Introduction
Since the outbreak of coronavirus disease 2019 (COVID-19) in December 2019, the number of infections and deaths has increased exponentially. In February 2020, Lu et al. suggested that the ocular surface could be a route of transmission for severe acute respiratory syndrome coronavirus–2 (SARS-CoV-2), and studies were initiated on the association between the virus and the ocular surface[1]. Zhou et al. demonstrated the presence of SARS-CoV-2 in the conjunctival sac of patients with COVID-19[2]. In addition, Chen et al. reported an association between conjunctival congestion, the main eye symptom associated with COVID-19, and conjunctivitis, which suggests that SARS-CoV-2 can cause conjunctivitis[3]. Daruich et al. [4] demonstrated that conjunctivitis can be the inaugural manifestation of the COVID-19 infection and their case report illustrates the interest of telemedicine in ophthalmology during the COVID-19 pandemic. Several articles have described ophthalmological conditions, with conjunctivitis or keratoconjunctivitis being the main condition from an ophthalmological perspective. Interstitial keratitis is an inflammatory process of the cornea that can be associated with systemic disease of different etiology. We present the first published case of early-onset bilateral interstitial keratitis in a COVID-19-positive patient.
Case report
A 25-year-old female nurse reported initially developing loss of smell and taste, fatigue, and decreased vision. PCR testing for COVID-19 was positive and analytical parameters no suggested activation of the cytokine storm (Leukocytes 7.7 103/μL, neutrophils 56.9% (4.4 103/μL), lymphocytes 33.5% (2.6 103/μL), monocytes 7.5% (0.6 103/μL), eosinophils 1.4% (0.1 103/μL). Hemoglobin 12.9 g/dl, hematocrit 39.9%, MCV 87.8 fl. Platelets 273 103/μL. PCR: 5.66 mg/dl, Fibrinogen 132 mg/dl, Dimer D 96.61 ng/mL., Ferritin 112 ng/ml.
The patient was treated at our center 10 days after the onset of symptoms. PCR testing was negative at that time. Examination revealed best-corrected visual acuity of 0.6 in both eyes. A 53% increase in stromal density was seen on biomicroscopy and in OCT corneal image (Fig. 1 ), with mild fluorescein-positive inferior corneal punctate staining in both eyes, without conjunctival involvement. Fundus examination was normal in both eyes. The treatment was intensive topical corticosteroid treatment was initiated (Dexamethasone 1 mg/ml 1 drop every 1 hour for 24 hours, tapering to every 2 hours for 48 hours, every 4 hours 1 week, every 6 hours 1 week, every 8 hours 1 week, every 12 hours 1 week and every 24 hours 1 week and dexamethasone ointment at night for first week). Fourteen days after treatment, the right cornea was completely transparent, and the left cornea showed remarkable improvement in transparency (Fig. 2 ) The patient's corrected visual acuity was 1.0 in both eyes. The patient was followed up to 6 months, showing no other recurrences.
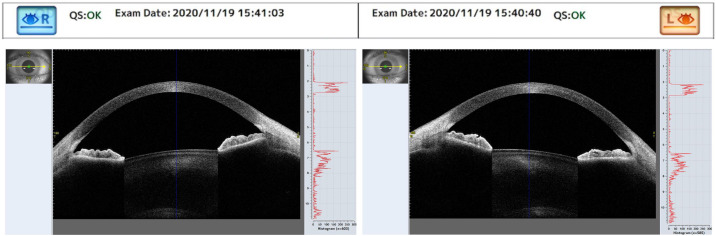
Figure 1.
Increased anterior stromal density with an increase of spike height in A-scan. Caliper measuring the denser anterior stroma and the transparent posterior stroma.
Figure 2.
Disappearance of stromal density in both eyes with a decrease of spike height in A-scan.
Discussion
Conjunctival involvement is the most frequent ophthalmological condition within the manifestations of COVID-19, although other conditions are possible and have been published. Until now, bilateral stromal involvement has not been reported in the literature. According to treatment guidelines for epithelial keratitis, glucocorticoids are generally not recommended for viral punctate epithelial keratitis because they are believed to promote viral replication although some authors as Dongyu Guo et al. [5] found that topical glucocorticoids played an important role in the recovery of keratoconjunctivitis in a patient with COVID- 19 and increased local cytokines.
In our case, stromal affectation does not raise doubts about the need for corticosteroid use [6]. In this case, the non-involvement in the cytokine storm, made us opt for topical treatment as the first choice with favorable evolution in just a few days[7]. No slit lamp photograph was taken as the change in stromal density was notorious in the anterior OCT. Stromal keratitis can occur early in patients with COVID-19, in the context of a local manifestation with loss of vision that requires diagnosis, treatment and monitoring by the ophthalmologist.
The non-association of this manifestation with the systemic inflammatory cascade makes systemic corticosteroid treatment unnecessary, being able to obtain satisfactory results with the use of topical corticosteroids.
Funding
The authors did not receive any funding.
Author contribution
All the authors contributed to the study concept and design, data collection and analysis, as well as the preparation of the material. The first draft of the manuscript was written by Antonio Cano-Ortiz, and all the authors provided their comments. All the authors read and approved the final version of the manuscript.
Disclosure of interest
The authors declare that they have no competing interest.
Statement of ethics
Study approval statement: “This study protocol was reviewed and approved by [Arruzafa hospital committee], approval number [05.2021.01].”
Consent to publish statement: written informed consent was obtained from the participant for publication of the details of their medical case and accompanying images.
Availability statement
All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author.
Acknowledgments
This manuscript does not include any nonauthor contributors to acknowledge.
References
- 1.Lu C. wei., Liu X. fen., Jia Z. fang. 2019-nCoV transmission through the ocular surface must not be ignored. Lancet. 2020;395:e39. doi: 10.1016/S0140-6736(20)30313-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang X., Chen X., Chen L., Deng C., Zou X., Liu W., et al. The evidence of SARS-CoV-2 infection on ocular surface. Ocul Surf. 2020;18:360–362. doi: 10.1016/j.jtos.2020.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen L., Deng C., Chen X., Zhang X., Chen B., Yu H., et al. Ocular manifestations and clinical characteristics of 535 cases of COVID-19 in Wuhan, China: a cross-sectional study. Acta Ophthalmol. 2020;98:e951–e959. doi: 10.1111/aos.14472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Daruich A., Martin D., Bremond-Gignac D. Ocular manifestation as first sign of Coronavirus Disease 2019 (COVID-19): Interest of telemedicine during the pandemic context. J Fr Ophtalmol. 2020;43:389–391. doi: 10.1016/j.jfo.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guo D., Xia J., Wang Y., Zhang X., Shen Y., Tong J.P. Relapsing viral keratoconjunctivitis in COVID-19: A case report. Virol J. 2020:17. doi: 10.1186/s12985-020-01370-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Austin A., Lietman T., Rose-Nussbaumer J. Update on the Management of Infectious Keratitis. Ophthalmology. 2017;124:1678–1689. doi: 10.1016/j.ophtha.2017.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wiersinga W.J., Rhodes A., Cheng A.C., Peacock S.J., Prescott H.C. Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review. JAMA - J Am Med Assoc. 2020;324:782–793. doi: 10.1001/jama.2020.12839. [DOI] [PubMed] [Google Scholar]