Abstract
Around 15% of children and adolescents in Germany are overweight or obese. To support the planning, implementation and evaluation of preventive activities, the Robert Koch Institute (RKI) has developed a population-wide monitoring of influencing factors relevant to the development of obesity during childhood (AdiMon). AdiMon is a web-based indicator system providing population-wide meaningful and regularly updated data on factors that influence obesity in kindergarten-age girls and boys (0- to 6-years-old). Towards the end of 2020, the RKI will expand the indicator system to also cover the 7- to 17-year-old age group. To this end, a systematic review of the literature was conducted, a process which served to identify over 80 relevant factors that influence the development of obesity. These factors have been attributed to the categories behaviour, environment, biology, pre- and postnatal, psychosocial factors and context. Compared to a previous literature review for kindergarten-age children, around one tenth of the influencing factors now identified are new, including ‘peer group influences’ and ‘bullying’. As the results highlight, an array of influencing factors must be considered when expanding the monitoring system, ranging from individual health behaviour to the social framework conditions and environmental factors.
Keywords: SYSTEMATIC REVIEW, OBESITY, CHILDREN AND ADOLESCENTS, PREVENTION, INFLUENCING FACTORS
1. Introduction
Obesity is considered one of the key public health challenges of our time. Around 15% of children and adolescents in Germany are overweight, approximately 6% are obese [1]. Frequently, obese children and adolescents are also likely to become overweight or obese adults [2]. Being overweight or obese during childhood and adolescence can already cause health problems, with potentially severe health implications later in life [3]. Adult-age obesity is related to metabolic disorders and cardiovascular diseases, certain types of cancer and increased mortality rates [4]. A positive energy balance (taking up more energy than one requires) and biological influencing factors cannot solely explain obesity. Rather, the condition results from a complex interplay between numerous factors [5]. Individual genetic dispositions interact with an environment that has undergone considerable change over the last century and which, in industrialised nations, is characterised for example by a general availability of energy-rich foods. The settings in which individuals live, such as family, school and the community, are themselves influenced by the social, economic and political framework conditions. Key risk and protective factors, such as a health-promoting lifestyle, are acquired during early childhood, meaning that the settings a child grows up in can either reinforce or reduce the influence of such factors. Preventing obesity during childhood and adolescence is therefore of particular importance [6]. To stop the spread of obesity, the World Health Organization (WHO) recommends broad monitoring [7]. Monitoring systems can play a vital role in the planning, implementation and evaluation of prevention measures. Against this backdrop, the Federal Ministry of Health (BMG) has funded the AdiMon project at the Robert Koch Institute (RKI) to develop a population-wide monitoring of factors that influence obesity at childhood age (AdiMon). AdiMon is an web-based indicator system that provides population-wide meaningful and regularly updated data on factors that influence obesity at kindergarten age (0- to 6-years-old) [8, 9]. To describe the diverse set of factors that influence obesity, numerous sources of data were used, and meaningful indicators were developed. These were put into scientific context and published in concise fact sheets.
Beyond kindergarten, school age is a further key stage for the prevention of obesity. The prevalence of obesity among school-age boys and girls increases significantly. While 3.2% of 3- to 6-year old girls and 1.0% of boys are obese, for 14- to 17-year-old adolescents the figures are 7.7% (girls) and 9.2% (boys) [1]. Yet it is not only the prevalences of obesity that increase at school age; children and adolescents who are obese at school age are also more frequently obese as adults than children who are obese in kindergarten [10, 11]. School entry age is therefore considered a critical moment for the manifestation of obesity among children and adolescents. Against this backdrop, it is important to focus on the causes and spread of obesity among girls and boys at school age. By the end of 2020, we will therefore have expanded the indicator system to also cover the 7- to 17-year-old group. For this age group, the school setting is a key factor whose importance is increasing with the spread of all-day schools [12]. Entering school leads to great changes in the lives of children. With primary school, children’s everyday family routines become fundamentally restructured and demands on children increase, e. g. the need to be punctual and sit all day [13]. Furthermore, adolescence is a life phase characterised by numerous changes and challenges. During the biological process of development, the puberty, adolescent’s bodies undergo physiological and hormonal changes that they must confront. At the psychosocial level, the step from childhood to adolescence is characterised by the development of a more individual personality structure and people’s ever greater independence in their social environment [13]. For adolescents, the role played by peers regarding health behaviour increases in a phase where they are becoming ever more independent of their parents [14, 15]. To take account of this special phase in life, and to expand the indicator system, a systematic review of the literature to detect relevant influencing factors for obesity in school-age girls and boys was conducted. In the following, we present and discuss the methodological approach that was applied in the literature review, as well as the results. The latter provided us with a basis to expand the current monitoring system, because so far systematically compiled data on the causes and levels of obesity among school-age girls and boys in Germany had not been available.
2. Methodology
This systematic review of the literature was conducted in December 2018 in the Scopus, PubMed and Embase databases, the Web of Science and the Cochrane Library. Systematic reviews published between 2006 and 2018 were taken into account. The search string was built on the terminological categories influencing factor (determinants, causes, correlates, predictors, factors, origins, etiology, and understanding), obesity (obesity, adiposity) and target group (child, youth, adolescent). By using Boolean operators, keywords and wildcards, a database conforming combination of the three categories was created, whereby searches were limited to the titles and abstracts of publications.
After removing duplicates, the titles and abstracts were reviewed and the full texts read. Articles were excluded which were (1) not systematic reviews; (2) conference contributions; or (3) systematic reviews on measures and interventions. Further exclusion criteria were (4) no relevance of the influencing factors in Germany (for example an analysis of the role played by socioeconomic status in developing countries); (5) no relevance of an influencing factor for the population as a whole (such as rare genetic diseases); (6) lacking relevance of an influencing factor for the 7- to 17-year-old age group; and (7) no obesity relevant outcome. Furthermore, when (8) articles were published in non-covered languages (all languages except for German, English, Spanish and Portuguese), or (9) when the full text of an article was not available, the corresponding publications were also excluded.
The influencing factors identified in the reviews were inserted into a table matrix and differentiated by influencing area. The entire process was conducted as a dual control process. The literature was reviewed and influencing factors identified independently by two researchers. When cross-checking resulted in differences in the identified influencing factors, these were discussed together with a third researcher until consensus was achieved.
For the identified influencing factors, the following step consisted in evaluating the evidence provided. Information on the methodology applied and the results of the studies considered by the reviews was therefore gathered (Figure 1). Three levels of evidence were distinguished: convincing, sufficient and insufficient. Influencing factors were excluded if in the majority of studies on which reviews were based (at least three studies), no indication could be provided for a relationship with the development of obesity during childhood and adolescence. Influencing factors with only insufficient evidence were nonetheless included to take into account more recent research results with fewer studies. The influencing factors identified by the literature review were discussed during a workshop in May 2019 with external experts from public health practice, politics and science, and consolidated and evaluated with regard to their relevance for the prevention of obesity.
Figure 1.
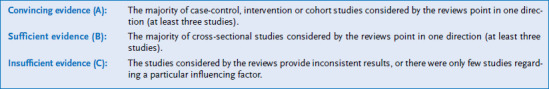
Evaluation of evidence
Source: Own figure
While the AdiMon system of indicators does consider measures and interventions relevant to the field of obesity, for methodological reasons these were not part of this literature review, because reviews on influencing factors and interventions appeared to require different search strategies. Correspondingly, over the course of the project, a further literature review will therefore be conducted. It will provide information on the scientific evidence regarding measures and interventions relevant to obesity at the individual, setting and population level.
3. Results
The described literature review provided 2,959 hits, of which 280 fulfilled our inclusion criteria (Figure 2). A total of 80 influencing factors that are relevant to the development of obesity in school-age girls and boys in Germany were identified. Around one tenth of these are factors that were not identified by the AdiMon project review conducted for kindergarten-age children [9].
Figure 2.
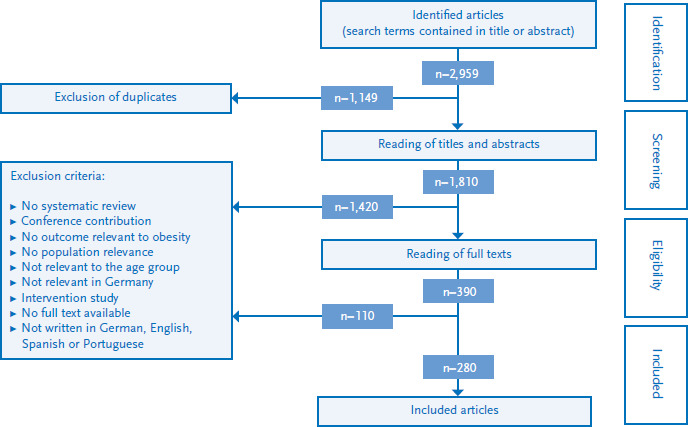
Flow diagram on the systematic literature review
Source: Own diagram
The detected influencing factors were categorised according to the areas behaviour, environment, biology, pre- and postnatal, psychosocial factors and context shown in the simplified cause and effect model (Figure 3). The model was developed during the initial phases of obesity monitoring for kindergarten-age children [8]. It shows that behavioural (such as physical activity) and biological factors (such as genetic disposition) are relevant for the development of obesity. Also prenatal factors (such as weight gain by mothers during pregnancy) and factors during early childhood (such as breastfeeding) influence the development of obesity. Furthermore, psychosocial factors (such as how parents perceive the weight of their children) can impact the development of obesity during childhood and adolescence. Environmental factors are mostly related to the settings a child grows up in, such as family, neighbourhood or kindergarten (for example the food offered there). The mentioned influencing factors are themselves influenced by contextual factors. These include cultural and sociodemographic factors (such as poverty). Moreover, prevention and health promotion measures can influence the levels of childhood obesity. We will now discuss these areas in more detail and describe them in correlation to the results of some identified reviews. An overview of all the influencing factors identified in the review of the literature is included in the annex (Annex Table 1).
Figure 3.
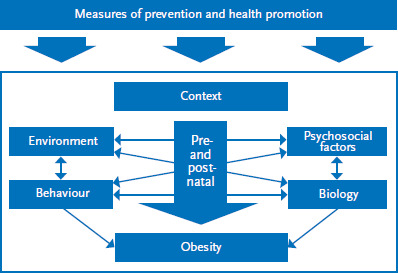
Simplified cause-effect model of obesity at child and adolescent age
Source: Modified according to Varnaccia et al. 2017 [8]
3.1 Behaviour
Nutrition
A positive energy balance, which occurs when caloric intake exceeds energy expenditure, is considered the central cause of obesity [16]. Consuming high-energy-dense foods and meals can favour a positive energy balance and promote obesity [17]. It is assumed that when consuming high-energy-dense meals compared to low-energy-dense meals, more energy is taken up by the body before satiety is felt [17]. Concerning nutrient intake, consuming large amounts of simple carbohydrates, proteins and fats are being discussed as factors that could encourage obesity, as opposed to consuming high amounts of dietary fibre, which it is presumed to reduce a person’s likelihood of becoming obese [18–21]. Numerous longitudinal studies have related the regular consumption of sugar-sweetened beverages and fast food to the development of obesity in children and adolescents [22, 23]. Regularly eating fruit and vegetables are considered factors that protect against becoming obese, even though the results of longitudinal studies for children and adolescents are not entirely consistent [24].
Physical activity, sedentary lifestyle and sleep
As it increases energy expenditure and contributes to a more even energy balance, physical activity is considered to be a factor protecting children and adolescents from becoming obese. Several cross-sectional and longitudinal studies have shown an inverse relationship between physical activity and childhood obesity [25, 26]. A sedentary lifestyle and in particular using screen-based media can promote obesity [27]. In addition to the reduced energy requirements of people with a sedentary lifestyle, the effects of advertisements for particular foods (such as sweets) and the consumption of energy-rich foods while using screen-based media are being discussed as potential causes for an increased obesity risk [28]. Studies concerning the 7- to 17-year-old population are, however, not consistent. Too little sleep is a further obesity risk factor currently being discussed, a habit that can cause alterations to the metabolism and at the hormonal level that favour obesity. Longitudinal study results support this hypothesis [29].
3.2 Environments
Living environments
The living environments of children and adolescents play an important role in the development of obesity. We use the term living environment here in the sense of a definable social system to describe the framework conditions in which people live, learn, work and consume [30]. Relevant living environments for school-age girls and boys are the family and home, school and their immediate neighbourhoods (such as the municipality in which they live). Parent weight and health behaviour are principal influencing factors of the family. A meta-analysis indicates that children whose parents are obese have a significantly higher obesity risk [31]. This relationship was stronger for older than for younger children, as well as when both parents were obese. Parent weight has a strong genetic and epigenetic component, which means there are overlaps with biological factors. A number of correlation studies provide insights into how parental health behaviour, such as dietary habits and levels of physical activity, play out in children [32]. Moreover, a review relying principally on cross-sectional studies indicated that shared family meals are associated with a lower obesity risk [33]. For the school environment, a negative influence of unhealthy food options on the weight of adolescents is being discussed; however, only very few studies to date have confirmed such a correlation [34]. For the living environment municipality, the availability of spaces that encourage physical activity [35], security of residential areas [36] and shopping and food options that promote a healthy diet [35] are considered to be factors that protect against obesity. However, the results in the identified reviews, which are mostly based on cross-sectional studies, are inconsistent.
Economic factors
Economic factors that are being discussed as influencing obesity in school-age children and adolescents include the cost of participating in physical activities as well as the price of food and meals. The few available studies show that accessible prices for exercise opportunities can help increase levels of physical activity, as well as that increases to the price of fruit and vegetables are associated with gaining weight [37, 38]. In addition, cross-sectional and longitudinal studies show that advertisements for high-energy-dense foods (TV ads for sweets or campaigns sponsored by the producers of foods that promote obesity) can increase the consumption of such foods and therefore promote obesity [39].
3.3 Biological factors
Numerous longitudinal studies have shown that genetic predispositions increase the obesity risk of children and adolescents [40, 41]. Furthermore, certain hormones (such as leptin [42]) and the composition of a person’s intestinal flora [43] are being discussed as relevant influencing factors for obesity. Leptin plays a role in managing hunger and satiety and is fundamental to the energy balance. Raised serum leptin levels have been observed in obese children [42]. A number of mechanisms are being discussed to explain the influence the gut microbiota has, such as gaining energy from indigestible carbohydrates as an additional source of energy [43]. Further potentially relevant biological influencing factors under discussion include certain diseases (such as asthma [44]), virus infections (for example adenovirus infections [45]), as well as the side-effects of certain medications (such as antibiotics [46]). Furthermore, levels of physical fitness have also been related to developing obesity. Several longitudinal studies show that high cardio-respiratory fitness (endurance), good motor capacity and pronounced muscular fitness can prevent obesity in children and adolescents [47–49]. Compared to physical activity, which describes a specific behaviour, physical fitness is a physical trait and therefore related to biology.
3.4 Pre- and postnatal
Pregnancy
Maternal obesity in the early stages of pregnancy increases the likelihood of their children being obese during childhood and adolescence. Numerous prospective studies provide consistent results for this hypothesis [50, 51]. In addition, several longitudinal show that high maternal weight gain during pregnancy and (gestational) diabetes are risk factors for the development of obesity during childhood and adolescence [51, 52]. The same holds true for mothers who smoke during pregnancy [53, 54].
Early childhood
The results of systematic reviews that consider a high birth weight and rapid weight gain after birth are largely consistent. The results show that these factors can promote obesity at child and adolescent age [55, 56]. Breastfeeding, to the contrary, appears to be a protective factor. As numerous longitudinal studies have shown, how long and how (e.g. exclusive breastfeeding or breastfeeding and complementary feeding) a baby is breastfed potentially influence obesity risks [57, 58].
3.5 Psychosocial factors
Children and adolescents
Certain psychosocial factors are being discussed as potentially relevant for child and adolescent obesity. Various long-term studies indicate depression could promote obesity among girls and boys [59]. It is assumed this association is bi-directional, i.e. obesity would then also be a risk factor for depression. Factors that could encourage obesity in the context of a manifest depression and that are currently being discussed include changes to appetite and dietary habits, such as developing a preference for carbohydrate-rich foods, as well as more sedentary habits and sleeping disorders [60]. A number of cross-sectional studies have highlighted a connection between stressful (traumatic) life events, such as suffering violence, and a greater risk of becoming obese [61, 62]. High levels of stress, eating disorders (such as binge eating) and suffering bullying are further influencing factors that encourage obesity and have been described in the literature [60–63]. Longitudinal studies have also shown a weak connection between low self-esteem and the risk of becoming overweight or obese [59]. Overall, the evidence for the stated psychosocial influencing factors has to be rated insufficient and there is a lack of models to explain relationships and effect mechanisms.
Parents and the peer group
Parents facing high levels of stress and mothers suffering from depression can increase a child’s obesity risk [64, 65]. How parents perceive a child’s weight can also be a relevant factor in whether a child becomes obese or not. It is assumed that parents who are conscious that their children are overweight will take action to prevent them from becoming obese [66]. In addition, low levels of parental health literacy could encourage childhood obesity [67]. Moreover, for adolescents, the influence of their peer group can lead to similar weight developments and obesity related behaviours [68]. To date, these influencing factors have only been insufficiently studied.
3.6 Context
Longitudinal studies indicate that in high income countries such as Germany children and adolescents of low socioeconomic status are more often overweight or obese than their peers from high status groups [69]. In particular, a low parental educational level is considered a risk factor for children and adolescents with regard to the development of obesity, and this factor plays out more heavily in younger than older children. [70]. It is assumed that a low parental educational level is often associated with little health knowledge and only insufficient health literacy, making a health-promoting lifestyle (for example a balanced diet) less probable and therefore supporting the development of obesity in children [70]. Longitudinal studies underline that a low household income can be a risk factor for the development of obesity in children and adolescents, as limited financial resources make it more difficult to access leisure-time activities that involve physical activity and to pay for a healthy diet [71].
In cross-sectional studies it has been observed that children and adolescents with a migration background are more frequently overweight or obese than adolescents with no migration background. Differences in diet and physical activity are thereby mentioned as possible explanations [72]. Importantly, however, the influence a migration background has on becoming obese depends on a number of different factors and having a migration background in Germany is often related to further factors that can encourage obesity (for example a lack of financial resources) [73].
4. Discussion
This article aims to provide an up-to-date overview of the factors influencing obesity in school-age girls and boys and which are the basis for the indicators of a population-wide monitoring system. As the results of the literature review emphasise, the causes of obesity in school-age girls and boys are diverse and not limited to factors of individual behaviour. Comparisons with the established explanatory models for obesity at child and adolescent age also highlight this [74, 75]. Between the identified factors, it is presumed that links and diverse interactions at numerous levels exist [76]. In addition, the different areas play out differently in the development of obesity regarding their direct or indirect influence (Figure 3). Based on this literature review, it is not possible to quantify the effects of particular factors, as other studies have attempted to do [77–79]. However, the diversity of the influencing factors that were identified highlights that tackling obesity in childhood and adolescence calls for measures in more than just one area. Rather, the strategy should aim to develop health promoting framework conditions in living environments, as this would encourage positive health behaviour [80]. However, this depends on equally addressing the political and economic framework conditions. Monitoring thereby plays a key role: it ensures that developments over time can be tracked and needs to take action can be recognised at an early stage, thereby providing important insights for the planning, implementation and evaluation of prevention measures and strategies [81].
Systematic literature reviews have their limitations. We have accounted for publications with the outcome obesity, but also with a number of alternative outcomes, such as changes of other anthropometric measures (such as body mass index) or behaviours relevant to obesity (such as physical activity). Restricting ourselves to systematic reviews and a search string that looks at titles and the abstract of publications are further limitations. There were also certain limitations with regard to the age groups. The age groups described in the literature often did not fit precisely the 7- to 17-year-old group and only considered a subgroup or also included younger and/or older people. To simplify matters, the terms child and adolescent were therefore used in the results section. It is also important to mention that substantial discrepancies existed in the number of studies found for each factor. The majority of the identified publications dealt with behaviour-related and biological influencing factors. For the areas environment, context, psychosocial factors, as well as pre- and postnatal factors, the search provided fewer systematic reviews. The differing number of identified reviews for specific influence fields possibly also influenced the evaluation of evidence. The synopsis of influencing factors included all factors associated with obesity. These include findings from cross-sectional studies, which do not allow a clean separation of cause and effect and are therefore less robust. This means that in some cases it remains unclear whether the observed relationships are causal, as well as which side of this causality is the effect and how the mechanisms underlying these effects are structured. In addition, the influencing factors which have been considered as only insufficiently researched should nonetheless be considered in the population-wide monitoring. Mostly these are from the areas environment and psychosocial factors, and were included to account for a broad spectrum of influencing factors. To prevent distortions in the compilation of influencing factors and the evaluation of supporting evidence, the results of the literature review were consolidated during a workshop with external experts.
Conclusion
The results of our systematic review of the literature highlight the complex structure of influencing factors that underlie obesity in school-age girls and boys. Compared to an earlier review on factors that influence the obesity of 0- to 6-year-old children, new influencing factors were identified for the 7- to 17-year-old group. These include aspects from the school environment and factors that gain in importance at secondary school age, such as the influence of the peer group or having suffered bullying.
The literature review also showed that over the last years the causes of obesity among children and adolescents have been amply researched. Further research is nonetheless required. For environmental and psychosocial influencing factors, for example, only few studies are so far available. More findings are required that would allow us to assess the relevance of particular influencing factors for the development of obesity, explain the underlying effect mechanisms and provide effective settings-based prevention measures. Furthermore, future concepts of obesity prevention will need to be based within a broader context. This could include considering the development of indicators to account for the interactions between obesity prevention and environmental and climate aspects [82].
The next step of the AdiMon project will involve reaching a consensus between experts on robust indicators for specific influencing factors, and acquiring the corresponding data sources. Until October 2020, the new indicators for school-age children and adolescents will be integrated into the existing system of indicators and published on the AdiMon website. In the medium to long term, AdiMon will be updated regularly and thereby allow us to map the changes of the diverse influencing factors. AdiMon will thereby provide starting points for new and adequate prevention strategies that will target the individual-, setting- and population-level.
Key statements
The systematic literature review provided over 80 factors relevant to the development of obesity in school-age girls and boys.
Obesity results from a complex interplay between numerous influencing factors from a number of fields.
Compared to a previous literature review for kindergarten-age children conducted in the context of the AdiMon project, the number of identified influencing factors has increased by around one tenth.
The identified reviews mostly focused on behavioural and biological influencing factors.
Environmental and psychosocial influencing factors were only examined by a small number of systematic reviews.
Annex Table 1.
Influencing factors of obesity in school-age girls and boys (updated: May 2019)
Source: Own table
| Influencing factor | Relationship | Literature* |
|---|---|---|
| Behaviour | ||
| Physical activity | ||
| Physical activity | Regular physical activity can help prevent obesity. | [1, 2] |
| Sports activity | Regular sports activity can help prevent obesity | [3, 4] |
| Sedentary behaviour | ||
| Sitting time | Regularly spending time sitting can favour obesity. | [5, 6] |
| Screen time | Regularly spending time in front of a screen can favour obesity. | [5, 7] |
| Diet | ||
| Energy intake | Taking up a high amount of energy can favour obesity. | [8] |
| Carbohydrates | Taking up large amounts of carbohydrates and/or consuming particular types of carbohydrates such as fructose, can favour obesity. | [9–11] |
| Proteins | Taking up large amounts of proteins in early childhood can favour obesity. | [12] |
| Fat | Taking up large amounts of fat can favour obesity. | [13] |
| Fibres | Taking up large amounts of fibres can help prevent obesity. | [14] |
| Vitamins and minerals | Vitamin and mineral uptake can be a relevant factor for obesity. | [15–17] |
| Energy density | High-energy-density foods can favour obesity. | [18] |
| Sugar-sweetened beverages | Regularly consuming sugar-sweetened beverages can favour obesity. | [19] |
| Fruit and vegetables | Regularly eating fruit and vegetables can prevent obesity. | [20] |
| Fast food | Regularly eating fast food can favour obesity. | [21, 22] |
| Milk and milk products | Regularly consuming milk and milk products can help prevent obesity. | [23] |
| Dietary patterns | Particular dietary patterns (such as eating mainly highly processed foods) can be a relevant factor for obesity. | [24] |
| Meal frequency | A high frequency of meals can help prevent obesity. | [25] |
| Breakfast | Regularly eating breakfast can help prevent obesity. | [26] |
| Sleep | ||
| Sleep duration | A short sleep duration can favour obesity. | [27–29] |
| Environment | ||
| Living environment | ||
| Parental obesity | Parental obesity can favour obesity in their children. | [30] |
| Parental health behaviour | A healthy parental lifestyle can help prevent obesity in their children. | [31] |
| Sibling health behaviour | A healthy lifestyle of siblings can help prevent obesity. | [31] |
| Home food environment | A balanced offer of food and meals at home can help prevent obesity. | [31] |
| Shared family meals | Shared family meals can help prevent obesity. | [32] |
| School food environment | A balanced offer of food and meals at school can help prevent obesity. | [33] |
| Opportunities for physical activity at school | Spaces and opportunities for physical activity at school can help prevent obesity. | [34] |
| Spaces for physical activity in the neighbourhood | Spaces for physical activity in the neighbourhood (such as parks, sports facilities, playground) can help prevent obesity. | [35] |
| Sports offers | Sports offers (for example sports clubs) can help prevent obesity. | [34] |
| Activity-promoting infrastructure | Activity-promoting infrastructure (for example walkability) can help prevent obesity. | [35] |
| Security in the neighbourhood | A secure environment in the neighbourhood or one that is perceived as being secure can help prevent obesity. | [36] |
| Shops and food options | Shops and food options (for example fast food restaurants) can be a relevant factor for obesity. | [35] |
| Degree of urbanisation | Growing up in rural communities can favour obesity. | [37] |
| Regional deprivation | Growing up in a deprived area can favour obesity. | [38] |
| Economic factors | ||
| Costs related to physical activities | Costs related to physical activities can be a relevant factor for obesity. | [34] |
| Prices of food and meals | The price of food and meals can be a relevant factor for obesity. | [39] |
| Advertisements | Advertisements for high-energy-density foods can favour obesity. | [40] |
| Other factors | ||
| Pollutants | Certain pollutants (such as bisphenol A) can favour obesity. | [41] |
| Portion sizes | Large portion sizes can favour obesity. | [42] |
| Biology | ||
| Genetic factors | ||
| Genes and gene combinations | Certain genes and combinations of genes can be relevant factors for obesity. | [43] |
| Hormonal factors | ||
| Hormones | Certain hormones (such as leptin) can be a relevant factor for obesity. | [44] |
| Micro-biological factors | ||
| Intestinal flora | Intestinal flora composition can be a relevant factor for obesity. | [45] |
| Physical fitness | ||
| Motor fitness | Strong motor fitness can help prevent obesity. | [46] |
| Cardio-respiratory fitness | Strong cardio-respiratory fitness can help prevent obesity. | [47] |
| Muscular fitness | Strong muscular fitness can help prevent obesity. | [48] |
| Other factors | ||
| Puberty | Precocious puberty can favour obesity. | [49] |
| Diseases and viruses | Certain diseases (such as autism and asthma) and viruses (such as adenoviruses) can favour obesity. | [50–52] |
| Medication | Certain medications (such as antibiotics) can favour obesity. | [53, 54] |
| Pre and postnatal | ||
| Pregnancy | ||
| Maternal body mass index | A high maternal body mass index in the early stages of pregnancy can favour childhood obesity. | [55, 56] |
| Maternal weight gain | A high maternal weight gain during pregnancy can favour childhood obesity. | [55, 57] |
| Maternal diabetes | Maternal (gestational) diabetes during pregnancy can favour childhood obesity. | [55, 58] |
| Maternal smoking | Maternal smoking during pregnancy can favour childhood obesity. | [59, 60] |
| Maternal passive smoking | Maternal passive smoking during pregnancy can favour childhood obesity. | [59, 61] |
| Early childhood | ||
| Weight at birth | A high birth weight can favour obesity. | [55, 62] |
| Caesarean section | Caesarean section can favour obesity. | [63] |
| Breastfeeding | Breastfeeding can help prevent obesity. | [64, 65] |
| Duration of breastfeeding | Breastfeeding over an extended period can help prevent obesity. | [64, 65] |
| Form of breastfeeding | The form of breastfeeding (for example any form of breastfeeding, exclusive breastfeeding, bottle feeding) can be a relevant factor for obesity. | [55] |
| Complementary feeding | Early complementary feeding (before the fourth month) can favour obesity. | [66] |
| Rapid weight gain | A rapid weight gain during the first months of life can favour obesity. | [67] |
| Tonsillectomy | A tonsillectomy can favour obesity. | [68] |
| Child-care attendance | Attending child-care at an early age (0- to 2-years) can favour obesity. | [55] |
| Psychosocial factors | ||
| Children and adolescents | ||
| Personality traits | Certain personality traits (such as impulsivity, self-regulation) can be relevant factors for obesity. | [69] |
| Self-esteem | Having low self-esteem can favour obesity. | [70] |
| Family climate | An unfavourable family climate can favour obesity. | [71] |
| Parent-child relationship | A weak parent-child relationship can favour obesity. | [72] |
| Social support | Social support can help prevent obesity. | [73] |
| Stress | High levels of stress can favour obesity. | [74] |
| Stressful life events | Stressful life events (such as maltreatment) can favour obesity. | [75, 76] |
| Bullying | Bullying can favour obesity. | [76] |
| Eating disorders | Eating disorders (such as restrictive eating and binge eating) can favour obesity. | [77] |
| ADHD | Attention Deficit and Hyperactivity Disorder (ADHD) can favour obesity. | [78] |
| Depression | Depression can favour obesity. | [79] |
| Peer group | ||
| Peer group | The peer group can be relevant for obesity. | [80, 81] |
| Parents | ||
| Stress levels | High levels of parental stress can favour obesity in their children. | [82] |
| Depression | Maternal depression can favour childhood obesity. | [83] |
| Parental perception of child’s body weight | Parental misperception of their child’s body weight can favour childhood obesity. | [84, 85] |
| Health literacy | Insufficient parental health literacy can favour obesity in their children. | [86] |
| Parenting style | An authoritative parenting style can help prevent obesity. | [87, 88] |
| Feeding style | How and when a child is given food can be relevant for obesity. | [87] |
| Context | ||
| Sociodemographic factors | ||
| Social status | A low social status can favour obesity. | [89, 90] |
| Child’s educational level | A low child’s educational level can favour obesity. | [91] |
| Parental educational status | A low parental educational status can favour obesity in their children. | [91] |
| Parent employment | The numbers of hours parents work can be relevant for obesity in their children. | [89] |
| Poverty | Financial poverty can favour obesity. | [92] |
| Migration background | A migration background can be relevant for obesity. | [93] |
| Single parent families | Growing up in a single-parent household can favour obesity. | [31] |
| Siblings | Growing up as an only child can favour obesity. | [94] |
| Order of birth | The order of birth can be relevant for obesity. | [94] |
* The references represent a selected number of publications (in the review of the literature 280 relevant publications were identified).
Funding Statement
AdiMon receives funding from the Federal Ministry of Health (funding code: ZMVI1-2518KIG700).
Footnotes
The German version of the article is available at: www.rki.de/journalhealthmonitoring
Conflicts of interest
The authors declared no conflicts of interest.
Disclaimer
Note: External contributions do not necessarily reflect the opinions of the Robert Koch Institute
References
- 1.Schienkiewitz A, Brettschneider AK, Damerow S, et al. (2018) Overweight and obesity among children and adolescents in Germany. Results of the cross-sectional KiGGS Wave 2 study and trends. Journal of Health Monitoring 3(1):15–22. https://edoc.rki.de/handle/176904/5627.2 (As at 02.02.2020) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Simmonds M, Llewellyn A, Owen C, et al. (2016) Predicting adult obesity from childhood obesity: a systematic review and meta analysis. Obes Rev 17(2):95–107 [DOI] [PubMed] [Google Scholar]
- 3.Friedemann C, Heneghan C, Mahtani K, et al. (2012) Cardiovascular disease risk in healthy children and its association with body mass index: systematic review and meta-analysis. BMJ 345:e4759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Park MH, Falconer C, Viner RM, et al. (2012) The impact of childhood obesity on morbidity and mortality in adulthood: a systematic review. Obes Rev 13(11):985–1000 [DOI] [PubMed] [Google Scholar]
- 5.Butland B, Jebb S, Kopelman P, et al. (2007) Forsight Tackling obesities: future choices – project report. Government Office for Science, United Kingdom: [DOI] [PubMed] [Google Scholar]
- 6.Birch LL, Ventura AK. (2009) Preventing childhood obesity: what works? Int J Obes (Lond) 33:S74–S81 [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization (2016) Report of the commission on ending childhood obesity. WHO, Geneva [Google Scholar]
- 8.Varnaccia G, Zeiher J, Lange C, et al. (2017) Factors influencing childhood obesity – the establishment of a population-wide monitoring system in Germany. Journal of Health Monitoring 2(2):85–97. https://edoc.rki.de/handle/176904/2658 (As at 02.04.2020) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zeiher J, Varnaccia G, Jordan S, et al. (2016) Was sind die Einflussfaktoren kindlicher Adipositas? Eine Literaturübersicht im Rahmen des Projekts “Bevölkerungsweites Monitoring adipositasrelevanter Einflussfaktoren im Kindesalter”. Bundesgesundheitsbl 59(11):1465–1475 [DOI] [PubMed] [Google Scholar]
- 10.Plachta-Danielzik S, Landsberg B, Seiberl J, et al. (2012) Längsschnittdaten der Kieler Adipositas-Präventionsstudie (KOPS). Bundesgesundheitsbl 55(6-7):885–891 [DOI] [PubMed] [Google Scholar]
- 11.von Kries R, Beyerlein A, Müller MJ, et al. (2012) Different age-specific incidence and remission rates in pre-school and primary school suggest need for targeted obesity prevention in childhood. Int J Obes (Lond) 36(4):505–510 [DOI] [PubMed] [Google Scholar]
- 12.Leibniz-Institut für Bildungsforschung und Bildungsinformation, Deutsches Jugendinstitut, Institut für Schulentwicklungsforschung et al. (2019) Ganztagsschule 2017/2018. Deskriptive Befunde einer bundesweiten Befragung. Studie zur Entwicklung von Ganztagsschulen. Frankfurt am Main, Dortmund, Gießen, München, P. 154–158 [Google Scholar]
- 13.Robert Koch-Institut (Ed) (2009) Lebensphasenspezifische Gesundheit von Kindern und Jugendlichen in Deutschland. Ergebnisse des Nationalen Kinder- und Jugendgesundheitssurveys (KiGGS). Beiträge zur Gesundheitsberichterstattung des Bundes. RKI, Berlin [Google Scholar]
- 14.Harring M, Böhm-Kasper O, Rohlfs C, et al. (2010) Peers als Bildungs- und Sozialisationsinstanzen – eine Einführung in die Thematik. In: Harring M, Böhm-Kasper O, Rohlfs C, et al. (Eds) Freundschaften, Cliquen und Jugendkulturen. VS Verlag für Sozialwissenschaften, Wiesbaden, P. 9–19 [Google Scholar]
- 15.Pinquart M, Silbereisen RK. (2002) Gesundheitsverhalten im Kindes- und Jugendalter. Bundesgesundheitsbl 45(11):873–878 [Google Scholar]
- 16.Bleich SN, Ku R, Wang YC. (2011) Relative contribution of energy intake and energy expenditure to childhood obesity: a review of the literature and directions for future research. Int J Obes (Lond) 35(1):1–15 [DOI] [PubMed] [Google Scholar]
- 17.Perez-Escamilla R, Obbagy JE, Altman JM, et al. (2012) Dietary energy density and body weight in adults and children: a systematic review. J Acad Nutr Diet 112(5):671–684 [DOI] [PubMed] [Google Scholar]
- 18.Harland JI, Garton LE. (2008) Whole-grain intake as a marker of healthy body weight and adiposity. Public Health Nutr 11(6):554–563 [DOI] [PubMed] [Google Scholar]
- 19.Morenga LT, Mallard S, Mann J. (2013) Dietary sugars and body weight: systematic review and meta-analyses of randomised controlled trials and cohort studies. BMJ 345:e7492. [DOI] [PubMed] [Google Scholar]
- 20.Pearce J, Langley-Evans SC. (2013) The types of food introduced during complementary feeding and risk of childhood obesity: a systematic review. Int J Obes (Lond) 37(4):477–485 [DOI] [PubMed] [Google Scholar]
- 21.Naude CE, Visser ME, Nguyen KA, et al. (2018) Effects of total fat intake on bodyweight in children. Cochrane Database Syst Rev (7):CD012960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rosenheck R. (2008) Fast food consumption and increased caloric intake: a systematic review of a trajectory towards weight gain and obesity risk. Obes Rev 9(6):535–47 [DOI] [PubMed] [Google Scholar]
- 23.Bucher Della Torre S, Keller A, Laure Depeyre J, et al. (2016) Sugar-sweetened beverages and obesity risk in children and adolescents: a systematic analysis on how methodological quality may influence conclusions. J Acad Nutr Diet 116(4):638–659 [DOI] [PubMed] [Google Scholar]
- 24.Ledoux T, Hingle M, Baranowski T. (2011) Relationship of fruit and vegetable intake with adiposity: a systematic review. Obes Rev 12(5):e143-e150 [DOI] [PubMed] [Google Scholar]
- 25.Jimenez-Pavon D, Kelly J, Reilly JJ. (2010) Associations between objectively measured habitual physical activity and adiposity in children and adolescents: systematic review. Int J Pediatr Obes 5(1):3–18 [DOI] [PubMed] [Google Scholar]
- 26.Lee JE, Pope Z, Gao Z. (2018) The role of youth sports in promoting children's physical activity and preventing pediatric obesity: a systematic review. Ann Behav Med 44(1):62–76 [DOI] [PubMed] [Google Scholar]
- 27.Biddle SJH, Bengoechea EG, Wiesner G. (2017) Sedentary behaviour and adiposity in youth: a systematic review of reviews and analysis of causality. Int J Behav Nutr Phys Act 14(43) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Osei-Assibey G, Dick S, Macdiarmid J, et al. (2012) The influence of the food environment on overweight and obesity in young children: a systematic review. BMJ Open 2:e001538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Miller MA, Kruisbrink M, Wallace J, et al. (2018) Sleep duration and incidence of obesity in infants, children, and adolescents: a systematic review and meta-analysis of prospective studies. Sleep 41(4):1–19 [DOI] [PubMed] [Google Scholar]
- 30.Rosenbrock R, Hartung S. (2015) Settingansatz/Lebenswelt. E-Book: Leitbegriffe der Prävention und Gesundheitsförderung: Glossar zu Konzepten, Strategien und Methoden BZgA, Köln [Google Scholar]
- 31.Wang Y, Min J, Khuri J, et al. (2017) A systematic examination of the association between parental and child obesity across countries. Adv Nutr 8(3):436–448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cislak A, Safron M, Pratt M, et al. (2012) Family-related predictors of body weight and weight-related behaviours among children and adolescents: a systematic umbrella review. Child Care Health Dev 38(3):321–331 [DOI] [PubMed] [Google Scholar]
- 33.Valdes J, Rodriguez-Artalejo F, Aguilar L, et al. (2013) Frequency of family meals and childhood overweight: a systematic review. Pediatr Obes 8(1):e1–e13 [DOI] [PubMed] [Google Scholar]
- 34.Silden KE. (2018) Impact of competitive foods in public schools on child nutrition: effects on adolescent obesity in the United States an integrative systematic literature review. Glob Health Action 11(1):1477492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Casey R, Oppert JM, Weber C, et al. (2014) Determinants of childhood obesity: What can we learn from built environment studies? Food Qual Prefer 31(1):164–172 [Google Scholar]
- 36.An R, Yang Y, Hoschke A, et al. (2017) Influence of neighbourhood safety on childhood obesity: a systematic review and meta-analysis of longitudinal studies. Obes Rev 18(11):1289–1309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Safron M, Cislak A, Gaspar T, et al. (2011) Micro-environmental characteristics related to body weight, diet, and physical activity of children and adolescents: a systematic umbrella review. Int J Environ Health Res 21(5):317–330 [DOI] [PubMed] [Google Scholar]
- 38.Leal C, Chaix B. (2011) The influence of geographic life environments on cardiometabolic risk factors: a systematic review, a methodological assessment and a research agenda. Obes Rev 12(3):217–230 [DOI] [PubMed] [Google Scholar]
- 39.Kelly B, King L, Chapman K, et al. (2015) A Hierarchy of Unhealthy Food Promotion Effects: Identifying Methodological Approaches and Knowledge Gaps. Am J Public Health 105(4):E86–E95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Albuquerque D, Nobrega C, Manco L, et al. (2017) The contribution of genetics and environment to obesity. Br Med Bull 123(1):159–173 [DOI] [PubMed] [Google Scholar]
- 41.Silventoinen K, Rokholm B, Kaprio J, et al. (2010) The genetic and environmental influences on childhood obesity: a systematic review of twin and adoption studies. Int J Obes (Lond) 34(1):29–40 [DOI] [PubMed] [Google Scholar]
- 42.Arslan N, Erdur B, Aydin A. (2010) Hormones and cytokines in childhood obesity. Indian Pediatr 47(10):829–839 [DOI] [PubMed] [Google Scholar]
- 43.Indiani C, Rizzardi KF, Castelo PM, et al. (2018) Childhood obesity and firmicutes/bacteroidetes ratio in the gut microbiota: a systematic review. Child Obes 14(8):501–509 [DOI] [PubMed] [Google Scholar]
- 44.Leinaar E, Alamian A, Wang L. (2016) A systematic review of the relationship between asthma, overweight, and the effects of physical activity in youth. Ann Epidemiol 26(7):504–510 [DOI] [PubMed] [Google Scholar]
- 45.Shang QL, Wang HP, Song YJ, et al. (2014) Serological data analyses show that adenovirus 36 infection is associated with obesity: a meta-analysis involving 5739 subjects. Obesity 22(3):895–900 [DOI] [PubMed] [Google Scholar]
- 46.Miller SA, Wu RKS, Oremus M. (2018) The association between antibiotic use in infancy and childhood overweight or obesity: a systematic review and meta-analysis. Obes Rev 19(11):1463–1475 [DOI] [PubMed] [Google Scholar]
- 47.Cattuzzo MT, Henrique RD, Re AHN, et al. (2016) Motor competence and health related physical fitness in youth: a systematic review. J Sci Med Sport 19(2):123–129 [DOI] [PubMed] [Google Scholar]
- 48.Mintjens S, Menting MD, Daams JG, et al. (2018) Cardiorespiratory fitness in childhood and adolescence affects future cardiovascular risk factors: a systematic review of longitudinal studies. Sports Medicine 48(11):2577–2605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Smith JJ, Eather N, Morgan PJ, et al. (2014) The health benefits of muscular fitness for children and adolescents: a systematic review and meta-analysis. Sports Medicine 44(9):1209–1223 [DOI] [PubMed] [Google Scholar]
- 50.Yu ZB, Han SP, Zhu JG, et al. (2013) Pre-pregnancy body mass index in relation to infant birth weight and offspring overweight/obesity: a systematic review and meta-analysis. PLoS ONE 8(4) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Baidal JAW, Locks LM, Cheng ER, et al. (2016) Risk factors for childhood obesity in the first 1,000 days: a systematic review. Am J Prev Med 50(6):761–779 [DOI] [PubMed] [Google Scholar]
- 52.Tie HT, Xia YY, Zeng YS, et al. (2014) Risk of childhood overweight or obesity associated with excessive weight gain during pregnancy: a meta-analysis. Arch Gynecol Obstet 289(2):247–257 [DOI] [PubMed] [Google Scholar]
- 53.Rayfield S, Plugge E. (2017) Systematic review and meta-analysis of the association between maternal smoking in pregnancy and childhood overweight and obesity. J Epidemiol Community Health 71(2):162–173 [DOI] [PubMed] [Google Scholar]
- 54.Qureshi R, Jadotte Y, Zha P, et al. (2018) The association between prenatal exposure to environmental tobacco smoke and childhood obesity: a systematic review. JBI Database System Rev Implement Rep 16(8):1643–1662 [DOI] [PubMed] [Google Scholar]
- 55.Schellong K, Schulz S, Harder T, et al. (2012) Birth weight and long-term overweight risk: systematic review and a meta-analysis including 643,902 persons from 66 studies and 26 countries globally. PLoS ONE 7(10):e47776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zheng M, Lamb KE, Grimes C, et al. (2018) Rapid weight gain during infancy and subsequent adiposity: a systematic review and meta-analysis of evidence. Obes Rev 19(3):321–332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yan J, Liu L, Zhu Y, et al. (2014) The association between breastfeeding and childhood obesity: a meta-analysis. BMC Public Health 14:1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Newsome K, Rashid T, Vonville HM, et al. (2016) Mapping of reviews on breastfeeding and obesity risk in children. Curr Nutr Rep 5(4):255–277 [Google Scholar]
- 59.Incledon E, Wake M, Hay M. (2011) Psychological predictors of adiposity: systematic review of longitudinal studies. Int J Pediatr Obes 6:sup3, e1-11 [DOI] [PubMed] [Google Scholar]
- 60.Mannan M, Mamun A, Doi S, et al. (2016) Prospective associations between depression and obesity for adolescent males and females - a systematic review and meta-analysis of longitudinal studies. PLoS ONE 11(6):e0157240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Danese A, Tan M. (2014) Childhood maltreatment and obesity: systematic review and meta-analysis. Mol Psychiatry 19(5):544–554 [DOI] [PubMed] [Google Scholar]
- 62.Midei AJ, Matthews KA. (2011) Interpersonal violence in childhood as a risk factor for obesity: a systematic review of the literature and proposed pathways. Obes Rev 12(501):e159–e172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Russell-Mayhew S, McVey G, Bardick A, et al. (2012) Mental health, wellness, and childhood overweight/obesity. Int J Obes (Lond) 2012:281801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.O'Connor SG, Maher JP, Belcher BR, et al. (2017) Associations of maternal stress with children's weight-related behaviours: a systematic literature review. Obes Rev 18(5):514–525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lampard AM, Franckle RL, Davison KK. (2014) Maternal depression and childhood obesity: a systematic review. Prev Med 59:60–67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tompkins CL, Seablom M, Brock DW. (2015) Parental perception of child’s body weight: a systematic review. J Child Fam Stud 24(5):1384–1391 [Google Scholar]
- 67.Marks R. (2015) Childhood obesity and parental health literacy. Advances in Obesity, Weight Management & Control 3(3):00055 [Google Scholar]
- 68.Cunningham SA, Vaquera E, Maturo CC, et al. (2012) Is there evidence that friends influence body weight? A systematic review of empirical research. Soc Sci Med 75(7):1175–1183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wu SQ, Ding YY, Wu FQ, et al. (2015) Socio-economic position as an intervention against overweight and obesity in children: a systematic review and meta-analysis. Sci Rep 5:11354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kim TJ, Roesler NM, von dem Knesebeck O. (2017) Causation or selection - examining the relation between education and overweight/obesity in prospective observational studies: a meta-analysis. Obes Rev 18(6):660–672 [DOI] [PubMed] [Google Scholar]
- 71.Barriuso L, Miqueleiz E, Albaladejo R, et al. (2015) Socioeconomic position and childhood-adolescent weight status in rich countries: a systematic review, 1990-2013. BMC Pediatr 15:129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Labree LJW, van de Mheen H, Rutten FFH, et al. (2011) Differences in overweight and obesity among children from migrant and native origin: a systematic review of the European literature. Obes Rev 12(501):e535–e547 [DOI] [PubMed] [Google Scholar]
- 73.Koschollek C, Bartig S, Rommel A, et al. (2019) The health of children and adolescents with a migration background in Germany – Results of the cross-sectional KiGGS Wave 2 study. 4(3):7–28. https://edoc.rki.de/handle/176904/6109 (As at 02.04.2020) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lytle LA. (2009) Examining the etiology of childhood obesity: the IDEA study. Am J Community Psychol 44(3–4):338–349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Davison KK, Birch LL. (2001) Childhood overweight: a contextual model and recommendations for future research. Obes Rev 2(3):159–171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Plachta-Danielzik S, Müller MJ. (2018) Determinanten des Übergewichts bei Kindern und Jugendlichen. In: Dadaczynski K, Quilling E, Walter U. (Eds) Übergewichtsprävention im Kindes und Jugendalter. Hogrefe, Bern, P. 43–52 [Google Scholar]
- 77.Plachta-Danielzik S, Kehden B, Landsberg B, et al. (2012) Attributable Risks for Childhood Overweight: Evidence for Limited Effectiveness of Prevention. Pediatrics 130(4):e865–e871 [DOI] [PubMed] [Google Scholar]
- 78.Kovács E, Hunsberger M, Reisch L, et al. (2015) Adherence to combined lifestyle factors and their contribution to obesity in the IDEFICS study. Obes Rev 16(S2):138–150 [DOI] [PubMed] [Google Scholar]
- 79.Kleiser C, Schaffrath Rosario A, Mensink GBM, et al. (2009) Potential determinants of obesity among children and adolescents in Germany: results from the cross-sectional KiGGS study. BMC Public Health 9(1):46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lange D, Plachta-Danielzik S, Landsberg B, et al. (2010) Soziale Ungleichheit, Migrationshintergrund, Lebenswelten und Übergewicht bei Kindern und Jugendlichen Ergebnisse der Kieler Adipositas-Präventionsstudie (KOPS). Bundesgesundheitsbl 53(7):707–715 [DOI] [PubMed] [Google Scholar]
- 81.Walter U, Dadaczynski K, Quilling E. (2018) Herausforderungen und Überlegungen für zukünftige Orientierungen – ein Fazit zur Prävention von Übergewicht bei Kindern und Jugendlichen. In: Dadaczynski K, Quilling E, Walter U. (Eds) Übergewichtsprävention im Kindes und Jugendalter. Hogrefe, Bern, P. 375–387 [Google Scholar]
- 82.Swinburn BA, Kraak VI, Allender S, et al. (2019) The global syndemic of obesity, undernutrition, and climate change: the Lancet Commission report. The Lancet 393(10173):791–846 [DOI] [PubMed] [Google Scholar]
References Annex
- 1.Elmesmari R, Martin A, Reilly JJ, et al. (2018) Comparison of accelerometer measured levels of physical activity and sedentary time between obese and non-obese children and adolescents: a systematic review. BMC Pediatr 18(106) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jimenez-Pavon D, Kelly J, Reilly JJ. (2010) Associations between objectively measured habitual physical activity and adiposity in children and adolescents: systematic review. International Int J Pediatr Obes 5(1):3–18 [DOI] [PubMed] [Google Scholar]
- 3.Lee JE, Pope Z, Gao Z. (2018) The role of youth sports in promoting children’s physical activity and preventing pediatric obesity: a systematic review. Behav Med 44(1):62–76 [DOI] [PubMed] [Google Scholar]
- 4.Nelson TF, Stovitz SD, Thomas M, et al. (2011) Do youth sports prevent pediatric obesity? A systematic review and commentary. Curr Sports Med Rep 10(6):360–370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Biddle SJH, Bengoechea EG, Wiesner G. (2017) Sedentary behaviour and adiposity in youth: a systematic review of reviews and analysis of causality. Int J Behav Nutr Phys Act 14(43) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.De Rezende LFM, Lopes MR, Rey-Lopez JP, et al. (2014) Sedentary behavior and health outcomes: an overview of systematic reviews. PLoS ONE 9(8) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang G, Wu L, Zhou LL, et al. (2016) Television watching and risk of childhood obesity: a meta-analysis. Eur J Public Health 26(1):13–18 [DOI] [PubMed] [Google Scholar]
- 8.Bleich SN, Ku R, Wang YC. (2011) Relative contribution of energy intake and energy expenditure to childhood obesity: a review of the literature and directions for future research. Int J Obes (Lond) 35(1):1–15 [DOI] [PubMed] [Google Scholar]
- 9.Morgan RE. (2013) Does consumption of high-fructose corn syrup beverages cause obesity in children? Pediatr Obes 8(4):249–254 [DOI] [PubMed] [Google Scholar]
- 10.Morenga LT, Mallard S, Mann J. (2013) Dietary sugars and body weight: systematic review and meta-analyses of randomised controlled trials and cohort studies. BMJ 345(7891) [DOI] [PubMed] [Google Scholar]
- 11.Aller E, Abete I, Astrup A, et al. (2011) Starches, Sugars and Obesity. Nutrients 3(3):341–369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pearce J, Langley-Evans SC. (2013) The types of food introduced during complementary feeding and risk of childhood obesity: a systematic review. Int J Obes (Lond) 37(4):477–485 [DOI] [PubMed] [Google Scholar]
- 13.Naude CE, Visser ME, Nguyen KA, et al. (2018) Effects of total fat intake on bodyweight in children. Cochrane Database Syst Rev (7):CD012960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harland JI, Garton LE. (2008) Whole-grain intake as a marker of healthy body weight and adiposity. Public Health Nutr 11(6):554–563 [DOI] [PubMed] [Google Scholar]
- 15.Cheng L. (2018) The convergence of two epidemics: vitamin D deficiency in obese school-aged children. J Pediatr Nurs 38:20–26 [DOI] [PubMed] [Google Scholar]
- 16.Hosseini B, Saedisomeolia A, Allman-Farinelli M. (2017) Association between antioxidant intake/status and obesity: a systematic review of observational studies. Biol Trace Elem Res 175(2):287–297 [DOI] [PubMed] [Google Scholar]
- 17.Uusi-Rasi K, Karkkainen MUM, Lamberg-Allardt CJE. (2013) Calcium intake in health maintenance – a systematic review. Food Nutr Res 57:21082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Perez-Escamilla R, Obbagy JE, Altman JM, et al. (2012) Dietary energy density and body weight in adults and children: a systematic review. J Acad Nutr Diet 112(5):671–684 [DOI] [PubMed] [Google Scholar]
- 19.Bucher Della Torre S, Keller A, Laure Depeyre J, et al. (2016) Sugarsweetened beverages and obesity risk in children and adolescents: a systematic analysis on how methodological quality may influence conclusions. J Acad Nutr Diet 116(4):638–659 [DOI] [PubMed] [Google Scholar]
- 20.Ledoux T, Hingle M, Baranowski T. (2011) Relationship of fruit and vegetable intake with adiposity: a systematic review. Obes Rev 12(5):e143–e150 [DOI] [PubMed] [Google Scholar]
- 21.Schneider BC, Dumith SC, Orlandi SP, et al. (2017) Diet and body fat in adolescence and early adulthood: a systematic review of longitudinal studies. Cien Saude Colet 22(5):1539–1552 [DOI] [PubMed] [Google Scholar]
- 22.Rosenheck R. (2008) Fast food consumption and increased caloric intake: a systematic review of a trajectory towards weight gain and obesity risk. Obes Rev 9(6):535–547 [DOI] [PubMed] [Google Scholar]
- 23.Café ACC, De Oliveira Lopes CA, Novais RLR, et al. (2018) Intake of sugar-sweetened beverages, milk and its association with body mass index in adolescence: a systematic review. Rev Paul Pediatr 36(1):91–99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ambrosini GL. (2014) Childhood dietary patterns and later obesity: a review of the evidence. Proc Nutr Soc 73(1):137–146 [DOI] [PubMed] [Google Scholar]
- 25.Kaisari P, Yannakoulia M, Panagiotakos DB. (2013) Eating frequency and overweight and obesity in children and adolescents: a meta-analysis. Pediatrics 131(5):958–967 [DOI] [PubMed] [Google Scholar]
- 26.Szajewska H, Ruszczynski M. (2010) Systematic review demonstrating that breakfast consumption influences body weight outcomes in children and adolescents in europe. Crit Rev Food Sci Nutr 50(2):113–119 [DOI] [PubMed] [Google Scholar]
- 27.Miller MA, Kruisbrink M, Wallace J, et al. (2018) Sleep duration and incidence of obesity in infants, children, and adolescents: a systematic review and meta-analysis of prospective studies. Sleep 41(4) [DOI] [PubMed] [Google Scholar]
- 28.Wu YH, Gong QH, Zou ZQ, et al. (2017) Short sleep duration and obesity among children: a systematic review and meta-analysis of prospective studies. Obes Res Clin Pract 11(2):140–150 [DOI] [PubMed] [Google Scholar]
- 29.Li L, Zhang S, Huang YB, et al. (2017) Sleep duration and obesity in children: a systematic review and meta-analysis of prospective cohort studies. J Paediatr Child Health 53(4):378–385 [DOI] [PubMed] [Google Scholar]
- 30.Wang Y, Min J, Khuri J, et al. (2017) A systematic examination of the association between parental and child obesity across countries. Adv Nutr 8(3):436–448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cislak A, Safron M, Pratt M, et al. (2012) Family-related predictors of body weight and weight-related behaviours among children and adolescents: a systematic umbrella review. Child Care Health Dev 38(3):321–331 [DOI] [PubMed] [Google Scholar]
- 32.Valdes J, Rodriguez-Artalejo F, Aguilar L, et al. (2013) Frequency of family meals and childhood overweight: a systematic review. Pediatr Obes 8(1):e1–e13 [DOI] [PubMed] [Google Scholar]
- 33.Silden KE. (2018) Impact of competitive foods in public schools on child nutrition: effects on adolescent obesity in the United States an integrative systematic literature review. Glob Health Action 11(1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Safron M, Cislak A, Gaspar T, et al. (2011) Micro-environmental characteristics related to body weight, diet, and physical activity of children and adolescents: a systematic umbrella review. Int J Environ Health Res 21(5):317–330 [DOI] [PubMed] [Google Scholar]
- 35.Casey R, Oppert JM, Weber C, et al. (2014) Determinants of childhood obesity: What can we learn from built environment studies? Food Qual Prefer 31(1):164–172 [Google Scholar]
- 36.An R, Yang Y, Hoschke A, et al. (2017) Influence of neighbourhood safety on childhood obesity: a systematic review and meta-analysis of longitudinal studies. Obes Rev 18(11):1289–1309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Johnson JA, Johnson AM. (2015) Urban-rural differences in childhood and adolescent obesity in the United States: a systematic review and meta-analysis. Child Obes 11(3):233–241 [DOI] [PubMed] [Google Scholar]
- 38.Lovasi GS, Hutson MA, Guerra M, et al. (2009) Built environments and obesity in disadvantaged populations. Epidemiol Rev 31:7–20 [DOI] [PubMed] [Google Scholar]
- 39.Leal C, Chaix B. (2011) The influence of geographic life environments on cardiometabolic risk factors: a systematic review, a methodological assessment and a research agenda. Obes Rev 12(3):217–230 [DOI] [PubMed] [Google Scholar]
- 40.Kelly B, King L, Chapman K, et al. (2015) A Hierarchy of Unhealthy Food Promotion Effects: Identifying Methodological Approaches and Knowledge Gaps. Am J Public Health 105(4):E86–E95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vrijheid M, Casas M, Gascon M, et al. (2016) Environmental pollutants and child health – a review of recent concerns. Int J Hyg Environ Health 219(4–5):331–342 [DOI] [PubMed] [Google Scholar]
- 42.Osei-Assibey G, Dick S, Macdiarmid J, et al. (2012) The influence of the food environment on overweight and obesity in young children: a systematic review. BMJ Open 2(6) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Albuquerque D, Nobrega C, Manco L, et al. (2017) The contribution of genetics and environment to obesity. Br Med Bull 123(1):159–173 [DOI] [PubMed] [Google Scholar]
- 44.Arslan N, Erdur B, Aydin A. (2010) Hormones and cytokines in childhood obesity. Indian J Pediatr 47(10):829–839 [DOI] [PubMed] [Google Scholar]
- 45.Indiani C, Rizzardi KF, Castelo PM, et al. (2018) Childhood obesity and firmicutes/bacteroidetes ratio in the gut microbiota: a systematic review. Child Obes 14(8):501–509 [DOI] [PubMed] [Google Scholar]
- 46.Cattuzzo MT, Henrique RD, Re AHN, et al. (2016) Motor competence and health related physical fitness in youth: a systematic review. J Sci Med Sport 19(2):123–129 [DOI] [PubMed] [Google Scholar]
- 47.Mintjens S, Menting MD, Daams JG, et al. (2018) Cardiorespiratory fitness in childhood and adolescence affects future cardiovascular risk factors: a systematic review of longitudinal studies. Sports Med 48(11):2577–2605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Smith JJ, Eather N, Morgan PJ, et al. (2014) The health benefits of muscular fitness for children and adolescents: a systematic review and meta-analysis. Sports Med 44(9):1209–1223 [DOI] [PubMed] [Google Scholar]
- 49.Kaplowitz PB. (2008) Link between body fat and the timing of puberty. Pediatrics 121 Suppl 3:S208–217 [DOI] [PubMed] [Google Scholar]
- 50.Zheng Z, Zhang L, Li SP, et al. (2017) Association among obesity, overweight and autism spectrum disorder: a systematic review and meta-analysis. Sci Rep 7:11697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Shang QL, Wang HP, Song YJ, et al. (2014) Serological data analyses show that adenovirus 36 infection is associated with obesity: a meta-analysis involving 5739 subjects. Obesity 22(3):895–900 [DOI] [PubMed] [Google Scholar]
- 52.Leinaar E, Alamian A, Wang L. (2016) A systematic review of the relationship between asthma, overweight, and the effects of physical activity in youth. Ann Epidemiol 26(7):504–510 [DOI] [PubMed] [Google Scholar]
- 53.Miller SA, Wu RKS, Oremus M. (2018) The association between antibiotic use in infancy and childhood overweight or obesity: a systematic review and meta-analysis. Obes Rev 19(11):1463–1475 [DOI] [PubMed] [Google Scholar]
- 54.Shao XQ, Ding XL, Wang B, et al. (2017) Antibiotic exposure in early life increases risk of childhood obesity: a systematic review and meta-analysis. Front Endocrinol 8:170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Baidal JAW, Locks LM, Cheng ER, et al. (2016) Risk factors for childhood obesity in the first 1,000 days: a systematic review. Am J Prev Med 50(6):761–779 [DOI] [PubMed] [Google Scholar]
- 56.Yu ZB, Han SP, Zhu JG, et al. (2013) Pre-pregnancy body mass index in relation to infant birth weight and offspring overweight/obesity: a systematic review and meta-analysis. PLoS ONE 8(4) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tie HT, Xia YY, Zeng YS, et al. (2014) Risk of childhood overweight or obesity associated with excessive weight gain during pregnancy: a meta-analysis. Arch Gynecol Obstet 289(2):247–257 [DOI] [PubMed] [Google Scholar]
- 58.Philipps LH, Santhakumaran S, Gale C, et al. (2011) The diabetic pregnancy and offspring BMI in childhood: a systematic review and meta-analysis. Diabetologia 54(8):1957–1966 [DOI] [PubMed] [Google Scholar]
- 59.Qureshi R, Jadotte Y, Zha P, et al. (2018) The association between prenatal exposure to environmental tobacco smoke and childhood obesity: a systematic review. JBI Database System Rev Implement Rep 16(8):1643–1662 [DOI] [PubMed] [Google Scholar]
- 60.Rayfield S, Plugge E. (2017) Systematic review and meta-analysis of the association between maternal smoking in pregnancy and childhood overweight and obesity. J Epidemiol Community Health 71(2):162–173 [DOI] [PubMed] [Google Scholar]
- 61.Riedel C, Schonberger K, Yang SM, et al. (2014) Parental smoking and childhood obesity: higher effect estimates for maternal smoking in pregnancy compared with paternal smoking – a meta-analysis. Int J Epidemiol 43(5):1593–1606 [DOI] [PubMed] [Google Scholar]
- 62.Schellong K, Schulz S, Harder T, et al. (2012) Birth weight and long-term overweight risk: systematic review and a meta-analysis including 643,902 persons from 66 studies and 26 countries globally. PLoS ONE 7(10) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kuhle S, Tong OS, Woolcott CG. (2015) Association between caesarean section and childhood obesity: a systematic review and meta-analysis. Obes Rev 16(4):295–303 [DOI] [PubMed] [Google Scholar]
- 64.Newsome K, Rashid T, Vonville HM, et al. (2016) Mapping of reviews on breastfeeding and obesity risk in children. Curr Nutr Rep 5(4):255–277 [Google Scholar]
- 65.Yan J, Liu L, Zhu Y, et al. (2014) The association between breastfeeding and childhood obesity: a meta-analysis. BMC Public Health 14:1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wang J, Wu Y, Xiong G, et al. (2016) Introduction of complementary feeding before 4 months of age increases the risk of childhood overweight or obesity: A meta-analysis of prospective cohort studies. Nutr Res 36(8):759–770 [DOI] [PubMed] [Google Scholar]
- 67.Zheng M, Lamb KE, Grimes C, et al. (2018) Rapid weight gain during infancy and subsequent adiposity: a systematic review and meta-analysis of evidence. Obes Rev 19(3):321–332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Jeyakumar A, Fettman N, Armbrecht ES, et al. (2011) A systematic review of adenotonsillectomy as a risk factor for childhood obesity. Otolaryngol Head Neck Surg 144(2):154–158 [DOI] [PubMed] [Google Scholar]
- 69.Liang J, Matheson BE, Kaye WH, et al. (2014) Neurocognitive correlates of obesity and obesity-related behaviors in children and adolescents. Int J Obes (Lond) 38(4):494–506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Incledon E, Wake M, Hay M. (2011) Psychological predictors of adiposity: systematic review of longitudinal studies. Int J Pediatr Obes 6(2–2):e1–e11 [DOI] [PubMed] [Google Scholar]
- 71.Halliday JA, Palma CL, Mellor D, et al. (2014) The relationship between family functioning and child and adolescent overweight and obesity: a systematic review. Int J Obes (Lond) 8(4):480–493 [DOI] [PubMed] [Google Scholar]
- 72.Blewitt C, Bergmeier H, Macdonald JA, et al. (2016) Associations between parent-child relationship quality and obesogenic risk in adolescence: a systematic review of recent literature. Obes Rev 17(7):612–622 [DOI] [PubMed] [Google Scholar]
- 73.Slopen N, Goodman E, Koenen KC, et al. (2013) Socioeconomic and other social stressors and biomarkers of cardiometabolic risk in youth: a systematic review of less studied risk factors. PLoS ONE 8(5) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Conklin AI, Guo SX, Tam AC, et al. (2018) Gender, stressful life events and interactions with sleep: a systematic review of determinants of adiposity in young people. BMJ Open 8(7):e019982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Danese A, Tan M. (2014) Childhood maltreatment and obesity: systematic review and meta-analysis. Mol Psychiatry 19(5):544–554 [DOI] [PubMed] [Google Scholar]
- 76.Midei AJ, Matthews KA. (2011) Interpersonal violence in childhood as a risk factor for obesity: a systematic review of the literature and proposed pathways. Obes Rev 12(501):e159–e172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Russell-Mayhew S, McVey G, Bardick A, et al. (2012) Mental health, wellness, and childhood overweight/obesity. J Obes 2012:281801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Cortese S, Moreira-Maia CR, St Fleur D, et al. (2016) Association between ADHD and obesity: a systematic review and meta-analysis. Am J Psychiatry 173(1):34–43 [DOI] [PubMed] [Google Scholar]
- 79.Mannan M, Mamun A, Doi S, et al. (2016) Prospective associations between depression and obesity for adolescent males and females – a systematic review and meta-analysis of longitudinal studies. PLoS ONE 11(6) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Badaly D. (2013) Peer similarity and influence for weight-related outcomes in adolescence: a meta-analytic review. Clin Psychol Rev 33(8):1218–1236 [DOI] [PubMed] [Google Scholar]
- 81.Cunningham SA, Vaquera E, Maturo CC, et al. (2012) Is there evidence that friends influence body weight? A systematic review of empirical research. Soc Sci Med 75(7):1175–1183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.O’Connor SG, Maher JP, Belcher BR, et al. (2017) Associations of maternal stress with children’s weight-related behaviours: a systematic literature review. Obes Rev 18(5):514–525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lampard AM, Franckle RL, Davison KK. (2014) Maternal depression and childhood obesity: a systematic review. Prev Med 59:60–67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Tompkins CL, Seablom M, Brock DW. (2015) Parental perception of child’s body weight: a systematic review. J Child Fam Stud 24(5):1384–1391 [Google Scholar]
- 85.Rietmeijer-Mentink M, Paulis WD, van Middelkoop M, et al. (2013) Difference between parental perception and actual weight status of children: a systematic review. Matern Child Nutr 9(1):3–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Marks R. (2015) Childhood obesity and parental health literacy. AOWMC 3(3):00055 [Google Scholar]
- 87.Shloim N, Edelson LR, Martin N, et al. (2015) Parenting styles, feeding styles, feeding practices, and weight status in 4–12 year-old children: a systematic review of the literature. Front Psychol 6:1849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Sokol RL, Qin B, Poti JM. (2017) Parenting styles and body mass index: a systematic review of prospective studies among children. Obes Rev 18(3):281–292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wu SQ, Ding YY, Wu FQ, et al. (2015) Socio-economic position as an intervention against overweight and obesity in children: a systematic review and meta-analysis. Sci Rep 5:11354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Barriuso L, Miqueleiz E, Albaladejo R, et al. (2015) Socioeconomic position and childhood-adolescent weight status in rich countries: a systematic review, 1990–2013. BMC Pediatr 15:129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kim TJ, Roesler NM, von dem Knesebeck O. (2017) Causation or selection – examining the relation between education and overweight/obesity in prospective observational studies: a meta-analysis. Obes Rev 18(6):660–672 [DOI] [PubMed] [Google Scholar]
- 92.Kim TJ, von dem Knesebeck O. (2018) Income and obesity: what is the direction of the relationship? A systematic review and meta-analysis. BMJ Open 8:e019862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Labree LJW, van de Mheen H, Rutten FFH, et al. (2011) Differences in overweight and obesity among children from migrant and native origin: a systematic review of the European literature. Obes Rev 12(501):e535–e547 [DOI] [PubMed] [Google Scholar]
- 94.Park SH, Cormier E. (2018) Influence of siblings on child health behaviors and obesity: a systematic review. J Child Fam Stud 27(7):2069–2081 [Google Scholar]


