Abstract
Background
Low‐back pain (LBP) is one of the most common and costly musculoskeletal problems in modern society. It is experienced by 70% to 80% of adults at some time in their lives. Massage therapy has the potential to minimize pain and speed return to normal function.
Objectives
To assess the effects of massage therapy for people with non‐specific LBP.
Search methods
We searched PubMed to August 2014, and the following databases to July 2014: MEDLINE, EMBASE, CENTRAL, CINAHL, LILACS, Index to Chiropractic Literature, and Proquest Dissertation Abstracts. We also checked reference lists. There were no language restrictions used.
Selection criteria
We included only randomized controlled trials of adults with non‐specific LBP classified as acute, sub‐acute or chronic. Massage was defined as soft‐tissue manipulation using the hands or a mechanical device. We grouped the comparison groups into two types: inactive controls (sham therapy, waiting list, or no treatment), and active controls (manipulation, mobilization, TENS, acupuncture, traction, relaxation, physical therapy, exercises or self‐care education).
Data collection and analysis
We used standard Cochrane methodological procedures and followed CBN guidelines. Two independent authors performed article selection, data extraction and critical appraisal.
Main results
In total we included 25 trials (3096 participants) in this review update. The majority was funded by not‐for‐profit organizations. One trial included participants with acute LBP, and the remaining trials included people with sub‐acute or chronic LBP (CLBP). In three trials massage was done with a mechanical device, and the remaining trials used only the hands. The most common type of bias in these studies was performance and measurement bias because it is difficult to blind participants, massage therapists and the measuring outcomes. We judged the quality of the evidence to be "low" to "very low", and the main reasons for downgrading the evidence were risk of bias and imprecision. There was no suggestion of publication bias. For acute LBP, massage was found to be better than inactive controls for pain ((SMD ‐1.24, 95% CI ‐1.85 to ‐0.64; participants = 51; studies = 1)) in the short‐term, but not for function ((SMD ‐0.50, 95% CI ‐1.06 to 0.06; participants = 51; studies = 1)). For sub‐acute and chronic LBP, massage was better than inactive controls for pain ((SMD ‐0.75, 95% CI ‐0.90 to ‐0.60; participants = 761; studies = 7)) and function (SMD ‐0.72, 95% CI ‐1.05 to ‐0.39; 725 participants; 6 studies; ) in the short‐term, but not in the long‐term; however, when compared to active controls, massage was better for pain, both in the short ((SMD ‐0.37, 95% CI ‐0.62 to ‐0.13; participants = 964; studies = 12)) and long‐term follow‐up ((SMD ‐0.40, 95% CI ‐0.80 to ‐0.01; participants = 757; studies = 5)), but no differences were found for function (both in the short and long‐term). There were no reports of serious adverse events in any of these trials. Increased pain intensity was the most common adverse event reported in 1.5% to 25% of the participants.
Authors' conclusions
We have very little confidence that massage is an effective treatment for LBP. Acute, sub‐acute and chronic LBP had improvements in pain outcomes with massage only in the short‐term follow‐up. Functional improvement was observed in participants with sub‐acute and chronic LBP when compared with inactive controls, but only for the short‐term follow‐up. There were only minor adverse effects with massage.
Keywords: Adult; Humans; Acute Pain; Acute Pain/therapy; Bias; Chronic Pain; Chronic Pain/therapy; Low Back Pain; Low Back Pain/therapy; Manipulation, Spinal; Massage; Massage/adverse effects; Massage/methods; Randomized Controlled Trials as Topic
Plain language summary
Massage for low‐back pain
Review question
What are the effects of massage therapy for people with low‐back pain (LBP)?
Background
LBP is very common. While most back pain gets better without medical treatment, about 10% of cases lasts for three months or more. There are many therapies that are used to treat the pain, and improve the lives of individuals with back pain. Massage is one of these treatments.
Search date
We updated the searches in 07 August 2014 and included 12 additional randomized controlled trials (RCTs) in this review update.
Study characteristics
In total we included 25 RCTs and 3096 participants in this review update. Only one trial included patients with acute LBP (pain duration less than four weeks), while all the others included patients with sub‐acute (four to 12 weeks) or chronic LBP (12 weeks or longer). In three studies, massage was applied using a mechanical device (such as a metal bar to increase the compression to the skin or a vibrating instrument), and in the remaining trials it was done using the hands. Pain intensity and quality were the most common outcomes measured in these studies, followed by back‐related function, such as walking, sleeping, bending and lifting weights.
Study funding sources
Seven studies did not report the sources of funding, Sixteen studies were funded by not‐for‐profit organizations. One study reported not receiving any funding, and one study was funded by a College of Massage Therapists.
Key results
There were eight studies comparing massage to interventions that are not expected to improve outcomes (inactive controls) and 13 studies comparing massage to other interventions expected to improve outcomes (active controls). Massage was better than inactive controls for pain and function in the short‐term, but not in the long‐term follow‐up. Massage was better than active controls for pain both in the short and long‐term follow‐ups, but we found no differences for function, either in the short or long‐term follow‐ups. There were no reports of serious adverse events in any of these trials. The most common adverse events were increased pain intensity in 1.5% to 25% of the participants.
Quality of the evidence
The quality of the evidence for all comparisons was graded "low " or "very low" which means that we have very little confidence in these results. This is because most of the included studies were small and had methodological flaws.
Summary of findings
Summary of findings for the main comparison. Massage versus inactive controls for sub‐acute and chronic LBP.
| Massage versus inactive controls for sub‐acute and chronic LBP | ||||||
| Patient or population: patients with LBP Settings: Intervention: Massage versus inactive controls for sub‐acute and chronic LBP | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Massage versus inactive controls for sub‐acute and chronic LBP | |||||
| Pain intensity (higher scores mean more pain) ‐ Short‐term follow‐up Numerical pain rating scales (higher scores mean more pain). Scale from: 0 to 100 points. Follow‐up: 0 to 6 months | The mean pain intensity in the inactive control group is 40.6 points (SD 26.7) VAS1 | The mean pain intensity in the massage group is
20.6 points (95%CI 16.6 to 24.6 points) |
Not applicable | 761 (7 studies, 2 studies were duplicated) | ⊕⊕⊝⊝ low2 | Medium, statistically significant effect size (SMD ‐0.75, 95% CI ‐0.90 to ‐0.60) |
| Pain intensity (higher scores mean more pain) ‐ Long‐term follow‐up VAS, Von Korff Pain Scale. Follow‐up: mean 6 months | The mean pain intensity in the inactive control group is 40.6 points (SD 26.7) VAS1 | The mean pain intensity in the massage group is 41.1 points (95%CI 36.6 to 45.4 points) | Not applicable | 615 (3 studies, 1 study is duplicated because it had two types of massage) | ⊕⊝⊝⊝ very low3,4 | Small, non‐significant effect size (SMD 0.02, 95% CI ‐0.15 to 0.18) |
| Function (higher scores mean more disability) ‐ Short‐term follow‐up Interference with daily activities (higher scores mean more disability) Follow‐up: 0 to 6 months | The mean function in the inactive control groups is 36.6 points (SD 17.7) Oswestry Disability Questionnaire1 | The mean function in the massage groups is 23.9 points (95% CI 18.0 to 29.7 points) | Not applicable | 725 (6 studies, 2 studies were duplicated) | ⊕⊕⊝⊝ low2 | Medium, statistically significant effect size SMD ‐0.72 (‐1.05 to ‐0.39) |
| Function (higher scores mean more disability) ‐ Long‐term follow‐up RDQ and ODI Follow‐up: 6 to 12 months | The mean function in the inactive control group is 36.6 points (SD 17.7) Oswestry Disability Questionnaire1 | The mean function in the massage group is 33.8 points (95%CI 30.9 to 36.8 points) | Not applicable | 615 (3 studies, 1 study is duplicated) | ⊕⊝⊝⊝ very low2,4 | Small, non‐significant effect size SMD ‐0.16 (‐0.32 to 0.01) |
| Adverse events Self‐reported | 4 per 1000 | 60 per 1000 (4 to 114) | See comment | 624 (4 studies, 1 study is duplicated) | ⊕⊝⊝⊝ very low2,4 | Small, non statistically significant difference (RD 0.06, 95% CI 0.00 to 0.11) |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio; ODI: Oswestry disability index; RDQ: Roland Disability Questionnaire; VAS: visual analog scale. | ||||||
| GRADE Working Group grades of evidence High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | ||||||
1Final scores. Poole 2007 is the most representative study of this meta‐analysis. 2Downgraded two levels because of risk of bias. The studies included in this meta‐analysis have high risks of selection, performance, attrition and measurement bias, and are unclear for reporting bias. 3Downgraded two levels because of risk of bias. The studies included in this meta‐analysis have unclear risk of selection bias and high risk of detection, performance and selective reporting bias. 4Downgraded one level because of imprecision. The CI includes the null hypothesis.
Summary of findings 2. Massage versus active controls for sub‐acute and chronic LBP.
| Massage versus active controls for sub‐acute and chronic LBP for LBP | ||||||
| Patient or population: patients with LBP Settings: Intervention: Massage versus active controls for sub‐acute and chronic LBP | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Massage versus active controls for sub‐acute and chronic LBP | |||||
| Pain intensity (higher scores mean more pain) ‐ Short‐term follow‐up Numerical pain rating scales (higher scores man more pain) Follow‐up: 0 to 6 months | The mean pain intensity in the active control group is 40.6 points (SD 26.7) VAS1 | The mean pain intensity in the massage group is 30.7 points (95%CI 24.0 to 37.1 points) | Not applicable | 964 (12 studies, 1 study is duplicated because it had two types of massage) | ⊕⊝⊝⊝ very low2,3 | Medium, statistically significant effect size (SMD ‐0.37, 95% CI ‐0.62 to ‐0.13) |
| Pain intensity (higher scores mean more pain) ‐ Long‐term follow‐up Back and Leg pain; VAS and Von Korff Pain Scale. Follow‐up: 6 to 12 months | The mean pain intensity in the active control group is 40.6 points (SD 26.7) VAS1 | The mean pain intensity in the massage group is 29.9 points (95%CI 19.2 to 40.3 points) | Not applicable | 757 (5 studies) | ⊕⊝⊝⊝ very low2,4,5 | Medium, statistically significant effect size SMD ‐0.4 (‐0.8 to ‐0.01) |
| Function (higher scores mean more disability) ‐ Short‐term follow‐up Interference with daily activities (higher scores mean more disability). Follow‐up: 0 to 6 months | The mean function in the active control group is 36.6 points (SD 17.7) Oswestery Disability Questionnaire1 | The mean function in the massage group is 32.4 points (95%CI 25.6 to 38.9 points) | Not applicable | 618 (6 studies) | ⊕⊝⊝⊝ very low2,6 | Small, non‐significant effect size SMD ‐0.24 (‐0.62 to 0.13) |
| Function (higher scores mean more disability) ‐ Long‐term follow‐up RMDQ and ODI. Follow‐up: 6 to 12 months | The mean function in the active control group is 36.6 points (SD 17.7) Oswestry Disability Questionnaire | The mean function in the massage group is 32.9 points (95%CI 26.0 to 39.6 points) | Not applicable | 616 (4 studies) | ⊕⊝⊝⊝ very low2,6,7 | Small, non‐significant effect size SMD ‐0.21 (‐0.6 to 0.17) |
| Adverse events Self‐reported | 29 per 1000 | 37 per 1000 (19 to 59) | See comment | 585 (5 studies) | ⊕⊝⊝⊝ very low2,6 | Small, non statistically significant difference (RD 0.01, 95% CI ‐0.01 to 0.03) |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio; ODI: Oswestry disability index; RMDQ: Roland Morris Disability Questionnaire; VAS: visual analog scale. | ||||||
| GRADE Working Group grades of evidence High quality: further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: we are very uncertain about the estimate. | ||||||
1Final scores. Poole 2007 was the most representative trial included in this meta‐analysis. 2Downgraded two levels because of risk of bias: The studies included in this meta‐analysis had high risk of selection, performance, detection and attrition bias. Unclear risk of reporting bias. 3Downgraded one level because of inconsistency. Although the I² statistic value was < 80%, we found that there was some underlying heterogeneity because 2 studies found the opposite results from this meta‐analysis (Lara‐Palomo 2013; Kumnerddee 2009). 4Downgraded one level because of inconsistency. The I² statistic value is 86%. 5Downgraded one level because of imprecision. The 95% CI includes a small effect. 6Downgraded one level becasue of imprecsision. The 95% CI includes "no effect". 7Downgraded one level because of inconsistency. The I² statistic value is 82%.
Background
Description of the condition
Low‐back pain (LBP) is a major health problem in modern society. The global point prevalence of LBP is estimated to be 12% (Hoy 2012). According to the 2010 Global Burden of Disease Study, it is estimated that LBP is among the top 10 diseases and injuries that account for the highest number of disability‐adjusted life years (DALYs) worldwide (Vos 2010). Although LBP is a benign and self‐limiting condition, many patients look for some type of therapy to relieve their symptoms and improve their function. For this reason, it is possible to list more than 50 potential therapies promising to relieve the pain, lessen the suffering and eliminate this problem (Haldeman 2008). However, there is sound evidence for only a minority of these therapies (Chou 2009). Most of the economic burden of LBP arises from the small number of people who develop chronic LBP (CLBP) because of the excessive use of diagnostic tests and therapeutic interventions, and inability to function (Dagenais 2008). Data from seven countries in Latin America show that the prevalence of CLBP is estimated between 4.2 and 10.1% of the population (Garcia 2014).
Description of the intervention
Therapeutical massage is defined as the manipulation of the soft tissue of whole body areas to bring about generalised improvements in health, such as relaxation or improved sleep, or specific physical benefits, such as relief of muscular aches and pains.(Vickers 1999) The use of massage for LBP is very popular. In Eastern cultures, massage is believed to have powerful analgesic effects. A systematic review of twenty‐two surveys across six countries (USA, UK, Canada, Australia, Singapore and South Korea) found that the 12‐month prevalence of visits to massage therapists by adults ranged from 0.4% to 20% and the median was 5.5%, while estimates for older adults were 1.5%‐16.2% (median 5.2%).(Harris 2014).
How the intervention might work
Soft‐tissue massage is thought to improve physiological and clinical outcomes by offering symptomatic relief of pain through physical and mental relaxation, and increasing the pain threshold through the release of endorphins (Ernst 1999). The gate‐control theory predicts that massaging a particular area stimulates large diameter nerve fibres. These fibres have an inhibitory input onto T‐cells (which are the first cells that project into the central nervous system within the spinal cord). T‐cell activity is depressed (whereas, conversely, small diameter nerve fibres (nociceptive fibres) have an excitatory input) and pain relief follows (Melzack 1996). Massage therapy may provide its benefits by shifting the autonomic nervous system from a state of sympathetic response to a state of parasympathetic response. However, support for this theory is not universal, and it has even been suggested that massage therapy may promote a sympathetic response of the autonomic nervous system (Moyer 2004). The mechanistic links between manipulation of body tissues and corresponding relief from a broad range of symptoms are not fully understood. Mechanistic studies are needed to delineate underlying biologic and psychological effects of massage and their relationship to outcomes.
Massage is recognized as a safe therapeutic modality, with few risks or adverse effects. However, there are contraindications, such as applying massage over an area with acute inflammation, skin infection, non‐consolidated fracture, burn area, deep vein thrombosis or over sites of active cancer tumour (Vickers 1999). Minor pain or discomfort was experienced by 13% of participants during or shortly after receiving massage (Cherkin 2001).
Massage has been investigated in the pain management area for its efficacy in relieving headaches (Jensen 1990), post‐exercise muscle pain (Weber 1994), cancer pain (Weinrich 1990) and mechanical neck pain (Gross 1999). These studies show little or no effect of massage in relieving these pain conditions. Moyer 2004 reported on a meta‐analysis of 37 randomized controlled trials (RCTs) (1802 participants) for many different health conditions. This meta‐analysis supports the general conclusion that massage therapy is effective. Thirty‐seven studies yielded a statistically significant overall effect as well as six specific effects out of nine that were examined. Significant results were found within the single‐dose and multiple‐dose categories, and for both physiological and psychological outcome variables.
Why it is important to do this review
In earlier versions of this Cochrane Review we concluded that massage was beneficial for CLBP (Furlan 2002; Furlan 2008). However, more recent trials have been published since Furlan 2008, Therefore it is important to update this Cochrane Review.
Objectives
To assess the effects of massage therapy for people with non‐specific LBP.
Methods
Criteria for considering studies for this review
Types of studies
We included RCTs as RCTs are the highest level of evidence to assess the effects of interventions. There were no language restrictions.
We excluded publications where we only had the abstract because there is evidence that most trials presented at conference never reach full publication, and those that are eventually published in full are systematically different from those never published in full (Scherer 2007). We listed these abstracts in the ongoing studies section.
Types of participants
We included adults (people older than 18 years) with non‐specific LBP. Non‐specific indicates that no specific cause is detectable, therefore we excluded studies when the population included LBP caused by infection, neoplasm, metastasis, osteoporosis, rheumatoid arthritis, fracture, inflammatory process or radicular syndrome.
LBP was classified as acute (< four weeks), sub‐acute (four to 12 weeks) or chronic (> 12 weeks).
We defined LBP as pain localized from the costal margin or 12th rib to the inferior gluteal fold.
Types of interventions
In this Cochrane Review we defined massage as soft‐tissue manipulation using hands or a mechanical device. Massage can be applied to any body part, to the lumbar region only or to the whole body. We used the taxonomy of massage treatments for musculoskeletal pain developed by Sherman 2006 to include studies in this review. The taxonomy was conceptualized as a three‐level classification system: goals of treatment, styles and techniques. Four categories described the principal goal of treatment: relaxation massage, clinical massage, movement re‐education and energy work. Each goal of treatment could be met using a number of different styles, with each style consisting of a number of specific techniques. A total of 36 distinct techniques were identified and described, many of which could be included in multiple styles (see Table 3). We excluded trials in which massage was not applied with any of the goals of treatment described above.
1. Taxonomy of massage practice (Sherman 2006).
| Treatment goal | Relaxation massage | Clinical massage | Movement re‐education | Energy work |
| Intention | Relax muscles, move body fluids, promote wellness | Accomplish specific goals such as releasing muscle spasms | Induce sense of freedom, ease and lightness in body | Hypothesized to free energy blockages |
| Commonly used styles (examples) | SM, spa massage, sports massage | Myofascial trigger points therapy, myofascial release, strain counterstrain | Proprioceptive, neuromuscular facilitation, strain counterstrain, trager | Acupressure, reiki, polarity, therapeutic touch, tuina |
| Commonly used techniques (examples) | Gliding, kneading, friction, holding, percussion, vibration | Direct pressure, skin rolling, resistive stretching, stretching manual, cross‐fibre‐friction | Contract‐relax, passive stretching, resistive stretching, rocking | Direction of energy, smoothing, direct pressure, holding, rocking, traction |
Abbreviations: SM: Swedish massage.
In physiotherapy, massage is considered an adjunct therapy or a complementary treatment to prepare the patient for exercise or other interventions; it is rarely the main treatment used. However, there are practitioners (e.g. massage therapists) that employ massage as the only intervention. In this Cochrane Review, we analyzed massage alone because it is difficult to reach definite conclusions when multiple treatments are involved.
Comparison groups
In this review update, we divided the comparison groups into two types: active controls and inactive controls. Other systematic reviews of massage have used this same approach and we used similar grouping for comparison groups. One review was massage for neck and shoulder pain (Kong 2013), and the other was massage for neck pain (Cheng 2014).
Inactive controls are interventions that are not expected to have an effect on the outcomes. They include sham therapy, no treatment, waiting list controls, or when all intervention arms received usual care including controls, and we can therefore say the control received no intervention beyond what the other arms received.
Active controls are interventions that are expected to have an effect on the outcomes: They include manipulation, mobilization, TENS, acupuncture, traction, relaxation, physical therapy, exercises or self‐care education. These comparison groups were combined because the participants randomized to the control group were told that they would receive another "study intervention". The participants in this comparison group were more active, in which they were actively engaged in the intervention; even in the relaxation therapies, the participants had to be actively engaged in these modalities.
Types of outcome measures
Primary outcomes
Primary outcomes were pain and back‐specific functional status. We divided the timing of the outcome measurements into two categories:
Short‐term: when the outcome assessment was taken ≤ six months after randomization.
Long‐term: when the outcome assessment was taken > six months after randomization. We also extracted data regarding adverse effects and complications related to massage.
Secondary outcomes
We only extracted secondary outcomes if there were no primary outcomes reported in the included studies, such as overall improvement, patient satisfaction, quality of life and work‐related status.
Search methods for identification of studies
Electronic searches
We searched the following databases:
Cochrane Central Register of Controlled Trials (CENTRAL; the Cochrane Library, Issue 6 of 12, June 2014) on 17 July 2014.
MEDLINE (OvidSP, 1946 to July Week 2 2014) on 17 July 2014.
MEDLINE In‐Process and Other Non‐Indexed Citations (OvidSP, 16 July 2014) on 17 July 2014.
EMBASE (OvidSP, 1980 to 2014 Week 28) on 17 July 2014.
Cumulative Index to Nursing and Allied Health Literature (CINAHL; EBSCO, 1981‐) on 17 July 2014.
Latin American and Caribbean Health Sciences Literature (LILACS, 1982‐) on 17 July 2014.
Index to Chiropractic Literature (ICL) on 21 July 2014.
Proquest Dissertation Abstracts on 17 July 2014.
PubMed (1946‐) on 7 August 2014.
For this review update we added the following databases: MEDLINE In‐Process and Other Non‐Indexed Citations, Index to Chiropractic Literature, LILACS, Proquest Dissertation Abstracts, and PubMed. We searched PubMed in August 2014 to capture studies published within the last year that may not be in MEDLINE; and we searched the other databases up to July 2014. Two databases from the 2008 review were not searched: Dissertation Abstracts from SilverPlatter is no longer available and we found that HealthSTAR from OvidSP does not add uniquely relevant content.
We have presented the strategies for each database in Appendix 1.
We used the search strategy recommended by the Cochrane Back and Neck (CBN) Review Group (Furlan 2009) to find RCTs for LBP. The CBN Trials Search Coordinator conducted and reviewed the literature searches. We merged the results using Reference Manager (RefMan 2010) and manually removed duplicates. We compared these results with the list of previously included and excluded studies from previous versions of this review (Furlan 2008), and removed duplicates.
We did not impose any language restrictions.
Searching other resources
We searched the reference lists of all included studies and other systematic reviews.
Data collection and analysis
Selection of studies
Two review authors (MG and AB) independently applied the inclusion criteria described above. When consensus was not reached we consulted a third review author (AF) to determine if the abstract or the full paper met the inclusion criteria.
Data extraction and management
Two review authors (AB and MG) independently extracted the data from each trial in Excel using a standardized form, and entered the data together in RevMan 2014. These review authors double‐checked data entry. When consensus could not be reached, they consulted a third review author (AF). We extracted the following data from each included trial in addition to the data for the 'Risk of bias' assessment: methods of patient recruitment, age of patients, country, ethnicity, work status, number of patients included in each arm, length of LBP episode, causes of LBP, previous surgery, types of interventions, number of sessions, types of outcomes measures, timing of outcome assessment, funding for the study, statistical analyses and the authors' conclusions about the effectiveness of the interventions.
Assessment of risk of bias in included studies
Two review authors (MG and AB) independently assessed the risk of bias of each included trial. In the case of disagreement, MG and AB tried to reach consensus and, if necessary, a third review author (AF) helped to resolve disagreements.
We assessed the risk of bias of the included trials using the criteria recommended in the method guidelines for systematic reviews in the CBN group (Furlan 2009) and the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), which are shown in Appendix 2. We scored each criterion as either "high", "low" or "unclear" risk. Five domains of bias were assessed in this Cochrane Review:
Selection bias: method of randomization, allocation concealment and similarity at baseline.
Performance bias: patient blinded, care provider blinded, co‐interventions and compliance.
Detection (or measurement) bias: outcome assessor blinded and timing of outcome assessment similar in all groups.
Attrition bias: drop‐out rate and intention‐to‐treat (ITT) analysis.
Reporting bias: selective outcome reporting.
There was also opportunity to identify any additional bias (other bias). We used the 'Risk of bias' assessment of the included trials for grading the quality of the evidence (see GRADE approach described below and additional information in Appendix 3).
Measures of treatment effect
We reported the results for continuous variables as weighted mean difference (WMD) when the outcome measures were identical, and standardized mean difference (SMD) when the outcome measures were different. We analysed the incidence of adverse events as dichotomous variables and reported and analyzed these as risk difference (RD) values.
Unit of analysis issues
Repeated measurements: when a trial measured the same outcome multiple times, we extracted the data from the outcome closer to three months for short‐term follow‐up, and one year for long‐term follow‐up.
Dealing with missing data
When trial authors performed data imputation, we used the data imputation as reported in the trial. We contacted trial authors to obtain information when there was missing data.
Assessment of heterogeneity
We used the random‐effects model for all meta‐analyses. This is recommended by the CBN Group Editorial Board because the assumptions underlying the random‐effects model are better suited to statistical combination of trials in this field.
Assessment of reporting biases
We analyzed the funnel plot to detect publication bias when there were at least 10 trials in a meta‐analysis. We used the method of independent visual inspection by two review authors (AF and MG). When there was disagreement, we consulted a third review author.
Data synthesis
We entered all quantitative results into RevMan 2014. Statistical pooling (meta‐analysis) was considered when there was homogeneity in terms of population (acute or subacute/chronic), comparison group (active or inactive), outcome (pain or function) and timing of follow‐up (short or long‐term). We rated the magnitude of the effect as small (effect sizes around 0.2), medium (effect sizes around 0.5) and large (effect sizes of 0.8 or higher).
The GRADE approach was used in order to provide the quality of the evidence. Justifications for downgrading the evidence can be referred to in Appendix 3. We only summarized the primary outcome measures in the 'Summary of findings' tables. As we included only RCTs in this Cochrane Review, the overall quality of the evidence for each outcome considered risk of bias, consistency of results, directness and precision (GRADE 2009; Higgins 2011),
Subgroup analysis and investigation of heterogeneity
We did not plan any subgroup or meta‐regression analyses.
Sensitivity analysis
We did not plan any sensitivity analysis.
Results
Description of studies
Results of the search
We have presented the flow of studies in the PRISMA chart in Figure 1.
1.

Study flow diagram.
In our previous review, Furlan 2008, we included 13 RCTs. For this review update we identified 12 additional trials for inclusion (Ajimsha 2014; Buttagat 2011; Cherkin 2011; Eghbali 2012; Kamali 2014; Kumnerddee 2009; Lara‐Palomo 2013; Little 2008; Quinn 2008; Sritoomma 2014; Yoon 2012; Zheng 2012).
Included studies
In total, we included 25 trials (3096 participants). Five studies were conducted in the USA (818 participants; Cherkin 2001; Cherkin 2011; Field 2007; Geisser 2005; Hernandez‐Reif 2001 ), five in Thailand (441 participants; Buttagat 2011; Chatchawan 2005; Kumnerddee 2009; Mackawan 2007; Sritoomma 2014), three in the UK (837 participants; Little 2008; Poole 2007; Quinn 2008), two in Taiwan (275 participants; Hsieh 2004; Hsieh 2006), two in Iran (110 participants; Eghbali 2012; Kamali 2014), one in Germany (190 participants; Franke 2000), one in Canada (104 participants; Preyde 2000), one in India (80 participants; Ajimsha 2014), one in China (64 participants; Zheng 2012), one in Spain (62 participants; Lara‐Palomo 2013), one in Hong Kong (61 participants; Yip 2004), one in Belgium (60 participants; Farasyn 2006) and one in Korea (24 participants; Yoon 2012). All trials were published in English except Franke 2000, which was published in German.
The population included in the trials was similar regarding the diagnosis, which was non‐specific LBP, but differed with respect to the duration of pain, previous treatments and distributions of age. One trial included participants with acute LBP (Yip 2004), six trials included patients with sub‐acute and chronic LBP (Farasyn 2006; Hsieh 2004; Hsieh 2006; Kumnerddee 2009; Preyde 2000; Yoon 2012) and the remaining trials were limited to patients with chronic pain (Ajimsha 2014; Buttagat 2011; Chatchawan 2005; Cherkin 2001; Cherkin 2011; Eghbali 2012, Field 2007; Franke 2000; Geisser 2005; Hernandez‐Reif 2001; Kamali 2014; Lara‐Palomo 2013; Little 2008; Mackawan 2007; Poole 2007; Quinn 2008; Sritoomma 2014; Zheng 2012).
The types of massage technique, duration and frequency of treatments varied among the included trials. In three studies the massage was applied with a mechanical device (Farasyn 2006; Franke 2000; Yoon 2012) while in the remaining studies it was done with hands. Three studies used a specific oil (Field 2007; Sritoomma 2014; Yip 2004). In four studies distinct techniques of massage were compared (Chatchawan 2005; Cherkin 2011; Franke 2000; Sritoomma 2014).
With respect to the outcome measures, pain intensity was used in most included studies, except Cherkin 2001 and Cherkin 2011 which assessed symptom bothersomeness. Seven studies (Buttagat 2011; Cherkin 2011; Hernandez‐Reif 2001; Hsieh 2004; Kumnerddee 2009; Preyde 2000; Sritoomma 2014) also included other dimensions of pain, i.e. pain characteristics/quality/perception of pain symptoms. Sixteen studies assessed function/disability (Ajimsha 2014; Chatchawan 2005; Cherkin 2001; Cherkin 2011; Farasyn 2006; Franke 2000; Geisser 2005; Hsieh 2006; Kamali 2014; Lara‐Palomo 2013; Little 2008; Preyde 2000; Poole 2007; Sritoomma 2014; Yip 2004; Yoon 2012).
We have provided details about each included trial in the Characteristics of included studies table.
Excluded studies
Many controlled studies studied massage in combination with other therapies (Ferrell 1997; Ginsberg 1987; Kankaanpää 1999; Koes 1992; Konrad 1992; Lindström 1970; Maniche 1991; Melzack 1980; Werners 1999). Although it is very common for massage to be used as an adjunct treatment for other physical treatments, we excluded these studies from this review because we could not extract the effect of massage separately. We have provided details about these studies and the reasons for exclusion in the Characteristics of excluded studies table.
Risk of bias in included studies
There was no suggestion of publication bias (Figure 2). A summary of the risk of bias for each article is shown in Figure 3.
2.
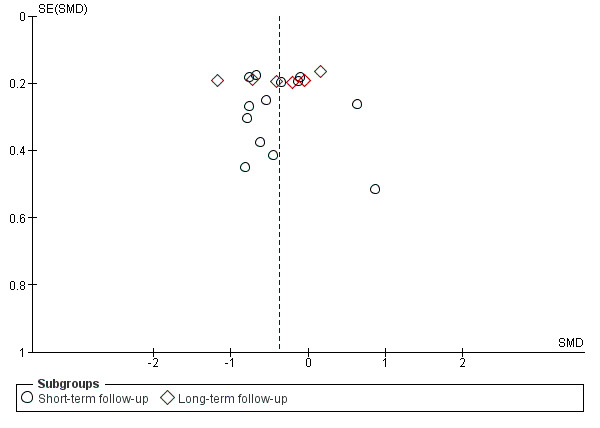
Funnel plot of comparison: 3 Massage versus active therapies for sub‐acute and chronic LBP, outcome: 3.1 Pain intensity (higher scores mean more pain).
3.
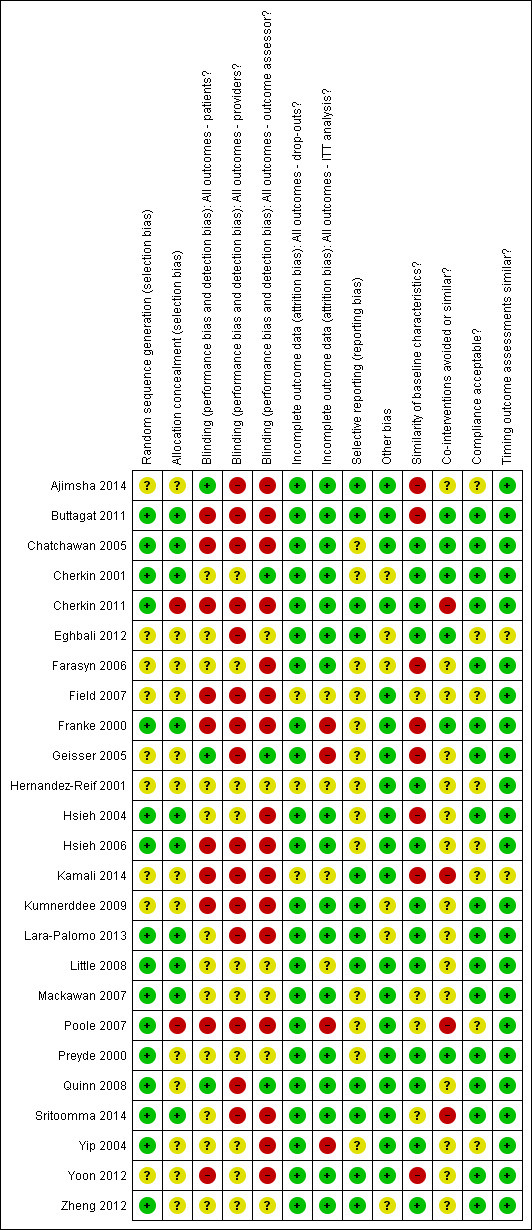
Summary of risks of bias
Allocation
Ten included trials were at low risk of bias (Buttagat 2011; Chatchawan 2005; Cherkin 2001; Franke 2000; Hsieh 2004; Hsieh 2006; Lara‐Palomo 2013; Little 2008; Mackawan 2007; Sritoomma 2014). Strict strategies to reach proper allocation concealment included the support from a statistician to generate the random numbers followed by another person to placed the numbers in sealed opaque numbered envelopes; both of these participants were not involved in the trial (Sritoomma 2014).
Blinding
The main risk of bias factors in the included studies were performance (blinding of participants/health care providers and co‐interventions avoided or similar) and detection bias (blinding of outcome assessors). Four studies attempted to blind the patients to the assigned intervention (Ajimsha 2014; Eghbali 2012; Geisser 2005; Quinn 2008). The risk of bias was considered low when the trial clearly described the strategy to blind them. In one of these studies, Geisser 2005, the patients were randomized to four groups and they assessed the success of patient's blinding by asking the question: "I believe I received an actual treatment from the therapist" (1 = completely disagree and 7 = completely agree). There was no significant difference between the groups. Ten studies attempted to blind the outcome assessors (Ajimsha 2014; Cherkin 2001; Cherkin 2011; Eghbali 2012, Geisser 2005; Kamali 2014; Kumnerddee 2009; Lara‐Palomo 2013; Mackawan 2007; Preyde 2000). However, when the outcome is a subjective measure, such as pain, and the patient is not blinded to the intervention, the attempt of blinding of outcome assessor is irrelevant.
Incomplete outcome data
The risk of attrition bias was judged low in 22 trials and only three did not explicitly report how many patients finished the study, therefore it was judged unclear (Field 2007; Hernandez‐Reif 2001; Kamali 2014).
Eleven of the 12 new trials included in this review update were at low risk of attrition bias (Ajimsha 2014; Buttagat 2011; Cherkin 2011; Eghbali 2012; Kumnerddee 2009; Lara‐Palomo 2013; Little 2008; Quinn 2008; Sritoomma 2014; Yoon 2012; Zheng 2012).
Selective reporting
The risk of reporting bias was low in 12 studies (Ajimsha 2014; Buttagat 2011; Cherkin 2011; Eghbali 2012; Kamali 2014; Kumnerddee 2009; Lara‐Palomo 2013; Little 2008; Quinn 2008; Sritoomma 2014; Yoon 2012; Zheng 2012). This item was the most difficult to judge as many included trials did not publish a protocol. We obtained most information from the methods section of the published studies.
Other potential sources of bias
Seven included trials did not provide funding details (Farasyn 2006; Franke 2000; Hsieh 2004; Hsieh 2006; Quinn 2008; Sritoomma 2014; Zheng 2012). Sixteen studies were funded by not‐for‐profit organizations such as a research grant from the University or government (Ajimsha 2014; Buttagat 2011; Chatchawan 2005; Cherkin 2001; Cherkin 2011; Eghbali 2012; Field 2007; Geisser 2005; Hernandez‐Reif 2001; Kamali 2014; Kumnerddee 2009; Little 2008; Mackawan 2007; Poole 2007; Yip 2004; Yoon 2012). One trial mentioned that no funding was received from any source (Lara‐Palomo 2013). One trial, Preyde 2000, was funded by an organization with potential conflict of interest: the College of Massage Therapists of Ontario.
Effects of interventions
The studies compared massage therapy to various control treatments: eight studies employed an inactive control group (Ajimsha 2014; Buttagat 2011; Cherkin 2011; Farasyn 2006; Geisser 2005; Little 2008;Poole 2007; Preyde 2000). Thirteen studies compared massage to various active controls (Cherkin 2001; Field 2007; Hernandez‐Reif 2001; Hsieh 2004; Hsieh 2006; Kumnerddee 2009; Lara‐Palomo 2013;Little 2008; Mackawan 2007; Poole 2007; Preyde 2000; Yoon 2012; Zheng 2012). We have summarized the comparisons in Table 4 and described them below:
2. Intervention effects.
| Intervention | Acute LBP | Sub‐acute and chronic LBP | |||
| Pain | Function | Pain | Function | ||
| Massage (M) versus inactive (I) controls | Short‐term follow‐up | M better than I (SMD ‐1.24, 95% CI ‐1.85 to ‐0.64; 51 participants, 1 trial ) "Very low" |
M the same as I (SMD ‐0.50, 95% CI ‐1.06 to 0.06; 51 participants, 1 trial ) "Very low" |
M better than I (SMD ‐0.75, 95% CI ‐0.90 to ‐0.60; 761 participants, 9 trials; I² statistic = 0%) "Low" |
M better than I (SMD ‐0.72, 95% CI ‐1.05 to ‐0.39; 725 participants, 8 trials; I² statistic = 74%) "Low" |
| Long‐term follow‐up | No evidence | No evidence | M the same as I (SMD 0.02, 95% CI ‐0.15 to 0.18; 615 participants, 4 trials; I² statistic = 0%) "Very low" |
M the same as I (SMD ‐0.16, 95% CI ‐0.32 to 0.01; 615 participants. 4 trials; I² statistic = 0%) "Very low" |
|
| Massage (M) versus active (A) controls | Short‐term follow‐up | No evidence | No evidence | M better than A (SMD ‐0.37, 95% CI ‐0.62 to ‐0.13; 964 participants. 13 trials; I² statistic = 68%) "Very low" |
M the same as A (SMD ‐0.24, 95% CI ‐0.62 to 0.13; 618 participants, 7 trials; I² statistic = 79%) "Very low" |
| Long‐term follow‐up | No evidence | No evidence | M better than A (SMD ‐0.40, 95% CI ‐0.80 to ‐0.01; 757 participants = 757, 6 trials; I² statistic = 86%) "Very low" |
M the same as A (SMD ‐0.21, 95% CI ‐0.60 to 0.17; 616 participants = 616, 5 trials; I² statistic = 82%) "Very low" |
|
Abbreviations: LBP: low‐back pain; M: massage; A: active controls; I: inactive controls.
1. Massage versus inactive controls for acute LBP
Based on the current evidence it is unclear whether or not massage is more effective than inactive controls for pain at short‐term follow‐up (SMD ‐1.24, 95% CI ‐1.85 to ‐0.64; 51 participants, one trial; very low quality evidence,Analysis 1.1), and that massage is not better than inactive controls for function on short‐term follow‐up (SMD ‐0.50, 95% CI ‐1.06 to 0.06; participants = 51; studies = 1; very low quality evidence,Analysis 1.2).
1.1. Analysis.
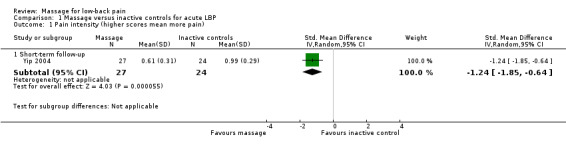
Comparison 1 Massage versus inactive controls for acute LBP, Outcome 1 Pain intensity (higher scores mean more pain).
1.2. Analysis.
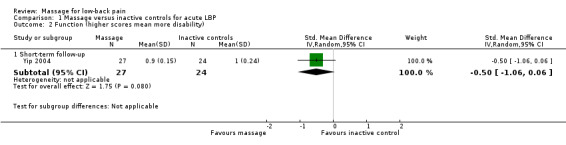
Comparison 1 Massage versus inactive controls for acute LBP, Outcome 2 Function (higher scores mean more disability).
There is no evidence for outcomes in the long‐term for this comparison.
2. Massage versus inactive controls for sub‐acute and chronic LBP
We have presented the meta‐analysis for pain in Figure 4. The summary of the results are shown in Table 1.
4.
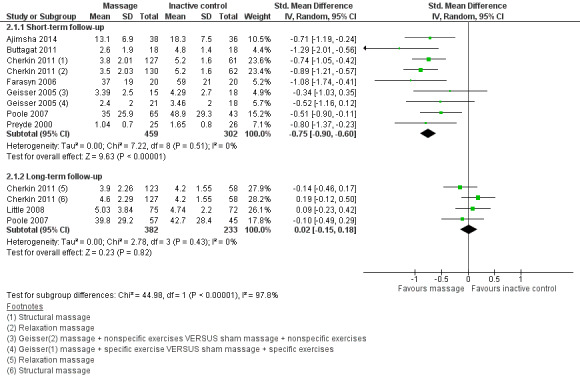
Forest plot of comparison: 2 Massage versus inactive controls for sub‐acute and chronic LBP, outcome: 2.1 Pain intensity (higher scores mean more pain).
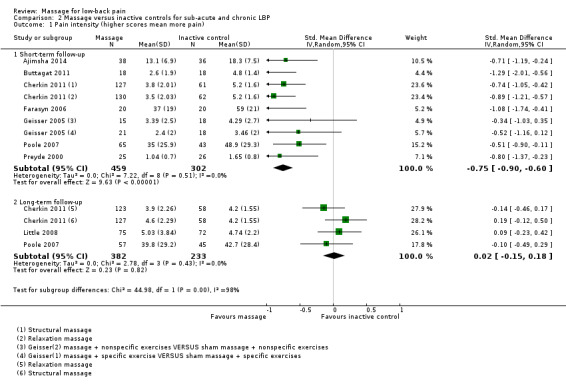
Massage may be more effective than inactive controls for pain (SMD ‐0.75, 95% CI ‐0.90 to ‐0.60; 761 participants, seven trials; I² statistic = 0%; low quality evidence, Analysis 2.1) and function (SMD ‐0.72, 95% CI ‐1.05 to ‐0.39; 725 participants, six trials; I² statistic = 74%; low quality evidence, Analysis 2.2) in the short‐term follow‐up.
2.1. Analysis.
Comparison 2 Massage versus inactive controls for sub‐acute and chronic LBP, Outcome 1 Pain intensity (higher scores mean more pain).
2.2. Analysis.
Comparison 2 Massage versus inactive controls for sub‐acute and chronic LBP, Outcome 2 Function (higher scores mean more disability).
Based on the current evidence it is unclear whether or not massage is better than inactive controls for pain (SMD 0.02, 95% CI ‐0.15 to 0.18; 615 participants, three trials; I² statistic = 0%; very low quality evidence, Analysis 2.1) and function (SMD ‐0.16, 95% CI ‐0.32 to 0.01; 615 participants, three trials; I² statistic = 0%; very low quality evidence, Analysis 2.2) in the long‐term follow‐up.
3. Massage versus active controls for acute LBP
There are no included trials for this comparison.
4. Massage versus active controls for sub‐acute and chronic LBP
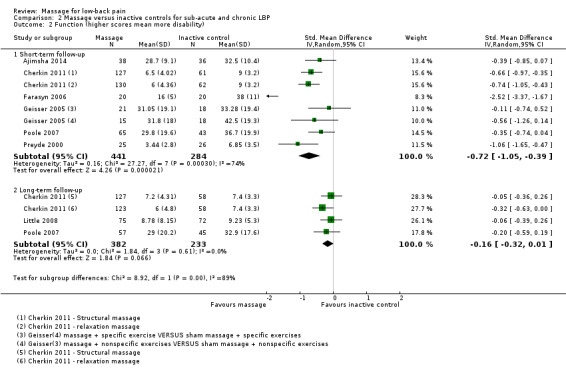
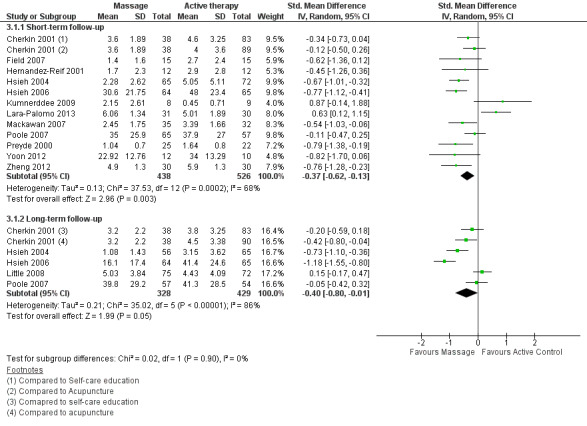
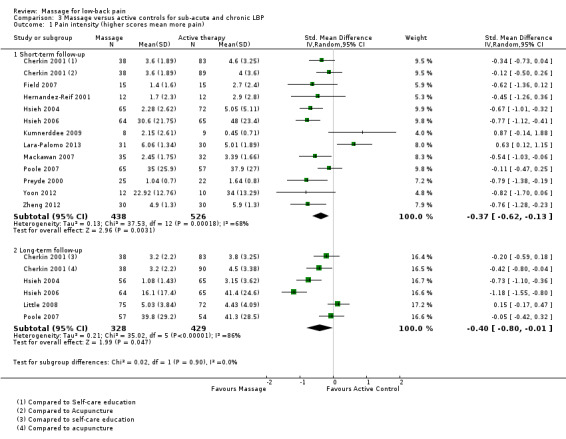
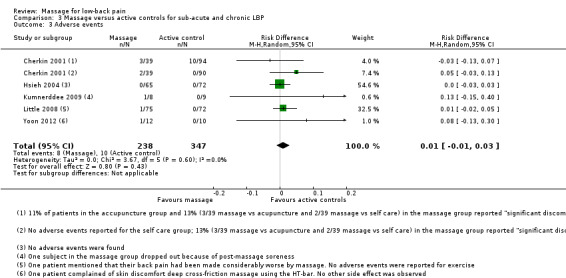
We have presented the meta‐analysis for pain in Figure 5 and the summary of the results in Table 2.
5.
Forest plot of comparison: 3 Massage versus active controls for sub‐acute and chronic LBP, outcome: 3.1 Pain intensity (higher scores mean more pain).
Based on the current evidence, it is unclear whether or not massage is more effective than active controls for pain (SMD ‐0.37, 95% CI ‐0.62 to ‐0.13; 964 participants, twelve trials; I² statistic = 68%; very low quality evidence, Analysis 3.1) in the short‐term follow‐up and for pain (SMD ‐0.40, 95% CI ‐0.80 to ‐0.01; 757 participants, five trials; I² statistic = 86%; very low quality evidence, Analysis 3.1) in the long‐term.
3.1. Analysis.
Comparison 3 Massage versus active controls for sub‐acute and chronic LBP, Outcome 1 Pain intensity (higher scores mean more pain).
Based on the current evidence, it is unclear whether or not massage is better than active controls for function (SMD ‐0.24, 95% CI ‐0.62 to 0.13; 618 participants, six trials; I² statistic = 79%; very low quality evidence, Analysis 3.2) in the short‐term follow‐up and for function (SMD ‐0.21, 95% CI ‐0.60 to 0.17; 616 participants, four trials; I² statistic = 82%; very low quality evidence, Analysis 3.2) in the long‐term follow‐up.
3.2. Analysis.
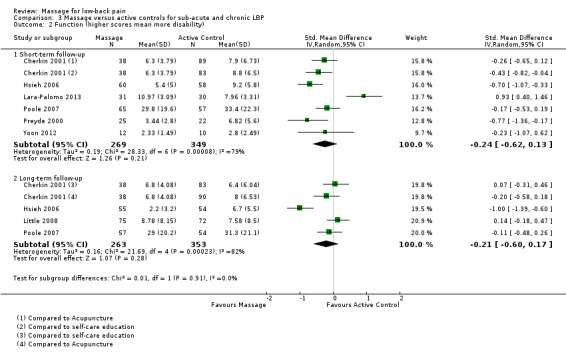
Comparison 3 Massage versus active controls for sub‐acute and chronic LBP, Outcome 2 Function (higher scores mean more disability).
5. Studies excluded from meta‐analyses
We excluded six trials in the meta‐analyses: four compared two massage techniques (Chatchawan 2005; Eghbali 2012; Franke 2000; Sritoomma 2014), one did not report precisely the amount of patients in each group (Kamali 2014) and one reported the median and interquartile values but not mean and standard deviation (SD) values (Quinn 2008). Two studies at low risk of bias compared Thai massage versus classic (Swedish) massage to measure their effects on pain and function in the short term, yielding different results: one trial, Chatchawan 2005, showed that both techniques had similar effects, but the other, Sritoomma 2014, reported better results with the Swedish massage (SM). One trial, Eghbali 2012, reported a higher reduction in pain after six weeks of reflexology than massage applied to the feet and lower back. Franke 2000 reported that acupuncture massage is better than SM for pain and function immediately after the treatment.
Adverse events
Fourteen studies did not report whether or not adverse events were measured (Buttagat 2011; Eghbali 2012; Farasyn 2006; Field 2007; Franke 2000; Geisser 2005; Hernandez‐Reif 2001; Hsieh 2006; Kamali 2014; Lara‐Palomo 2013; Mackawan 2007; Poole 2007; Preyde 2000; Zheng 2012).
There is no report of adverse events in the trial of massage for acute low‐back pain (Analysis 1.3), Based on the current evidence, it is unclear whether or not there is any difference in the incidence of adverse events between massage and inactive controls (RD 0.06, 95% CI 0.00 to 0.11; 624 participants, four trials; I² statistic = 73%; Analysis 2.3), or between massage and active controls (RD 0.01, 95% CI ‐0.01 to 0.03; 585 participants, five trials; I² statistic = 0%; Analysis 3.3).
1.3. Analysis.
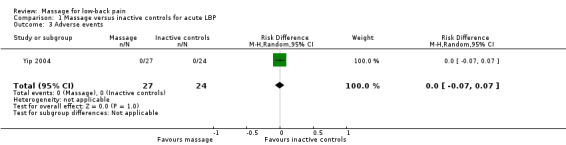
Comparison 1 Massage versus inactive controls for acute LBP, Outcome 3 Adverse events.
2.3. Analysis.
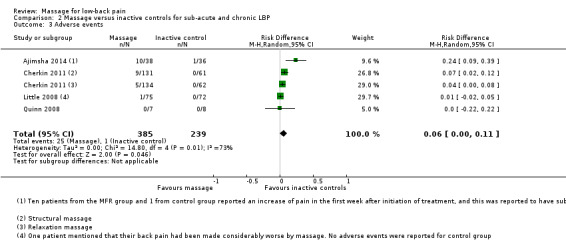
Comparison 2 Massage versus inactive controls for sub‐acute and chronic LBP, Outcome 3 Adverse events.
3.3. Analysis.
Comparison 3 Massage versus active controls for sub‐acute and chronic LBP, Outcome 3 Adverse events.
Increased pain was the most common adverse event in the patients randomized to the massage group and it was reported in 25% of patients in Ajimsha 2014, 13% in Cherkin 2001, 7% in Cherkin 2011, and in one patient in Little 2008. Allergic reaction to the massage oil (rash and pimples) occurred in 5.5% of the patients randomized to the SM in Chatchawan 2005. In Kumnerddee 2009 one patient reported intense post treatment soreness, and in Yoon 2012 there was one patient who reported skin discomfort. One patient reported nausea, shortness of breath and chest pain but this was not considered as a side effect of structural massage by the authors of the trial (Cherkin 2011). Four studies found that no adverse events occurred in the study population, either in the massage or control groups (Hsieh 2004; Quinn 2008; Sritoomma 2014; Yip 2004).
Discussion
Summary of main results
We included 12 new RCTs of massage for LBP in this Cochrane Review update. In contrast to our previous review (which was more postive), the current review shows that we have very little confidence that massage is an effective treatment for LBP. The results are conflicting for the long‐term follow‐up (massage versus inactive controls) and for the outcome of function (massage versus active controls), with some comparisons showing that massage is better than the control groups, and others showing no significant differences.
Not all the included trials showed that massage was better than the other treatment: one trial reported that acupuncture was better than Thai massage in military personnel (Kumnerddee 2009); another trial showed that acupuncture had similar effects for the relief of pain than SM in the short term (Cherkin 2001); and one trial, Lara‐Palomo 2013, reported better results with interferential current electro‐massage when compared with superficial massage for the relief of pain and function in the short term.
Even though reflexology is a massage technique that is not applied directly to the back, we included three studies in this Cochrane Review that studied reflexology. It is considered a manual manipulation of soft body tissues (Sherman 2006). One trial reported better results with reflexology than with sham therapy (Quinn 2008); one trial, Eghbali 2012, reported better results with reflexology than massage to the feet and lower back; and one trial reported better results with reflexology than usual care, but no differences when compared to relaxation (Poole 2007).
Overall completeness and applicability of evidence
We did not find any large effect size. The magnitude of the effect was small to medium in all meta‐analyses of continuous outcomes. All of the meta‐analyses of continuous outcomes had to be performed using SMD values because the included trials used different measurement instruments for the outcomes of interest (pain and function). The disadvantage of using SMD values is that clinicians and patients are unlikely to relate to this way of presenting results. (Guyatt 2013). Therefore, in the 'Summary of findings' tables we used a transformation to a common, well‐known measurement to report the results in a meaningful way.
Only 11 trials measured adverse events. The remaining trials did not mention whether or not adverse events were measured. There were no serious adverse events in these trials, and the most common adverse event was increased pain after the massage sessions.
Fourteen trials employed statistical adjustments to control the type I error (Buttagat 2011; Chatchawan 2005; Cherkin 2001; Cherkin 2011; Franke 2000; Hernandez‐Reif 2001; Hsieh 2004; Hsieh 2006; Lara‐Palomo 2013; Little 2008; Poole 2007; Preyde 2000; Sritoomma 2014; Yip 2004). Not all studies considered sample size calculations based on the Minimal Clinically Important Difference (MCID) either for pain or function to yield more clinically meaningful results; three out of the 14 trials did not consider a MCID for the sample size (Buttagat 2011; Hernandez‐Reif 2001; Sritoomma 2014). Moreover, the cut‐off point is still debatable when considering the methods to operationalize or quantify the MCID (King 2011). A MCID of 19 out of 100 points in the VAS and 10 points in the Oswestry is proposed; this cut‐off point was obtained by the standard error of measurement and by global transition questions to subtract the mean score of "unchanged" from "better" (Hägg 2003). A rationale to decide the MCID should be carried out a priori for more meaningful clinical estimates, otherwise, statistical differences could be obtained but not necessarily clinically important.
Quality of the evidence
This updated review is also different from previous versions in relation to the quality of the evidence. The current approach yielded "low" to "very low" quality evidence, which differs from the previous version of this review, (Furlan 2008), where the quality of the evidence was judged "moderate" for most comparisons. The explanation for these changes could be: first, we grouped more studies in the same comparisons, therefore increasing the types of biases that were introduced in each comparison; and second, the definitions of imprecision and inconsistency were stricter in the current than in the previous review.
In this review update we found high risk of selection, performance, attrition and measurement bias, suggesting that blinding patients, health care providers and outcomes were the most challenging methodological steps in clinical trials of massage. One trial, Geisser 2005, used a questionnaire to measure the success of patient blinding, so this strategy seemed to help in reducing the bias when patients themselves assess the outcomes of pain and function. On the other hand, the methods for allocation concealment were unclearly reported in half of the trials. It has been suggested that small trials with inadequate allocation concealment may exaggerate the effect of the interventions when they were compared to larger studies (Kjaergard 2001).
Potential biases in the review process
In this review update we grouped the comparison groups to yield more meaningful comparisons. Massage was compared to active and inactive controls. Massage is not a standardized treatment and many variables may affect its potential effect over painful conditions, such as the massage technique, the duration, frequency and number of treatment sessions, the intensity of pressure, the location over the body, the experience of the therapist, the level of stress, heterogeneity of participants and confounding variables, such as co‐interventions or emotional effect of counselling from the therapist. One limitation of this meta‐analysis is the relative lack of studies for each technique of massage; amid a large number of variables involved in the massage techniques and small samples (Hernandez‐Reif 2001; Kumnerddee 2009; Quinn 2008; Yoon 2012), some associations may be obtained merely by chance (type I error). As randomization might not be enough for balancing groups in their baseline conditions, risk stratification (Wagner 2009) or multivariable analysis (Wahlgren 2008) have been proposed to overcome this potential pitfall.
Agreements and disagreements with other studies or reviews
A recent non‐Cochrane review reviewed the effects of massage for many pain conditions including shoulder pain, fibromyalgia and back pain (Bervoets 2015). This review included adults with common musculoskeletal disorders and compared massage versus no treatment (wait list control, sham, rest or usual care) and massage versus other active treatments (exercise therapy, joint manipulation, relaxation therapy). This review included eight RCTs of patients with LBP: six out of the 25 studies that were included in this Cochrane Review; the other two studies were excluded from this Cochrane Review because we considered that the massage technique was not properly delivered. This could also be explained by a different search strategy and differences in inclusion criteria. The eight studies comprised short and long term follow‐up of either pain and function of massage compared to active or inactive therapies. Bervoets 2015 pooled two studies (one included and one excluded from our review), and found that massage was ineffective for LBP.
We published a systematic review of complementary and alternative medicine therapies for back and neck pain (Furlan 2012). This review included 10 trials of massage for LBP. In the comparisons of massage versus inactive treatments, massage had significantly better (effect in reducing) pain intensity and disability for acute/subacute non‐specific LBP, but in subjects with non‐specific CLBP there was no significant difference from no treatment or placebo in pain intensity or disability. When compared to active treatments, massage was significantly better in reducing pain compared to relaxation or physical therapy for subjects with non‐specific CLBP, but there was no significant difference between massage and usual care ‐consisting of advice and exercise‐ for people with non‐specific CLBP.
Authors' conclusions
Implications for practice.
We have very little confidence that massage is an effective treatment for LBP. For acute LBP, massage improved pain but not function when compared to inactive controls in the short‐term follow‐up. For sub‐acute and chronic LBP, massage improved pain and function outcomes in the short‐term but not in the long‐term follow‐up when it was compared to inactive controls. Compared with active controls, massage improved pain in the short and long‐term follow‐ups, but it did not improve function at any follow‐up. There were only minor adverse effects with massage.
The benefits of massage for patients with acute, sub‐acute and chronic non‐specific LBP were found mostly in the short‐term follow‐up period (up to six months after randomization) for pain outcomes. The inclusion of new studies in this Cochrane Review update allowed for a larger population and amount of studies. It objectively revealed heterogeneity and low quality of the evidence, suggesting the need for meta‐analysis of larger and better studies with more specific populations, interventions, co‐interventions and outcome measures.
Implications for research.
As most outcomes in LBP are subjective measures, the ideal control group is one that ensures that treatments are equally credible and acceptable to patients to minimize placebo effects and high dropout rates (Haraldsson 2006). There are numerous techniques of massage therapy, and each one needs to be evaluated for effectiveness and cost‐effectiveness. There are also different settings (private practice, hospital, primary care, pain clinics) and populations (acute or chronic pain, presence of other aggravating factors, different countries with different cultures) that need to be assessed separately. Future trials may also consider whether the benefits of massage can be increased if the therapist has many years of experience or is a licensed therapist.
Trials should examine the role of session length by including two (or more) levels of this variable, and the experience of the therapist by employing various people with different experience and training. Trial authors should discuss the clinical relevance of the results and include long‐term follow‐up. Trial authors are encouraged to follow the CONSORT statement for reporting their trials (Moher 2001) and use the standard outcomes for trials of LBP as described by Deyo 1998, in order to provide homogenous information for future systematic reviews and meta‐analyses. When presenting the results, researchers are encouraged to show the baseline characteristics using point estimates (mean, median) with SDs (for continuous variables), and the number of patients in each category (for categorical variables) and for every follow‐up measure.
Studies could consider treatment‐based subgroups according to prognostic factors (risk stratification) in order to obtain more homogeneous categories of patients; subsequently, it might yield much larger treatment effects for selective groups of patients with LBP, instead of inconsistent estimates due to heterogeneous populations. Kamper 2010 outlined a wide spectrum of subgroup approaches, including pathoanatomy, psychosocial characteristics and patterns of signs and symptoms and a rationale process to postulate the a priori candidate factors, a hypothesis verification and replication to confirm the estimates derived from subgroup‐factors analysis.
What's new
| Date | Event | Description |
|---|---|---|
| 25 August 2015 | New citation required and conclusions have changed | We included 12 new trials in this review update. In this review update we grouped the comparison groups to yield more meaningful comparisons. Massage was compared to active and inactive controls. More sources of bias were identified, lowering the quality of the evidence. |
| 17 July 2014 | New search has been performed | We updated the literature search and revised the search strategies. There were no language restrictions. We included MEDLINE In‐Process & Other Non‐Indexed Citations, Index to Chiropractic Literature, Proquest Dissertation Abstracts, LILACS, and PubMed as new databases. Comparison groups have been combined into active and inactive controls. |
| 2 December 2009 | New search has been performed | The literature search was updated. We identified eight additional trials: we included two (Little 2008; Quinn 2008), and excluded six (Buerger 1980; Li 2006; Rasmussen‐Barr 2003; Wu 2004; Zhang 2004). The conclusions did not change. |
| 11 July 2008 | Amended | We converted to a new review format. |
| 31 May 2008 | New search has been performed | We updated the literature search. |
History
Protocol first published: Issue 1, 2000 Review first published: Issue 4, 2000
| Date | Event | Description |
|---|---|---|
| 31 January 2002 | New citation required and conclusions have changed | This first update included four recent trials that were published since the original review. The conclusions changed in face of the new evidence. |
| 31 January 2002 | New search has been performed | literature search updated |
Acknowledgements
We thank the CBN Editors for their excellent comments and suggestions, the CBN managing editor Claire Munhall for proofreading and making excellent suggestions to improve the manuscript, and the CBN Group Trials Search Coordinators Rachel Couban and Shireen Harbin.
Joanna Liu from the CBN gave her support with the search and translation of Chinese articles and help us to extract data to determine the inclusion criteria when necessary, for which we are grateful. We are grateful to Dr. Sergio Terreri for his help in translating and extracting data from the German paper (Franke 2000). Also we thank Dr. Annegret Franke (author of one included trial) for double checking the data extracted from her paper and for providing further information about the trial. We acknowledge Vivian Welch, Jean Wong, Lucie Brosseau and Trish Dryden, co‐authors of previous versions of this Cochrane Review, for their participation.
Appendices
Appendix 1. Electronic search strategies
MEDLINE
Last searched July 17, 2014. We revised the search strategy 2013.
randomized controlled trial.pt.
controlled clinical trial.pt.
randomi#ed.ti,ab.
placebo.ti,ab.
randomly.ti,ab.
controlled.ti,ab.
prospective.ti,ab.
trial.ti,ab.
groups.ti,ab.
or/1‐9
(animals not (humans and animals)).sh.
10 not 11
dorsalgia.ti,ab.
exp Back Pain/
backache.ti,ab.
exp Low Back Pain/
(lumbar adj pain).ti,ab.
coccyx.ti,ab.
coccydynia.ti,ab.
sciatica.ti,ab.
sciatic neuropathy/
spondylosis.ti,ab.
lumbago.ti,ab.
back disorder$.ti,ab.
or/13‐24
exp Massage/
exp Therapeutic Touch/
exp Reflexotherapy/
myotherapy.mp.
rolfing.mp.
shiatsu.mp.
exp Acupressure/
reflexology.mp.
(polarity adj therapy).mp.
(myofascial adj release).mp.
(craniosacral adj therapy).mp.
reiki.mp.
(trager adj psychophysical).mp.
(hakomi adj method).mp.
(jin adj shin).mp.
(neuromuscular adj therapy).mp.
(pfrimmer adj25 therapy).mp.
(alexander adj technique).mp.
(feldenkrais adj method).mp.
or/26‐44
massage.mp.
exp Heart Massage/
46 not 47
45 or 48
12 and 25 and 49
limit 50 to yr=2013‐2014
limit 50 to ed=20130601‐20140717
53 51 or 52
2008 search strategy
Clinical Trial.pt.
randomized.ab,ti.
placebo.ab,ti.
dt.fs.
randomly.ab,ti.
trial.ab,ti.
groups.ab,ti.
or/1‐7
Animals/
Humans/
9 not (9 and 10)
8 not 11
dorsalgia.ti,ab.
exp Back Pain/
backache.ti,ab.
(lumbar adj pain).ti,ab.
coccyx.ti,ab.
coccydynia.ti,ab.
sciatica.ti,ab.
sciatica/
spondylosis.ti,ab.
lumbago.ti,ab.
exp low back pain/
or/13‐23
exp Massage/
exp Therapeutic Touch/
exp Reflexotherapy/
myotherapy.mp.
rolfing.mp.
shiatsu.mp.
exp Acupressure/
reflexology.mp.
(polarity adj therapy).
(myofascial adj release).mp.
(craniosacral adj therapy).mp.
reiki.mp.
(trager adj psychophysical).mp
(hakomi adj method).mp.
(jin adj shin).mp.
(neuromuscular adj therapy).mp
(pfrimmer adj25 therapy).mp.
(alexander adj technique).mp.
(feldenkrais adj method).mp
or/25‐43
12 and 24 and 44
limit 45 to yr="2007 ‐ 2008"
MEDLINE In‐Process & Other Non‐Indexed Citations
Searched July 17, 2014
random$.ti,ab.
placebo.ti,ab.
controlled.ti,ab.
prospective.ti,ab.
trial.ti,ab.
groups.ti,ab.
or/1‐6
dorsalgia.ti,ab.
back pain.ti,ab.
backache.ti,ab.
(lumbar adj pain).ti,ab.
coccyx.ti,ab.
coccydynia.ti,ab.
sciatica.ti,ab.
spondylosis.ti,ab.
lumbago.ti,ab.
back disorder$.ti,ab.
or/8‐17
massage.mp.
therapeutic touch.mp.
reflexotherapy.mp.
myotherapy.mp.
rolfing.mp.
shiatsu.mp.
acupressure.mp.
reflexology.mp.
(polarity adj therapy).mp.
(myofascial adj release).mp.
(craniosacral adj therapy).mp.
reiki.mp.
(trager adj psychophysical).mp.
(hakomi adj method).mp.
(jin adj shin).mp.
(neuromuscular adj therapy).mp.
(pfrimmer adj25 therapy).mp.
(alexander adj technique).mp.
(feldenkrais adj method).mp.
or/19‐37
massage.mp.
heart massage.mp.
39 not 40
38 or 41
7 and 18 and 42
EMBASE
Last searched July 17, 2014. We revised the animal studies filter in 2013 and the RCT filter in 2014.
Clinical Article/
exp Clinical Study/
Clinical Trial/
Controlled Study/
Randomized Controlled Trial/
Major Clinical Study/
Double Blind Procedure/
Multicenter Study/
Single Blind Procedure/
Phase 3 Clinical Trial/
Phase 4 Clinical Trial/
crossover procedure/
placebo/
or/1‐13
allocat$.mp.
assign$.mp.
blind$.mp.
(clinic$ adj25 (study or trial)).mp.
compar$.mp.
control$.mp.
cross?over.mp.
factorial$.mp.
follow?up.mp.
placebo$.mp.
prospectiv$.mp.
random$.mp.
((singl$ or doubl$ or trebl$ or tripl$) adj25 (blind$ or mask$)).mp.
trial.mp.
(versus or vs).mp.
or/15‐29
14 or 30
exp animals/ or exp invertebrate/ or animal experiment/ or animal model/ or animal tissue/ or animal cell/ or nonhuman/
human/ or normal human/ or human cell/
32 and 33
32 not 34
31 not 35
dorsalgia.mp.
back pain.mp.
exp BACKACHE/
(lumbar adj pain).mp.
coccyx.mp.
coccydynia.mp.
sciatica.mp.
exp ISCHIALGIA/
spondylosis.mp.
lumbago.mp.
exp Low Back Pain/
back disorder$.mp.
or/37‐48
exp massage/
therapeutic touch.mp.
reflexotherapy.mp.
exp ROLFING/
exp SHIATSU/
exp reflexology/
myotherapy.mp.
(polarity adj therapy).mp.
(myofascial adj release).mp.
(craniosacral adj therapy).mp.
exp REIKI/ (244)
(trager adj psychophysical).mp.
(hakomi adj method).mp.
(jin adj shin).mp.
(neuromuscular adj therapy).mp.
(pfrimmer adj25 therapy).mp.
(alexander adj technique).mp.
exp Alexander Technique/
(feldenkrais adj method).mp.
MASSAGEMETHODEN.mp.
MASSAGEINST.mp.
MASSAGEBEHANDLUNG.mp.
MASSAGEE.mp.
MASSAGED.mp.
MASSAGE‐WERE.mp.
MASSAGE‐TYPE.mp.
MASSAGE‐TUINA‐THERAPIE.mp.
MASSAGE‐LIKE.mp.
MASSAGE‐INDUCED.mp.
MASSAGE‐ENHANCED.mp.
MASSAGE‐CONTROL.mp.
MASSAGE‐CONTINUED.mp.
MASSAGE‐AND‐PRESSURE.mp.
or/50‐82
fascia manipulation.mp.
massage.mp.
exp heart massage/ or exp carotid sinus massage/
85 not 86
83 or 84 or 87
36 and 49 and 88
limit 89 to yr=2013‐2014
limit 89 to em=201321‐201428
90 or 91
2008 search strategy
Clinical Article/
exp Clinical Study/
Clinical Trial/
Controlled Study/
Randomized Controlled Trial/
Major Clinical Study/
Double Blind Procedure/
Multicenter Study/
Single Blind Procedure/
Phase 3 Clinical Trial/
Phase 4 Clinical Trial/
crossover procedure/
placebo/
or/1‐13
allocat$.mp.
assign$.mp.
blind$.mp.
(clinic$ adj25 (study or trial)).mp.
compar$.mp.
control$.mp.
cross?over.mp.
factorial$.mp.
follow?up.mp.
placebo$.mp.
prospectiv$.mp.
random$.mp.
((singl$ or doubl$ or trebl$ or tripl$) adj25 (blind$ or mask$)).mp.
trial.mp.
(versus or vs).mp.
or/15‐29
14 and 30
human/
Nonhuman/
exp ANIMAL/
Animal Experiment/
33 or 34 or 35
32 not 36
31 not 36
37 and 38
38 or 39
dorsalgia.mp.
back pain.mp.
exp BACKACHE/
(lumbar adj pain).mp.
coccyx.mp.
coccydynia.mp.
sciatica.mp.
exp ISCHIALGIA/
spondylosis.mp.
lumbago.mp.
exp Low Back Pain/
or/41‐51
exp massage/
therapeutic touch.mp.
reflexotherapy.mp.
exp ROLFING/
exp SHIATSU/
exp reflexology/
myotherapy.mp.
(polarity adj therapy).mp.
(myofascial adj release).mp.
(craniosacral adj therapy).mp.
exp REIKI/
(trager adj psychophysical).mp.
(hakomi adj method).mp.
(jin adj shin).mp.
(neuromuscular adj therapy).mp.
(pfrimmer adj25 therapy).mp.
(alexander adj technique).mp.
exp Alexander Technique/
(feldenkrais adj method).mp.
MASSAGEMETHODEN.mp.
MASSAGEINST.mp.
MASSAGEBEHANDLUNG.mp.
MASSAGEE.mp.
MASSAGED.mp.
MASSAGE‐WERE.mp.
MASSAGE‐TYPE.mp.
MASSAGE‐TUINA‐THERAPIE.mp.
MASSAGE‐LIKE.mp.
MASSAGE‐INDUCED.mp.
MASSAGE‐ENHANCED.mp.
MASSAGE‐CONTROL.mp.
MASSAGE‐CONTINUED.mp.
MASSAGE‐AND‐PRESSURE.mp.
or/53‐85
40 and 52 and 86
limit 87 to yr="2007 ‐ 2008"
CENTRAL
Last searched July 17, 2014
#1 MeSH descriptor: [Back Pain] explode all trees
#2 dorsalgia
#3 backache
#4 MeSH descriptor: [Low Back Pain] explode all trees
#5 lumbar next pain OR coccyx OR coccydynia OR sciatica OR spondylosis
#6 MeSH descriptor: [Spine] explode all trees
#7 MeSH descriptor: [Spinal Diseases] explode all trees
#8 lumbago OR discitis OR disc near degeneration OR disc near prolapse OR disc near herniation
#9 spinal fusion
#10 spinal neoplasms
#11 facet near joints
#12 MeSH descriptor: [Intervertebral Disk] explode all trees
#13 postlaminectomy
#14 arachnoiditis
#15 failed near back
#16 MeSH descriptor: [Cauda Equina] explode all trees
#17 lumbar near vertebra*
#18 spinal near stenosis
#19 slipped near (disc* or disk*)
#20 degenerat* near (disc* or disk*)
#21 stenosis near (spine or root or spinal)
#22 displace* near (disc* or disk*)
#23 prolap* near (disc* or disk*)
#24 MeSH descriptor: [Sciatic Neuropathy] explode all trees
#25 sciatic*
#26 back disorder*
#27 back near pain
#28 #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27
#29 MeSH descriptor: [Massage] this term only
#30 MeSH descriptor: [Therapeutic Touch] explode all trees
#31 MeSH descriptor: [Reflexotherapy] explode all trees
#32 MeSH descriptor: [Acupressure] explode all trees
#33 myotherapy
#34 rolfing
#35 shiatsu
#36 reflexology
#37 "polarity therapy"
#38 "myofascial release"
#39 "craniosacral therapy"
#40 reiki
#41 trager
#42 hakomi
#43 "jin shin"
#44 "neuromuscular therapy"
#45 pfrimmer
#46 "alexander technique"
#47 feldenkrais
#48 "fascia manipulation"
#49 #29 or #30 or #31 or #32 or #33 or #34 or #35 or #36 or #37 or #38 or #39 or #40 or #41 or #42 or #43 or #44 or #45 or #46 or #47 or #48
#50 massage
#51 massage:ti,ab,kw (Word variations have been searched)
#52 MeSH descriptor: [Heart Massage] this term only
#53 (cardiac or heart) and massage:ti,ab,kw (Word variations have been searched)
#54 ((#50 or #51) not (#52 or #53))
#55 #49 or #54
#56 #28 and #55
#57 #56 Publication Year from 2013 to 2014, in Trials
CINAHL
Last searched July 17, 2014. The strategy was revised for EBSCO in 2013.
S67 S65 OR S66
S66 S64 and EM 201306‐
S65 S64 Limiters ‐ Published Date: 20130601‐20140731
S64 S49 AND S63
S63 S59 OR S62
S62 S60 NOT S61
S61 (MH "Heart Massage")
S60 "massage"
S59 S50 OR S51 OR S52 OR S53 OR S54 OR S55 OR S56 OR S57 OR S58
S58 "reflexotherapy"
S57 (MH "Reiki")
S56 (MH "Polarity Therapy")
S55 (MH "Therapeutic Touch")
S54 (MH "Structural‐Functional‐Movement Integration+")
S53 (MH "Reflexology")
S52 (MH "Myofascial Release")
S51 (MH "Craniosacral Therapy")
S50 (MH "Massage+")
S49 S28 and S48
S48 S35 or S43 or S47
S47 S44 or S45 or S46
S46 "lumbago"
S45 (MH "Spondylolisthesis") OR (MH "Spondylolysis")
S44 (MH "Thoracic Vertebrae")
S43 S36 or S37 or S38 or S39 or S40 or S41 or S42
S42 lumbar N2 vertebra*
S41 (MH "Lumbar Vertebrae")
S40 "coccydynia"
S39 "coccyx"
S38 "sciatica"
S37 (MH "Sciatica")
S36 (MH "Coccyx")
S35 S29 or S30 or S31 or S32 or S33 or S34
S34 lumbar N5 pain
S33 lumbar W1 pain
S32 "backache"
S31 (MH "Low Back Pain")
S30 (MH "Back Pain+")
S29 "dorsalgia"
S28 S26 NOT S27
S27 (MH "Animals")
S26 S7 or S12 or S19 or S25
S25 S20 or S21 or S22 or S23 or S24
S24 volunteer*
S23 prospectiv*
S22 control*
S21 followup stud*
S20 follow‐up stud*
S19 S13 or S14 or S15 or S16 or S17 or S18
S18 (MH "Prospective Studies+")
S17 (MH "Evaluation Research+")
S16 (MH "Comparative Studies")
S15 latin square
S14 (MH "Study Design+")
S13 (MH "Random Sample")
S12 S8 or S9 or S10 or S11
S11 random*
S10 placebo*
S9 (MH "Placebos")
S8 (MH "Placebo Effect")
S7 S1 or S2 or S3 or S4 or S5 or S6
S6 triple‐blind
S5 single‐blind
S4 double‐blind
S3 clinical W3 trial
S2 "randomi?ed controlled trial*"
S1 (MH "Clinical Trials+")
2008 search strategy. The service provider was Ovid.
Randomized Controlled Trials.mp.
clinical trial.pt.
exp Clinical Trials/
(clin$ adj25 trial$).tw.
((singl$ or doubl$ or trebl$ or tripl$) adj25 (blind$ or mask$)).tw.
exp PLACEBOS/
placebo$.tw.
random$.tw.
exp Study Design/
(latin adj square).tw.
exp Comparative Studies/
exp Evaluation Research/
Follow‐Up Studies.mp.
exp Prospective Studies/
(control$ or prospectiv$ or volunteer$).tw.
Animals/
or/1‐15
17 not 16
dorsalgia.mp.
exp Back Pain/
backache.mp.
(lumbar adj pain).mp
exp COCCYX/
exp SCIATICA/
coccyx.mp.
sciatica.mp.
exp Low Back Pain/
coccydynia.mp.
sciatica.mp. or exp SCIATICA/
exp Lumbar Vertebrae/ or exp Spondylolisthesis/ or exp Spondylolysis/
lumbago.mp.
or/19‐31
exp MASSAGE/
exp Therapeutic Touch/
reflexotherapy.mp.
exp ROLFING/
exp SHIATSU/
exp REFLEXOLOGY/
myotherapy.mp.
(polarity adj therapy).mp.
(myofascial adj release).mp.
(craniosacral adj therapy).mp.
exp REIKI/
(trager adj psychophysical).mp.
(hakomi adj method).mp.
(jin adj shin).mp.
(neuromuscular adj therapy).mp.
(pfrimmer adj25 therapy).mp.
(alexander adj technique).mp.
exp Alexander Technique/
(feldenkrais adj method).mp.
or/33‐51
18 and 32 and 52
limit 53 to yr="2007 ‐ 2008"
Index to Chiropractic Literature
Last searched July 21, 2014
S1 , Publication Type:Clinical Trial
S2 , Publication Type:Controlled Clinical Trial
S3 , Publication Type:Randomized Controlled Trial
S4 Subject:"Clinical Trials" OR Subject:"Clinical Trials as Topic" OR Subject:"Controlled Clinical Trials"
S5 All Fields:random* OR All Fields:placebo OR All Fields:sham
S6 All Fields:versus OR All Fields:vs
S7 Subject:"Randomized Controlled Trials as Topic" OR Subject:"Prospective Studies" OR Subject:"Comparative Study"
S9 All Fields:double‐blind OR All Fields:"double blind"
S10 All Fields:single‐blind OR All Fields:"single blind"
S11 All Fields:"Clinical Trial" OR All Fields:"Controlled Trial"
S12 , Publication Type:Clinical Trial OR , Publication Type:Controlled Clinical Trial OR , Publication Type:Randomized Controlled Trial OR Subject:"Clinical Trials" OR Subject:"Clinical Trials as Topic" OR Subject:"Controlled Clinical Trials" OR All Fields:random* OR All Fields:placebo OR All Fields:sham OR All Fields:versus OR All Fields:vs OR Subject:"Randomized Controlled Trials as Topic" OR Subject:"Prospective Studies" OR Subject:"Comparative Study" OR All Fields:double‐blind OR All Fields:"double blind" OR All Fields:single‐blind OR All Fields:"single blind" OR All Fields:"Clinical Trial" OR All Fields:"Controlled Trial"
S13 Subject:"Back" OR Subject:"Back Injuries" OR Subject:"Back Pain"
S14 Subject:"Low Back Pain" OR Subject:"Lumbar" OR Subject:"Lumbosacral Region"
S15 Subject:"Sciatica" OR All Fields:sciatica OR Subject:"Lumbar Vertebrae"
S16 Subject:"Coccyx" OR Subject:"Sacroiliac Joint" OR Subject:"Sacrum"
S17 Subject:"Back" OR Subject:"Back Injuries" OR Subject:"Back Pain" OR Subject:"Low Back Pain" OR Subject:"Lumbar" OR Subject:"Lumbosacral Region" OR Subject:"Sciatica" OR All Fields:sciatica OR Subject:"Lumbar Vertebrae" OR Subject:"Coccyx" OR Subject:"Sacroiliac Joint" OR Subject:"Sacrum"
S18 All Fields:massage OR Subject:"Massage"
S19 All Fields:"Therapeutic Touch" OR Subject:"Therapeutic Touch"
S20 All Fields:"Craniosacral Therapy" OR Subject:"Craniosacral Therapy"
S21 All Fields:"Myofascial Release" OR All Fields:Reflexology OR All Fields:"Polarity Therapy"
S22 All Fields:reiki OR All Fields:reflexotherapy
S23 All Fields:"acupressure" OR Subject:"Acupressure"
S24 Subject:"Shiatsu" OR All Fields:shiatsu
S25 All Fields:"Alexander Technique" OR All Fields:Feldenkrais OR All Fields:Hellerwork
S26 All Fields:trager OR All Fields:Rolfing
S27 All Fields:hakomi OR All Fields:pfrimmer
S28 All Fields:"fascia manipulation"
S29 All Fields:massage OR Subject:"Massage" OR All Fields:"Therapeutic Touch" OR Subject:"Therapeutic Touch" OR All Fields:"Craniosacral Therapy" OR Subject:"Craniosacral Therapy" OR All Fields:"Myofascial Release" OR All Fields:Reflexology OR All Fields:"Polarity Therapy" OR All Fields:reiki OR All Fields:reflexotherapy OR All Fields:"acupressure" OR Subject:"Acupressure" OR Subject:"Shiatsu" OR All Fields:shiatsu OR All Fields:"Alexander Technique" OR All Fields:Feldenkrais OR All Fields:Hellerwork OR All Fields:trager OR All Fields:Rolfing OR All Fields:hakomi OR All Fields:pfrimmer OR All Fields:"fascia manipulation"
S30 , Publication Type:Clinical Trial OR , Publication Type:Controlled Clinical Trial OR , Publication Type:Randomized Controlled Trial OR Subject:"Clinical Trials" OR Subject:"Clinical Trials as Topic" OR Subject:"Controlled Clinical Trials" OR All Fields:random* OR All Fields:placebo OR All Fields:sham OR All Fields:versus OR All Fields:vs OR Subject:"Randomized Controlled Trials as Topic" OR Subject:"Prospective Studies" OR Subject:"Comparative Study" OR All Fields:double‐blind OR All Fields:"double blind" OR All Fields:single‐blind OR All Fields:"single blind" OR All Fields:"Clinical Trial" OR All Fields:"Controlled Trial" AND Subject:"Back" OR Subject:"Back Injuries" OR Subject:"Back Pain" OR Subject:"Low Back Pain" OR Subject:"Lumbar" OR Subject:"Lumbosacral Region" OR Subject:"Sciatica" OR All Fields:sciatica OR Subject:"Lumbar Vertebrae" OR Subject:"Coccyx" OR Subject:"Sacroiliac Joint" OR Subject:"Sacrum" AND All Fields:massage OR Subject:"Massage" OR All Fields:"Therapeutic Touch" OR Subject:"Therapeutic Touch" OR All Fields:"Craniosacral Therapy" OR Subject:"Craniosacral Therapy" OR All Fields:"Myofascial Release" OR All Fields:Reflexology OR All Fields:"Polarity Therapy" OR All Fields:reiki OR All Fields:reflexotherapy OR All Fields:"acupressure" OR Subject:"Acupressure" OR Subject:"Shiatsu" OR All Fields:shiatsu OR All Fields:"Alexander Technique" OR All Fields:Feldenkrais OR All Fields:Hellerwork OR All Fields:trager OR All Fields:Rolfing OR All Fields:hakomi OR All Fields:pfrimmer OR All Fields:"fascia manipulation"
S31 , Year: from 2013 to 2014
S32 , Publication Type:Clinical Trial OR , Publication Type:Controlled Clinical Trial OR , Publication Type:Randomized Controlled Trial OR Subject:"Clinical Trials" OR Subject:"Clinical Trials as Topic" OR Subject:"Controlled Clinical Trials" OR All Fields:random* OR All Fields:placebo OR All Fields:sham OR All Fields:versus OR All Fields:vs OR Subject:"Randomized Controlled Trials as Topic" OR Subject:"Prospective Studies" OR Subject:"Comparative Study" OR All Fields:double‐blind OR All Fields:"double blind" OR All Fields:single‐blind OR All Fields:"single blind" OR All Fields:"Clinical Trial" OR All Fields:"Controlled Trial" AND Subject:"Back" OR Subject:"Back Injuries" OR Subject:"Back Pain" OR Subject:"Low Back Pain" OR Subject:"Lumbar" OR Subject:"Lumbosacral Region" OR Subject:"Sciatica" OR All Fields:sciatica OR Subject:"Lumbar Vertebrae" OR Subject:"Coccyx" OR Subject:"Sacroiliac Joint" OR Subject:"Sacrum" AND All Fields:massage OR Subject:"Massage" OR All Fields:"Therapeutic Touch" OR Subject:"Therapeutic Touch" OR All Fields:"Craniosacral Therapy" OR Subject:"Craniosacral Therapy" OR All Fields:"Myofascial Release" OR All Fields:Reflexology OR All Fields:"Polarity Therapy" OR All Fields:reiki OR All Fields:reflexotherapy OR All Fields:"acupressure" OR Subject:"Acupressure" OR Subject:"Shiatsu" OR All Fields:shiatsu OR All Fields:"Alexander Technique" OR All Fields:Feldenkrais OR All Fields:Hellerwork OR All Fields:trager OR All Fields:Rolfing OR All Fields:hakomi OR All Fields:pfrimmer OR All Fields:"fascia manipulation" AND , Year: from 2013 to 2014
LILACS
Last searched July 17, 2014
(“back pain” or “low back pain” or “Dolor de Espalda” or “Dor nas Costas” or backache or dorsalgia or Lumbosacra$ or Lombossacral or Sciatic$ or Ciática or Spondylosis or Espondilosis or Espondilose or Lumbalgia or Lumbociatica or “Dolor lumbosacro” or “dolor lumbo sacro” or “sacrolumbalgia” or ciatica or “dolor bajo de espalda” or Lombalgia or Lombalgias or “Dores nas costas” or “Dor lombar” or “Dores lombares” or “Dor ciática” or “Dor do nervo ciático” or Espondilolistese) AND (Massage or Masaje or Massagem or Reflexolog$ or “Zone Therapy” or “Therapeutic Touch” or “Tacto Terapéutico” or “Toque Terapêutico” or Reflexotherapy or Reflejoterapia or Reflexoterapia or Myotherapy or rolfing or shiatsu or shiatzu or “Chih Ya” or “Zhi Ya” or Acupressure or Acupresión or Acupressão or "polarity therapy" or “myofascial release” or “craniosacral therapy” “terapia cranio sacra” or reiki or “trager psychophysical” or hakomi method” or “método hakomi” or “pfrimmer therapy” or “terapia pfrimmer” or “alexander technique” or “técnica Alexander” or “feldenkrais method” or “método feldenkrais” or “jin shin” or “neuromuscular therapy” or “fascia manipulation” or “Manipulação fascial” or mioterapia or “liberación miofascial” or “terapia neuromuscular” or “manipulacion fascial” or “terapia tuina” or “masaje tuina” or “terapia polaridad”) , limited to 2013‐2014
using iAH form, searching Words field
Proquest Dissertation Abstracts
Last searched July 17, 2014, through Proquest aggregated databases (which included Dissertation Abstracts). We searched the database directly in 2013 and used the same strategy without any limits.
all ((dorsalgia OR "Back Pain" OR "backache" OR (lumbar NEAR/3 pain) OR coccyx OR coccydynia OR sciatic* OR spondylosis OR lumbago OR "low back pain" OR "back disorder*")) AND all((Massage OR "Therapeutic Touch" OR Reflexotherapy OR cryotherapy OR rolfing OR shiat?u OR Acupressure OR reflexology OR "polarity therapy" OR "myofascial release" OR "craniosacral therapy" OR reiki OR "trager psychophysical" OR "hakomi method" OR "jin shin" OR "neuromuscular therapy" OR "pfrimmer therapy" OR "alexander technique" OR feldenkrais OR "neuromuscular therapy" OR "fascia manipulation"))
Limit to Dissertations & Theses and Conference Papers & Proceedings
ALL field = Anywhere except full‐text
Pubmed
Last searched August 7, 2014
((back pain[Title/Abstract]) AND massage[Title/Abstract]) AND ("2013/07/01"[Date ‐ Publication] : "3000"[Date ‐ Publication]) NOT MEDLINE[sb]
Appendix 2. 'Risk of bias' criteria
Random sequence generation (selection bias)
Selection bias (biased allocation to interventions) due to inadequate generation of a randomized sequence
There is a low risk of selection bias if the investigators describe a random component in the sequence generation process such as: referring to a random number table, using a computer random number generator, coin tossing, shuffling cards or envelopes, throwing dice, drawing of lots, minimization (minimization may be implemented without a random element, and this is considered to be equivalent to being random).
There is a high risk of selection bias if the investigators describe a non‐random component in the sequence generation process, such as: sequence generated by odd or even date of birth, date (or day) of admission, hospital or clinic record number; or allocation by judgement of the clinician, preference of the participant, results of a laboratory test or a series of tests, or availability of the intervention.
Allocation concealment (selection bias)
Selection bias (biased allocation to interventions) due to inadequate concealment of allocations prior to assignment
There is a low risk of selection bias if the participants and investigators enrolling participants could not foresee assignment because one of the following, or an equivalent method, was used to conceal allocation: central allocation (including telephone, web‐based and pharmacy‐controlled randomization); sequentially‐numbered drug containers of identical appearance; or sequentially‐numbered, opaque, sealed envelopes.
There is a high risk of bias if participants or investigators enrolling participants could possibly foresee assignments and thus introduce selection bias, such as allocation based on: using an open random allocation schedule (e.g. a list of random numbers); assignment envelopes were used without appropriate safeguards (e.g. if envelopes were unsealed or non‐opaque or not sequentially numbered); alternation or rotation; date of birth; case record number; or other explicitly unconcealed procedures.
Blinding of participants
Performance bias due to knowledge of the allocated interventions by participants during the study
There is a low risk of performance bias if blinding of participants was ensured and it was unlikely that the blinding could have been broken; or if there was no blinding or incomplete blinding, but the review authors judge that the outcome is not likely to be influenced by lack of blinding.
Blinding of personnel/care providers (performance bias)
Performance bias due to knowledge of the allocated interventions by personnel/care providers during the study
There is a low risk of performance bias if blinding of personnel was ensured and it was unlikely that the blinding could have been broken; or if there was no blinding or incomplete blinding, but the review authors judge that the outcome is not likely to be influenced by lack of blinding.
Blinding of outcome assessor (detection bias)
Detection bias due to knowledge of the allocated interventions by outcome assessors
There is low risk of detection bias if the blinding of the outcome assessment was ensured and it was unlikely that the blinding could have been broken; or if there was no blinding or incomplete blinding, but the review authors judge that the outcome is not likely to be influenced by lack of blinding, or:
for patient‐reported outcomes in which the patient was the outcome assessor (e.g. pain, disability): there is a low risk of bias for outcome assessors if there is a low risk of bias for participant blinding (Boutron 2005)
for outcome criteria that are clinical or therapeutic events that will be determined by the interaction between patients and care providers (e.g. co‐interventions, length of hospitalisation, treatment failure), in which the care provider is the outcome assessor: there is a low risk of bias for outcome assessors if there is a low risk of bias for care providers (Boutron 2005)
for outcome criteria that are assessed from data from medical forms: there is a low risk of bias if the treatment or adverse effects of the treatment could not be noticed in the extracted data (Boutron 2005)
Incomplete outcome data (attrition bias)
Attrition bias due to amount, nature or handling of incomplete outcome data
There is a low risk of attrition bias if: there were no missing outcome data; reasons for missing outcome data were unlikely to be related to the true outcome (for survival data, censoring unlikely to be introducing bias); missing outcome data were balanced in numbers, with similar reasons for missing data across groups; for dichotomous outcome data, the proportion of missing outcomes compared with the observed event risk was not enough to have a clinically‐relevant impact on the intervention effect estimate; for continuous outcome data, the plausible effect size (difference in means or standardized difference in means) among missing outcomes was not enough to have a clinically‐relevant impact on observed effect size, or missing data were imputed using appropriate methods (if drop‐outs are very large, imputation using even 'acceptable' methods may still suggest a high risk of bias) (van Tulder 2003). The percentage of withdrawals and drop‐outs should not exceed 20% for short‐term follow‐up and 30% for long‐term follow‐up and should not lead to substantial bias (these percentages are commonly used but arbitrary, not supported by literature) (van Tulder 2003).
Selective reporting (reporting bias)
Reporting bias due to selective outcome reporting
There is a low risk of reporting bias if the study protocol is available and all of the study's pre‐specified (primary and secondary) outcomes that are of interest in the review have been reported in the pre‐specified way, or if the study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified (convincing text of this nature may be uncommon).
There is a high risk of reporting bias if not all of the study's pre‐specified primary outcomes have been reported; one or more primary outcomes is reported using measurements, analysis methods or subsets of the data (e.g. subscales) that were not pre‐specified; one or more reported primary outcomes were not pre‐specified (unless clear justification for their reporting is provided, such as an unexpected adverse effect); one or more outcomes of interest in the review are reported incompletely so that they cannot be entered in a meta‐analysis; the study report fails to include results for a key outcome that would be expected to have been reported for such a study.
Group similarity at baseline (selection bias)
Bias due to dissimilarity at baseline for the most important prognostic indicators.
There is low risk of bias if groups are similar at baseline for demographic factors, value of main outcome measure(s), and important prognostic factors (examples in the field of back and neck pain are duration and severity of complaints, vocational status, percentage of patients with neurological symptoms) (van Tulder 2003).
Co‐interventions (performance bias)
Bias because co‐interventions were different across groups
There is low risk of bias if there were no co‐interventions or they were similar between the index and control groups (van Tulder 2003).
Compliance (performance bias)
Bias due to inappropriate compliance with interventions across groups
There is low risk of bias if compliance with the interventions was acceptable, based on the reported intensity/dosage, duration, number and frequency for both the index and control intervention(s). For single‐session interventions (e.g. surgery), this item is irrelevant (van Tulder 2003).
Intention‐to‐treat analysis
There is low risk of bias if all randomized patients were reported/analyzed in the group to which they were allocated by randomization.
Timing of outcome assessments (detection bias)
Bias because important outcomes were not measured at the same time across groups
There is low risk of bias if all important outcome assessments for all intervention groups were measured at the same time (van Tulder 2003).
Other bias
Bias due to problems not covered elsewhere in the table
There is a low risk of bias if the study appears to be free of other sources of bias not addressed elsewhere (e.g. study funding).
Appendix 3. GRADE approach to evidence synthesis
1. Study design
In this review we only included RCTs.
2. Risk of bias
Limitations in the study design and implementation may bias the estimates of the treatment effect. Our confidence in the estimate of the effect and in the following recommendation decreases if studies suffer from major limitations. We examined all studies on five types of biases: selection, performance, detection, attrition and selective reporting bias.
The overall risk of bias for each study was used in the GRADE synthesis. When we judged all studies to be at "low risk of bias" for all five types of categories, we did not downgrade the evidence. The evidence was downgraded as follows:
by one level when < three categories were judged to be at either "high" or "unclear" risk of bias.
by two levels when four or more categories were judged to be at either "high" or "unclear" risk of bias.
3. Inconsistency
Inconsistency refers to an unexplained heterogeneity of results. Widely differing estimates of the treatment effect (i.e. heterogeneity or variability in results) across studies suggest true differences in underlying treatment effect. Inconsistency may arise from differences in: populations (e.g. drugs may have larger relative effects in sicker populations), interventions (e.g. larger effects with higher drug doses), or outcomes (e.g. diminishing treatment effect with time). This item does not apply when there is only one study. We downgraded the quality of evidence as follows:
by one level: when the heterogeneity or variability in results was large (e.g. I² statistic > 80%)
by two levels: when the heterogeneity or variability in results was large and there was inconsistency arising from populations, interventions or outcomes.
4. Indirectness
Indirect population, intervention, comparator, or outcome – the question being addressed in this systematic review is different from the available evidence regarding the population, intervention, comparator or an outcome in the included RCT. The quality of evidence was downgraded as follows:
by one level: when there was indirectness in only one area.
by two levels: when there was indirectness in two or more areas.
5. Imprecision
Results are imprecise when studies include relatively few patients and few events and thus have wide CIs around the estimate of the effect. In this case we judged the quality of the evidence lower than it otherwise would because of resulting uncertainty in the results. Each outcome is considered separately.
Dichotomous outcomes
We considered imprecision for either of the following two reasons:
There is only one study. When there is > one study, the total number of events is < 300 (a threshold rule‐of‐thumb value) (Mueller 2007)
95% CI around the pooled or best estimate of effect includes both 1) no effect and 2) appreciable benefit or appreciable harm. The threshold for "appreciable benefit" or "appreciable harm" is a relative risk reduction (RRR) or relative risk increase (RRI) greater than 25%.
We downgraded the quality of the evidence as follows:
by one level: when there was imprecision due to (1) or (2).
by two levels: when there was imprecision due to (1) and (2).
For continuous outcomes
We considered imprecision for either of the following two reasons:
There is only one study. When there is > one study, total population size is < 400 (a threshold rule‐of‐thumb value; using the usual α and β, and an effect size of 0.2 SD, representing a small effect)
95% CI includes no effect and the upper or lower confidence limit crosses an effect size (SMD) of 0.5 in either direction.
We downgraded the quality of the evidence as follows:
by one level: when there was imprecision due to (1) or (2).
by two levels: when there was imprecision due to (1) and (2).
6. Publication bias
Publication bias is a systematic underestimate or an overestimate of the underlying beneficial or harmful effect due to the selective publication of studies. The quality of evidence was downgraded as follows:
by one level: when the funnel plot suggested publication bias.
Data and analyses
Comparison 1. Massage versus inactive controls for acute LBP.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain intensity (higher scores mean more pain) | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Short‐term follow‐up | 1 | 51 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.24 [‐1.85, ‐0.64] |
| 2 Function (higher scores mean more disability) | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Short‐term follow‐up | 1 | 51 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐1.06, 0.06] |
| 3 Adverse events | 1 | 51 | Risk Difference (M‐H, Random, 95% CI) | 0.0 [‐0.07, 0.07] |
Comparison 2. Massage versus inactive controls for sub‐acute and chronic LBP.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain intensity (higher scores mean more pain) | 8 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Short‐term follow‐up | 7 | 761 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.75 [‐0.90, ‐0.60] |
| 1.2 Long‐term follow‐up | 3 | 615 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.15, 0.18] |
| 2 Function (higher scores mean more disability) | 7 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Short‐term follow‐up | 6 | 725 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.72 [‐1.05, ‐0.39] |
| 2.2 Long‐term follow‐up | 3 | 615 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐0.32, 0.01] |
| 3 Adverse events | 4 | 624 | Risk Difference (M‐H, Random, 95% CI) | 0.06 [0.00, 0.11] |
Comparison 3. Massage versus active controls for sub‐acute and chronic LBP.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain intensity (higher scores mean more pain) | 13 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Short‐term follow‐up | 12 | 964 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐0.62, ‐0.13] |
| 1.2 Long‐term follow‐up | 5 | 757 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐0.80, ‐0.01] |
| 2 Function (higher scores mean more disability) | 7 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Short‐term follow‐up | 6 | 618 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐0.62, 0.13] |
| 2.2 Long‐term follow‐up | 4 | 616 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐0.60, 0.17] |
| 3 Adverse events | 5 | 585 | Risk Difference (M‐H, Random, 95% CI) | 0.01 [‐0.01, 0.03] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ajimsha 2014.
| Methods | Country: India. Funding: this research was supported by a grant from the Mahatma Gandhi University, Kottayam, India. Blinding: the outcome assessors were blinded. Recruited: between July 2010 and June 2012, 93 nursing professionals were referred to the Myofascial Therapy and Research Foundation with a diagnosis of CLBP. Those who met the inclusion criteria and provided written informed consent were randomized. Randomized: 80 patients were randomized to treatment group (myofascial release) and control group (sham myofascial release). Followed: myofascial release group, n = 38; control group, n = 36. Analysis: statistical analysis of the data was performed using a 2 x 3 (group x time) analysis of variance (ANOVA) and 2 x 2 (group x time) and 2 x 3 (group x time) repeated‐measures ANOVA. The between‐groups (group), within‐groups (time) and mixed‐groups (group x time) interactions were examined. |
|
| Participants | Population: nursing professionals aged 20 to 40 years old with a diagnosis of CLBP (defined as pain of ≥ 3 months duration). Settings: Myofascial Therapy and Research Foundation. Funding: economic incentives for patients were not reported. Mean age: myofascial release group 35.8 ± 8.4, sham myofascial release group 34.2 ± 9.3. % Female: myofascial release group 76%, sham myofascial release group 77.7%. Ethnicity: not described. The study was performed in the city of Kerala, India. Work status: all patients were nursing professionals. The time of job for myofascial release group was 9.8 ± 7.5 years and for sham myofascial release group was 8.1 ± 6.9 years. Pain duration (mo): myofascial release group 28.3 ± 14.7, sham myofascial release group 26.8 ± 16.0. Previous surgery: not described. Diagnoses: CLBP (defined as pain of ≥ 3 months duration), with a primary complaint of CLBP, and who were judged to have musculoskeletal pain based on evaluation by the musculoskeletal physician and physical therapist. Patients were excluded if they displayed: 1) osteoporosis of the spine; 2) primary joint disease such as active rheumatoid arthritis; 3) metabolic bone disease; 4) malignant bone disease; 5) fracture; 6) hypermobility of the lumbar/sacral spine; 7) cardiovascular or other medical disorder preventing the person from engaging in strenuous exercise; 8) evidence of radiculopathy, or primary complaint of radiating pain; 9) pregnancy; or 10) severe psychiatric disturbance. Use of oral/systemic steroids, use of analgesics on > 10 days a month and any other treatment for CLBP during the previous 6 months were also excluded from the study. |
|
| Interventions | Massage technique: myofascial release (MFR), or a sham myofascial release (SMFR). The 2 interventions were provided 3 times weekly for 8 weeks (weeks 1 to 8), with a minimum of a 1‐day gap between the 2 sessions; the duration of each treatment session was 60 min (40 min for MFR or SMFR and 20 min for specific back exercises).
|
|
| Outcomes | * used in the meta‐analyses: Measured at baseline, immediately after (8th week) and short‐term (12th week): a. Pain: McGill Pain Questionnaire (MPQ)*‐ Pain Rating Index (PRI). b. Function: Quebec Back Pain Disability Scale (QBPDS)*. c. Adverse events: no serious adverse events. Ten patients from the MFR group and 1 from control group reported an increase of pain in the first week after initiation of treatment, and this was reported to have subsided within a week without any medications. Measured in the long‐term: none. |
|
| Notes | a. Pain intensity (MPQ) (range, lower means "better", higher means "worse"):
b. Function (QBPDS) (lower means "less disabled"):
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of randomization is not described. |
| Allocation concealment (selection bias) | Unclear risk | The method of allocation is not described. |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | Low risk | Patients were blinded to the type of therapy. |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Providers were not blinded.. |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | High risk | Assessors were blinded to group but patients are the source of information for the outcome questionnaires and they were not blinded. |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | Drop outs were 2 (5%) and 4 (10%) for MFR group and control group, respectively. |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | All patients were analyzed in the group to which they were allocated by randomization. |
| Selective reporting (reporting bias) | Low risk | Pain and function were measured as defined in the methodology. |
| Other bias | Low risk | No other bias was detected. |
| Similarity of baseline characteristics? | High risk | Other potential conditions that could affect the report of outcomes were not reported, such as physical demands at job or body mass index. |
| Co‐interventions avoided or similar? | Unclear risk | Specific exercises were taken from Sahrman (2002) and Bookhout (1997) and combined with self‐corrections, stretches, and strengthening exercises for 20 min per session both for MFR and control groups. Medications at baseline or follow‐up are not described, although patients were asked to complete a dairy. |
| Compliance acceptable? | Unclear risk | Not completely well described. |
| Timing outcome assessments similar? | Low risk | All patients were evaluated at baseline, immediately after and at 2 weeks. |
Buttagat 2011.
| Methods | Country: Thailand. Funding: Khon Kaen University's Graduate Research Fund Academic Year 2007. Blinding: there is no description about blinding ofo participants, care providers or outcome assessors. Recruited: 36, from Khon Kaen province using bulletin boards and oral requests for participants during a 7‐month period between September 2007 and March 2008. Randomized: 36. Followed: 36. Analysis: Mean and SDs for descriptive statistics. Paired t‐tests were used to compare outcome variables at baseline with outcome measures immediately after the treatment or control period within each respective group. Covariance (ANCOVA) was used to compare the difference in post‐test values between the control and treatment groups after adjusting for differences in baseline values, for each outcome measure. |
|
| Participants | Population: patients with back pain associated with myofascial trigger points (MTrPs), according to criteria specified by Travell and Simons (1983). In > 88% of all cases, the most painful trigger point of each patient was found in the lower part of the back. Upper back pain was not excluded. Settings: the study was conducted in the Division of Physical Therapy, Faculty of Associated Medical Sciences, Khon Kaen University, Thailand. Funding: no monetary incentives for patients. Mean age: 22.6 ± 2.9 years % Female: 55.6%. Ethnicity: All recruited from Khon Kaen province without more descriptions about ethnicity. Work status: student 30 (83.3%), physical Therapist 4 (11.1%), teacher 1 (2.8%), policeman 1 (2.8%). Pain duration: > 12 weeks. Previous surgery: none of the patients. Diagnoses: apparently healthy participants. Disorders affecting the heart rate variability were excluded, such as myocardial infarction, hypertension, neuropathy diabetes mellitus, fever, a history of acute trauma, spinal fracture, inflammatory arthritis (rheumatoid arthritis or gout), muscle diseases, evidence of neurological deficits, or skin diseases. |
|
| Interventions | Massage technique: traditional Thai massage (TTM), 30‐min session, confined to the back area only on TTM‐patients lying in the prone position, during the period between 10.00 and 13.00 h on the day of the study. The technique was in accordance to the system of royal Thai massage, which applies the theory of "Sen Sib" or the 10 meridian lines. Massage points were located along two lines and at an additional, single, point along the paravertebral muscles on each side of the spine. Gentle, gradually increasing, pressure through the therapist's thumb, fingers or palm. Pressure is applied until the patient starts to feel slight discomfort after which this pressure is maintained for 5 to 10 seconds at a time. This sequence can be repeated several times for each massage point. Experience of therapist: "well‐trained massage therapist". No more details were described. Group 1: TTM (n = 18 randomized to this group) Group 2: relaxation (n = 18 randomized to this group). Patients in this group relaxed by lying prone quietly in the same environment and for the same period of time as the treatment group. |
|
| Outcomes | * used in the meta‐analyses: Measured at baseline and immediately after: a. Pain: VAS for pain*, b. Function: none c. Adverse events: not reported d. Other measures:
Measured in the short‐term: none. Measured in the long‐term: none. |
|
| Notes | Results: Pain intensity (VAS) (0 to 10, lower means "better").
Authors' conclusions: TTM can increase HRV and improve stress‐related parameters in this patient population. The results of this study suggest that TTM onto the back muscle for 30 min in the prone position is effective in increasing cardiac parasympathetic activity, reducing sympathetic activity and reducing pain and stress in patients with back pain associated with MTrP. This treatment technique is a non‐pharmacologic intervention with no side effects. Since, this massage technique can be easily taught to partners or family members of patients, we suggest that TTM should be considered as one of the alternative treatments for MTrP. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomized allocation (computer generated) with block sizes of 2, 4 and 6. |
| Allocation concealment (selection bias) | Low risk | Pre‐generated random assignment scheme enclosed in envelopes. |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Participants either received massage or had to lie down and relax. The patients would know if he/she received massage or just lied down. |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | There is no description of blinding the providers to the type of therapy. |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | High risk | Patients self‐reported pain (VAS). There is no description of blinding the patients to the therapy. Since patients were not blinded to the intervention, they were not blinded for outcome assessment. |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | All randomized patients were analysed |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | All patients were analyzed in the group to which they were allocated by randomization. |
| Selective reporting (reporting bias) | Low risk | The pain intensity‐VAS was measured before and after the 30 min session of Massage as specified in the methods section of the manuscript. |
| Other bias | Low risk | No other bias was identified. |
| Similarity of baseline characteristics? | High risk | Missing information about scoliosis, practice of sports, history of longstanding trauma or spinal injuries. Exclusion criteria addressed factors affecting heart rate. Duration of back pain was 5 months more in the massage group. Pain intensity slightly more in the massage group. |
| Co‐interventions avoided or similar? | Low risk | At the end of the study, all participants in both groups were given the opportunity for instruction in a series of back exercises to conduct at home. |
| Compliance acceptable? | Low risk | All patients complied with the interventions. |
| Timing outcome assessments similar? | Low risk | It was done at the end of intervention in both groups. |
Chatchawan 2005.
| Methods | Country: Thailand. Funding: study grant from the Office of the Higher Education Commission, Ministry of Education, Thailand. Blinding: outcome assessor. Recruited: 214. Randomized: 180. Followed: 177 at post treatment; 172 at one month. Analyses: paired t‐tests for comparisons immediately before and after treatment and follow‐ups. ANCOVA for comparisons between groups. | |
| Participants | Population: back pain associated with myofascial trigger points. Settings: Department of Physical Therapy, Faculty of Associated Medical Sciences, Khon Kaen University, Thailand. Mean age: 36.4 years. % female: 114 (63%). % White: not reported. Work status: heavy work: N = 9 (5%); lighter work: N = 171 (95%). Pain duration: 35.7 months. Previous surgery: not included in the study if back surgery. Diagnoses: presence of at least one trigger point diagnosed as the presence of local tenderness at a palpable nodule in a taut band and with pain recognition. |
|
| Interventions | All eligible patients received one of two treatments, either traditional Thai massage (TTM) or Swedish massage (SM), during six sessions over a period of 3 to 4 weeks. Treatment was given for 30 mins and followed by 10 mins of passive stretching, which was similar in both groups. Massage technique: TTM was performed according to the system of royal Thai massage. Massage points included in this method are located along two lines and at an additional, single, point on each side of the back. The first line of massage starts from a point 2 cm above the posterior superior iliac spine (PSIS) and ends at the thoraco‐cervical junction or C7. Each point on this line is approximately one finger breadth away from the spinous process. The second line follows the same course but is about two finger breadths away from the spinous process. The single massage points on each side of the back are located three finger breadths away from the spinous process of the L2 vertebra. The pressing technique employed in TTM uses the body weight of the massage therapist to apply gentle, gradually increasing, pressure through the therapist's thumb finger, palm and elbow. Pressure is applied until the patient starts to feel some pain (pain threshold) after which the pressure is maintained for 5 to 10 seconds at a time. This sequence can be repeated several times for each massage point. SM: this treatment was performed using body oil (jojoba oil) for lubrication of the skin. Pressure was applied on the area of the back between PSIS and C7. This pressure was enough to reach deep into the skin and subcutaneous tissue, but insufficient to reach the pain threshold of each patient. SM techniques used in this study included light stroking or effleurage, and petrissage (which consist of kneading with the thumb, digit and palm; wringing and skin rolling). Massage technique: along two lines on each side of the back: approximately one finger breadth away from the spinous process from 2 cm above the posterior superior iliac spine to C7; about two finger breadths away from the spinous process at the same course. One single massage point on each side of the back three finger breadths away from the spinous process of L2; employed the body weight of the massage therapist to apply gentle, gradually increasing, pressure through the therapist's thumb finger, palm and elbow, until the patient starts to feel some pain after which the pressure is maintained for 5 to 10 seconds at a time, for 30 minutes, 10 minutes passive stretching during for six sessions over a period of three to four weeks. Experience of therapist: four, eight and 20 years of experience. Group 1: TTM (90 randomized to this group). Group 2: SM (90 randomized to this group). |
|
| Outcomes | Measured at baseline, immediately after first treatment; during intervention period (three weeks) and one month after last treatment. a. Pain: VAS. b. Overall improvement: not measured. c. Function: Thai version of the Oswestry disability questionnaire (ODQ). d. Patient satisfaction: 4‐point scale (1 = completely dissatisfied to 4 = very satisfied); % of very satisfied. e. PPT algometry; Thoracolumbar ROM, body flexibility (sit‐and‐reach box). f. Adverse events: soreness, allergic reaction (rashes and pimples) to the massage oil. |
|
| Notes | a. VAS:
b. Function: ODQ (baseline, 3 weeks and 1 month FU):
c. PPT:
d. Patient satisfaction:
Authors' conclusions: "TTM or SM treatment can be used, with equal expected effectiveness, in the treatment of back pain associated with myofascial trigger points. We therefore recommend that TTM and SM be more widely promoted as alternative primary health care treatments for this disorder." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization was performed using block randomized allocation with block sizes of 2, 4 and 6. Groups were assigned using a pre‐generated random assignment scheme. |
| Allocation concealment (selection bias) | Low risk | Random assignment scheme enclosed in envelopes. |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Authors reported "it was not feasible for the patients to be blinded". |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Not blinded. |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | High risk | "All outcome measures were assessed by one physical therapist with 15 years of experience, for whom the treatment groups were blinded." However, the outcomes are self‐reported by patients and patients were not blinded. |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | At the end of the study 85/90 patients of TTM and 87/90 of SM completed the treatment and follow‐up. |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | The trial authors state that all analysis were performed on an ITT basis. |
| Selective reporting (reporting bias) | Unclear risk | Trial authors reported all primary outcomes: pain and back‐specific functional status. However, the satisfaction with the treatment at 1 month, the adverse effects, the medication used and the range of motion were not reported for the last evaluation at 1 month. |
| Other bias | Low risk | No other bias was identified. |
| Similarity of baseline characteristics? | Low risk | No major differences between groups on demographics, physical work load of occupation, causes of back pain, height, weight, duration of back pain, time since last episode of back pain, stress level and main outcomes (pain, disability and patient's satisfaction). |
| Co‐interventions avoided or similar? | Low risk | Both groups received 10 minutes of stretching after the treatment. A home care program was recommended including back stretching exercises and health care education (correct posture and lifting techniques). The adherence to the home care program was not measured. It could be different between groups. |
| Compliance acceptable? | Low risk | "in the majority of patients, treatment occurred according to the planned schedule of two sessions a week for 3 weeks". |
| Timing outcome assessments similar? | Low risk | Yes. |
Cherkin 2001.
| Methods | Country: USA. Funding: grants from Group Health Cooperative, The Group Health Foundation, Seattle, Wash, and the John E. Fetzer Institute, Kalamazoo, Mich; and by grant HS09351 from the Agency for Healthcare Research and Quality. Method of randomization: computer‐generated random sequence. 3996 letters were mailed. 693 consent forms returned. The first 262 enrollees confirmed eligible were randomized. Patients were HMO enrollees, six weeks after a primary care visit for back pain. Period of study: May to Oct 1997. Follow‐up: 4, 10 and 52 weeks after randomization. 95% were followed up to 52 weeks. |
|
| Participants | Settings: this study was conducted at Group Health Cooperative, a large staff‐model health maintenance organization (HMO) in Washington State. Average age: 44.9 years. 58% women. 84% white. 84% employed or self‐employed. Previous treatments: 6% operation, 3% acupuncture, 16% massage. Length of pain: at least 6 weeks, 61% lasted > 1 year. |
|
| Interventions | 1. Licensed therapist. At least three years of experience. Manipulation of soft tissue (i.e. muscle and fascia). Swedish (71%), movement reeducation (70%), deep‐tissue (65%), neuromuscular (45%), and trigger and pressure point (48%), Moist heat or cold (51%). Prohibited: energy techniques (Reiki, therapeutic touch). Proscribed meridian therapies (acupressure and shiatsu) and approaches deemed too specialized (craniosacral and Rolfing). Massage therapists recommended exercise, typically stretching. 59% also used "body awareness" techniques to help clients become more aware of their physical and kinaesthetic sensations, including potential early warning signals of injury. Mean (SD) number of visits = 8.0 (2.4). 2. Traditional Chinese medical acupuncture. Mean (SD) number of visits = 8.3 (2.3). 3. Self‐care education: high‐quality and inexpensive educational material designed for persons with chronic back pain: a book and two professionally produced videotapes. | |
| Outcomes | * used in the meta‐analyses: Measured before, after 4, 10* and 52* weeks of the randomization. Primary outcome measures: a. Bothersomeness of back pain (0 to 10); bothersomeness of leg pain (0 to 10), or bothersomeness of numbness or tingling (0 to 10). The higher (of the 3) score was used (valid). b. Modified Roland Disability Scale (reliable, valid and sensitive)*. Secondary outcome measures: c. Disability: National Health Interview Survey. d. Utilization: provider visits, RXs, operations, hospitalizations, medication use, visits to other massage or acupuncture practitioners. e. Satisfaction. f. SF‐12, Mental Health summary scales. h. Number of days of exercise. i. Adverse events: No serious adverse effects. Eleven percent of patients in the acupuncture group and 13% in the massage group reported "significant discomfort or pain" during or shortly after treatment. |
|
| Notes | Authors' conclusions: therapeutic massage was effective for persistent LBP, apparently providing long‐lasting benefits. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random sequence. |
| Allocation concealment (selection bias) | Low risk | By using computer assisted telephone interviewing, patients were randomly allocated without stratification using a computer‐generated random sequence. |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | Unclear risk | It is not described whether or not patients were blinded to which group they belonged to. |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | Unclear risk | Not described in the text. |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | Low risk | Interviewers masked to treatment group used computer assisted telephone interviews to assess outcomes 4, 10, and 52 weeks after randomization. |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | Follow‐up in the three groups was between 92% and 97%. |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | Authors reported: "...within the context of an intent‐to‐treat analysis using analysis of covariance (ANCOVA) with adjustment for baseline values..." |
| Selective reporting (reporting bias) | Unclear risk | The outcomes described in the methodology were: symptoms (back pain, leg pain, numbness and tingling), back specific functional status (Modified Roland Morris Questionnaire), disability (number of days spent in bed, home from work or school, or with reduced activity according to data from National Health Interview survey), satisfaction with the overall treatment, well being (SF‐12 Physical and Mental Health summary scales), utilization of health care services covered by HMO and cost (data from health maintenance organization ‐HMO‐), utilization of services not covered by HMO, use of medications and practice of aerobic exercise in the last week. The study did not report or reported partial data in 3 of 10 outcomes. Wellbeing is not reported for the 1 year follow‐up. The hospitalizations were not recorded for the 1 year follow‐up period. The use of medication is reported only for the follow‐up in the week 4. |
| Other bias | Unclear risk | Differences in adherence to exercise is unclear among the three groups. |
| Similarity of baseline characteristics? | Low risk | There were no significant differences among the 3 treatment groups for any of the baseline characteristics measured: age, gender, educational status, white ethnical group, family income, employment status, quality of life (SF 12), duration of pain, hospitalizations for back pain, back surgeries, previous massage or acupuncture, > 90 days in LBP in the last 6 months, radiation of the pain, Roland Disability scale score, > 1 day work‐loss day due to LBP in the past month, > 7 days of restricted activity due to LBP in the last month, medication in the past week, taking narcotics of analgesics and satisfaction with overall care. |
| Co‐interventions avoided or similar? | Low risk | Exercise at home was recommended in all groups. "Medication use by the acupuncture and massage groups did not differ from each other but was significantly below that in the self‐care group (P>0.05)". "In patient who received acupuncture, other commonly used therapies were infrared or other lamp heat (82% of patients), cupping (66%), and electrostimulation of the needles (51%)". "A mean of 12 needles (range, 5‐16) were inserted at each visit, with significant differences among acupuncturists (P,.001)". "Acupuncturists recommended exercise for about half of their patients, usually stretching, walking, or swimming". "Massage therapists recommended exercise, typically stretching, at the conclusion of 64% of initial visits. Most massage therapists (59%) also used “body awareness” techniques to help clients become more aware of their physical and kinaesthetic sensations, including potential early warning signals of injury". |
| Compliance acceptable? | Low risk | Ninety‐four percent of patients in the acupuncture group and 95% in the massage group visited their assigned provider and made a mean (SD) of 8.0 (2.4) and 8.3 (2.3) visits, respectively. Visits to massage therapists and acupuncturists averaged approximately 1 hour. |
| Timing outcome assessments similar? | Low risk | Yes: baseline, 4 weeks, 10 weeks and 1 year. |
Cherkin 2011.
| Methods | Country: USA. Funding: National Institute of Health's National Center for Complementary and Alternative Medicine (NCCAM). Blinding: care providers were not blinded to the intervention. Study personnel assessing trial outcomes were blinded to study assignment. Conflict between protocol and final published paper (Cherkin 2011) regarding the participants: Protocol: participants were called to be informed about the type of Massage they would receive. Full published article: participants knew whether they received massage but were blinded to type. Recruited: 9127 invitations and evaluated 1161 responses; 402 persons (35%) were eligible and were randomly allocated. Randomized: 402 persons (35%) were eligible and were randomly allocated. Pre‐programmed computer‐generated sequence of blocked random numbers for each therapist to assign the participant. 401 participants assigned to relaxation massage (n = 136), structural massage (n = 132), or usual care (n = 133). Duration of pain: > 1 year in 77%, 72% and 78%. Followed: follow‐up analysis, structural massage:
Follow‐up analysis, relaxation massage (RM):
Usual care (n = 133). Follow‐up analysis, control:
Analysis: analyses were conducted by using regression through generalized estimating equations (12) with an independent working correlation structure and robust SE estimates taking into account multiple outcomes per participant. Follow‐up times were treated as categorical variables using dummy variables for each treatment, each time point, and all 2‐way interactions between follow‐up time and treatment. Adjusted models included baseline covariates that were prespecified, were imbalanced at baseline (that is, potential confounders), or were associated with a primary outcome (that is, precision variables): age, group, sex, baseline Roland Morris Disability Questionnaire (RMDQ) and symptom bothersomeness scores, education level, body mass index, type of work, original cause of back pain, > 7 days of reduced activities because of back pain, and medication use in the previous week. The adjusted analysis as the primary analysis was prespecified. For continuous and binary outcome measures, the linear and modified Poisson regression were applied, respectively, with robust SEs. Modified Poisson regression allows estimation of relative risks for non‐rare outcomes using Poisson regression and corrects the misidentification of the variance using robust SEs in a generalized estimating equation framework. To control for multiple comparisons, the least‐significant‐difference approach was used, in which pairwise treatment comparisons were evaluated at a given time only if the overall omnibus P value was statistically significant at 0.05. Mean differences, 95% CIs and omnibus P values for treatment group effect and pairwise significance were presented. To assess effects of individual providers on the RMDQ outcome, an adjusted mixed‐effects model with a random intercept for each provider was fitted by using only data from the 2 massage groups. The intraclass correlation coefficient was calculated to quantify the degree of variability due to providers relative to the overall variability of the outcome. |
|
| Participants | Population: group health members with in‐plan visits of the Puget Sound region of western Washington, between 20 and 65 years of age with non‐radicular CLBP of mechanical origin (as opposed to infectious, neoplastic, or inflammatory causes). Settings: 27 licensed therapists' offices. Funding: to minimize disappointment (and possibly losses to follow‐up), participants assigned to UC (continued usual care) received USD 50. Mean age: age (SD). Structural massage 46 (12), relaxation massage 47 (11), controls 48(11). % Female: structural massage 66%, relaxation massage 65%, controls 62%. Ethnicity: white race 86% in structural massage, 87% in relaxation Massage, 86% in controls. Work status:
Pain duration:
Previous surgery: patients with surgery in the previous 3 years were excluded. No further details are given about the surgery in previous years for the included participants. Diagnoses: back pain for > three months without 2 or more pain‐free weeks. Original cause of LBP unknown: 23% in SM, 13% in RM and 14% in controls. Pain below knee 11%, 15% and 19% respectively. No further details about other causes or related conditions. |
|
| Interventions | Massage technique: both techniques consisted of visits lasting 50 to 60 minutes. Structural massage (it included Clinical Massage and Movement Re‐education techniques). Relaxation massage: therapists were given time limits for each body region, including 7 to 20 minutes on the back and buttocks. Control: usual care participants received no special care, but were paid USD 50. Experience of therapist: care providers were 27 licensed massage therapists with at least 5 years of experience.
|
|
| Outcomes | * used in the meta‐analyses: Measured at baseline, in the short‐term (10 weeks)*, in the long term (26 and 52 weeks)*: a. Pain: none. b. Function: Roland Morris Disability Questionnaire (RMDQ)*. c. Adverse effects: Five of 134 (4%) relaxation massage recipients and 9 of 131 (7%) structural massage recipients reported adverse events possibly related to massage, mostly increased pain. One event in the structural massage group (nausea, shortness of breath, and chest pain) was classified as serious and considered unrelated to treatment. d. Other measures:
Measured immediately after: none. |
|
| Notes | Results: a. Pain: No scales were measured. b. Function: RMDQ, (range from 0 to 23 points, lower means "less limitations due to the back pain", "better"). From baseline [Mean] (SD) to short term week 10 [Mean Value] (95% CI) to long term week 26 [Mean Value] (95% CI) to long term week 52 [Mean Value] (95% CI).
c. Well‐being (physical and mental health Short Form‐12 Health Survey) (range from 0 to 100, where a zero score indicates the lowest level of self‐perceived health measured by the scales and 100 indicates the highest level. It tracks how patient feel affected by the medical condition to be able to do usual activities work outside the home and housework, climbing stairs, recreational activities, emotional self‐perception and social interaction). From baseline [Mean] (SD) to short term week 10 [Mean Value] (95% CI) to long term week 52 [Mean Value] (95% CI). Physical Short Form‐12:
Mental Short Form‐12:
Authors' conclusions: massage therapy may be effective for treatment of chronic back pain, with benefits lasting at least 6 months. No clinically meaningful difference between relaxation and structural massage was observed in terms of relieving disability or symptoms. In summary, our findings suggest that both relaxation massage and structural massage are reasonable treatment options for persons with chronic LBP. The findings may suggest a relative advantage for relaxation massage because it is based on techniques that are taught in almost all massage schools and is thus more readily accessible and slightly less expensive than structural and other more specialized forms of massage, which require additional training. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The protocol describes a two stage randomization procedure. The first stage was to randomize to massage group and control. The second to randomize the type of treatment, by computer‐generated sequence of blocked random numbers for each therapist to assign the participant, with equal probability to structural or relaxation massage. |
| Allocation concealment (selection bias) | High risk | Protocol: the randomization database was built to ensure that treatment allocation cannot be viewed prior to randomization and cannot be changed after randomization. Published trial: a research specialist (RS) provided the baseline questionnaire, asked participants about preferred location and provided the participant's contact information to the therapist and specified which type of massage the participant was to receive. |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Participants knew whether they received massage but were blinded to type of massage. However, massage and control groups were not indistinguishable for the patients and the success of blinding was not tested among the patients. |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Therapists were not blinded to the type of massage that they provided. |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | High risk | Protocol: all interviews were conducted using computer assisted telephone interviews (CATI). Patients reporting the outcomes were not blinded. However, the outcomes are subjective and self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | Follow‐up was done for > 90% of the randomized patients, except for the controls at the 52 week that was 87%. Provided reasons for missing data. |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | Adequate methods of imputation for missing data. All patients were analyzed in the group to which they were allocated by randomization |
| Selective reporting (reporting bias) | Low risk | Roland Morris Questionnaire and Short Form‐12 Health Survey were completed as planned in the protocol. |
| Other bias | Low risk | No other bias was identified. |
| Similarity of baseline characteristics? | Low risk | Figures are similar for age, gender, marital status, body mass index, educational level, income, physical demands at job, duration of LBP, medication use in past week, SF‐12 and RMQ. |
| Co‐interventions avoided or similar? | High risk | Structural and relaxation massage groups received a predefined list of 7 exercises, 6 of which were common to both treatments. However, control group did not receive this information. Besides, in the relaxation massage group, therapists could provide a compact disk of a 2.5‐minute relaxation exercise to be done at home, while the structural massage group was advised to continue with psoas stretch. It is not possible to measure the impact of any of these differences over the results. |
| Compliance acceptable? | Low risk | Study treatment visits were: Structural massage: 8 to 10 visits: 116 (88%). 0 to 7 visits: 16 (12%). Relaxation massage: 8 to 10 visits: 126 (93%). 0 to 7 visits: 10 (7%). |
| Timing outcome assessments similar? | Low risk | 10, 26 and 52 weeks for all groups. |
Eghbali 2012.
| Methods | Country: USA. Funding: Isfahan University of Medical SciencesBlinding. Recruited: 50 patients. Randomized: 25 to intervention group and 25 to control group. Followed: 50. Analysis: descriptive and inferential statistics, including independent t‐test and Chi² test, were used to analyze the data. |
|
| Participants | Population: the study population consisted of all nurses working in hospitals affiliated to Isfahan University of Medical Sciences. Nurses were included if they had LBP, chronic non‐specific back pain diagnosed by a neurosurgery specialist for > 3 months, healthy feet without injury or damage, and willingness to participate in the study. Settings: every day, the researchers referred to Al‐Zahra and Kashani Hospitals to carry out the interventions in the morning from 8 to 12 and in the afternoon from 2 to 6, respectively. Funding: patients were all nurses working in hospitals affiliated to Isfahan University of Medical Sciences, the same institution that approved and supported the study. Mean age: the mean (SD) age of subjects was 42.28 (8.02) years in the test group and 39.48 (5.73) years in the control group. Ethnicity: not described. The study was done in Isfahan, Iran. Work status: mean (SD) work experience was 17.68 (8.06) in the test group and 15.72 (5.79) in the control group. Pain duration: > 3 months. Onset (weeks): not described. Previous surgery: not described. Diagnoses: not described. Exclusion criteria: subjects were excluded if they had participated in another clinical research during the past 3 months, had an experience or knowledge of reflexology, were pregnant or lactating, used other methods of complementary therapy during the study, or had a vascular disease, thrombophlebitis or diseases such as urinary tract infection or kidney stones (with pain in the lower back). They were also excluded if any physical damage, making the subjects unable to continue their participation, was made or if they used new medical treatments (new drugs effective on pain, physical therapy or other methods). |
|
| Interventions | Massage technique: reflexology to the intervention group and massage to feet and low back in the control group. The intervention was applied as 6 forty‐minute sessions of interventions, i.e. twice a day, three days a week for two weeks. Experience of therapist: after learning the technique under the supervision of a qualified reflexology expert, the researchers performed the intervention. Interventions in the test and control groups were conducted during the first and second two weeks, respectively.
|
|
| Outcomes | Measured at baseline: Numerical Analogue Scale for pain. Measured immediately after: Numerical Analogue Scale for pain. Measured in the short‐term: none. Measured in the long‐term: none. |
|
| Notes | Pain intensity (PNRS (Pain numeric rating scale) (range 0‐100, lower means "better"). Results:
Authors' conclusions: recognizing the impact of reflexology on chronic back pain makes it possible to use this technique as a complementary intervention with other treatments for complicated conditions such as back pain in which patients do not usually benefit from other methods. In addition, reflexology can be easily taught to people in order to take effective steps to reduce chronic pain. The treatment team can also take advantage of this method for treating LBP patients. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method for generating random numbers is not described. After participants were recruited they were randomly numbered. Then, individuals with odd and even numbers were assigned to treatment or control interventions respectively. |
| Allocation concealment (selection bias) | Unclear risk | Individuals with odd and even numbers were assigned to each of the groups, respectively. The independence of the person performing the allocation to each groups is not described. |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | Unclear risk | The patients and the questioner were blinded to the groupings. However, it is unclear how this was done. |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Providers were not blinded. Interventions in the test and control groups were conducted during the first and second two weeks, respectively. There are no descriptions about the strategies that were taken to blind the outcome providers to the fact that patients were distributed in different weeks. |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | Unclear risk | Outcome assessors (questioner) was blinded to the groupings. However, it is unclear how the patients were blinded and the outcomes are subjective. |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | The study does not mention any drop‐outs |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | The patients were analyzed in the same group that they were assigned. |
| Selective reporting (reporting bias) | Low risk | The study assessed and reported pain as it was intended in the objectives and methodology. |
| Other bias | Unclear risk | The study population consisted of all nurses working in hospitals affiliated to Isfahan University of Medical Sciences, the same school approving the study. |
| Similarity of baseline characteristics? | Low risk | The study reported that there were no significant statistical differences between the two groups when the age, gender, pain characteristics, and pain scores were compared. |
| Co‐interventions avoided or similar? | Low risk | Patients were excluded if other methods of complementary therapy during the study or if they used new medical treatments (new drugs effective on pain, physical therapy or other methods). |
| Compliance acceptable? | Unclear risk | The compliance of the participants is not described, either in the intervention or control group. |
| Timing outcome assessments similar? | Unclear risk | The time and the strategies to control the timing of outcome assessments in both groups are not well described. |
Farasyn 2006.
| Methods | Country: Belgium. Funding: not reported. Blinding: outcome assessor for Pressure Pain Thresholds (PPT) measurement. Recruited: 170. Randomized: 60. Followed: 60. Analyses: baseline: ANOVA for continuous variables and Chi² for categorical variables, including post‐hoc comparisons with LSD‐tests. Owestry Disability Questionnaire (ODQ) and Visual Analogue Scale (VAS) scores were analyzed by Wilcoxon‐tests. | |
| Participants | Mean age: 43 in placebo group, 41 in treatment group and 40 in control group. % female: 55% males in placebo group, 65% males in treatment group and 56% males in control group. % White: not reported. Work status: not reported. Pain duration: between three and 12 weeks (subacute Low Back Pain (LBP)). Previous surgery: not reported. Diagnoses: non‐specific LBP. | |
| Interventions | Massage technique: roptrotherapy: 30‐minute deep cross‐friction massage with the aid of a myofascial T‐bar made of bronze (neutral material to skin) to use by hand and to contribute to the compression force by their weight (0.8 kg), within the threshold of pain that was tolerable, applying a compressive force of 5 to 10 kg/cm². One session.
Experience of therapist: not reported. Endermology (placebo): 30‐minute session of endermology to account for the touching effects of massage, a device with a suction head was adjusted to a minimal but continuous section power and applied across the middle and lower back (T6‐L3) and buttocks. Groups:
|
|
| Outcomes | * used in the meta‐analyses: When measured: one week after session*. a. Pain: PPT. Pain VAS in mm (before and one week after the treatment*). b. Function: Oswestry Disability Questionnaire (ODQ)*. c. Overall improvement: no. d. Patient satisfaction: no. e. Adverse events: not reported. f. Costs: not reported. g. Work‐related: no. |
|
| Notes | Results: a. Pain (VAS):
b. Function (Oswestry):
Authors' conclusions: "The results of this study provide direct evidence that one deep cross‐friction massage with the aid of copper myofascial T‐bar applied to the lumbo pelvic region, can reduce effectively local pressure pain sensitivity, pain rating and disability in patients with subacute non‐specific LBP." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear from text. Done by an statistician. A different article that resembles this study described this procedure: Journal of Musculoskeletal Pain, Vol. 15(1) 2007: The group was randomly assigned, blocked per 5 subjects. |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | Unclear risk | Not reported. |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | Unclear risk | Not reported. |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | High risk | The outcome assessor was blinded only for the PPT outcome. With regards to pain and disability, there was no blinding of outcome assessors. |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | No dropouts. |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | All patients were analyzed in the group to which they were allocated by randomization. |
| Selective reporting (reporting bias) | Unclear risk | Pain: PPT and VAS and Back specific functional status measured by standard Oswestry Disability Questionnaire were all reported at 1 week. |
| Other bias | Unclear risk |
|
| Similarity of baseline characteristics? | High risk | The following variables were analysed: age, gender, body mass index, weeks of onset of LBP, PPTs measured at the level of the Erector spinae of L1 & L3, and Gluteus maximus, ODI. However, the baseline VAS was much higher in the T group than in the C group, and the Oswestry was much higher in the T group than in the C group. |
| Co‐interventions avoided or similar? | Unclear risk | Unclear from text. |
| Compliance acceptable? | Low risk | All patients received only one session. |
| Timing outcome assessments similar? | Low risk | Reported as measured in all patients at baseline and follow‐up. |
Field 2007.
| Methods | Country: USA. Method of randomization: not described. Methods of recruitment: not described. Funding: National Institute of Mental Health Research Scientist Award and Research Grant. Blinding: not blinded. Recruited: not described. Randomized: 30. Followed: not described. Analyses: repeated measures ANOVA. | |
| Participants | Mean age: 41. 16 male, 14 female. 67% Caucasian, 9% Hispanic, 16% African American, 8% Asian. Work status: not reported. Pain duration: at least six months. Previous surgery: not reported. Diagnoses: Chronic Low Back Pain (CLBP) co‐morbidity: not reported. | |
| Interventions | Massage to the entire back, legs and knees, using a Biotone oil, two 30 minute sessions per week for five weeks Experience of therapist: not reported Groups:
|
|
| Outcomes | When measured: pre and post last day (immediately after the end of the 10 sessions*) a. Pain: Visual Analogue Scale (VAS)*. b. Function: trunk Range of Motion (ROM). c. Depression: Profil e of Mood State s Depres sion Scale (POMS‐D). d. Stress: State Anxiety Inventory (STAI). e. Sleep scale: VAS. f. Adverse events: not reported. g. Costs: not reported. h. Work‐related: level of job productivity 0 to 5. | |
| Notes | Results: Pain
Authors' conclusions: These data, nonetheless, suggest that massage effectively reduces pain, sleep disturbances and the anxiety and depressed mood states associated with lower back pain. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of randomization is not described. |
| Allocation concealment (selection bias) | Unclear risk | The method of allocation concealment is not described. |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Patients were not blinded. |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Providers were not blinded. |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | High risk | Not described, but since patients were not blinded and all outcomes are subjective and self‐reported, there is high risk of detection bias. |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Unclear risk | Not described. |
| Selective reporting (reporting bias) | Unclear risk | Pain (Visual analogue scale (VAS) ‐ VITAS) was reported in a table. Absenteeism measure (Ordinal scale of productivity 0‐5) was described in the text has showing no differences. |
| Other bias | Low risk | No other bias was identified. |
| Similarity of baseline characteristics? | Unclear risk | Unclear from text. There are no tables about it. |
| Co‐interventions avoided or similar? | Unclear risk | Unclear from text. Not described. |
| Compliance acceptable? | Unclear risk | Unclear from text. Two 30‐min massage therapy sessions per week over 5 weeks. And 30‐min sessions at home twice a week for 5 weeks and to keep a log on the times they spent in relaxation therapy. No results were published about what happened at the end of the 5 week study. |
| Timing outcome assessments similar? | Low risk | Five‐week study. |
Franke 2000.
| Methods | Country: Germany Design: 2 x 2 factorial design. 190 patients were randomized. Methods of recruitment: not mentioned. Period of study: 14 months, until the end of 1997. All medications needed to be discontinued before the beginning of the study protocol. Follow‐up: until end of sessions. Drop‐outs: 11 patients (5.8%). | |
| Participants | Settings: study conducted in Bad Andersheim City, Park Rehabilitation Clinic Duration of pain: > one year. Participants needed to speak German to be included. Age: 25 to 55 years (45 ± 8.1), 61% male. Previous treatments: analgesics, anti‐inflammatory drugs, muscle relaxants, antidepressants. Most diagnoses included: lumbar disc prolapse without myelopathy, 28% LBP and 23% ischialgia. |
|
| Interventions | 1. Acupuncture massage according to Penzel: follow the rules of massage from Physical Medicine and of acupuncture from neural therapy according to Huneke and Quirotherapy Uses a manual metal roller for meridians treatment. Treats one unique point with a special vibrating instrument that stimulates the acupuncture point superficially (not needle insertion). 2. Teil massage (classic Sweedish massage (SM)). The objective is to tonify and defonify muscle structures by increasing circulation in the skin and muscle, decrease adhesions. 3. Individual exercises:
4. Group exercises same as individual exercises, but in group mode. Study groups: (1) + (3) (1) + (4) (2) + (3) (2) + (4) |
|
| Outcomes | Measured before and after the sessions: a. Pain: VAS (1 to 10 cm). b. Overall improvement: not measured. c. Function: Hanover Function Score Questionnaire for Low Back Pain (LBP) (FFbH‐R) 0 to 100%. d. Physical examination: lumbar flexion and extension (degrees). e. adverse events: not reported. f. Costs: not reported. g. Work‐related outcomes: not measured. |
|
| Notes | Authors' conclusions: the observed effect sizes with acupuncture massage are promising and warrant further investigation in replication studies.
Acupuncture massage showed beneficial effects for both disability and pain compared with SM.
Marked improvement observed in Acupuncture massage + group exercise. Acupuncture massage improved function (with individual or group exercises). Classic massage did not change function.
Most decrease in pain occurred in the acupuncture massage + individual exercise group. Acupuncture massage (with individual or group exercise) reduced pain.
Mean difference between acupuncture and classic massage groups: 7.0% (function) and 0.8cm Visual Analogue Scale (VAS). ANOVAS: Acupuncture massage is more effective than SM for function (P = 0.008) and for pain (P = 0.038) Both exercises groups (individual or in group) are not statistically significantly different for function (P = 0.55) or for pain (P = 0.55). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number tables. |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes. |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Not feasible for physiotherapists and patients; not possible for investigator due to capacity problems in routine care of the hospital. |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Not feasible for physiotherapists and patients; not possible for investigator due to capacity problems in routine care of the hospital. |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | High risk | Not mentioned, but because the outcomes were subjective and self‐reported by patients, there is high risk of detection bias. |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | Only 11 patients (5.8%) abandoned the study protocol. |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | High risk | 3 out of 109 patients changed treatment on own request and were unwilling to complete the questionnaires. A sensitivity analysis was carried out to estimate the robustness of the results. For this reason missing post‐treatment values were replaced by the worst values found between the 10th and 90th percentile of the sample. |
| Selective reporting (reporting bias) | Unclear risk | Both outcome variables were presented at the end of the study. Pain: VAS (1 to 10cm) and Function: Hanover Function Score Questionnaire for LBP (FFbH‐R) 0 to 100%. |
| Other bias | Low risk | No other bias was identified. |
| Similarity of baseline characteristics? | High risk | Due to some differences between groups at baseline, groups‐standardized outcomes were used for analysis. |
| Co‐interventions avoided or similar? | Low risk | All medications needed to be discontinued before the beginning of the study protocol. |
| Compliance acceptable? | Low risk | 11 patients (5.8%) abandoned the study protocol. |
| Timing outcome assessments similar? | Low risk | Study period was 14 months. The study had to be finished prior to the intended sample size due to remarkable changes within the German system of welfare regarding rehabilitation. |
Geisser 2005.
| Methods | Country: USA. Funding: National Institute of Health. Blinding: outcome assessor. Recruited: 100 patients. Randomized: 100 patients. Followed: 72 patients. Analyses: MANOVA and MANCOVA for comparisons between groups. | |
| Participants | Settings: University of Michigan Spine Program. Mean age: 40.7 years old. 41% female. 85% white. 34% not working due to pain. Pain duration: mean 76.9 months. 18% had previous surgery. Diagnoses: not reported. |
|
| Interventions | Massage: muscle energy technique (MET) weekly for five weeks. Experience of therapists: physical therapist with 12 years postgraduate training in manual medicine. * post‐treatment scores. (N = randomized, completed the study).
|
|
| Outcomes | * used in the meta‐analyses. Measures taken at baseline, then at the end of the 5th session (last visit). a. Pain: a1) pain rating scales (from McGill Questionnaire) and a2) Visual Analogue Scale (VAS)*. b. Function: b1) QBPDS* and b2) Interference subscale of the Multidimensional Pain Inventory (MPI). c. Overall improvement: not measured. d. Patient satisfaction: four questions with seven‐point Likert scale. f. Adverse events: not measured. g. Costs: not reported. h. Work‐related: not measured. |
|
| Notes | a. Pain (VAS):
b. Function (Quebec):
c. Satisfaction with overall therapy:
Authors' conclusions: "massage therapy with specific adjuvant exercise appears to be beneficial in treating chronic low‐back pain. Despite changes in pain, perceived function did not improve". |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear from text. "Participants were randomly assigned to 1 of 4 treatment conditions. To obtain equal numbers of patients in each group, the randomization order was determined prior to the study" |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | Low risk | "The treating therapist ...attempted to keep patients blind to their group assignment". Group 2: "sham manual therapy with specific adjuvant exercise (sham MT‐SE)". Group 4: "sham manual therapy and nonspecific exercise (sham MT‐NE)". |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | "The treating therapist was not blind to the treatment group of the patient…" |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | Low risk | "...the principal investigator, who was blind to the treatment condition of the patient". The outcomes are subjective, but the patients were kept blinded to the group they were assigned. |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | Drop outs: 5 and 4 for each group. Reasons were not given. "The rate of attrition in the study was 28%". patients who dropped out of the study displayed significantly higher levels of pain and disability, were more likely to be receiving compensation, and were more likely to be male. |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | High risk | They analysed only 72 of the 100 randomized patients. No method for inputation of missing data was used. |
| Selective reporting (reporting bias) | Unclear risk | All outcome variables were presented. PAIN: VAS, MPQ, DISABILITY: QBPDS, WELL BEING: Interference subscale of the Multidimensional Pain Inventory (MPI), SATISFACTION: 1) satisfaction with the feedback provided by the therapist about their condition; 2) satisfaction with the amount of pain relief from therapy; 3) overall satisfaction with therapy; and 4) overall satisfaction with the therapist. |
| Other bias | Low risk | No other bias was identified. |
| Similarity of baseline characteristics? | High risk | Although there are some big differences in the baseline characteristics presented in table 1, the authors conclude: "Chi‐square tests and ANOVA were used to compare the groups… no significant group differences were observed, although there was a trend for patients in the sham MT‐NE group to be older" Patient's age in the sham MT‐NE group was 46.3, while in the other groups it was: 39.3; 38.7 and 36.5." "According to the authors: "none". However, even though they were not statistically significant, the authors wisely used multivariate analyses and adjusted for baseline characteristics." |
| Co‐interventions avoided or similar? | Unclear risk | 1. All patients were allowed to continue their use of pain medications, but were asked to not change their usage during the course of the study. 25 took no prescription medication for pain, 48 took NSAIDs, 35 took opioids, 25 were on antidepressants (for depression, analgesia, sleep disturbance or a combination of all these), 12 took antispasmodic medication and 8 were on anxiolytics and 6 took anticonvulsants. 2."...and were also given exercises specifically designed to treat identified musculoskeletal dysfunctions". 3. Examples of these exercises included: 1) quadriceps stretch; 2) double or single knee to chest stretch; 3) sitting hamstring stretch; and 4) prone on elbows. In addition, patients in this group were asked to perform aerobic exercise 3 times per week. Participants were free to choose how they performed aerobic exercise. 4. "...patients were asked to do stretches and/or self‐corrections twice daily (usually 10 repetitions each time). Patients were asked to hold each stretch for 30 seconds. |
| Compliance acceptable? | Low risk | Not with massage, only with exercise. |
| Timing outcome assessments similar? | Low risk | After 5th session (weekly sessions). "...Some patients rescheduled visits, prolonging the time between the first and last visit." It seems to be the same for both groups. |
Hernandez‐Reif 2001.
| Methods | Country: USA. Funding: National Institutes of Mental Health and Johnson & Johnsons. Method of randomization: not described. 24 were randomized. Recruitment of patients: self‐referred. Study conducted in the USA. Period of study: not described. Follow‐up: post sessions and last day of sessions. |
|
| Participants | Settings: not described. Average age: 39.6 years. 54.1% women. 67% Caucasians, 8% Hispanic, 17% African American and 8% Asian. Duration of pain: at least six months. Previous treatments: not described. |
|
| Interventions | 1. 30‐minute massage therapy sessions per week over five weeks by trained massage therapist. Each session started with the participant in the prone position resting the ankles on a small cushion. The massage consisted of the following techniques applied to the entire back at a level tolerant to the subject: 1) moving the flat of the hands across the back, 2) kneading and pressing of muscles and 3) short back and forth rubbing movements to the muscles next to the spine and later to the hip bones. The following techniques were administered to the legs: 1) long gliding strokes to the entire leg, 2) kneading and moving the skin in the thigh area, 3) pressing and releasing, and back and forth rubbing movements to the area between the hip and the knee and 4) short rubbing movements to the small muscles around the knees. In the supine position with a bolster under the knee, subjects received: 1) long gliding strokes and kneading of the neck muscles, 2) moving the flats of the hands across the abdomen, 3) pinching and moving the skin on the abdomen in all directions and 4) kneading the muscles that bend the trunk forward. Then, to the entire leg: 1) stroking, 2) kneading followed by pressing and releasing the anterior thigh region, 3) slow flexing of the thigh and knee, and 4) slow pulling of both legs. 2. Relaxation therapy: (to control for potential placebo effects and the effects of increased attention given to the massage subjects): The relaxation group was instructed on progressive muscle relaxation exercises tensing and relaxing large muscle groups starting with the feet and progressing to the calves, thighs, hands, arms, back and face. The subjects were asked to conduct these 30‐minute session at home twice a week for five weeks and to keep a log. | |
| Outcomes | * used in the meta‐analyses. Measured before and after each session*. a. Pain measures:
b. Function: none. c. Adverse events: not reported. d. Other measures:
|
|
| Notes | Authors' conclusions: massage therapy is effective in reducing pain, stress hormones and symptoms associated with CLBP. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Unclear risk | Not described. |
| Selective reporting (reporting bias) | Unclear risk | The pain was measured with the McGill and VITAS questionnaires. Both were reported as mentioned in the methodology: First day (pre and post), last day (pre and post). |
| Other bias | Low risk | No other bias was identified. |
| Similarity of baseline characteristics? | Low risk | Baseline characteristics in Table 1. No major differences. |
| Co‐interventions avoided or similar? | Unclear risk | Not described. |
| Compliance acceptable? | Unclear risk | Not described. |
| Timing outcome assessments similar? | Low risk | The assessments were made before and after the sessions on the first and last days of the 5 week study. |
Hsieh 2004.
| Methods | Country: Taipei, Taiwan, China. Funding: not reported. Recruited: 250. Randomized: 146. Followed: post treatment = 146; at six months = 121. Analyses: independent t‐test for continuous variables; Chi² test for categorical variables; Wilcoxon rank sum test for comparisons between the two treatment groups; Wilcoxon sign‐rank test for changes before and after treatment. | |
| Participants | Settings: regional.
orthopedic hospital in the Kaoshiung, Taiwan area, which offers routine orthopedic operation and rehabilitation of physical therapy. Mean age: acupressure group: 47.6; physical therapy (control) group: 47.6. Gender: acupressure group: 30 male, 39 female; physical therapy (control) group: 40 male, 37 female. Ethnicity: not reported (possible that all were Chinese patients). Work status: (n) acupressure versus PT. Labour 15 versus 10; office 21 versus 31; householder 21 versus 19; other 12 versus 17. Pain duration: 67% of patients over 6 months (range one month to over 10 years). Previous surgery: not reported. Diagnoses: not detailed. |
|
| Interventions | Massage technique: six acupressure sessions over a four‐week period, lasting approximately 15 minutes (no more details were reported). Experience of therapist: performed by a designed senior therapist to render uniform technique and to ensure consistent experience to all patients. Groups:
|
|
| Outcomes | * used in the meta‐analyses. Measured at baseline, then immediately after 6 sessions of treatment*, and at the six‐month follow‐up*: a. Pain:
b. Function: not measured. c. Adverse events: no adverse direct of side effects were reported in the acupressure group. d. Other measures:
|
|
| Notes | a. Pain score (range 0 to 45, where zero is no pain):
b. SF‐PQ: pain descriptors: significant difference between groups. Post treatment: throbbing, shooting, stabbing, sharp, cramping, aching, sickening, punishing‐cruel; At 6 month FU: cramping, aching, tiring‐exhausting. Authors' conclusions: "Our results suggest that acupressure is another effective alternative medicine in reducing low‐back pain, although the standard operating procedures involved with acupressure treatment should be carefully assessed in the future." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random allocation number generated from a random table. |
| Allocation concealment (selection bias) | Low risk | The random allocation numbers were managed by an independent research assistant and not decoded until the intervention was assigned. |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | Unclear risk | Not described. Not possible to define whether the Index and control groups were indistinguishable for the patients (physical therapy or acupressure). No sham therapy for acupressure. |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | Unclear risk | Not described. Not possible to decide whether the Index and control groups were indistinguishable for the care providers. |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | High risk | The research assistant who conducted the follow‐up interviews by telephone was informed beforehand not to ask the participant about the details of intervention to keep blind to the intervention group as much as they can do. For SF‐PQ, each participant was requested to answer the inventories, but patients were not blinded. Since all outcomes are subjective and self‐reported, there is high risk of detection bias. |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | Low risk for the follow‐up after 1 month. Drop outs after 6 months were 18% and 15% of the initial samples of acupressure and physical therapy groups, respectively. |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | For the short‐term follow‐up there was low risk because all patients were analyzed in the group to which they were allocated by randomization. |
| Selective reporting (reporting bias) | Unclear risk | Short‐Form Pain Questionnaires (SF‐PQ) was reported for pre and post treatment pain scores as mentioned in the methodology. |
| Other bias | Low risk | No other bias was identified. |
| Similarity of baseline characteristics? | High risk | The duration of LBP episodes for these patients ranged from 1 month to over 10 years. This was not analysed in Table 3. |
| Co‐interventions avoided or similar? | Unclear risk | Unclear from text. |
| Compliance acceptable? | Low risk | Methodology: "Both groups received six treatment sessions over a 4‐week period". Not described in detail in the results. |
| Timing outcome assessments similar? | Low risk | Yes. |
Hsieh 2006.
| Methods | Country: Taiwan, China. Funding: none. Recruited: 188. Randomized: 129. Followed: 122 at one month; 109 at six months. Analyses: for comparisons between groups: 1) Wilcoxon rank sum test (Roland and Morris), jack‐knife method to calculate 95% confidence intervals (CIs); 2) ANCOVA for VAS and Oswestry, adjusted for pretreatment score alone or together with other possible baseline variables such as duration of LBP; 3) logistic regression to estimate the odds ratio of having significant disability as measured by Roland and Morris; 4) cumulative logit models to the ordinal property of disability defined by Oswestry. | |
| Participants | Settings: outpatients of a specialist orthopaedic clinic in Kaoshiung, Taiwan, which offered standardised physical therapy. Mean age: 50.2 in the acupressure group; 52.6 in the physical therapy group. Gender: 41% female. Ethnicity: not reported, (assume all Chinese). Work status: N (%) acupressure versus PT. Household keeper 18 (28) versus 16 (25); office worker 17 (27) versus 8 (12); heavier labour 9 (14) versus 8 (12); other 20 (31) versus 33 (51). Pain duration: median (range) time since onset of pain (years): acupressure group: 3.3 (0.2 to 33.3) versus physical therapy group: 1.6 (0.2 to 34.3) Median (range) length of latest pain period (months): acupressure group: 14.5 (0.02 to 360) versus physical therapy group: 12 (0.25 to 432) Previous surgery: none (inclusion criteria) Diagnoses: CLBP over four months by orthopaedic surgeon. |
|
| Interventions | Massage technique: acupressure six sessions within a month. Experience of therapist: one senior acupressure therapist delivered each session to ensure a consistent experience. No detail on time of experience.
|
|
| Outcomes | * used in the meta‐analyses: Measured at baseline, after six sessions of treatment* and at six months FU* a. Pain: VAS (01‐100)*. b. Function: 1. RMDQ (primary outcome) (range: 0 ‐ 24); 2. modified Oswestry disability questionnaire*. c. Overall improvement: Chinese version of the standard core outcome measures (degree of how bothersome). d. Patient satisfaction: as part of the core outcome measures: satisfaction of life with symptoms; satisfaction with previous treatment. f. Adverse events: not reported. |
|
| Notes | a. Pain (100 mm VAS):
b1. Function (Roland and Morris):
b2. Function (Oswestry):
c. Satisfaction of life with symptoms:
d. Days off work:
Authors' conclusions: "This study shows that acupressure is more efficacious in alleviating low‐back pain than is physical therapy, as measured by pain VAS, core outcome measures, Roland and Morris disability questionnaire and Oswestry disability questionnaire." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Pre‐determined random table. |
| Allocation concealment (selection bias) | Low risk | A research assistant independently randomized participants and they were randomly allocated to two arms. |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Patients were not blinded. |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Not possible to define whether the Index and control groups were indistinguishable for the care providers. |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | High risk | "The research assistant who did the post‐treatment and six month follow‐up interviews by telephone was also blind to pretreatment assessment and was told beforehand not to ask the participants about the details of the intervention in order to remain blind to the intervention as far as possible." "...assessor was blind to intervention group before analysis of data was complete". However the outcomes were subjective and self‐reported by the patients who were not blinded. |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | Drop outs after 1 month were 3% and 9% of the initial samples of acupressure and physical therapy groups, respectively. Drop outs after 6 months were 14% and 17% of the initial samples of acupressure and physical Therapy groups, respectively. Two patients swapped the group in each arm of the study. |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | Researchers substituted missing data for patients lost to follow‐up with baseline or posttreatment data by assuming no change since last contact. All patients were analyzed in the group to which they were allocated by randomization. |
| Selective reporting (reporting bias) | Unclear risk | Pain (VAS) and back‐specific functionality (RMDQ) were all reported at pretreatment, post‐treatment and at 6 months follow‐up |
| Other bias | Low risk | No other bias was identified. |
| Similarity of baseline characteristics? | Low risk | Table 1: age, gender, marital status, education level, occupation, time since onset of pain, length of latest pain period. |
| Co‐interventions avoided or similar? | Unclear risk | Unclear from text. |
| Compliance acceptable? | Unclear risk | Unclear from text. |
| Timing outcome assessments similar? | Low risk | Yes. |
Kamali 2014.
| Methods | Country: Iran. Funding: Vice‐Chancellery for Research Office, Shiraz University of Medical Sciences. Recruited: 30. Randomized: 30 to two groups (not stated but assumed 15 per group). Followed: 30. Analysis: paired t‐tests and independent sample t‐tests were run with a significance level of 0.05. |
|
| Participants | Population: patients with subacute or chronic non‐specific LBP. Settings: physical therapy centre of Shiraz University of Medical Sciences. Funding for participants: not described. Mean age: 33.96 ± 10.93 years. % female: 100%. Ethnicity: not described. Iran. Work status: not described. Pain duration: 9.68 ± 3.38 months. Previous surgery: excluded. Diagnoses: several conditions were excluded; nothing specific included. |
|
| Interventions | Massage technique: Group 1: massage (n = 15?). SM performed by physical therapists. 15 minutes a day for 10 days. Prescribed exercise too. Group 2: physical therapy (n = 15?). Received electro therapy, TENS, ultrasound and exercise. Unclear how long each session was or how many sessions provided. |
|
| Outcomes | Measured at baseline and immediately after: a. Pain: pain intensity (Numerical Rating Scale). b. Function: functional disability (ODI). c. Adverse events: not reported. d. Other measures:
Measured in the short‐term: none. Measured in the long‐term: none. |
|
| Notes | a. Pain intensity (Numerical Rating Scale, lower means "better"):
b. Function (ODI, lower means "better"):
c. Function (Flexion ROM, lower means "worse")
Given the large differences in baseline between groups, the results of this study have not been included in the meta‐analyses of this current review. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of randomization was not described. |
| Allocation concealment (selection bias) | Unclear risk | The method of allocation was not described. |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Patients were not blinded to the group. |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Providers were not blinded to the group. |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | High risk | Assessors were blinded to the group but the patients were not. Two of the tools were self‐report and the participants likely knew which group they were in. This could have introduced bias into the study. Only one was objective (external assessor). The blinding of these assessors likely had little impact on the bias in the study. |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Unclear risk | It was not reported whether there were dropouts or not. |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Unclear risk | It was not described. |
| Selective reporting (reporting bias) | Low risk | All primary outcomes were reported according to the methodology. |
| Other bias | Low risk | No additional bias found. |
| Similarity of baseline characteristics? | High risk | No details provided about baseline characteristics. |
| Co‐interventions avoided or similar? | High risk | Medication or other interventions were not clearly reported. Exercise seems to be different in both groups. |
| Compliance acceptable? | Unclear risk | No data about compliance. |
| Timing outcome assessments similar? | Unclear risk | It is unclear whether it was similar or different between the groups. |
Kumnerddee 2009.
| Methods | Country: Thailand. Funding: the study was supported by The Institute of Thai Traditional Medicine by sending qualified masseurs to perform Thai massage. The trial author wishes to thank Dr. Ukrit Jirapatarasuntorn for assistance in pain threshold evaluation. Recruited: 26 recruited; 8 excluded. The on‐service male military personnel from the 4th Battalion, 1st Regiment, King‐own Bodyguard were enrolled for the study. The aim, including procedures of the massage and acupuncture was explained and also demonstrated to all volunteers. Randomized: 18. Followed: 17; 1 dropped out of the massage group. Analysis: mean and SDs for descriptive statistics. Paired t‐tests were used to compare change scores from baseline to follow‐up. Unpaired t‐test were used to compare scores between groups. |
|
| Participants | Population: on‐service Thai male military personnel, King‐own bodyguard between 20 to 40, with history of posture‐induced LBP plus the tender spot producing the referred pain down to the hip or leg. Settings: Department of Physical Medicine and Rehabilitation, Phramongkutklao College of Medicine Funding: for patients is not indicated. Mean age: Thai massage = 26.25 ± 6.84; acupuncture = 29.00 ± 6.84. % female: 0%. Ethnicity: only Thai men recruited (no additional details). Work status: only on‐service military personnel recruited. Pain duration: onset (weeks): Thai massage = 12.78 + 22.71; acupuncture = 14.81 + 22.73. Previous surgery: excluded. Diagnoses: several conditions were excluded; nothing specific included. Exclusion criteria: individuals with the history of acute back injury within 3 months, previous history of back surgery, disc herniation, spine fracture, spine infection, spondyloarthropathy, presence of coagulation disorder, skin infection over the area of the selected acupoints, neurodeficit or spinal deformity. |
|
| Interventions | Massage technique: Thai massage (Rachasmnak) – 5 sessions every 2 to 3 days over 10 days. One hour treatment to legs, back (from feet to level of 7th vertebrae) including 40 sec on femoral artery called "open the wind gate". Experience of therapist: 4 Thai traditional massage therapists from Institute of Thai Traditional Medicine who had passed 800 hours of training by the Ministry of Public Health. Group 1: Thai massage (n = 8 randomized to this group). Group 2: Acupuncture (n = 9 randomized to this group). |
|
| Outcomes | * used in the meta‐analyses. Measured at baseline and in the short‐term: a. Pain: Back symptom = Thai version of MPQ, VAS (mm)(before day 3 and day 8 and end of treatment)*, The pain threshold in each trigger point was measured by a pressure algometer. The minimal pressure required to produce pain at each point was summarized and recorded in kilogram (kg). b. Function: none. c. Adverse events: one patient of the Thai massage group experienced intense posttreatment soreness and asked to be withdrawn from the study Measured immediately after: none Measured in the long‐term: none |
|
| Notes | Results: a. Back symptom (Thai MPQ – pain descriptors) (15 items from 0‐3, lower means “better”) Group 1: from 16.13 ± 8.94 [baseline] to 12.13 ± 7.72 [day 3] to 9.13 ± 7.45 [day 8] to 10.25 ± 11.02 [day 10] to Group 2: from 15.78 ± 8.41 [baseline] to 6.67 ± 5.79 [day 3] to 3.11 ± 2.71 [day 8] to 10.25 ± 11.02 [day 10 b. Pain threshold algometry: lower means “worse”) Group 1: from 9.08 ± 5.83 [baseline] to 9.54 ± 5.05 [day 3] to 10.41 ± 5.75 [day 8] to 12.48 ± 7.04 [day 10] Group 2: from 9.69 ± 5.16 [baseline] to 13.71 ± 10.28 [day 3] to 16.61 ± 9.41 [day 8] to 9.74 ± 12.46 [day 10] c. Back Symptom (Thai MPQ – VAS) (1 item from 10 to 100mm, lower means “better”) Group 1: from 4.56 ± 1.37 [baseline] to 3.46 ± 1.98 [day 3] to 2.66 ± 1.71 [day 8] to 2.15 ± 2.61 [day 10] Group 2: from 4.19 ± 2.70 [baseline] to 2.08 ± 1.65 [day 3] to 1.28 ± 1.69 [day 8] to 0.46 ± 0.71 [day 10] Authors' conclusions: five sessions of Thai traditional massage and acupuncture were effective in the treatment of myofascial back pain in young Thai military personnel. Significant effects in both groups began after the first session. Acupuncture was more effective than Thai traditional massage when affective aspects were also evaluated. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not described in detail. "Patients were randomly divided into two groups (simple randomization)". |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Patients not blinded. |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Providers knew what they were providing. |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | High risk | Blind measurements were collected by a family physician. It is unclear how the physician was unaware of the type of treatment. In addition, patients were not blinded and the outcomes are all subjective and self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | Only one subject in the massage group dropped out because of post‐massage soreness. |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | Drop out was very low and all patients were analyzed in the group to which they were allocated by randomization. |
| Selective reporting (reporting bias) | Low risk | Thai version of MPQ and VAS (mm) were measured as defined in the methods section of the manuscript. |
| Other bias | Unclear risk | Personnel in military service would have different daily activities according to their range, experience, charge or division. The effect of their daily activities, regular exercise, demands at workplace, fitness status, body mass index or state of license are not described, so it is not possible to be measured or controlled over the results. Two patients had myofascial pain of the upper back and shoulder. Their group allocation is unknown. |
| Similarity of baseline characteristics? | Low risk | Age, onset of pain, McGill and VAS were similar at baseline. |
| Co‐interventions avoided or similar? | Unclear risk | The regular practice of exercise in this military sample was not described. |
| Compliance acceptable? | Low risk | Eight patients at the massage group and 9 in the Thai group completed the study. |
| Timing outcome assessments similar? | Low risk | From baseline and day 10. |
Lara‐Palomo 2013.
| Methods | Country: Spain. Funding: the research received no specific grant from any funding agency in the public, commercial, or not‐for‐profit sectors. Recruited: 80 recruited; 62 met inclusion criteria and consented. They were referred by their primary care physician to the clinical unit of the Health Science School of the University of Almeria (Spain) between 1 September 2011 and 29 February 2012. Randomized: 62. Followed: 61; 1 was lost to follow‐up in the experimental group. Analysis: mean and SDs for descriptive statistics. Paired t‐tests were used to compare change scores from baseline to follow‐up. Independent Student t‐tests for continuous data and Chi² tests for categorical data were used to compare scores between groups. Separate 2 × 2 mixed model ANOVA with repeated measurements for the time factor need to be conducted in order to test between‐groups differences in VAS, McQuade Test, range of trunk anteflexion motion, ODI, Roland Morris Disability Questionnaire (RMDQ), Tampa Scale for Kinesiophobia and quality of life as the dependent variables, with group (electro‐massage or superficial massage) as the between‐subjects variable and time (baseline, post treatment). Frequency counts were used to quantify clinically meaningful worsening of functional status (RMDQ increase of 2.5 according to baseline affection values points or more), such that absolute risk reduction (ARR), relative risk reduction (RRR) and number needed to treat (NNT) could be calculated. Effect size was tested. |
|
| Participants | Population: patients between 18 and 65 years, with non‐specific CLBP. They were referred by primary care physician. Settings: Health Science School of the University of Almeria (Spain). Funding for participants: not indicated. Mean age: 48 ± 15 years. % female: 67.80%. Ethnicity: not indicated. Work status: not indicated. Pain duration: > 3 months. Not specifically indicated. Previous surgery: excluded. Diagnoses: LBP longer than 3 months, localized below the costal margin persisting for 12 weeks or more, score ≥ 4 on the RMDQ and inability to achieve lumbar muscle flexion–relaxation in trunk flexion. Exclusion criteria were: clinical signs of radiculopathy, presence of lumbar stenosis, fibromyalgia or spondylolisthesis, a history of spinal surgery or neuromuscular kinesio‐tape therapy, treatment with corticosteroids in the past two weeks, and disease of the central or peripheral nervous system. |
|
| Interventions | Massage technique: superficial manual massage – effleurage, superficial pressure and skin rolling on lower back for 20 mins. Experience of therapist: not indicated.
|
|
| Outcomes | * used in the meta‐analyses: Measured at baseline and in the short‐term (10 weeks)*: a. Pain: pain with the VAS*. b. Function: disability with ODI and RMDQ. c. Adverse events: not reported. d. Other measures:
Measured immediately after: none. Measured in the long‐term: none. |
|
| Notes | Results: a. Pain intensity (VAS) (lower means "better"):
b. Function (ODI):
c. Function (RMDQ):
Authors' conclusions: "individuals with non‐specific chronic low back pain experienced a significant improvement in pain level, disability and quality of life after 20 interferential current electro‐massage sessions, but these effects may be medium to be clinically worthwhile. Further research is warranted on outcomes of electro‐massage therapy for longer periods and/or in combination with exercise programs." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Patients were randomized by computer‐generated randomized table of numbers. |
| Allocation concealment (selection bias) | Low risk | Concealed allocation by a researcher (ICL‐P) not involved in either recruitment or treatment of the patients. A second therapist (AMC‐S) blinded to the baseline findings opened the envelope and proceeded with treatment according to the group assignment. |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | The massage provider was not blinded to which type of therapy the patient was receiving (massage with interferential current versus superficial massage). |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | High risk | All outcomes are subjective and self‐reported by patients who were not blinded to which treatment they were receiving. All data were gathered before the first treatment session (baseline) and immediately after the final treatment session by a trained physical therapist assessor blinded to the treatment allocation of the patients. |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | There was a drop out of one of 31 patients that was randomized to electromassage. No drop‐outs in the control group. |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | Low drop‐out rate and all patients were analyzed in the group to which they were allocated by randomization. |
| Selective reporting (reporting bias) | Low risk | Outcomes were assessed as proposed by the study: pain with the VAS, disability with ODI and RMDQ; health status with the SF‐36 Quality of life questionnaire. These outcomes were measured at the baseline and at the end of the study 10 weeks after. |
| Other bias | Unclear risk | The onset of pain, demands at workplace, fitness status, body mass index or medications were not measured. |
| Similarity of baseline characteristics? | Low risk | Age, gender, mild acute complaints in past 2 years and sleep difficulties were similar at baseline. |
| Co‐interventions avoided or similar? | Unclear risk | There is no description about injections, medications or other modalities of therapies. |
| Compliance acceptable? | Low risk | The study does not report concerns about the compliance. It describes that patients completed the 20 sessions of the intervention in each group. |
| Timing outcome assessments similar? | Low risk | 10 weeks in both groups. |
Little 2008.
| Methods | Country: UK. Funding: Medical Research Council and the Rufford Maurice Laing Foundation. |
|
| Participants | Total sample size: 579. % male: 30.5. Mean age: 45.5 years. Eligibility: patients with recurrent or CLBP, presenting to primary care with LBP > 3 months (currently scoring ≥ 4 on Roland Morris Disability Questionnaire (RMDQ), current pain for ≥ 3 weeks (to exclude recurrence of short duration) . |
|
| Interventions | * Data used in the meta‐analysis. * 1a. Massage only versus normal care n = 147. * 1b. Massage versus exercise, n = 147. 2a. Six Alexander technique lessons. 2b. Six Alexander lessons + exercise, n = 144 3a. 24 Alexander lessons. 3b. 24 Alexander lessons + exercise, n = 144. 4a. Normal care = 72. 4b. Normal care + exercise, n = 144. Frequency and treatment duration:
Personal communication with author (Paul Little): "all groups had usual care which was GPs normal practice for treatment and/or referral so like most normal care somewhat variable and not standardised, but well distributed across the trial groups" |
|
| Outcomes | * used in the meta‐analyses: Data measured at 3 and 12 months: a. Pain: median days with no pain (IQR), Von Korff Pain*. b. Function: Roland disability score*. c.Adverse events: worse pain in one patient. d. Other measures
|
|
| Notes | Results: a. Pain intensity (Von Korff Pain) (lower means "better"):
b. Function (Roland Disability score):
Control from 10.7 ± 4.8 [baseline] to 7.58 ± 8.5 [long term]. Conclusions: Massage is helpful in the short term, which supports tentative conclusions from previous research. Benefit in the longer term is probably less, which is supported by previous comparison with a self care booklet,35 although this trial did find benefit compared with acupuncture. Acupressure may possibly be more effective than the classic massage we used. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomized to one of eight groups by the practice nurse telephoning the central coordinating centre. A statistician had prepared a secure program using computer‐generated random numbers so that the next allocation could not be guessed. For each practice contributing 10 patients, a block of eight numbers existed, and two were added from a block that supplied four other practices. Practices were not told how many patients would be recruited to each trial group or informed of the block randomization. |
| Allocation concealment (selection bias) | Low risk | Participants were randomized to one of eight groups by the practice nurse telephoning the central coordinating centre. |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | Unclear risk | Not mentioned. |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | Unclear risk | Not mentioned. |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | Unclear risk | Not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | The trial authors reported: "We found no evidence of confounding or bias from losses to follow‐up". Follow‐up was 80.1% at 3 months and 79.9% at 6 months. |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Unclear risk | Not described. |
| Selective reporting (reporting bias) | Low risk | The back specific functionality (RMDQ), Quality of Life (SF36‐physical score), pain (number of days free of pain) and overall improvement (Von Korff scale, Deyo "troublesomeness" scale and health transition) were all reported at three months and 1 year. Exept for the SF36‐physical score, using health transition and the specific scale developed by the trial authors, the rest of the measures were reported for the baseline. |
| Other bias | Low risk | No other bias was identified. |
| Similarity of baseline characteristics? | Low risk | Yes: Age, gender, marital status, education status, unemployment, von Korff overall, Roland Disability score, Deyo troublesomeness, Median No of days (interquartile range) in pain in past four weeks. |
| Co‐interventions avoided or similar? | Unclear risk | Not mentioned. |
| Compliance acceptable? | Low risk | Good adherence (see bmj.com for definitions) was achieved by 91% (108/119) of patients in the group receiving massage, 94% (106/113) in the group receiving six Alexander technique lessons, and 81% (95/117) in the group receiving 24 lessons. Adequate adherence for exercise prescription was achieved by 76% (211/278) of patients. |
| Timing outcome assessments similar? | Low risk | Similar in both groups. |
Mackawan 2007.
| Methods | Country: Thailand. Funding: 2002 to 2003 Khon Kaen University research grant, Khon Kaen University, Khon Kaen, Thailand. Recruited: not reported. Randomized: 67. Followed: 67. Analyses: Ancova to compare the difference between groups. | |
| Participants | Mean age: Traditional Thai Massage (TTM): 38.97 (SD = 7.85). Joint mobilization (Mob): 38.57 (SD = 7.66). % female: 61.19%. % white: not reported. Work status:
Pain duration: > 12 weeks Previous surgery: excluded from study. Diagnoses: non‐specific LBP. |
|
| Interventions | Massage technique:
TTM: deep massage with prolonged pressure (5 to 10sec per point) on low‐back muscles between L2 and L5 using the theory of "10 Sens".
Experience of therapist: experienced physiotherapist (time not specified).
One session of 10 minute duration. Groups:
|
|
| Outcomes | * used in the meta‐analyses: Measured: immediately after a. Pain: VAS (before and five minutes after the treatment)* b. Function: no c. Overall improvement: no d. Patient satisfaction: no e. Adverse events: not reported |
|
| Notes | Results: a. Pain Visual Analogue Scale (VAS):
Authors' conclusions: "Based on the results of this study, we conclude that both TTM and joint mobilization can temporarily relieve pain in patients with non‐specific low‐back pain. However, TTM yields slightly more beneficial effects than joint mobilization" Review authors' comments: poor description of the population, demographics, co‐medications, previous use of TTM or mobilization, prior beliefs, co‐morbidity, duration of pain episode, previous treatments. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 67 patients who met the inclusion criteria and were randomly assigned to one of the two treatment arms using block randomized allocation with block sizes of 2, 4 and 6. Groups were assigned using a pre‐generated random assignment scheme enclosed in envelopes. |
| Allocation concealment (selection bias) | Low risk | Groups were assigned using a pre‐generated random assignment scheme enclosed in envelopes. |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | Unclear risk | The evaluation was done by one person only, who was blind to the treatment group allocation. However all outcomes were subjective and self‐reported by the patients. |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | The outcome measures were analyzed 5 min after each treatment. No losses to follow‐up. |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | All patients were analysed in the same group to which they were allocated. |
| Selective reporting (reporting bias) | Unclear risk | Pain (VAS) was reported before and after treatment with 1 session of TTM, as mentioned in the methodology. |
| Other bias | Low risk | No other bias was identified. |
| Similarity of baseline characteristics? | Unclear risk | Unclear from text. The duration of pain is not reported in the baseline characteristics. |
| Co‐interventions avoided or similar? | Unclear risk | Unclear from text. Not described in the article (unclear to define whether patients had taken medications before the therapy sessions or not). |
| Compliance acceptable? | Low risk | Yes. |
| Timing outcome assessments similar? | Low risk | Yes. Five minutes after the therapy sessions. |
Poole 2007.
| Methods | Country: England. Funding: not reported. Patients were recruited from primary care sources. Recruited: 650 letters sent by 12 GPs ‐ 278 replies. Randomized: 243. Follow‐up: 191 at baseline (78%); 165 at end of six sessions (68%); 156 at six months (64% of 243). ITT analysis: no. Analyses: repeated measures ANCOVA. |
|
| Participants | Setting: Private clinic. Reflexology: mean 47.2 (SD 10.5). Relaxation: mean 45.6 (SD 12.0). Non intervention: mean 47.45 (SD 10.2). Gender (female/male): Reflexology: 48/29. Relaxation: 53/29. Non‐intervention: 38/37. Working status: reflexology: > 50%; relaxation: > 50%. Non‐intervention: > 50%. Duration of pain (months): reflexology: 120.6; relaxation: 128. No intervention: 114.7. Co‐morbidity: not described. | |
| Interventions | Massage technique: foot reflexology ‐ Morrell technique (application of firm but gentle compression to the feet).
No standardized protocol provided.
Six sessions of approximately one hour duration over a period of six to eight weeks.
Experienced therapist: trained to diploma level, professional indemnity insurance and extensive experience. Adjuvant therapy: usual care. Groups:
|
|
| Outcomes | * used in the meta‐analyses. Measured at: baseline, after the end of all sessions, at six months after the end of sessions: a. Pain: VAS* b. Function: Oswestry (primary)* c. Adverse events: not reported d. Other measures:
|
|
| Notes | Results: SF‐36 Pain ‐ Mean (SD):
VAS
Authors' conclusions: "The current study does not indicate that adding reflexology to usual care for the management of CLBP is any effective than usual care alone." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Minimization technique. |
| Allocation concealment (selection bias) | High risk | Not concealed. The first trial author randomized patients to one of three groups. |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Patients were informed of their group of allocation by letter. |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | The therapists were not blinded to the type of therapy they were providing. |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | High risk | Patients completed the self report questionnaire booklet on their own and returned by post to the first author. Patients were not blinded to the group of allocation. |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | Drop outs after assessment #1 were 11%, 28% and 15% of the initial samples for reflexology, usual care and relaxation groups, respectively. Drop outs after assessment #2 were 15%, 42% and 30% for reflexology, usual care and relaxation groups, respectively. |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | High risk | The trial authors mentioned that the analysis was based on ITT, but they had a lot of dropouts and it is unclear if they had any imputation of missing data. Therefore, they analyzed all patients available at follow‐up and not all patients randomized. |
| Selective reporting (reporting bias) | Unclear risk | Pain (VAS), Quality of Life (SF36), back specific functionality (RMDQ) and depression (Beck depression inventory II (BDI‐II)) were all reported at pretreatment, post‐treatment and at six months follow‐up. |
| Other bias | Low risk | No other bias was identified. |
| Similarity of baseline characteristics? | Unclear risk | Unclear from text. Work status was not reported in tables or results, although mentioned to be taken in account in methodology. Duration of pain was taken in account. |
| Co‐interventions avoided or similar? | High risk | Were not similar, according to Table 2. |
| Compliance acceptable? | Unclear risk | Unclear from text. |
| Timing outcome assessments similar? | Low risk | It seems to be similar. |
Preyde 2000.
| Methods | Country: Canada. Funding: College of Massage Therapists of Ontario. 165 patients were recruited, 107 met the inclusion criteria and 104 were randomized. 92% were followed. Outcome assessor of range of motion was blinded. Patients were recruited by university e‐mails, flyers sent to family physicians and advertisements in the local newspapers in Ontario. Period of study: 1998 to 1999. Follow‐up: one month after end of treatment. |
|
| Participants | Settings: this study was conducted at the Health and Performance Centre, University of Guelph, Guelph, Ontario, which offers multidisciplinary services such as sports medicine, physiotherapy and chiropractic manipulation. Average age: 46 years. 51% female. Average duration of pain: three months (1 week to 8 months). Previous treatments not described. |
|
| Interventions |
|
|
| Outcomes | * used in the meta‐analyses: Measured at baseline, at the end of the treatment* and at one month follow‐up: a. Pain: Present Pain Index (PPI): PPI score* (valid, reliable), PRI: PRI score (valid, reliable). b. Function: RMDQ: RMDQ score* (valid, reliable, sensible). c. Adverse events: not reported. d. Other measures:
|
|
| Notes | Authors' conclusions: massage is beneficial for patients with subacute LBP. Measured at the end of all sessions and one month after the end of sessions. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers table. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | Unclear risk | Not reported in the text. Patients either received comprehensive massage, with exercises and postural education, soft tissue manipulation only, posture and remedial exercises only or placebo of sham laser. The method to blind patients to the treatment is not clearly described, in particular comprehensive massage therapy versus soft tissue manipulation. |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | Unclear risk | Unclear from text. |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | Unclear risk | Unclear whether patients were blinded for pain and function outcomes. It seems like patients under sham therapy were blinded, but is unclear for other groups. |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | Drop outs were 7%, 18% , 12% and 11% of the initial samples of comprehensive massage therapy, soft tissue manipulation, remedial exercise and posture education, placebo (sham with laser treatment) groups, respectively. |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | Outcome data were analysed by ITT. All patients were analyzed in the group to which they were allocated by randomization. |
| Selective reporting (reporting bias) | Unclear risk | The MPQ (PPI for intensity of pain and PRI for quality of pain), the RMDQ for LBP specific functionality were reported. All measures were reported as mentioned in the methodology, after 1 month of treatment and follow‐up measures that were obtained 1 month after treatment ended. |
| Other bias | Low risk | No other bias was identified. |
| Similarity of baseline characteristics? | Low risk | Described in Table 2: age, gender, marital status, education, mean body mass index, occupational activity, duration of LBP, previous episode of LBP, possible etiology factor and outcome measures at baseline. |
| Co‐interventions avoided or similar? | Low risk | Co‐interventions were avoided. Participants were invited to stop medication and they were asked not to seek additional therapy for their backs for the 2 months that they were involved in the study. |
| Compliance acceptable? | Low risk | Yes. Described in Table 1. |
| Timing outcome assessments similar? | Low risk | Yes. |
Quinn 2008.
| Methods | Country: UK. Funding: not reported. |
|
| Participants | Total sample size: 15. % male: 32.2. Mean age: 43.5 years. Eligibility: staff employed at the University of Ulster with non‐specific LBP, any physiotherapy, medication or other treatments for LBP has been stabilized for at least 3 months. Pain duration: not reported if acute or chronic, but assumed to be sub‐acute or chronic. |
|
| Interventions | Group 1: massage ‐ reflexology, n = 7 Group 2: sham (foot massage), n = 8 Frequency: 1 treatment/week Duration: 6 weeks |
|
| Outcomes | Data measured at 3 months: a. Pain: VAS‐primary outcome measure; MPQ. b. Function: RMDQ; SF‐36 health survey. c. Adverse effects: no harms reported. |
|
| Notes | Results: median (1st and 3rd interquartiles). Group 1 versus Group 2. VAS: baseline 4.7 (3.5 to 6.6) versus 3.4 (3.0 to 4.2). Roland‐Morris: baseline 5 (4 to 8.6) versus 7.5 (3 to 9.3). Conclusion: reflexology appears to offer promise as a treatment in the management of LBP; however, an adequately powered trial is required before any more definitive pronouncements are possible. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number table. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | Low risk | All participants were blinded to their group allocation. Participants were told that they would either receive a reflexology treatment or a foot massage. As participants were reflexology‐naive they should not have been aware of which treatment they received. |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | It was not possible to conceal group allocation from the therapist, as this person administered the treatment. |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | Low risk | The outcome assessor was also blinded to group allocation. Patients scored the VAS and MPQ and they were previously blinded to the group of allocation. |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | No loss to follow‐up. No drop outs. |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | All patients were analyzed in the group to which they were allocated by randomization. |
| Selective reporting (reporting bias) | Low risk | The VAS for pain, the MPQ (PRI for quality of pain), the RMDQ for LBP specific functionality and SF 36 for quality of life were all reported. All measures were reported as mentioned in the methodology, at baseline (before the first treatment in week 1), post‐treatment (after the last treatment in week 6), week 12 (follow‐up), and week 18 (follow‐up). |
| Other bias | Low risk | No other bias was identified. |
| Similarity of baseline characteristics? | Low risk | Table 1 describes baseline characteristics regarding the intensity of pain, Roland Morris Questionnaire and MPQ. Gender was 6/1 in reflexology group, 4/4 in sham group for woman/man. However, other variables were not included, such as occupation and duration of pain. |
| Co‐interventions avoided or similar? | Unclear risk | "Any physiotherapy, medication or other treatment for their LBP had been stabilized for at least 3 months, no involvement in other research projects within the past 3 months, reflexology naïve (with no detailed knowledge of specific reflexology points), not pregnant." "Two participants received physiotherapy during the follow‐up period". No further details were described, regarding co‐interventions. |
| Compliance acceptable? | Low risk | It is described that all participants received the treatment. |
| Timing outcome assessments similar? | Low risk | Yes. |
Sritoomma 2014.
| Methods | Country: Thailand. Funding: unclear. Recruited: 164 assessed, 24 excluded. Randomized: 140. Followed: 138; 2 discontinued TTM intervention. Analysis: means and SDs presented for continuous variables; repeated measures ANOVA. |
|
| Participants | Population: people aged ≥ 60 who were diagnosed with CLBP (lasting > 12 weeks). Settings: massage clinic. Funding for participants: unclear. Mean age: not described. % Female: 80%. Ethnicity: Thailand. Work status: labourer, business, teaching, jobless. Pain duration: minimum 12 weeks. Previous surgery: excluded. Diagnoses: several conditions were excluded; nothing specific included. |
|
| Interventions | Massage technique:
|
|
| Outcomes | Measured at baseline and immediately after end of 10 sessions (6 weeks) and short‐term (15 weeks): a. Pain: VAS for back pain, present pain intensity scale, MPQ b. Function: Oswestry Disability Questionnaire c. Adverse effects: no adverse events were identified. d. Other outcomes were: n/a Note: the VAS was also measured immediately after each single session of massage |
|
| Notes | a. Back symptom (Thai MPQ – pain descriptors) (15 items from 0 to 3, lower means "better"):
b. Pain intensity (VAS from 0 to 100, lower means "better"):
c. Pain intensity (present pain intensity):
d. Function (Oswestry Disability Questionnaire (lower means less disabled)):
Authors' conclusions: both types of massage resulted in positive change in back pain intensity over time, although there was a significant difference between Swedish and Thai massage groups in the extent of that change. Although the study lacked a placebo group, it still compared the treatment intervention with a relevant control group. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A statistician not involved in the study prepared a randomization schedule using a random number generated by computer with permuted block randomization (blocks of 10) prior to the enrolment of the first participant. |
| Allocation concealment (selection bias) | Low risk | Another person not involved in the study placed randomized numbers into opaque envelopes. The assignments were placed in sealed opaque numbered envelopes prior to the onset of the study and treatments were determined after the baseline assessments had been completed. Each person who met the eligibility criteria was given the next opaque envelope treatment in sequential order. |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | Unclear risk | Participants may have known which group they were in (ginger odour versus no ginger odour or type of techniques depending on familiarity). |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Providers knew which intervention they were providing. |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | High risk | Patients were not blinded in self‐report measures. |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | Only two patients dropped out in the control group. |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | All patients were analyzed in the group to which they were allocated by randomization. |
| Selective reporting (reporting bias) | Low risk | All measures seemed to be used and reported as defined in the methodology. |
| Other bias | Low risk | No additional risk identified. |
| Similarity of baseline characteristics? | Unclear risk | Duration of pain was not compared between the two groups. |
| Co‐interventions avoided or similar? | High risk | Possible other interventions, such as exercise or injections were not described. Medications were not published, in spite of monitoring their use. One group receives massage and ginger oil. A second group receives Thai massage. Two different types of massage and the addition of a treatment additive. |
| Compliance acceptable? | Low risk | Patients completed the protocol, according to Figure 1. |
| Timing outcome assessments similar? | Low risk | They were all assessed at similar timing intervals (6 weeks and 15 weeks). |
Yip 2004.
| Methods | Country: Hong Kong, China. Funding: partial support of the School of Nursing, Departmental Research Committee for this study. Recruited: 61. Randomized: 61. Followed: 51 (84%). Analyses: Mean ratio change = X2/X1, where X2 was the mean score at post one‐week follow‐up, X1 was the mean score at baseline, comparison between groups by Mann‐Whitney U test. | |
| Participants | Settings: the research was carried out among members of the community centre, Old‐Aged Home and Women Workers Association, recruited via notices on bulletin boards. Mean age: 45.81 years. % female: 97%. Ethnicity: not reported, but assume all Chinese. Work status: not reported. Previous surgery: not reported. Diagnoses: non‐specific sub‐acute LBP defined as pain on most days in the past 4 weeks in the area between the lower coastal margins and the gluteal folds without known specific cause, such as a spinal deformity. Pain duration: of current episode:
|
|
| Interventions | Massage technique: Acupressure consisting of the application of a light to medium finger press with 3% lavender oil with grape seed oil as the massage lubricant on eight (4 bilateral) fixed acupoints for 2 minutes each: San‐Jiao‐Shu (UB22), Shen‐Shu (UB23), Da‐Chang‐Shu (UB25) and Wei‐Zhong (UB40); for 35 to 40 minutes, 8 times over a 3‐week period. Before massage: 10 minutes 'relaxation' with a digital Electronic Muscle Stimulator (7.69 Hz at 0.05 mA) delivered by five pairs of medium sized (2.5 cm) electrode pads on five bilateral acupoints [Shou‐San‐Li (LI10), Qu‐Chi (LI11), Nao‐Shu (SI10), Tian‐Liao (TW15) and Tian‐Zhu (BL10). Experience of therapist: nurse trained in Chinese Medicinal Nursing. The precision of the acupressure was confirmed by deqi.
|
|
| Outcomes | * used in the meta‐analyses: Measured at baseline and one week after the end of treatment: a. Pain: VAS (primary outcome)*. b. Function: ROM of lateral spine flexion (lateral fingertip‐to‐ground distance in cm), walking time for 15m (50ft); interference in daily activities (modified Aberdeen LBP scale* ‐ effect of LBP on sleeping, walking distance, housework/work and leisure‐time activities). Higher scores mean greater interference. c. Adverse events: No adverse effects were reported from subjects. d. Other measures:
|
|
| Notes | a. Pain (VAS)
Mean ratio change:
b. Function: ROM (P = 0.01)
Walking time (P = 0.05):
Insignificant interference with daily activities. Authors' conclusions: "Our results show that eight‐sessions of acupoints stimulation followed by acupressure with aromatic lavender oil were an effective method for short‐term LBP relief. No adverse effects were reported. To complement mainstream medical treatment for sub‐acute LBP, the combined therapy of acupoint stimulation followed by acupressure with aromatic lavender oil may be one of the choices as an add‐on therapy for short‐term reduction of LBP." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers table into intervention or control group. |
| Allocation concealment (selection bias) | Unclear risk | Unclear. Participants were allocated by the research team. |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | Unclear risk | Not mentioned. |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | Unclear risk | Not mentioned. |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | High risk | Outcome measures were collected by nursing staff using face‐to‐face interviews and body measurements. The nurses were not blinded to patient group. |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | Drop outs were 17% and 16% of the initial samples of control and intervention groups, respectively. |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | High risk | ITT was not done. |
| Selective reporting (reporting bias) | Unclear risk | The pain intensity‐VAS and modified Aberdeen LBP Scale (Interference with daily activities (sleeping, walking distance, housework/work and leisure‐time activities) were all reported. Results were reported as difference in the scores of mean of score in post‐1 week/mean of score at baseline between both groups. The duration of pain was described in the text. |
| Other bias | Low risk | No other bias was identified. |
| Similarity of baseline characteristics? | Low risk | At baseline, there were no significant differences between the groups regarding age, gender, occupation, education level and the outcome measures of pain intensity, pain duration, interference on daily activities, walking time and spinal flexion. |
| Co‐interventions avoided or similar? | Unclear risk | Co‐interventions not described. The conventional treatment alone is not described, however both groups received it. |
| Compliance acceptable? | Unclear risk | Unclear from text. |
| Timing outcome assessments similar? | Low risk | Yes. |
Yoon 2012.
| Methods | Country: Korea. Funding: this study was supported by a grant of the Korea Healthcare Technology R&D Project (A091220), Ministry for Health, Welfare & Family Aff airs, Republic of Korea Recruited: 26 but two were exclude afterwards due to lumbar surgery and history of recent injury respectively. Randomized: 24 patients were randomly divided into two groups. Followed: 22. Analysis: the Mann‐Whitney test was used to compare group age, duration and initial data for PNRS, ODI, and RMDQ. A Chi² test was used to compare group gender. A Wilcoxon signed rank test was used to compare the effect between baseline and immediate after treatment, and baseline and 2 weeks after cessation of treatment in each group. A P value < 0.05 were considered statistically significant. |
|
| Participants | Population: people with LBP for over 3 months and a PNRS (0‐100) over 30, between the ages of 20 and 65 were included. Settings: Department of Rehabilitation Medicine, Jesus Hospital, 68, Seowonro, Wansangu, Jeonju 560‐750, Korea. Funding: No funding for patients. Mean age: roptrotherapy group: 50.25 (6.69), TENS group: 53.30 (6.67). % Female: roptrotherapy group: (7/12), TENS group: (6/10). Ethnicity: not reported. The study is published from the city of Jeonju, Korea. Work status: not described. Pain duration: LBP for over 3 months. Previous surgery: one patient, who was excluded. Diagnoses: people 20 to 65 years old with LBP rated by the numeric rating scale (PNRS, 0‐100) over 30. The exclusion criteria included: acute or subacute LBP within 3 months, recent LBP treated within the previous 1 month, history of diabetes or thyroid disease, general disease such as rheumatic disease, pregnancy or breastfeeding, pacemaker or implanted electrical device, suspicious malignancy or thrombosis, scoliosis, vertebral fracture, myopathy, traumatic LBP, current disc herniation, history of lumbar surgery, neurological problems of the central or peripheral nervous systems. |
|
| Interventions | Massage technique:
|
|
| Outcomes | * used in the meta‐analyses: Measured at baseline, immediately after and in the short‐term*: a. Pain: PNRS*. b. Function: ODI RMDQ*. c. Adverse effects: One patient complained of skin discomfort deep cross‐friction massage using the HT‐bar. Measured in the long‐term: None. |
|
| Notes | a. Pain intensity (PNRS) (range 0 to 100, lower means "better")
b. Function (ODI) (range 0 to 100%, lower means "better")
c. RMDQ, (range from 0 to 23 points, lower means “less limitations due to the back pain”).
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Patients were randomly divided into two groups. The method of randomization is not described. |
| Allocation concealment (selection bias) | Unclear risk | The allocation is not described. |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Patients were not blinded to group. |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | High risk | Patients were not blinded to group and all outcomes were subjective and self‐reported by patients. |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | All 12 patients randomized to the treatment group were analysed. Two out of 12 patients dropped out from the control group. |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | Drop out was very low and all patients were analyzed in the group to which they were allocated by randomization. |
| Selective reporting (reporting bias) | Low risk | Pain and function were reported according to the methodology. |
| Other bias | Low risk | No other bias were detected. |
| Similarity of baseline characteristics? | High risk | Occupation or level of activity was not described at the baseline. Other potential conditions that could affect the report of outcomes were not reported, such as: educational level, physical demands at job. |
| Co‐interventions avoided or similar? | Unclear risk | Medication at baseline or follow‐up is not described. Other therapies were avoided by the group, but there is no report whether the patients visited other centres for the management of pain. |
| Compliance acceptable? | Low risk | Patients completing < 10 sessions were excluded. |
| Timing outcome assessments similar? | Low risk | All patients were evaluated at baseline, immediately after and at 2 weeks. |
Zheng 2012.
| Methods | Country: China. Funding: not indicated. Recruited: 64. Randomized: 64. Followed: 60. There were four drop‐out cases in this study; 2 failed to adhere to treatment and follow‐up in the control group and 2 discontinued treatment due to a worse pain after the deep massage. Analysis: mean and SDs for descriptive statistics. Independent sample t‐test were used to compare scores between groups. |
|
| Participants | Population: patients with non‐specific LBP lasting > 3 months and between 21 to 75 years. Settings: outpatients from the rehabilitation medicine centre of Chinese PLA General Hospital. Funding: for patients not indicated. Mean age: massage group = 43 ± 15; control group = 42 ± 15. % Female: massage group = 44%; control group = 50%. Ethnicity: not indicated as per Chinese population. Work status: not indicated. Pain duration: treatment versus control group: course of disease ranging from 4.0 months to 6.0 years (2.7 ± 1.1) versus from 5.0 months to 7 years (2.6 ± 1.4). Previous surgery: not indicated. Diagnoses: several conditions were excluded; nothing specific included. Non‐specific LBP is defined as pain under the scapulas, above the cleft of the buttocks, with or without radiation to the lower extremities. Exclusion criteria: language barriers and those with LBP caused by neoplasm, osteoporosis, vertebral fracture, rheumatoid arthritis, acute herniated disc accompanied by nerve root entrapment and unstable spondylolisthesis. |
|
| Interventions | Massage technique: deep slide massage, 8 to 10 seconds following feeling of slight discomfort, repeated 4 to 5 times; treatment twice a week with lumbar traction once daily. Treatment over 3 weeks. Experience of therapist: not indicated.
|
|
| Outcomes | * used in the meta‐analyses: Measured at baseline and immediately after*: a. Pain: pain threshold, pain intensity*. b. Function: none. c. Adverse effects: not reported. d. Other measures:
Measured in the short‐term: not measured. Measured in the long‐term: not measured. |
|
| Notes | Results: Pain intensity (VAS) (0 to 100 mm, lower means "better"):
Authors' conclusions: "We found a statistically significant (P < 0.05) increase in PPT, decreased muscle hardness, and lower VAS score after treatment in the treatment group compared to the control group in this study, suggesting improved therapeutic efficiency from the application of tender point deep tissue massage in combination with lumbar traction than with lumbar traction alone." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers were generated using Microsoft Office Excel. |
| Allocation concealment (selection bias) | Unclear risk | Not clearly described. "A single designated person was responsible for the allocation tableusing the treatment sequence". |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | Unclear risk | Not clearly described. |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | Unclear risk | Not clearly described. |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessor? | Unclear risk | Not clearly described. |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | Less than 10% in each group. Two patients were lost to follow‐up in the lumbar traction group and two discontinued intervention in the massage group when got worst after deep massage. |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | Patients that were lost to follow‐up or discontinued the treatment were not included for analysis at the end of the study. However the number of drop‐outs was very low 4/64 (6.25%) and this might not have biased the results if these patients did not receive the intervention that they were randomized to. |
| Selective reporting (reporting bias) | Low risk | The pain intensity was measured at the end of the study, as proposed in the methodology. |
| Other bias | Unclear risk | However, demands at workplace, current treatments, fitness status or body mass index were not measured. |
| Similarity of baseline characteristics? | Low risk | Gender, age, course of disease and VAS were measured and similar at the baseline. |
| Co‐interventions avoided or similar? | Unclear risk | Other interventions during the study were not recorded or if so, were not reported. |
| Compliance acceptable? | Low risk | The study does not report concerns about the compliance. |
| Timing outcome assessments similar? | Low risk | In both groups it was 3 weeks after treatment started. |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Anderson 2005 | This doctoral thesis is a RCT that compared the effect of Pilates versus massage in patients having CLBP and recurrent LBP (RLBP). We excluded this article because the definition used for this study included patients with lesions of inert structures, such as disc lesions, ligament lesions, joint instabilities and bony abnormalities (e.g. osteophytes, stenosis and degenerative changes), as well as ligament and capsular sprains, disc fissures and herniations, stress fractures, and effects of disc degeneration that can lead to a mechanical compromise of neural structures. |
| Barnes 1997 | This RCT compared a group that received myofascial release versus no myofascial release. We excluded this study because it included patients with unilateral anterior rotation rather than LBP and the outcome was the amount of change in mean linear distance from each ASIS to a central reference point. These are not inclusion criteria for this Cochrane Review, regarding the population and the primary outcomes. |
| Buerger 1980 | We excluded this RCT because massage was not applied as in routine practice. It was used as a sham treatment for manipulation. |
| Dishman 2001 | This RCT was excluded because the population consisted of asymptomatic volunteers. They were randomized to either a spinal manipulation, massage or control group. The purpose of the study was to compare the magnitude and duration of motoneuron inhibition occurring as a sequel to spinal manipulation or paraspinal and limb massage. |
| Farasyn 2007 | This is a RCT of roptrotherapy versus placebo on 65 patients with subacute LBP. Even though they measure pain‐VAS and Oswestry disability, the only outcome reported is PPT. We excluded this trial because PPT is not considered a primary outcome in this Cochrane Review. The placebo group also received roptrotherapy after the 2nd week. |
| Ferrell 1997 | This RCT investigated a mixed population with chronic musculoskeletal pain including LBP. Patients were randomly assigned to one of three groups: 1) supervised program of walking; 2) pain education program: heat, cold, massage, relaxation and distraction; and 3) usual care. We excluded it from this review because of a mixture of patients and because the effects of massage could not be extracted separately. |
| Fraser 1993 | This RCT was designed to measure the effects of back massage on anxiety levels of elderly residents in a long‐term care facility. We excluded it from this review because massage is not applied to treat LBP. |
| Ginsberg 1987 | This double‐blinded placebo controlled trial was designed to test the effects of Rado‐Salil ointment in mechanical LBP compared to placebo. Massage was employed in both groups (Rado‐Salil and placebo). |
| Godfrey 1984 | We included this RCT in the two previous versions of this Cochrane Review (Furlan 2000; Furlan 2002). However, we decided to exclude this trial from Furlan 2008 because it uses massage as a control group for another active intervention, and therefore massage therapy was not delivered appropriately as it is in practice. |
| Haas 2014 | This is a RCT that randomized 400 participants with non‐specific CLBP to receive a dose of 0, 6, 12 or 18 spinal manipulative therapy (SMT) sessions from a chiropractor to the intervention groups and non‐time‐equivalent sessions of massage. We excluded this study because massage was applied to the control group as 5‐minutes‐light massage, so it was not properly delivered. |
| Hoehler 1981 | We included this RCT in the two previous versions of this Cochrane review (Furlan 2000; Furlan 2002). However, we excluded this trial from Furlan 2008 because it uses massage as a control group for another active intervention, and therefore massage therapy was not delivered appropriately as it is in practice. |
| Kalaoukalani 2001 | This article is a sub‐analysis of the data derived from the RCT published by Cherkin 2011 et al (which is included in this review). Kalaoukalani 2001 does not have information about the effects of the interventions. The objective of this sub‐analysis was to evaluate the association of a patient's expectation for benefit from a specific treatment with improved functional outcome. |
| Kankaanpää 1999 | This is a RCT of 59 patients with non‐specific CLBP. The main intervention was "active rehabilitation" consisting of exercises, behavioral support and ergonomic advice. The control group received massage plus thermal therapy, once a week (four treatment sessions). The study authors stated that the control group was considered a placebo treatment because massage and thermal therapy are assumed to be ineffective in the treatment for LBP. We excluded this trial from Furlan 2008 because: 1) the effects of massage could not be distinguished from the effects of thermal therapy; and 2) massage was seen as placebo therefore it was applied with no intention to relieve the patient's symptoms. |
| Koes 1992 | This is a randomized clinical trial of 256 patients with non‐specific back and neck complaints. Patients were given three types of management: physiotherapy (exercises, massage, physical modalities), manual therapy (manipulation or mobilization) and care delivered by general practitioner (drugs: analgesics, advices about posture, home exercise and bed rest). A 4th group received placebo treatment consisting of detuned shortwave and detuned ultrasound. We excluded this trial from this review because the population consists of a mixture of back and neck complaints, and because the effects of massage therapy could not be extracted separately from the other interventions. |
| Kolich 2000 | This RCT was designed to determine the effects of a massaging lumbar support system on low‐back muscle activity. We excluded it because the population consisted of healthy subjects. |
| Kong 2012 | This RCT included patients with non‐specific LBP. We excluded it from this review because both groups received massage and the intervention under study was the herbal ointment. |
| Konrad 1992 | Intervention was underwater massage, which consisted of massage and movement while a stream of hot water (37°C), 1 atm, 10 cm) was applied to the affected part. In this case it is difficult to know if the therapeutic effect was due to the massage, the water relaxation or the superficial heat. |
| Lauche 2012 | This study assessed the pain (VAS) in 21 patients with chronic neck pain and 19 patients with CLBP that were randomized to Gua Sha Therapy or a waiting list control group. We excluded this study because such a technique was not considered a massage therapy. |
| Lei 2011 | This RCT analyzed the effects on pain by comparison between Santong tuina therapy versus tuina therapy. However, we excluded it because it included patients with lumbar intervertebral disc protrusion (LIDP) diagnosed by CT or MRI, and not only patients with non‐specific LBP. |
| Li 2006 | This is a RCT comparing acupuncture massage with mobilization in a population with typical symptoms of lumbar intervertebral disc protrusion with clinical positive signs and diagnosed by CT or MRI aged between 20 to 55 years. The trial was excluded from this review because the LBP was caused specifically by confirmed disc herniation. |
| Lindström 1970 | This is a RCT of 62 patients with LBP and sciatica. The interventions were: 1) hot packs, massage, mobilizing and strengthening exercises for the spine; 2) intermittent pelvic traction, isometric training of the abdominal and hip extensor muscles; and 3) hot packs and rest only. We excluded this RCT because the effects of massage could not be extracted separately. |
| Liu 2009 | This RCT included patients with shoulder and back fasciitis. We excluded it from this systematic review because both groups received massage. |
| Maniche 1991 | Three articles reporting on the same controlled trial of intensive extensor exercises compared to: 1) light extensor exercises; and 2) thermotherapy, massage and mild exercises. We excluded it from this review because the effects of massage therapy cannot be extracted separately from the other therapies. |
| Melzack 1980 | Intervention was ice massage, which consisted of holding an ice cube with a gauze pad and gently massaging the skin. In this case it is difficult to know if the therapeutic effect was due to the superficial cold or the massage. |
| Melzack 1983 | We included this RCT in the two previous versions of this systematic review (Furlan 2000; Furlan 2002). However, we excluded this trial from Furlan 2008 because it uses massage as a control group for another active intervention, and therefore massage therapy was not delivered appropriately as it is in practice. |
| Movaghar 2012 | This is a semi‐empirical study, which might suggest that this is not a well‐defined randomized study. We excluded it because it included only patients with discopathy, which does not match with the population of this review as idiopathic LBP. |
| Pope 1994 | We included this RCT in Furlan 2000 and Furlan 2002. However, we decided to exclude this trial from Furlan 2008 because it uses massage as a control group for another active intervention, and therefore massage therapy was not delivered appropriately as it is in practice. |
| Rasmussen‐Barr 2003 | The manual treatment described does not fit with "massage therapy". They applied stretching, traction, manipulation and mobilization techniques. |
| Romanowski 2012 | This study compared the effectiveness of two different kind of massage in patients with CLBP: therapeutic and deep tissue massage. We excluded it because it is a non‐RCT. The patients were separated into 2 groups with no randomization. |
| Silveira 2006 | This study included massage as a therapeutic measure for triathlon athletes. There was no LBP and it was not a randomized study. We excluded it because it did not match the population nor the methodology for this Cochrane Review. |
| Walach 2003 | This is a RCT of classic massage compared to standard medical care. We excluded it because it included a mixed population of back, neck, shoulders, head and limbs pain. |
| Wang 2005 | This is a quasi‐randomized study by the order of entry of patients with non‐specific LBP to assess the effects of massage and exercise on pain. We excluded it because both groups received Tuina massage and the only difference was the exercise, which is not the scope of this review. |
| Werners 1999 | This is a RCT of 152 patients with LBP in a primary care setting, comparing interferential therapy with motorized lumbar traction plus massage. We excluded it from this review because the effects of massage could not be extracted separately. |
| Wilkinson 1997 | This Master's thesis investigated the effect of therapeutic touch on the acute pain experience in postoperative lumbar laminectomy patients. We excluded this RCT from this review because the intervention did not involve touch, and did not have manual contact between the therapist and patient. Hands were moved over the subject's body from head to toe at a distance of 2 to 4 inches over the body. |
| Wu 2004 | This was a quasi‐RCT (method of randomization involved visit number) of early intervention consisting of exercise plus massage for non‐specific LBP. It compared exercise plus massage to massage alone. We excluded it from this review because both groups received massage. |
| Zhang 2004 | This was a quasi‐randomized clinical trial (divided into groups according to hospitalization time) of traction, massage and massage plus exercise for patients with lumbar disc herniation. We excluded it from this review because the population included a specific cause of LBP (disc herniation). |
| Zhou 2008 | In this controlled clinical trial, the population does not seem to have non‐specific LBP. The intervention is manipulation and not massage. We excluded it because the study design does not seem to be randomized and the outcome is "deviation of the spinous process", which is not an outcome of interest in our review. |
Characteristics of ongoing studies [ordered by study ID]
Mandala 2001.
| Trial name or title | Mandala 2001 |
| Methods | Randomized trial |
| Participants | Chronic low‐back pain |
| Interventions | Shiatsu massage reflex therapy |
| Outcomes | Not reported |
| Starting date | |
| Contact information | |
| Notes | Abstract presented at a conference. |
Differences between protocol and review
In the previous versions of this Cochrane Review there were five primary outcomes: pain, overall improvement, back‐specific functional status, well being and disability (Furlan 2000; Furlan 2002; Furlan 2008). In this review update, we included only three primary outcomes: pain, functional status and adverse events. We listed the other outcomes as secondary outcomes.
In the previous review versions the types of included studies were published and unpublished reports of completed RCTs, quasi‐RCTs, and controlled clinical trials (CCTs) with no language restrictions (Furlan 2000; Furlan 2002; Furlan 2008). We included abstracts of ongoing studies. In the current review version we included only published RCTs.
In the previous versions of this review the comparisons consisted of the following: 1) Massage versus inert treatment; 2a) Massage versus spinal manipulation or joint mobilization; 2b) Massage versus exercise; 2c) Massage versus relaxation therapy; 2d) Massage versus acupuncture; 2e) massage versus self‐care education; 2f) acupuncture massage versus physiotherapy; 3) massage as a component of a combined therapy versus other treatments without massage; 4) different techniques of massage (Furlan 2000; Furlan 2002; Furlan 2008). In this review update we grouped the comparison groups as follows: 1) massage versus inactive controls for acute LBP; 2) massage versus inactive controls for sub‐acute and chronic LBP; 3) massage versus active controls for acute LBP; and 4) massage versus active controls for sub‐acute and chronic LBP.
Contributions of authors
MG and AB selected the studies for this updated review. AF, EI, and MI selected and appraised the studies for the previous reviews. MG, AB and AF performed 'Risk of bias' assessments and extracted data for this updated review. AF and MG wrote the final manuscript draft. MI, AB and EI reviewed and edited the final manuscript draft.
Sources of support
Internal sources
Institute for Work & Health, Canada.
External sources
-
Canadian Institutes for Health Research (CIHR), Canada.
Andrea Furlan received a CIHR New Investigator Award (2012‐2017)
Declarations of interest
None of the authors has made or is involved in a clinical study which fulfills the inclusion criteria of this review. Amanda Baskwill is a registered massage therapist in Ontario. No funds from external sources were received to conduct this Cochrane Review.
New search for studies and content updated (conclusions changed)
References
References to studies included in this review
Ajimsha 2014 {published data only}
- Ajimsha MS, Daniel B, Chithra S. Effectiveness of Myofascial release in the management of chronic low back pain in nursing professionals. Journal of Bodywork and Movement Therapies 2014;18(2):273‐81. [DOI] [PubMed] [Google Scholar]
Buttagat 2011 {published data only}
- Buttagat V, Eungpinichpong W, Chatchawan U, Kharmwan S. The immediate effects of traditional Thai massage on heart rate variability and stress‐related parameters in patients with back pain associated with myofascial trigger points. Journal of Bodywork and Movement Therapies 2011;15(1):15‐23. [DOI] [PubMed] [Google Scholar]
Chatchawan 2005 {published data only}
- Chatchawan U, Thinkhamrop B, Kharmwan S, Knowles J, Eungpinichpong W. Effectiveness of traditional Thai massage versus Swedish massage among patients with back pain associated with myofascial trigger points. Journal of Bodywork and Movement Therapies 2005;9(4):298‐309. [Google Scholar]
Cherkin 2001 {published data only}
- Cherkin DC, Eisenberg D, Sherman KJ, Barlow W, Kaptchuk TJ, Street J, et al. Randomized trial comparing traditional Chinese medical acupuncture, therapeutic massage, and self‐care education for chronic low back pain. Archives of Internal Medicine 2001;161(8):1081‐8. [DOI] [PubMed] [Google Scholar]
- Meng SHIG, Cherkin DC. A randomized trial comparing acupuncture massage and self‐care for chronic low back pain. Hebei Journal of Traditional Chinese Medicine 2000;22:204. [Google Scholar]
Cherkin 2011 {published data only}
- Cherkin DC. A comparison of the effects of 2 types of massage and usual care on chronic low back pain: a randomized, controlled trial. Journal of the Australian Traditional‐Medicine Society 2011;17(4):239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherkin DC, Sherman KJ, Kahn J, Erro JH, Deyo RA, Haneuse SJ, et al. Effectiveness of focused structural massage and relaxation massage for chronic low back pain: protocol for a randomized controlled trial. Trials 2009;10:96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherkin DC, Sherman KJ, Kahn J, Wellman R, Cook AJ, Johnson E, et al. A comparison of the effects of 2 types of massage and usual care on chronic low back pain: a randomized, controlled trial. Annals of Internal Medicine 2011;155(1):1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherkin DC, Sherman KJ, Kahn J, Wellman R, Cook AJ, Johnson E, et al. Summaries for patients a comparison of massage therapy and usual medical care for chronic low back pain. Annals of Internal Medicine. 2011; Vol. 155:I‐28. [DOI] [PubMed]
Eghbali 2012 {published data only}
- Eghbali M, Safari R, Nazari F, Abdoli S. The effects of reflexology on chronic low back pain intensity in nurses employed in hospitals affiliated with Isfahan University of Medical Sciences. Iranian Journal of Nursing and Midwifery Research 2012;17(3):239‐43. [PMC free article] [PubMed] [Google Scholar]
Farasyn 2006 {published data only}
- Farasyn A, Meeusen R, Nijs J. A pilot randomized placebo‐controlled trial of roptrotherapy in patients with subacute non‐specific low back pain. Journal of Back and Musculoskeletal Rehabilitation 2006;19(4):111‐7. [Google Scholar]
Field 2007 {published data only}
- Field T, Hernandez‐Reif M, Diego M, Fraser M. Lower back pain and sleep disturbance are reduced following massage therapy. Journal of Bodywork and Movement Therapies 2007;11(2):141‐5. [Google Scholar]
Franke 2000 {published data only}
- Franke A. Acupuncture massage vs Swedish exercises in low back pain sufferers ‐ a randomised clinical trial in a 2x2 factorial design. Deutsche Zeitschrift für Akupunktur 2000;43:41. [Google Scholar]
- Franke A, Franke K, Gebauer S, Brockow T. Acupuncture massage vs. Swedish massage and individual exercises vs group exercises in low back pain sufferers: a randomized clinical trial in a 2x2 factorial design. Focus on Alternative and Complementary Therapies 2000;5(1):88‐9. [DOI] [PubMed] [Google Scholar]
- Franke A, Gebauer S, Franke K, Brockow T. Acupuncture massage vs Swedish massage and individual exercise vs group exercise in low back pain sufferers‐‐a randomized controlled clinical trial in a 2 x 2 factorial design [German]. Forschende Komplementärmedizin und klassische Naturheilkunde 2000;7(6):286‐93. [DOI] [PubMed] [Google Scholar]
Geisser 2005 {published data only}
- Geisser ME, Wiggert EA, Haig AJ, Colwell MO. A randomized controlled trial of manual therapy and specific adjuvant exercise for chronic low back pain. Clinical Journal of Pain 2005;21(6):463‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hernandez‐Reif 2001 {published data only}
- Hernandez‐Reif M, Field T, Krasnegor J, Theakston H. Lower back pain is reduced and range of motion increased after massage therapy. International Journal of Neuroscience 2001;106(3‐4):131‐45. [DOI] [PubMed] [Google Scholar]
Hsieh 2004 {published data only}
- Hsieh LLC, Kuo CH, Yen MF, Chen TH. A randomized controlled clinical trial for low back pain treated by acupressure and physical therapy. Preventive Medicine 2004;39(1):168‐76. [DOI] [PubMed] [Google Scholar]
Hsieh 2006 {published data only}
- Hsieh LLC, Kuo CHK, Lee LH, Yen AMFY, Chien KL, Chen THH. Treatment of low back pain by acupressure and physical therapy: randomised controlled trial. BMJ 2006;332(7543):696‐700. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kamali 2014 {published data only}
- Kamali F, Panahi F, Ebrahimi S, Abassi L. Comparison between massage and routine physical therapy in women with sub acute and chronic nonspecific low back pain. Journal of Back and Musculoskeletal Rehabilitation 2014;27(4):475‐80. [DOI] [PubMed] [Google Scholar]
Kumnerddee 2009 {published data only}
- Kumnerddee W. Effectiveness comparison between Thai traditional massage and Chinese acupuncture for myofascial back pain in Thai military personnel: a preliminary report. Journal of the Medical Association of Thailand 2009;92(Suppl 1):S117‐23. [PubMed] [Google Scholar]
Lara‐Palomo 2013 {published data only}
- Lara‐Palomo I, Aguilar‐Ferrándiz ME, Matarán Peñarrocha GA, Saavedra‐Hernández M, Granero‐Molina J, Fernández‐Sola C, et al. Short‐term effects of interferential current electro‐massage in adults with chronic non‐specific low back pain: a randomized controlled trial. Clinical Rehabilitation 2013;27(5):439‐49. [DOI] [PubMed] [Google Scholar]
Little 2008 {published data only}
- Hollinghurst S, Sharp D, Ballard K, Barnett J, Beattie A, Evans M, et al. Randomised controlled trial of Alexander technique lessons, exercise, and massage (ATEAM) for chronic and recurrent back pain: economic evaluation. BMJ 2008;337:a2656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little P, Lewith G, Webley F, Evans M, Beattie A, Middleton K, et al. Randomised controlled trial of Alexander technique lessons, exercise, and massage (ATEAM) for chronic and recurrent back pain. BMJ 2008;337:a884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little P, Lewith G, Webley F, Evans M, Beattie A, Middleton K, et al. Randomised controlled trial of Alexander technique lessons, exercise, and massage (ATEAM) for chronic and recurrent back pain. British Journal of Sports Medicine 2008;42(12):965‐8. [PubMed] [Google Scholar]
Mackawan 2007 {published data only}
- Mackawan S, Eungpinichpong W, Pantumethakul R, Chatchawan U, Hunsawong T, Arayawichanon P. Effects of traditional Thai massage versus joint mobilization on substance P and pain perception in patients with non‐specific low back pain. Journal of Bodywork and Movement Therapies 2007;11(1):9‐16. [Google Scholar]
Poole 2007 {published data only}
- Poole H, Glenn S, Murphy P. A randomised controlled study of reflexoloty for the management of chronic low back pain. European Journal of Pain 2007;11(8):878‐87. [DOI] [PubMed] [Google Scholar]
Preyde 2000 {published data only}
- Preyde M. Effectiveness of massage therapy for subacute low‐back pain: a randomized controlled trial. Canadian Medical Association Journal 2000;162(13):1815‐20. [PMC free article] [PubMed] [Google Scholar]
Quinn 2008 {published data only}
- Quinn F, Baxter D, Hughes C. Reflexology in the treatment of low back pain: a pilot RCT. Focus on Alternative & Complementary Therapies 2005;10(Suppl 1):44. [Google Scholar]
- Quinn F, Hughes CM, Baxter GD. Reflexology in the management of low back pain: a pilot randomised controlled trial. Complementary Therapies in Medicine 2008;16(1):3‐8. [DOI] [PubMed] [Google Scholar]
Sritoomma 2014 {published data only}
- Sritoomma N, Moyle W, Cooke M, O'Dwyer S. The effectiveness of Swedish massage with aromatic ginger oil in treating chronic low back pain in older adults: a randomized controlled trial. Complementary Therapies in Medicine 2014;22(1):26‐33. [DOI] [PubMed] [Google Scholar]
Yip 2004 {published data only}
- Yip YB, Tse SHM. The effectiveness of relaxation acupoint stimulation and acupressure with aromatic lavender essential oil for non‐specific low back pain in Hong Kong: a randomised controlled trial. Complementary Therapies in Medicine 2004;12(1):28‐37. [DOI] [PubMed] [Google Scholar]
Yoon 2012 {published data only}
- Yoon YS, Yu KP, Lee KJ, Kwak SH, Kim JY. Development and application of a newly designed massage instrument for deep cross‐friction massage in chronic non‐specific low back pain. Annals of Rehabilitation Medicine 2012;36(1):55‐65. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zheng 2012 {published data only}
- Zheng Z, Wang J, Gao Q, Hou J, Ma L, Jiang C, et al. Therapeutic evaluation of lumbar tender point deep massage for chronic non‐specific low back pain. Journal of Traditional Chinese Medicine 2012;32(4):534‐37. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Anderson 2005 {published data only}
- Anderson BD. Randomized clinical trial comparing active versus passive approaches to the treatment of recurrent and chronic low back pain [PhD thesis]. Miami, Florida: University of Miami, 2005. [Google Scholar]
Barnes 1997 {published data only}
- Barnes MF, Gronlund RT, Little MF, Personius WJ. Efficacy study of the effect of a myofascial release treatment technique on obtaining pelvic symmetry. Journal of Bodywork and Movement Therapies 1997;1(5):289‐96. [Google Scholar]
Buerger 1980 {published data only}
- Buerger AA. A controlled trial of rotational manipulation in low back pain. Manuelle Medizin 1980;18(2):17‐26. [Google Scholar]
Dishman 2001 {published data only}
- Dishman JD, Bulbulian R. Comparison of effects of spinal manipulation and massage on motoneuron excitability. Electromyography and Clinical Neurophysiology 2001;41(2):97‐106. [PubMed] [Google Scholar]
Farasyn 2007 {published data only}
- Farasyn A, Meeusen R. Effect of roptrotherapy on pressure‐pain thresholds in patients with subacute nonspecific low back pain. Journal of Musculoskeletal Pain 2007;15(1):41‐53. [Google Scholar]
Ferrell 1997 {published data only}
- Ferrell BA, Josephson KR, Pollan AM, Loy S, Ferrell BR. A randomized trial of walking versus physical methods for chronic pain management. Aging (Milano) 1997;9(1‐2):99‐105. [DOI] [PubMed] [Google Scholar]
Fraser 1993 {published data only}
- Fraser J, Kerr JR. Psychophysiological effects of back massage on elderly institutionalized patients. Journal of Advanced Nursing 1993;18(2):238‐45. [DOI] [PubMed] [Google Scholar]
Ginsberg 1987 {published data only}
- Ginsberg F, Famaey JP. A double‐blind study of topical massage with Rado‐Salil ointment in mechanical low‐back pain. Journal of International Medical Research 1987;15(3):148‐53. [DOI] [PubMed] [Google Scholar]
Godfrey 1984 {published data only}
- Godfrey CM, Morgan PP, Schatzker J. A randomized trial of manipulation for low‐back pain in a medical setting. Spine 1984;9(3):301‐4. [DOI] [PubMed] [Google Scholar]
Haas 2014 {published data only}
- Haas M, Vavrek D, Peterson D, Polissar N, Neradilek MB. Dose‐response and efficacy of spinal manipulation for care of chroniclow back pain: a randomized controlled trial. The Spine Journal 2014;14(7):1106–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hass M, Segman A, Peterson D, Aickin M, Vavrek D. Dose‐Response and Efficacy of Spinal Manipulation for Chronic Cervicogenic Headache: A Pilot Randomized Controlled Trial. Spine J 2010;10:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vavrek D, Haas M, Peterson D, Neradilek M, Polissar N. Determinants of Responders in a Dose‐Response Trial of Spinal Manipulation for the Care of Chronic Low Back Pain. The Journal of Alternative and Complementary Medicine 2014;20:A14‐A14. [Google Scholar]
- Vavrek D, Sharma R, Hass M. Cost‐Analysis Related to Dose‐Response for Spinal Manipulative Therapy for Chronic Low Back Pain: Outcomes from a Randomized Controlled Trial.. The Journal of Alternative and Complementary Medicine 2014;20 (5):A18‐A18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hoehler 1981 {published data only}
- Hoehler FK, Tobis JS, Buerger AA. Spinal manipulation for low back pain. JAMA 1981;245(18):1835‐8. [PubMed] [Google Scholar]
Kalaoukalani 2001 {published data only}
- Kalaoukalani D, Cherkin DC, Sherman KJ, Koepsell TD, Deyo RA. Lessons from a trial of acupuncture and massage for low back pain: patient expectations and treatment effects. Spine 2001;26(13):1418‐24. [DOI] [PubMed] [Google Scholar]
Kankaanpää 1999 {published data only}
- Kankaanpää M, Taimela S, Airaksinen O, Hänninen O. The efficacy of active rehabilitation in chronic low back pain. Effect on pain intensity, self‐experienced disability, and lumbar fatigability. Spine 1999;24(10):1034‐42. [DOI] [PubMed] [Google Scholar]
Koes 1992 {published data only}
- Koes BW, Bouter LM, Mameren H, Essers AH, Verstegen GJ, Hofhuizen DM, et al. A randomized clinical trial of manual therapy and physiotherapy for persistent back and neck complaints: subgroup analysis and relationship between outcome measures. Journal of Manipulative and Physiological Therapeutics 1993;16(4):211‐9. [PubMed] [Google Scholar]
- Koes BW, Bouter LM, Mameren H, Essers AH, Verstegen GM, Hofhuizen DM, et al. Randomized clinical trial of manipulative therapy and physiotherapy for persistent back and neck complaints: results of one year follow up. BMJ 1992;304(6827):601‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kolich 2000 {published data only}
- Kolich M, Taboun SM, Mohamed AI. Low back muscle activity in an automobile seat with a lumbar massage system. International Journal of Occupational Safety and Ergonomics 2000;6(1):113‐28. [DOI] [PubMed] [Google Scholar]
Kong 2012 {published data only}
- Kong LJ, Fang M, Zhan HS, Yuan WA, Tao JM, Qi GW, et al. Chinese massage combined with herbal ointment for athletes with nonspecific low back pain: a randomized controlled trial. Evidence‐based Complementary and Alternative Medicine 2012;2012:695726. [DOI] [PMC free article] [PubMed] [Google Scholar]
Konrad 1992 {published data only}
- Konrad K, Tatrai T, Hunka A, Vereckei E, Korondi I. Controlled trial of balneotherapy in treatment of low back pain. Annals of the Rheumatic Diseases 1992;51(6):820‐2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lauche 2012 {published data only}
- Lauche R, Wübbeling K, Lüdtke R, Cramer H, Choi KE, Rampp T, et al. Randomized controlled pilot study: pain intensity and pressure pain thresholds in patients with pain and low back pain before and after traditional East Asian "gua sha" therapy. American Journal of Chinese Medicine 2012;40(5):905‐17. [DOI] [PubMed] [Google Scholar]
Lei 2011 {published data only}
- Lei LM, Huang JJ, Lin GQ, Chen JS, Pang YH, He YF, et al. Lumbar intervertebral disc protrusion treated with Santong tuina therapy: a multi‐central randomized controlled trial [Chinese]. Zhongguo Zhen Jiu [Chinese Acupuncture & Moxibustion] 2011;31(3):253‐7. [PubMed] [Google Scholar]
Li 2006 {published data only}
- Li ZY, Chen PQ, Gong L, Gu F, Shen GQ, Yan ZT. Analgesic effect on lumbar intervertebral disc protrusion‐induced back‐leg pain by kneading method of taking the tender point as acupoint. Chinese Journal of Clinical Rehabilitative Tissue Engineering Research 2006;10(23):25‐7. [Google Scholar]
Lindström 1970 {published data only}
- Lindström A, Zachrisson M. Physical therapy on low back pain and sciatica. An attempt at evaluation. Scandinavian Journal of Rehabilitative Medicine 1970;2(1):37‐42. [PubMed] [Google Scholar]
Liu 2009 {published data only}
- Liu BX, Xu M, Huang CJ, Tang FY, Lou YM, Liang Z, et al. Controlled clinical trials on the treatment and prevention of shoulder and back fasciitis using horizontal bar exercises [Chinese]. Zhongguo Gu Shang [Chinese Journal of Orthopaedics and Traumatology] 2009;22(9):662‐4. [PubMed] [Google Scholar]
Maniche 1991 {published data only}
- Maniche C, Hesselsøe G, Bentzen L, Christensen I, Lundberg E. Clinical trial of intensive muscle training for chronic low back pain. Lancet 1988;2(8626‐7):1473‐6. [DOI] [PubMed] [Google Scholar]
- Manniche C, Lundberg E, Christensen I, Bentzen L, Hesselsøe G. Intensive dynamic back exercises for chronic low back pain: a clinical trial. Pain 1991;47(1):53‐63. [DOI] [PubMed] [Google Scholar]
- Manniche C, Lundberg E, Christensen I, Hesselsøe G, Bentzen L. Intensive dynamic back exercises for patients with chronic low back pain. A controlled study [Danish]. Ugeskrift for Laeger 1989;151(32):2030‐4. [PubMed] [Google Scholar]
Melzack 1980 {published data only}
- Melzack R, Jeans ME, Stratford JG, Monks RC. Ice massage and transcutaneous electrical stimulation: comparison of treatment for low‐back pain. Pain 1980;9(2):209‐17. [DOI] [PubMed] [Google Scholar]
Melzack 1983 {published data only}
- Melzack R, Vetere P, Finch L. Transcutaneous electrical nerve stimulation for low back pain. A comparison of TENS and massage for pain and range of motion. Physical Therapy 1983;63(4):489‐93. [DOI] [PubMed] [Google Scholar]
Movaghar 2012 {published data only}
- Movaghar M, Fathi M, Zandi M. The effect of foot reflexology on the reduction of low back pain caused by discopathy. Journal of Zanjan University of Medical Sciences and Health Services 2012;20(83):62‐9. [Google Scholar]
Pope 1994 {published data only}
- Hsieh CY, Phillips RB, Adams AH, Pope MH. Functional outcomes of low back pain: comparison of four treatment groups in a randomized controlled trial. Journal of Manipulative and Physiological Therapeutics 1992;15(1):4‐9. [PubMed] [Google Scholar]
- Pope M. A prospective randomized three week trial of spinal manipulation, transcutaneous muscle stimulation, massage and corset in the treatment of subacute low back pain. Proceedings Of The International Conference On Spinal Manipulation. 1993; Vol. 1:109‐10. [DOI] [PubMed]
- Pope MH, Philips RB, Haugh LD, Hsieh CY, MacDonald L, Haldeman S. A prospective randomized three‐week trial of spinal manipulation, transcutaneous muscle stimulation, massage and corset in the treatment of subacute low back pain. Spine 1994;19(22):2571‐7. [DOI] [PubMed] [Google Scholar]
Rasmussen‐Barr 2003 {published data only}
- Rasmussen‐Barr E, Nilsson‐Wikmar L, Arvidsson I. Stabilizing training compared with manual treatment in sub‐acute and chronic low‐back pain. Manual Therapy 2003;8(4):233‐41. [DOI] [PubMed] [Google Scholar]
Romanowski 2012 {published data only}
- Romanowski M, Romanowska J, Grześkowiak M. A comparison of the effects of deep tissue massage and therapeutic massage on chronic low back pain. Studies in Health Technology and Informatics 2012;176:411‐4. [PubMed] [Google Scholar]
Silveira 2006 {published data only}
- Silveira MA, Haupenthal A, Mannrich G, Torres SF. Physiotherapy performance in Ironman Brazil [Atuaçao fisioterapêutica no ironman Brasil]. Fisioterapia em Movimento 2006;19(1):35‐40. [Google Scholar]
Walach 2003 {published data only}
- Walach H, Güthlin C, König M. Efficacy of massage therapy in chronic pain: a pragmatic randomized trial. Journal of Alternative and Complementary Medicine 2003;9(6):837‐46. [DOI] [PubMed] [Google Scholar]
Wang 2005 {published data only}
- Wang B, Wu JX, Wang J. Active exercise and massage for nonspecific low back pain: a clinical randomized controlled trial [Chinese]. Chinese Journal of Clinical Rehabilitation 2005;9(10):1‐3. [Google Scholar]
Werners 1999 {published data only}
- Werners R, Pynsent PB, Bulstrode CJ. Randomized trial comparing interferential therapy with motorized lumbar traction and massage in the management of low back pain in a primary care setting. Spine 1999;24(15):1579‐84. [DOI] [PubMed] [Google Scholar]
Wilkinson 1997 {unpublished data only}
- Wilkinson TL. The effect of therapeutic touch on the experience of acute pain in postoperative laminectomy patients [Dissertation]. Bellarmine College,. Louisville, KY, 1997.
Wu 2004 {published data only}
- Wang B, Wu JX, Wang J. Active exercise and massage for nonspecific low back pain: A clinical randomized controlled trial [Chinese]. Chinese Journal of Clinical Rehabilitation 2005;9(10):1‐3. [Google Scholar]
- Wu JX, Wang B. Early intervention of aerobic exercise to rehabilitation of non‐specific low back pain. Chinese Journal of Clinical Rehabilitation 2004;8(26):5718‐20. [Google Scholar]
- Wu JX, Wang B. Early intervention of aerobic exercise to rehabilitation of non‐specific low back pain. Zhongguo Linchuang Kangfu 2004;8:5718‐20. [Google Scholar]
Zhang 2004 {published data only}
- Zhang JF, Chen WH. Curative effect of non‐operative therapy for the lumbar disc herniation. Chinese Journal of Clinical Rehabilitation 2004;8(11):2006‐7. [Google Scholar]
Zhou 2008 {published data only}
- Zhou XB, Jin T, Shi RH, Wang Z, Qi H, Huang MB, et al. Controlled clinical trials on the treatment of lumbar disk herniation by Dingweiban and Xieban manipulation. Zhongguo Gu Shang [China Journal of Orthopaedics and Traumatology] 2008;21(12):895‐8. [PubMed] [Google Scholar]
References to ongoing studies
Mandala 2001 {unpublished data only}
- Mandala G, Bordonato R, DiGangi A, Marino V, Negrini S. Effectiveness of back school or shiatsu massage reflex therapy in chronic low back pain: a prospective, randomized controlled blind trial. First World Congress of International Society of Physical and Rehabilitation Medicine. 2001:76.
Additional references
Bervoets 2015
- Bervoets DC, Luijsterburg PA, Alessie JJ, Buijs MJ, Verhagen AP. Massage therapy has short‐term benefits for people with common musculoskeletal disorders compared to no treatment: a systematic review. Journal of Physiotherapy 2015;61(3):106‐16. [PUBMED: 26093806] [DOI] [PubMed] [Google Scholar]
Boutron 2005
- Boutron I, Estellat C, Ravaud P. A review of blinding in randomized controlled trials found results inconsistent and questionable. Journal of Clinical Epidemiology 2005;58(12):1220‐6. [DOI] [PubMed] [Google Scholar]
Cheng 2014
- Cheng YH, Huang GC. Efficacy of massage therapy on pain and dysfunction in patients with neck pain: a systematic review and meta‐analysis. Evidence‐Based Complementary and Alternative Medicine 2014;2014:204360. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chou 2009
- Chou R, Loeser JD, Owens DK, Rosenquist RW, Atlas SJ, Baisden J, Carragee EJ, Grabois M, Murphy DR, Resnick DK, Stanos SP, Shaffer WO, Wall EM. American Pain Society Low Back Pain Guideline Panel. Interventional therapies, surgery, and interdisciplinary rehabilitation for low back pain: an evidence‐based clinical practice guideline from the American Pain Society. Spine (Phila Pa 1976) 2009 May 1;34(10):1066‐77. [PUBMED: 19363457] [DOI] [PubMed] [Google Scholar]
Dagenais 2008
- Dagenais S, Caro J, Haldeman S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J 2008 Jan‐Feb;8(1):8‐20. [PUBMED: 18164449] [DOI] [PubMed] [Google Scholar]
Deyo 1998
- Deyo R, Battie M, Beurskens AJHM, Bombarider C, Croft P, Koes BW, et al. Outcome measures for low back pain research. A proposal for standardized use. Spine 1998;23(18):2003‐13. [DOI] [PubMed] [Google Scholar]
Ernst 1999
- Ernst E. Massage therapy for low back pain: a systematic review. Journal of Pain and Symptom Management 1999;17(1):65‐9. [DOI] [PubMed] [Google Scholar]
Furlan 2009
- Furlan AD, Pennick V, Bombardier C, Tulder M, Editorial Board, Cochrane Back Review Group. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine 2009;34(18):1929‐41. [DOI] [PubMed] [Google Scholar]
Furlan 2012
- Furlan AD, Yazdi F, Tsertsvadze A, Gross A, Tulder M, Santaguida L, et al. A systematic review and meta‐analysis of efficacy, cost‐effectiveness, and safety of selected complementary and alternative medicine for neck and low‐back pain. Evidence‐Based Complementary and Alternative Medicine 2012;2012:953139. [DOI: 10.1155/2012/953139] [DOI] [PMC free article] [PubMed] [Google Scholar]
Garcia 2014
- Garcia JB, Hernandez‐Castro JJ, Nunez RG, Pazos MA, Aguirre JO, Jreige A, et al. Prevalence of low back pain in Latin America: a systematic literature review. Pain Physician 2014;17(5):379‐91. [PubMed] [Google Scholar]
GRADE 2009
- Schünemann H, Brożek J, Oxman A, editors. GRADE handbook for grading quality of evidence and strength of recommendationVersion 3.6. http://tech.cochrane.org/gradepro 2009.
Gross 1999
- Gross AR, Aker PD, Goldsmith CH, Peloso P. Physical medicine modalities for mechanical neck disorders. Cochrane Database of Systematic Reviews 1999, Issue 2. [DOI: 10.1002/14651858.CD000961] [DOI] [PMC free article] [PubMed] [Google Scholar]
Guyatt 2013
- Guyatt G, Thorlund K, Oxman A, Walter S, Patrick D, Furukawa T, et al. GRADE guidelines: 13. Preparing summary of findings tables and evidence profiles ‐ continuous outcomes. Journal of Clinical Epidemiology 2013;66(2):173‐83. [DOI] [PubMed] [Google Scholar]
Haldeman 2008
- Haldeman S, Dagenais S. A supermarket approach to the evidence‐informed management of chronic low back pain. Spine Journal 2008;8(1):1‐7. [DOI] [PubMed] [Google Scholar]
Haraldsson 2006
- Haraldsson BG, Gross AR, Myers CD, Ezzo JM, Morien A, Goldsmith C, et al. Massage for mechanical neck disorders. Cochrane Database of Systematic Reviews 2006, Issue 3. [DOI: 10.1002/14651858.CD004871.pub3] [DOI] [PubMed] [Google Scholar]
Harris 2014
- Harris PE, Cooper KL, Relton C, Thomas KJ. Prevalence of visits to massage therapists by the general population: a systematic review. Complement Ther Clin Pract 2014 Feb;20(1):16‐20. [PUBMED: 24439639] [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Hoy 2012
- Hoy D, Bain C, Williams G, March L, Brooks P, Blyth F, et al. A systematic review of the global prevalence of low back pain. Arthritis and Rheumatism 2012;64(6):2028‐37. [PUBMED: 22231424] [DOI] [PubMed] [Google Scholar]
Hägg 2003
- Hägg O, Fritzell P, Nordwall A, Swedish Lumbar Spine Study Group. The clinical importance of changes in outcome scores after treatment for chronic low back pain. European Spine Journal 2003;12(1):12‐20. [DOI] [PubMed] [Google Scholar]
Jensen 1990
- Jensen OK, Nielsen FF, Vosmar L. An open study comparing manual therapy with the use of cold packs in the treatment of post‐traumatic headache. Cephalalgia 1990;10(5):241‐50. [DOI] [PubMed] [Google Scholar]
Kamper 2010
- Kamper SJ, Maher CG, Hancock MJ, Koes BW, Croft PR, Hay H. Treatment‐based subgroups of low back pain: a guide to appraisal of research studies and a summary of current evidence. Best Practice & Research. Clinical Rheumatology 2010;24(2):181‐91. [DOI] [PubMed] [Google Scholar]
King 2011
- King MT. A point of minimal important difference (MID): a critique of terminology and methods. Expert Review of Pharmacoeconomics & Outcomes Research 2011;11(2):171‐84. [DOI] [PubMed] [Google Scholar]
Kjaergard 2001
- Kjaergard LL, Villumsen JV, Gluud C. Reported methodologic quality and discrepancies between large and small randomized trials in meta‐analyses. Annals of Internal Medicine 2001;135(11):982‐9. [DOI] [PubMed] [Google Scholar]
Kong 2013
- Kong LJ, Zhan HS, Cheng YW, Yuan WA, Chen B, Fang M. Massage therapy for neck and shoulder pain: a systematic review and meta‐analysis. Evidence‐Based Complementary and Alternative Medicine 2013;2013:613279. [DOI] [PMC free article] [PubMed] [Google Scholar]
Melzack 1996
- Melzack R, Wall PD. The Challenge of Pain. 2nd Edition. London: Penguin Books, 1996. [Google Scholar]
Moher 2001
- Moher D, Schulz KF, Altman DG, CONSORT GROUP (Consolidated Standards of Reporting Trials). The CONSORT statement: revised recommendations for improving the quality of reports of parallel‐group randomized trials. Annals of Internal Medicine 2001;134(8):657‐62. [DOI] [PubMed] [Google Scholar]
Moyer 2004
- Moyer CA, Rounds J, Hannum JW. A meta‐analysis of massage therapy research. Psychological Bulletin 2004;130(1):3‐18. [DOI] [PubMed] [Google Scholar]
Mueller 2007
- Mueller PS, Montori VM, Bassler D, Koenig BA, Guyatt GH. Ethical issues in stopping randomized trials early because of apparent benefit. Annals of Internal Medicine 2007;146(12):878‐81. [DOI] [PubMed] [Google Scholar]
RefMan 2010
- Reference Manager (RefMan) [Computer program]. Version 12.0.3. Philadelphia, PA: Thomson Reuters, 2010.
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Scherer 2007
- Scherer RW, Langenberg P, Elm E. Full publication of results initially presented in abstracts. Cochrane Database of Systematic Reviews 2007, Issue 2. [DOI: 10.1002/14651858.MR000005.pub3] [DOI] [PubMed] [Google Scholar]
Sherman 2006
- Sherman KJ, Dixon MW, Thompson D, Cherkin DC. Development of a taxonomy to describe massage treatments for musculoskeletal pain. BMC Complementary and Alternative Medicine 2006;6:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
van Tulder 2003
- Tulder M, Furlan A, Bombardier C, Bouter L, Editorial Board of the Cochrane Collaboration Back Review Group. Updated method guidelines for systematic reviews in the Cochrane Collaboration Back Review Group. Spine 2003;28(12):1290‐9. [DOI] [PubMed] [Google Scholar]
Vickers 1999
- Vickers A, Zollman C. ABC of complementary medicine. Massage therapies. BMJ 1999;319(7219):1254‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vos 2010
- Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990‐2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2010;380(9859):2163‐96. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wagner 2009
- Wagner M, Balk EM, Kent DM, Kasiske BL, Ekberg H. Subgroup analyses in randomized controlled trials: the need for risk stratification in kidney transplantation. American Journal of Transplantation 2009;9(10):2217‐22. [DOI: 10.1111/j.1600-6143.2009.02802.x] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wahlgren 2008
- Wahlgren N, Ahmed N, Eriksson N, Aichner F, Bluhmki E, Dávalos A, et al. Multivariable analysis of outcome predictors and adjustment of main outcome results to baseline data profile in randomized controlled trials: Safe Implementation of Thrombolysis in Stroke‐MOnitoring STudy (SITS‐MOST). Stroke 2008;39(12):3316‐22. [DOI] [PubMed] [Google Scholar]
Weber 1994
- Weber MD, Servedio FJ, Woodall WR. The effects of three modalities on delayed onset muscle soreness. Journal of Orthopaedic and Sports Physical Therapy 1994;20(5):236‐42. [DOI] [PubMed] [Google Scholar]
Weinrich 1990
- Weinrich SP, Weinrich MC. The effect of massage on pain in cancer patients. Applied Nursing Research 1990;3(4):140‐5. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Furlan 2000
- Furlan AD, Brosseau L, Welch V, Wong J. Massage for low back pain. Cochrane Database of Systematic Reviews 2000, Issue 4. [DOI: 10.1002/14651858.CD001929.pub2] [DOI] [PubMed] [Google Scholar]
Furlan 2002
- Furlan AD, Brosseau L, Imamura M, Irvin E. Massage for low back pain. Cochrane Database of Systematic Reviews 2002, Issue 2. [DOI: 10.1002/14651858.CD001929] [DOI] [PubMed] [Google Scholar]
Furlan 2008
- Furlan AD, Imamura M, Dryden T, Irvin E. Massage for low‐back pain. Cochrane Database of Systematic Reviews 2008, Issue 4. [DOI: 10.1002/14651858.CD001929.pub2] [DOI] [PubMed] [Google Scholar]


