Abstract
Introduction
This study uses multiple measures of excess deaths to analyze racial disparities in COVID-19 mortality across Georgia.
Methods
The Georgia Department of Public Health provided monthly mortality data for 2010–2020 stratified by race/ethnicity, age, county, and recorded cause of death. We first calculate crude mortality rates by health district during the time period for all groups for March through June for our historical period to identify significant time-series outliers in 2020 distinguishable from general trend variations. We then calculate the mean and standard deviation of mortality rates by age and racial subgroup to create historic confidence intervals that contextualize rates in 2020. Lastly, we use risk ratios to identify disparities in mortality between Black and White mortality rates both in the 2010–2019 period and in 2020.
Results
Time-series analysis identified three health districts with significant increases in mortality in 2020, located in metro Atlanta and Southwest Georgia. Mortality rates decreased sharply in 2020 for children in both racial categories in all sections of the state, but rose in a majority of districts for both categories in adult and older populations. Risk ratios also increased significantly in 2020 for children and older populations, showing rising disparities in mortality during the pandemic even as crude mortality rates declined for children classified as Black.
Conclusions
Increased mortality during the COVID-19 outbreak disproportionately affected African-Americans, possibly due, in part, to pre-existing disparities prior to the pandemic linked to social determinants of health. The pandemic deepened these disparities, perhaps due to unequal resources to effectively shelter-in-place or access medical care. Future research may identify local factors underlying geographically heterogenous differences in mortality rates to inform future policy interventions.
Keywords: COVID19, Excess deaths, Racial disparities, Social determinants of health, Spatial analysis, Georgia
1. Introduction
At the time of this paper, the COVID-19 outbreak is still ongoing across the United States, but multiple studies have already shown its disproportionate impact on communities of color, particularly Black communities (Chen and Krieger, 2020; Raifman and Raifman, 2020; Townsend et al., 2020; Yehia et al., 2020). These disparities are created through a number of factors related to structural racism, including increased exposure in the workplace and already existing comorbidities linked to increased rates of poverty (Thakur et al., 2020). These differences reflect ongoing disparities that shape multiple social determinants of health (SDOH), including educational, justice, housing, and public health systems (Egede and Walker, 2020). As the validity of data on COVID related mortality has come under question publicly (Knight and Appleby, 2020), some researchers have relied on measurements of excess death to document the extent of the disease's impact (Weinberger et al., 2020).
This paper analyzes mortality data by health district stratified by both age and race in the state of Georgia to identify how COVID impacted already existing geographic and racial disparities in mortality rates. While some previous analyses have used sub-state level data (Chen and Krieger, 2020), in many states public mortality data are only available at state level. By drawing from this granular dataset, our analysis identifies how and where the COVID outbreak amplified already existing racial disparities in mortality and identifies social determinants that may have contributed to this effect.
2. Methods
2.1. Study area
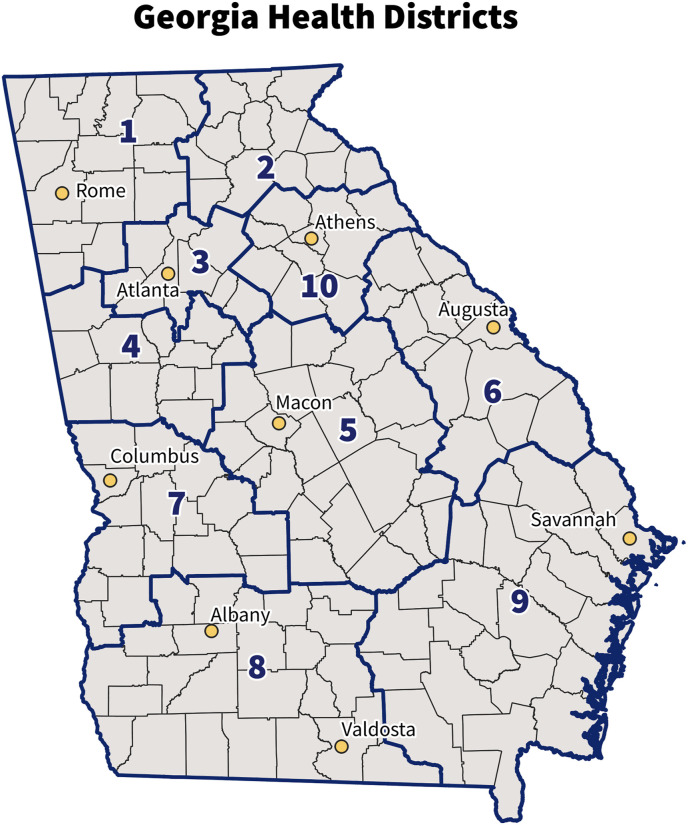
This analysis examined mortality in the state of Georgia, which enacted some of the fewest restrictions on COVID during the height of the outbreak and was the site of one of the first major outbreaks in the city of Albany (Jarvie, 2020). Fig. 1 shows the state's counties and major health districts, the latter of which were used for our analysis.
Fig. 1.
Georgia counties, health districts, and major cities.
Table 1 provides a summary of key demographic characteristics of these regions, compiled from the U.S. Census (American Community Survey, 2021), National Center for Health Statistics (NCHS, 2021), and Minnesota Population Center IPUMS data (Manson et al., 2021). The state has a diverse social landscape. Statewide, in 2020, the U.S. Census Bureau classified 52% of the population as non-Hispanic white, 33% as non-Hispanic Black, 10% as Hispanic or Latino, and 4% Asian. Subgroups classified as non-Hispanic White and Black—the two largest groups statewide--are most concentrated in metro Atlanta (District 3) and southern, largely rural parts of the state (Districts 5 through 9). These areas also have the highest poverty rates, lowest rates of insurance (either public or private), and lowest life expectancies in the state.
Table 1.
Demographic characteristics of Georgia's health districts. Source: U.S. Census, CDC, IPUMS.
| District | Population | % pop. In urban areas | % White, non-Hispanic | % Black, non-Hispanic | % Asian | % Hispanic/Latinx | % with health insurance | % <200% poverty | Median life expectancy (years) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 1,145,870 | 61.9 | 77.6 | 7.9 | 1.1 | 10.8 | 86.9 | 27.5 | 76.6 |
| 2 | 702,650 | 57.7 | 74.2 | 5.1 | 5.1 | 13.5 | 87 | 22.8 | 78.2 |
| 3 | 4,076,437 | 97.7 | 37.4 | 40.6 | 7 | 12.2 | 86.5 | 24.8 | 78.1 |
| 4 | 853,494 | 64.7 | 60.1 | 29.2 | 2.2 | 5.9 | 89.2 | 24.8 | 76.4 |
| 5 | 679,423 | 57.8 | 53.8 | 38.5 | 1.6 | 4.2 | 87.8 | 34.6 | 75.5 |
| 6 | 485,069 | 69.4 | 50.1 | 39.7 | 2 | 5.1 | 88.3 | 31.4 | 74.6 |
| 7 | 369,428 | 65.6 | 45.3 | 43.3 | 1.8 | 6.6 | 87.9 | 36.3 | 74.9 |
| 8 | 602,704 | 54.9 | 52.6 | 38.2 | 1 | 6.4 | 83.2 | 39.9 | 75.5 |
| 9 | 986,975 | 62.4 | 59.9 | 28.4 | 1.5 | 7.3 | 85.7 | 33.1 | 75.3 |
| 10 | 501,797 | 57 | 70.1 | 17.6 | 2.4 | 7.7 | 87.4 | 27.9 | 76.5 |
2.2. Data
Mortality data were obtained through a records request to the Georgia Department of Public Health (DPH, August 27, 2020) and analyzed in 2020. Recorded deaths were provided from January 2010 through mid-August 2020 and stratified by county, age, race/ethnicity, and recorded cause of death based on the National Center for Health Statistics coding. Age groups were categorized as under 18, 18 to 64, and 65 and older, and for this analysis we focused on the three racial/ethnic groups present across most of the state: non-Hispanic White, non-Hispanic Black, and Hispanic/Latinx. Our study period for this analysis is from March 2020, the date of the first recorded COVID case in the state, through June 2020, when the first wave of infections was subsiding.
To normalize the mortality data, we use county level estimates of total population by racial category from the U.S. Census (U.S. Census Bureau, 2020). These yearly data are interpolated to monthly estimates for the study period using the ‘approxfun' function in the R statistical software program (version 3.6.0), with an interpolated value for 2020 derived through linear regression from previous years. We aggregate these county level data on mortality and population by Georgia's ten health districts for the purpose of analysis, using them to calculate the crude mortality rate of each subgroup (based on age and race/ethnicity) within each district.
2.3. Statistical analysis
We use two measures of excess deaths for the purposes of this paper. First, we use an outlier detection algorithm for time series (Chen and Liu, 1993), implemented via the ‘tsoutliers' package (López-de-Lacalle, 2019), to identify excess deaths during our study period based on crude mortality rate. This algorithm uses best-fit ARIMA models to first identify potential anomalous time periods and then refits the ARIMA with the anomalous time periods removed to produce a counter-factual time series. This analysis thus identifies the values expected in a time period based on previous trends and compares them to actual values. Time points with t-statistics in excess of 3.5 are considered candidate outlier time points in order to minimize false-positive outliers. This approach is less likely to identify spurious outliers and more accurately produces a counterfactual time series reflecting underlying trends. More information on this algorithm is available in other publications (Chen and Liu, 1993; López-de-Lacalle, 2019).
Second, we calculate the mean and standard deviation for mortality rates for the 2010-19 baseline period by month for the total population and each subgroup (age, health district, and racial classification) across health districts, which are our spatial variable. Since only two racial classifications (non-Hispanic White and Black) are common across all health districts, we focus on only those two groups for this analysis. Based on the mean and standard deviation, we calculate a 95% confidence interval for yearly rates within the study period. We similarly calculate mortality rates by subgroup for March through June 2020 and identify whether this rate fits within the historical confidence interval.
Third, to identify racial disparities within race and geographic groups, we calculate a risk ratio showing the relationship of Black to White crude mortality rates for each year of the historical period and in 2020. We calculate the mean value of this ratio for the historical period as well as a 95% confidence interval. Lastly, we calculate the percentage change in mortality rates and risk ratios to identify changes during the COVID outbreak.
3. Results
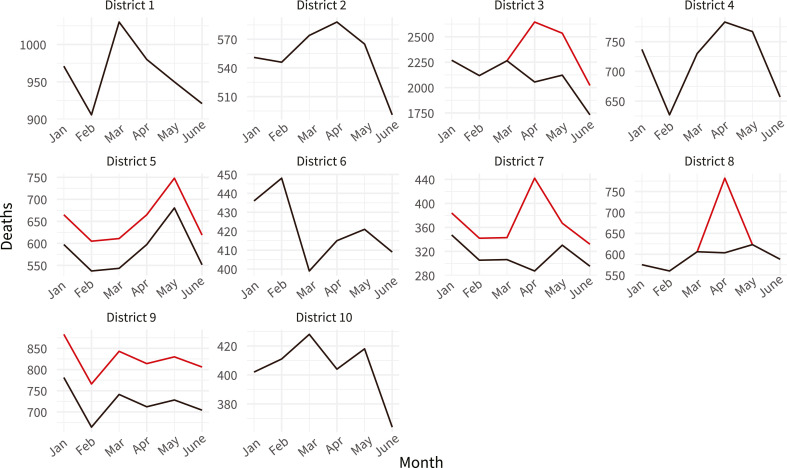
Fig. 2 shows the results of a time-series analysis of all deaths across districts from January through June 2020. While the first two months are prior to the COVID outbreak, they are included to differentiate districts that had already experienced a previous shift (districts 5 and 9) from those with outliers during the outbreak. This figure identifies districts with statistically significant increases in mortality. The black lines in this graph show the expected values provided by the time-series models. If outliers were detected by the models, the black lines show the trends with those outliers removed, and the red lines show the data with outliers included. If no red line is present, then no time-series outliers were detected by the models. In districts 5, 7, and 9, there was an upwards shift in mortality prior to the COVID outbreak. Only districts 3, 7, and 8 are outliers coincident with COVID based on this analysis. If we sum the difference between the actual values and the time series with outliers removed—the distance between the red and black lines--and subtract the prior time shift for district 7, we find an estimated 1587 excess deaths during this time period in these three districts.
Fig. 2.
Predicted deaths with outliers removed (black) and observed deaths (red, where outliers are detected) rates of mortality for Georgia health districts by month. Predictions are based on best-fit ARIMA models for time-series outliers and the y-axis is rescaled by district. (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
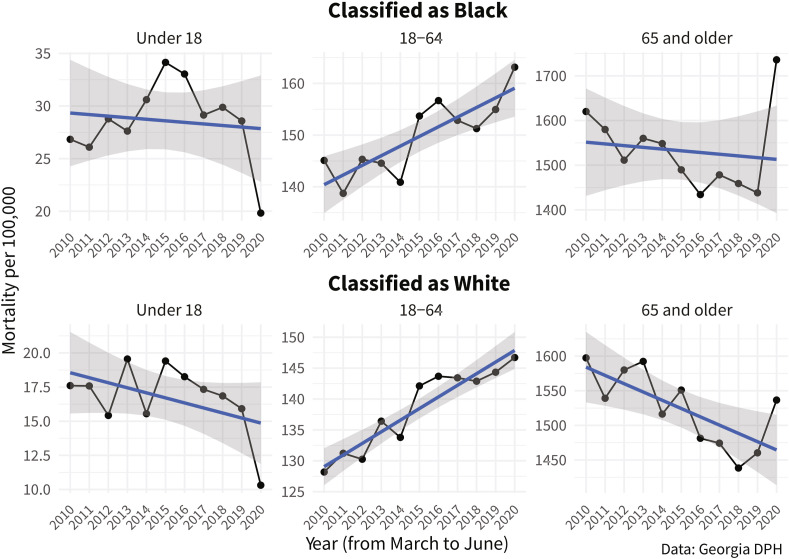
Fig. 3 provides a visualization of statewide mortality rates from all causes of death stratified by age and race from 2010 through 2020, including just the March through June study periods for the two largest racial categories. Three trends are especially notable on this graph. First, mortality drops sharply for children in both racial categories, from 28.6 to 20 per 100,000 from 2019 to 2020 for those classified as Black and from 16.1 to 10.5 for those classified as White. Despite these drops, the rate for Black children in 2020 is still higher than the historic maximum for White children (19.6 in 2013). Second, while rates increased modestly for the middle age group among those classified as Black, the increase for those classified as White was in line with previous historical trends. Lastly, while mortality rates increased in 2020 for both groups over 65 compared to the previous year, this rise was much higher for those classified as Black (21% higher than 2019) compared to those classified as White (5%). To estimate the impact of these increases, we use the coefficient from a linear regression for the historical period (2010–19) to extrapolate the 2019 rate for older adults to an expected rate in 2020 and then calculate the expected number of deaths based on this rate. Recorded deaths in 2020 are 1064 above this expected amount for older adults classified as Black and a similar 1177 for those classified as White, even though the population size of the latter group is roughly three times that of the former (1,022,293 vs. 336,070).
Fig. 3.
Mortality rates from March to June from 2010 to 2020, stratified by age and racial category. The blue line shows the linear trend identified through regression and the gray area is a 95% confidence interval around that estimate. The y-axis is rescaled by district. (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
We present the results of the historical analysis of mortality rates by subgroup in Table 2 . Trends are broadly similar across racial classifications. For individuals under 18, mortality decreased in every section of the state for the subgroups classified as Black and as White. These drops were large in magnitude. For the subgroup classified as White, only two health districts (1 and 5) had a decline of less than 10%, and declines in the remaining districts ranged between 39% and 79%. For the subgroup classified as Black, just one district (7) had a decline of less than 10% and the remaining areas had declines between 24% and 52%. Although most districts historically report less than 100 deaths for this age group during the study period each year, rates in 2020 were well outside the historic confidence interval (8 of 10 districts for both racial classifications).
Table 2.
Mortality rates and associated confidence intervals in the 2010-19 study period and mortality rates in 2020 by racial classification, age, and health district. Risk ratios comparing Black to White mortality rates also shown for both study periods. 2020 rates outside the historic confidence interval are bolded and highlighted with an asterisk.
| Classified as white |
Classified as Black |
Risk ratio: Black to white subgroups |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Under 18 |
Under 18 |
Under 18 |
|||||||||||||
| District |
Historic |
Conf Int |
2020 |
Change |
Direction |
Historic |
Conf Int |
2020 |
Change |
Direction |
Historic |
Conf Int |
2020 |
Change |
Direction |
| 1 |
15.97 |
(14.41, 17.53) |
15.4 |
−4% |
– |
26.54 |
(19.76, 33.32) |
15.82* |
−40% |
– |
1.696 |
(1.21, 2.18) |
1.027 |
−39% |
– |
| 2 |
15.68 |
(13.05, 18.31) |
5.69* |
−64% |
– |
24.45 |
(15.69, 33.21) |
11.73* |
−52% |
– |
1.66 |
(0.96, 2.36) |
2.062 |
24% |
+ |
| 3 |
12.89 |
(11.23, 14.55) |
7.86* |
−39% |
– |
27.26 |
(25.92, 28.6) |
17.84* |
−35% |
– |
2.198 |
(1.9, 2.5) |
2.27 |
3% |
+ |
| 4 |
17.84 |
(15.63, 20.05) |
7.64* |
−57% |
– |
25.94 |
(21.57, 30.31) |
18.79* |
−28% |
– |
1.547 |
(1.18, 1.91) |
2.459 |
59% |
+ |
| 5 |
18.66 |
(16, 21.32) |
17.6 |
−6% |
– |
33.09 |
(28.05, 38.13) |
20.08* |
−39% |
– |
1.813 |
(1.52, 2.11) |
1.141 |
−37% |
– |
| 6 |
30.11 |
(22.31, 37.91) |
6.19* |
−79% |
– |
38.14 |
(33.34, 42.94) |
22.04* |
−42% |
– |
1.472 |
(1.06, 1.88) |
3.561 |
142% |
+ |
| 7 |
20.43 |
(15.72, 25.14) |
13.3* |
−35% |
– |
37.18 |
(32.54, 41.82) |
35.87 |
−4% |
– |
2.06 |
(1.54, 2.58) |
2.697 |
31% |
+ |
| 8 |
26.55 |
(23.9, 29.2) |
14.46* |
−46% |
– |
34.78 |
(30.67, 38.89) |
23.66* |
−32% |
– |
1.329 |
(1.15, 1.51) |
1.636 |
23% |
+ |
| 9 |
21.26 |
(19.06, 23.46) |
14.34* |
−33% |
– |
32.63 |
(27.43, 37.83) |
24.81* |
−24% |
– |
1.562 |
(1.28, 1.84) |
1.73 |
11% |
+ |
| 10 |
18.94 |
(15.92, 21.96) |
8.42* |
−56% |
– |
23.28 |
(13.14, 33.42) |
17.51 |
−25% |
– |
1.304 |
(0.75, 1.86) |
2.08 |
59% |
+ |
| 18–64 |
18–64 |
18–64 |
|||||||||||||
| District |
Historic |
Conf Int |
2020 |
Change |
Direction |
Historic |
Conf Int |
2020 |
Change |
Direction |
Historic |
Conf Int |
2020 |
Change |
Change |
| 1 |
156.74 |
(150.67, 162.81) |
173.66* |
11% |
+ |
136.9 |
(127.4, 146.4) |
170.62* |
25% |
+ |
0.872 |
(0.82, 0.92) |
0.982 |
13% |
+ |
| 2 |
139.03 |
(135.43, 142.63) |
141.91 |
2% |
+ |
143.02 |
(137.22, 148.82) |
122.04* |
−15% |
– |
1.032 |
(0.97, 1.1) |
0.86 |
−17% |
– |
| 3 |
101.47 |
(99.87, 103.07) |
97.11* |
−4% |
– |
123.17 |
(119.3, 127.04) |
131.2* |
7% |
+ |
1.216 |
(1.17, 1.26) |
1.351 |
11% |
+ |
| 4 |
152.04 |
(147.59, 156.49) |
161.22* |
6% |
+ |
136.36 |
(130.13, 142.59) |
162.3* |
19% |
+ |
0.898 |
(0.86, 0.94) |
1.007 |
12% |
+ |
| 5 |
165.89 |
(160.07, 171.71) |
185.44* |
12% |
+ |
175.93 |
(163.09, 188.77) |
187.7 |
7% |
+ |
1.06 |
(0.99, 1.13) |
1.012 |
−5% |
– |
| 6 |
162.17 |
(154.48, 169.86) |
172.52* |
6% |
+ |
179.62 |
(168.47, 190.77) |
180.81 |
1% |
+ |
1.114 |
(1.02, 1.21) |
1.048 |
−6% |
– |
| 7 |
150.97 |
(138.79, 163.15) |
178.83* |
18% |
+ |
197.04 |
(184.62, 209.46) |
248.73* |
26% |
+ |
1.317 |
(1.22, 1.41) |
1.391 |
6% |
+ |
| 8 |
170.15 |
(155.94, 184.36) |
195.28* |
15% |
+ |
189.84 |
(180.07, 199.61) |
270.06* |
42% |
+ |
1.13 |
(1.04, 1.22) |
1.383 |
22% |
+ |
| 9 |
153.57 |
(144.79, 162.35) |
185.36* |
21% |
+ |
159.08 |
(149.2, 168.96) |
163.89 |
3% |
+ |
1.038 |
(0.99, 1.09) |
0.884 |
−15% |
– |
| 10 | 128.86 | (120.92, 136.8) | 130.31 | 1% | + | 170.79 | (159.61, 181.97) | 182.46* | 7% | + | 1.334 | (1.23, 1.43) | 1.4 | 5% | + |
| 65 and over | 65 and over | 65 and over | |||||||||||||
| District |
Historic |
Conf Int |
2020 |
Change |
Direction |
Historic |
Conf Int |
2020 |
Change |
Direction |
Historic |
Conf Int |
2020 |
Change |
Change |
| 1 | 1477.66 | (1427.17, 1528.15) | 1462.88* | −1% | – | 1384.48 | (1272.91, 1496.05) | 1312.25 | −5% | – | 0.938 | (0.87, 1.01) | 0.897 | −4% | – |
| 2 | 1328.76 | (1288.96, 1368.56) | 1329.84 | 0% | + | 1257.45 | (1124.51, 1390.39) | 1465.54* | 17% | + | 0.948 | (0.84, 1.06) | 1.102 | 16% | + |
| 3 | 1347.85 | (1282.11, 1413.59) | 1334.98 | −1% | – | 1267.31 | (1217.97, 1316.65) | 1441.56* | 14% | + | 0.942 | (0.92, 0.97) | 1.08 | 15% | + |
| 4 | 1504.14 | (1455.74, 1552.54) | 1556.19* | 3% | + | 1400.26 | (1339.14, 1461.38) | 1672.28* | 19% | + | 0.932 | (0.89, 0.97) | 1.075 | 15% | + |
| 5 | 1539.13 | (1499.9, 1578.36) | 1595.32* | 4% | + | 1516.71 | (1450.14, 1583.28) | 1752.77* | 16% | + | 0.985 | (0.94, 1.03) | 1.099 | 12% | + |
| 6 | 1616.29 | (1552.59, 1679.99) | 1478.19* | −9% | – | 1608.37 | (1549.75, 1666.99) | 1666.26 | 4% | + | 0.996 | (0.96, 1.03) | 1.127 | 13% | + |
| 7 | 1602.14 | (1579.28, 1625) | 1715.71* | 7% | + | 1548.04 | (1495.23, 1600.85) | 1857.66* | 20% | + | 0.966 | (0.93, 1) | 1.083 | 12% | + |
| 8 | 1626.75 | (1576.17, 1677.33) | 1725.19* | 6% | + | 1571.98 | (1522.94, 1621.02) | 2172.18* | 38% | + | 0.968 | (0.94, 0.99) | 1.259 | 30% | + |
| 9 | 1485.31 | (1439.51, 1531.11) | 1433.46* | −3% | – | 1552.38 | (1486.44, 1618.32) | 1645.38* | 6% | + | 1.046 | (1.02, 1.07) | 1.148 | 10% | + |
| 10 | 1428.64 | (1358.11, 1499.17) | 1470.13 | 3% | + | 1531.04 | (1414.83, 1647.25) | 1650.66* | 8% | + | 1.072 | (1.01, 1.13) | 1.123 | 5% | + |
For adults (ages 18 to 64), mortality rates generally increased in 2020 compared to historic averages. For the subgroup classified as White, only district 3 (the Atlanta metro) had a decline in mortality rates during this period. Increases in districts 2 and 10 were 2% and 1% respectively and within historic confidence intervals. The remaining districts saw increases in mortality between 6 and 21%. For the subgroup classified as Black, only district 2 (northeast Georgia, with a Black population of only 5.1%) had a decline in mortality rates. Six districts had increases outside the historic confidence interval, ranging from 7% to 42%. The highest value was in district 8, which includes Albany and was an early hotspot.
For older adults (age 65 and over), most districts also saw increases, but this differed by racial classifications. For the subgroup classified as White, only four districts (4, 5, 7, and 8--central and Southeast Georgia) had increases outside the historic confidence interval, and these were all under 10%. For the subgroup classified as Black, all but district 1 (northwest Georgia) had increased mortality rates, and of these, all but district 6 were above the historic confidence interval. These values ranged from 6% to 38%, notably higher than for the subgroup classified as White.
The risk ratios shown in Table 2 show the relative change in mortality rates by racial classification. For children, both racial categories had significant declines in mortality during this period. Yet the ratio of Black to White mortality rates increased in eight of ten health districts and were above the historical range in six of them, located in south and central Georgia. In these areas, mortality rates for children classified as White dropped more steeply than for children classified as Black. In districts 3, 4, 5, 7, and 9, mortality rates for children classified as Black in 2020—during the first wave of the pandemic—were higher than the pre-pandemic average rates for children classified as White. In district 6, the risk ratio for mortality increased 142% (from 1.47 to 3.56) during the 2020 study period despite the fact that mortality decreased by 42% for children classified as Black during this time. In all districts besides 2 and 7, the confidence interval for the risk ratio was higher than one historically and this was true for all districts in 2020, indicating higher mortality rates for children classified as Black.
For adults, the change in risk ratios was mixed. Historically, those classified as Black have had higher mortality rates than those classified as White, with the exception of district 1 (risk ratio: 0.872, or 13% lower mortality). This risk ratio decreased to levels below the historical confidence interval in districts 2 and 9 in 2020. However, in the early hotspots of districts 3 and 8, the risk ratios increased 11% and 22% respectively, also outside the historical range.
Lastly, for older adults, the historical risk ratios were below one in all but districts 9 and 10, and confidence intervals had a range fully below one in districts 3, 4, and 8, Atlanta and parts of western Georgia. This indicates generally lower mortality rates for the subgroup classified as Black. However, for 2020, only district 1, where only 8% of the population is classified as Black, had a risk ratio less than one, declining 4% from its historic value. In all other districts, risk ratios increased between 5 and 30% and these increases were above the historical range in all but district 10. The largest increase was in district 8, which increased from 0.966 (3% lower mortality) to 1.259 (26% higher mortality) for older adults classified as Black during the pandemic's first phase.
4. Discussion
This analysis identified geographic and racial disparities in mortality for the first wave of the COVID-19 outbreak in Georgia. Our initial analysis of excess deaths showed clear effects of the pandemic's first wave in three sections of the state: Atlanta and two health districts in Southwest Georgia. These numbers support official estimates by the state's Department of Public Health. Both our statewide and regional analyses show that the first wave of the impact had a disproportionate impact on the subgroup classified as Black.
Historical analysis of these numbers contextualizes them within ongoing disparities in mortality rates across racial classification. In almost every health district in the state, mortality rates were higher for the subgroup under 65 among the subgroup classified as Black prior to the pandemic compared to those classified as White. For those under 18 and over 65, disparities between Black and White subgroups widened in a majority of districts during the pandemic, even outside districts 3, 7, and 8 where the first impacts of COVID were most evident.
Two trends were especially notable in this analysis. First, both White and Black children saw drops in mortality during the pandemic consistent with a protective effect from lockdowns. During the first wave of pandemic cases in the United States, spanning from mid-March to the end of April, approximately 95% of Americans were under a shelter-in-place order of some kind (Mervosh et al., 2020). Thus, young people were at home. Most schools were cancelled, all extracurricular activities were cancelled, and general patterns of movement were greatly diminished, thus decreasing the daily risk faced by young people. In addition, children are more likely to be covered by insurance—in the state of Georgia, public insurance programs for children are much more generous than they are for adults, meaning that Medicaid and “PeachCare”, Georgia's SCHIP program, would open the door for more young people to seek the care that they need. The latest clinical evidence of virus transmission and the intensity of disease when contracted shows that children, especially the very young (<5 years of age), have lower transmission rates and cases tend to be far less severe relative to adults (Leeb et al., 2020; Lu et al., 2020; Ludvigsson, 2020). Yet, our results suggest protective effects from shelter-in-place may have resulted in much steeper declines for children classified as White than those classified as Black, increasing the disparity in mortality rates between these two groups.
Secondly, although older adults classified as Black had generally lower mortality rates than those classified as White prior to the pandemic, these rates increased substantially during the first wave throughout the state. The initially lower rates match the finding of Ferdows et al. (2020) for crude rates at the national level, and they match trends we confirmed independently using the same CDC WONDER database. The effects of higher rates of mortality at younger ages, evident both in our data and in national studies (Woolf and Schoomaker, 2019), may explain these lower rates in Georgia. Despite these initial conditions, the significant increase in the risk ratios seen throughout the state for this age group indicate a much greater level of vulnerability for older adults classified as Black.
These results demonstrate potential impacts from Social Determinants of Health (CDC, 2020). Examining SDOH for Black versus White subgroups shows significant disparity in the type of employment by race (Egede and Walker, 2020; Tai et al., 2020). The “essential workers” terminology used early and often in the COVID-19 pandemic applies to healthcare workers, but also food service, frontline customer service in grocery stores and convenience stores, and custodial work (National Conference of State Legislatures, 2020). Black Americans are more likely to be in these high-exposure, and thus high risk jobs (Hawkins, 2020; Poteat et al., 2020; Selden and Berdahl, 2020); they simply have been more likely to encounter the virus because hourly low-wage jobs do not offer the same protections and options for telework that salaried jobs do.
Another aspect of the SDOH framework is healthcare access (CDC, 2020). Uninsurance and underinsurance is more likely for Black households than White households (Artiga et al., 2020; Garfield and Damico, 2015). Thus, households may have had differing resources for seeking care related to COVID, such as treating comorbidities or accessing care when ill. This disparity is exacerbated in Georgia since the state has not participated in Medicaid expansion (Artiga et al., 2020; Garfield and Damico, 2015; Poteat et al., 2020). The supply-side dynamic is also important here, too, given that physicians choose whether to accept out-of-pocket uninsured individuals and Medicaid patients (Hsiang et al., 2019; Neprash et al., 2018). Many physicians do not accept such patients, which exacerbates the complex landscape of healthcare access for low-income families and people of color.
Finally, the issue of comorbidities is also an important consideration. The Centers for Disease Control and Prevention have established and published the chronic conditions that put an individual in a high-risk category for developing complications with COVID-19 or experiencing a more serious illness when contracting the virus. People of color have higher prevalence of many of these chronic conditions, including obesity and severe obesity, heart disease, Type II diabetes, renal disease, and Sickle Cell Disease (American Cancer Society, 2019; Chang et al., 2017; Payne et al., 2020). Most of these comorbidities are linked to ongoing racialized economic inequality (Thakur et al., 2020).
In this context, the data for children included in our analysis is especially striking. Even as the pandemic provided a protective effect for children classified as Black, racial gaps with White children widened. This is perhaps due to the greater ability of White households to effectively shelter-in-place or access needed healthcare services as needs arose. It also underscores how SDOH might result not only in increased risks to health problems, but also decreased capacity to protect self and others even as overall exposure to risk declines. Similarly, although mortality rates were generally lower for older adults classified as Black prior to the pandemic, ongoing comorbidities, poor access to healthcare, and/or greater exposure may have been responsible for the significantly higher mortality rates in may regions of the state during the pandemic's first wave.
4.1. Limitations
This analysis includes only the first wave of COVID-19 in Georgia, and the virus remains a public health crisis both within the state and nationally at the time we are writing this article. Our results are thus inherently preliminary. State officials who provided these data also advised us that it can be up to a year before mortality figures are finalized, and this may have been a limiting factor in our analysis. Our analysis is also primarily descriptive, and thus does not control for potential confounding variables responsible for the patterns we observe. Similarly, we identify trends in our data, but given our observational data we are unable to identify causal mechanisms for these results. We did create models using both geographic access to a medical center and health insurance coverage as independent variables, but these were inconclusive. Future research could explore potential drivers of spatial heterogeneity.
5. Conclusion
In this first wave of infection, our research reveals notable racial disparities in mortality rates. These disparities are geographically heterogeneous, but statewide overall trends demonstrate ongoing and deepening inequity during the COVID outbreak. These patterns differed across age groups. In the early hot spots such as Albany and Atlanta, mortality for older adults spiked even as rates for children decreased. Yet racial disparities in mortality grew significantly for children and older adults in almost all sections of the state. The disparities we identify reflect persistent racialized inequality across several SDOH, including workplace vulnerability, access to healthcare, and factors responsible for already existing comorbidities.
While our analysis revealed clear racial disparities in COVID19's impact, the differences we observed across health districts could be the basis of future research, identifying how local factors such as healthcare access and quality have mediated the impact of this outbreak. COVID19 has highlighted the health vulnerabilities created by racial inequality. By understanding how and where these effects are most visible, future research can inform efforts to close these gaps.
Credit author statement
Shannon: Conceptualization, Methodology, Formal analysis, Writing (both original and reviewed), Visualization. Abraham: Conceptualization, Writing-original draft. Bagwell-Adams: Conceptualization, Writing-original draft. Hauer: Conceptualization, Methodology, Formal analysis, Writing-Original draft.
References
- American Cancer Society . 2019. Cancer Facts and Figures for African Americans 2019-2021.https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/cancer-facts-and-figures-for-african-americans/cancer-facts-and-figures-for-african-americans-2019-2021.pdf Retrieved from. [Google Scholar]
- American Community Survey 2021. https://www.census.gov/programs-surveys/acs Retrieved from.
- Artiga S., Orgera K., Damico A. Kaiser Family Foundation; 2020. Changes in Health Coverage by Race and Ethnicity since the ACA, 2010-2018.https://www.kff.org/racial-equity-and-health-policy/issue-brief/changes-in-health-coverage-by-race-and-ethnicity-since-the-aca-2010-2018/ Retrieved from. [Google Scholar]
- CDC . 2020. CDC Research on SDOH.https://www.cdc.gov/socialdeterminants/index.htm [Google Scholar]
- Chang S.H., Yu Y.C., Carlsson N.P., Liu X., Colditz G.A. Racial disparity in life expectancies and life years lost associated with multiple obesity-related chronic conditions. Obesity. 2017;25(5):950–957. doi: 10.1002/oby.21822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C., Liu L.-M. Joint estimation of model parameters and outlier effects in time series. J. Am. Stat. Assoc. 1993;88(421):284. doi: 10.2307/2290724. [DOI] [Google Scholar]
- Chen J.T., Krieger N. Journal of Public Health Management and Practice. 2020. Revealing the unequal burden of COVID-19 by income, race/ethnicity, and household crowding: US county versus zip code analyses.https://journals.lww.com/jphmp/Fulltext/9000/Revealing_the_Unequal_Burden_of_COVID_19_by.99237.aspx Retrieved from. [DOI] [PubMed] [Google Scholar]
- Egede L.E., Walker R.J. Structural racism, social risk factors, and Covid-19—a dangerous convergence for black Americans. N. Engl. J. Med. 2020;383(12):e77. doi: 10.1056/NEJMp2023616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferdows N.B., Aranda M.P., Baldwin J.A., Baghban Ferdows S., Ahluwalia J.S., Kumar A. Assessment of racial disparities in mortality rates among older adults living in US rural vs urban counties from 1968 to 2016. JAMA Network Open. 2020;3(8) doi: 10.1001/jamanetworkopen.2020.12241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garfield R., Damico A. 2015. The Coverage Gap: Uninsured Poor Adults in States that Do Not Expand Medicaid. The Kaiser Commission on Medicaid and the Uninsured; pp. 1–9.http://kaiserfamilyfoundation.files.wordpress.com/2013/10/8505-the-coverage-gap-uninsured-poor-adults8.pdf Retrieved from. [Google Scholar]
- Hawkins D. Differential occupational risk for COVID-19 and other infection exposure according to race and ethnicity. Am. J. Ind. Med. 2020;63(9):817–820. doi: 10.1002/ajim.23145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsiang W.R., Lukasiewicz A., Gentry M., Kim C.-Y., Leslie M.P., Pelker R., Wiznia D.H. Medicaid patients have greater difficulty scheduling health care appointments compared with private insurance patients: a meta-analysis. Inquiry: The Journal of Health Care Organization, Provision, and Financing. 2019;56 doi: 10.1177/0046958019838118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarvie J. Los Angeles Times; 2020. Georgia Reopened First. What the Data Show Is a Matter of Fierce Debate.https://www.latimes.com/world-nation/story/2020-05-23/georgia-reopened-first-the-data-say-whatever-you-want-them-to Retrieved from. [Google Scholar]
- Knight V., Appleby J. 2020. How COVID Death Counts Become the Stuff of Conspiracy Theories.https://khn.org/news/how-covid-death-counts-become-the-stuff-of-conspiracy-theories/ Retrieved November 20, 2020, from Kaiser Health News website: [Google Scholar]
- Leeb R.T., Price S., Sliwa S., Kimball A., Szucs L., Caruso E. COVID-19 trends among school-aged children — United States, March 1-september 19, 2020. MMWR (Morb. Mortal. Wkly. Rep.) 2020;69(39):1410–1415. doi: 10.15585/mmwr.mm6939e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- López-de-Lacalle J. 2019. R Package Tsoutliers. [Google Scholar]
- Lu X., Zhang L., Du H., Zhang J., Li Y.Y., Qu J., Li Y. SARS-CoV-2 infection in children. N. Engl. J. Med. 2020;382(17):1663–1665. doi: 10.1056/NEJMc2005073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ludvigsson J.F. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatrica, International Journal of Paediatrics. 2020;109(6):1088–1095. doi: 10.1111/apa.15270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manson S., Schroder J., Van Riper D., Kugler T., Ruggles S. 2021. IPUMS National Historical Geographic Information System. [DOI] [Google Scholar]
- Mervosh S., Lu D., Swales V. 2020. See Which States and Cities Have Told Residents to Stay at Home.https://www.nytimes.com/interactive/2020/us/coronavirus-stay-at-home-order.html New York Times. Retrieved from. [Google Scholar]
- National Conference of State Legislatures . 2020. COVID-19: Essential Workers in the States.https://www.ncsl.org/research/labor-and-employment/covid-19-essential-workers-in-the-states.aspx [Google Scholar]
- NCHS . 2021. Life Expectancy.https://www.cdc.gov/nchs/data-visualization/life-expectancy/ Retrieved from. [Google Scholar]
- Neprash H.T., Zink A., Gray J., Hempstead K. Physicians' participation in medicaid increased only slightly following expansion. Health Aff. 2018;37(7):1087–1091. doi: 10.1377/hlthaff.2017.1085. [DOI] [PubMed] [Google Scholar]
- Payne A.B., Mehal J.M., Chapman C., Haberling D.L., Richardson L.C., Bean C.J., Hooper W.C. Trends in Sickle Cell disease–related mortality in the United States, 1979 to 2017. Ann. Emerg. Med. 2020;76(3):S28–S36. doi: 10.1016/j.annemergmed.2020.09.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poteat T., Millett G.A., Nelson L.R.E., Beyrer C. Understanding COVID-19 risks and vulnerabilities among black communities in America: the lethal force of syndemics. Ann. Epidemiol. 2020;47:1–3. doi: 10.1016/j.annepidem.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raifman M.A., Raifman J.R. Disparities in the population at risk of severe illness from COVID-19 by race/ethnicity and income. Am. J. Prev. Med. 2020;59(1):137–139. doi: 10.1016/j.amepre.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selden T.M., Berdahl T.A. COVID-19 and racial/ethnic disparities in health risk, employment, and household composition. Health Aff. 2020;39(9):1624–1632. doi: 10.1377/hlthaff.2020.00897. [DOI] [PubMed] [Google Scholar]
- Tai D.B.G., Shah A., Doubeni C.A., Sia I.G., Wieland M.L. Clinical Infectious Diseases; 2020. The Disproportionate Impact of COVID-19 on Racial and Ethnic Minorities in the United States. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thakur N., Lovinsky-Desir S., Bime C., Wisnivesky J.P., Celedón J.C. The structural and social determinants of the racial/ethnic disparities in the U.S. COVID-19 pandemic what's our role? Am. J. Respir. Crit. Care Med. 2020;202(7):943–949. doi: 10.1164/rccm.202005-1523PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Townsend M.J., Kyle T.K., Stanford F.C. Outcomes of COVID-19: disparities in obesity and by ethnicity/race. Int. J. Obes. 2020;44(9):1807–1809. doi: 10.1038/s41366-020-0635-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau . 2020. County Population Totals: 2010-2019. [Google Scholar]
- Weinberger D.M., Chen J., Cohen T., Crawford F.W., Mostashari F., Olson D., Viboud C. Estimation of excess deaths associated with the COVID-19 pandemic in the United States, March to may 2020. JAMA Internal Medicine. 2020:6520. doi: 10.1001/jamainternmed.2020.3391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolf S.H., Schoomaker H. Life expectancy and mortality rates in the United States, 1959-2017. JAMA - Journal of the American Medical Association. 2019;322(20):1996–2016. doi: 10.1001/jama.2019.16932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yehia B.R., Winegar A., Fogel R., Fakih M., Ottenbacher A., Jesser C., Cacchione J. Association of race with mortality among patients hospitalized with coronavirus disease 2019 (COVID-19) at 92 US hospitals. JAMA Network Open. 2020;3(8) doi: 10.1001/jamanetworkopen.2020.18039. [DOI] [PMC free article] [PubMed] [Google Scholar]