Abstract
Background:
Familiarity among cardiac surgery team members may be an important contributor to better outcomes and thus serve as a target for enhancing outcomes.
Methods:
Adult cardiac surgical procedures (n=4445) involving intraoperative providers were evaluated at a tertiary hospital between 2016–20. Team familiarity (mean of prior cardiac surgeries performed by participating surgeon/non-surgeon pairs within 2 years before the operation) were regressed on cardiopulmonary bypass duration (primary - an intraoperative measure of care efficiency) and postoperative complication outcomes (major morbidity, mortality), adjusting for provider experience, surgeon 2-year case volume prior to the surgery, case start time, weekday and perioperative risk factors. The relationship between team familiarity and outcomes was assessed across predicted risk strata.
Results:
Median (IQR) cardiopulmonary bypass duration was 132 minutes (91–192), and 698 (15.7%) patients developed major postoperative morbidity. The relationship between team familiarity and cardiopulmonary bypass duration significantly differed across predicted risk strata (p=0.0001). High (relative to low) team familiarity was associated with reduced cardiopulmonary bypass duration for medium-risk (−24min) and high-risk (−27min) patients. Increasing team familiarity was not significantly associated with the odds of major morbidity and mortality.
Conclusions:
Team familiarity, which was predictive of improved intraoperative efficiency without compromising major postoperative outcomes, may serve as a novel quality improvement target in the setting of cardiac surgery.
INTRODUCTION
Significant variation in clinical outcomes persists in the setting of cardiac surgery despite nearly universal participation in The Society of Thoracic Surgeons Adult Cardiac Surgery Database, advancements in technology, and adoption of safety and procedural checklists. Prior work has shown that only 2% of interhospital variation in outcomes is explained through existing registry data.1 Other high-risk sectors outside of medicine (e.g., nuclear power plants, off-shore oil rigs, civil aviation) have highlighted the importance of evaluating non-technical skills, including communication and teamwork, as mechanisms for assuring competency and achieving key outcomes given the complexity and interconnectedness of tasks across a number of integral team members. The conduct of cardiac surgery relies heavily on care coordination across a number of team members (surgeons, anesthesiologists, perfusionists, physician assistants, scrub nurses), thus supporting the usefulness of advancing measurement of intraoperative teamwork in this setting.
Surgical teamwork comprises three important and interrelated elements; information exchange, shared understanding and the coordination of team activities.2 Team members who have previously worked together in the operating room may be more likely to effectively communicate and function cohesively.3 Indeed, prior work has documented the role of team training exercises on advancing non-technical skills,4 enhancing team member satisfaction,5 and reducing patient mortality.6 While teams that function well together may achieve improved efficiency and safety scores, less is known about the impact of team familiarity on intra- and postoperative outcomes. Furthermore, the leveraging of registry data as a proxy for surgical team non-technical skills is underutilized and may provide a leading measure of team function in every surgical case without the need for human observers.
With this in mind, the present observational, single-center study focused on associating team familiarity (the mean of prior cardiac surgeries performed by surgeon/non-surgeon pairs within 2 years before the operation) with intraoperative process of care efficiency and postoperative major complications.
METHODS
Institutional Review Board approval (HUM00162272) was obtained with waiver of patient consent. The study team followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines throughout the conduct of this study.7 Data were extracted from The Society of Thoracic Surgeons Adult Cardiac Surgery Database (STS-ACSD) and our institution’s local perioperative anesthesia database (Centricity ®, GE Healthcare, Barrington, IL).
Study Population
The study population included both male and female adult patients ≥18 years) undergoing cardiac surgery including valve, coronary artery bypass, and aortic procedures in isolation or combination at one academic medical center from January 2016 to June 2020. Only the index operation was used for patients undergoing multiple repeated procedures meeting inclusion criteria.
Team Familiarity Measure
For ease of interpretation, a single composite team familiarity score for each surgical procedure was derived via a multi-step process. First, the primary intraoperative providers involved in the cardiac surgical operation were identified, defined as the cardiac surgeon attending of record, as well as the anesthesiology attending, perfusionist, physician assistant, scrub nurse, and surgical resident (if present) signed into the operation for the greatest number of minutes. Next, the number of prior cardiac surgical procedures were tabulated for each surgeon/non-surgeon pair (e.g., surgeon/anesthesiologist, surgeon/perfusionist) performed together during the 2 years prior to the surgery date. Finally, the values for each provider pair were averaged to arrive at the composite team familiarity score, which was stratified into terciles: low (1.0–17.0 prior operations within 2 years), medium (17.2–27.2), and high (>27.2). Similar measures of team familiarity have been used in the intraoperative setting including breast,8 orthopaedic,9 and cardiac surgery.10
Intraoperative and Postoperative Study Outcomes
The duration of cardiopulmonary bypass (a measure of care efficiency) served as the primary intraoperative study outcome. Cardiopulmonary bypass duration was selected, given this segment of the cardiac surgical case (including the initiation and cessation of bypass) is the critical portion involving teamwork across all intraoperative team members. In addition, duration of bypass is less biased by factors dependent primarily on a single team member (e.g., anesthetic induction, prepping and draping) or outside of the control of the intraoperative team (e.g., delay in patient transport from the operating room related to intensive care unit bed availability). In cases with multiple cardiopulmonary bypass events, the duration was calculated as the cumulative number of minutes across all cardiopulmonary bypass events. Secondary binary outcomes included a composite of mortality and STS major complications (renal failure, prolonged ventilation, deep sternal wound infection, stroke, unplanned reoperation), as well as each individual component of the composite secondary outcome (eMethods). Finally, continuous secondary outcomes included intensive care unit (ICU) hours and ventilation hours.
Covariates
To provide risk adjustment for studying the association between team familiarity and outcomes, provider, patient, and surgical characteristics were included into a multivariable model. To distinguish between team familiarity and provider seniority, adjustments for provider seniority were made by including the number of years since the completion of each provider’s clinical training as a study covariate. Similarly, to distinguish between team familiarity and provider experience, adjustments for experience were made by including the number of cardiac surgical procedures performed by each provider during the prior 2 years before the surgery date. To account for potential differences in clinical workflow between cases performed with and without surgical residents, the presence of a surgical resident was also included as a single binary covariate. A priori patient demographics (including sex), comorbidity, and preoperative characteristics, as well as characteristics of the type of surgical procedure performed were captured as described in Table 1. Using covariate data, the EuroSCORE-II values were calculated for all patients, as has been previously used for risk adjustment among cardiac surgical procedures.11,12
Table 1 –
Study Cohort Characteristics: Overall and Trend by Team Familiarity Terciles
| Overall Team Familiarity Terciles | |||||
|---|---|---|---|---|---|
| Variable | Overall | Low (1.0–17.0) | Medium (17.2–27.2) | High (>27.2) | p-trend |
| Frequency | 4445 | 1474 | 1486 | 1485 | |
| Provider Experience, years | |||||
| Surgeon | 12.18 [5.83, 21.92] | 6.70 [1.45, 14.85] | 13.82 [10.40, 21.30] | 20.94 [9.16, 24.28] | <.0001 |
| Anesthesiologist | 4.37 [2.16, 10.55] | 4.10 [2.01, 10.63] | 4.38 [2.20, 10.31] | 4.65 [2.30, 10.62] | 0.0829 |
| Perfusionist | 4.22 [1.31, 16.78] | 3.72 [0.90, 20.50] | 4.42 [1.39, 17.50] | 4.34 [1.66, 10.45] | 0.0249 |
| Physician Assistant | 20.55 [5.25, 26.66] | 19.08 [4.29, 25.66] | 20.11 [4.73, 26.79] | 24.21 [12.85, 27.09] | <.0001 |
| Surgical resident experience (if present) | 5.61 [2.82,6.88] | 5.37 [2.70,6.65] | 5.62 [2.80,6.99] | 5.73 [2.98,6.91] | 0.0185 |
| Surgical Resident Present, % yes | 2507 (56.4) | 757 (51.4) | 900 (600.6) | 850 (57.2) | <.0001 |
| Surgeon volume 2 yr prior to the surgery (Median [IQR]) | 355.00 [324.00, 435.00] | 326.00 [177.00, 368.50] | 387.00 [339.00, 447.75] | 370.00 [337.00, 436.00] | <.0001 |
| EuroSCORE-II (Median [IQR]) (%) | 3.91 [1.65,9.54] | 4.63 [1.99, 10.33] | 3.61 [1.52,9.40] | 3.58 [1.51,9.22] | <.0001 |
| <.0001 | |||||
| low (<2.2%) | 1485 (33.4) | 415 (28.2) | 522 (35.1) | 548 (36.9) | |
| medium (2.2–6.9%) | 1478 (33.3) | 519 (35.2) | 489 (32.9) | 470 (31.6) | |
| high (>6.9 %) | 1482 (33.3) | 540 (36.6) | 475 (32.0) | 467 (31.4) | |
| Demographics | |||||
| Age (median [IQR]) | 63.00 [54.00, 71.00] | 64.00 [55.00, 71.00] | 64.00 [54.00, 71.00] | 63.00 [52.00, 71.00] | 0.0192 |
| Male, % yes | 2921 (65.7) | 1039 (70.5) | 938 (63.1) | 944 (63.6) | <.0001 |
| Body Surface Area, m2 | |||||
| Median [IQR] | 2.04 [1.86, 2.22] | 2.06 [1.89, 2.25] | 2.03 [1.85, 2.21] | 2.02 [1.84, 2.21] | 0.0001 |
| 0.0194 | |||||
| <1.6 | 223 (5.0) | 61 (4.1) | 86 (5.8) | 76 (5.1) | |
| 1.6–1.8 | 636 (14.3) | 191 (13.0) | 218 (14.7) | 227 (15.3) | |
| 1.8–2.0 | 1091 (24.5) | 343 (23.3) | 359 (24.2) | 389 (26.2) | |
| >=2.0 | 2495 (56.1) | 879 (59.6) | 823 (55.4) | 793 (53.4) | |
| Risk Factors | |||||
| Diabetes on insulin, % yes | 399 (9.0) | 146 (9.9) | 127 (8.5) | 126 (8.5) | 0.1771 |
| Poor Mobility, % yes | <.0001 | ||||
| None | 1916 (43.1) | 722 (49.0) | 614 (41.3) | 580 (39.1) | |
| <6 sec | 1733 (39.0) | 527 (35.8) | 599 (40.3) | 607 (40.9) | |
| >=6 sec | 796 (17.9) | 225 (15.3) | 273 (18.4) | 298 (20.1) | |
| Cardiovascular Disease | |||||
| Renal Impairment, % yes | 0.7434 | ||||
| Normal | 2326 (52.3) | 789 (53.5) | 770 (51.8) | 767 (51.6) | |
| Moderately Impaired Renal Function (50–85 ml/min) | 1602 (36.0) | 519 (35.2) | 546 (36.7) | 537 (36.2) | |
| Severely Impaired Renal Function (<50 ml/min) off Dialysis | 412 (9.3) | 138 (9.4) | 132 (8.9) | 142 (9.6) | |
| On Dialysis | 105 (2.4) | 28 (1.9) | 38 (2.6) | 39 (2.6) | |
| Chronic Lung Disease (moderate and severe), % yes | 287 (6.5) | 111 (7.5) | 94 (6.3) | 82 (5.5) | 0.0263 |
| Extracardiac Arteriopathy, % yes | <.0001 | ||||
| None | 3208 (72.2) | 1004 (68.1) | 1062 (71.5) | 1142 (76.9) | |
| Peripheral Arterial Disease | 615 (13.8) | 262 (17.8) | 188 (12.7) | 165 (11.1) | |
| Carotid Occlusion or >50% Stenosis | 622 (14.0) | 208 (14.1) | 236 (15.9) | 178 (12.0) | |
| Active Endocarditis, % yes | 182 (4.1) | 67 (4.5) | 50 (3.4) | 65 (4.4) | 0.8202 |
| Canadian Cardiovascular Society Class 4 angina, % yes | 700 (15.7) | 312 (21.2) | 203 (13.7) | 185 (12.5) | <.0001 |
| NY Heart Association Class, % yes | 0.0026 | ||||
| None | 2573 (57.9) | 920 (62.4) | 813 (54.7) | 840 (56.6) | |
| Class I | 150 (3.4) | 48 (3.3) | 52 (3.5) | 50 (3.4) | |
| Class II | 779 (17.5) | 217 (14.7) | 279 (18.8) | 283 (19.1) | |
| Class III | 613 (13.8) | 194 (13.2) | 215 (14.5) | 204 (13.7) | |
| Class IV | 330 (7.4) | 95 (6.4) | 127 (8.5) | 108 (7.3) | |
| Left Ventricular Ejection Fraction, % yes | 0.3466 | ||||
| >50% | 3434 (77.3) | 1137 (77.1) | 1133 (76.2) | 1164 (78.4) | |
| 31–50% | 644 (14.5) | 229 (15.5) | 218 (14.7) | 197 (13.3) | |
| 21–30% | 157 (3.5) | 50 (3.4) | 57 (3.8) | 50 (3.4) | |
| <20% | 210 (4.7) | 58 (3.9) | 78 (5.2) | 74 (5.0) | |
| Recent Myocardial Infarction (within 21d), % yes | 1589 (35.7) | 571 (38.7) | 527 (35.5) | 491 (33.1) | 0.0013 |
| Pulmonary Hypertension, % yes | <.0001 | ||||
| Normal or | 2244 (50.5) | 766 (52.0) | 718 (48.3) | 760 (51.2) | |
| Unknown | |||||
| Moderate (Systolic 31–55mmHg) | 1662 (37.4) | 577 (39.1) | 567 (38.2) | 518 (34.9) | |
| Severe (Systolic >55mmHg) | 539 (12.1) | 131 (8.9) | 201 (13.5) | 207 (13.9) | |
| Acuity, % yes | <.0001 | ||||
| Elective | 3247 (73.0) | 973 (66.0) | 1109 (74.6) | 1165 (78.5) | |
| Emergent | 222 (5.0) | 133 (9.0) | 58 (3.9) | 31 (2.1) | |
| Urgent | 976 (22.0) | 368 (25.0) | 319 (21.5) | 289 (19.5) | |
| Previous Cardiac Surgery, % yes | 1913 (43.0) | 617 (41.9) | 612 (41.2) | 684 (46.1) | 0.0208 |
| Procedure | |||||
| Surgery Type, % yes | <.0001 | ||||
| Isolated | 669 (15.1) | 304 (20.6) | 221 (14.9) | 144 (9.7) | |
| Single, Non Coronary Artery Bypass Grafting | 2460 (55.3) | 799 (54.2) | 781 (52.6) | 880 (59.3) | |
| 2–3 procedures | 882 (19.8) | 235 (15.9) | 324 (21.8) | 323 (21.8) | |
| Other | 434 (9.8) | 136 (9.2) | 160 (10.8) | 138 (9.3) | |
| Surgery on Thoracic Aorta, % yes | 1147 (25.8) | 572 (38.8) | 299 (20.1) | 276 (18.6) | <.0001 |
| Day of the Week (%) | |||||
| Sunday | 101 (2.3) | 50 (3.4) | 35 (2.4) | 16 (1.1) | |
| Monday | 853 (19.2) | 314 (21.3) | 292 (19.7) | 247 (16.6) | |
| Tuesday | 941 (21.2) | 276 (18.7) | 264 (17.8) | 401 (27.0) | |
| Wednesday | 806 (18.1) | 342 (23.2) | 314 (21.1) | 150 (10.1) | |
| Thursday | 833 (18.7) | 216 (14.7) | 262 (17.6) | 355 (23.9) | |
| Friday | 791 (17.8) | 223 (15.1) | 276 (18.6) | 292 (19.7) | |
| Saturday | 120 (2.7) | 53 (3.6) | 43 (2.9) | 24 (1.6) | |
| Procedure Start Time (%) | <.0001 | ||||
| Afternoon | 924 (20.8) | 315 (21.4) | 352 (23.7) | 257 (17.3) | |
| Evening | 103 (2.3) | 50 (3.4) | 38 (2.6) | 15 (1.0) | |
| Morning | 3324 (74.8) | 1048 (71.1) | 1071 (72.1) | 1205 (81.1) | |
| Overnight | 94 (2.1) | 61 (4.1) | 25 (1.7) | 8 (0.5) | |
| Year (%) | <.0001 | ||||
| 2016 | 521 (11.7) | 143 (9.7) | 171 (11.5) | 207 (13.9) | |
| 2017 | 1016 (22.9) | 295 (20.0) | 354 (23.8) | 367 (24.7) | |
| 2018 | 1189 (26.7) | 479 (32.5) | 342 (23.0) | 368 (24.8) | |
| 2019 | 1214 (27.3) | 404 (27.4) | 457 (30.8) | 353 (23.8) | |
| 2020 | 505 (11.4) | 153 (10.4) | 162 (10.9) | 190 (12.8) | |
Poor Mobility - Measured using the average of three 5-meter walk tests
Chronic Lung Disease - long term use of bronchodilators or steroids for lung disease
Active Endocarditis - patient still on antibiotic treatment for endocarditis at time of surgery
To test the trend of these variables across the ordered team familiarity terciles, the Cochran-Armitage trend tests were used for the binary variables, Cochran-Mantel_Haenszel tests were used for the categorical variables with more than two levels, Jonckheere-Terpstra trend tests were used for the continuous variables.
Statistical Analysis
Categorical variables were presented as N (%) and continuous variables as median and interquartile range (IQR). To test trends across the team familiarity terciles (low, medium and high), Cochran-Armitage, Cochran-Mantel-Haenszel, and Janckheere-Terpstra tests for binary, multiple-level categorical, and continuous variables were respectively used. Data with <5% missingness were imputed to the mean for continuous variables and to the lowest risk level for categorical variables. Data with >5% missingness was retained as a missing level or a missing indicator. To assess for patterns within provider pairings, ramer’s V statistics were calculated for each surgeon/non-surgeon provider pairing, ranging from 0 (completely random surgeon/non-surgeon pairings) to 1 (perfect association between pairs).
Next, risk-adjusted associations between team familiarity and outcomes were analyzed via generalized linear regression models. The models adjusted for patients’ risk using EuroSCORE-II, admission acuity, STS procedure type, provider experience (surgeon, anesthesiologist, perfusionist, physician assistant, surgical residents if present), surgeon 2-year case volume prior to the surgery, procedure start time of the day, and procedure day of week, an indicator of surgical residents’ presence. Team familiarity scores were modeled as a continuous variable, and where appropriate for ease of interpretation, terciles (low, medium, high). To assess the influence of underlying surgical risk on the association between team familiarity and outcomes, the interaction between team familiarity and EuroSCORE-II risk strata were tested as terciles (low, medium and high risk). All analyses were performed in SAS version 9.4 (SAS Institute, Cary, NC) and R version 3.5.2.
Sensitivity Analyses
To assess the robustness of study results, a sensitivity analysis was performed for all study outcomes, in which primary intraoperative providers were defined as those signed into the case while on cardiopulmonary bypass (as opposed to the entire case) for the greatest number of minutes. Additionally, to assess the potential differential impact of surgeon/non-surgeon pairs across non-surgeon roles, an analysis including familiarity scores for each surgeon/non-surgeon pair as separate covariates (i.e., surgeon/anesthesiologist, surgeon/perfusionist, surgeon/scrub nurse, surgeon/physician assistant, and surgeon/surgery resident) was performed. Finally, a simplified analysis excluding consideration of providers in training (i.e., surgical residents) was performed.
Subgroup Analyses
To assess the generalizability of study results, multiple subgroup analyses were performed for all study outcomes, including (i) cases with a start time between 07:00 and noon in which intraoperative handovers were rare; (ii) cases stratified by EuroSCORE-II weight of surgical intervention; and (iii) cases stratified by those performed on the thoracic aorta versus those which were not.
RESULTS
Study Population - Baseline Characteristics
The study cohort comprised 4,445 adult cardiac surgical procedures, Table 1. The study population consisted of a median (IQR) age of 63 (54–71) years; 34.3% were women, and the median (IQR) EuroSCORE II predicted risk of mortality was 3.9% (1.7–9.5%). When partitioned into risk strata, EuroSCORE-II risk was <2.2% for the low risk strata, 2.2–6.9% for moderate risk, and >6.9% for the high risk strata. Valve procedures were performed on 1,497 (33.7%) patients while procedures on the thoracic aorta occurred among 1,147 (25.8%) of patients.
Team Familiarity Measures
Cardiac surgical procedures were performed by the following providers, including cardiac surgeons (n=12), anesthesiologists (n=24), perfusionists (n=25), physician assistants (n=13), scrub nurses (n=72), and surgical residents (n =77 across 2,507 cases performed with surgical residents). Median (IQR) team familiarity for each surgeon/non-surgeon pair included surgeon-anesthesiologist (15 [9–22]), surgeon-perfusionist (18 [8–29]), surgeon-physician assistant (33 [17–58]), surgeon-scrub nurse (12 [5–26]), and surgeon-surgery resident (11 [5–21]) if present. Weak correlations were observed between surgeon and anesthesiologist pairings ramer’s V statistic = 0.104), perfusionists (0.100), physician assistants (0.173), and scrub nurses (0.269), whereas moderate correlations were observed between surgeon and surgery resident pairings (0.347).
Intraoperative and Postoperative Study Outcomes
The median (IQR) cardiopulmonary bypass duration was 132 (91–192) minutes, Table 2. Thirty-day mortality occurred among 2.3% of patients. Major morbidity occurred among 15.7% of patients, including prolonged ventilation >24 hours (12.3%), postoperative renal failure (4.1% total; among these, 56.4% receiving renal replacement therapy), unplanned reoperation (2.5%), stroke (2.0%), and deep sternal wound infection (0.3%). Median (IQR) ICU length of stay was 56 (29–102) hours, and ventilation duration was 5.2 (3.1–12.7) hours.
Table 2:
Study Outcomes: Overall and Trend by Team Familiarity Terciles
| Overall Team Familiarity Terciles | |||||
|---|---|---|---|---|---|
| Overall | Low | Medium | High | p-trend | |
| Primary | |||||
| Cardiopulmonary Bypass Duration, minutes (Median [IQR]) | 132.00 [91.00, 192.00] | 162.50 [114.00, 222.00] | 122.00 [87.00, 177.00] | 113.00 [80.00, 169.00] | <.0001 |
| Secondary | |||||
| Major Morbidity (%) | 698 (15.7) | 261 (17.7) | 217 (14.6) | 220 (14.8) | 0.0309 |
| Prolonged Ventilation | 545 (12.3) | 210 (14.2) | 170 (11.4) | 165 (11.1) | 0.0094 |
| Deep Sternal Wound Infection | 15 (0.3) | 7 (0.5) | 4 (0.3) | 4 (0.3) | 0.3357 |
| Permanent Stroke | 91 (2.0) | 38 (2.6) | 24 (1.6) | 29 (2.0) | 0.2311 |
| Reoperation | 113 (2.5) | 49 (3.3) | 33 (2.2) | 31 (2.1) | 0.0328 |
| Renal Failure | 181 (4.1) | 69 (4.7) | 55 (3.7) | 57 (3.8) | 0.2469 |
| Acute Kidney Injury (Stage 3) | 180 (4.0) | 69 (4.7) | 55 (3.7) | 56 (3.8) | 0.2099 |
| Creatinine Clearance (Median [IQR]) | 87.96 [65.95, 115.84] | 89.17 [66.36, 116.06] | 87.55 [66.00, 115.83] | 87.34 [65.50, 115.69] | 0.3358 |
| Intensive Care Unit (ICU) Duration, hours (Median [IQR]) | |||||
| Initial | 56.45 [29.20, 102.30] | 66.40 [34.10, 113.30] | 53.00 [28.50, 98.25] | 53.45 [28.60, 101.47] | 0.0134 |
| Total (+any additional ICU hrs) | 61.75 [29.67, 110.67] | 68.10 [36.70, 115.70] | 54.80 [28.90, 100.60] | 57.05 [28.80, 113.45] | 0.0451 |
| 30 day Mortality | 101 (2.3) | 32 (2.2) | 28 (1.9) | 41 (2.8) | |
Team Familiarity Terciles: Low (<18 prior operations within 2 years), Medium (18–28), High (>28)
Major morbidity includes any of the following: renal failure, prolonged ventilation, deep sternal wound infection, stroke, unplanned reoperation
Creatinine clearance (ml/min) = (140-age (years)) × weight (kg) × (0.85 if female) / [72 × serum creatinine (mg/dl)]
Associations with Study Outcomes
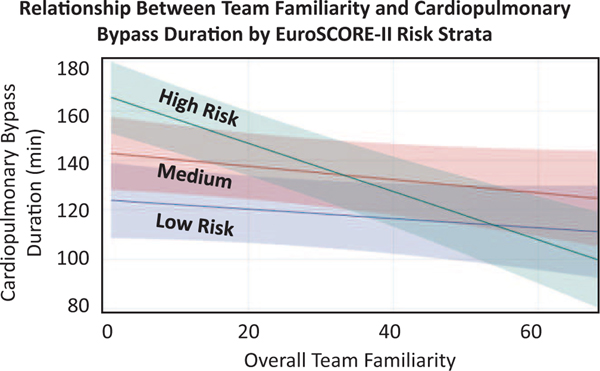
The relationship between team familiarity and cardiopulmonary bypass duration significantly differed across strata of predicted risk (p=0.0001). Each unit increase in team familiarity was associated with 0.27 fewer minutes (p=0.077) and 0.98 fewer minutes (p<.0001) perfusion time for medium-risk and high-risk patients respectively. Relative to low team familiarity tercile, the high team familiarity tercile was associated with a decreased cardiopulmonary bypass duration of 24.0 minutes for medium-risk patients and a decreased duration of 27.4 minutes for high-risk patients (Figure 1).
Figure 1.
The composite overall team familiarity score is represented on the x-axis, and cardiopulmonary bypass duration on the y-axis. Patient risk was estimated using the EuroSCORE-II mortality prediction model, with patients stratified as low (<12.2%), medium (2.2%−6.9%) and high (>6.9%). The relationship between team familiarity and cardiopulmonary bypass duration significantly differed across strata of predicted risk, p=0.0001. The risk adjusted variables were fixed at the following values: surgeon experience=13.1, anesthesiologist experience=7.5, perfusionist experience=10.2, PA experience=17.6, surgeon volume=360, resident absence=1, admission acuity=emergent, STS procedure type=valve, case start time=afternoon, weekdays=Friday.
Increasing one-unit of team familiarity was not significantly associated with renal failure (OR=0.991, p=0.304), ICU hours (−0.173 hour decrease, p = 0.346) or 30-day mortality (OR=0.987, p=0.243). Increasing team familiarity was associated with ventilation hours (−0.46 hour decrease, p=0.0174) as well as a 3.4% lower odds of major morbidity (OR=0.966, p=0.0014) for patients at lower EuroSCORE-II risk strata, 1.8% increasing odds of major morbidity (OR=1.018, p=0.0138) for patients at medium EuroSCORE-II risk strata, although not major morbidity (OR=0.992, p=0.186) among patients at higher EuroSCORE-II risk strata, Table 3.
Table 3 –
Risk-Adjusted Relationship between Team Familiarity and Study Outcomes by EuroSCORE-II Risk
| Overall | EuroSCORE-II Strata | |||||||
|---|---|---|---|---|---|---|---|---|
| Low (<2.2%) | Medium (2.2%−6.9%) | High (>6.9%) | ||||||
| Outcome | Measure of Association# | p-value | Measure of Association# | p-value | Measure of Association# | p-value | Measure of Association# | p-value |
| Primary | ||||||||
| Cardiopulmonary Bypass Duration, minutes | −0.189 | 0.213 | −0.272 | 0.077 | −0.978 | <.0001 | ||
| Secondary | ||||||||
| Intensive Care Units, hours | −0.173 | 0.346 | ||||||
| Ventilation hours | −0.461 | 0.017 | ||||||
| Major Morbidity (%) | 0.966 | 0.001 | 1.018 | 0.014 | 0.992 | 0.186 | ||
| Prolonged Ventilation | 0.956 | 0.002 | 1.021 | 0.012 | 0.996 | 0.494 | ||
| Deep Sternal Wound Infection | 0.977 | 0.505 | ||||||
| Permanent Stroke | 0.987 | 0.691 | 1.025 | 0.190 | 0.965 | 0.049 | ||
| Reoperation | 0.981 | 0.082 | ||||||
| Renal Failure | 0.991 | 0.304 | ||||||
| Acute Kidney Injury (Stage 2 or 3) | 0.993 | 0.259 | ||||||
| Acute Kidney Injury (Stage 3) | 0.991 | 0.272 | ||||||
| 30 day Mortality | 0.987 | 0.244 | ||||||
Measures of Association#: Beta coefficients are presented for continuous measures: cardiopulmonary bypass duration (minutes), intensive care unit (hours) and ventilation (hours). Odds ratios are presented for the binary outcome measures.
Major morbidity includes any of the following: renal failure, prolonged ventilation, deep sternal wound infection, stroke, unplanned reoperation
When the interaction term with EuroSCORE-II is significant, overall association is reported. When the interaction term with EuroSCORE-II is not significant, EuroSCORE-II strata specific associations are reported. Thus, some of the cells are shaded when not reported.
Sensitivity and Subgroup Analyses
A sensitivity analysis in which primary providers were defined as those signed into the case for the greatest number of minutes while on cardiopulmonary bypass yielded similar associations as with the primary analysis (Supplementary Table 1). Similar findings were additionally observed for procedure subgroups, including morning case starts (Supplementary Table 2), EuroSCORE-II surgical intervention weight strata (Supplementary Table 3), and procedures performed and not performed on the thoracic aorta (Supplementary Table 4). In a sensitivity analysis handling each surgeon/non-surgeon pairing as independent covariates rather than averaged, surgeon/anesthesiologist and surgeon/surgery resident pairings were observed as independently associated with cardiopulmonary bypass duration for high surgical risk strata, whereas other pairings were not (Supplementary Table 5). Finally, a sensitivity analysis using a simplified set of providers excluding providers in training (i.e., surgical residents) yield similar findings as the primary analysis (Supplementary Table 6).
DISCUSSION
This single-center observational study evaluated the relationship between team familiarity and intra- and postoperative outcomes in the setting of adult cardiac surgery. Importantly, higher terciles of team familiarity were associated with reduced cardiopulmonary bypass time, with stronger effect sizes among patients at higher baseline risk. In addition, higher team familiarity terciles were not associated with adverse postoperative outcomes. Together, these findings, which remained robust to multiple sensitivity and subgroup analyses, suggest that greater team familiarity is predictive of improved intraoperative efficiency (e.g., cardiopulmonary bypass duration) without compromising postoperative outcomes.
Findings from this study support efforts to evaluate measures reflecting surgical teamwork. First, this study: (i) extends the measurement of intraoperative team familiarity to broadly include members potentially impacting operating room efficiency and outcomes, and (ii) explores the role of team familiarity on clinical outcomes. Several prior studies have examined the number of procedures previously performed collaboratively as a metric of surgical team familiarity in breast,8 orthopaedic,9 and cardiac surgery.10 These studies have narrowly defined team familiarity to solely include attending surgeons, surgical fellows and assistants; nonetheless, these reports have reported significant relationships between familiarity and intraoperative processes (e.g., operative time). The only prior study within cardiac surgery found a relationship between familiarity and reduced cardiopulmonary bypass and cross clamp duration.10 By controlling for provider career experience and pairing attending cardiac surgeons with anesthesiologists, perfusionists, physician assistants, scrub nurses, and surgical residents our single center study: (i) mitigates the impact of confounding from individual clinician knowledge or skill acquired over time, (ii) supports the relationship between familiarity and cardiopulmonary bypass duration, (iii) extends prior reports by identifying no adverse impacts on postoperative outcomes.
In the current report, cardiopulmonary bypass duration - including transition periods during initiation and cessation of bypass - was selected as the primary intraoperative outcome. The rationale for selecting cardiopulmonary bypass duration was: (i) as a measure of efficiency and (ii) longer duration is associated with increased morbidity and mortality and represents a potential target to improve surgical outcomes. Beyond a plausible mechanistic linkage, cardiopulmonary bypass duration remains a clinically relevant study endpoint, previously reported to be associated with mortality13 and other adverse outcomes.14 Further, team-based interactions during (i) initiation of bypass, (ii) preparation for cessation, and (iii) cessation of bypass remain amenable to interventions aimed at enhancing team dynamics, including simulation training15 and establishment of verbal communication standards.16 Although team familiarity as measured in this study was simply a surrogate for team dynamics, the significant association between team familiarity and cardiopulmonary bypass duration (and especially among patients at highest preoperative risk) underscores the potential importance of team dynamics for influencing efficiency and safety metrics for cardiac surgery. Additionally, surgeon/non-surgeon familiarity during varying stages of a cardiac surgical procedure may have lesser or greater impact on case progression; in a sensitivity analysis examining each surgeon/non-surgeon provider role as a separate covariate, we observed surgeon/anesthesiologist and surgeon/surgery resident pairings as having the strongest independent association with cardiopulmonary bypass duration for high surgical risk strata compared to other pairs. Beyond the cardiopulmonary bypass phase, further work is needed to elucidate whether particular stages of a cardiac surgical operation may similarly exhibit differential associations with pairwise familiarity between two specific intraoperative team member roles. Finally, similar to the development of objective metrics for non-technical skills, the development of objective metrics for team dynamics and communication17 - and interventions for improving such metrics18 - represent promising areas for future studies.
This study importantly identified no significant associations between team familiarity and postoperative outcomes. Nonetheless, our findings highlight non-significant reductions in STS-ACSD reported outcomes, including post-operative renal failure. The 0.9% non-significant reduction in the degree of renal injury is likely attributable to its relationship with cardiopulmonary bypass duration.14 The mechanism underlying the relationship between team familiarity and duration of cardiopulmonary bypass is not elucidated from this present study. This finding may be due to 1) other factors such as surgical technique or postoperative ICU duration that may have a greater impact than team familiarity on other morbidities, or 2) the study sample size may be too small to detect a significant relationship between team familiarity and other morbid post-operative outcomes.
It is important to recognize a number of limitations associated with this study. First, while there is limited generalizability inherent with any single-center study, this study leverages data fields and definitions from the STS to enhance replicability of our findings. Second, as with any observational cohort study, there is a risk of unmeasured confounding. While this study accounts for previously identified patient and intraoperative risk factors, and the experience of surgeon and non-surgeon team members, other important unaccounted for covariates (e.g., team members performing other non-cardiac surgical procedures together, occasional non-random pairing of intraoperative team members) may distort the reported relationship between team familiarity and outcomes. Third, correlations between the scheduling of surgeon/non-surgeon provider pairings were weak to moderate, suggesting that provider pairings were frequently but not necessarily random. Sources of selection bias impacting the scheduling of provider pairs were beyond the scope of this study, but may have included patient requests, non-clinical scheduling requests (e.g., vacation, administrative days, conferences), and on-call preferences. Surgical residents may additionally select cases based on clinical training requirements, potentially explaining the slightly greater correlation between the scheduling of surgeon-surgeon resident pairs. Finally, while our measure of team familiarity includes surgeons and non-surgeons, other potentially impactful team members were not accounted for, including but not limited to non-surgical trainees.
Conclusions
In summary, this large single center study reports a significant relationship between team familiarity and reduced cardiopulmonary bypass duration without an impact on postoperative outcomes. Given the lack of reliable measures characterizing the impact of non-technical practices and outcomes during and following cardiac surgery, our results may inform the design of future quality improvement targets focused on intraoperative team interactions and interventions.
Supplementary Material
Team familiarity (the mean of prior cardiac surgeries performed by surgeon/non-surgeon pairs within 2 years before the operation) was independently associated with shorter cardiopulmonary bypass duration without impacting outcomes. The importance of this finding is that intraoperative team familiarity may serve as a novel quality improvement target given this measure was predictive of improved intraoperative efficiency without compromising postoperative outcomes.
Acknowledgments
Funding/Support:
This work was supported by the US National Institutes of Health - National Heart, Lung, and Blood Institute [grant number R01HL146619]. Donald S. Likosky and Francis D. Pagani receive extramural support from the Agency for Healthcare Research and Quality (AHRQ: R01HS026003). Donald S. Likosky serves as a consultant to the American Society of Extracorporeal Technology. Francis D. Pagani is a member of the scientific advisory board of FineHeart, Inc., member of the Data Safety Monitoring Board for Carmat, Inc., member of the Data Safety Monitoring Board for the NHLBI PumpKIN clinical trial, and Chair of The Society of Thoracic Surgeons, Intermacs Task Force. Michael R. Mathis receives extramural support from the NHLBI (K01HL141701). Steven J. Yule, PhD and Roger D. Dias, MD, MBA, PhD report extramural support from the NHLBI (R01HL126896), and National Aeronautics and Space Administration/ Translation Research Institute for Space Health during the conduct of the study. Steven J. Yule, PhD is a member of the Johnson & Johnson Institute Global Education Council. Allison M. Janda, M.D. reports extramural support from the NIH through a T32 Research Fellowship (5T32GM103730-07) during the conduct of the study. Sarah L. Krein, Ph.D., R.N. reports extramural support from the Department of Veterans Affairs, Health Services Research and Development Service (RCS 11-222) during the conduct of the study.
The opinions, beliefs, and viewpoints expressed by the authors do not necessarily reflect the opinions, beliefs, and viewpoints of the National Institutes of Health, or any of its employees, or The AHRQ or the US Department of Health and Human Services or the US Department of Veterans Affairs. Industry contributors have had no role in the study.
The authors gratefully acknowledge Alexandra Anastasopulos, M.D. (Department of Cardiac Surgery, Brigham and Women’s Hospital, Boston, MA) for her interpretation of the data.
Presented as a QuickShot Presentation at the 16th Annual Academic Surgical Virtual Congress (February 2-4, 2021). This Congress was held virtually.
Meeting/Presentations for Societal Papers:
The results of this manuscript have been previously presented on February 2, 2021 at the 2021 Academic Surgical Congress (ASC) Virtual Conference (held virtually) under the auspices of the Society of University Surgeons (SUS).
Footnotes
COI/Disclosure:
The authors report no conflicts of interest during the conduct of the study.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Brescia AA, Rankin JS, Cyr DD, Jacobs JP, Prager RL, Zhang M, et al. Determinants of Variation in Pneumonia Rates After Coronary Artery Bypass Grafting. Ann Thorac Surg. 2018. February;105(2):513–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yule S, Gupta A, Gazarian D, Geraghty A, Smink DS, Beard J, et al. Construct and criterion validity testing of the Non-Technical Skills for Surgeons (NOTSS) behaviour assessment tool using videos of simulated operations. Br J Surg. 2018. May;105(6):719–27. [DOI] [PubMed] [Google Scholar]
- 3.Bogdanovic J, Perry J, Guggenheim M, Manser T. Adaptive coordination in surgical teams: an interview study. BMC Health Serv Res. 2015. April 1;15:128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Robertson JM, Dias RD, Yule S, Smink DS. Operating Room Team Training with Simulation: A Systematic Review. J Laparoendosc Adv Surg Tech A. 2017. May;27(5):475–80. [DOI] [PubMed] [Google Scholar]
- 5.Arriaga AF, Gawande AA, Raemer DB, Jones DB, Smink DS, Weinstock P, et al. Pilot testing of a model for insurer-driven, large-scale multicenter simulation training for operating room teams. Ann Surg. 2014. March;259(3):403–10. [DOI] [PubMed] [Google Scholar]
- 6.Neily J, Mills PD, Young-Xu Y, Carney BT, West P, Berger DH, et al. Association between implementation of a medical team training program and surgical mortality. JAMA. 2010. October 20;304(15):1693–700. [DOI] [PubMed] [Google Scholar]
- 7.Elm E von, von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, et al. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies [Internet]. Vol. 335, BMJ. 2007. p. 806–8. Available from: 10.1136/bmj.39335.541782.ad [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maruthappu M, Duclos A, Zhou CD, Lipsitz SR, Wright J, Orgill D, et al. The impact of team familiarity and surgical experience on operative efficiency: a retrospective analysis. J R Soc Med. 2016. April;109(4):147–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xu R, Carty MJ, Orgill DP, Lipsitz SR, Duclos A. The teaming curve: a longitudinal study of the influence of surgical team familiarity on operative time. Ann Surg. 2013. December;258(6):953–7. [DOI] [PubMed] [Google Scholar]
- 10.Elbardissi AW, Duclos A, Rawn JD, Orgill DP, Carty MJ. Cumulative team experience matters more than individual surgeon experience in cardiac surgery. J Thorac Cardiovasc Surg. 2013. February;145(2):328–33. [DOI] [PubMed] [Google Scholar]
- 11.Nashef SAM, Roques F, Sharples LD, Nilsson J, Smith C, Goldstone AR, et al. EuroSCORE II. Eur J Cardiothorac Surg. 2012. April;41(4):734–44; discussion 744–5. [DOI] [PubMed] [Google Scholar]
- 12.Häkkinen U, Kurki T, Vento A, Peltola M. Risk adjustment in coronary bypass grafting: How EuroSCORE is related to cost, healthrelated quality of life, and cost-effectiveness. 2009; Available from: https://www.julkari.fi/bitstream/handle/10024/80203/828989df-7043-4e56-b7e6-61913a2e7f7b.pdf?sequence=1 [Google Scholar]
- 13.Salis S, Mazzanti VV, Merli G, Salvi L, Tedesco CC, Veglia F, et al. Cardiopulmonary bypass duration is an independent predictor of morbidity and mortality after cardiac surgery. J Cardiothorac Vasc Anesth. 2008. December;22(6):814–22. [DOI] [PubMed] [Google Scholar]
- 14.Axtell AL, Fiedler AG, Melnitchouk S, D’Alessandro DA, Villavicencio MA, Jassar AS, et al. Correlation of cardiopulmonary bypass duration with acute renal failure after cardiac surgery. J Thorac Cardiovasc Surg [Internet]. 2019. January 31; Available from: 10.1016/j.jtcvs.2019.01.072 [DOI] [PubMed] [Google Scholar]
- 15.Bruppacher HR, Alam SK, LeBlanc VR, Latter D, Naik VN, Savoldelli GL, et al. Simulation-based training improves physicians’ performance in patient care in high-stakes clinical setting of cardiac surgery. Anesthesiology. 2010. April;112(4):985–92. [DOI] [PubMed] [Google Scholar]
- 16.de Lind van Wijngaarden RAF, Siregar S, Legué J, Fraaije A, Abbas A, Dankelman J, et al. Developing a Quality Standard for Verbal Communication During CABG Procedures. Semin Thorac Cardiovasc Surg. 2019. Autumn;31(3):383–91. [DOI] [PubMed] [Google Scholar]
- 17.Jones LK, Jennings BM, Higgins MK, de Waal FBM. Ethological observations of social behavior in the operating room. Proc Natl Acad Sci U S A. 2018. July 17;115(29):7575–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Agency for Healthcare Research and Quality. Improving Communication and Teamwork in the Surgical Environment Module: Facilitator Notes [Internet]. 2017. [cited 2021 Jan 9]. Available from: https://www.ahrq.gov/hai/tools/ambulatory-surgery/sections/implementation/training-tools/improving-fac-notes.html [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.