Abstract
Purpose of Review
The purpose of this review is to review recent literature focusing on proximal humerus anatomy, epidemiology of these fractures, diagnosis and treatment options, and clinical outcomes.
Recent Findings
Non- or minimally displaced proximal humerus fractures treated nonoperatively do not lead to short- or long-term complication and do not cross over to operative treatment. There is a higher rate of operative management with older age, increased injury severity score, treatment at an adult hospital, and private insurance. Operative management is preferred with closed or open reduction and percutaneous pinning, but elastic nailing and plate fixation are other options with good postoperative outcomes.
Summary
Pediatric proximal humerus fractures occur after fall onto the affected shoulder or arm. Diagnosis is usually made with radiographs. Understanding the proximal humerus anatomy is critical to the proper management of these injuries to aid reduction and predict remodeling potential. There is considerable debate around the management of proximal humerus fractures in the pediatric population. Treatment is based on patient age, fracture displacement, and remodeling capacity. Nonoperative management is successful in younger patients or less displaced fractures, and operative management is usually considered in older patients with more displaced fractures.
Keywords: Pediatric proximal humerus fractures, Pediatric trauma, Proximal humerus fracture treatment, Shoulder injury, Pediatric fractures
Introduction
Proximal humerus fractures comprise approximately 0.45 to 2% of all fractures and about 14% of upper extremity fractures in the pediatric population [1, 2]. There have been several recent studies focusing on the diagnosis and management of this injury, and it is important to understand issues for providers that manage these injuries in children. The purpose of this review is to review recent literature focusing on proximal humerus anatomy, epidemiology of these fractures, diagnosis and treatment options, and clinical outcomes.
Anatomy
Prior to discussing fractures of the proximal humerus, it is important to understand the anatomy and vascularity of the proximal humerus. The proximal humerus is an integral part of the shoulder girdle and allows for motion in multiple planes. It serves as the site of insertion for several important muscles including the deltoid, pectoralis major, latissimus dorsi, and rotator cuff muscles. These muscles act as deforming forces in the setting of a fracture. Specifically, the pectoralis major inserts into the lateral lip of the bicipital groove and displaces the humerus shaft medially and anteriorly. The fracture fragment involving the greater tuberosity is externally rotated due to the pull of the supraspinatus, infraspinatus, and teres minor (Fig. 1). Vascularity of the proximal humerus is derived from the terminal branches of the axillary artery. A study in adult cadavers demonstrated that the anterior and posterior humeral circumflex arteries are the primary blood supply of the proximal humerus, with the posterior humeral circumflex artery providing 64% of the blood supply to the humeral head while the anterior circumflex artery supplies 36%. These anatomic considerations, deformity forces, and vascularity are integral in fracture reduction, fixation, and healing [3].
Fig. 1.

Deforming forces of the proximal humerus. a The supraspinatus, infraspinatus, and teres minor insert into the greater tuberosity and externally rotate the fragment. b The subscapularis displaces the lesser tuberosity of the medially. c The deltoid abducts the humeral shaft. d The pectoralis major inserts into the lateral lip of the bicipital groove and displaces the humerus shaft medially and anteriorly
Other anatomic considerations are important in fracture reduction and fixation in pediatric patients. Closed reduction of displaced proximal humerus fractures can be complicated by interposing tissue such as the biceps tendon. The biceps tendon is located intraarticularly in the glenohumeral joint, making it both vulnerable to injury during proximal humerus fracture and at risk for soft tissue entrapment during repair. The biceps tendon is the most common soft tissue interposed in the fracture space in failed closed reductions of the proximal humerus. Other impediments to closed reduction within the fracture site include the thick periosteum in children, deltoid muscle, joint capsule, and bony comminution [4–6]. These soft tissues and other structures can block closed reduction of the proximal humerus and are indications for open reduction in highly displaced fractures after failed attempts at closed reduction.
Understanding physeal anatomy is important in pediatric patients as well. The proximal humeral physis accounts for approximately 80% of the longitudinal growth of the humerus and begins to close starting centrally around age 14 in females and 16 in males and ends around 17 to 18 years of age [7]. At birth, the humeral head is largely cartilaginous, but within a few months, ossification centers begin to develop. The humeral head ossification center arises at the medial humeral head around 2–4 months followed by the greater tuberosity at 7–10 months [8]. Fusion of the ossification centers begins at age 3 and is complete by late puberty with the lesser tuberosity being the last to fuse [8–10] These ossification centers can elucidate the bony maturity of patients, but more importantly, they allow for significant remodeling after fractures especially in younger children [8].
Epidemiology and Classification
Pediatric proximal humerus fractures have an annual incidence of approximately 31.4/100,000 [2, 11•]. Approximately 40% of metaphyseal proximal humerus fractures are non- or minimally displaced and more commonly require operative treatment as compared to epiphyseal fractures which are non- or minimally displaced in 85% of cases [12, 13]. There is a bimodal distribution of incidence, peaking between ages of 10–14 and again at 80–84 years [14]. Boys are 3–4 times more likely to sustain this injury, although reports have varied across studies [10, 15•]. Proximal humerus fractures at birth are rare at 10.1/100,000 births [16]. These fractures in children under 18 months may require careful consideration for non-accidental trauma [17, 18].
Proximal humerus fractures most often occur upon falling backwards onto an outstretched hand with an extended elbow and externally rotated shoulder or through direct traumatic impact to the shoulder. Approximately 25% of proximal humerus fractures in children resulting from traumatic falls are related to sports, and another 33% are due to motor vehicle accidents [12]. Fractures resulting from proximal humeral overuse have also been described in children participating in sports. “Little leaguer’s shoulder” is one of the more extensively described types of such an injury. Radiologic findings include widening of the physis with calcification or lateral fragmentation on the side of the throwing arm [19]. Trauma during the birthing process as well as non-accidental trauma, may also lead to fractures of the proximal humerus, particularly in very young patients.
Pathologic fractures caused by conditions such as bone cysts and other lesions are another key cause of fracture at the proximal humerus in pediatric patients. These injuries may result from low energy mechanisms. Unicameral bone cysts are benign, fluid-filled lesions lined with fibrous tissue along the metaphysis of long bones most commonly in children and adolescents. These lesions are most common in the femur and proximal humerus and may expand and weaken the impacted bone, leading to pathologic fractures in about 75% of cases [20, 21]. Interestingly, unicameral bone cysts heal spontaneously following proximal humerus pathologic fracture and result in excellent clinical outcomes, though the rate of healing is lower in adolescent patients and patients with active lesions [21]. Other lesions such as nonossifying fibromas, aneurysmal bone cysts, osteosarcomas, and fibrous dysplasia can also lead to pathologic fractures of the proximal humerus [22].
The Neer-Horowitz system is the most widely used classification system for proximal humerus fractures in children and is graded by severity of displacement (Table 1) [23]. Grade I fractures have no displacement, grade II fractures have displacement no greater than one-third of shaft width, grade III fractures have displacement greater than one-third but no greater than two-thirds of shaft width, and grade IV fractures have displacement greater than two-thirds of shaft width. Another classification commonly used in pediatrics is the Salter-Harris classification. However, this classification is applicable to physeal fractures, and often, pediatric proximal humerus fractures are metaphyseal.
Table 1.
Neer-Horowitz classification of proximal humerus fractures [23]
| Grade | Displacement |
|---|---|
| I | <5 mm |
| II | <1/3 of shaft width |
| III | 1/3–2/3 of shaft width |
| IV | >2/3 of shaft width |
Diagnosis
History and physical examination is critical diagnosing a proximal humerus fracture and must be catered to the patient age. Generally, a detailed history will help to localize the affected anatomic area and diagnostic possibilities. In neonates, a history of forced obstetric maneuvers, high gestational weight, and breech presentation are risk factors for upper extremity fractures during birth [24, 25]. In contrast, children and adolescents more classically present with trauma such as fall onto an outstretched arm. On examination, there may be swelling, tenderness, visible deformity, and unwillingness to move the shoulder by holding the arm close to the body [26, 27]. The overlying soft tissues should be inspected if concern for an open fracture. Associated injuries to the brachial plexus, clavicle, and scapula should not be missed. A thorough evaluation of the distal motor function, distal perfusion, and sensory function including of the axillary nerve must be performed. High energy injuries resulting in fracture-dislocation can cause injury to the axillary nerve or artery [28]. However, the overall incidence of neurovascular injury with proximal humerus fractures is extremely low and usually occurs in elderly patients who have lost elasticity to the vessel wall [29, 30].
The diagnosis of these fractures is usually made using radiography. Standard radiographs of the shoulder including AP, scapula Y, and axillary views are generally sufficient to characterize the fracture morphology. An axillary view is critical to rule out dislocation and evaluate the true angulation of the fracture. However, this view can be very difficult to obtain as it requires abducting the injured arm. Options in this case include giving adequate pain medication or sedation to obtain the radiograph or instead obtaining a Velpeau view, in which the patient’s arm may remain in a sling.
In general, indications for a CT scan for proximal humerus fractures in children are limited due to the risk of ionizing radiation on the developing body. In cases with difficulty obtaining orthogonal radiography or a complex fracture pattern or dislocation, CT may be indicated for classification and surgical planning. In the adult literature, CT has greater reliability than radiographs in classifying fractures, but there is still debate as to whether obtaining a CT scan affects management decisions [31, 32]. When radiographs are indeterminate, CT scans can provide clinically useful information in complex fractures or fracture-dislocations [33, 34]. If there is a suspected pathological fracture that is unclear on radiographs, MRI is the imaging modality of choice [35].
Ultrasonography is an accessible and inexpensive imaging modality for the diagnosis of proximal humerus fractures in neonates. Advantages of ultrasound are it may show greater details of the deformity compared to x-ray without exposure to radiation [36]. The sensitivity of ultrasound is 94% and the specificity 100% for diagnosis of proximal humerus fractures in children [37]. The main disadvantage is that many orthopedic surgeons do not interpret ultrasonography as readily as radiography, and its clinical utility is unclear at this time.
Management
The majority of proximal humerus fractures in children can be treated successfully with nonoperative management due to the immense remodeling potential of the physis (Fig. 2). Moreover, the majority (85%) of proximal humerus fractures are non- or minimally displaced [15•]. Indications for nonoperative management are still debated based on age and fracture morphology. Until age 12, correction of up to 60 degrees in the coronal and sagittal plane is possible and up to 40 degrees in children older than 12 years [1]. Hohloch et al. introduced an evidence-based treatment algorithm for the management of pediatric proximal humerus fracture. Based on meta-analysis, non- or minimally displaced fractures with an angulation less than 20° or Neer-Horowitz grade I/II can be successfully treated nonoperatively with immobilization in a sling and swathe independent of patient age. Once the decision is made for nonoperative management at the initial visit, further fracture displacement reversing management to surgery occurs in less than 1% of cases [1, 38, 39]. In neonates, the treatment is almost always nonoperative due to the immense remodeling power of the growth plate. Treatment with gentle swaddling is effective in this age group without long-term deformity [24, 27]. In older children, immobilization can be obtained with slings, shoulder immobilizers, hanging arm casts, shoulder spica casts, and sling and swathes for a period of 3 to 4 weeks. The authors prefer the use of slings or shoulder immobilizers for minimally displaced injuries and hanging arm casts for further displaced injuries. A shoulder spica is rarely needed and may add additional burden to the caregiver.
Fig. 2.
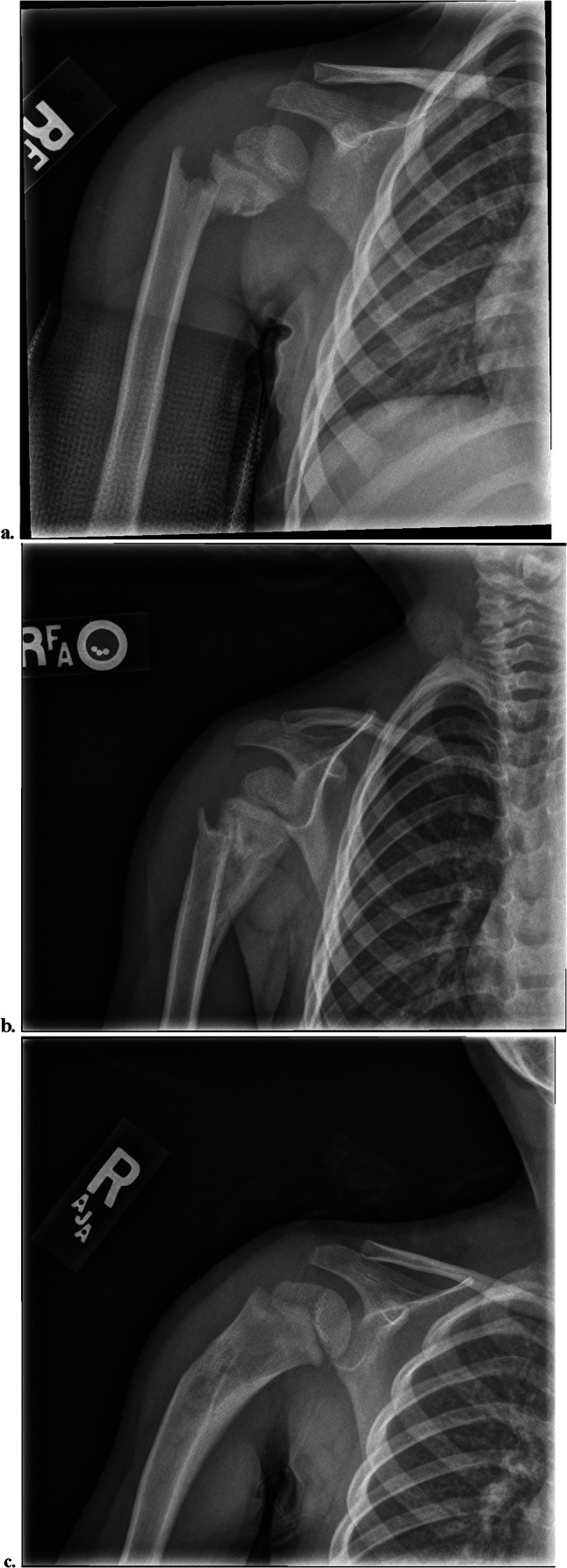
Nonoperative management of proximal humerus fractures. a This is a 3 year-old girl who was struck by a car and sustained a Neer-Horowitz IV proximal humerus fracture which was treated nonoperatively with a hanging arm cast. b Radiographs 2 months following injury demonstrate signs of callus formation and progressive bony remodeling. c Six months after initial injury, the alignment of the proximal humerus has improved with progressive bony remodeling
While it is generally agreed that nonoperative management is preferred whenever possible, there is no consensus on the criteria for operative versus nonoperative treatment of proximal humerus fractures in children, and there has been an increase in use surgical fixation in the past several years [11•]. The individual patient’s skeletal maturity and severity of injury must be considered together in developing a treatment plan. Operative treatment should be considered in Neer-Horowitz grade III and IV fractures and greater fracture angulation in older children. The exact radiographic parameters indicating operative treatment are still debated (Table 2) [1, 10, 12, 15•, 40–42]. Nonoperative treatment of displaced fractures in older patients is associated with increasing discrepancies in arm length and residual angulation [25]. However, there are no randomized controlled trials comparing the outcomes of operative versus nonoperative treatment for displaced fractures. Factors increasing likelihood of operative management are older age, male sex, non-Medicaid payer status, increased injury severity score, and admission to an adult hospital [11•, 15•]. The rate of operative management for pediatric proximal humerus fractures is 43.2% across children’s and adult hospitals compared to 11.9% at children’s hospitals [15, 43]. Neuromuscular disorders or nerve palsies which may unpredictably impact muscular forces may also be indications for operative fixation [10].
Table 2.
Indication for operative management
| Beaty 1992 [40] |
100% translation or >70° angulation, under 5 years >50% translation or angulation <70° in younger and >40° in older children, age 5–10 years Translation >50% or angulation >40°, patients >11 years |
| Binder et al. 2016 [1] |
>60° angulation in children up to 12 years >30° angulation in children older than 12 years |
| Cruz et al. 2018 [15•] |
Neer-Horowitz grade II and IV >60° angulation in patients under 10 years >30° angulation in patients 10 and older |
| Dobbs et al. 2003 [41] |
>75° angulation in children 7 and under >60° angulation in children 8 to 11 years >45° angulation in children 12 and older |
| Lefèvre et al. 2014 [12] |
>100% translation and/or angulation >70°, patients <10 years >50% translation and/or angulation >40°, patients aged 10–13 years >30% translation and/or angulation >20°, patients >13 years |
| Pahlavan et al. 2011 [42] |
Nonoperative, <10 years Case-by-case basis, age 10–13 Displaced fracture, age >13 years |
| Popkin et al. 2015 [10] | Neer-Horowitz grade III and IV fractures in children older than 11 years |
While the majority of fractures can be closed reduced, approximately 10% of operatively managed patients required an open reduction due to interposition of the long biceps tendon, periosteum, capsule, or deltoid [1, 5, 42]. Failure of closed reduction should be addressed with open reduction and subsequent assessment of trapped structures. Open reduction is typically performed via a deltopectoral approach. Both closed and open approaches require mindful avoidance of injury to the axillary artery or nerve. Fixation options include percutaneous pinning, intramedullary nails, cannulated screws, and plates. Percutaneous pinning remains the most commonly used fixation strategy with the benefit of shorter surgical time and decreased estimated blood loss as compared to ESIN, though complication rates may be higher [12, 44]. Additionally, percutaneous pinning while leaving the pins exposed is a more cost-effective fixation strategy with an average cost saving of $4,502 per patient compared to intramedullary nailing, with the disadvantage of higher superficial infection rates from the exposed implant [45]. Closed reduction with percutaneous pinning is the most common method of fixation, but many studies have also shown excellent outcomes with elastic stable intramedullary nailing (ESIN) technique [6, 46, 47]. Preservation of the surrounding soft tissue is key for healing and plate fixation in children is rarely indicated [11•]. A relative stability construct such as intramedullary nailing allows for remodeling, but in older children with severe deformity, absolute stability with screw and plate fixation may be indicated.
Author’s Preferred Technique
The patient is positioned in the supine or modified beach chair position to allow for orthogonal imaging, and the entire extremity is draped. Closed reduction is achieved using a combination of traction, abduction, and internal or external rotation. If the fracture is unable to be reduced after multiple closed reduction attempts, an open reduction is performed via a deltopectoral approach. Blocks to reduction are addressed, and the fracture is reduced. Once the fracture is reduced, two 2.5 mm threaded Kirschner wires are used to fix the fracture, and the pins are further secured with pin-to-pin clamps (Fig. 3). The fracture is followed biweekly to assess healing, and the pins are removed at 4 weeks in the office or under conscious sedation (Fig. 4) [48•].
Fig. 3.
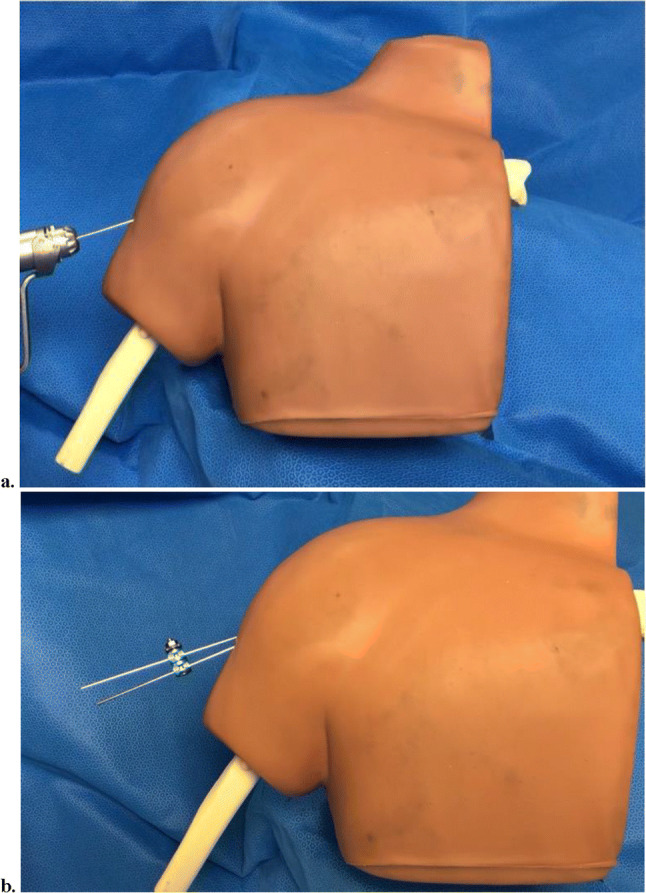
Preferred technique for operative management of proximal humerus fracture: a Two 2.5mm k-wires are placed for fixation after closed or open reduction. b The two k-wires are held with an ex-fix clamp for further stability
Fig. 4.

Operative management of proximal humerus fractures. a This is a 14-year-old boy who sustained a Neer-Horowitz III proximal humerus fracture while wrestling. X-ray shows fracture at the proximal physis with significant varus angulation of the humeral head with respect to the shaft. b The patient was treated with external fixation with two pins as described in the authors’ preferred techniques. c X-ray at 12 months shows healing and remodeling of humeral metaphysis with stable alignment following surgical fixation
Outcomes
Outcomes of proximal humerus fractures in children are generally excellent with both nonoperative and operative treatment. In neonates with nonoperative management, fracture union was noted within 2 weeks, and radiographs at 6 months demonstrate complete remodeling of the fractures [24]. In older children, 90% of surgical patients have excellent outcomes, and 96.9% of nonoperatively managed patients have excellent outcomes [1]. A systematic review of proximal humerus fractures in children demonstrated range of motion is better in nonoperatively treated patients, and 22% of operatively treated patients had pain at follow-up compared to 7% of nonoperatively treated patients [42]. Patients with Neer-Horowitz grade IV fractures had worse outcomes with greater pain, shortening, restriction of motion, and greater angulation compared to lower grade fractures regardless of treatment type [42].
Complications after proximal humerus fractures in children are rare. One study noted a complication rate of 9% with K-wire fixation, 7% with ESIN, and 8% with nonoperative treatment [25]. Potential complications of nonoperative treatment are malunion and stiffness, but malunions are well tolerated in the proximal humerus. In a study of 69 pediatric patients treated nonoperatively, 7.2% had limitations in range of motion, 4.3% had pain, and 1.4% had weakness, consistent with previously reported literature [42, 49•]. After operative treatment, the most common complication is superficial pin site infection followed by malunion [11•, 50]. Other very rare complications are axillary nerve or artery injury, avascular necrosis of the humeral head, hypertrophic scars after open reduction, or pin migration (more common with smooth pins). Careful dissection and minimal disruption of the soft tissues during the approach are recommended to avoid these complications.
Conclusion
Proximal humerus fractures in children commonly occur after a traumatic fall. An understanding of proximal humerus anatomy is critical to understanding fracture displacement and implications to fracture remodeling. Diagnosis of these injuries is made by history, physical exam, and radiographic assessment. In select cases, a CT scan may be helpful to assess fracture pattern or joint dislocation. Treatment is based on patient age, fracture displacement, and remodeling capacity. Nonoperative management is successful in younger patients or less displaced fractures, and operative management is usually considered in older patients with more displaced fractures. In general, most patients have good outcomes with operative and nonoperative management of proximal humerus fractures.
Declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
Arin E. Kim, Hannah Chi, and Ishaan Swarup declare that they have no conflict of interest.
Footnotes
This article is part of the Topical Collection on Pediatric Orthopedics
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Binder H, Tiefenboeck TM, Payr S, Schurz M, Aldrian S, Sarahrudi K. Treatment of proximal humerus fractures in children and young adolescents. Wiener klinische Wochenschrift. 2016;128:120–124. doi: 10.1007/s00508-015-0879-3. [DOI] [PubMed] [Google Scholar]
- 2.Landin LA. Epidemiology of children’s fractures. J Pediatr Orthop B. 1997;6:79–83. doi: 10.1097/01202412-199704000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Hettrich CM, Boraiah S, Dyke JP, Neviaser A, Helfet DL, Lorich DG. Quantitative assessment of the vascularity of the proximal part of the humerus. J Bone Joint Surg Am. 2010;92:943–948. doi: 10.2106/JBJS.H.01144. [DOI] [PubMed] [Google Scholar]
- 4.Pandya NK, Behrends D, Hosalkar HS. Open reduction of proximal humerus fractures in the adolescent population. J Child Orthop. 2012;6:111–118. doi: 10.1097/BPB.0b013e32833ce424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bahrs C, Zipplies S, Ochs BG, Rether J, Oehm J, Eingartner C, Rolauffs B, Weise K. Proximal humeral fractures in children and adolescents. J Pediatr Orthop. 2009;29:238–242. doi: 10.1097/BPO.0b013e31819bd9a7. [DOI] [PubMed] [Google Scholar]
- 6.King ECB, Ihnow SB. Which proximal humerus fractures should be pinned? Treatment in Skeletally Immature Patients. J Pediatr Orthop. 2016;36(Suppl 1):S44–S48. doi: 10.1097/BPO.0000000000000768. [DOI] [PubMed] [Google Scholar]
- 7.Pritchett JW. Growth plate activity in the upper extremity. Clin Orthop Relat Res. 1991;268:235–242. [PubMed] [Google Scholar]
- 8.Zember JS, Rosenberg ZS, Kwong S, Kothary SP, Bedoya MA. Normal skeletal maturation and imaging pitfalls in the pediatric shoulder. RadioGraphics. 2015;35:1108–1122. doi: 10.1148/rg.2015140254. [DOI] [PubMed] [Google Scholar]
- 9.Kwong S, Kothary S, Poncinelli LL. Skeletal development of the proximal humerus in the pediatric population: MRI features. Am J Roentgenology. 2014;202:418–425. doi: 10.2213/AJR.13.10711. [DOI] [PubMed] [Google Scholar]
- 10.Popkin C, Levine W, Ahmad C. Evaluation and management of pediatric proximal humerus fractures. J Am Acad Orthop Surg. 2015;23:77–86. doi: 10.5435/JAAOS-D-14-00033. [DOI] [PubMed] [Google Scholar]
- 11.Hannonen J, Hyvönen H, Korhonen L, Serlo W, Sinikumpu J-J. The incidence and treatment trends of pediatric proximal humerus fractures. BMC Musculoskelet Disord. 2019;20:571. doi: 10.1186/s12891-019-2948-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lefèvre Y, Journeau P, Angelliaume A, Bouty A, Dobremez E. Proximal humerus fractures in children and adolescents. Orthop Traumatol Surg Res. 2014;100(Suppl 1):S149–S156. doi: 10.1016/j.otsr.2013.06.010. [DOI] [PubMed] [Google Scholar]
- 13.Hinson JA. Anatomy and classification of proximal humerus fractures. In: Crosby LA, Neviaser RJ, editors. Proximal Humerus Fractures: Evaluation and Management. Cham: Springer International Publishing; 2015. pp. 1–22. [Google Scholar]
- 14.Kim SH, Szabo RM, Marder RA. Epidemiology of humerus fractures in the United States: nationwide emergency department sample, 2008. Arthritis Care Res. 2012;64:407–414. doi: 10.1002/acr.21563. [DOI] [PubMed] [Google Scholar]
- 15.Cruz AI, Jr, Kleiner JE, Gil JA, Goodman AD, Daniels AH, Eberson CP. Inpatient surgical treatment of paediatric proximal humerus fractures between 2000 and 2012. J Child Orthop. 2018;12:111–116. doi: 10.1302/1863-2548.12.170220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.von Heideken J, Thiblin I, Högberg U. The epidemiology of infant shaft fractures of femur or humerus by incidence, birth, accidents, and other causes. BMC Musculoskelet Disord. 2020;21:840. doi: 10.1186/s12891-020-03856-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pandya NK, Baldwin KD, Wolfgruber H, Drummond DS, Hosalkar HS. Humerus fractures in the pediatric population: an algorithm to identify abuse. J Pediatr Orthop B. 2010;19:535–541. doi: 10.1097/BPB.0b013e32833ce424. [DOI] [PubMed] [Google Scholar]
- 18.Shaw BA, Murphy KM, Shaw A, Oppenheim WL, Myracle MR. Humerus shaft fractures in young children: accident or abuse? J Pediatr Orthop. 1997;17:293–297. [PubMed] [Google Scholar]
- 19.Carson WG, Gasser SI. Little leaguer’s shoulder. Am J Sports Med. 1998;26:575–580. doi: 10.1177/03635465980260041901. [DOI] [PubMed] [Google Scholar]
- 20.Pretell-Mazzini J, Murphy RF, Kushare I, Dormans JP. Unicameral bone cysts: general characteristics and management controversies. J Am Acad Orthop Surg. 2014;22:295–303. doi: 10.5435/JAAOS-22-05-295. [DOI] [PubMed] [Google Scholar]
- 21.Kim M-C, Joo S-D, Jung S-T. The role of fractures on pathologic bone in healing of proximal humerus unicameral bone cysts. J Orthop Surg. 2018;26:2309499018778366. doi: 10.1177/2309499018778366. [DOI] [PubMed] [Google Scholar]
- 22.Ortiz EJ, Isler MH, Navia JE, Canosa R. Pathologic fractures in children. Clin Orthop Relat Res. 2005;432:116–126. doi: 10.1097/01.blo.0000155375.88317.6c. [DOI] [PubMed] [Google Scholar]
- 23.Neer CS, Horwitz BS. Fractures of the proximal humeral epiphysial plate. Clin Orthop Relat Res. 1965;41:24–31. doi: 10.1097/00003086-196500410-00003. [DOI] [PubMed] [Google Scholar]
- 24.Sherr-Lurie N, Bialik GM, Ganel A, Schindler A, Givon U. Fractures of the humerus in the neonatal period. Isr Med Assoc J. 2011;13:363–365. [PubMed] [Google Scholar]
- 25.Hohloch L, Eberbach H, Wagner FC, Strohm PC, Reising K, Südkamp NP, et al. Age- and severity-adjusted treatment of proximal humerus fractures in children and adolescents—a systematical review and meta-analysis. van Griensven M, editor. PLoS ONE. 2017;12:e0183157. doi: 10.1371/journal.pone.0183157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dias E. Bilateral humerus fracture following birth trauma. J Clin Neonatol. 2012;1:44–45. doi: 10.4103/2249-4847.92230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Basha A, Amarin Z, Abu-Hassan F. Birth-associated long-bone fractures. Int J Gynaecol Obstet. 2013;123:127–130. doi: 10.1016/j.ijgo.2013.05.013. [DOI] [PubMed] [Google Scholar]
- 28.Cotman SJ, Trinh TQ. Vincent S, backes jr. proximal humerus fracture-dislocation with laceration of the axillary artery: a case report. Iowa Orthop J. 2017;37:53–55. [PMC free article] [PubMed] [Google Scholar]
- 29.McLaughlin JA, Light R, Lustrin I. Axillary artery injury as a complication of proximal humerus fractures. J Shoulder Elbow Surg. 1998;7:292–294. doi: 10.1016/S1058-2746(98)90058-1. [DOI] [PubMed] [Google Scholar]
- 30.Peters RM, Menendez ME, Mellema JJ, Ring D, Smith RM. Axillary artery injury associated with proximal humerus fracture: a report of 6 cases. Arch Bone Jt Surg. 2017;5:52–57. [PMC free article] [PubMed] [Google Scholar]
- 31.Ramappa AJ, Patel V, Goswami K, Zurakowski D, Yablon C, Rodriguez EK, Appleton P, DeAngelis J. Using computed tomography to assess proximal humerus fractures. Am J Orthop. 2014;43:E43–E47. [PubMed] [Google Scholar]
- 32.Stoddart M, Pearce O, Smith J, McCann P, Sheridan B, Al-Hourani K. Proximal humerus fractures: reliability of Neer versus AO classification on plain radiographs and computed tomography. Cureus. 2020; 10.7759/cureus.8520. [DOI] [PMC free article] [PubMed]
- 33.Castagno AA, Shuman WP, Kilcoyne RF, Haynor DR, Morris ME, Matsen FA. Complex fractures of the proximal humerus: role of CT in treatment. Radiology. 1987;165:759–762. doi: 10.1148/radiology.165.3.3685356. [DOI] [PubMed] [Google Scholar]
- 34.Bahrs C, Rolauffs B, Südkamp NP, Schmal H, Eingartner C, Dietz K, Pereira PL, Weise K, Lingenfelter E, Helwig P. Indications for computed tomography (CT-) diagnostics in proximal humeral fractures: a comparative study of plain radiography and computed tomography. BMC Musculoskelet Disord. 2009;29:238–242. doi: 10.1186/1471-2474-10-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Farr S, Balacó IMS, Martínez-Alvarez S, Hahne J, Bae DS. Current trends and variations in the treatment of unicameral bone cysts of the humerus: a survey of EPOS and POSNA members. J Pediatr Orthop. 2020;40:e68–e76. doi: 10.1097/BPO.0000000000001376. [DOI] [PubMed] [Google Scholar]
- 36.Ackermann O, Eckert K, Rülander C, Endres S, von Schulze Pellengahr C. Ultraschallbasierte Therapiesteuerung bei subkapitalen Humerusfrakturen im Wachstumsalter. Z Orthop Unfall. 2013;151:48–51. doi: 10.1055/s-0032-1328193. [DOI] [PubMed] [Google Scholar]
- 37.Ackermann O. Sonographische Diagnostik der subkapitalen Humerusfraktur im Wachstumsalter. Unfallchirurg. 2010;113:839–844. doi: 10.1007/s00113-010-1825-5. [DOI] [PubMed] [Google Scholar]
- 38.Gladstein AZ, Schade AT, Howard AW, Camp MW. Reducing resource utilization during non-operative treatment of pediatric proximal humerus fractures. Orthop Traumatol Surg Res. 2017;103:115–118. doi: 10.1016/j.otsr.2016.09.022. [DOI] [PubMed] [Google Scholar]
- 39.Crawford DC, Miller LE, Block JE. Conservative management of symptomatic knee osteoarthritis: a flawed strategy? Orthop Rev (Pavia). 2013;5:e2. doi: 10.4081/or.2013.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Beaty JH. Fractures of the proximal humerus and shaft in children. Instr Course Lect. 1992;41:369–372. [PubMed] [Google Scholar]
- 41.Dobbs MB, Luhmann SL, Gordon JE, Strecker WB, Schoenecker PL. Severely displaced proximal humeral epiphyseal fractures. J Pediatr Orthop. 2003;23:208–215. [PubMed] [Google Scholar]
- 42.Pahlavan S, Baldwin KD, Pandya NK, Namdari S, Hosalkar H. Proximal humerus fractures in the pediatric population: a systematic review. J Child Orthop. 2011;5:187–194. doi: 10.1007/s11832-011-0328-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kim A, Swarup I. Rates and predictors of operative management of proximal humerus fractures in adolescents. Unpublished data.
- 44.Hutchinson PH, Bae DS, Waters PM. Intramedullary nailing versus percutaneous pin fixation of pediatric proximal humerus fractures: a comparison of complications and early radiographic results. J Pediatr Orthop. 2011;31:617–622. doi: 10.1097/BPO.0b013e3182210903. [DOI] [PubMed] [Google Scholar]
- 45.Shore BJ, Hedequist DJ, Miller PE, Waters PM, Bae DS. Surgical management for displaced pediatric proximal humeral fractures: a cost analysis. J Child Orthop. 2015;9:55–64. doi: 10.1007/s11832-015-0643-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Canavese F, Athlani L, Marengo L, Rousset M, Rouel-Rabiau N, Samba A, Andreacchio A. Evaluation of upper-extremity function following surgical treatment of displaced proximal humerus fractures in children. J Pediatr Orthop B. 2014;23:144–149. doi: 10.1097/BPB.0000000000000009. [DOI] [PubMed] [Google Scholar]
- 47.Khan A, Athlani L, Rousset M, Samba A, Canavese F. Functional results of displaced proximal humerus fractures in children treated by elastic stable intramedullary nail. Eur J Orthop Surg Traumatol. 2014;24:165–172. doi: 10.1007/s00590-013-1177-2. [DOI] [PubMed] [Google Scholar]
- 48.Swarup I, Hughes MS, Bram JT, Horn BD, Ganley TJ. Percutaneous pinning of pediatric proximal humeral fractures. JBJS Essent Surg Tech. 2019;9:e33. doi: 10.2106/JBJS.ST.19.00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Baker C, Larson N, Shaughnessy W, Stans A, Milbrandt T. Rate of complications and subsequent shoulder complaints for non-operatively managed pediatric proximal humerus fractures. Front Surg. 2020;7:48. doi: 10.3389/fsurg.2020.00048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ali AM, Fawzy SI, Moaty M, Abelaziz M. Treatment of proximal humerus fractures in children with a modified palm tree technique. J Pediatr Orthop B. 2018;27:99–102. doi: 10.1097/BPB.0000000000000452. [DOI] [PubMed] [Google Scholar]


