Abstract
Purpose
To develop and evaluate MyoMapNet, a rapid myocardial T1 mapping approach that uses fully connected neural networks (FCNN) to estimate T1 values from four T1-weighted images collected after a single inversion pulse in four heartbeats (Look-Locker, LL4).
Method
We implemented an FCNN for MyoMapNet to estimate T1 values from a reduced number of T1-weighted images and corresponding inversion-recovery times. We studied MyoMapNet performance when trained using native, post-contrast T1, or a combination of both. We also explored the effects of number of T1-weighted images (four and five) for native T1. After rigorous training using in-vivo modified Look-Locker inversion recovery (MOLLI) T1 mapping data of 607 patients, MyoMapNet performance was evaluated using MOLLI T1 data from 61 patients by discarding the additional T1-weighted images. Subsequently, we implemented a prototype MyoMapNet and LL4 on a 3 T scanner. LL4 was used to collect T1 mapping data in 27 subjects with inline T1 map reconstruction by MyoMapNet. The resulting T1 values were compared to MOLLI.
Results
MyoMapNet trained using a combination of native and post-contrast T1-weighted images had excellent native and post-contrast T1 accuracy compared to MOLLI. The FCNN model using four T1-weighted images yields similar performance compared to five T1-weighted images, suggesting that four T1 weighted images may be sufficient. The inline implementation of LL4 and MyoMapNet enables successful acquisition and reconstruction of T1 maps on the scanner. Native and post-contrast myocardium T1 by MOLLI and MyoMapNet was 1170 ± 55 ms vs. 1183 ± 57 ms (P = 0.03), and 645 ± 26 ms vs. 630 ± 30 ms (P = 0.60), and native and post-contrast blood T1 was 1820 ± 29 ms vs. 1854 ± 34 ms (P = 0.14), and 508 ± 9 ms vs. 514 ± 15 ms (P = 0.02), respectively.
Conclusion
A FCNN, trained using MOLLI data, can estimate T1 values from only four T1-weighted images. MyoMapNet enables myocardial T1 mapping in four heartbeats with similar accuracy as MOLLI with inline map reconstruction.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12968-021-00834-0.
Keywords: Inversion-recovery cardiac T1 mapping, Machine learning, Myocardial tissue characterization, Cardiovascular magnetic resonance
Introduction
Cardiovascular magnetic resonance (CMR) myocardial T1 and extracellular volume (ECV) mapping enable non-invasive quantification of diffuse interstitial fibrosis [1]. Generally, myocardial T1 mapping consists of a preparation pulse and collection of a series of images to sample the recovering longitudinal magnetization at different time points. Based on the evolution of the longitudinal magnetization across the acquired T1-weighted images, T1 at each pixel could be determined [2–4]. Over the past decade, there have been significant advances in myocardial T1 mapping sequence with different choices of magnetization preparation (e.g., inversion [5, 6], saturation [3, 7], or a combination of both [8]), number of collected T1-weighted images, and recovery period between different imaging blocks [6, 9]. Trade-offs depend on accuracy and precision [2, 10]. There are also differences in terms of coverage (e.g., single 2D, interleaved multislice 2D, or 3D) and respiratory motion compensation (free breathing vs. breath-holding) [11–15]. There is also growing interest in using a single sequence to simultaneously measure different tissue relaxation times [16–22]. These approaches often require a more complicated fitting model with more parameters, resulting in a loss of precision and significantly longer reconstruction time, which reduce their clinical utility.
Among different myocardial T1 mapping sequences, Modified Look-Locker inversion recovery (MOLLI) is the most widely used due to its high precision and broad vendor availability [5]. Within a single breath-hold scan, MOLLI performs three sets of Look-Locker inversion-recovery experiments to collect 3, 3, and 5 electrocardiogram (ECG)-triggered T1-weighted images, respectively, with 3 resting heartbeats between every two Look-Locker experiments for magnetization recovery. This acquisition scheme is referred to as MOLLI3(3)3(3)5. A 3-parameter inversion-recovery model with Look-Locker correction is used to calculate T1. However, MOLLI3(3)3(3)5 suffers from inaccurate T1 estimates and long 17 heartbeat breath-holding time. Subsequently, several derivations of MOLLI have been proposed to improve accuracy, precision, or shorten imaging time. For example, MOLLI5(3)3 and MOLLI4(1)3(1)2 protocols both reduce single breathholding to 11 heart beats(9), and the latter improves precision for short T1 times. Shortened MOLLI (ShMOLLI) uses a 5(1)1(1)1 scheme to further reduce imaging time and alleviate effects of heart rate variation by using a conditional fitting algorithm [6]. Inversion group fitting has also been proposed, consisting of a shorter waiting period between Look-Locker experiments, albeit with lower precision [23, 24].
Alternatives to standard curve-fitting techniques in parametric mapping include dictionary-based reconstruction [16, 25, 26], simulated signal recovery [27], and machine learning [28, 29]. Shao et al. used Bloch equation simulation with slice profile correction to model the signal evolution for MOLLI T1 accuracy [27]. They extended this algorithm using deep learning (DL) for rapid T1 map reconstruction [30]. Similarly, Zhang et al. and Hamilton et al. used DL to rapidly reconstruct T1 and T2 maps from images collected using MR fingerprinting [29, 31]. To reduce motion artifacts, an interleaved T1 mapping sequence with radial sampling used a convolutional neural network model to reconstruct highly accelerated T1-weighted image to minimize the acquisition window of the single-shot image [32]. DL was also recently used for joint saturation- and inversion-recovery T1 mapping to improve precision [33]. These studies indicated that DL has the potential to improve myocardial tissue characterization by increasing precision, reducing reconstruction time, decreasing motion sensitivity, and addressing imaging confounders of the myocardial T1 mapping sequence. However, none reduce the overall scan time for myocardial T1 mapping.
In this study, we sought to develop and evaluate a rapid myocardial T1 mapping technique, referred to as MyoMapNet, to perform myocardial T1 mapping in 4 heartbeats with similar accuracy and precision as conventional MOLLI. A single Look-Locker experiment is performed to collect four T1-weighted images (LL4), which are subsequently used in a fully connected neural network (FCNN) to rapidly build T1 map. We hypothesize that a DL-based method can learn T1 from a limited number of T1-weighted samples along the inversion-recovery curve. After initial development and evaluation, we implemented a MyoMapNet prototype on the scanner for seamless integration into the T1 mapping acquisition and reconstruction clinical workflow.
Methods
MyoMapNet
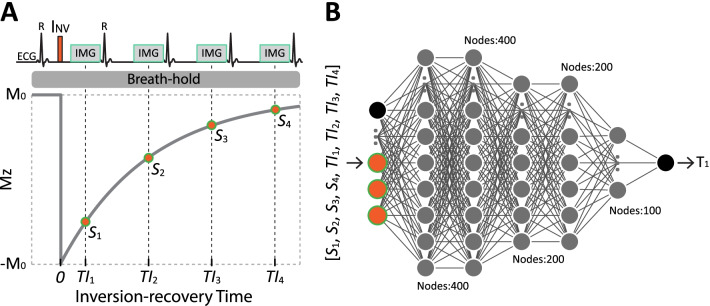
LL4 performs an inversion pulse followed by four ECG-triggered single-shot balanced steady-state free precession (bSSFP) images acquired on successive cardiac cycles within a single breath-hold (Fig. 1A). The inversion-recovery time, defined as the period between the inversion pulse and the acquisition of the central k-space line, is TI1 for the first image and TI1 + (n-1)*RR for the image acquired in the nth cardiac cycle. Subsequently, an FCNN is used to estimate T1 from four T1-weighted signals with corresponding TIs at each pixel (Fig. 1B). A detailed description of the FCNN architecture and optimization are presented in the training section.
Fig. 1.
Image acquisition and map estimation in MyoMapNet. A The proposed breath-hold T1 mapping sequence (referred to as Look-Locker 4 (LL4)) consists of an inversion pulse (INV) followed by four single-shot Electrocardiogram (ECG)-triggered images. B A fully connected neural network (FCNN) is then used to determine T1 at each pixel with T1-weighted signals (i.e., Si) and inversion times (i.e., TIi)
We first sought to investigate the performance of MyoMapNet trained with three different datasets: (1) using only the first 4 images from native T1 mapping data by MOLLI5(3)3 (MyoMapNet4, PreGd); (2) using only the first 4 images from post-contrast T1 mapping data by MOLLI4(1)3(1)2 (MyoMapNet4, PostGd); and (3) using the first 4 images of both native and post-contrast T1 mapping data according to their respective MOLLI protocols (MyoMapNet4, Pre+PostGd).
Considering the potential loss of T1 precision using only four T1-weighted images, we also investigated the model's performance using five T1-weighted images. Given that existing MOLLI data were used for training, only MOLLI5(3)3 acquired prior to contrast injection was available. We therefore only evaluated MyoMapNet with five native T1-weighted signals. We refer to this model as MyoMapNet5, PreGd. Additional file 1: Table S1 summarizes inputs and nature of data used for training of each model. We subsequently used these four models to estimate phantom and in-vivo T1 with and without contrast to determine whether two separate FC networks for native and post-contrast T1 estimation were needed or if a single model for a single sequence could be used to simplify imaging and map estimation.
Existing data for training, validation, and testing
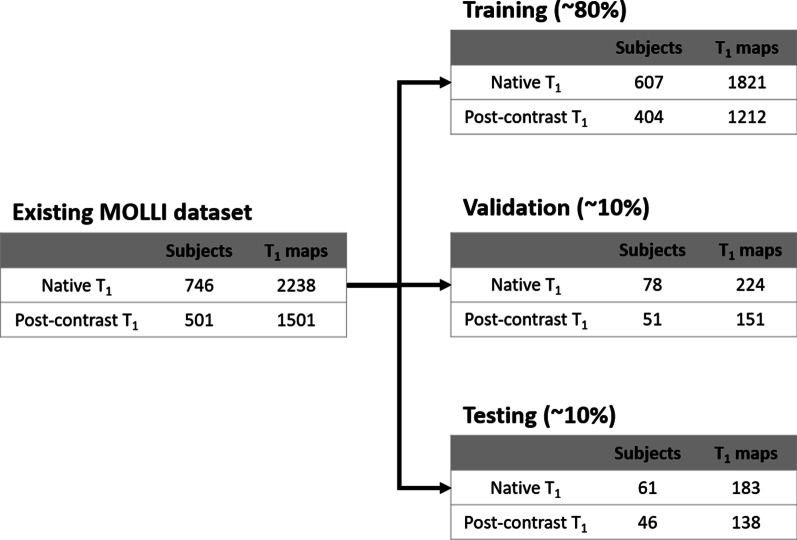
T1 mapping data from 749 patients (407 male; 16–96 yrs) undergoing MOLLI scans between Jan 1, 2019, and Oct 15, 2020, were retrospectively collected (Fig. 2). Patients were referred for a clinical CMR exam for various cardiovascular indications. Our local institutional review board approved use of in-vivo data for research with a consent waiver. Patient information was handled in compliance with the Health Insurance Portability and Accountability Act (HIPAA).
Fig. 2.
Summary of existing MOLLI T1 mapping data used for training, validation, and testing, collected in patients undergoing a clinical CMR exam. Native and post-contrast T1 mapping were performed using MOLLI5(3)3 and MOLLI4(1)3(1)2, respectively
Every patient had either native or both native and post-contrast T1-weighted images acquired by MOLLI5(3)3 and MOLLI4(1)3(1)2 for three left-ventricle (LV) short-axis view slices. All images were collected on a 3 T CMR scanner (MAGNETOM Vida, Siemens Healthineers, Erlangen, Germany) using body and spine phased-array coils. Imaging parameters used in both sequences are summarized in Additional file 1: Table S2. Post-contrast T1 mapping was scanned 15–20 min after injection of 0.1 mmol/kg Gd-DTPA (Gadavist, Bayer Healthcare, Berlin, Germany). The motion-correction algorithm of the vendor was used to align the myocardium across T1-weighted images for each scan. T1 maps for both sequences were calculated offline using a 3-parameter inversion-recovery model with Look-Locker correction. We randomly divided this dataset into training (~ 80%), validation (~ 10%), and testing (~ 10%) (Fig. 2).
MyoMapNet training
MyoMapNet was implemented in Python using the PyTorch library (1.4.0). Training, validation, and testing were performed on a DGX-1 workstation (NVIDIA Santa Clara, California, USA) equipped with 88 Intel Xeon central processing units (2.20 GHz), one NVIDIA Tesla V100 graphics processing unit (GPU) with 32 GB memory and 5120 Tensor cores, and 504 GB RAM.
In the training step, we first sought to investigate the choice of hyperparameters and training performance to obtain the best model. We investigated various hyperparameters, including the number of hidden layers from 2 to 6; the number of neurons in each hidden layer (50, 100, 200, 400); activation functions such as rectified linear activation (Relu) and Leaky Relu; different sizes of mini-batches (32, 40, 64, 80); different optimizers(Adam and stochastic gradient descent (SGD)); and different learning rates (0.001, 0.01).
The model parameters consisted of all weights and biases that were learned during training by minimizing the mean absolute error (MAE):
| 1 |
To avoid overfitting or underfitting, T1 estimation errors of the training and validation datasets were monitored during training. For the training dataset, T1 estimation error over the entire image and expected T1 ranges (i.e., myocardium and blood) were calculated. In addition to reporting global T1 estimation error over the image in the validation dataset, we also monitored and reported errors for the myocardium and blood.
The trained network and instructions on how to use the network are publicly available (https://github.com/HMS-CardiacMR/MyoMapNet).
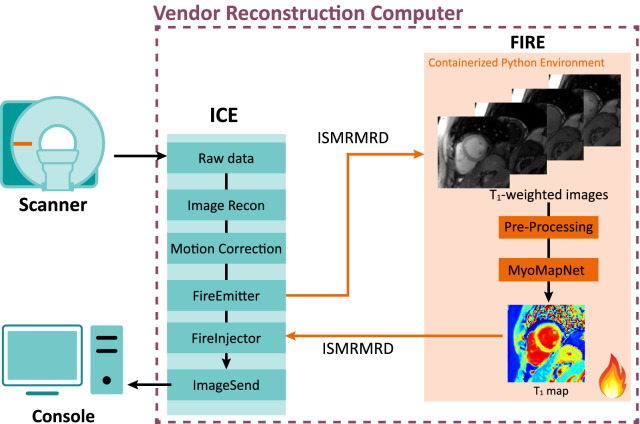
Inline integration
The trained MyoMapNet prototype was deployed on a 3 T CMR scanner (MAGNETOM Vida, Siemens Healthineers, Erlangen, Germany) for inline T1 map building (Fig. 3). The inline integration was implemented using the Siemens Framework for Image Reconstruction (FIRE) prototype framework. Briefly, the FIRE framework provides an interface for raw data or image between the Siemens Image Reconstruction Environment (ICE) pipeline and an external environment similar to Python. The pre-trained MyoMapNet4, Pre+PostGd model was deployed in a containerized (chroot) Python 3.6 environment compatible with the FIRE framework. Data acquired on the scanner underwent standard image reconstruction and motion correction in the Siemens ICE pipeline. Motion-corrected T1-weighted images were then converted into International Society of Magnetic Resonance in Medicine Raw Data format (ISMRMRD) [34]. Before feeding into MyoMapNet, the T1-weighted signals were normalized to 0–1.1. T1 map was then reconstructed by MyoMapNet and sent back to the ICE pipeline in ISMRMRD format, where distortion correction and DICOM images were generated and displayed on the CMR console.
Fig. 3.
Schematic of the implemented inline integration of MyoMapNet using the Siemens Framework for Image Reconstruction (FIRE) prototype. The pre-trained MyoMapNet model was deployed in a containerized (chroot) Python 3.6 environment compatible with the FIRE framework. Data acquired on the scanner underwent standard image reconstruction and motion correction in the Siemens ICE pipeline, and T1-weighted images were converted into ISMRM Raw Data format (ISMRMRD) and sent to the MyoMapNet model. In the pre-processing step, the T1-weighted signals were normalized to the range of 0–1.1. After prediction, T1 map was sent back to the ICE pipeline in the ISMRMRD format where distortion correction and DICOM images were generated and displayed on the CMR console
MyoMapNet performance
Phantom evaluation
A T1MES prototype phantom containing 12 vials with different T1 and T2 values for cardiac T1 mapping at 3 T was used [35]. Reference T1 and T2 of phantom vials were measured by inversion-recovery spin-echo (IR-SE) and Carr-Purcell-Meiboom-Gill spin-echo (CPMG-SE), respectively. MOLLI5(3)3, MOLLI4(1)3(1)2, and LL4 were performed at a simulated heart rate of 60 bpm. Each sequence was repeated ten times, and repetitions of all sequences were performed in random order. Imaging parameters for all sequences are described in Additional file 1: Table S2. T1 maps for two MOLLI sequences were fitted offline using a three-parameter inversion-recovery signal model with Look-Locker correction.
In-vivo evaluation using existing MOLLI data
We evaluated four trained MyoMapNet models (Additional file 1: Table S1) using existing MOLLI data. Similar to the training steps, we extracted the first four or five T1-weighted images of MOLLI5(3)3 or MOLLI4(1)3(1)2 and their TIs, which were then fed into MyoMapNet to predict T1 values. For this evaluation, we included data from 61 patients, of which 40 had both native and post-contrast T1 images, and 21 had only native T1 data. Since these datasets were not used in either training or validation, they were new to the model.
In-vivo evaluation using prospectively collected LL4
To further evaluate MyoMapNet performance for accelerated T1 mapping LL4, we prospectively recruited 28 subjects consisting of 20 patients (12 male; 61 ± 12 yrs) referred for a clinical CMR and 8 healthy subjects (5 male; 27 ± 14 yrs). These in-vivo experiments were HIPAA compliant and approved by our Institutional Review Board. Written informed consent was obtained from each subject prior to imaging. Native T1 data was collected in 25 subjects and post-contrast T1 data in 16 subjects. Due to IRB restrictions, gadolinium was not administered to any healthy subjects, and four patients did not receive contrast as part of their clinical protocol. In addition to clinical T1 mapping by MOLLI, we collected T1-weighted images for a single mid-LV slice using LL4 within a single breath-hold. All imaging parameters, RF shape, gradient waveforms, and timing of LL4 were identical to conventional MOLLI, with the only difference being the number of T1-weighted images. Imaging parameters are described in Additional file 1: Table S2. A T1 map using our prototype inline MyoMapNet4, Pre+PostGd was reconstructed on the scanner. To further evaluate model performance, we exported images and then used each model to predict T1.
Statistical analysis
For phantom T1, a circular region of interest (ROI) composed of ~ 120 pixels was drawn on each vial. The mean, standard deviation (SD), and coefficient of variation (CV) of T1 pixels within each ROI were calculated. For each sequence, mean, SD, and CV for each vial were averaged across all ten repetitions.
For each in-vivo T1 map, contours for the endo- and epicardium boundaries and blood pool were manually drawn to measure the entire LV myocardium and blood T1. T1 was reported as mean ± SD. CV was then calculated to compare the intrasubject variation. ECV was calculated for the subject who had both native and post-contrast T1 with their blood hematocrit sampled prior to CMR imaging. For MyoMapNet5, PreGd (if any) and MyoMapNet4, PreGd, ECV was calculated with post-contrast T1 from MyoMapNet4, PostGd.
Bland–Altman analysis was performed to determine agreement in T1 or ECV values between the two methods (i.e., MOLLI and MyoMapNet). Paired Student’s t-test was also used for pair-wise comparisons. A P-value less than 0.05 was considered statistically significant. Statistical analyses were performed using GraphPad Prism (version 9.2.0, GraphPad Software, San Diego, California, USA).
Results
MyoMapNet training
Table 1 lists the MAE for various hyperparameters. Based on these preliminary optimization results, we chose the model with six layers. The number of neurons for each layer is 400, 400, 100, 100, 50, and 50. The activation function is Leaky Relu with a mini-batch of 64. The Adam optimizer was used with a learning rate of 0.01 and a weight decay of 0.0001.
Table 1.
Results of hyperparameter optimization
| Layers | Number of neurons in each layer | Activation function | Batch size | Learning rate | Mean Error of estimated T1 (ms) | ||
|---|---|---|---|---|---|---|---|
| All pixels | Myocardium | Blood | |||||
| 3 | 400, 400, 1 | Leaky Relu | 64 | 0.01 | 145.5 | -26.7 | 17.9 |
| 4 | 400, 200, 100, 1 | Leaky Relu | 32 | 0.01 | 145.8 | -22.6 | 9.1 |
| 5 | 400, 400, 200, 100, 1 | Relu | 64 | 0.01 | 176.5 | 26.2 | 192.8 |
| 6 | 400, 400, 200, 200, 100, 1 | Leaky Relu | 64 | 0.01 | 111.8 | -9.4 | -7.9 |
| 7 | 400, 400, 400, 400, 200, 100, 1 | Relu | 64 | 0.001 | 137.6 | 18.1 | 60.2 |
Adam optimizer yields the best result in all experiments. The selected hyperparameters for MyoMapNet are highlighted as bold
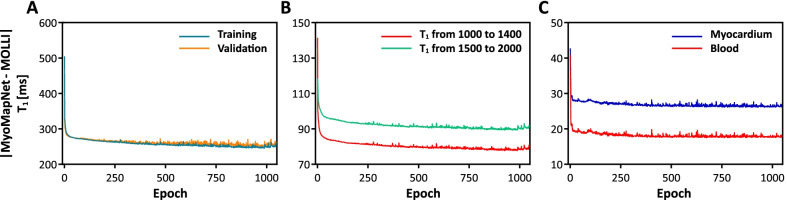
Loss curves for MyoMapNet4, Pre+PostGd, calculated over the entire image, show the stability of the model (Fig. 4A). The training and validation losses decrease to the point of stability with small differences between validation and training. For the training dataset, the loss curves for T1 ranged from 1000 to 1400 ms and from 1500 to 2000 ms demonstrates similar performance as the loss calculated over the entire image (Fig. 4B). A similar observation was made when calculating the losses in the validation dataset (Fig. 4C). For the validation dataset, MAE for myocardium and blood were ~ 27 ms and ~ 10 mm, respectively.
Fig. 4.
Loss curves for MyoMapNet4, Pre+PostGd calculated across the entire image for both training and validation (A), for specific ranges of T1 using training dataset (B), and for the myocardium and blood pool of the validation dataset (C). Losses for both training and validation decrease with each epoch until a point of stability at ~ 1000 epochs, when learning is stopped by an early stopping, as 70 epochs were passed without improvement
Phantom evaluation
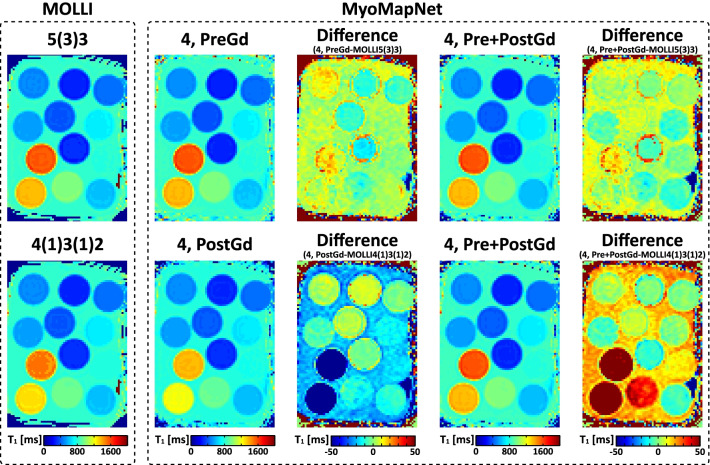
There was no significant visual difference between phantom T1 maps scanned by MOLLI and LL4 with three MyoMapNet models (Fig. 5). Bland–Altman analysis (Fig. 6) shows excellent agreement between MyoMapNet and MOLLI with negligible bias in T1 estimate (mean bias of less than 1 ms). There was no difference in SD or CV between MOLLI and MyoMapNet, indicating the similar precision among different methods (Additional file 1: Table S3).
Fig. 5.
Phantom T1 maps from two MOLLI sequences (MOLLI5(3)3 and MOLLI4(1)3(1)2) and LL4 with different MyoMapNet models. T1 difference maps between them were included. All MyoMapNet models show similar map quality, except for the model trained using only post-contrast T1 mapping data. In the T1 analysis for the post-contrast models, vials with larger T1 values (> 900 ms) were excluded. While the model trained using only in-vivo data, phantom data show that the model can reliably estimate T1 values for vials with T1/T2s that are not necessarily well represented in the training dataset
Fig. 6.
Bland–Altman plots for examining the phantom T1 agreement between MyoMapNet and MOLLI. The red line indicates the mean difference, and the dotted lines show the 95% confidence interval on the limits of agreement. For post-contrast T1 evaluation (MyoMapNet4, PostGd and MOLLI4(1)3(1)2), phantom vials with T1 larger than 900 ms were excluded
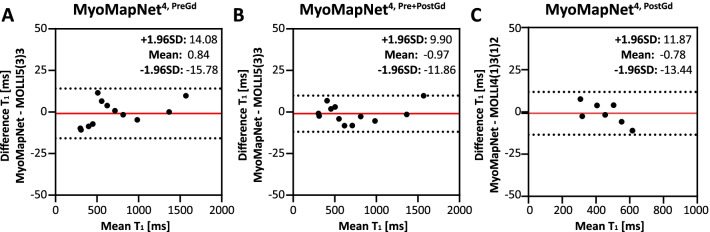
In-vivo evaluation using existing data
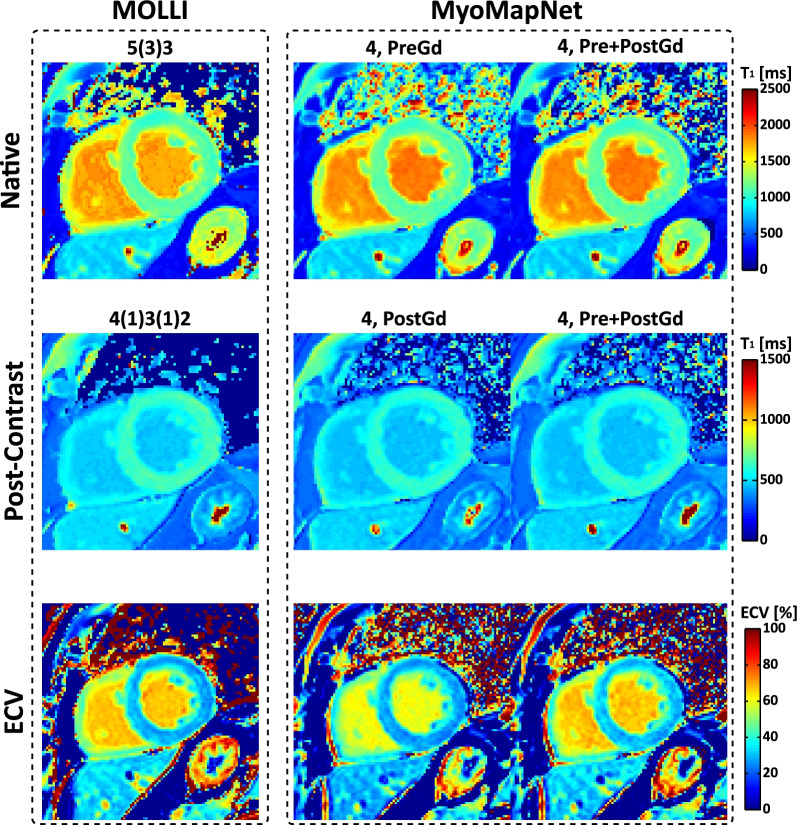
T1 maps for all subjects across all methods are available on our laboratory Harvard Dataverse. Visually, both maps from MOLLI and MyoMapNet have good image quality with homogeneous signal across the whole LV myocardium and clear boundaries (Fig. 7). Mean, SD, and CV values of native/post-contrast T1 and corresponding ECV values (if any) averaged across all subjects across all methods are summarized in Table 2 and Additional file 1: Table S4. For both native myocardium and blood T1, excellent agreement was achieved between MyoMapNet and MOLLI5(3)3 with a mean T1 difference of 2 ms and -3 ms (MyoMapNet 4, PreGd vs. MOLLI5(3)3), 2 ms and -2 ms (MyoMapNet 4, Pre+PostGd vs. MOLLI5(3)3), and 1 ms and 0 ms (MyoMapNet 5, PreGd vs. MOLLI5(3)3). The 95% confidence interval (CI) for T1 differences between MyoMapNet and MOLLI5(3)3 ranged from -10 ms to 14 ms for myocardium and ranged from -51 ms to 46 ms for blood. Bland–Altman analysis also showed excellent agreement between MyoMapNet and MOLLI4(1)3(1)2 for post-contrast T1 estimation (Fig. 8). The mean myocardium and blood T1 difference between them was -2 ms and 2 ms (MyoMapNet 4, PostGd vs. MOLLI4(1)3(1)2), and -3 ms and 1 ms (MyoMapNet 4, Pre+PostGd vs. MOLLI4(1)3(1)2), respectively. The corresponding 95% CI for T1 difference ranged from -15 ms to 9 ms for myocardium and from -11 ms to 12 ms for blood. The mean difference in ECV between MyoMapNet and MOLLI was ~ 0.4% with 95% CI from -1.1% to 1.9% (all P < 0.05) (Fig. 8).
Fig. 7.
Representative native, post-contrast T1, and ECV maps by MOLLI and MyoMapNet from a subject in the existing MOLLI dataset. For MyoMapNet images, T1-weighted images from MOLLI were extracted; therefore, both MOLLI and MyoMapNet were reconstructed from the same scan. For MyoMapNet 4, PreGd and MyoMapNet 5, PreGd, the ECV map was reconstructed with post-contrast T1 map from MyoMapNet 4, PostGd
Table 2.
Native, post-contrast T1 and corresponding ECV for the esixting data by MyoMapNet and MOLLI. MyoMapNet T1 were calculated by discarding T1-weighted images from the MOLLI sequence
| Myocardium | Blood | |
|---|---|---|
| Native T1 (ms) | ||
| MyoMapNet4, Pre | 1190 ± 38§ | 1847 ± 99 |
| MyoMapNet4, Pre+PostGd | 1190 ± 39§ | 1849 ± 100 |
| MyoMapNet5, Pre | 1190 ± 38 | 1850 ± 104 |
| MOLLI5(3)3 | 1188 ± 40 | 1850 ± 100 |
| Post-Contrast T1 (ms) | ||
| MyoMapNet4, PostGd | 573 ± 54§ | 432 ± 69§ |
| MyoMapNet4, Pre+PostGd | 572 ± 56§ | 430 ± 68 |
| MOLLI4(1)3(1)2 | 575 ± 54 | 429 ± 70 |
| ECV (%) | ||
| MyoMapNet4, Pre | 28.5 ± 2.7§ | |
| MyoMapNet4, Pre+PostGd | 28.5 ± 2.8§ | |
| MyoMapNet5, Pre | 28.5 ± 2.7§ | |
| MOLLI | 28.1 ± 2.9 | |
ECV Extracellular volume. Mean and standard deviation were calculated by averaging the corresponding results of each subject across all subjects
§p-value < 0.05 when compared to MOLLI5(3)3 or MOLLI4(1)3(1)2
Fig. 8.
Bland–Altman plots showing individual patient comparisons between MyoMapNet and two MOLLI sequences for myocardium and blood T1 in the existing MOLLI data. Mean difference and 95% limits of agreement are indicated as red and dotted lines, respectively. Each data point was averaged across three left ventricular slices of one patient. Native and post-contrast T1 used for calculating ECV are indicated for each method
In terms of precision (Additional file 1: Table S4), SD of the myocardium and blood T1 from MyoMapNet were ~ 2 ms and ~ 4 ms slightly higher than those from MOLLI5(3)3, and ~ 5 ms and ~ 7 ms higher than those from MOLLI4(1)3(1)2 (all P < 0.05), respectively. The native myocardium and blood T1 CV were 5.0% and 2.0% by MOLLI or all three MyoMapNet models (all P < 0.05). For post-contrast myocardium and blood T1, CV was 5.2% and 2.2% from MOLLI4(1)3(1)2, and ~ 6.0% and 3.7% from MyoMapNet models (all P < 0.05), respectively.
We found that MyoMapNet5, PreGd with 5 T1-weighted images did not significantly improve T1 precision compared to MyoMapNet4, PreGd or MyoMapNet4, Pre+PostGd with only 4 T1-weighted images for native T1 or both native and post-contrast T1. The latter two could again save ~ 1 s imaging time. Therefore, MyoMapNet5, PreGd was no longer used in any prospective evaluations.
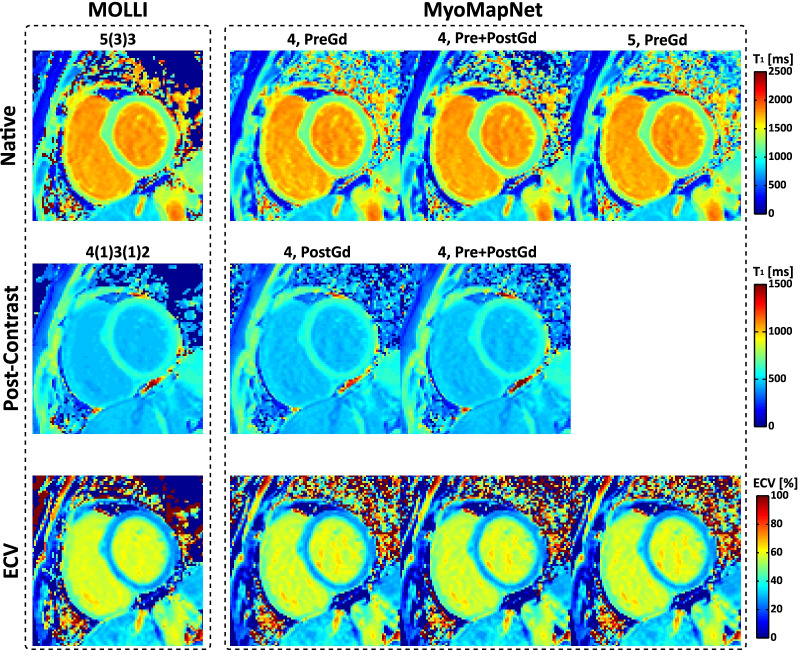
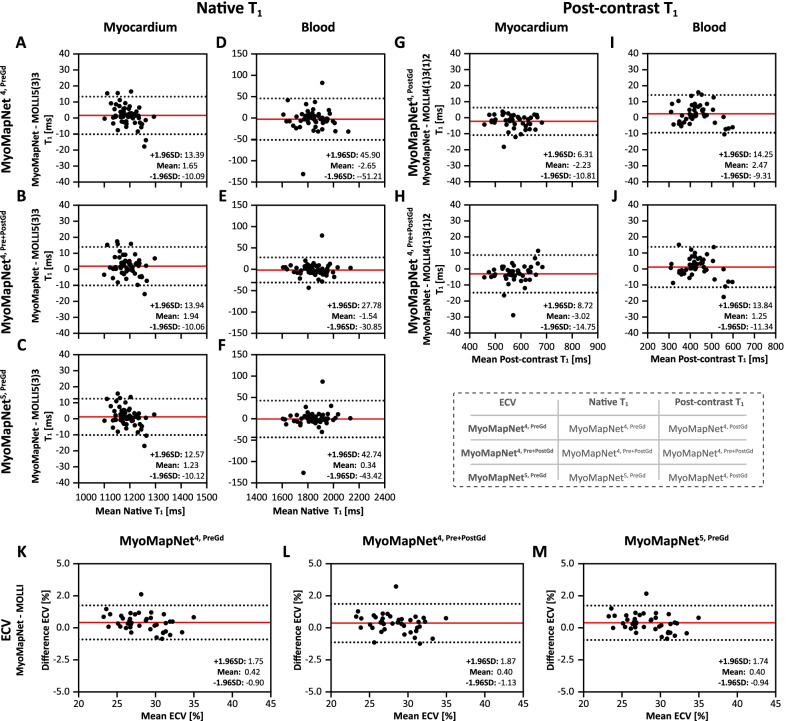
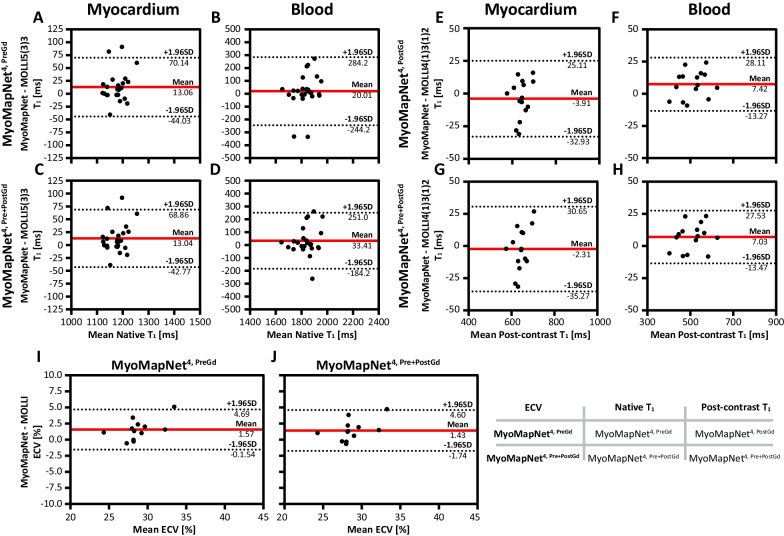
In-vivo evaluation using LL4 data
In-vivo scanning by LL4 was successfully completed in all subjects. In maps from all MyoMapNet models and two MOLLI sequences, myocardium and blood had homogeneous signals (Fig. 9). Mean T1 differences in native myocardium and blood between MyoMapNet and MOLLI was 13 ms and 20 ms (MyoMapNet4, PreGd vs. MOLLI5(3)3), and 13 ms and 33 ms (MyoMapNet4, Pre+PostGd vs. MOLLI5(3)3) (Fig. 10A–D). Mean post-contrast myocardium and blood T1 difference was -4 ms and 7 ms between MyoMapNet4, PostGd and MOLLI4(1)3(1)2, and -2 ms and 7 ms between MyoMapNet4, Pre+PostGd and MOLLI4(1)3(1)2, respectively (Fig. 10E–H). ECV for MOLLI and MyoMapNet were ~ 28% and ~ 30% (All P < 0.05, Fig. 10I–J and Table 3).
Fig. 9.
Native, post-contrast T1, and ECV maps by LL4 with MyoMapNet and MOLLI. In this case, maps are calculated from two different scans, one from conventional MOLLI and one from LL4
Fig. 10.
Bland–Altman plots comparing myocardium and blood T1 and extracellular volume fraction (ECV) values between LL4 with MyoMapNet and MOLLI, acquired in two separate scans. Mean difference and 95% limits of agreement are indicated as red and dotted lines, respectively. Each data point represents one patient. Native and post-contrast T1 used for ECV measurement are indicated for each method
Table 3.
Native and post-contrast T1 values for prospectively collected data by LL4 with MyoMapNet and MOLLI
| Myocardium | Blood | |
|---|---|---|
| Native T1 (ms) | ||
| MyoMapNet4, Pre | 1183 ± 56§ | 1840 ± 34 |
| MyoMapNet4, Pre+PostGd | 1183 ± 57§ | 1854 ± 34 |
| MOLLI5(3)3 | 1170 ± 55 | 1820 ± 29 |
| Post-Contrast T1 (ms) | ||
| MyoMapNet4, PostGd | 641 ± 29 | 515 ± 15§ |
| MyoMapNet4, Pre+PostGd | 630 ± 30 | 514 ± 15§ |
| MOLLI4(1)3(1)2 | 645 ± 26 | 508 ± 9 |
§p-value < 0.05 when compared to MOLLI5(3)3 or MOLLI4(1)3(1)2
SD for native myocardium T1 did not differ between MOLLI5(3)3 and MyoMapNet4, PreGd (P = 0.95) or MyoMapNet4, Pre+PostGd (P = 0.59) (Additional file 1: Table S5). SD of the native blood T1 from MyoMapNet was higher than that from MOLLI5(3)3 (34 ms vs. 29 ms, all P < 0.05). For post-contrast T1, SD of myocardium T1 was 26 ms from MOLLI4(1)3(1)2 and ~ 30 ms from MyoMapNet (MOLLI4(1)3(1)2 vs. MyoMapNet4, PostGd: P = 0.24; MOLLI4(1)3(1)2 vs. MyoMapNet4, Pre+PostGd: P = 0.04). Similar to the native T1 measurement, the SD for blood T1 from MyoMapNet was higher than that from MOLLI4(1)3(1)2 (15 ms vs. 9 ms, all P < 0,05). The mean CV of native myocardium and blood T1 was ~ 5% and 2% by MOLLI5(3)3 and MyoMapNet. The CV of the post-contrast T1 by MyoMapNet was higher than those by MOLLI5(3)3 (myocardium: 4.3% vs. 3.8%; blood: 2.7% vs. 1.7%, all P < 0,05; Additional file 1: Table S5).
Discussion
In this study, we developed and evaluated MyoMapNet, an accelerated myocardial T1 mapping approach that can perform T1 mapping within four heartbeats. An FCNN was trained to estimate T1 values using four T1 weighted signals sampled along a single Look-Locker inversion-recovery curve. Through phantom and in-vivo validation using existing data and prospectively collected data, we demonstrated that a MyoMapNet model trained with a combination of native and post-contrast T1 mapping data can be used to calculate T1 for both native and post-contrast T1 mapping. Thus, a single FCNN model for both native and post-contrast T1 mapping using a single LL4 sequence is sufficient. Our inline implementation of the model demonstrated feasibility for rapidly deploying such a model on the scanner.
It is well established that MOLLI has several confounders (e.g., heart rate, T2 sensitivity, magnetization transfer) [2, 36, 37]. In addition, MOLLI T1 is lower than actual T1 due to the intermittent bSSFP readout compared to a standard continuous gradient-echo Look-Locker acquisition. Since we used MOLLI data for training the model, the current implementation of MyoMapNet has theoretically similar limitations as MOLLI. Alternative approaches in which the model is trained using a more accurate T1 mapping sequence could improve the accuracy of MypMapNet. Numerical simulations using the Bloch equation could be used to generate synthetic data for training with the ground truth. A combination of simulated and in-vivo signals could also be used to train the network to further improve MyoMaoNet accuracy and robustness.
We investigated MyoMapNet performance in terms of accuracy and precision using only four T1-weighted images and compared it with conventional MOLLI. However, one can create T1 map using a reduced number of T1-weighted images using a conventional 2 or 3-parameter fitting model. Fitts et al. [38] proposed an arrhythmia insensitive rapid cardiac T1 mapping pulse sequence based on only two T1-weighted images; however, estimated T1 values differed with conventional MOLLI [39]. Our group had previously compared MyoMapNet versus a conventional fitting model using the same number of T1-weighted imaging. In comparison to MyoMapNet, conventional fitting had lower precision and larger bias. Additionally, curve-fitting performance differs for images with different signal-to-noise ratios and T1 values. For the existing MOLLI dataset used in this study, we performed a head-to-head comparison of both approaches (results are included in Supplementary Materials), which also demonstrated similar loss of precision and increased bias.
We randomly divided our existing MOLLI dataset into 80%-10%-10% for training, validation, and testing. While there is no optimal split percentage, using 60–80% of the data for training is quite common. The model performance could be impacted by the splitting ratio [40]. Since we used independent prospectively collected data for further evaluation of the final trained model and its generalizability, we did not investigate different data splitting ratios. An alternative approach would be to stratify the data based on the distribution of T1 values, so all expected ranges of T1 are represented in the training dataset. Further studies are warranted to further improve the training and generalizability of the model by studying the optimal dataset size and splitting ratio.
We used an FCNN for MyoMapNet to estimate T1 from the reduced number of T1-weighted images. The evaluation indicated that such an FCNN model had comparable precision with MOLLI and was better than curve-fitting method (Additional file 2: Figures S3 and S4). In this model, each pixel is treated independently. Alternatively, a convolutional neural network that incorporates data from neighboring pixels could also be used. In a prior preliminary study, we implemented such a model (data not shown) and observed superior noise performance that could potentially improve T1 precision. Further investigation is warranted to evaluate alternative DL models for MyoMapNet.
Respiratory motion can cause image artifacts in myocardial T1 mapping. Breath-holding or free-breathing imaging with slice tracking in combination with image registration has been used to reduce effects of motion on the parametric mapping [41–43]. In MyoMapNet, we used motion correction to remove any potential misalignment between different T1-weighted images [44]. Further investigation is needed to evaluate whether the breath-hold requirement can be potentially eliminated to reduce patient burden.
We collected prospectively accelerated data to further evaluate MyoMapNet beyond the existing dataset. Although both sequences use similar imaging parameters, there are differences such as breath-holding and in-flow. This was reflected in the greater difference between the two methods in the experiment with prospectively accelerated data than existing MOLLI data. However, such evaluation is necessary to evaluate the performance of an accelerated method in CMR. An inline implementation of MyoMapNet substantially facilitates prototyping and testing of different models on the scanner. We are also taking additional steps to make MyoMapNet and its inline implementation freely available.
DL is rapidly improving the clinical workflow of myocardial tissue characterization. Recent studies have demonstrated the potential of DL to automate analysis and image quality control [45–48]. These methods could automatically perform motion correction, segmentation, and parameter quantification, thereby reducing the burden of manual analysis and observer-related variability. MyoMapNet could be easily integrated with an automated analysis and quality control method to facilitate rapid data collection and the analysis workflow.
In T1 mapping, the choice of inversion time can impact the accuracy and precision [49]. In LL4, after the inversion pulse, samplings along the relaxation curve are separated by the cardiac cycle. Hence, the effective inversion-recovery times are determined by the RR interval length [2, 8]. Except for the first image shortly acquired after the inversion pulse, the rest of the images have a long inversion-recovery time (> RR interval length). This would reduce sensitivity to T1 relaxation when the patient has a low heart rate or mis-triggered heartbeat during imaging, which impacts the T1 map quality, especially post-contrast T1 [49]. In our study, we did not investigate the optimal choice of inversion time of the first T1-weighted images, as we used conventional MOLLI sequence timing and parameters. Other acquisition schemes can potentially be developed to reduce sensitivity to heart rate and improve performance for short T1 values.
Limitations
Our study has several limitations. We did not evaluate the optimal choice of DL architecture; however, the results from the FCNN show excellent agreement with MOLLI. We used existing MOLLI data for training, and it is widely known that MOLLI has intrinsic underestimation. We did not investigate how different confounders, such as B1 or B0 inhomogeneity, could impact MyoMapNet performance. We used a large patient dataset with various clinical indications; however, we did not evaluate the performance of MyoMapNet for specific cardiomyopathies with abnormal T1 values. Finally, data from a single vendor and field strength were used for training, and the generalizability of the trained network should be studied.
Conclusion
The MyoMapNet enables fast myocardial T1 mapping from only four T1-weighted images collected by a single Look-Locker sequence, leading to shorter scan time and rapid map reconstruction.
Supplementary Information
Additional file 1: Table S1. Notation, input, training, prediction, and application of each model. Table S2. Imaging parameters for all sequences used in this study. Table S3. Mean, standard deviation and coefficient of variation (CV) of T1 of each phantom estimated by MOLLI and three MyoMapNet models. Table S4. Standard deviation and coefficient of variation (CV) of T1 of existing data estimated by MOLLI and MyoMapNet. Table S5. Standard deviation and coefficient of variation (CV) of T1 for prospectively collected data by MOLLI and LL4 with MyoMapNet. Table S6. Native, post-contrast T1, and corresponding ECV for existing MOLLI data estimated by curve-fitting methods.
Additional file 2: Figure S1. Simulation results. Bland–Altman plots show the mean difference and 95% limits of agreement in simulated T1 with different signal-to-noise (SNR) between MyoMapNet and MOLLI5(3)3, and LL5-3P-fitting and MOLLI5(3)3. Figure S2. Representative in-vivo T1 and corresponding ECV maps from the different number of T1-weighted images of MOLLI using MyoMapNet and curve-fitting methods. Figure S3. Comparison between MyoMapNet and curve-fitting methods (LL4- and LL5-3P-fitting) for myocardium T1 from four or five T1 weighted images, using MOLLI as reference: MOLLI5(3)3 for native T1 and MOLLI4(1)3(1)2 for post-contrast T1. Each data point was averaged across three LV slices for each patient. Mean difference and 95% limits of agreement are indicated as red and dotted lines, respectively. Figure S4. Comparison of MyoMapNet and curve-fitting methods for blood T1 from a few T1-weighted images (4 or 5) to reference sequences. MOLLI5(3)3 was the reference for native T1, and MOLLI4(1)3(1)2 was the reference for post-contrast T1. Mean difference and 95% limits of agreement are indicated as red and dotted lines for each subfigure, respectively. Figure S5. Comparing ECV from MyoMapNet models and curve fitting (LL4- and LL5-3P-fitting) to MOLLI. Mean difference and 95% limits of agreement are indicated as red and dotted lines for each subfigure, respectively. Native and post-contrast T1 values used for ECV measurement are indicated for each method.
Acknowledgements
The authors thank Dr. Warren J. Manning for his editorial assistance.
Abbreviations
- 2D
Two dimensional
- 3D
Three dimensional
- bSSFP
Balanced steady-state free precession
- CI
Confidence interval
- CMR
Cardiovascular magnetic resonance
- CPMG-SE
Carr-Purcell-Meiboom-Gill spin echo
- CPU
Central processing unit
- CV
Coefficient of variation
- DL
Deep learning
- ECG
Electrocardiogram
- ECV
Extracellular volume
- FCNN
Fully connected neural network
- FIRE
Framework for image reconstruction environment
- Gd
Gadolinium
- GPU
Graphics processing units
- ICE
Siemens Image reconstruction environment.
- IR-SE
Inversion recovery spin echo
- LL4
Look-Locker in 4 heartbeats
- ISMRMRD
International Society of Magnetic Resonance in Medicine Raw Data format
- LV
Left ventricle/left ventricular
- MAE
Mean absolute error
- MOLLI
Modified Look-Locker inversion recovery
- NN
Neural networks
- ROI
Region of interest
- RR
Duration of one heartbeat
- SD
Standard deviation
- ShMOLLI
Shortened modified Look-Locker inversion recovery
- SNR
Signal-to-noise ratio
- TI
Inversion time
Authors' contributions
RG performed all data collection, neural network training, validation, analysis, and preparation of manuscript. HE implemented and tested an initial prototype of the neural network. AA implemented an alternative version of the neural network for a secondary validation and reproducibility assessment. He also performed additional optimization of the learning of the implemented model. SA, XC, XB, and KC involved in implementation of the inline reconstruction and revised manuscript. JC, TY and LN performed image segmentation and data analysis. RN contributed to study design, validation, data interpretation and manuscript revision. All authors critically revised the paper. All authors read and approved the final manuscript.
Funding
Reza Nezafat receives grant funding from the National Institutes of Health (NIH) 1R01HL129185, 1R01HL129157, 1R01HL127015 and 1R01HL154744 (Bethesda, MD, USA); and the American Heart Association 15EIA22710040 (Waltham, MA, USA). Xiaoying Cai, Kelvin Chow and Xiaoming Bi are employees of Siemens Medical Solutions USA, Inc. Reza Nezafat has a research agreement with Siemens.
Availability of data and materials
MyoMapNet is an investigational technique and not available by the vendor as a research tool or product. MyoMapNet codes are openly available on GitHub (https://github.com/HMS-CardiacMR/MyoMapNet). All reconstructed T1 maps are available on Harvard dataverse (https://dataverse.harvard.edu/dataverse/cardiacmr), reference number (https://doi.org/10.7910/DVN/5MZYAH).
Declarations
Ethics approval and consent to participate
This study was approved by the BIDMC Institutional Review Board (IRB) and was Health Insurance Portability and Accountability Act (HIPPA)-compliant.
Consent for publication
All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Competing interests
There is a pending patent application for MyoMapNet. The authors declare that they have no other competing interests. Dr. Matthias Stuber served as a Guest Editor for this manuscript.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Messroghli DR, Moon JC, Ferreira VM, Grosse-Wortmann L, He T, Kellman P, Mascherbauer J, Nezafat R, Salerno M, Schelbert EB, Taylor AJ, Thompson R, Ugander M, van Heeswijk RB, Friedrich MG. Clinical recommendations for cardiovascular magnetic resonance mapping of T1, T2, T2* and extracellular volume: a consensus statement by the Society for Cardiovascular Magnetic Resonance (SCMR) endorsed by the European Association for Cardiovascular Imaging (EACVI) J Cardiovasc Magn Reson. 2017;19(1):75. doi: 10.1186/s12968-017-0389-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kellman P, Hansen MS. T1-mapping in the heart: accuracy and precision. J Cardiovasc Magn Reson. 2014;16:2. doi: 10.1186/1532-429X-16-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chow K, Flewitt JA, Green JD, Pagano JJ, Friedrich MG, Thompson RB. Saturation recovery single-shot acquisition (SASHA) for myocardial T(1) mapping. Magn Reson Med. 2014;71(6):2082–2095. doi: 10.1002/mrm.24878. [DOI] [PubMed] [Google Scholar]
- 4.Xue H, Greiser A, Zuehlsdorff S, Jolly M-P, Guehring J, Arai AE, Kellman P. Phase-sensitive inversion recovery for myocardial T1 mapping with motion correction and parametric fitting. Magn Reson Med. 2013;69(5):1408–1420. doi: 10.1002/mrm.24385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Messroghli DR, Radjenovic A, Kozerke S, Higgins DM, Sivananthan MU, Ridgway JP. Modified Look-Locker inversion recovery (MOLLI) for high-resolution T1 mapping of the heart. Magn Reson Med. 2004;52(1):141–146. doi: 10.1002/mrm.20110. [DOI] [PubMed] [Google Scholar]
- 6.Piechnik SK, Ferreira VM, Dall'Armellina E, Cochlin LE, Greiser A, Neubauer S, Robson MD. Shortened Modified Look-Locker Inversion recovery (ShMOLLI) for clinical myocardial T1-mapping at 1.5 and 3 T within a 9 heartbeat breathhold. J Cardiovasc Magn Reson 2010;12: 69. [DOI] [PMC free article] [PubMed]
- 7.Higgins DM, Ridgway JP, Radjenovic A, Sivananthan UM, Smith MA. T1 measurement using a short acquisition period for quantitative cardiac applications. Med Phys. 2005;32(6):1738–1746. doi: 10.1118/1.1921668. [DOI] [PubMed] [Google Scholar]
- 8.Weingartner S, Akcakaya M, Basha T, Kissinger KV, Goddu B, Berg S, Manning WJ, Nezafat R. Combined saturation/inversion recovery sequences for improved evaluation of scar and diffuse fibrosis in patients with arrhythmia or heart rate variability. Magn Reson Med. 2014;71(3):1024–1034. doi: 10.1002/mrm.24761. [DOI] [PubMed] [Google Scholar]
- 9.Kellman P, Wilson JR, Xue H, Ugander M, Arai AE. Extracellular volume fraction mapping in the myocardium, part 1: evaluation of an automated method. J Cardiovasc Magn Reson. 2012;14:63. doi: 10.1186/1532-429X-14-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Roujol S, Weingartner S, Foppa M, Chow K, Kawaji K, Ngo LH, Kellman P, Manning WJ, Thompson RB, Nezafat R. Accuracy, precision, and reproducibility of four T1 mapping sequences: a head-to-head comparison of MOLLI, ShMOLLI, SASHA, and SAPPHIRE. Radiology. 2014;272(3):683–689. doi: 10.1148/radiol.14140296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weingartner S, Roujol S, Akcakaya M, Basha TA, Nezafat R. Free-breathing multislice native myocardial T1 mapping using the slice-interleaved T1 (STONE) sequence. Magn Reson Med. 2014;74(1):115–124. doi: 10.1002/mrm.25387. [DOI] [PubMed] [Google Scholar]
- 12.Guo R, Chen Z, Wang Y, Herzka DA, Luo J, Ding H. Three-dimensional free breathing whole heart cardiovascular magnetic resonance T1 mapping at 3 T. J Cardiovasc Magn Reson. 2018;20(1):64. doi: 10.1186/s12968-018-0487-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guo R, Cai X, Kucukseymen S, Rodriguez J, Paskavitz A, Pierce P, Goddu B, Nezafat R. Free-breathing whole-heart multi-slice myocardial T(1) mapping in 2 minutes. Magn Reson Med. 2021;85(1):89–102. doi: 10.1002/mrm.28402. [DOI] [PubMed] [Google Scholar]
- 14.Weingartner S, Akcakaya M, Roujol S, Basha T, Stehning C, Kissinger KV, Goddu B, Berg S, Manning WJ, Nezafat R. Free-breathing post-contrast three-dimensional T1 mapping: Volumetric assessment of myocardial T1 values. Magn Reson Med. 2015;73(1):214–222. doi: 10.1002/mrm.25124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weingartner S, Akcakaya M, Roujol S, Basha T, Tschabrunn C, Berg S, Anter E, Nezafat R. Free-breathing combined three-dimensional phase sensitive late gadolinium enhancement and T1 mapping for myocardial tissue characterization. Magn Reson Med. 2015;74(4):1032–1041. doi: 10.1002/mrm.25495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hamilton JI, Jiang Y, Chen Y, Ma D, Lo WC, Griswold M, Seiberlich N. MR fingerprinting for rapid quantification of myocardial T1, T2, and proton spin density. Magn Reson Med. 2017;77(4):1446–1458. doi: 10.1002/mrm.26216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Christodoulou AG, Shaw JL, Nguyen C, Yang Q, Xie Y, Wang N, Li D. Magnetic resonance multitasking for motion-resolved quantitative cardiovascular imaging. Nat Biomed Eng. 2018;2(4):215–226. doi: 10.1038/s41551-018-0217-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Akcakaya M, Weingartner S, Basha TA, Roujol S, Bellm S, Nezafat R. Joint myocardial T1 and T2 mapping using a combination of saturation recovery and T2 -preparation. Magn Reson Med. 2016;76(3):888–896. doi: 10.1002/mrm.25975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Santini F, Kawel-Boehm N, Greiser A, Bremerich J, Bieri O. Simultaneous T1 and T2 quantification of the myocardium using cardiac balanced-SSFP inversion recovery with interleaved sampling acquisition (CABIRIA) Magn Reson Med. 2015;74(2):365–371. doi: 10.1002/mrm.25402. [DOI] [PubMed] [Google Scholar]
- 20.Guo R, Cai X, Kucukseymen S, Rodriguez J, Paskavitz A, Pierce P, Goddu B, Thompson RB, Nezafat R. Free-breathing simultaneous myocardial T1 and T2 mapping with whole left ventricle coverage. Magn Reson Med 2020. [DOI] [PubMed]
- 21.Blume U, Lockie T, Stehning C, Sinclair S, Uribe S, Razavi R, Schaeffter T. Interleaved T1 and T2 relaxation time mapping for cardiac applications. J Magn Reson Imaging. 2009;29(2):480–487. doi: 10.1002/jmri.21652. [DOI] [PubMed] [Google Scholar]
- 22.Kvernby S. Simultaneous three-dimensional myocardial T1 and T2 mapping in one breath hold with 3D-QALAS. J Cardiovasc Magn Reson. 2013;16:2. doi: 10.1186/s12968-014-0102-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sussman MS, Wintersperger BJ. Modified look-locker inversion recovery (MOLLI) T1 mapping with inversion group (IG) fitting - A method for improved precision. Magn Reson Imaging. 2019;62:38–45. doi: 10.1016/j.mri.2019.06.002. [DOI] [PubMed] [Google Scholar]
- 24.Sussman MS, Yang IY, Fok KH, Wintersperger BJ. Inversion group (IG) fitting: A new T1 mapping method for modified look-locker inversion recovery (MOLLI) that allows arbitrary inversion groupings and rest periods (including no rest period) Magn Reson Med. 2016;75(6):2332–2340. doi: 10.1002/mrm.25829. [DOI] [PubMed] [Google Scholar]
- 25.Zhu Y, Kang J, Duan C, Nezafat M, Neisius U, Jang J, Nezafat R. Integrated motion correction and dictionary learning for free-breathing myocardial T1 mapping. Magn Reson Med. 2019;81(4):2644–2654. doi: 10.1002/mrm.27579. [DOI] [PubMed] [Google Scholar]
- 26.Doneva M, Börnert P, Eggers H, Stehning C, Sénégas J, Mertins A. Compressed sensing reconstruction for magnetic resonance parameter mapping. Magn Reson Med. 2010;64(4):1114–1120. doi: 10.1002/mrm.22483. [DOI] [PubMed] [Google Scholar]
- 27.Shao J, Rapacchi S, Nguyen KL, Hu P. Myocardial T1 mapping at 3.0 tesla using an inversion recovery spoiled gradient echo readout and bloch equation simulation with slice profile correction (BLESSPC) T1 estimation algorithm. J Magn Reson Imaging. 2016;43(2):414–425. doi: 10.1002/jmri.24999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cohen O, Zhu B, Rosen MS. MR fingerprinting Deep RecOnstruction NEtwork (DRONE) Magn Reson Med. 2018;80(3):885–894. doi: 10.1002/mrm.27198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang Q, Su P, Chen Z, Liao Y, Chen S, Guo R, Qi H, Li X, Zhang X, Hu Z, Lu H, Chen H. Deep learning–based MR fingerprinting ASL ReconStruction (DeepMARS) Magn Reson Med. 2020;84(2):1024–1034. doi: 10.1002/mrm.28166. [DOI] [PubMed] [Google Scholar]
- 30.Shao J, Ghodrati V, Nguyen KL, Hu P. Fast and accurate calculation of myocardial T(1) and T(2) values using deep learning Bloch equation simulations (DeepBLESS) Magn Reson Med. 2020;84(5):2831–2845. doi: 10.1002/mrm.28321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hamilton JI, Currey D, Rajagopalan S, Seiberlich N. Deep learning reconstruction for cardiac magnetic resonance fingerprinting T1 and T2 mapping. Magn Reson Med. 2021;85(4):2127–2135. doi: 10.1002/mrm.28568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nezafat M, El-Rewaidy H, Kucukseymen S, Hauser TH, Fahmy AS. Deep convolution neural networks based artifact suppression in under-sampled radial acquisitions of myocardial T 1 mapping images. Phys Med Biol. 2020;65(22):225024. doi: 10.1088/1361-6560/abc04f. [DOI] [PubMed] [Google Scholar]
- 33.Gatsoni O, Aletras AH, Heiberg E, Berggren K. T1 Mapping By Means Of Deep Learning Neural Networks Using Both Saturation Recovery and Inversion Recovery Data. FL: Society for Cardiovascular Magnetic Resonance (SCMR) Orlando; 2020. [Google Scholar]
- 34.Inati SJ, Naegele JD, Zwart NR, Roopchansingh V, Lizak MJ, Hansen DC, Liu CY, Atkinson D, Kellman P, Kozerke S, Xue H, Campbell-Washburn AE, Sørensen TS, Hansen MS. ISMRM Raw data format: a proposed standard for MRI raw datasets. Magn Reson Med. 2017;77(1):411–421. doi: 10.1002/mrm.26089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Captur G, Gatehouse P, Keenan KE, Heslinga FG, Bruehl R, Prothmann M, Graves MJ, Eames RJ, Torlasco C, Benedetti G, Donovan J, Ittermann B, Boubertakh R, Bathgate A, Royet C, Pang W, Nezafat R, Salerno M, Kellman P, Moon JC. A medical device-grade T1 and ECV phantom for global T1 mapping quality assurance-the T1 Mapping and ECV Standardization in cardiovascular magnetic resonance (T1MES) program. J Cardiovasc Magn Reson. 2016;18(1):58. doi: 10.1186/s12968-016-0280-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chow K, Flewitt J, Pagano JJ, Green JD, Friedrich MG, Thompson RB. T2-dependent errors in MOLLI T1 values: simulations, phantoms, and in-vivo studies. J Cardiovasc Magn Reson. 2012;14(Suppl 1):P281. [Google Scholar]
- 37.Robson MD, Piechnik SK, Tunnicliffe EM, Neubauer S. T1 measurements in the human myocardium: the effects of magnetization transfer on the SASHA and MOLLI sequences. Magn Reson Med. 2013;70(3):664–670. doi: 10.1002/mrm.24867. [DOI] [PubMed] [Google Scholar]
- 38.Fitts M, Breton E, Kholmovski EG, Dosdall DJ, Vijayakumar S, Hong KP, Ranjan R, Marrouche NF, Axel L, Kim D. Arrhythmia insensitive rapid cardiac T1 mapping pulse sequence. Magn Reson Med. 2013;70(5):1274–1282. doi: 10.1002/mrm.24586. [DOI] [PubMed] [Google Scholar]
- 39.Hong K, Kim D. MOLLI and AIR T1 mapping pulse sequences yield different myocardial T1 and ECV measurements. NMR Biomed. 2014;27(11):1419–1426. doi: 10.1002/nbm.3221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Xu Y, Goodacre R. On splitting training and validation set: a comparative study of cross-validation, bootstrap and systematic sampling for estimating the generalization performance of supervised learning. J Anal Test. 2018;2(3):249–262. doi: 10.1007/s41664-018-0068-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Roujol S, Foppa M, Weingartner S, Manning WJ, Nezafat R. Adaptive registration of varying contrast-weighted images for improved tissue characterization (ARCTIC): application to T1 mapping. Magn Reson Med. 2015;73(4):1469–1482. doi: 10.1002/mrm.25270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.El-Rewaidy H, Nezafat M, Jang J, Nakamori S, Fahmy AS, Nezafat R. Nonrigid active shape model-based registration framework for motion correction of cardiac T1 mapping. Magn Reson Med. 2018;80(2):780–791. doi: 10.1002/mrm.27068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bush MA, Ahmad R, Jin N, Liu Y, Simonetti OP. Patient specific prospective respiratory motion correction for efficient, free-breathing cardiovascular MRI. Magn Reson Med. 2019;81(6):3662–3674. doi: 10.1002/mrm.27681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Xue H, Shah S, Greiser A, Guetter C, Littmann A, Jolly MP, Arai AE, Zuehlsdorff S, Guehring J, Kellman P. Motion correction for myocardial T1 mapping using image registration with synthetic image estimation. Magn Reson Med. 2012;67(6):1644–1655. doi: 10.1002/mrm.23153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fahmy AS, El-Rewaidy H, Nezafat M, Nakamori S, Nezafat R. Automated analysis of cardiovascular magnetic resonance myocardial native T1 mapping images using fully convolutional neural networks. J Cardiovasc Magn Reson. 2019;21(1):7. doi: 10.1186/s12968-018-0516-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Leiner T, Rueckert D, Suinesiaputra A, Baessler B, Nezafat R, Isgum I, Young AA. Machine learning in cardiovascular magnetic resonance: basic concepts and applications. J Cardiovasc Magn Reson. 2019;21(1):61. doi: 10.1186/s12968-019-0575-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhang Q, Hann E, Werys K, Wu C, Popescu I, Lukaschuk E, Barutcu A, Ferreira VM, Piechnik SK. Deep learning with attention supervision for automated motion artefact detection in quality control of cardiac T1-mapping. Artif Intell Med. 2020;110:101955. doi: 10.1016/j.artmed.2020.101955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhu Y, Fahmy AS, Duan C, Nakamori S, Nezafat R. Automated myocardial T2 and extracellular volume quantification in cardiac mri using transfer learning–based myocardium segmentation. Radiology. 2020;2(1):e190034. doi: 10.1148/ryai.2019190034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Akcakaya M, Weingartner S, Roujol S, Nezafat R. On the selection of sampling points for myocardial T1 mapping. Magn Reson Med. 2015;73(5):1741–1753. doi: 10.1002/mrm.25285. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. Notation, input, training, prediction, and application of each model. Table S2. Imaging parameters for all sequences used in this study. Table S3. Mean, standard deviation and coefficient of variation (CV) of T1 of each phantom estimated by MOLLI and three MyoMapNet models. Table S4. Standard deviation and coefficient of variation (CV) of T1 of existing data estimated by MOLLI and MyoMapNet. Table S5. Standard deviation and coefficient of variation (CV) of T1 for prospectively collected data by MOLLI and LL4 with MyoMapNet. Table S6. Native, post-contrast T1, and corresponding ECV for existing MOLLI data estimated by curve-fitting methods.
Additional file 2: Figure S1. Simulation results. Bland–Altman plots show the mean difference and 95% limits of agreement in simulated T1 with different signal-to-noise (SNR) between MyoMapNet and MOLLI5(3)3, and LL5-3P-fitting and MOLLI5(3)3. Figure S2. Representative in-vivo T1 and corresponding ECV maps from the different number of T1-weighted images of MOLLI using MyoMapNet and curve-fitting methods. Figure S3. Comparison between MyoMapNet and curve-fitting methods (LL4- and LL5-3P-fitting) for myocardium T1 from four or five T1 weighted images, using MOLLI as reference: MOLLI5(3)3 for native T1 and MOLLI4(1)3(1)2 for post-contrast T1. Each data point was averaged across three LV slices for each patient. Mean difference and 95% limits of agreement are indicated as red and dotted lines, respectively. Figure S4. Comparison of MyoMapNet and curve-fitting methods for blood T1 from a few T1-weighted images (4 or 5) to reference sequences. MOLLI5(3)3 was the reference for native T1, and MOLLI4(1)3(1)2 was the reference for post-contrast T1. Mean difference and 95% limits of agreement are indicated as red and dotted lines for each subfigure, respectively. Figure S5. Comparing ECV from MyoMapNet models and curve fitting (LL4- and LL5-3P-fitting) to MOLLI. Mean difference and 95% limits of agreement are indicated as red and dotted lines for each subfigure, respectively. Native and post-contrast T1 values used for ECV measurement are indicated for each method.
Data Availability Statement
MyoMapNet is an investigational technique and not available by the vendor as a research tool or product. MyoMapNet codes are openly available on GitHub (https://github.com/HMS-CardiacMR/MyoMapNet). All reconstructed T1 maps are available on Harvard dataverse (https://dataverse.harvard.edu/dataverse/cardiacmr), reference number (https://doi.org/10.7910/DVN/5MZYAH).