Abstract
Rotationplasty is an established technique that is indicated as part of the surgical reconstruction for certain patients with primary bone tumors around the knee who undergo tumor resection. There is considerable variation in the application of rotationplasty by surgeons as well as acceptance of the procedure by patients who may be candidates for this procedure. We qualitatively studied the decision-making process of families of patients who had undergone rotationplasty by interviewing 4 patients and their families using semi-structured interviews. Thematic analysis identified the following themes that were important in the decision-making process: (1) the desire for good information sources, (2) finding value in meeting with other patients who had been faced with a similar decision, (3) prioritizing function over cosmesis, (4) a desire to limit the need for revision surgeries, and (5) accepting that a return to normalcy is not an option with a surgery. Physicians and patients faced with a similar decision can benefit from a better understanding of the process, and by the normalization of anxieties and concerns that they may experience.
Keywords: Cancer, clinician–patient relationship, medical decision making, rotationplasty, osteosarcoma, Ewing’s sarcoma
Introduction
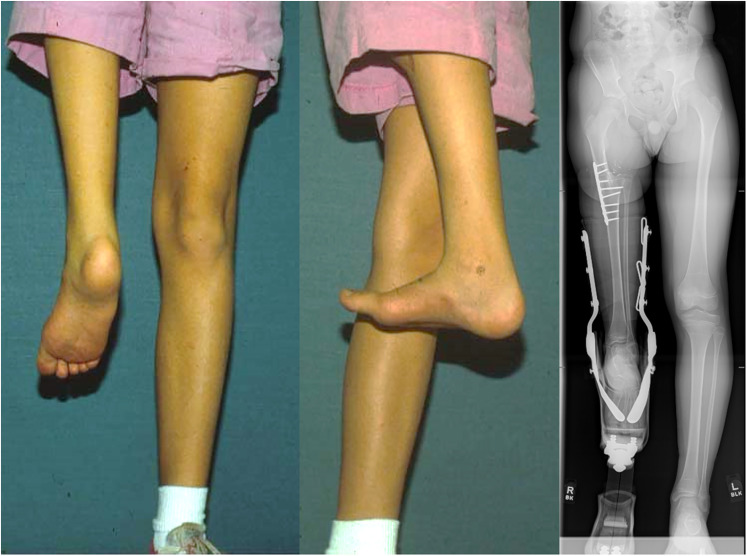
Rotationplasty is a well-established surgical procedure for reconstruction following resection of the primary bone sarcoma in the lower extremity. It was first described by Borggreve (1) in 1930 in the German literature for limb shortening and tuberculous knee ankylosis and then in 1950 in the English literature by Van Nes (2) for the management of proximal femoral focal deficiency. Its use for reconstruction of the lower extremity following tumor resection was first described in 1982 by Kotz and Salzer (3), and a series documenting good results with this application of rotationplasty followed (4,5). It is performed in pediatric patients with tumors of the distal femur and proximal tibia, with variations performed following resection of tumors at other lower extremity sites (6,7). The most common variant involves the substitution of the function of the resected knee with the ankle by rotation of the calf and ankle 180°, and subsequent fixation of the tibia to the femur. The non-anatomical appearance (Figure 1) resulting from this surgery deviates from the natural form and is considered unacceptable by some patients and surgeons. In certain clinical situations, limb salvage surgery with endoprosthetic reconstruction or rotationplasty is both surgically feasible and studies have shown equivalent functional outcomes in both patient groups (5,8–10). The non-anatomical nature and appearance of the lower extremity following a rotationplasty is a factor in the divergence in opinions regarding this procedure among medical professionals, and this makes it imperative that the surgeon, the patient, and his or her family engage in a process of shared decision-making.
Figure 1.
Post-operative photographs and radiograph of a patient who had undergone a rotationplasty.
The patients undergoing rotationplasty for oncologic indications are predominantly in the pediatric age group, and this adds significant complexity to decision-making. The patients’ parents are making the decision as a surrogate decision-maker for the patient for surgery with a significant life-long functional, cosmetic impact on the patient.
It was not uncommon for patients' families to travel some distance to seek out surgeons with experience in rotationplasty to perform this surgery. Occasionally, this decision was made in disagreement with an orthopedic surgeon with who they had already consulted (11). We thus decided to explore this aspect of decision-making, and this aspect of self-selection that has been proposed by some authors as a contribution to the favorable emotional and psychosocial outcomes in patients who undergo rotationplasty (12). Studies have focused on the outcomes of patients who underwent rotationplasty, documenting the non-inferiority of rotationplasty as compared to limb-sparing surgery, but they do not explain how patients’ families choose between the options.
Qualitative studies have investigated the decision-making processes of patients’ families who choose to undergo elective amputations for functionally impaired limbs (13), and in patients who suffered open tibial fractures (14). There are however no studies to date outlining similar issues in the field of musculoskeletal oncology in patients who have undergone rotationplasty. The purpose of this qualitative study was to describe how the families of patients with primary lower extremity bone sarcoma chose rotationplasty following tumor resection. In particular, we sought to identify common characteristics and themes in the lived experiences of this self-selected group of patients and their families. With the knowledge gained from this study, more effective counseling of patients could be performed.
Methodology
Following institutional review board approval, parents of patients and patients who had undergone rotationplasty for lower extremity osteosarcoma at our institution were invited to participate in this study, including patients undergoing rotationplasty and those on follow-up. Four patients were recruited for this study. All interviews were performed in person by a single interviewer; 2 were conducted within a week of surgery, 1 at 1.5 years and the last at 5.5 years post-surgery. The interviewer was not an attending surgeon involved in the surgery of the patients. The interviews comprised a semi-structured interview with the patient and either 1 or both of the patient's parents. The semi-structured interviews were used for consistency of the scope of the interview while permitting interviewees to elaborate and interject on topics as they deemed fit. The areas explored in the interview included how subjects researched the surgical options, the subjects understanding of the surgical options, what factors affected their decision making, their reflection on their decision following the surgery, and their lived experience following surgery. Questions regarding the decision-making process were posed to the patient's parents, with the opportunity for the patients to add their thoughts after the parent had concluded. Questions regarding the lived experience were posed to the patient and with the opportunity to add further perspective offered to the patient's parent(s) after the patient had concluded their remarks.
Interviews were audio-recorded, reducing the need for extensive note-taking and facilitating rapport between interviewee and interviewer. The interviews were then transcribed verbatim for thematic analysis (15). Using this inductive technique, open coding was performed for each transcript converting each into a series of codes. The codes identified in each transcript were then compared with those from other transcripts. Transcripts were reviewed again to assess for concordance of these codes. Finally, these codes were organized into separate themes that described the decision-making process of the study subjects
Results
The study group comprised 4 patients and their parents. The 2 patients interviewed within a week of surgery were each interviewed together with both of their parents, while the 2 patients interviewed at 1.5 and 5.5 years postoperatively were interviewed with their mothers (Table 1).
Table 1.
Demographics of Study Subjects.
| Subjects no. | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| Age at time of diagnosis | 8 years 1 month | 8 years 5 months | 13 years | 9 years |
| Gender | Male | Female | Male | Male |
| Age at time of interview | 14 years | 10 years | 13 years | 9 years |
| Diagnosis | Osteosarcoma | Osteosarcoma | Ewing's sarcoma | Osteosarcoma |
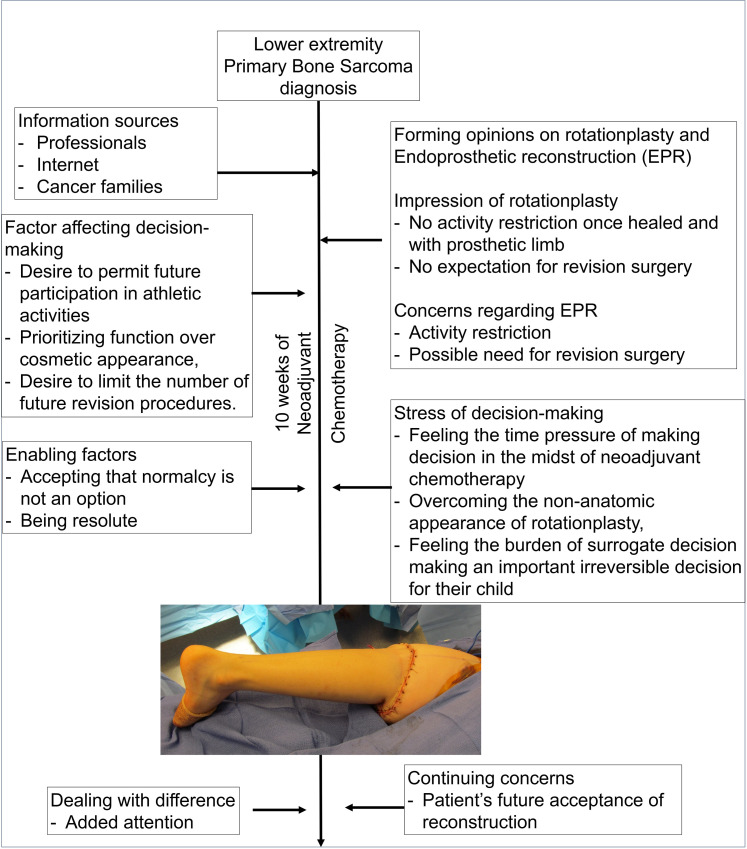
The interviews highlighted various stages that subjects went through in the decision-making process and following the procedure (Figure 2).
Figure 2.
Flowchart illustrating typical decision-making process toward rotationplasty in study group.
Information Sources
All patients and their families reported doing research on the internet to explore the surgical options, including rotationplasty. This was in addition to the information from professional sources and a lack of information was not noted by any subject. The mother of one patient #4 noted that the availability of surgical options left her feeling as having little clear guidance.
All interviewees related meeting other families and patients who had undergone either rotationplasty, endoprosthetic reconstruction, or both. There was value placed in accounts of personal experience over information from professional sources. Regarding how she valued accounts of personal experiences the mother of patient #1 explained, “when you got a kid who has, um, cancer that supposed that's however many in a million, statistics don’t mean a whole lot after that.”
Forming Opinions of Rotationplasty and Endoprosthetic Reconstruction
All interviewees expressed an element of shock when first being presented with the idea of rotationplasty. They discussed the aspects of rotationplasty that distinguished it from endoprosthetic reconstruction being the potential for no further surgeries and the lack of restriction on high impact activity.
Their views on limb-sparing endoprosthetic reconstructive surgery appeared to be predominated by their concern surrounding the risks of complications of the surgery such as infection, and the potential need for revision surgery in the future. The restriction on high-impact physical activity is also featured in the accounts of subjects.
Factors Influencing the Decision-Making Process
Three factors surfaced in the accounts of interviewees that influenced the decision-making process: (1) the desire to permit future participation in athletic activities, (2) prioritizing function over external appearance, and (3) the desire to limit the number of future procedures.
Two parents expressed their desire to keep options open for their children, by choosing a surgery associated with a smaller chance of needing to restrict future participation in sports. These parents viewed their children as athletic and recounted the patients’ enthusiasm for sports as the rationale for them viewing the durability of rotationplasty as a feature that made it favorable to them. The parent of patient 1 reflected on the desire to keep options open with respect to sporting participation saying, “As you grow, and change what you enjoy doing. I mean he's doing so many more activities now than he used to do when I mean at the age of 7, you don’t really know what is this person going to do when they grow.” While the parent of patient 4 put it as, “I think the one thing we didn’t want to do for (patient's name) was to make a decision for what he's able to do or not do in his life because we chose one of the other options which we believed would limit what he could do.”
This desire for function was recounted by 2 of the parents explicitly valuing function over appearance. Mother of patient 2 recounted, “(The surgeon) said do you want her to look normal, or do you want her to function normal. And that sealed it for me.”
Finally, the desire to avoid future surgeries was highlighted by 2 of the parents as an important factor in their decision. The mother of patient 3 stated emphatically, “We didn’t want the ongoing surgeries in the future,” while the mother of patient 2 stated, “And no more surgeries, you know, just the one surgery, instead of having to go back again.”
Stress of Decision-Making
The lived experiences of the patients and their families featured the following themes in the decision-making process: (1) feeling the time pressure of making the decision regarding the nature of reconstruction in the midst of the patient undergoing chemotherapy, (2) overcoming the non-anatomical appearance of rotationplasty, and (3) feeling the burden of making an important irreversible decision on behalf of the patient.
The pressure to make a decision regarding the nature of the reconstruction especially in the midst of chemotherapy and prior to a set date was a stressor. Compounding this time pressure was the need to accept the non-anatomical appearance of rotationplasty. The mother of patient 2 expressed some of her fears regarding the possibility of the patient being made fun of subsequently and also regarding whether the patient would accept the decision that had been made on her behalf. While the mother of patient 4 recounted her process of overcoming the issue of the external appearance in saying: “I mean it's different. Certainly is. To me, I’ve said all along. If we can get rid of this cancer, we can live with this.”
The parents of the patients also felt the burden of making an important irreversible decision as to their child's surrogate decision-maker.
Factors Enabling Coming to a Decision
Study subjects described that coming to their final decision was aided by accepting that a return to normalcy was not an option and reflected feelings of being resolute about their decision. They shared insight into their process of acceptance that no surgical option would return the patient to normalcy, but that they felt rotationplasty was the best option for them with the mother of patient 4 saying “I mean we’re not believing that things are going to go back to normal. We understand.” Being resolute about their decision-making and seeing their decision through was recounted in several ways, the mother of patient 4 recounted, “ I mean I knew when I saw it that was what we needed to do.”
Post-Operative Issues
The 2 study subjects that had undergone rotationplasty over 2 years prior also reflected on several aspects of their lived experiences post-surgery. Both described their experiences with dealing with the differences, specifically the added attention they had received, how they had used humor to deal with these situations and how they had used that as an opportunity to raise awareness about bone sarcoma. Issues with managing a prosthetic leg that had not been anticipated prior to the surgery were also raised by both of these study subjects. The time and effort required for prosthetic maintenance and this was related to being accepted as “part of the package.”
Discussion
The purpose of this study was to describe the decision-making process and lived experience of patients and families of patients who underwent rotationplasty. This has not been investigated previously and this study presents a unique aspect of how decisions are made regarding this type of surgery. Issues that are important to patients and their families may not factor into the decision-making processes of medical professionals. This improved understanding is instructive for physicians caring for such patients, allowing these issues to be pre-empted, and is beneficial for patients and their families in normalizing their experiences and the anxieties that are common to many undergoing a similar experience.
The decision between opting for a limb preserving reconstruction or for a rotationplasty in the setting of surgical management of bone sarcoma is complex. Decision-making models in medicine serve to distinguish the varying roles of the doctor and the patient and his or her advocates played in this process (16). The paternalistic, the informed and the shared decision-making (SDM) models vary in the extent of participation by the patient and the physician in the process of decision making. In practice, intermediate approaches are also employed depending on the nature of the medical condition and the preferences of the patient. Studies have explored SDM about cancer treatment (17) and outlined the roles of physicians and patients in this model. Boomhof-Roordnik et al. (17) in their shared decision-making model divided the duties between the oncologists and the patients, with oncologists’ duties including determining and explaining the possible treatments, emphasizing the importance of patients’ opinions, getting to know the patients, guiding the patients and providing treatment recommendations, and patients responsibilities including asking questions, expressing thoughts and feelings, considering options, offering opinions, and deciding or delegating decisions to oncologists.
The decision regarding rotationplasty is not a decision regarding the treatment of cancer per se, but rather regarding functional reconstruction. However, considering that the resection and reconstruction are performed at the same time the decision regarding rotationplasty is inextricably linked to the management of cancer and may be viewed through a similar lens of decision making in cancer care.
Our study highlighted factors those patients' families recounted in their decision-making process. The valuing of information sources from other cancer patients over professional sources of information was highlighted by patients. Physicians with patients and families faced with this decision should attempt to have these patients put in touch with other patients who have been in a similar situation to aid these patients in their decision-making.
The impression of study subjects focused on their experience and expectations of rotationplasty with respect to not need to limit the patients’ weight-bearing and participation in high impact activities, and not anticipating the need for revision surgery. While with an endoprosthetic reconstruction there were concerns regarding the need for future revision surgery and the need to limit impact activities. Owing to this study comprising only patients who underwent rotationplasty, this reflects the impression and concerns in this group of the two contrasting reconstructions. This information may be used in the counseling of the patient being planned for endoprosthetic reconstruction so that their concerns regarding activity limitation as well as the risk of revision can be adequately addressed.
The factors identified as important in their decision-making were the desire to permit future participation in athletic activities, prioritizing function over external appearance, and the desire to limit the number of future procedures. It is well documented that rotationplasty is not inferior to limb-sparing surgeries with respect to functional outcomes (9). In fact, several studies have documented that the superior functional outcomes of rotationplasty in the setting of sarcoma resection (8,12,18). The need to prioritize function over external appearance is important to highlight owing to the uniquely non-anatomical nature of this reconstruction. Patients' families in our study did raise their concerns about the psychosocial impact on patients. These specific psychosocial concerns have also been previously studied. A study by Akahane et al. (19) comparing patients who underwent rotationplasty, endoprosthetic reconstruction, and amputation did not find any differences in functional or emotional domains of the Short Form-36. Other authors have also put forth reasons to account for this including that patients who underwent rotationplasty are self-selected, their young age at the time of surgery making acceptance of their condition easier, and the patients’ expectation of requiring fewer future operative interventions being beneficial for their emotional well-being (12,20).
Our study also highlights that the complexity of the decision-making is compounded by several factors: the time pressure of the decision-making, the burden felt as a surrogate decision-maker, and the acceptance of the outward appearance that could be described as “deviant” from the normal. Understanding these concerns faced by patients' families would allow physicians to normalize these anxieties in other patients and families, and help them realize that they “are not the only ones” with such anxieties.
In finalizing their decision, patients' families also reflected on their acceptance that a complete return to normalcy was not an option afforded by any reconstructive option and they chose the option that best met their values and priorities. This experience of how patients handled their expectations echoes the findings in a similar qualitative study by Quon et al. (13) regarding the decision-making process of patients choosing to undergo elective amputation for a functionally impaired lower limb. Setting realistic expectations was noted to be important in minimizing dissatisfaction regarding functional and esthetic outcomes (13).
Despite the literature documenting the favorable results in functional domains, and the lack of significant psychosocial or emotional differences in patient experience, rotationplasty for primary bone sarcoma remains an uncommon procedure in the United States and patients may travel considerable distances to consult with physicians owing to the procedure not being offered by their local physicians (11). The values and priorities held by patients and families may also not always be aligned to those of their physicians. In the setting of shared decision-making or informed decision-making model, these patients may seek out medical care that aligns with their own values and priorities.
It should at the same time be recognized that patients differ in their preferences regarding the extent of involvement in medical decision-making they desire (21) and some patients do prefer to defer to their physicians regarding treatment decisions. For patients who delegate the final recommendation to their physicians, the process as described in this study would be expected to still be part of the lived experience of patients and their parents.
Our study does have several limitations. Firstly, it is a small study. Rotationplasty is a procedure that is performed infrequently among patients with a rare malignancy thus making a larger study challenging. This notwithstanding the findings in this qualitative study are still of value to patients and clinicians who provide care to this small subset of unique patients. Secondly, coding of the transcripts was performed by an individual, rather than multiple coders. Lastly, our study also focuses exclusively on the perspective of patients and their families. The shared decision-making process involves both patients and medical professionals, and the approach of the surgeons in their pre-operative counseling may affect the result of the decision-making process. The surgeons’ experience of their pre-operative counseling may thus be an area for further study.
The practice in the senior author's institution in pre-operative counseling of patients considering rotationplasty includes introducing the reconstructive surgical procedure early in the course of treatment to provide ample time for thoughtful consideration by patients’ and their families and placing them in contact with other families of patients who have previously undergone rotationplasty. The findings of this study affirm the value of this approach to patients in this situation.
Conclusion
In conclusion, this study outlines the lived experience and the factors deemed important in decision-making by patients and their families in deciding to and going through a rotationplasty for the management of lower extremity primary bone sarcoma includes the desire for good information sources, meeting with peers, and other families who have gone through a similar course of treatment, a reflection on their prioritizing function while accepting cosmetic disadvantages, stresses inherent to deciding on a major surgery in the midst of neoadjuvant chemotherapy and the acceptance that a return to normalcy is not an option with a surgery. Physicians and patients faced with a similar decision can benefit from a better understanding of the process experienced by others, and by the normalization of anxieties and concerns that they may experience.
Acknowledgments
The authors wish to acknowledge the invaluable role that Brandi Nunn, RN, BSN plays in the care of the unique group of patients that this article discusses.
Footnotes
Ethical Approval: Ethical approval for this study was obtained from the University of Florida Institutional Review Board (ID:201401039).
Statement of Human and Animal Rights: All procedures in this study were conducted in accordance with the University of Florida Institutional Review Board (ID:201401039).
Statement of Informed Consent: Written informed consent was obtained from the patients’ parents for their anonymized information to be published in this article.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Chung M Chan https://orcid.org/0000-0001-8110-1417
References
- 1.Borggreve. Kniegelenksersatz durch das in der beinlängsachse um 180° gedrehte fußgelenk. Arch Für Orthop Unf-Chir Mit Bes Berücksicht Frakturenlehre Orthop-Chir Tech. 1930;28:175-8. [Google Scholar]
- 2.Van Nes CP. Rotation-plasty for congenital defects of the femur. J Bone Joint Surg Br. 1950;32-B:12-6. [Google Scholar]
- 3.Kotz R, Salzer M. Rotation-plasty for childhood osteosarcoma of the distal part of the femur. J Bone Joint Surg Am. 1982;64:959-69. [PubMed] [Google Scholar]
- 4.Merkel KD, Gebhardt M, Springfield DS. Rotationplasty as a reconstructive operation after tumor resection. Clin Orthop. 1991;270:231-6. [PubMed] [Google Scholar]
- 5.Hillmann A, Hoffmann C, Gosheger G, Krakau H, Winkelmann W. Malignant tumor of the distal part of the femur or the proximal part of the tibia: endoprosthetic replacement or rotationplasty. Functional outcome and quality-of-life measurements. J Bone Joint Surg Am. 1999;81:462-8. [DOI] [PubMed] [Google Scholar]
- 6.Winkelmann WW. Rotationplasty for tibial tumours. J Bone Joint Surg Br. 1991;73:697. [DOI] [PubMed] [Google Scholar]
- 7.Winkelmann W. [Rotation osteotomy in malignant tumors of the proximal femur]. Z Orthop Ihre Grenzgeb. 1983;121:547-9. [DOI] [PubMed] [Google Scholar]
- 8.Ginsberg JP, Rai SN, Carlson CA, Meadows AT, Hinds PS, Spearing EM, et al. A comparative analysis of functional outcomes in adolescents and young adults with lower-extremity bone sarcoma. Pediatr Blood Cancer. 2007;49:964-9. [DOI] [PubMed] [Google Scholar]
- 9.Hopyan S, Tan JW, Graham HK, Torode IP. Function and upright time following limb salvage, amputation, and rotationplasty for pediatric sarcoma of bone. J Pediatr Orthop. 2006;26:405-8. [DOI] [PubMed] [Google Scholar]
- 10.Bekkering WP, Vliet Vlieland TPM, Koopman HM, Schaap GR, Bart Schreuder HW, Beishuizen A, et al. Functional ability and physical activity in children and young adults after limb-salvage or ablative surgery for lower extremity bone tumors. J Surg Oncol. 2011;103:276-82. [DOI] [PubMed] [Google Scholar]
- 11.Betsy M, Capozzi JD, Rhodes R. The human form: accepting the prioritization of patient values. J Bone Joint Surg Am. 2005;87:1653-5. [DOI] [PubMed] [Google Scholar]
- 12.Rödl RW, Pohlmann U, Gosheger G, Lindner NJ, Winkelmann W. Rotationplasty–quality of life after 10 years in 22 patients. Acta Orthop Scand. 2002;73:85-8. [DOI] [PubMed] [Google Scholar]
- 13.Quon DL, Dudek NL, Marks M, Boutet M, Varpio L. A qualitative study of factors influencing the decision to have an elective amputation. J Bone Joint Surg Am. 2011;93:2087-92. [DOI] [PubMed] [Google Scholar]
- 14.Aravind M, Shauver MJ, Chung KC. A qualitative analysis of the decision-making process for patients with severe lower leg trauma. Plast Reconstr Surg. 2010;126:2019-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chapman AL, Hadfield M, Chapman CJ. Qualitative research in healthcare: an introduction to grounded theory using thematic analysis. J R Coll Physicians Edinb. 2015;45:201-5. [DOI] [PubMed] [Google Scholar]
- 16.Slover J, Shue J, Koenig K. Shared decision-making in orthopaedic surgery. Clin Orthop. 2012;470:1046-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bomhof-Roordink H, Fischer MJ, Duijn-Bakker Nv, van Baas‐Thijssen MC, Weijden TVD, Stiggelbout AM, et al. Shared decision making in oncology: a model based on patients’, health care professionals’, and researchers’ views. Psychooncology. 2019;28:139-46. [DOI] [PubMed] [Google Scholar]
- 18.Fuchs B, Kotajarvi BR, Kaufman KR, Sim FH. Functional outcome of patients with rotationplasty about the knee. Clin Orthop Relat Res. 2003;415:52-8. [DOI] [PubMed] [Google Scholar]
- 19.Akahane T, Shimizu T, Isobe K, Yoshimura Y, Fujioka F, Kato H. Evaluation of postoperative general quality of life for patients with osteosarcoma around the knee joint. J Pediatr Orthop B. 2007;16:269-72. [DOI] [PubMed] [Google Scholar]
- 20.Hanlon M, Krajbich JI. Rotationplasty in skeletally immature patients. Long-term followup results. Clin Orthop. 1999;358:75-82. [PubMed] [Google Scholar]
- 21.Levinson W, Kao A, Kuby A, Thisted RA. Not all patients want to participate in decision making. A national study of public preferences. J Gen Intern Med. 2005;20:531-5. [DOI] [PMC free article] [PubMed] [Google Scholar]