Abstract
Objective
A reliable measure of the burden of inflammatory bowel diseases (IBDs), including ulcerative colitis and Crohn’s disease, are essential to monitor their epidemiology and plan appropriate health services.
Methods
This is a population-based study carried out in the Milan Agency for Health Protection. Incident and prevalent cases were identified according to specific codes in hospital discharges and copayment exemptions. Age-standardized incidence rates were computed for 2015–2018 and yearly rates from 2010 to 2018, as well as annual prevalence and prevalence on 31 December 2018. Incidence and prevalence estimates for Italy were also produced.
Results
During 2015–2018, 3434 citizens had an IBD diagnosis, 2154 (62.7%) ulcerative colitis and 1.280 (37.3%) Crohn’s disease. Age-adjusted incidence rates were 15.3 [95% confidence interval (CI), 14.7–16.0] for ulcerative colitis and 9.4 (8.9–9.9) for Crohn’s disease. Incidence was stable during 2010–2018 for both diseases. On 31 December 2018, there were 15 141 prevalent patients, corresponding to a proportion of 442.3 every 100 000 inhabitants/year (95% CI, 435.6–449.8). Prevalence proportion has increased to around +10% per year from 2010 to 2018. Projections for Italy assessed the burden of IBD in more than 15 000 new cases/year (55% ulcerative colitis) and around 260 000 prevalent cases (62% ulcerative colitis).
Conclusions
The exploitation of administrative data provides reliable and up-to-date measures of the burden of disease. Incidence of IBDs is stable while prevalence notably grows. The burden of IBDs and the consequent need for care and follow-up is going to increase in the future.
Keywords: burden, Crohn’s disease, incidence, prevalence, ulcerative colitis
Introduction
Crohn’s disease and ulcerative colitis are chronic inflammatory bowel diseases (IBDs) of unknown etiology, characterized by a state of chronic inflammation of the gastrointestinal system and even extraintestinal involvement [1].
IBDs are historically more frequent in Western-style countries with the highest rates in North America, Europe and Australia [2]. Moreover, IBDs incidence and prevalence are generally increasing [3], with the recent growth of rates also in Africa, Asia and South America [4].
In Italy, the available incidence estimates are generally based on relatively small populations. A review based on 16 studies reported for the early 2010s incidence rates of Crohn’s disease as 3.5–4 cases per 100 000 inhabitants per year [5], sensibly lower than those measured in other studies [6,7]. As regards ulcerative colitis (UC), incidence ranged from around 10 [7,8] to around 15 cases per 100 000 inhabitants per year [6,9,10].
Global Burden of Disease (GBD) estimates for 2017 account IBD prevalence in Italy as 76 581 cases [3]. However, a no-profit IBDs patients’ organization, Associazione Nazionale per le Malattie Infiammatorie Croniche dell’Intestino (https://amiciitalia.eu), doubles or triples the estimate up to 150 000–200 000 prevalent cases [11]. Moreover, national projections based on recently estimated prevalence for the Tuscan region, they would indicate 500 000 the order of magnitude of the cases in our country [12].
IBDs are life-lasting diseases with a clinical course that alternates relative well-being with exacerbations [13]. Therefore, IBD patients request periodic endoscopic, radiologic and biopsic follow-up, and pharmaceutical (including immunosuppressive and biological drugs) and surgical treatment [14].
The present study aims to provide a reliable population-based measure of IBDs incidence and prevalence for the area of the Milan Agency for Health Protection (AHP) and use them also for national estimates.
Methods
Study design
This is a retrospective cohort study based on current healthcare databases of the AHP.
Population and data sources
IBDs cases were identified among the residents in the area (about 3.5 million) registered with the regional universal coverage healthcare system. For IBDs definition, we applied the algorithms defined by the Region Lombardia (Regional Decision No. 6164 and No. 7655) [15].
The period considered for the identification of IBD patients goes from 1 January 2000 to 31 December 2018.
Data anonymization was provided by an internal code used in every administrative database and was used for deterministic record linkage on a unique identifier.
In more details, our analysis used record-linkage procedures of the following administrative databases:
-
(1)
AHP population registry.
-
(2)
Hospital records, selecting ICD9-CM codes in principal and secondary diagnosis: 555. xx (Crohn’s disease) and 556. xx (ulcerative colitis). We considered 2010–2018 as the first years of hospitalization (cases diagnosed in 2000–2009 were excluded). This source of information includes all the patients who needed admission to a public or an accredited private hospital with a specific IBD code mentioned in the diagnosis. No information from scheduled outpatient visits or endoscopy unit was available.
-
(3)
Exemption registry, selecting people with code 009.* This source contains all IBD patients who had applied for a medical exemption certificate for IBD-related medical examinations and services. The certificate is issued upon presentation of medical records, pathology reports, etc., demonstrating the diagnosis.
The identification of subjects relied on specific administrative codes. Therefore, clinical, pathological and endoscopic information was not available.
Individual characteristics
Demographic variables, including the type of IBD, age, gender and comorbidity were extracted from the current healthcare databases of the AHP.
The available sources of information did not include personal (e.g. family history of IBD, socioeconomic characteristics, smoking status, etc.) or IBD characteristics (pattern and extent of disease, and presence of extraintestinal manifestations, etc.).
Estimation of incidence and prevalence
Incidence has been computed for both single years during 2010–2018 and as an average for 2015–2018. Cases with a first hospitalization or tax exemption from 2000 to 2009 were excluded from the incidence. Results include also patients who moved outside the area or deceased after diagnosis. The denominator for each year/period is the resident population (the mean between the population on 1 January and that on 31 December) [16].
For prevalence, we computed both prevalences on 31 December 2018 and annual prevalence from 2010 to 2018. The former computation included at the numerator all the IBD patients alive on the date and at the denominator the AHP population. Annual prevalence includes subjects diagnosed with ulcerative colitis or Crohn’s disease during the year, included those deceased or who moved outside the area during the year, and as the denominator the mean resident population [16]. Yearly and point prevalent cases may have been diagnosed since 2000.
Statistical analysis
The characteristics of the cohort were described using absolute numbers, percentages and mean.
Variables distributions have been tested with Student’s t-test if continuous and χ2 if categorical.
Incidence rates, annual prevalence and prevalence proportions on 31 January 2018 have been age-standardized according to the most recent European standard population [17]. 95% Confidence intervals (CIs) were also computed.
Linear regression has been applied for evaluating the annual average percent change (AAPC) of age-standardized incidence trends during 2010–2018.
Projections to Italy have been carried out applying, for incidence, 2015–2018 age, sex and disease-specific rates, and for prevalence, age, sex and disease-specific proportions measured in AHP on 31 December 2018, to the resident Italian population on 1 January 2019 [16].
All the analyses have been carried out with Stata 12.1 (www.stata.com).
Ethics committee approval and consent to participate
This is an observational study based on data routinely collected by the Agency for Health Protection (ATS) of Milan, a public body of the Regional Health Service – Lombardy Region. The ATS has among its institutional functions, the government of the care pathway at the individual level in the regional social and healthcare system, the evaluation of the services provided to, and the outcomes of patients residing in the covered area. According to the function attributed to the ATS from the Regional legislation (R.L. 23/2015, 11 August /2015 http://normelombardia.consiglio.regione.lombardia.it/NormeLombardia/Accessibile/main.aspx?view=showdoc&iddoc=lr002015081100023), ethical approval was deemed not necessary. This study is also ethically compliant with the National Law (D.Lgs. 101/2018 https://www.gazzettaufficiale.it/eli/id/2018/09/04/18G00129/sg) and the ‘General Authorisation to Process Personal Data for Scientific Research Purposes’ (n.8 and 9/2016, referred to in the Data Protection Authority action of 13 December 2018 https://www.garanteprivacy.it/home/docweb/-/docweb-display/docweb/9068972). Administrative permission to perform the study was granted by the General Direction of the Agency for Health Protection (ATS) of Milan, resolution n°36 16 January 2018 (http://80.88.164.206/ULISS-eAsl/Bacheca/coatti01.aspx?bac_codice=50&idSessione=p1wyp32vyc3urymjzo5vvh45&men_id=00.00.00). Data were anonymized before its use for the present study.
Results
Incidence
During 2015–2018 in the AHP, there were 3434 newly diagnosed IBD patients, 2157 (62.7%) with ulcerative colitis (among them 45.8% women) and 1280 (37.3%) affected by Crohn’s disease (45.2% women).
The mean age at diagnosis was 45.3 years[standard deviation (SD) 20.0] for Crohn’s disease (higher among women, 47.2 than men 43.7 years, P = 0.0016) and 51.1 years (SD 21.5) for ulcerative colitis (52.1 for women and 50.3 for men, P = 0.047).
The case-series comprised 211 cases diagnosed before 18 years of age, 119 (56.4%) ulcerative colitis and 92 (43.6%) Crohn’s disease.
The average crude incidence rate for 2015–2018 was 15.6 cases per 100 000 citizens/years for ulcerative colitis (95% CI, 14.5–16.8) and 9.3 for Crohn’s disease (95% CI, 7.8–10.8) (Table 1). In both diseases, crude rates are higher among men [ulcerative colitis 17.5 (15.3–19.7) and Crohn’s disease 10.5 (7.6–13.4)] than women [ulcerative colitis 13.9 (11.6–16.2) and Crohn’s disease 8.2 (5.1–11.2)].
Table 1.
Milan Agency for Health Protection inflammatory bowel diseases, 2015–2018: number of cases, crude and age-standardized incidence rates per 100.000 people/year with corresponding 95% confidence intervals, for Crohn’s disease and ulcerative colitis and sex
| Crohn’s disease | Ulcerative colitis | |||||||
|---|---|---|---|---|---|---|---|---|
| n. | Crude rate | Std. rate | CI 95% | n. | Crude rate | Std. rate | CI 95% | |
| Women | 579 | 8.2 | 8.3 | 7.6–8.9 | 987 | 13.9 | 13.5 | 12.6–14.3 |
| Men | 701 | 10.5 | 10.6 | 9.0–11.4 | 1167 | 17.5 | 17.4 | 16.4–18.4 |
| People | 1280 | 9.3 | 9.4 | 8.9–9.9 | 2154 | 15.6 | 15.3 | 14.7–16.0 |
CI, confidence intervals.
In Table 1, there are the age-standardized rates with corresponding 95% CIs. Incidence rates were higher for UC than for Crohn’s disease for women (13.5 vs. 8.3), men (17.4 vs. 10.6) and people (15.3 vs. 9.4).
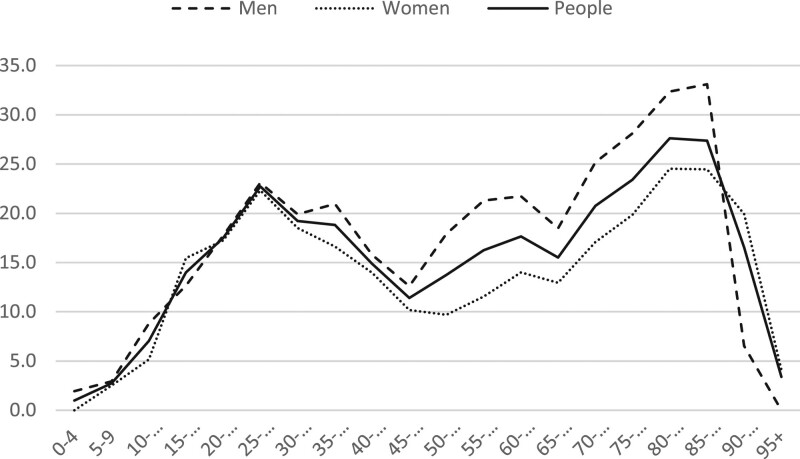
As regards the age distribution, ulcerative colitis patients showed (Fig. 1), a bimodal pattern in both sexes with two peaks, one around the 20 years and another, more evident, around the eighth decade of life (more pronounced for men).
Fig. 1.
Milan Agency for Health Protection. Ulcerative colitis: average age-specific incidence rates per 100.000 inhabitants, 2015–2018, by sex.
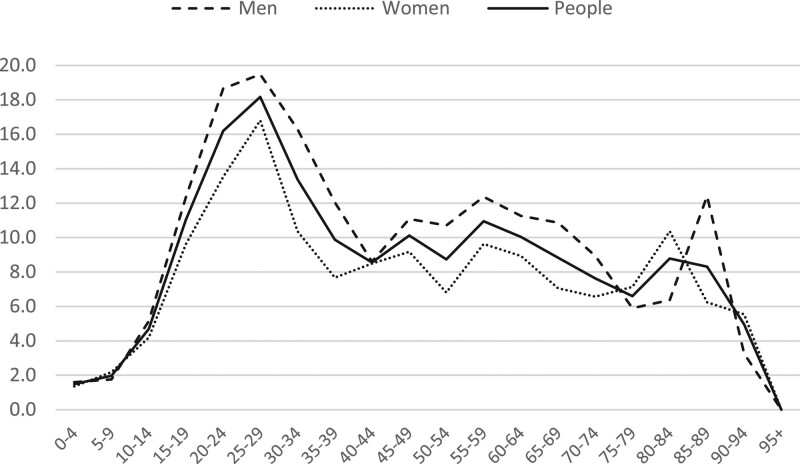
Crohn’s disease is more frequent during the second and third decades (Fig. 2), then age-specific rates decrease.
Fig. 2.
Milan Agency for Health Protection. Crohn’s disease, average age-specific incidence rates per 100.000 inhabitants, 2015–2018, by sex.
During 2010–2018 in the AHP, there were 7667 newly diagnosed IBD patients, 4881 (63.7%) with ulcerative colitis (among them 46.6% women) and 2786 (36.3%) affected by Crohn’s disease (45.8% women).
The mean age at diagnosis was 45.0 years (SD 20.2) for Crohn’s disease (higher among women, 46.2 than men 44.0 years, P = 0.0044) and 50.4 years (SD 20.7) for ulcerative colitis (50.8 for women and 50.1 for men, P = 0.28).
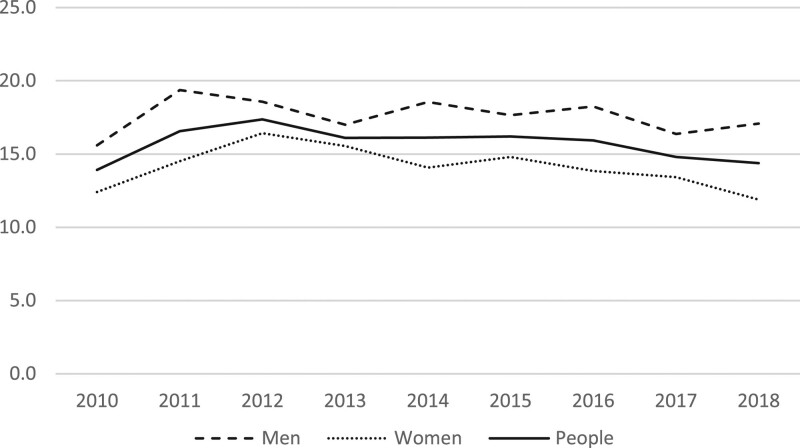
As regards the time trend during 2010–2018, age-standardized incidence rates for UC showed a stable pattern for men (AAPC = −0.26, 95% CI, −2.28; +1.76) and women (AAPC = −0.69, −2.28; +0.91) (Fig. 3).
Fig. 3.
Milan Agency for Health Protection. Ulcerative colitis, annual age-standardized incidence rates for 2010–2018, by sex.
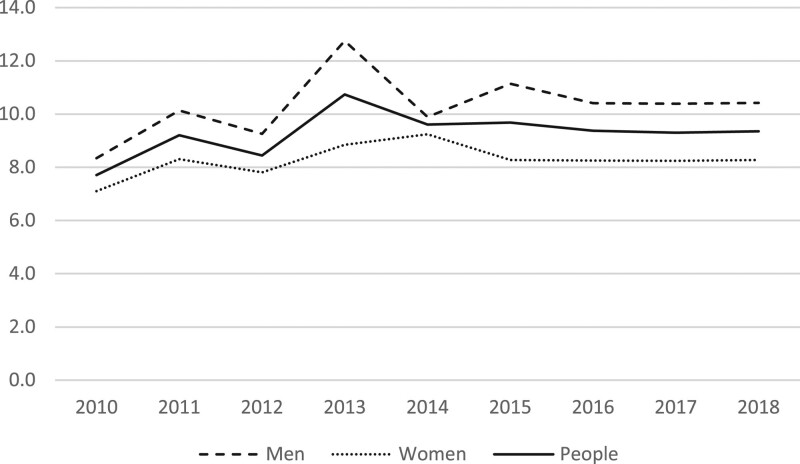
Besides, age-standardized incidence rates for Crohn’s disease show a stable trend (people AAPC = 1.39, −1.29; +4.03) in both sexes during the analyzed years (Fig. 4).
Fig. 4.
Milan Agency for Health Protection. Crohn’s disease, annual age-standardized incidence rates for 2010–2018, by sex.
Point prevalence
On 31 December 2018, in the AHP population there were 15 141 people with a previous IBD diagnosis, 9420 (62.2%) with ulcerative colitis and 5721 (37.8%) Crohn’s disease.
Such prevalence has to be considered as 18-year prevalence because the source of information from which data have been retrieved are available since 2000.
The average age at diagnosis is younger for Crohn’s disease than ulcerative colitis both among men (41.8 vs. 46.0, P < 0.001) and women (43.2 vs. 46.4, P < 0.001). The length of disease is homogeneously over 10 years, 10.7 for Crohn’s disease (range 0.2–19.7 years) and 10.7 ulcerative colitis (0.2–19.7). About half of the patients did not have any comorbidity, around one-fourth had 1, about 15% two and 8–10% three or more.
The most frequent comorbidities were cardiovascular diseases (31.3%), cancer (16.0%), endocrine diseases (13.9%), chronic obstructive pulmonary disease (8.7%), diabetes (7.4%), neurologic diseases (4.8%), immunologic diseases (3.8%) and chronic renal failure (1.5%).
The crude point prevalence, that is the proportion of citizens in the population that on 31 December 2018 had a previous IBD diagnosis, is 437.0 (430.1–444.0) every 100 000 inhabitants, 271.9 (266.4–277.4) with ulcerative colitis and 165.1 (160.9–169.4) Crohn’s disease.
As regards sex and a specific disease, for ulcerative colitis prevalence was 308.7 (300.3–317.1) for men and 237.3 (230.1–244.4) for women and Crohn’s disease 184.1 (177.6–190.6) 147.2 (141.6–152.9), respectively.
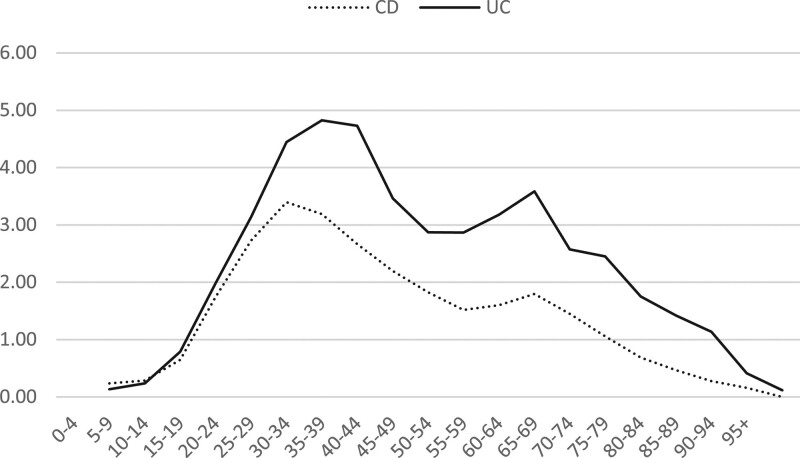
The point prevalence for both ulcerative colitis and Crohn’s disease changes in different ages (Fig. 5). The highest proportion occurs (in both sexes) during the 3°e 4° decade where proportions reach almost 8‰ for ulcerative colitis and 3‰ for Crohn’s disease, and with a second smaller peak, in particular for ulcerative colitis, in the 7° decade.
Fig. 5.
Milan Agency for Health Protection. Age-specific point prevalence (on 31 December 2018) for Crohn’s diseases and ulcerative colitis.
The median age of prevalent patients was 43.2 years (mean 44.7 and SD 17.4 years).
Figure 5 clearly shows that point prevalence changes across ages, therefore, to produce comparable measures overtime we computed age-standardized point prevalence.
Age-standardized prevalence is for ulcerative colitis 304.7 per 100 000 subject/year (296.3–313.0) for men and 242.8 (235.3–250.2) among women (272.9 for people), for Crohn’s disease 184.4 (177.9–191.0) and 155.1 (149.0–161.1), respectively (1.69.8 for people). The overall age-standardized prevalence proportion of IBD is 489.1 (478.5–499.7) for men, 397.8 (388.2–407.4) women and 442.7 (435.6–449.8) people.
Period prevalence
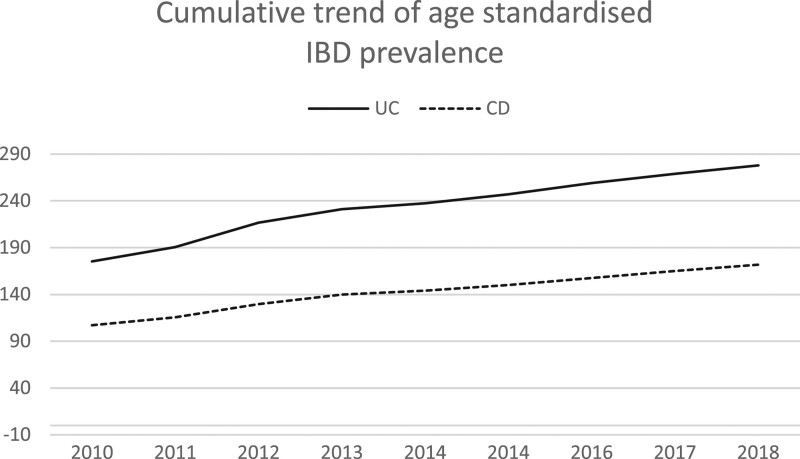
In Fig. 6, age-standardized cumulative prevalence for Crohn’s disease and ulcerative colitis are shown for single years, from 2010 to 2018. Age-standardized prevalence increased for ulcerative colitis from 175.3 per 100 000 people/year (170.9–179.9) in 2010 to 277.9 (272.3–283.5) with an AAPC of +12.4 (10.4–14.5). Annual cumulative prevalence has grown also for Crohn’s disease, from 107.1 to 171.8, with AAPC = +7.9 (6.9–8.8).
Fig. 6.
Milan Agency for Health Protection. Inflammatory bowel diseases (IBDs) age-standardized yearly cumulative prevalence for Crohn’s diseases and ulcerative colitis from 2010 to 2018.
Projections to Italy
If IBD incidence was in Italy similar to that measured in Milan AHP during 2015–2018, the expected yearly number of IBD incident patients in 2019 would be 15 189, 8332 ulcerative colitis and 6874 Crohn’s disease.
As regards prevalence, projecting what measured in Milan AHP on 31 December 2018, to the Italian population, the expected number of prevalent IBD patients on 1 January 2019 would be 264.013 subjects, 164.250 ulcerative colitis and 99.763 Crohn’s disease.
In Table 2, numbers are presented for 5-year age-groups, sex and type of IBD.
Table 2.
Estimate of the point prevalence of inflammatory bowel diseases in Italy on 1 January 2019, by disease and sex
| Crohn’s disease | Ulcerative colitis | IBDs | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Men | Women | All | Men | Women | All | Men | Women | All | |
| 0–4 | 274 | 289 | 562 | 225 | 96 | 322 | 499 | 385 | 884 |
| 5–9 | 414 | 367 | 782 | 381 | 267 | 648 | 796 | 634 | 1430 |
| 10–14 | 1068 | 791 | 1859 | 1226 | 1037 | 2263 | 2294 | 1827 | 4122 |
| 15–19 | 2771 | 2276 | 5047 | 2808 | 2929 | 5737 | 5579 | 5206 | 10 784 |
| 20–24 | 4478 | 3687 | 8165 | 4957 | 4432 | 9389 | 9435 | 8119 | 17 554 |
| 25–29 | 5750 | 5155 | 10 905 | 7594 | 6687 | 14 282 | 13 345 | 11 842 | 25 187 |
| 30–34 | 5924 | 4814 | 10 738 | 8836 | 7414 | 16 250 | 14 759 | 12 229 | 26 988 |
| 35–39 | 5376 | 4493 | 9869 | 9569 | 7940 | 17 508 | 14 945 | 12 432 | 27 377 |
| 40–44 | 5551 | 4140 | 9691 | 8487 | 6803 | 15 290 | 14 038 | 10 943 | 24 981 |
| 45–49 | 4716 | 4083 | 8799 | 7767 | 6075 | 13 842 | 12 483 | 10 158 | 22 640 |
| 50–54 | 4315 | 3175 | 7491 | 8459 | 5678 | 14 137 | 12 775 | 8853 | 21 628 |
| 55–59 | 4047 | 3027 | 7074 | 8528 | 5530 | 14 058 | 12 575 | 8557 | 21 132 |
| 60–64 | 3748 | 3177 | 6925 | 8347 | 5484 | 13 831 | 12 096 | 8661 | 20 756 |
| 65–69 | 2792 | 2292 | 5084 | 5134 | 3891 | 9025 | 7926 | 6183 | 14 109 |
| 70–74 | 1647 | 1775 | 3422 | 3987 | 3957 | 7945 | 5635 | 5732 | 11 367 |
| 75–79 | 668 | 1194 | 1863 | 2340 | 2453 | 4792 | 3008 | 3647 | 6655 |
| 80–84 | 272 | 739 | 1011 | 1435 | 1667 | 3102 | 1707 | 2406 | 4113 |
| 85–89 | 151 | 229 | 380 | 528 | 1037 | 1566 | 679 | 1266 | 1945 |
| 90–94 | 21 | 74 | 95 | 42 | 204 | 246 | 63 | 278 | 341 |
| 95+ | 0 | 0 | 0 | 0 | 19 | 19 | 0 | 19 | 19 |
| 53 986 | 45 777 | 99 763 | 90 650 | 73 600 | 164 250 | 144.636 | 119.377 | 264.013 | |
IBD, inflammatory bowel disease.
Assuming the observed rate of increase in cumulative prevalence stable over time and valid for Italy, the overall national burden of IBDs will approach half a million cases in 2025 (around 331 000 ulcerative colitis and 158 000 Crohn’s disease).
Discussion
This is a real-world study carried out in a northern Italian area where the health services are highly digitized and belong to a unique informatics system. Such administrative records have been widely used to evaluate a broad range of diseases [18–22], including the economic burden of IBDs [23]. The AHP provides care to about three 3 500 000 inhabitants. Therefore, the current study used large administrative databases related to a large and unselected population. Moreover, in the Milan area, IBDs are formally defined together with other acute and chronic diseases [15]. Therefore, the results of the present study can be reproduced and compared.
We measured, in a dataset of more than 3400 IBDs patients, an age-standardized incidence rate of 15.3 for ulcerative colitis and 9.4 for Crohn’s disease per 100.000 people/year. Such values are comparable with those computed in further recent Italian population-based studies [6,8–10]. Besides, the incidence for both ulcerative colitis and Crohn’s disease in the present study agreed with recent UK estimates [24].
Incidence was significantly higher among men than women for both ulcerative colitis and Crohn’s disease.
Incidence showed stable rates during the analyzed period, for both ulcerative colitis and Crohn’s disease, in agreement with what was recently reported worldwide [4].
The point prevalence of IBD on 31 December 2018 was 442.7 every 100 000 inhabitants, 272.9 with ulcerative colitis and 169.8 Crohn’s disease. These values are higher than those identified for Southern Europe [4].
We measured higher prevalence among men in both ulcerative colitis and Crohn’s disease. This result agrees with other Italian studies [6,9] but it is the opposite than in a recent GBD estimate [3]. We are not able to argue the reasons for such a difference. GBD methodology aims at worldwide estimates, and some of the applied assumptions may contribute to explain such differences in comparison with our observed data.
The age of onset of IBD varies in different studies. Early young age of onset has been related to a more severe clinical course and aggressive surgical and medical therapy. However, the role of age-related guidelines also contributes to the heterogeneity of results. The mean age measured in this survey was in agreement with most of the European studies collected in a review with a younger age of onset for Crohn’s disease than for UC, in both sexes [25].
However, considering the quite young age of IBDs onset and their good prognosis, prevalence estimates are strongly influenced by the length of the period for which data are available. In the present study, prevalence is up to 18 years. This may be the most sensible explanation for the difference with the Di Domenicantonio et al. [9] values, based on the same selection criteria but for a sensibly shorter period.
Half of the Milan prevalent cases were younger than 44 years that corresponds, for the general population, to at least 40 years of expected life [16]. Some studies reported no differences in general mortality between IBDs patients and the general population [26,27]. On the contrary, others evidenced an excess risk of death for IBDs patients with both child-onset [28] and late-onset [29]. However, the measure of the hazard ratios cannot seriously affect the overall amount of the estimated cohort.
Moreover, the prevalence proportion has increased in the Milan area from 2010 to 2018 at an impressive annual rate of around +12% per year for ulcerative colitis and +7% for Crohn’s disease. Therefore, the availability of figures based on a long period of follow-up makes more realistic the estimates and boosts the burden of prevalence.
We applied the figures measured in the AHP to the Italian population to provide the order of magnitude of the burden of newly diagnosed and prevalent IBDs cases. The suitability of Milan estimates for the whole country may be debated. Previous Italian studies have documented, for Crohn’s disease, average lower incidence rates than in Milan. However, many of these studies were based on small numbers [5]. In addition, also a decreasing north to south trend is arguable. In fact, the highest Southern European rate for Crohn’s disease has been documented in the South of Italy [30]. The pattern is even more complex considering that a particularly low prevalence, especially for Crohn’s disease (Crohn’s disease 15 × 104, ulcerative colitis 124 × 104), has been measured in a different Italian southern region [31].
International studies show that countries seem harmonized for IBDs level according to their level of westernization [3,4].
We are well aware of the limitations of our study that derive from the use of administrative data. For example, the use of hospital data may have underreported the true incidence/prevalence excluding mild cases. Moreover, a possible weakness is that we identified patients based on specific hospitalization and exemption codes, therefore errors in such codes could bring to underestimate. Moreover, subjects who were not registered with the regional universal coverage healthcare system could not be identified. However, both conditions might bring a negligible underestimation considering that in Italy, the national healthcare system is universal and fully covers the population. In addition, some cases may have been hospitalized only more than 18 years before and be underreported.
The observed growth of the IBDs prevalence from 2010 to 2018 in the Milan area, might pose a warning for all the other Italian areas and the Country as a whole. IBDs’ are complex [1] and costly [11,23] diseases, which affect a quite young population, with remissions and flares that may last for patients’ whole life, that is many decades. The provided Italian estimates should only be considered until a national study will provide more reliable numbers, avoiding the possible causes of overreporting (e.g. geographical heterogeneity) and underreporting.
Our figures, age, sex and disease-specific, can be useful for clinicians and policymakers, to properly plan the IBDs’ health system in the coming years.
Conclusion
This real-world study, based on administrative health data, provides recent estimates for IBDs incidence and prevalence, showing high rates and an incessant increase in the burden of patients. Our results are coherent with other studies carried out in Italy and Europe. According to our results, more than 15 000 new cases are expected in Italy every year, about 8300 ulcerative colitis and 6900 Crohn’s disease. Also, there are at least 264 000 Italian citizens with an IBDs diagnosis, and, at the current prevalence growth, the burden is expected to reach 500 000 in 2025.
Acknowledgements
The research reported in this publication was supported by Roche S.p.A. The funder had no role in the study design, data collection and analysis, decision to publish, or preparation of the article.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Sairenji T, Collins KL, Evans DV. An update on inflammatory bowel disease. Prim Care 2017; 44:673–692. [DOI] [PubMed] [Google Scholar]
- 2.Kaplan GG, Bernstein CN, Coward S, Bitton A, Murthy SK, Nguyen GC, et al. The impact of inflammatory bowel disease in Canada 2018: epidemiology. J Can Assoc Gastroenterol 2019; 2:S6–S16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.GBD 2017 Inflammatory Bowel Disease Collaborators. The global, regional, and national burden of inflammatory bowel disease in 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol 2020; 5:17–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ng SC, Shi HY, Hamidi N, Underwood FE, Tang W, Benchimol EI, et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet 2018; 390:2769–2778. [DOI] [PubMed] [Google Scholar]
- 5.Galeone C, Pelucchi C, Barbera G, Citterio C, La Vecchia C, Franchi A. Crohn’s disease in Italy: a critical review of the literature using different data sources. Dig Liver Dis 2017; 49:459–466. [DOI] [PubMed] [Google Scholar]
- 6.Macaluso FS, Mocci G, Orlando A, Scondotto S, Fantaci G, Antonelli A, et al. Prevalence and incidence of inflammatory bowel disease in two Italian islands, Sicily and Sardinia: a report based on health information systems. Dig Liver Dis 2019; 51:1270–1274. [DOI] [PubMed] [Google Scholar]
- 7.Piscaglia AC, Lopetuso LR, Laterza L, Gerardi V, Sacchini E, Leoncini E, et al. Epidemiology of inflammatory bowel disease in the Republic of San Marino: the “EPIMICI - San Marino” study. Dig Liver Dis 2019; 51:218–225. [DOI] [PubMed] [Google Scholar]
- 8.Fornari C, Madotto F, Fiorino G, Ardizzone S, Bortoli A, Caprioli F, et al. Inflammatory bowel diseases in Italy: incidence trends and patients’ characteristics. Value Health 2013; 16:7. [Google Scholar]
- 9.Di Domenicantonio R, Cappai G, Arcà M, Agabiti N, Kohn A, Vernia P, et al. Occurrence of inflammatory bowel disease in central Italy: a study based on health information systems. Dig Liver Dis 2014; 46:777–782. [DOI] [PubMed] [Google Scholar]
- 10.Valpiani D, Manzi I, Mercuriali M, Giuliani O, Ravaioli A, Colamartini A, et al. A model of an inflammatory bowel disease population-based registry: the Forlì experience (1993-2013). Dig Liver Dis 2018; 50:32–36. [DOI] [PubMed] [Google Scholar]
- 11.Ruggeri M, Armuzzi A, Leone S, Rolli FR, Cicchetti A, Previtali E. Il burden economico delle Mici in Italia. https://amiciitalia.eu/sites/default/files/Burden_economico_mici_mail.pdf. [Accessed 14 July 2020].
- 12.Francesconi P. Le malattie croniche in Toscana epidemiologia e impatto sui servizi. Documenti ARS Toscana, n. 104 ottobre 2019. https://www.ars.toscana.it/images/pubblicazioni/Collana_ARS/2019/Doc_104_MACRO_2019_finale_27_11.pdf. [Accessed 14 July 2020].
- 13.Bernstein CN, Benchimol EI, Bitton A, Murthy SK, Nguyen GC, Lee K, et al. The impact of inflammatory bowel disease in Canada 2018: extra-intestinal diseases in IBD. J Can Assoc Gastroenterol 2019; 2:S73–S80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.European Crohn´s and Colitis Organisation. European Crohn’s and Colitis Organisation (ECCO) guidelines. https://www.ecco-ibd.eu/publications/ecco-guidelines-science.html. [Accessed 14 July 2020].
- 15.Regione Lombardia. Modalità di avvio del percorso di presa in carico del paziente cronico e/o fragile in attuazione della dgr n. x/6551 del 04/05/2017. https://www.regione.lombardia.it/wps/portal/istituzionale/HP/DettaglioRedazionale/servizi-e-informazioni/Enti-e-Operatori/sistema-welfare/attuazione-della-riforma-sociosanitaria-lombarda/dgr2017-7655-avvio-presa-carico-cronici/dgr2017-7655-avvio-presa-carico-cronici [Accessed 4 February 2021].
- 16.ISTAT. Italian National Institute of Statistics. www.demo.istat.it
- 17.Eurostat. Revision of the European Standard Population Report of Eurostat’s task force. 2013 edition. Luxembourg: European Commission. [Google Scholar]
- 18.Murtas R, Russo AG. Effects of pollution, low temperature and influenza syndrome on the excess mortality risk in winter 2016-2017. BMC Public Health 2019; 19:1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Andreano A, Rebora P, Valsecchi MG, Russo AG. Adherence to guidelines and breast cancer patients survival: a population-based cohort study analyzed with a causal inference approach. Breast Cancer Res Treat 2017; 164:119–131. [DOI] [PubMed] [Google Scholar]
- 20.Tunesi S, Bosio M, Russo AG. Do autistic patients change healthcare services utilisation through the transition age? An Italian longitudinal retrospective study. BMJ Open 2019; 9:e030844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Murtas R, Decarli A, Greco MT, Andreano A, Russo AG. Latent composite indicators for evaluating adherence to guidelines in patients with a colorectal cancer diagnosis. Medicine (Baltimore) 2020; 99:e19277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Andreano A, Bosio M, Russo AG. Emergency attendance for acute hyper- and hypoglycaemia in the adult diabetic population of the metropolitan area of Milan: quantifying the phenomenon and studying its predictors. BMC Endocr Disord 2020; 20:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Capri S, Russo A. I costi dei pazienti con patologie infiammatorie dell’intestino (Malattia di Crohn e colite ulcerosa). Studio real world in Italia. Glob Regional Health Technol Assess 2018; 5:1–66. [Google Scholar]
- 24.Pasvol TJ, Horsfall L, Bloom S, Segal AW, Sabin C, Field N, Rait G. Incidence and prevalence of inflammatory bowel disease in UK primary care: a population-based cohort study. BMJ Open 2020; 10:e036584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Duricova D, Burisch J, Jess T, Gower-Rousseau C, Lakatos PL; ECCO-EpiCom. Age-related differences in presentation and course of inflammatory bowel disease: an update on the population-based literature. J Crohns Colitis 2014; 8:1351–1361. [DOI] [PubMed] [Google Scholar]
- 26.Manninen P, Karvonen AL, Huhtala H, Rasmussen M, Salo M, Mustaniemi L, et al. Mortality in ulcerative colitis and Crohn’s disease. A population-based study in Finland. J Crohns Colitis 2012; 6:524–528. [DOI] [PubMed] [Google Scholar]
- 27.Selinger CP, Andrews J, Dent OF, Norton I, Jones B, McDonald C, et al.; Sydney IBD Cohort Study Group. Cause-specific mortality and 30-year relative survival of Crohn’s disease and ulcerative colitis. Inflamm Bowel Dis 2013; 19:1880–1888. [DOI] [PubMed] [Google Scholar]
- 28.Olén O, Askling J, Sachs MC, Frumento P, Neovius M, Smedby KE, et al. Increased mortality of patients with childhood-onset inflammatory bowel diseases, compared with the general population. Gastroenterology 2019; 156:614–622. [DOI] [PubMed] [Google Scholar]
- 29.Olén O, Askling J, Sachs MC, Neovius M, Smedby KE, Ekbom A, Ludvigsson JF. Mortality in adult-onset and elderly-onset IBD: a nationwide register-based cohort study 1964-2014. Gut 2020; 69:453–461. [DOI] [PubMed] [Google Scholar]
- 30.Cottone M, Renda MC, Mattaliano A, Oliva L, Fries W, Criscuoli V, et al. Incidence of Crohn’s disease and CARD15 mutation in a small township in Sicily. Eur J Epidemiol 2006; 21:887–892. [DOI] [PubMed] [Google Scholar]
- 31.Sardu C, Cocco E, Mereu A, Massa R, Cuccu A, Marrosu MG, Contu P. Population based study of 12 autoimmune diseases in Sardinia, Italy: prevalence and comorbidity. PLoS One 2012; 7:e32487. [DOI] [PMC free article] [PubMed] [Google Scholar]