ABSTRACT.
Tropical alluvial gold and gem miners are often an especially at-risk population for malaria infection. Geographical areas of mining-associated malaria epidemics in the recent past include Southeast Asia (Cambodia, Thailand, and Myanmar); the Amazon basin (Brazil, French Guyana, Suriname, Columbia, and Peru); and tropical Africa. Mobile populations of young adult men engaged in the hard labor of mining may experience severe malaria especially if they lack preexisting immunity and are irregularly consuming antimalarial drugs. Particular problems occur because much of this informal mining activity is illegal and done in isolated areas without access to health services and with evidence of emerging antimalarial drug resistance. Concentrating vulnerable populations in an ecologically disturbed landscape is often conducive to epidemics, which can then spread as these highly mobile workers return to their homes. Mining-associated malaria endangers malaria elimination efforts and miners need to be addressed as a group of particular concern.
Recently malaria control efforts have been circumvented or delayed by mobile mining populations who accept malaria as an occupational hazard in an already risky business that often leads to exploitation for many and riches for a few. Gem mining has been a major focus of malaria drug resistance in southeast Asia and gold mining has driven relapsing malaria through much of the Amazon basin. Common risk profiles include marginalized largely male populations conducting illegal activity in areas with a disturbed ecology, few health facilities, and poorly controlled use of limited antimalarial drugs. This brief review describes mine-associated malaria epidemiology and points toward interventions that may assist the eventual goal of malaria elimination.
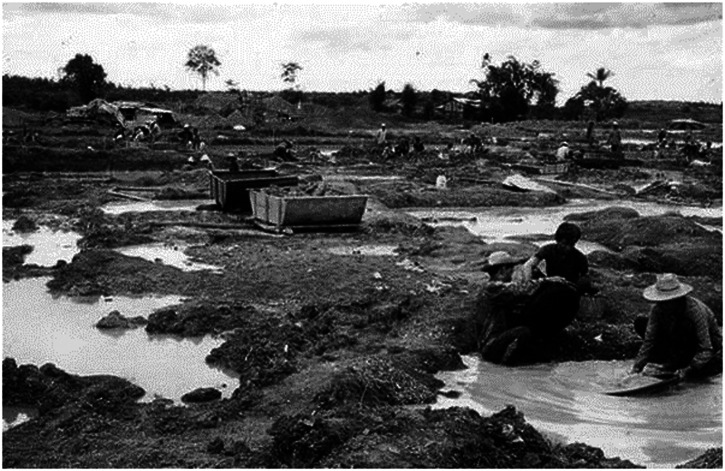
Armed conflict in southeast Asia created gem mining opportunities in border regions of Cambodia and Myanmar (Burma). After the Khmer Rouge were expelled from most of Cambodia, a poorly controlled borderland resulted in many tens of thousands of miners washing gravel searching for rubies and sapphires on both sides of the Thai–Cambodian border from the late 1980s1 (see Figure 1.) This disturbed landscape favored breeding of the usually forest fringe Anopheles vectors, especially An. dirus, even years after miners left the area. Screening of Burmese and Mon ethnic gem miners in Borai, on the Thai–Cambodian border in 1990 showed > 90% were young adult men of which 75% were blood slide positive for malaria. The Thai Malaria Control Program found 65,500 cases (90% Plasmodium falciparum) with 7,000 severe cases (including 300 with cerebral malaria) and 97 deaths in 1990 in mining areas. Mine-associated malaria in southeast Thailand made up nearly a quarter of the country’s total.1
Figure 1.
Gem miners washing soil to search for rubies and sapphires in Borai District, Trat Province, Thailand, in 1989. Photo credit: Malaria Division, Department of Communicable Diseases Control, Thai Ministry of Public Health (via Dr. Krongthong Thimasarn).
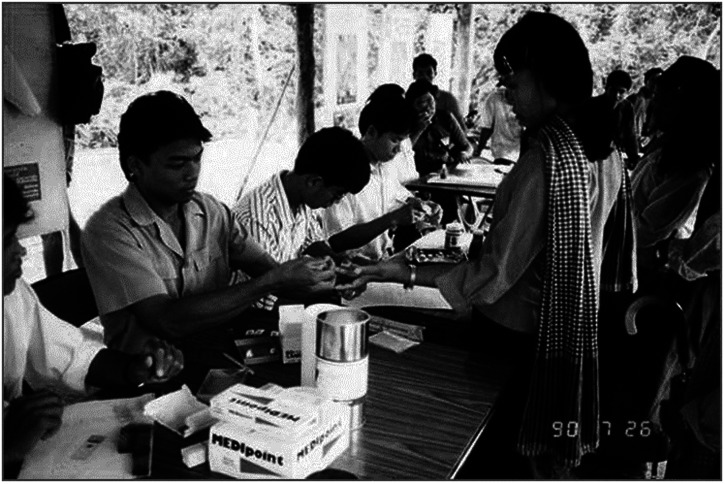
Conflict constrained any governmental actions and health services were largely restricted to malaria posts on the Thai border waiting for sick miners to stagger back to a source of microscopic diagnosis and antimalarial drugs (Figure 2). Miners with new infections mixed with men whose suppressed parasites had been treated weeks before with the long-acting drug mefloquine to create a perfect storm of gametocytemic individuals and subtherapeutic drug concentrations selecting for drug resistance.2 The lure of winning the lottery to find a large gemstone led under employed Thai civilians to try their luck on the mining fields access to which was controlled by the Khmer Rouge who charged for guidance around the many areas with explosive antipersonnel mines. Gem mining and explosive mines were linked in a cycle of exploitation that secondarily drove malaria drug resistance.3
Figure 2.
A temporary clinic setup by the Thailand Malaria Division to conduct malaria screening by blood smears among gem miners along the Thai–Cambodian border circa 1990. Photo credit: Malaria Division, Department of Communicable Diseases Control, Thai Ministry of Public Health (via Dr. Krongthong Thimasarn).
Furthermore, this malaria drug resistance was spread across Thailand to Myanmar by a direct transportation link moving men and minerals to the other major gem fields on the periphery of Myanmar where long-running ethnic conflicts created another malaria disaster zone.4 Transient mining populations make poor malaria study populations, but increasing therapeutic failure rates were documented in the surrounding civilian/refugee populations on the Thai–Burmese borders as first mefloquine-sulphadoxine-pyrimethamine (MSP) and then artemisinin combination therapies were successively introduced. In 1989, a therapeutic efficacy study (TES) of MSP with 42 days follow-up showed 53% efficacy in Borai and 55% in Maesod on the Burmese border. By 1990, TES of MSP with 28 day follow-up in Maesod showed a drop in efficacy to 36%.4 Driven by political and economic factors, the gem mining population was an important source of malaria infections across the entire region especially because of their highly mobile character. In the north, jade mining for China was important and likely resulted in the poorly documented disease deaths of Chinese miners in Myanmar’s Kachin State. As China has eliminated indigenous malaria, there is now a risk of reintroduction of malaria by miners and other migrant workers traveling across the Burmese border areas.
More recently, in southeast Asia, secular trends such as deforestation and travel restrictions because of the coronavirus pandemic have led to decreased incidence of malaria. However, as fewer malaria cases occur, evolutionary selection often means they are of the most drug-resistant types. In Myanmar (Bago region across from Tak Province in Thailand), malaria parasite surveillance in gold miners showed a high rate of Pfk13 mutants, validated artemisinin resistance markers, and detection of isolates with increased pfmdr1 copy number suggested a decline in artemisinin combination therapy (ACT) efficacy.5 When approaching malaria elimination the most important populations remaining with malaria are often also the most difficult to access such as those transiently working in illegal mining operations in border regions.
Alluvial gold mining in Latin America has been a major driver of malaria epidemiology across the Amazon basin as this largely illegal activity crosses borders from Brazil, French Guiana, Suriname, Columbia, and Peru.6 The possibility of breaking out of poverty via a gold strike drives large numbers of impoverished miners to work in isolated jungle areas as documented in French Guiana.7 More than 10,000 miners working across 700 different mining sites results in an huge informal sector, which extracts literally tons of gold. These “garimpeiros” promote deforestation and riverine rearrangements, which favor the main vector Anopheles darlingi. Despite difficulties in recruitment to formal studies, 22% of 421 French Guianese miners studied were found to be nucleic acid positive for P. vivax of which 84% were asymptomatic.7 Unlike southeast Asia, the malaria problem in Latin America is predominately because of relapsing P. vivax whose residual hepatic stages (hypnozoites) promote infections that often occur months later far from the original site of infection. For a continent aspiring to malaria elimination within the next decade, gold mining is a major threat to this ambition because of the mobile mining populations where some exceptional mining communities even have a P. falciparum predominance.8,9 Risk factors in the Brazil-French Guiana border region mining area were investigated and parasitemia (mostly asymptomatic) was found associated with age > 15 years, remote location with a history of previous malaria infection and anemia.9
An analogous situation existed in southern Peru where unstable transmission exists in Madre de Dios10 (Figure 3). Over a decade from 2001, 30,811 malaria infections in southern Peruvian mining areas were found from > 200,000 febrile episodes (15%). Factors associated with malaria included being near illegal mining areas, from where the health networks reported > 30 times more cases compared with areas with low mining activities. Significantly more cases (16 times) were also reported from a health facility distant from the major routes of transportation.10 Almost all of the confirmed cases received treatment, but over 90% of treatment provided was unsupervised especially in the illegal gold mining areas. Malaria was seasonal concentrated at the beginning of the year and highly correlated to the amount of gold extracted the previous month. Successful control of most of the southern Peruvian focus of malaria largely depended on governmental actions to suppress the illegal trade and limit access to the mining areas.10
Figure 3.
Gold mining activity in Huaypetue River in Madre de Dios region of Peru circa 2011. Photo credit: Dr. Juan F. Sanchez, Department of International Health of Johns Hopkins Bloomberg School of Public Health.
In South America, the key shift affecting malaria has been the political difficulties experienced in Venezuela, previously an outstanding example of malaria control. Currently, Venezuelan malaria makes up a majority of all malaria infections in South America which are mostly vivax malaria.11 Malaria control activities inside Venezuela have been greatly curtailed without foreign exchange to purchase insecticides and other commodities such as drugs. Because of social and economic stress there has been a flow of people out of Venezuela into the broader Amazon region some of whom have been involved in alluvial gold mining activities. In the southern Bolivar State, deforestation and associated alluvial gold mining has become a chronic “hotspot” of malaria transmission and workers from there have spread parasites into the triangular area of Roraima State of Brazil, Guyana, and Venezuela. Cross border malaria is an increasing problem in northern Brazil again largely driven by transient gold mining populations.12 As this involves close to half a million cases of malaria annually, it becomes obvious that this subregion is not moving toward malaria elimination. Genetic analysis of P. falciparum samples collected from Bolivar in 2018 showed that drug-resistant mutations in Pfdhfr, Pfdhps, and Pfcrt were still present, but SP and chloroquine are no longer used for the treatment of falciparum malaria.13 Unlike southeast Asia mutations associated with artemisinin resistance or delayed parasite clearance in the Pfk13 gene were not detected.13 However, it is important to continue monitoring drug-resistant malaria in this mining population as selection of artemisinin resistance polymorphisms is likely an emerging problem.14
Gold miners are a diverse and difficult to study group. Spatial analyses of Brazilian gold miners in Roraima State where a majority of the 520 persons studied had malaria parasitemia noted 90% were linked to gold mining sites in either Venezuela or Guyana.15 Lack of education, lack of knowledge of malaria transmission patterns, and promiscuous use of antimalarial drugs outside a mass drug administration program are only some of the issues noted during surveys of gold miners with malaria.16 One travel medicine related intervention being tested in “Malakit” a self-testing and self-treatment system meant to get effective therapy delivered to difficult to contact populations such as miners.17
In Africa, mining-associated malaria is noted when new populations move into gold mining areas such as West Africa (Nigeria, Ghana). The largest recent epidemic in expatriate miners was noted in China when 874 cases (95% P. falciparum) were seen in Shanglin County 99% of whom had returned from gold mining operations in Ghana.18 This epidemic was largely noted because the Ghanaian government had moved against quasi-legal mining operations driving many expatriates back to their home countries. It is likely that this level of infection (22% of those screened by microscopy) was this population baseline as many (34%) were asymptomatic and the epidemic was only accurately observed by the sudden shift of the miners from Ghana to China. It is likely that such high levels of infection also exist in local work forces as well as other national expatriate groupings as the example from Thai miners returned from Nigeria shows in four of six persons with falciparum infections and one death.19
Malaria epidemics are associated with mining operations on three continents despite great differences in populations, vectors, and ecology. Commonalities include large mobile populations of marginalized men with little previous experience with malaria working under difficult conditions. Their difficulties are compounded by the mining activity often being illegal and therefore outside of regular governmental health services, which are often avoided to escape official attention. Their indifferent use of antimalarial drugs only increases the number of suppressed and potentially drug-resistant infections. More formal mining industry operations in the tropics still experience malaria epidemics such as the predictable post–Christmas leave outbreaks observed at the Ok Tedi mine in Papua New Guinea by fly in–fly out workers whose exposure is in their home villages as opposed to the well-controlled mine site in the mountains.20 Other New Guinea mines such as on Lihir Island are making good progress toward malaria elimination on a small island shared with a relatively small civilian population.21 Improved forms of malaria chemotherapy capable of long-lasting prophylaxis, elimination of hypnozoites and transmission blocking would be of great use in mitigating malaria problems associated with mining especially in areas dominated by relapsing malaria in South America. One can hope that the newly registered 8-aminoquinoline, tafenoquine can be adapted to such practical purposes.22
ACKNOWLEDGMENTS
We acknowledge Krongthong Thimasarn, formerly Director of Malaria Division, Department of Communicable Disease Control, Thai Ministry of Public Health and Malaria Regional Advisor, WHO SEARO, Delhi, India, for useful discussion and two photos. We also acknowledge Juan F. Sanchez of the Johns Hopkins Bloomberg School of Public Health for providing a photo of mining activity in Peru as well as medical librarians who have unselfishly provided data and found papers for this manuscript especially the librarians at the Australian Defence Force Library at Gallipoli Barracks, Queensland.
REFERENCES
- 1.Konchom S, Singhasivanon P, Kaewkungwal J, Chuprapawan S, Thimasarn K, Kidson C, Yimsamran S, Rojanawatsirivet C, 2005. Chronicle of malaria epidemics in Thailand, 1980–2000. Southeast Asian J Trop Med Public Health 36: 64–67. [PubMed] [Google Scholar]
- 2.Wongsrichanalai C, Sirichaisinthop J, Karwacki JJ, Congpuong K, Miller RS, Pang L, Thimasarn K, 2001. Drug resistant malaria on the Thai-Myanmar and Thai-Cambodian borders. Southeast Asian J Trop Med Public Health 32: 41–49. [PubMed] [Google Scholar]
- 3.Durham J, Battle K, Rickart K, Shanks GD, 2014. Geographical origin of post-landmine injury malaria infections. Disaster Med Public Health Prep 8: 417–421. [DOI] [PubMed] [Google Scholar]
- 4.Wongsrichanalai C, Pickard AL, Wernsdorfer WH, Meshnick SR, 2002. Epidemiology of drug-resistant malaria. Lancet Infect Dis 2: 209–218. [DOI] [PubMed] [Google Scholar]
- 5.Nyunt MH, Wang B, Aye KM, Aye KH, Han J-H, Lee S-K, Han KT, Htut Y, Han E-T, 2017. Molecular surveillance of artemisinin resistance falciparum malaria among migrant goldmine workers in Myanmar. Malar J 16: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Castellanos A, Chaparro-Narváez P, Morales-Plaza CD, Alzate A, Padilla J, Arévalo M, Herrera S, 2016. Malaria in gold-mining areas in Colombia. Mem Inst Oswaldo Cruz 111: 59–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Douine M, Musset L, Corlin F, Pelleau S, Pasquier J, Mutricy L, Adenis A, Djossou F, Brousse P, Perotti F, 2016. Prevalence of Plasmodium spp. in illegal gold miners in French Guiana in 2015: a hidden but critical malaria reservoir. Malar J 15: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Feachem RG, Chen I, Akbari O, Bertozzi-Villa A, Bhatt S, Binka F, Boni MF, Buckee C, Dieleman J, Dondorp A, 2019. Malaria eradication within a generation: ambitious, achievable, and necessary. Lancet 394: 1056–1112. [DOI] [PubMed] [Google Scholar]
- 9.Mosnier E, Roux E, Cropet C, Lazrek Y, Moriceau O, Gaillet M, Mathieu L, Nacher M, Demar M, Odonne G, 2020. Prevalence of Plasmodium spp. in the Amazonian Border Context (French Guiana–Brazil): associated factors and spatial distribution. Am J Trop Med Hyg 102: 130–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sanchez JF, Carnero AM, Rivera E, Rosales LA, Baldeviano GC, Asencios JL, Edgel KA, Vinetz JM, Lescano AG, 2017. Unstable malaria transmission in the southern Peruvian Amazon and its association with gold mining, Madre de Dios, 2001–2012. Am J Trop Med Hyg 96: 304–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grillet ME, Moreno JE, Hernández-Villena JV, Vincenti-González MF, Noya O, Tami A, Paniz-Mondolfi A, Llewellyn M, Lowe R, Escalante AA, 2021. Malaria in southern Venezuela: the hottest hotspot in Latin America. PLoS Negl Trop Dis 15: e0008211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Arisco NJ, Peterka C, Castro MC, 2021. Cross-border malaria in northern Brazil. Malar J 20: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pacheco MA, Forero-Peña DA, Schneider KA, Chavero M, Gamardo A, Figuera L, Kadakia ER, Grillet ME, Oliveira-Ferreira J, Escalante AA, 2020. Malaria in Venezuela: changes in the complexity of infection reflects the increment in transmission intensity. Malar J 19: 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mathieu LC, Cox H, Early AM, Mok S, Lazrek Y, Paquet J-C, Ade M-P, Lucchi NW, Grant Q, Udhayakumar V, 2020. Local emergence in Amazonia of Plasmodium falciparum k13 C580Y mutants associated with in vitro artemisinin resistance. eLife 9: e51015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Louzada J, de Almeida NCV, de Araujo JLP, Silva J, Carvalho TM, Escalante AA, Oliveira-Ferreira J, 2020. The impact of imported malaria by gold miners in Roraima: characterizing the spatial dynamics of autochthonous and imported malaria in an urban region of Boa Vista. Mem Inst Oswaldo Cruz 115: e200043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Murta FLG, Marques LLG, Santos APC, Batista TSB, Mendes MO, Silva ED, da Silva Neto AV, Fabiano MP, Rodovalho SR, Monteiro WM, 2021. Perceptions about malaria among Brazilian gold miners in an Amazonian border area: perspectives for malaria elimination strategies. Malar J 20: 286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Douine M, Sanna A, Galindo M, Musset L, de Santi VP, Marchesini P, Magalhaes ED, Suarez-Mutis M, Hiwat H, Nacher M, 2018. Malakit: an innovative pilot project to self-diagnose and self-treat malaria among illegal gold miners in the Guiana shield. Malar J 17: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li Z, Yang Y, Xiao N, Zhou S, Lin K, Wang D, Zhang Q, Jiang W, Li M, Feng X, 2015. Malaria imported from Ghana by returning gold miners, China, 2013. Emerg Infect Dis 21: 864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Matsee W, Chatapat L, Chotivanich K, Piyaphanee W, 2018. Case report: a cluster of Plasmodium falciparum malaria cases among Thai workers in Gembu, Nigeria. Am J Trop Med Hyg 99: 623–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shanks G, Edstein M, Kereu R, Spicer P, Rieckmann K, 1993. Postexposure administration of halofantrine for the prevention of malaria. Clin Infect Dis 17: 628–631. [DOI] [PubMed] [Google Scholar]
- 21.Mitjà O, Paru R, Selve B, Betuela I, Siba P, De Lazzari E, Bassat Q, 2013. Malaria epidemiology in Lihir Island, Papua New Guinea. Malar J 12: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Haston JC, Hwang J, Tan KR, 2019. Guidance for using tafenoquine for prevention and antirelapse therapy for malaria—United States, 2019. MMWR 68: 1062. [DOI] [PMC free article] [PubMed] [Google Scholar]