 7.27 | < .0001 |
| Hemiarthroplasty | 256,505 | 67,425 | 30.29 | 70,175 | 29.96 | 63,230 | 29.31 | 55,675 | 29.24 | 0.0009 |
| Internal fixation | 550,415 | 142,280 | 63.91 | 149,140 | 63.68 | 137,580 | 63.78 | 121,415 | 63.77 | 0.6919 |
Income quartiles for 2018 are defined as follows: quartile one, $1–$45,999 per year; quartile two, $46,000–$58,999 per year; quartile three, $59,000–$78,999 per year; and quartile four, $79,000 + per year. The discharge disposition “other transfers” includes transfer to skilled nursing facility, intermediate care facility, inpatient rehabilitation facility, or hospice facility. * indicates that a value is not applicable; ** indicates that values are mean and standard error of the mean
Length of stay between the four quartiles significantly declined with highest LOS in quartile one 5.85 days (SE 0.02) to the least in quartile four at 5.43 days (SE 0.02) (p < 0.0001). Total hospital charges increased from $79,183 (SE $342) in quartile one to $80,797 (SE $345) in quartile four, with quartiles two and three having charges of $74,758 (SE $299) and $76,200 (SE $318), respectively (p < 0.0001) (Fig. 1a and b). In-hospital mortality was highest in the lower income groups, 1.62% of quartile one compared to quartile four at 1.39%, and there was a declining trend within the quartiles (p = 0.01).
Fig. 1.
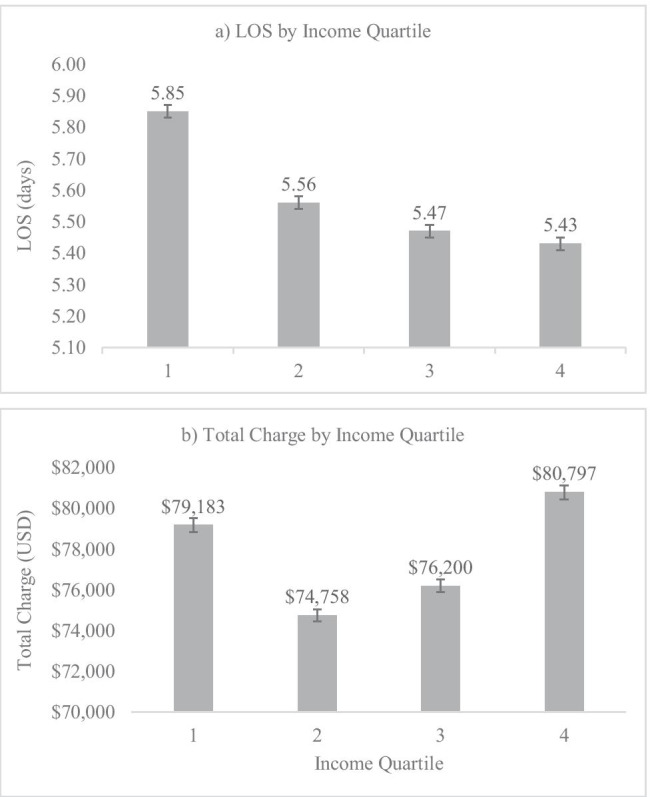
Mean a hospital length of stay and b total charge by income quartile in patients admitted for hip fracture in the USA from 2016 to 2018
The LOS was lowest in patients who underwent THA at 5.10 days (SE 0.03) and was the highest for hemiarthroplasty at 5.66 days (SE 0.01) while total charge was highest for THA at $89,227 (SE $583) followed by hemiarthroplasty at $78,781 (SE $242) and internal fixation at $74,142 (SE $223) (Fig. 2a and b).
Fig. 2.
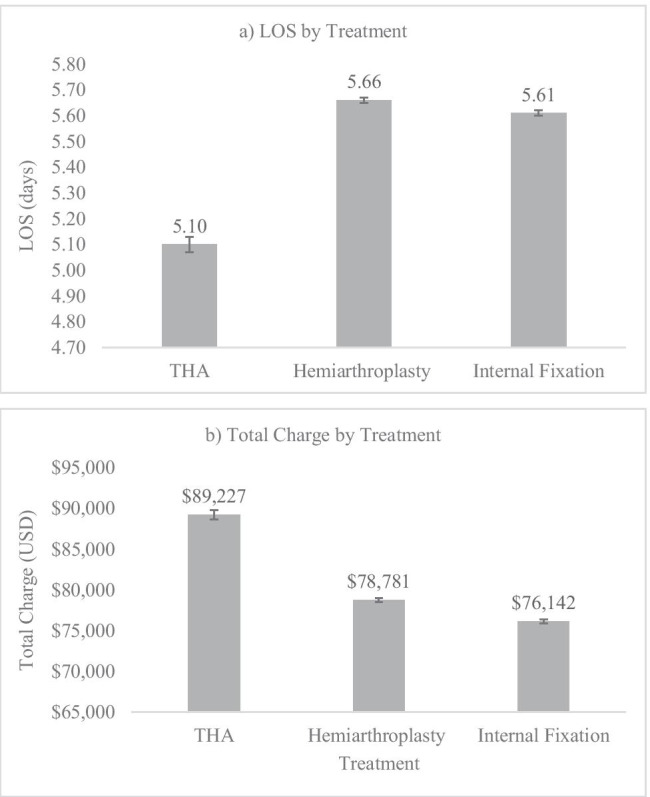
Mean a hospital length of stay and b total charge by treatment in patients admitted for hip fracture in the USA from 2016 to 2018
The multivariate regression analysis showed that income quartile had a significant negative correlation indicating increased LOS with decreasing income quartile (p = 0.0003) (Table 2). Among other significant variables that had a statistically significant impact on the LOS, time to surgery post-admission, significantly increased LOS (p < 0.0001). Patients with underlying comorbidities including lung disease, kidney disease, dementia, and heart disease had significantly increased LOS. However, other clinically relevant comorbidities including diabetes mellitus, peripheral vascular disease, hypertension, hyperlipidemia, alcohol abuse, and tobacco use did not increase LOS (Table 2).
Table 2.
Multivariate analysis of factors affecting hospital LOS in patients admitted for hip fracture in the USA from 2016 to 2018
| Parameter | Estimate | Lower CL | Upper CL | p value |
|---|---|---|---|---|
| Income quartile | − 0.0338123 | − 0.0520724 | − 0.0155522 | 0.0003 |
| Age | − 0.0244092 | − 0.0273682 | − 0.0214501 | < .0001 |
| Male gender (Relative to Female) | 0.3449496 | 0.3004535 | 0.3894458 | < .0001 |
| Race (relative to non-Hispanic White) | ||||
| Non-Hispanic Black | 0.7760883 | 0.6446756 | 0.9075010 | < .0001 |
| Hispanic | 0.3676909 | 0.2662212 | 0.4691606 | < .0001 |
| Asian/Pacific Islander | 0.1874194 | 0.0091960 | 0.3656429 | 0.0393 |
| Native American | 0.5286209 | 0.1677877 | 0.8894541 | 0.0041 |
| Others | 0.5354398 | 0.3727321 | 0.6981475 | < .0001 |
| Hospital type (relative to urban teaching) | ||||
| Rural | − 0.4867898 | − 0.5385295 | − 0.4350502 | < .0001 |
| Urban non-teaching | − 0.3548064 | − 0.3929594 | − 0.3166533 | < .0001 |
| Payer (relative to Medicare) | ||||
| Medicaid | 1.6975248 | 1.5038933 | 1.8911562 | < .0001 |
| Private (including HMO) | 0.5575911 | 0.4777067 | 0.6374754 | < .0001 |
| Self-pay | 1.2887966 | 1.0304067 | 1.5471866 | < .0001 |
| No charge | 1.1761948 | 0.4855325 | 1.8668571 | 0.0008 |
| Others | 0.7326667 | 0.5690949 | 0.8962385 | < .0001 |
| Treatment (relative to Internal fixation) | ||||
| THA | − 0.4316309 | − 0.4993724 | − 0.3638894 | < .0001 |
| Hemiarthroplasty | − 0.0518672 | − 0.0905698 | − 0.0131646 | 0.0086 |
| Time to procedure from admission | 1.1451689 | 1.1073847 | 1.1829531 | < .0001 |
| Discharge disposition (relative to routine) | ||||
| Transfer to other hospital | 1.0878288 | 0.7350175 | 1.4406401 | < .0001 |
| Other transfers | 1.0683765 | 0.9657489 | 1.1710042 | < .0001 |
| Home healthcare | 0.4672939 | 0.3585180 | 0.5760698 | < .0001 |
| Against medical advice | 0.3864527 | − 0.0279033 | 0.8008087 | 0.0676 |
| Unknown | 2.6177450 | − 0.6648302 | 5.9003201 | 0.1181 |
| Comorbidities | ||||
| Diabetes mellitus | 0.0147745 | − 0.0316435 | 0.0611924 | 0.5327 |
| Heart disease | 0.3749145 | 0.3330805 | 0.4167485 | < .0001 |
| Lung disease | 1.1385519 | 1.0888682 | 1.1882357 | < .0001 |
| Kidney disease | 0.7736794 | 0.7174082 | 0.8299505 | < .0001 |
| Liver disease | 0.7885916 | 0.6339791 | 0.9432042 | < .0001 |
| Peripheral vascular disease | − 0.1671887 | − 0.2473531 | − 0.0870243 | < .0001 |
| Hyperlipidemia | − 0.2997099 | − 0.3355533 | − 0.2638665 | < .0001 |
| Hypertension | 0.0319242 | -0.0081930 | 0.0720414 | 0.1188 |
| Cancer | 0.4885585 | 0.3770717 | 0.6000454 | < .0001 |
| Dementia | 0.3918989 | 0.3488988 | 0.4348991 | < .0001 |
| Cerebrovascular disease | 0.5301047 | 0.4344116 | 0.6257978 | < .0001 |
| Alcohol abuse | − 0.1868915 | − 0.3420123 | − 0.0317707 | 0.0182 |
| Tobacco use | − 0.1462290 | − 0.3858038 | 0.0933458 | 0.2316 |
| Obesity | 0.2798295 | 0.1806582 | 0.3790008 | < .0001 |
R2 = 0.2351
Male gender was significantly associated with increased LOS when compared to female gender (p < 0.0001). When compared to white race, LOS was significantly higher for all other races, with the highest being seen in black race (p < 0.0001). Patients receiving treatment in rural hospitals and urban non-teaching hospitals had longer LOS compared to urban teaching hospitals (p < 0.0001). When compared to Medicare, all other payer types had an increased LOS, with the highest LOS in Medicaid patients (p < 0.0001). Patients who underwent THA (p < 0.0001) and hemiarthroplasty (p = 0.0086) had shorter LOS compared to patients who underwent internal fixation. Compared to routine discharge, other transfer (which includes transfer to skilled nursing facility, intermediate care facility, inpatient rehabilitation facility, or hospice facility), transfer to other hospital, and discharge to home healthcare all significantly increased LOS (p < 0.0001). Full data analysis on LOS can be seen in Table 2.
Income quartile was positively correlated with hospital charge (p < 0.0001) indicating that higher quartile patients had higher charges than lower quartile patients. Increasing time to procedure after admission significantly increased total charge (p < 0.0001). Most of the comorbidities had a positive association with total charge. Interestingly, diabetes mellitus, peripheral vascular disease, hyperlipidemia, hypertension, tobacco use, and alcohol abuse did not increase total charge. Further analysis on variable effects on total charge can be seen in Table 3.
Table 3.
Multivariate analysis of factors affecting total hospital charge in patients admitted for hip fracture in the USA from 2016 to 2018
| Parameter | Estimate | Lower CL | Upper CL | p value |
|---|---|---|---|---|
| Income quartile | 734.176 | 427.590 | 1040.763 | < .0001 |
| Age | − 789.216 | − 843.774 | − 734.658 | < .0001 |
| Male gender (relative to female) | 5497.610 | 4770.967 | 6224.254 | < .0001 |
| Race (relative to non-Hispanic White) | ||||
| Non-Hispanic Black | 8585.047 | 6369.874 | 10,800.220 | < .0001 |
| Hispanic | 27,249.672 | 25,482.119 | 29,017.224 | < .0001 |
| Asian/Pacific Islander | 19,707.042 | 16,588.052 | 22,826.032 | < .0001 |
| Native American | − 3886.628 | − 8973.109 | 1199.854 | 0.1342 |
| Others | 18,068.392 | 14,886.066 | 21,250.718 | < .0001 |
| Hospital type (relative to Urban teaching) | ||||
| Rural | − 22,962.096 | − 23,657.348 | − 22,266.843 | < .0001 |
| Urban non-teaching | 28.225 | − 590.476 | 646.926 | 0.9288 |
| Payer (relative to Medicare) | ||||
| Medicaid | 16,066.887 | 13,122.847 | 19,010.928 | < .0001 |
| Private (including HMO) | 6080.776 | 4687.410 | 7474.142 | < .0001 |
| Self-pay | 10,391.994 | 6241.777 | 14,542.211 | < .0001 |
| No charge | 10,888.640 | − 475.734 | 22,253.013 | 0.0604 |
| Others | 6339.343 | 3274.674 | 9404.013 | < .0001 |
| Treatment (relative to internal fixation) | ||||
| THA | 13,112.799 | 11,754.191 | 14,471.408 | < .0001 |
| Hemiarthroplasty | 4551.68 | 3917.600 | 5185.636 | < .0001 |
| Time to procedure after admission | 10,387.969 | 8667.779 | 12,108.160 | < .0001 |
| Discharge disposition (relative to routine) | ||||
| Transfer to other hospital | 19,769.583 | 13,863.912 | 25,675.254 | < .0001 |
| Other transfer | 16,030.845 | 14,414.475 | 17,647.216 | < .0001 |
| Home healthcare | 4780.185 | 3213.279 | 6347.091 | < .0001 |
| Against Medical advice | 18,920.802 | 11,508.289 | 26,333.315 | < .0001 |
| Unknown | 46,291.044 | − 20,146.620 | 112,728.708 | 0.1721 |
| Comorbidities | ||||
| Diabetes mellitus | − 1459.965 | − 2235.945 | − 683.985 | 0.0002 |
| Heart disease | 4188.305 | 3433.418 | 4943.192 | < .0001 |
| Lung disease | 15,149.144 | 14,258.215 | 16,040.073 | < .0001 |
| Kidney disease | 9730.572 | 8769.190 | 10,691.955 | < .0001 |
| Liver disease | 6810.460 | 4215.930 | 9404.989 | < .0001 |
| Peripheral vascular disease | − 1542.662 | − 2794.878 | − 290.447 | 0.0158 |
| Hyperlipidemia | − 4024.687 | − 4607.579 | − 3441.794 | < .0001 |
| Hypertension | − 101.337 | − 742.134 | 539.460 | 0.7566 |
| Cancer | 3707.647 | 2113.767 | 5301.527 | < .0001 |
| Dementia | 1589.351 | 955.488 | 2223.213 | < .0001 |
| Cerebrovascular disease | 3116.060 | 1621.014 | 4611.105 | < .0001 |
| Alcohol abuse | 1281.596 | − 1810.083 | 4373.275 | 0.4165 |
| Tobacco use | − 3852.610 | − 7509.885 | − 195.336 | 0.0390 |
| Obesity | 4954.150 | 3194.214 | 6714.086 | < .0001 |
R2 = 0.1428
Male gender was observed to significantly increase total charge (p < 0.0001). When compared to white race, all races except Native American race (p = 0.2111) had significantly increased charges (p < 0.0001) with Hispanic race having the highest total charge. Compared to urban teaching hospitals, subjects treated in rural hospitals had a significantly lower total charges (p < 0.0001). Compared to Medicare, payment using Medicaid, private insurance, or self-pay had significantly higher total charges (p < 0.0001). Compared to internal fixation, both THA and hemiarthroplasty significantly increased total charge with THA having a larger effect (p < 0.0001). Lastly, when compared to routine discharge, transfer to other hospital, other transfer, and home healthcare led to increases in total charges (p < 0.0001).
Discussion
LOS is significantly increased in the lowest income quartile compared to the highest, and income quartile was demonstrated to be an independent contributor to LOS when controlling for all other variables. Contrarily, total charge did not increase proportionate to income quartile; rather, the charges were highest in the highest income group and lowest in the middle two quartiles. Additionally, income quartile was an independent contributor to total charge. Time to surgery after hospital admission differed significantly between quartiles and had a significant impact on both LOS and total charge. The data also showed that the prevalence of comorbidities in patients surgically treated for hip fracture is higher in the lowest income quartile and that the majority of the comorbidities contribute significantly to both LOS and cost. Gender, race, hospital location and teaching status, payer type, treatment, and discharge disposition all have varying degrees of impact on LOS and total charge.
Hospital LOS decreased from an average of 5.85 days in the highest quartile to 5.43 days in the lowest quartile. That difference of around 0.42 days is statistically significant. That difference might seem minute and perhaps not very clinically relevant. However, any reduction in LOS decreases the total cost to the healthcare system and allows proper utilization of hospital and human resources that are freed up by discharging a hip fracture patient earlier. In the setting of the COVID-19 pandemic, it has never been clearer how important proper utilization of hospital resources is. Additionally, decreasing LOS decreases the chances for contracting nosocomial infections such as hospital acquired pneumonia or urinary tract infection, thereby reducing the potential cost from those complications, as well as freeing up a bed and healthcare providers to care for another patient in need [20, 21].
As previously stated, income quartile was demonstrated to be an independent contributor to LOS. Similar to our findings, previous research has found that more financially deprived patients stayed longer in the hospital when controlling for other characteristics, as noted in two studies of 59,067 and 218,907 hip fracture patients in England [22, 23]. Contrarily, other studies of hip fracture patients in Nottingham and Denmark have found that income level does not have a significant impact on LOS but is associated with other important outcomes including mortality and readmission risk [8, 10]. A relationship between income level and LOS has been observed in other populations of orthopedic patients as well. A study done using NIS data from 2009 to 2011 that included 1,924,432 total knee arthroplasty patients also found that income quartile was an independent variable affecting LOS [24]. It is important to once again note that while LOS did significantly differ across quartiles, the difference between the lowest income quartile and the highest income quartile was less than 1 day. However, lower income groups not only stay longer, but they are also more likely to sustain a hip fracture in the first place, as was noted in our data and reported in several different populations [10, 25, 26].
Income quartile was observed to independently affect total hospital charge with more of a U-shaped relationship than that which was observed for LOS, in contrast to what was reported in the aforementioned study on hip fracture patients in England [22]. This seemingly paradoxical relationship between income quartile, LOS, and total charges may be in part due to the difference in treatment modalities received by each quartile. Quartile four, the highest earning quartile, had a significantly larger portion of its cohort undergo THA as hip fracture treatment, whereas the lower quartiles were more likely to undergo hemiarthroplasty compared to quartile four, while there was no difference in internal fixation between the groups. Looking at the data for THA compared to the other two treatment modalities in this study, the cost was significantly higher, and the LOS was significantly lower for all patients undergoing THA compared to all patients undergoing internal fixation or hemiarthroplasty. The increased cost of THA observed can be attributed to several factors, the most important one being higher implant costs compared to hemiarthroplasty and internal fixation [27]. Previous studies that have compared LOS in THA and hemiarthroplasty have found that LOS is similar between the two procedures, with some evidence leaning towards hemiarthroplasty having shorter LOS, potentially due to increased early ambulation in these patients [28]. Another important point about total hospital charge is that while quartile four had the highest charge, quartile one had the second highest charge. This is most likely driven by the increased LOS and prevalence of comorbidities in the lowest income quartile. This study demonstrates that the majority of comorbidities analyzed significantly increase cost, consistent with previous studies [22, 29, 30]. Another hypothesis for the increased charges seen with quartile one is that along with increased prevalence of comorbidities, patients in this quartile may also have more severe comorbid disease than in the other three quartiles, requiring more intensive treatment in the perioperative period. However, this is solely a hypothesis as we were unable to obtain any measure of disease severity from the data available in the NIS. These along with a majority of the variables analyzed having influence on both LOS and total charge significantly add to the complexity of this analysis.
Time to surgery was another variable examined in this study. In our analysis, we saw that time to procedure following admission significantly differed between lower and higher income quartiles. We also see that time to procedure is significantly correlated with both LOS and total charge. While a previous study found that early surgery, defined as surgery on the day of or day after admission, had minimal impact on both LOS and total charge, other studies have shown that time to surgery has a significant impact on LOS in hip fracture patients [22, 31]. However, the exact timing of surgery after admission for optimal outcomes is still not clearly defined. Two recent studies have found that surgery within 24 h of admission results in improved outcomes, including decreased LOS and lower medical costs, in hip fracture patients [32, 33]. Other literature has looked at time to surgery following hip fracture and found that surgery within 48 h of admission is associated with decreased rates of complications and mortality [34, 35]. However, there does seem to be a point of diminishing returns with respect to globally improved outcomes with earlier surgery. The HIP ATTACK international randomized controlled trial found that while surgery within 6 h did decrease time to hospital discharge from randomization, it did not improve mortality or risk of major complications compared to standard care [36]. Further research is required in order to define the optimal time window for hip fracture surgery once a patient is admitted to the hospital. The data from this study showed that lower income groups have increased time to surgery, and this is a likely important factor affecting LOS and total charge.
Male gender was associated with increased LOS and total charge in our analysis. This is consistent with the findings of other previously published literature on LOS following hip fracture [22, 37], though there is evidence that this may not be generalizable to all orthopedic patients [38]. While it appears there is a relationship between male gender and our variables of interest, it is worth mentioning that these fractures are much more common in women as a large proportion of hip fractures are related to osteoporosis. In fact, it is estimated that approximately one-third of women that live to age 80 will sustain a hip fracture, while approximately 17% of men living to age 80 will sustain this injury. Hip fractures in men do appear to confer more mortality risk as approximately one-third of men with hip fracture die within 1 year of sustaining the fracture [2]. Males sustaining hip fractures tend to be younger and less healthy than their largely osteoporotic female counterparts, contributing to the outcome differences between genders [39].
Looking at race, we found that compared to white race; black race, Hispanic race, and Asian/Pacific Islander race are all associated with increased LOS and total charge. This in large part is consistent with the published literature [24, 40]. Contrarily, one study found that white race was associated with increased LOS, but no significant effect on total charge [22]. One possible contributing factor is that the latter study was performed using a sample from England, whereas this study and the two cited studies with similar findings were using database samples from the USA.
There were also interesting differences between the different hospital types examined. Our analysis suggests that being treated for hip fracture at urban teaching hospitals is associated with longer LOS compared to urban non-teaching and rural hospitals. Previous literature has shown mixed relationships between hospital location and teaching status and LOS [24, 41, 42]. When examining total charge differences between hospital types, we found that rural hospitals were associated with decreased costs, while urban non-teaching hospitals were non-significantly associated with increased costs compared to urban teaching hospitals. This is another variable that contributes to our unexpected relationship between income quartile, LOS, and total charge, as a significantly higher proportion of the lowest income quartile was treated in rural hospitals when compared to the highest quartile, leading to increased costs in the highest earning quartile relative to the lowest earning quartile.
As expected with an injury primarily occurring in the elderly population, the vast majority of all patients had Medicare as their payer type. We found in our data that all other payer types are associated with increased LOS and total charge, with Medicaid increasing both variables to the greatest degree. Several studies in hip fracture patients as well as other orthopedic populations have found this association as well [7, 24, 43]. This is an important association as the percentage of patients on Medicaid in the lowest income quartile is more than double the percentage of the highest quartile. With regard to discharge disposition, routine discharge was associated with decreased LOS and costs when compared to discharge to skilled nursing facility, intermediate care facility, inpatient rehabilitation facility, or home healthcare, which is consistent with findings in hip fracture patients and other orthopedic populations as well [22, 24, 44]. We see in the data from Table 1 that a higher proportion of the lowest income quartile was discharged to home compared to the other three quartiles, especially the highest earning quartile. This likely has a significant effect on the LOS difference observed being relatively small at less than 1 day between quartile four and quartile one, though the difference is still statistically significant.
One of the major strengths of this study is the large sample size and nationally representative data. There are also limitations to this study. Similar to other database studies, data from the NIS database was collected from ICD-10 coding, and underreporting or inaccurate modifier coding may have occurred and may have introduced some degree of reporting error. National databases have also been shown to report significantly different prevalence of some comorbidities, such as obesity, which could potentially diminish the effect of these specific comorbidities on our variables of interest [45]. However, it is possible that these variables are uniformly underreported across all four income quartiles. The ideal way to characterize patient income levels would be to collect this information on an individual patient basis, but since individual patient incomes were not available, median income by zip code was used to generalize the income quartiles. This may lead to some misrepresentation of patients’ income levels; however, with the large number of subjects included, this effect is likely minimal.
Conclusion
Income quartile was demonstrated to be an independent contributor to both LOS and total charge, suggesting that socioeconomic factors continue to have an effect within the US healthcare system. Differences also exist between income quartiles and race, hospital type at which they are treated, payer type, treatment received, discharge disposition, and presence of comorbidities; all of which have varying degrees of effects on LOS and total hospital charge. This study suggests that the summation of these effects leads to small but significant differences between income quartiles on in-hospital outcomes following hip fracture.. Future studies are required to identify steps that can be taken to help reduce and hopefully eventually eliminate these differences in outcomes.
Supplementary Information
Below is the link to the electronic supplementary material.
Data availability
National Inpatient Sample data from the Healthcare Cost and Utilization Project published by the Agency for Healthcare Research and Quality is available from https://www.hcup-us.ahrq.gov/tech_assist/centdist.jsp.
Code availability
Not applicable.
Declarations
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bhandari M, Swiontkowski M. Management of acute hip fracture. N Engl J Med. 2017;377:2053–2062. doi: 10.1056/NEJMcp1611090. [DOI] [PubMed] [Google Scholar]
- 2.Veronese N, Maggi S. Epidemiology and social costs of hip fracture. Injury. 2018;49:1458–1460. doi: 10.1016/j.injury.2018.04.015. [DOI] [PubMed] [Google Scholar]
- 3.Wright NC, Saag KG, Curtis JR, Smith WK, Kilgore ML, Morrisey MA, Yun H, Zhang J, Delzell ES. Recent trends in hip fracture rates by race/ethnicity among older US adults. J Bone Miner Res. 2012;27:2325–2332. doi: 10.1002/jbmr.1684. [DOI] [PubMed] [Google Scholar]
- 4.Cooper C, Campion G, Melton LJ., 3rd Hip fractures in the elderly: a world-wide projection. Osteoporos Int. 1992;2:285–289. doi: 10.1007/BF01623184. [DOI] [PubMed] [Google Scholar]
- 5.Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporos Int. 1997;7:407–413. doi: 10.1007/PL00004148. [DOI] [PubMed] [Google Scholar]
- 6.Benetou V, Orfanos P, Feskanich D, et al. Education, marital status, and risk of hip fractures in older men and women: the CHANCES project. Osteoporos Int. 2015;26:1733–1746. doi: 10.1007/s00198-015-3054-9. [DOI] [PubMed] [Google Scholar]
- 7.Dy CJ, Lane JM, Pan TJ, Parks ML, Lyman S. Racial and socioeconomic disparities in hip fracture care. J Bone Joint Surg Am. 2016;98:858–865. doi: 10.2106/JBJS.15.00676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kristensen PK, Thillemann TM, Pedersen AB, Søballe K, Johnsen SP. Socioeconomic inequality in clinical outcome among hip fracture patients: a nationwide cohort study. Osteoporos Int. 2017;28:1233–1243. doi: 10.1007/s00198-016-3853-7. [DOI] [PubMed] [Google Scholar]
- 9.Omsland TK, Eisman JA, Naess Ø, et al. Educational inequalities in post-hip fracture mortality: a NOREPOS study. J Bone Miner Res. 2015;30:2221–2228. doi: 10.1002/jbmr.2579. [DOI] [PubMed] [Google Scholar]
- 10.Quah C, Boulton C, Moran C. The influence of socioeconomic status on the incidence, outcome and mortality of fractures of the hip. J Bone Joint Surg Br. 2011;93:801–805. doi: 10.1302/0301-620X.93B6.24936. [DOI] [PubMed] [Google Scholar]
- 11.Reyes C, García-Gil M, Elorza JM, et al. Socioeconomic status and its association with the risk of developing hip fractures: a region-wide ecological study. Bone. 2015;73:127–131. doi: 10.1016/j.bone.2014.12.019. [DOI] [PubMed] [Google Scholar]
- 12.Somersalo A, Paloneva J, Kautiainen H, Lönnroos E, Heinänen M, Kiviranta I. Incidence of fractures requiring inpatient care. Acta Orthop. 2014;85:525–530. doi: 10.3109/17453674.2014.908340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weycker D, Li X, Barron R, Bornheimer R, Chandler D. Hospitalizations for osteoporosis-related fractures: economic costs and clinical outcomes. Bone Rep. 2016;5:186–191. doi: 10.1016/j.bonr.2016.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lingsma HF, Bottle A, Middleton S, Kievit J, Steyerberg EW, Marang-van de Mheen PJ. Evaluation of hospital outcomes: the relation between length-of-stay, readmission, and mortality in a large international administrative database. BMC Health Serv Res. 2018;18:116. doi: 10.1186/s12913-018-2916-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lawrence TM, White CT, Wenn R, Moran CG (2005) The current hospital costs of treating hip fractures. Injury 36:88–91; discussion 92 [DOI] [PubMed]
- 16.Arora V, Moriates C, Shah N. The challenge of understanding health care costs and charges. AMA J Ethics. 2015;17:1046–1052. doi: 10.1001/journalofethics.2015.17.11.stas1-1511. [DOI] [PubMed] [Google Scholar]
- 17.Yoo J, Lee JS, Kim S, Kim BS, Choi H, Song DY, Kim WB, Won CW. Length of hospital stay after hip fracture surgery and 1-year mortality. Osteoporos Int. 2019;30:145–153. doi: 10.1007/s00198-018-4747-7. [DOI] [PubMed] [Google Scholar]
- 18.Aletto C, Aicale R, Pezzuti G, Bruno F, Maffulli N. Impact of an orthogeriatrician on length of stay of elderly patient with hip fracture. Osteoporos Int. 2020;31:2161–2166. doi: 10.1007/s00198-020-05510-0. [DOI] [PubMed] [Google Scholar]
- 19.(2021) HCUP NIS Database Documentation. Agency for Healthcare Research and Quality. https://www.hcup-us.ahrq.gov/db/nation/nis/nisdbdocumentation.jsp. Accessed 19 July 2021
- 20.Arefian H, Hagel S, Fischer D, Scherag A, Brunkhorst FM, Maschmann J, Hartmann M (2019) Estimating extra length of stay due to healthcare-associated infections before and after implementation of a hospital-wide infection control program. PLoS One 14:e0217159 [DOI] [PMC free article] [PubMed]
- 21.Jia H, Li L, Li W, et al. Impact of healthcare-associated infections on length of stay: a study in 68 hospitals in China. Biomed Res Int. 2019;2019:2590563. doi: 10.1155/2019/2590563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Castelli A, Daidone S, Jacobs R, Kasteridis P, Street AD. The determinants of costs and length of stay for hip fracture patients. PLoS One. 2015;10:e0133545. doi: 10.1371/journal.pone.0133545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Patel R, Bhimjiyani A, Ben-Shlomo Y, Gregson CL. Social deprivation predicts adverse health outcomes after hospital admission with hip fracture in England. Osteoporos Int. 2021;32:1129–1141. doi: 10.1007/s00198-020-05768-4. [DOI] [PubMed] [Google Scholar]
- 24.El Bitar YF, Illingworth KD, Scaife SL, Horberg JV, Saleh KJ. Hospital length of stay following primary total knee arthroplasty: data from the nationwide inpatient sample database. J Arthroplasty. 2015;30:1710–1715. doi: 10.1016/j.arth.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 25.Guilley E, Herrmann F, Rapin CH, Hoffmeyer P, Rizzoli R, Chevalley T. Socioeconomic and living conditions are determinants of hip fracture incidence and age occurrence among community-dwelling elderly. Osteoporos Int. 2011;22:647–653. doi: 10.1007/s00198-010-1287-1. [DOI] [PubMed] [Google Scholar]
- 26.Hansen L, Judge A, Javaid MK, Cooper C, Vestergaard P, Abrahamsen B, Harvey NC. Social inequality and fractures-secular trends in the Danish population: a case-control study. Osteoporos Int. 2018;29:2243–2250. doi: 10.1007/s00198-018-4603-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Axelrod D, Tarride J, Ekhtiari S, Blackhouse G, Johal H, Bzovsky S, Schemitsch EH, Heels-Ansdell D, Bhandari M, Sprague S. Is total hip arthroplasty a cost-effective option for management of displaced femoral neck fractures? A trial-based analysis of the HEALTH study. J Orthop Trauma. 2020;34(Suppl 3):S37–s41. doi: 10.1097/BOT.0000000000001932. [DOI] [PubMed] [Google Scholar]
- 28.Tang X, Wang D, Liu Y, Chen J, Zhou Z, Li P, Ning N. The comparison between total hip arthroplasty and hemiarthroplasty in patients with femoral neck fractures: a systematic review and meta-analysis based on 25 randomized controlled trials. J Orthop Surg Res. 2020;15:596. doi: 10.1186/s13018-020-02122-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nikkel LE, Fox EJ, Black KP, Davis C, Andersen L, Hollenbeak CS. Impact of comorbidities on hospitalization costs following hip fracture. J Bone Joint Surg Am. 2012;94:9–17. doi: 10.2106/JBJS.J.01077. [DOI] [PubMed] [Google Scholar]
- 30.Cuesta-Peredo D, Arteaga-Moreno F, Belenguer-Varea Á, Llopis-Calatayud JE, Sivera-Gimeno S, Santaeugenia SJ, Avellana-Zaragoza JA, Tarazona-Santabalbina FJ. Influence of hospital adverse events and previous diagnoses on hospital care cost of patients with hip fracture. Arch Osteoporos. 2019;14:88. doi: 10.1007/s11657-019-0638-6. [DOI] [PubMed] [Google Scholar]
- 31.Mitchell SM, Chung AS, Walker JB, Hustedt JW, Russell GV, Jones CB. Delay in hip fracture surgery prolongs postoperative hospital length of stay but does not adversely affect outcomes at 30 days. J Orthop Trauma. 2018;32:629–633. doi: 10.1097/BOT.0000000000001306. [DOI] [PubMed] [Google Scholar]
- 32.Pablos-Hernández C, González-Ramírez A, da Casa C, Luis MM, García-Iglesias MA, Julián-Enriquez JM, Rodríguez-Sánchez E, Blanco JF. Time to surgery reduction in hip fracture patients on an integrated orthogeriatric unit: a comparative study of three healthcare models. Orthop Surg. 2020;12:457–462. doi: 10.1111/os.12633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pincus D, Wasserstein D, Ravi B, Huang A, Paterson JM, Jenkinson RJ, Kreder HJ, Nathens AB, Wodchis WP. Medical costs of delayed hip fracture surgery. J Bone Joint Surg Am. 2018;100:1387–1396. doi: 10.2106/JBJS.17.01147. [DOI] [PubMed] [Google Scholar]
- 34.Alvi HM, Thompson RM, Krishnan V, Kwasny MJ, Beal MD, Manning DW (2018) Time-to-surgery for definitive fixation of hip fractures: a look at outcomes based upon delay. Am J Orthop (Belle Mead NJ) 47: [DOI] [PubMed]
- 35.Simunovic N, Devereaux PJ, Sprague S, Guyatt GH, Schemitsch E, Debeer J, Bhandari M. Effect of early surgery after hip fracture on mortality and complications: systematic review and meta-analysis. CMAJ. 2010;182:1609–1616. doi: 10.1503/cmaj.092220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.(2020) Accelerated surgery versus standard care in hip fracture (HIP ATTACK): an international, randomised, controlled trial. Lancet 395:698–708 [DOI] [PubMed]
- 37.Knoll OM, Lakomkin N, Shen MS, Adebayo M, Kothari P, Dodd AC, Attum B, Lee N, Chona D, Sethi MK. A predictive model for increased hospital length of stay following geriatric hip fracture. J Clin Orthop Trauma. 2019;10:S84–s87. doi: 10.1016/j.jcot.2019.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dunn JC, Lanzi J, Kusnezov N, Bader J, Waterman BR, Belmont PJ., Jr Predictors of length of stay after elective total shoulder arthroplasty in the United States. J Shoulder Elbow Surg. 2015;24:754–759. doi: 10.1016/j.jse.2014.11.042. [DOI] [PubMed] [Google Scholar]
- 39.Sterling RS. Gender and race/ethnicity differences in hip fracture incidence, morbidity, mortality, and function. Clin Orthop Relat Res. 2011;469:1913–1918. doi: 10.1007/s11999-010-1736-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gholson JJ, Noiseux NO, Otero JE, Gao Y, Shah AS. Patient factors systematically influence hospital length of stay in common orthopaedic procedures. Iowa Orthop J. 2017;37:233–237. [PMC free article] [PubMed] [Google Scholar]
- 41.Akhras A, Wahood W, Alvi MA, Yolcu YU, Elder BD, Bydon M. Does hospital teaching status affect the outcomes of patients undergoing anterior cervical discectomy and fusion? World Neurosurg. 2020;144:e395–e404. doi: 10.1016/j.wneu.2020.08.164. [DOI] [PubMed] [Google Scholar]
- 42.Paterson JM, Williams JI, Kreder HJ, Mahomed NN, Gunraj N, Wang X, Laupacis A. Provider volumes and early outcomes of primary total joint replacement in Ontario. Can J Surg. 2010;53:175–183. [PMC free article] [PubMed] [Google Scholar]
- 43.Maman SR, Andreae MH, Gaber-Baylis LK, Turnbull ZA, White RS. Medicaid insurance status predicts postoperative mortality after total knee arthroplasty in state inpatient databases. J Comp Eff Res. 2019;8:1213–1228. doi: 10.2217/cer-2019-0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Berman JE, Mata-Fink A, Kassam HF, Blaine TA, Kovacevic D. Predictors of length of stay and discharge disposition after shoulder arthroplasty: a systematic review. J Am Acad Orthop Surg. 2019;27:e696–e701. doi: 10.5435/JAAOS-D-18-00244. [DOI] [PubMed] [Google Scholar]
- 45.Bohl DD, Basques BA, Golinvaux NS, Baumgaertner MR, Grauer JN. Nationwide inpatient sample and national surgical quality improvement program give different results in hip fracture studies. Clin Orthop Relat Res. 2014;472:1672–1680. doi: 10.1007/s11999-014-3559-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
National Inpatient Sample data from the Healthcare Cost and Utilization Project published by the Agency for Healthcare Research and Quality is available from https://www.hcup-us.ahrq.gov/tech_assist/centdist.jsp.
Not applicable.


