American Indian (AI) and First Nations (i.e., Indigenous) communities withstand unequal burdens of historical and psychosocial stressors relative to non-Indigenous people [1, 2]. Included among these social determinants of health is ongoing discrimination and marginalization of Indigenous people, inequities in access to health care, and historical trauma, the accumulating, ongoing, and intergenerational transmission of psychological pain resulting from collective exposure to historically traumatic experiences (e.g., boarding schools, relocation programs, etc.) [1, 2, 3]. These historically anchored and enduring factors result in substance misuse and mental health disparities for some Indigenous groups [3] that contribute heavily to heightened premature mortality rates [4]. Yet, we know little about psychiatric disorders among Indigenous people, particularly in the context of life course development. Without such data, targets for optimizing prevention and treatment are unclear, lessening potential to improve health in Indigenous communities.
Among the data that do exist are findings from the Great Smoky Mountains Study (GSMS) where AI youth reported slightly lower prevalence of mental disorders compared to White youth in a shared geographic region [5]. As they age through adolescence, however, Indigenous people appear to experience disproportionately high rates of substance use disorders (SUD) and related consequences [5, 6]. Importantly, rates of disorder vary tremendously across the exceptionally diverse tribal communities of North America [7, 8], highlighting the value of within-culture studies.
Evidence from diverse populations suggests that early mental illness foretells later problems including adult psychiatric disorders [9, 10], but how this plays out in Indigenous communities is less clear. For instance, Indigenous youth may experience earlier onset SUD [6, 11], and earlier intoxication has been linked to adolescent and early adult SUD in an urban AI sample [12]; yet national data show high rates of AI alcohol abstinence in adulthood [13–15]. In addition, there appear to be relatively low levels of internalizing disorders like depression [7, 16] among Indigenous adults despite high exposure to early life risks [8, 17] and indicators of extreme psychological suffering (e.g., heightened youth suicide) [18]. These findings suggest unique patterns of disorder for Indigenous communities vis-à-vis non-Indigenous groups.
A more general limitation of the psychiatric epidemiological literature is a dearth of prospective studies of disorders in which individuals are re-assessed as they develop. Prospective studies are critical because retrospective approaches underestimate actual burden due to recall bias [19, 20]. For instance, lifetime disorder prevalence was doubled in prospective compared to retrospective data among 32-year-olds [21], and two-to-twelve times greater in a sample that extending into older adulthood [20]. Prospective data spanning critical transitional periods of the life course (e.g., adolescence to adulthood) is especially sparse. The GSMS is a notable exception and included oversampling of Indigenous youth [22]. While period (past-year) prevalence rates in the GSMS were relatively low at 13%, the cumulative lifetime psychiatric disorder rate by age 21 was higher than 90% for the most frequently assessed study cohort [19].
In sum, limited evidence hints at unique developmental experiences with mental disorders (i.e., lower internalizing disorders, earlier onset and recovery from SUDs) for Indigenous people. There is little prospective data on psychiatric disorders generally and especially for Indigenous communities where burden of risk may be greatest and developmental rates of disorders are unknown. We contribute new information to these issues by documenting cumulative and twelve-month prevalence of select DSM-IV psychiatric disorders across the early life course among Indigenous young adults from a single cultural group. We also compare prospective and retrospective reporting of lifetime mental disorders.
Methods
Data are from Healing Pathways, a prospective, community-based participatory research (CBPR) project with four reservations in the Northern Midwest US and four Canadian First Nations reserves, all representing a single Indigenous cultural group. We do not explicitly name the cultural background or sites involved in the study to honor community requests for anonymity. The study originated in the early 2000’s with requests from tribal members to generate reliable data on the scope of mental health and substance use issues in their communities, and to identify targets for substance use prevention and health promotion with resulting data. Community research councils (CRCs) are supported in each partnering site by project funding and are co-leaders on project design, implementation, and data interpretation activities; CRCs have also been active and creative in advising team efforts to translate scientific data into locally useful products. Outcomes of this process include tribally-based presentations of research findings, creation of comprehensive technical reports shared with tribal leaders and service providers for local grant-writing and reporting needs, translation of manuscripts into infographics for community use, social media posts and newsletters to communicate study progress, and a YouTube channel to highlight major findings. In the most recent waves of data collection, we assessed participant views on the usefulness of the study and personal experiences associated with participation. Participants expressed overwhelming support for the study, project staff, and the potential impact of the work (e.g., “It has given me a sense of honor to help future generation of American Indians, because I hope to make positive improvement with others in my community and for my community,” and “It reminds me of the importance to study cultures who are ignored by mainstream US culture. It reminds me how valuable and important my culture and ethnicity is to myself and future generations.”).
The original study consisted of eight waves of data collected annually with a target adolescent and at least one primary caregiver beginning in 2002. Eligible adolescents were aged 10–12 years, enrolled tribal members, and living on or near (within 50 miles) the reservation/reserve. For more information on the study design and sampling procedure see [23]. Wave 9 data was collected from 2017–2018 with original target adolescents were aged 24–27 years.
Diagnostic data were collected via computer-assisted personal interviews by trained tribal community interviewers. Participants received $40 for waves 1 – 8 and $50 at wave 9. Study procedures were collaboratively developed by community and university team members and approved by the University institutional review boards. All manuscripts are reviewed by reservation/reserve CRCs prior to submission for publication.
The sample consists of 735 adolescents who enrolled at baseline1 representing a response rate of 79.4%. Diagnostic interviews were conducted at waves 1 (mean age=11.1 years), 4 (mean age=14.3 years), 6 (mean age=16.2 years), 8 (mean age=18.3 years), and 9 (mean age=26.3 years). Of the 735 baseline target adolescents, 659 were interviewed at wave 4, 655 at wave 6, 591 at wave 8, and 453 at wave 9; 27 adolescents passed away by wave 9, and 3 became ineligible due to disability or military service, and 3 did not complete a wave 9 diagnostic interview.. After accounting for deceased and ineligible participants, retention rates were 90.5%, 90.1%, 81.9%, and 64.3%, respectively. Participants who remained in the study were no more likely to meet criteria for any of the mental disorders than those not interviewed at wave 9, but those missed at wave 9 were more likely to be male.
The wave 9 sample was 42.3% male and 57.0% female (0.7% reported non-binary gender identity). Two-thirds (67%) reported living on a reservation/reserve. Approximately 28% did not finish high school, 39.5% finished high school/earned a GED, 18.5% had some college education, 9.1% completed an associate’s degree or trade school, and 3.8% had a bachelor’s degree. The mean annual personal income was $18,163.
Measures
Psychiatric disorders were assessed with the Diagnostic Interview Schedule for Children-Revised (DISC-R) when the participants adolescents (waves 1–8) and the World Mental Health Survey Initiative Version of the World Health Organization Composite International Diagnostic Interview (CIDI) when participants were young adults (wave 9). Both instruments are fully-structured and intended for use with lay interviewers [24, 25].
We assessed select DSM-IV-TR [26] lifetime and past-year alcohol abuse and dependence, marijuana abuse and dependence, other drug abuse and dependence, generalized anxiety disorder (GAD), major depressive disorder (MDD), dysthymic disorder (DD), and attention deficit/hyperactivity disorder (ADHD). Adolescents and a caregiver were interviewed at waves 1 and 4, and the adolescent/young adult only thereafter. We present combined parent-adolescent reports for waves 1 and 4 based on reliability research on the DISC [27] and common practice in epidemiological research (separate parent and adolescent reports have been presented elsewhere [28]. We calculated cumulative lifetime rates for each disorder as the sum of the cases from the prior wave plus any new cases who met criteria in the current wave [29].
We included several other variables for use in this report, including two categories of disorder for each wave: (1) substance use disorder (alcohol abuse and dependence, marijuana abuse and dependence, other drug abuse and dependence); and (2) mood disorder (MDD and dysthymia). We also calculated the prevalence of participants who met criteria for at least one disorder and for two or more disorders at each wave.
Results
Cumulative Prevalence and Comorbidity
By wave 9 (mean age = 26.3 years) the cumulative lifetime prevalence of meeting diagnostic criteria for any mental disorder assessed in this study reached 77.3% and prevalence of any two or more disorders was 56.4% (Table 1). Lifetime disorder and comorbidity at wave 9 was higher among females than males; this difference was not statistically significant. Past-year prevalence of any disorder at wave 9 was 28.7% and past-year comorbidity 6.7%. Highest observed estimates of past-year prevalence and comorbidity occurred at wave 4 when participants were on average 14.3 years of age.
Table 1.
Past-Year and Cumulative Lifetime Prevalence of DSM-IV Disorders
Note.
Lifetime (all alcohol/SUDs) + past year (GAD, mood disorders, and ADHD Wave 1–8; Lifetime (all disorders) Wave 9. Combined caretaker and youth reports Waves 1, 4; Youth reports only, Waves 6, 8, 9.
p<.10;
p<.05;
p<.01
SUDs
SUDs represented the highest prevalence of the observed cumulative lifetime disorders in this sample (68.2%, wave 9). Peak rates of past-year SUDs (alcohol, marijuana) were seen at wave 6 (mean age = 16.2 years). Nearly all of those meeting criteria for a SUD between waves 1 – 8 did so for alcohol or marijuana use disorders; rates of “other” SUDs hovered around 0 – 1%. At wave 9, however, cumulative lifetime rates of other SUDs rose to 11.1% and 18.7% for abuse and dependence, respectively. Past-year estimates of wave 9 “other” SUDs were 2.9% for abuse and 6% for dependence. The three most commonly endorsed other drugs of abuse and dependence were stimulants, opioids, and painkillers.
Internalizing Disorders
Lifetime estimates of GAD were significantly higher among females than males. Past-year GAD at wave 9 was 5.6% overall, representing the highest period estimate of GAD across longitudinal assessments. At wave 9, nearly one-quarter of the sample reported cumulative lifetime MDD and 7.3% met past-year criteria. Cumulative lifetime DD was 5.6% and past-year rates 1.1% at wave 9.
Attention Deficit/Hyperactivity Disorder (ADHD)
Cumulative lifetime rates of ADHD at wave 9 were 18.4% with few cases meeting past-year criteria (2.9%). Peak period estimates of ADHD were observed at wave 1 (9.6%).
Specific Comorbidity
Past-year and lifetime wave 9 estimates of specific combinations of comorbid disorders are displayed in Table 2. Among the 94 participants meeting past-year criteria for SUDs (top half of table), 12.8% met criteria for GAD, and 11.7% met criteria for MDD. Two-thirds of participants met lifetime criteria for SUD (bottom half of table). Of those, 27.7% met criteria for comorbid MDD, and 21.2% for ADHD. Rates of SUD with comorbid internalizing conditions were greater for females than males in both past-year and lifetime estimates.
Table 2.
Past year and lifetime comorbidity for DSM-IV Disorders, Wave 9
| Total (n = 450) | Males (n = 190) | Females (n = 260) | ||||
|---|---|---|---|---|---|---|
| Past year comorbidity | n | % | n | % | n | % |
| SUD | 94 | 20.9 | 44 | 23.2 | 50 | 19.2 |
| with MDD | 11 | 11.7 | 1 | 2.3 | 10 | 20.0 |
| with GAD | 12 | 12.8 | 5 | 11.4 | 7 | 14.0 |
| with ADHD | 3 | 3.2 | 0 | 0.0 | 3 | 6.0 |
| MDD | 33 | 7.3 | 9 | 4.7 | 24 | 9.2 |
| with SUD | 11 | 33.3 | 1 | 11.1 | 10 | 41.7 |
| with GAD | 12 | 36.4 | 4 | 44.4 | 8 | 33.3 |
| with ADHD | 4 | 12.1 | 2 | 22.2 | 2 | 8.3 |
| GAD | 25 | 5.3 | 9 | 4.7 | 16 | 6.2 |
| with SUD | 12 | 48.0 | 5 | 55.6 | 7 | 43.8 |
| with MDD | 12 | 48.0 | 4 | 44.4 | 8 | 50.0 |
| with ADHD | 1 | 4.0 | 1 | 11.1 | 0 | 0.0 |
| ADHD | 13 | 2.9 | 4 | 2.1 | 9 | 3.5 |
| with SUD | 3 | 23.1 | 0 | 0.0 | 3 | 33.3 |
| with MDD | 4 | 30.8 | 2 | 50.0 | 2 | 22.2 |
| with GAD | 1 | 7.7 | 1 | 25.0 | 0 | 0.0 |
| Lifetime comorbidity | n | % | n | % | n | % |
| SUD | 307 | 68.2 | 125 | 65.8 | 182 | 70.0 |
| with MDD | 85 | 27.7 | 23 | 18.4 | 62 | 34.1 |
| with GAD | 55 | 17.9 | 11 | 8.8 | 44 | 34.2 |
| with ADHD | 65 | 21.2 | 25 | 20.0 | 40 | 22.0 |
| MDD | 108 | 24.0 | 33 | 17.4 | 75 | 28.8 |
| with SUD | 85 | 78.7 | 23 | 69.7 | 62 | 82.7 |
| with GAD | 41 | 38.0 | 11 | 33.3 | 30 | 40.0 |
| with ADHD | 31 | 28.7 | 9 | 27.3 | 22 | 29.3 |
| GAD | 70 | 15.6 | 17 | 8.9 | 53 | 20.4 |
| with SUD | 55 | 78.6 | 11 | 64.7 | 44 | 83.0 |
| with MDD | 41 | 58.6 | 11 | 64.7 | 30 | 56.6 |
| with ADHD | 24 | 34.3 | 7 | 41.2 | 17 | 32.1 |
| ADHD | 83 | 18.4 | 38 | 20.0 | 45 | 17.3 |
| with SUD | 65 | 78.3 | 25 | 65.8 | 40 | 88.9 |
| with MDD | 31 | 37.3 | 9 | 23.7 | 22 | 48.9 |
| with GAD | 24 | 28.9 | 7 | 18.4 | 17 | 37.8 |
Although fewer participants met criteria for disorders other than SUD, large proportions of those who did met criteria for co-occurring disorders. The most frequent comorbid disorder among participants with past-year MDD (n=33) was GAD (36.4%) followed closely by SUD (33.3%). MDD with GAD was more common for male compared to female participants, and MDD with SUD was higher for females than males. A sizeable proportion of the 108 participants who met lifetime criteria for MDD also had a lifetime history of SUD (78.7%).
Comorbid SUD or MDD was present for roughly half of the 25 participants meeting criteria for past-year GAD. Among participants who met lifetime criteria for GAD (n=70), over three-quarters also had a lifetime history of SUD and 58.6% MDD.
Of the thirteen participants meeting criteria for past-year ADHD, three (all females) also had past-year SUDs and four comorbid MDD. Among the 83 participants meeting lifetime ADHD criteria, 78.3% also reported lifetime SUDs. Lifetime ADHD combined with lifetime SUD among females represented the highest estimate of comorbidity observed in Table 2, reaching 88.9%.
Retrospective and Cumulative Comparisons
We compared cumulative rates of disorder to retrospective assessments at wave 9 and plotted these comparisons for SUDs (i.e., the disorders with lifetime reports at all waves of the study), any one disorder, and comorbidities in Figures 1 and e1. Wave 9 retrospective assessment of any lifetime disorder underestimated prevalence by 13.5% compared to cumulative rates; comorbidity was underestimated by 22.8%. Underestimation was most pronounced for marijuana dependence (16.5%).
Figure 1.
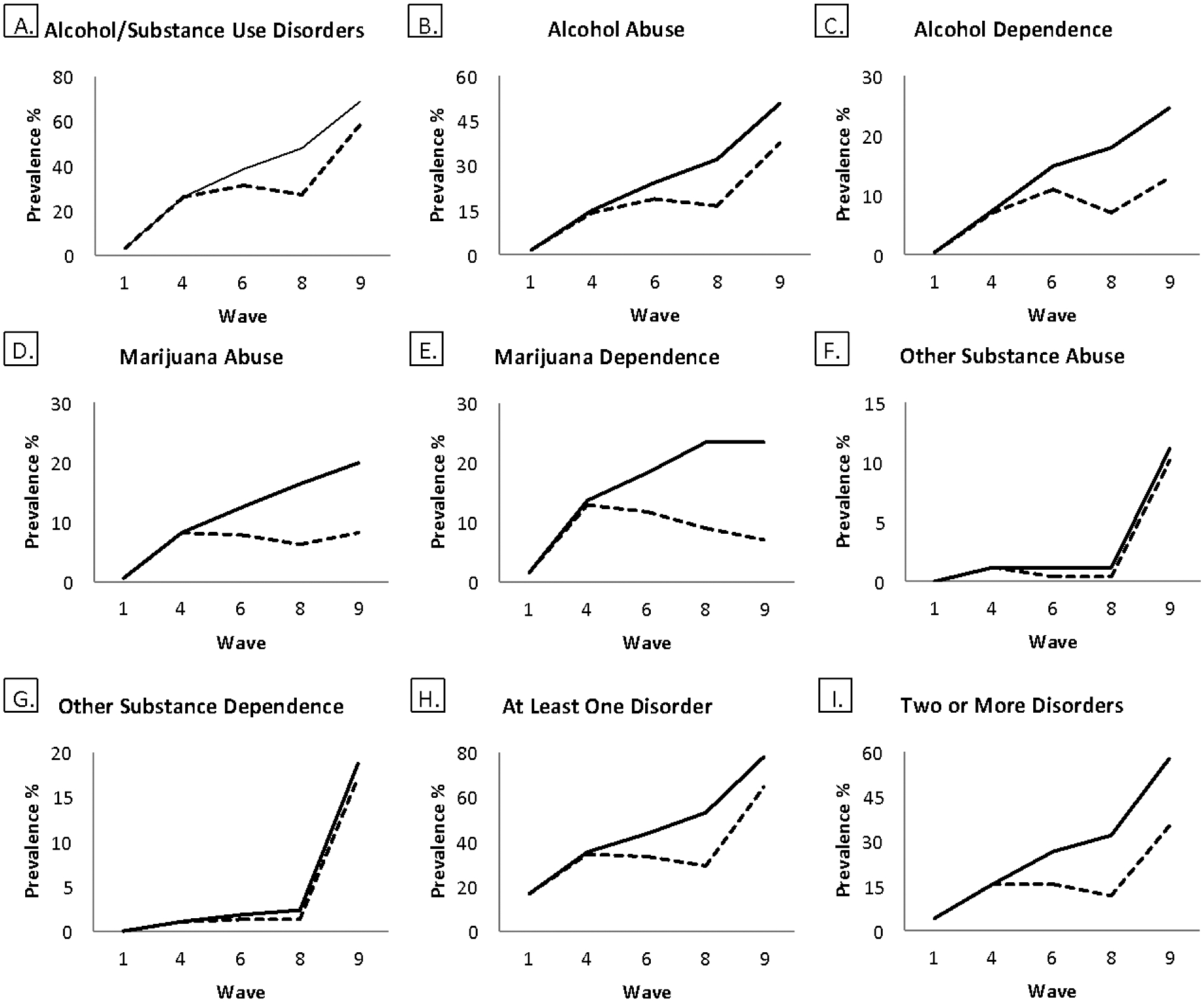
Prevalence rates for cumulative and retrospective lifetime mental and substance use disorders
Discussion
This study provides new evidence of the cumulative, early life course burden of select psychiatric disorders and reinforces prior assertions that a majority of people will experience a mental disorder in their lifetime [21]. Our prospective design is significant in that most existing community-based psychiatric studies rely on retrospective reports of lifetime experiences and yield severe underestimations of true disorder prevalence and uncertainty about mental health service needs. The sample includes Indigenous young adults, a group differentially exposed to historical and contemporary mental health risk factors but lacking representation in psychiatric epidemiological data. At an average of 26.3 years of age, cumulative lifetime rates of disorder in this study reached 77.3%. Our estimate is lower than reports from a previous prospective design that included AIs where peak cumulative lifetime disorder was 90% [19], though this discrepancy may be partially due to the fact that we assessed fewer disorders and accumulated fewer assessments than the comparison study. Cumulative comorbidity by wave 9 reached 56.4%. Greater proportions of females compared to males who met criteria for past-year or lifetime GAD or MDD also met criteria for co-occurring SUD, although this trend was not consistently statistically significant. These gender differences were most pronounced at wave 9 and may signal need for gender-responsive prevention and treatment initiatives for Indigenous youth and young adults.
Across all waves, SUDs were the most commonly occurring class of psychiatric disorders with cumulative wave 9 lifetime and past-year rates reaching 68.2% and 20.9%, respectively. Lifetime alcohol use disorders (abuse = 50.4%; dependence = 24.4%) were comparatively higher than one cumulative estimate comparison (26% alcohol use disorders) [20], yet lower than the Dunedin longitudinal study (31.8% alcohol dependence) [21]. Marijuana abuse (19.6%) and dependence (22.7%) were similar in our sample to a cumulative estimate of 21% for cannabis use/dependence in the GSMS that included AIs [30]. Prior research suggests median age of onset of 20 years for SUDs [31]. The GSMS sample of AI and white young adults demonstrated trajectories of cannabis use disorders across ethnicities that peaked in early adulthood [30]. It is therefore compelling that peak past-year rates for SUD in the current sample occurred at wave 6 when participants were an average of 16.2 years of age. The fact that a majority of lifetime cases of SUD can be accounted for prior to age 18 in these data corroborates previous reports of earlier onset and problematic substance use in some Indigenous communities [32, 33]. Paradoxically, wave 9 (early adult) past-year SUD was lower than reported at adolescent assessments (waves 4, 6, 8) and not attributable to sample attrition (see Methods). Thus, research to identify factors relevant to recovery from SUD for Indigenous people across diverse tribal contexts is warranted.
A notable jump in “other” SUDs at wave 9 was largely accounted for by increases in abuse and dependence to painkillers, stimulants, and opioids. Early descriptions of the opioid crisis suggested heaviest impacts among rural and White Americans [34], and some national data demonstrate that AIs are less likely to die than Whites of opioid overdose [35]. Yet, AIs had a faster rate of increase in opioid-related deaths than did Whites between 1999–2015 [36], and AIs in Minnesota (one state from which participants were drawn) were over 6 times more likely to die of opioid overdose than non-Natives between 2011 and 2015 [35, 37]. These findings underscore the importance of local surveillance, cultural variations within ethnic groups, and attention to racial/ethnic disparities hidden by popular headlines. Existing evidence-based treatments for SUDs rely largely on evidence accumulated without Indigenous participants or perspectives, and tribal community members have expressed concerns about the cultural appropriateness of such interventions. The data presented here provide another compelling call for policymakers to take notice: Indian Health Service (IHS), tribal, urban, and AIAN research funding allocations to address AI needs should be increased and match community priorities for culturally grounded solutions.
Rates of cumulative internalizing disorders in this study sample were generally closer to those reported in prior longitudinal research. For instance, our cumulative estimations of lifetime MDD and GAD were 24% and 15.6% by age 26. This compares to cumulative estimates for MDD of 13.1% [20] and 14.2% for GAD [21]. A notable exception in this trend is a 41.4% estimated prevalence of MDD among 32 year-olds in the Dunedin study [21]. Our DSM-derived estimates of depression seem low given heightened exposure to risk factors and evidence that other indicators of psychological suffering like suicidality are disproportionately high in many Indigenous communities [18]. The validity of measures of internalizing symptoms across cultures has been previously critiqued [38], and our finding could be a signal that current operationalization of MDD misaligns with Indigenous expressions of distress [39, 40].
Given the lack of comparability between prospective and retrospective data, we further discuss our findings vis-à-vis existing epidemiological literature using retrospective reports and past-year prevalence. Wave 9 retrospective reports of lifetime disorder were 64.9%. This finding is higher than results from the AI-SUPERPFP study including 15 – 54 year old AI adults from two reservations (Southwest Tribe = 41.9%; Northern Plains Tribe = 44.5%) [7]. Our estimate is on par with a national sample of AIANs (66.5%) [41], 10% greater than reported for non-Hispanic Whites (57.5%) [41], and higher than both the widely cited prevalence rate of 46.4% for lifetime disorders from the National Comorbidity Survey sample overall, as well as the 18 – 29 year old NCS cohort whose prevalence was estimated at 52.4% [31]. The discrepancy in retrospective assessments of any lifetime disorder at wave 9 compared to calculated cumulative prevalence (64.9% vs. 77.3%), a difference not nearly as large as the mismatch reported in previous literature ranging from two-to-twelve times higher [20].
Nearly 30% of our sample met criteria for wave 9 past-year disorders compared to 21% (Southwest) and 24.3% (Northern Plains) of AI-SUPERPFP participants [7], 43.4% (women) and 41.5% (men; Axis 1 disorders only) of AIs nationally [41], and 26.2% of the U.S. general population [31]. Similar to lifetime reports, past-year SUDs were the most commonly reported class of disorders among current study participants.
In sum, the cumulative data reveal generally similar or, in some cases, lower rates of overall psychiatric disorder in this sample of Indigenous young adults relative to other prospective studies. Alternatively, comparisons of retrospectively reported lifetime disorder suggest greater burden of disorder in this sample than in other similar study designs with non-Indigenous people, underscoring the importance of longitudinal assessments to understand true prevalence and trajectories of mental health problems across communities. At wave 9, overall rates of past-year disorder were comparable to previous research. In total, overall prevalence of disorder appears similar in this sample to other epidemiological surveys; yet, a critical finding centers around the disproportionately high rates of lifetime SUD in this study relative to other reports. For example, wave 9 lifetime alcohol abuse reached an accumulated rate of 50.4% (37.3% retrospective report) compared to 12.8% for 18 – 29-year-olds in the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) [42]. Past-year rates of alcohol abuse, however, were nearly identical between the young Indigenous adults in this study (7.6%) and NESARC estimates (7.0%), suggesting a paradoxically high rate of recovery despite early onset (adolescent) SUD.
Limitations and Future Directions
We assessed select disorders due to resource limitations and efforts to reduce participant burden. Thus, overall cumulative prevalence of lifetime disorder experiences may be larger than estimated. Measurement validity is a concern in research outside of Euro-middle-class contexts, with special considerations for interpreting research with Indigenous communities [43]. Diagnostic interview schedules like those used in this study rely on “rigid rules” and highly standardized question sets with absence of professional clinical expertise in the diagnostic process [44]. Diagnostic dichotomies (yes/no) may overshadow nuances of distress more evident in continuous measures. Roughly 30% of the young adults in this study met past-year criteria for a wave 9 disorder, 10% less than previously reported by their own adult caregivers [16] and suggesting possible resilience across generations. Further, 59.2% of the young adults in this study are current parents/caregivers, and 59% report desire to have/have more children. An important future investigation involves intergenerational stability and/or desistence of mental disorders for the current cohort of participants to identify those factors that create opportunities for breaking intergenerational cycles of mental health problems.
Conclusion
There are several unique findings in this study relative to prior reporting on psychiatric disorders over the life course. First, discrepancies between retrospective and prospective reports were not as large as observed in previous longitudinal designs. Whether these unique patterns are common to other Indigenous cultural groups remains an empirical question. Second, SUDs were the most commonly reported disorders in our sample whereas internalizing disorders are the highest ranking diagnostic category in many general population studies. Relatedly, and third, compared to non-Indigenous study samples, peak periods of SUD emerged earlier for these Indigenous participants. Fourth, declines in rates of SUD seem to occur for these Indigenous participants during periods of heightened risk identified in non-Indigenous samples (i.e., early adulthood) [42]. These findings thus provide compelling evidence of cultural variation in psychiatric epidemiology, provide targets for early SUD prevention, and intimate important lessons are to be learned from Indigenous communities regarding early life course recovery from psychiatric disorders, particularly SUDs.
Supplementary Material
Key points and relevance.
This is one of few psychiatric epidemiological studies to provide prospective data on the cumulative prevalence of select mental disorders over the early life-course.
Rates of cumulative lifetime psychiatric disorder for the Indigenous participants in this study reached 77.3% by age 26 years, with lifetime comorbidity estimated at 56.4%.
The most commonly occurring class of disorders observed within this sample were substance use disorders), which peaked in terms of past-year prevalence when participants were on average 16.3 years of age.
Declines in rates of SUD occurred during early adulthood for these Indigenous participants, a period of increased risk for SUD observed in other non-Indigenous samples.
Findings imply need for early prevention of SUDs in Indigenous communities and suggest there are important lessons to be learned regarding early life course recovery from psychiatric disorders, particularly SUDs.
Acknowledgements:
The Healing Pathways team includes David Bruyere, Laura Bruyere, Annabelle Jourdain, Priscilla Simard, Trisha Bruyere, Jake Becker, Laureen Bruyere, Frances Whitfield, GayeAnn Allen, Tina Handeland, Victoria Soulier, Bagwajikwe Madosh, Betty Jo Graveen, Clinton Isham, Carol Jenkins, Bill Butcher Jr., Delores Fairbanks, Devin Fineday, Bernadette Gotchie, Gloria Mellado. Christina Howard Marilyn Bowstring, Gary Charwood, Gina Stender, Roberta Roybal, Jim Bedeau, Kathy Dudley, Geraldine Brun, June Holstein, Frances Miller, Brenna Pemberton, Ed Strong, Barbara Thomas, Charity Prentice-Pemberton, FaLeisha Jourdain, Penny King, Valerie King, Linda Perkins, Christie Prentice, Gabe Henry, Howard Kabestra, Dallas Medicine, Glenn Cameron, Jackie Cameron, Gerilyn Fisher, Virginia Pateman, Irene Scott, Cindy McDougall, Whitney Accobee Celeste Cloud, Pat Moran, Stephanie Williams, Natalie Bergstrom, Bonnie Badboy, Elizabeth Kent, Sue Trnka and Laurie Vilas.
Research reported in this manuscript was supported by the National Institute on Drug Abuse of the National Institutes of Health under Award Number R01 DA039912 (M. Walls, PI). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Conflict of Interest: The authors declare that they have no conflict of interest.
N = 11 families enrolled at wave 1 of the study in two remote First Nation communities but were not re-interviewed at subsequent waves and thus are excluded from the current sampling frame (i.e., we did not attempt to contact them for inclusion in the longitudinal study).
References
- 1.American Psychological Association (2016) Stress in America: The Impact of Discrimination. Stress in America Survey [Google Scholar]
- 2.Warne D, Frizzell LB (2014) American Indian Health Policy: Historical Trends and Contemporary Issues. Am J Public Health 104:S263–S267. 10.2105/AJPH.2013.301682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.King M, Smith A, Gracey M (2009) Indigenous health part 2: The underlying causes of the health gap. The Lancet 374:76–85. 10.1016/S0140-6736(09)60827-8 [DOI] [PubMed] [Google Scholar]
- 4.Shiels MS, Chernyavskiy P, Anderson WF, et al. (2017) Trends in premature mortality in the USA by sex, race, and ethnicity from 1999 to 2014: An analysis of death certificate data. The Lancet 389:1043–1054. 10.1016/S0140-6736(17)30187-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Costello EJ, Farmer EMZ, Angold A, et al. (1997) Psychiatric disorders among American Indian and white youth in Appalachia: the Great Smoky Mountains Study. Am J Public Health 87:827–832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Whitbeck LB, Sittner Hartshorn KJ, Crawford DM, et al. (2014) Mental and substance use disorders from early adolescence to young adulthood among indigenous young people: final diagnostic results from an 8-year panel study. Soc Psychiatry Psychiatr Epidemiol 49:961–973. 10.1007/s00127-014-0825-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beals J, Manson SM, Whitesell NR, et al. (2005) Prevalence of DSM-IV Disorders and Attendant Help-Seeking in 2 American Indian Reservation Populations. Arch Gen Psychiatry 62:99–108. 10.1001/archpsyc.62.1.99 [DOI] [PubMed] [Google Scholar]
- 8.Koss MP, Yuan NP, Dightman D, et al. (2003) Adverse childhood exposures and alcohol dependence among seven Native American tribes. Am J Prev Med 25:238–244. 10.1016/S0749-3797(03)00195-8 [DOI] [PubMed] [Google Scholar]
- 9.Federman EB, Costello EJ, Angold A, et al. (1997) Development of substance use and psychiatric comorbidity in an epidemiologic study of white and American Indian young adolescents the Great Smoky Mountains Study. Drug Alcohol Depend 44:69–78 [DOI] [PubMed] [Google Scholar]
- 10.Harrington R, Fudge H, Rutter M, et al. (1990) Adult Outcomes of Childhood and Adolescent Depression: I. Psychiatric Status. Arch Gen Psychiatry 47:465–473. 10.1001/archpsyc.1990.01810170065010 [DOI] [PubMed] [Google Scholar]
- 11.Whitbeck LB, Johnson KD, Hoyt DR, Walls ML (2006) Prevalence and Comorbidity of Mental Disorders among American Indian Children in the Northern Midwest. J Adolesc Health 39:427–434. 10.1016/j.jadohealth.2006.01.004 [DOI] [PubMed] [Google Scholar]
- 12.Henry KL, McDonald JN, Oetting ER, et al. (2011) Age of Onset of First Alcohol Intoxication and Subsequent Alcohol Use Among Urban American Indian Adolescents. Psychol Addict Behav J Soc Psychol Addict Behav 25:48–56. 10.1037/a0021710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barnes PM, Adams PF, Powell-Griner E (2010) Health Characteristics of the American Indian or Alaska Native Adult Population: United States, 2004–2008. Centers for Disease Control, National Center for Health Statistics, Hyattsville, MD: [PubMed] [Google Scholar]
- 14.May PA (1996) Overview of Alcohol Abuse Epidemiology for American Indian Populations. In: Sandefur GD, Rindfuss RR, Cohen B (eds) Changing Numbers, Changing Needs: American Indian Demography and Public Health. National Academy Press, Washington, DC, pp 235–256 [PubMed] [Google Scholar]
- 15.Spicer P, Beals J, Croy CD, et al. (2003) The Prevalence of DSM-III-R Alcohol Dependence in Two American Indian Populations. Alcohol Clin Exp Res 27:1785–1797. 10.1097/01.ALC.0000095864.45755.53 [DOI] [PubMed] [Google Scholar]
- 16.Whitbeck LB, Hoyt D, Johnson K, Chen X (2006) Mental disorders among parents/caretakers of American Indian early adolescents in the Northern Midwest. Soc Psychiatry Psychiatr Epidemiol 41:632–640. 10.1007/s00127-006-0070-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Warne D, Dulacki K, Spurlock M, et al. (2017) Adverse Childhood Experiences (ACE) among American Indians in South Dakota and Associations with Mental Health Conditions, Alcohol Use, and Smoking. J Health Care Poor Underserved 28:1559–1577. 10.1353/hpu.2017.0133 [DOI] [PubMed] [Google Scholar]
- 18.Indian Health Service (2015) Trends in Indian Health: 2014 Edition. Indian Health Service, Rockville, MD [Google Scholar]
- 19.Copeland WE, Shanahan L, Costello EJ, Angold A (2011) Cumulative Prevalence of Psychiatric Disorders by Young Adulthood: A Prospective Cohort Analysis From the Great Smoky Mountains Study. J Am Acad Child Adolesc Psychiatry 50:252–261. 10.1016/j.jaac.2010.12.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Takayanagi Y, Spira AP, Roth KB, et al. (2014) Accuracy of Reports of Lifetime Mental and Physical Disorders: Results From the Baltimore Epidemiological Catchment Area Study. JAMA Psychiatry 71:273–280. 10.1001/jamapsychiatry.2013.3579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moffitt TE, Caspi A, Taylor A, et al. (2010) How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychol Med 40:899–909. 10.1017/S0033291709991036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Costello EJ, Angold, Adrian A, Burns BJ, et al. (1996) The Great Smoky Mountains Study of Youth. Goals, design, methods, and the prevalence of DSM-III-R disorders. Arch Gen Psychiatry 53:1129–1136 [DOI] [PubMed] [Google Scholar]
- 23.Whitbeck LB, Sittner Hartshorn KJ, Walls ML (2014) Indigenous Adolescent Development : Psychological, Social and Historical Contexts. Routledge/Taylor & Francis Group [Google Scholar]
- 24.Kessler RC, Üstün TB (2004) The World Mental Health (WMH) Survey Initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). Int J Methods Psychiatr Res 13:93–121. 10.1002/mpr.168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shaffer D, Schwab-Stone M, Fisher P, et al. (1993) The Diagnostic Interview Schedule for Children-Revised Version (DISC-R): I. Preparation, Field Testing, Interrater Reliability, and Acceptability. J Am Acad Child Adolesc Psychiatry 32:643–650 [DOI] [PubMed] [Google Scholar]
- 26.American Psychiatric Association (2000) Diagnostic and statistical manual of mental disorders: DSM-IV-TR. American Psychiatric Association, Washington, DC [Google Scholar]
- 27.Jensen P, Roper M, Fisher P, et al. (1995) Test-Retest Reliability of the Diagnostic Interview Schedule for Children (DISC 2.1) Parent, Child, and Combined Algorithms. Arch Gen Psychiatry 52:61–71 [DOI] [PubMed] [Google Scholar]
- 28.Whitbeck LB, Yu M, Johnson KD, et al. (2008) Diagnostic Prevalence Rates from Early to Mid-Adolescence among Indigenous Adolescents: First Results from a Longitudinal Study. J Am Acad Child Adolesc Psychiatry 47:890–900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Angold A, Erkanli A, Costello EJ, Rutter M (1996) Precision, Reliability and Accuracy in the Dating of Symptom Onsets in Child and Adolescent Psychopathology. J Child Psychol Psychiatry 37:657–664. 10.1111/j.1469-7610.1996.tb01457.x [DOI] [PubMed] [Google Scholar]
- 30.Copeland WE, Hill S, Costello EJ, Shanahan L (2017) Cannabis use and disorder from childhood to adulthood in a longitudinal community sample with American Indians. J Am Acad Child Adolesc Psychiatry 56:124–132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kessler RC, Chiu WT, Demler O, Walters EE (2005) Prevalence, Severity, and Comorbidity of 12-Month DSM-IV Disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 62:617–627. 10.1001/archpsyc.62.6.617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Roski J, Perry C, McGovern P, et al. (1998) Psychosocial Factors Associated with Alcohol Use Among Young Adolescent American Indians and Whites. J Child Adolesc Subst Abuse 7:1–18. 10.1300/J029v07n02_01 [DOI] [Google Scholar]
- 33.Stanley LR, Swaim RC (2015) Initiation of alcohol, marijuana, and inhalant use by American-Indian and white youth living on or near reservations. Drug Alcohol Depend 155:90–96. 10.1016/j.drugalcdep.2015.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dasgupta N, Beletsky L, Ciccarone D (2018) Opioid Crisis: No Easy Fix to Its Social and Economic Determinants. Am J Public Health 108:182–186. 10.2105/AJPH.2017.304187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Scholl L, Seth P, Kariisa M, et al. (2019) Drug and Opioid-Involved Overdose Deaths — United States, 2013–2017. MMWR Morb Mortal Wkly Rep 67:1419–1427. 10.15585/mmwr.mm6751521e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Joshi S, Weiser T, Warren-Mears V (2018) Drug, Opioid-Involved, and Heroin-Involved Overdose Deaths Among American Indians and Alaska Natives — Washington, 1999–2015. MMWR Morb Mortal Wkly Rep 67:1384–1387. 10.15585/mmwr.mm6750a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Minnesota Department of Health (2018) Race Rate Disparity in Drug Overdose Deaths. Minnesota Department of Health, St. Paul, MN [Google Scholar]
- 38.Nichter M (2010) Idioms of distress revisited. Cult Med Psychiatry 34:401–416. 10.1007/s11013-010-9179-6 [DOI] [PubMed] [Google Scholar]
- 39.Kaufman CE, Beals J, Croy C, et al. (2013) Multilevel context of depression in two American Indian tribes. J Consult Clin Psychol 81:1040–1051. 10.1037/a0034342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.O’Nell TD (1996) Disciplined hearts: history, identity, and depression in an American Indian community. University of California Press, Berkeley [Google Scholar]
- 41.Brave Heart MYH, Lewis-Fernández R, Beals J, et al. (2016) Psychiatric disorders and mental health treatment in American Indians and Alaska Natives: results of the National Epidemiologic Survey on Alcohol and Related Conditions. Soc Psychiatry Psychiatr Epidemiol 51:1033–1046. 10.1007/s00127-016-1225-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hasin DS, Grant BF (2015) The National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Waves 1 and 2: review and summary of findings. Soc Psychiatry Psychiatr Epidemiol 50:1609–1640. 10.1007/s00127-015-1088-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Walls ML, Whitesell NR, Barlow A, Sarche M (2017) Research with American Indian and Alaska Native populations: Measurement matters. J Ethn Subst Abuse 1–21. 10.1080/15332640.2017.1310640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wakefield JC, Schmitz MF (2009) The Measurement of Mental Disorder. In: Scheid TL, Brown TN (eds) A Handbook for the Study of Mental Health: Social Contexts, Theories, and Systems, 2nd ed. Cambridge University Press, Cambridge, UK, pp 20–45 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


