Abstract
A 63-year-old male, with no significant past history and not on any regular medications previously, had mild respiratory symptoms post the first dose of the AstraZeneca (Cambridge, England) coronavirus disease 2019 (COVID-19) vaccine, which were self-limiting. Following the second dose of the vaccine, he arrived at the emergency department (ED) with worsening shortness of breath.
During this admission, he was assumed to have interstitial lung disease due to a possible past history of occupational exposure. He responded to a short-term course of corticosteroids and antibiotics and was discharged home.
However, he reported again to the emergency department three weeks later, with persistent dyspnoea along with myalgia. His blood tests and imaging from scans suggested myositis, pneumonitis, and myopericarditis. Since he recently had the COVID-19 AstraZeneca vaccine, it was postulated as the most likely cause of the symptoms. He was managed with intravenous (IV) corticosteroids followed by oral corticosteroids with symptom resolution.
Keywords: mri cardiac, covid-19 myositis, covid-19 pneumonitis, covid-19 myopericarditis, covid 19
Introduction
When dealing with the global pandemic of coronavirus disease 2019 (COVID-19), there was an urgent need for immunity that could boost the natural immune system. The answer was herd immunity from the various vaccines. on the market, recommended by the World Health Organization (WHO) [1]. The WHO issued emergency use listings (EULs) for two versions of the AstraZeneca/Oxford (Cambridge, England) COVID-19 vaccine [2]. There was funding, including indemnity given by governments across the globe to accelerate the mass production and availability of COVID-19 vaccines to the masses [3]. Vaccines and, in particular, adjuvant contents of vaccines have been shown to increase the antigen-specific immune response toward immunogenicity. This may also have negative outcomes, inducing autoimmunity [4].
We present a unique case with combined pneumonitis, myositis and myopericarditis post-COVID-19 vaccination, which responded to conservative management, highlighting the need to be aware of the prompt management of such patients with favourable outcomes.
Case presentation
A 62-year-old male had the first dose of the AstraZeneca/Oxford COVID-19 (ChAdOx1 S {recombinant}) vaccine (AZ) three months after recovery from asymptomatic COVID-19 infection, He developed mild respiratory symptoms and was managed in primary care with oral antibiotics. Respiratory tract symptoms recurred after the second dose of the AZ vaccine two months later; he was again managed in primary care with a course of antibiotics for a lower respiratory tract infection.
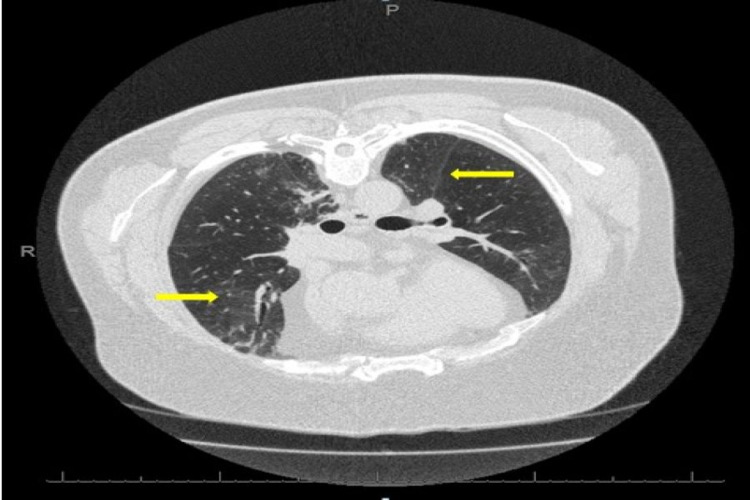
After three weeks with persisting symptoms of dyspnoea and chest tightness, he arrived at the emergency department and was referred to the medical team on-call for further assessment. His initial observations showed oxygen saturation of 88% on air and improvement to 94% with 2 litres of oxygen. As a landlord, there was a possible exposure to bird droppings and dust at building sites while visiting various properties he was renovating. Initial blood tests and high-resolution computed tomogram (HRCT) suggested an impression of probable hypersensitivity pneumonitis (Figure 1). He was started on a weaning course of steroids with outpatient follow-up in the respiratory clinic.
Figure 1. HRCT-axial view.
There is diffuse and patchy ground-glass attenuation (yellow arrows) with tiny nodules in the upper and mid zones, and there are multifocal areas of peripheral consolidation with tractional bronchiolar dilatation within both lower lobes.
HRCT: high-resolution computed tomogram
Twelve days later, he presented again to the emergency department with a referral to the medical team for review. This time, he was admitted to the respiratory ward in insolation with significant myalgia, weakness and dyspnoea and was detected to have very high creatinine kinase (CK) levels of 4053 u/L (22-198), troponin levels of 472 (0-< 14) ng/ml, aspartate transaminase (AST) of 217 u/L (1-45) and C-reactive protein of 60 (-5) (Table 1).
Table 1. Progressive downward trend of biochemical blood markers towards resolution.
| Parameter | Day 1 | Day 2 | Day 3 |
| Troponin | 472 | 399 | 204 |
| Creatinine Kinase (CK) | 4053 | - | 1526 |
| Aspartate Transaminase (AST) | 217 | - | 88 |
| C-Reactive Protein (CRP) | 60 | 27 | 6 |
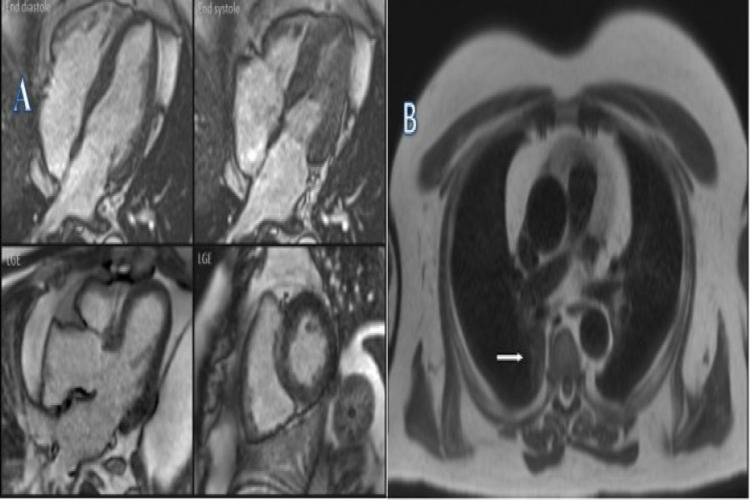
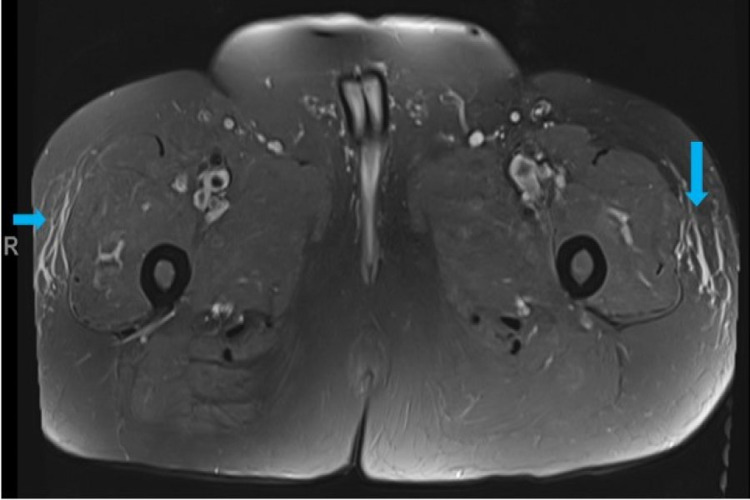
Although the ECG was non-specific, cardiac magnetic resonance imaging (MRI) did show mild fibrosis of the septum and inferior and lateral walls (Figure 2). MRI of the left quadriceps showed non-specific sub-cutaneous fat tissue oedema (Figure 3).
Figure 2. Cardiac MRI.
A. STIR-T2 images: Mild fibrosis of the basal septum and inferior and lateral walls. No myocardial inflammation or infarction. B. Gadolinium study: In the late phase, there is a mild mid-wall enhancement in the basal septum and inferior and lateral walls. There is an area of increased signal in the posterior right lung (white arrow).
STIR: short tau inversion recovery
Figure 3. MRI-left quadriceps: axial view.
There is diffuse oedema in the subcutaneous fat tissue on the anterolateral sides of both thighs (blue arrows).
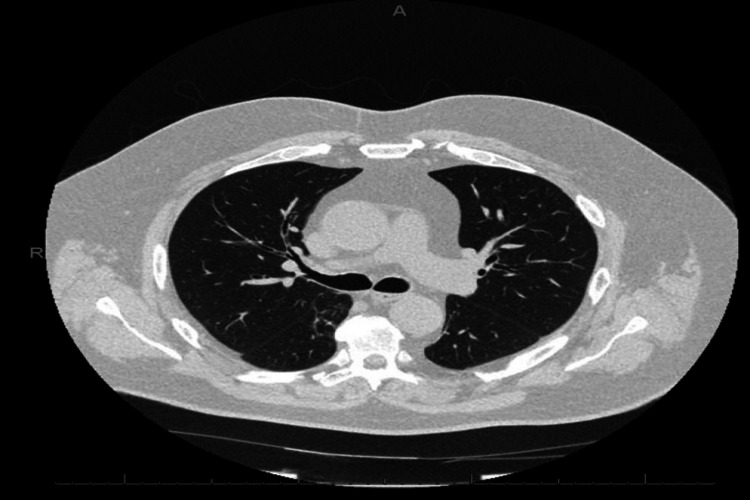
A clinical diagnosis of probable AZ COVID-19 vaccine-related inflammatory myositis, myopericarditis and pneumonitis was made. He was managed with IV methylprednisolone for three days followed by oral prednisolone 40 mg daily with weekly tapering, with appropriate proton pump inhibitor (for acid protection) and vitamin D (bone protection) while on steroids. The anti-nuclear antibody (ANA) level was 1:80 while extra-nuclear antibody (ENA) and double-stranded deoxyribonucleic antibody (dsDNA) were negative. There was a gradual improvement of CK, troponin, AST and CRP levels noted. His repeat HRCT also showed significant resolution (Figure 4). Following recovery, the patient was discharged and booked for outpatient follow-up by the rheumatology and respiratory teams.
Figure 4. HRCT-repeat: axial view.
Almost complete resolution of peripheral areas of radiologically presumed organising pneumonia.
HRCT: high-resolution computed tomogram
Discussion
A number of studies have suggested an association of co-morbidities with the COVID-19 infection [5-8]. Similarly, a number of side effects have also been reported with the use of the vaccines. Some were immediate while others present in a sub-acute fashion. These include COVID-19 vaccine-related rashes [9] and dural venous sinus thrombosis [10]. Side effects related to pneumonitis, which has been demonstrated in transgenic mice studies [11]. A number of studies have demonstrated post-COVID-19 vaccine-related myositis [12-14]. There was also cardiovascular involvement including myocarditis and myopericarditis [15-16].
It is questionable whether the introduction of a booster vaccination would have any further impact on side effects [17-18]. Additionally, National Institute for Clinical Excellence (NICE, UK) and Centre for Disease Control (CDC, USA) guidelines would need to be updated. Fortunately, the monoclonal antibody treatment by AstraZeneca has been approved by the Food and Drug Administration (FDA) USA for emergency use on December 8, 2021, for the long-term prevention of COVID-19 among people with weakened immune systems before they have been exposed to coronavirus with six-monthly injections [19]. The UK's Medicines and Healthcare products Regulatory Agency (MHRA) made the announcement on December 31, 2021, for the pill - Paxlovid, towards reducing the risk of hospitalisation and death [20]. Hopefully, these steps would ensure more safety and more favourable outcomes with a lower incidence of side effects.
We present here a unique case report of a patient who developed an augmented reaction to the second dose of the COVID-19 vaccine with pneumonitis, myopericarditis and myositis that responded well to the tapering doses of steroids. While it would be interesting to see other cases that may be reported and the outcomes of their management, it gives us some hope that there is treatment available to manage such outcomes, albeit short term.
Conclusions
Symptomatic management with corticosteroids, either intravenous or oral, depending on the patient’s status is advised and has shown good results. Since, irrespective of vaccination, the incidence of various side effects, including myositis, pneumonitis, myopericarditis and widespread rashes, is more frequent, there is a need to update NICE UK and CDC USA guidelines and for more awareness of management.
In particular, there is an increasing need to update the guidelines related to side effects with plans to roll out booster vaccinations in the upcoming autumn season.
Acknowledgments
Dr. Mariya Farooq and Dr. Mohammed Yaser are joint first co-authors involved in the care of the patient; they designed the case report and collected the references. Dr. Mansoor Zafar is the corresponding author and was involved in designing the case report and collecting the references. Dr. Dawpadee Dharmasena was involved in the care of the patient. Dr. Usman Iqbal Rana was involved in the proofreading and editing of the case report. Dr. Osei Kankam was involved in the overall care of the patient and reviewed the manuscript for intellectual input. The authors would like to thank the Respiratory Ward team and Radiology team at Conquest Hospital, East Sussex Healthcare NHS Trust for their help in providing the necessary images highlighting the side-effects post-COVID-19 vaccination. Special thanks to Dr. Rita Joarder, Consultant Radiology, Dr. Bernal, Consultant Radiology, and Dr. Hacikurt, Consultant Radiology, for help and support towards identifying and reporting symptom resolution on repeat CT and musculoskeletal MRI images, respectively.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study
References
- 1.WHO. Coronavirus disease (COVID-19): vaccines. https://www.who.int/news-room/q-a-detail/coronavirus-disease-(covid-19)-vaccines?topicsurvey=v8kj13)&gclid=Cj0KCQjw4ImEBhDFARIsAGOTMj8HXX50axr69EryvnvgwUac4oENW65GBFGblUiBIAH87wYC0SGiwJIaArAkEALw_wcB 2021
- 2.Oxford/AstraZeneca Covid vaccine research ‘was 97% publicly funded’. The Guardian. https://www.theguardian.com/science/2021/apr/15/oxfordastrazeneca-covid-vaccine-research-was-97-publicly-funded 2021
- 3.UK government grants Pfizer civil legal indemnity for COVID-19 vaccine. Jurist. https://www.jurist.org/news/2020/12/uk-government-grants-pfizer-civil-legal-indemnity-for-covid-19-vaccine/ 2020
- 4.Post-vaccination myositis and myocarditis in a previously healthy male. Cheng MP, Kozoriz MG, Ahmadi AA, Kelsall J, Paquette K, Onrot JM. Allergy Asthma Clin Immunol. 2016;12:6. doi: 10.1186/s13223-016-0114-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vitamin D levels and mortality with SARS-COV-2 infection: a retrospective two-centre cohort study. Zafar M, Karkhanis M, Shahbaz M, et al. https://pubmed.ncbi.nlm.nih.gov/34489318/ Postgrad Med J. 2021 doi: 10.1136/postgradmedj-2021-140564. [DOI] [PubMed] [Google Scholar]
- 6.A retrospective observational study: is absolute lymphocyte count a prognostic marker in COVID-19? Zafar M, Shahbaz M, Karkhanis M, et al. https://pubmed.ncbi.nlm.nih.gov/34327110/ Cureus. 2021;13:0. doi: 10.7759/cureus.16554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.A UK nationwide study of people with type 1 diabetes admitted to hospital with COVID-19 infection. Ruan Y, Ryder RE, De P, et al. https://pubmed.ncbi.nlm.nih.gov/33966090/ Diabetologia. 2021;64:1717–1724. doi: 10.1007/s00125-021-05463-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Can HbA1c levels be used as an independent marker of mortality and morbidity risk in patients with COVID19 positive swabs? - a retrospective observational study. Zafar M, Randhawa R S, Hegner W, et al. https://www.utmj.org/index.php/UTMJ/article/view/1494 Univ Tor Med J. 2021;98:0. [Google Scholar]
- 9.COVID-19 vaccination-induced rash: does the choice of vaccine matter? Zafar M, Ewnetu B, Ahmed S, Iqbal U, Whitehead M. Cureus. 2021;13:0. doi: 10.7759/cureus.15490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thrombocytopenia and intracranial venous sinus thrombosis after "COVID-19 vaccine AstraZeneca" exposure. Wolf ME, Luz B, Niehaus L, Bhogal P, Bäzner H, Henkes H. J Clin Med. 2021;10:1599. doi: 10.3390/jcm10081599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pathogenesis of SARS-CoV-2 in transgenic mice expressing human angiotensin-converting enzyme 2. Jiang RD, Liu MQ, Chen Y, et al. Cell. 2020;182:50–58. doi: 10.1016/j.cell.2020.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.COVID-19 vaccine-related myositis. Theodorou DJ, Theodorou SJ, Axiotis A, Gianniki M, Tsifetaki N. QJM. 2021;114:424–425. doi: 10.1093/qjmed/hcab043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Paraspinal myositis in patients with COVID-19 infection. Mehan WA, Yoon BC, Lang M, Li MD, Rincon S, Buch K. AJNR Am J Neuroradiol. 2020;41:1949–1952. doi: 10.3174/ajnr.A6711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.COVID-19-associated myositis with severe proximal and bulbar weakness. Zhang H, Charmchi Z, Seidman RJ, Anziska Y, Velayudhan V, Perk J. Muscle Nerve. 2020;62:0–60. doi: 10.1002/mus.27003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.COVID-19 vaccine-induced myocarditis: case report with literature review. Nassar M, Nso N, Gonzalez C, et al. Diabetes Metab Syndr. 2021;15:102205. doi: 10.1016/j.dsx.2021.102205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Temporal association between the COVID-19 Ad26.COV2.S vaccine and acute myocarditis: a case report and literature review. Sulemankhil I, Abdelrahman M, Negi SI. Cardiovasc Revasc Med. 2021;[Epub ahead of print] doi: 10.1016/j.carrev.2021.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.COVID-19 vaccination: a guide to booster vaccination - GOV.UK. https://www.gov.uk/government/publications/covid-19-vaccination-booster-dose-resources/covid-19-vaccination-a-guide-to-booster-vaccination. 2021
- 18.Covid-19: booster vaccine to be rolled out in autumn as UK secures 60m more Pfizer doses. Mahase E. https://www.bmj.com/content/373/bmj.n1116. BMJ. 2021;373:1116. doi: 10.1136/bmj.n1116. [DOI] [PubMed] [Google Scholar]
- 19.FDA clears first covid antibody treatment for immunocompromised before exposure. NBC News. https://www.nbcnews.com/health/health-news/fda-clears-astrazenecas-covid-antibody-treatment-immunocompromised-rcna8130 NBC News. 2021
- 20.Pfizer covid pill approved In UK for those most at risk. The Independent. https://www.independent.co.uk/news/uk/home-news/paxlovid-covid-pill-pfizer-uk-b1984885.html Independent. 2021