Abstract
Background & Aims
Immune checkpoint inhibitors (ICIs) improve the survival of patients with advanced tumors. However, immune-related adverse events limit the use of ICIs. Although liver toxicity has been concerned gradually, little is known about bile duct injury associated with ICIs. Hence, this review aims to describe clinicopathological features, imaging, and management of immune-mediated cholangitis (IMC) induced by ICIs.
Methods
We retrieved the literature from the PubMed database for case reports and series of IMC induced by ICIs. IMC was then classified as small-ducts type, large-ducts type and mixed type. Biochemical parameters, pathological characteristics, imaging features, treatment and response were evaluated and compared among three patterns.
Results
Fifty-three cases of IMC were enrolled. The median values of alkaline phosphatase and alanine transaminase of IMC were 1328 and 156 IU/L. The ALP level of the large-ducts type was higher than that of the small-ducts type (P = 0.021). The main pathological characteristics of small-ducts cholangitis were portal inflammation, bile duct injury and ductular reaction. The imaging features of large-duct cholangitis were bile duct dilatation, stenosis and bile duct wall thickening and irregularity. Forty-eight (90%) cases received immunosuppression therapy. Biliary enzymes reduced in 79% of cases receiving immunosuppression therapy, but only 8.5% of cases returned to normal. It took a long time for biliary enzymes to recover.
Conclusions
The clinicians should be aware of the possibility of IMC if the biliary enzymes increase significantly after the use of ICIs. The liver function can be improved partially by immunosuppressive therapy in the majority of IMC.
Keywords: cholangitis, hepatitis, immune checkpoint inhibitors, immune-related adverse events
Introduction
Immune checkpoint inhibitors (ICIs) have dramatically changed the landscape of cancer therapy and improved the survival of patients with advanced tumors. ICIs targeting cytotoxic T lymphocyte-associated antigen-4 (CTLA-4), programmed cell death-1 receptor (PD-1) and its ligand (PD-L1) promote T cell response against the tumor-specific antigens [1]. Due to the increasing use of ICIs in oncohaematology, immune-related adverse events (irAEs) associated with ICIs are rising correspondingly, which can involve any organ or tissue [2]. Some irAEs are severe and even fatal, limiting the use of ICIs. Rapid identification and reasonable management of irAEs are important to ameliorate clinical outcomes and bring new challenges for oncology and other specialists.
ICI-associated liver toxicity is referred to as immune-mediated hepatitis (IMH) [3]. The incidences of IMH are 4–7% in patients with monotherapy and 37% in patients with the combination of anti-PD-1 and anti-CTLA-4 therapy [4–6]. In comparison with IMH, cholangitis induced by ICIs is rarely reported. In 2017, two different patterns of nivolumab-related cholangitis were reported for the first time [7,8]. In the case reported by Gelsominon et al., interlobular bile ducts aggression, intraductal microabscesses and ductular proliferation were identified by liver biopsy, but there were no significant changes in intra- or extrahepatic bile duct by imaging [7,9]. The cases described by Kawakami et al. presented as dilation and hypertrophy of extrahepatic bile duct on imaging, while the pathology did not show any signs of interlobular bile duct injury [8]. Gelsminon referred to the former as ‘small-ducts cholangitis’ and the latter as ‘large-ducts cholangitis’ [9].
The terms used for cholangitis induced by ICIs are confused. Large-ducts cholangitis has often been termed as ‘sclerosing cholangitis’ and ‘secondary sclerosing cholangitis (SSC) [10–15]. Small-ducts cholangitis has been named ‘cholangitis liver disease’, ‘cholangiopathy’, ‘biliary injury’ and so on [7,16–19]. In order to correspond with IMH, ICIs-related cholangitis is referred to ‘immune-mediated cholangitis’ (IMC) in this review.
At present, there is limited knowledge about the clinical features of IMC induced by ICIs. This study reviewed the published cases of IMC, with a focus on biochemical results, pathological characteristics, imaging features, treatment strategies and outcomes, to provide new insights into the diagnosis and therapy of IMC.
Materials and methods
This review was carried out following the guideline of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).
Eligibility criteria
We aimed to search for the case reports and case series of IMC induced by ICIs. The inclusion criteria were as followed: (1) case reports and case series of IMC induced by ICIs, (2) the diagnosis of cholangitis was determined by imaging or pathology and (3) the cases were published in English.
Search strategies
We performed literature search by use of PubMed database, with the search strings as follow: (‘immune checkpoint inhibitors’[All Fields] OR ‘cytotoxic t lymphocyte-associated antigen 4’[All Fields] OR ‘programmed cell death’[All Fields] OR ‘immune-related adverse events’[All Fields]) AND (‘cholangitis’[All Fields] OR ‘cholangitides’[All Fields] OR ‘cholangiopathy’[All Fields] OR ‘biliary injury’[All Fields] OR ‘cholestatic’[All Fields]). The final search was performed in February 2021. The reference lists of relevant cases were also searched.
Study selection and data collection
All titles and abstracts were assessed for inclusion. Full texts of relevant articles were independently assessed by two reviewers. Disagreements were resolved by discussion. Data items extracted included country, patient demographics, primary cancer type, ICIs type, ICIs cycles until onset, classification of IMC, biochemical parameters, pathological and radiological findings, treatment of IMC and response to the treatment.
IMC was classified as three patterns, on the basis of the anatomy of the biliary system [20]. (1) Small-ducts type: the lesions were located at the intrahepatic small bile ducts, including septal ducts, interlobular ducts, ductules, and canal of Hering. (2) Large-ducts type: the lesions were located at the intrahepatic and extrahepatic large bile ducts, including segmental ducts, area ducts, the left and right hepatic duct, common hepatic duct and common bile duct. (3) Mixed type: both the small and larger bile ducts were involved.
The definition of the biochemical response was according to the Barcelona criteria of primary biliary cirrhosis (PBC) [21]. The completed response was defined as a normalization of alkaline phosphatase (ALP). The poor response was defined as a decrease of ALP <40%. The partial response was defined as a decrease of ALP ≥40%, but not to the normal level. For a few cases without detailed information of ALP level, it was considered as a partial response if the improvement of ALP was judged by the authors themselves.
Statistics and analysis
Continuous variables were presented as median with range and compared using Mann–Whitney U test or Kruskal–Wallis H test. Categorical variables were presented as a number with percentage and compared using Fisher’s exact test or Chi-square tests. The two-tailed P value less than 0.05 was considered statistically significant.
Results
Retrieved results
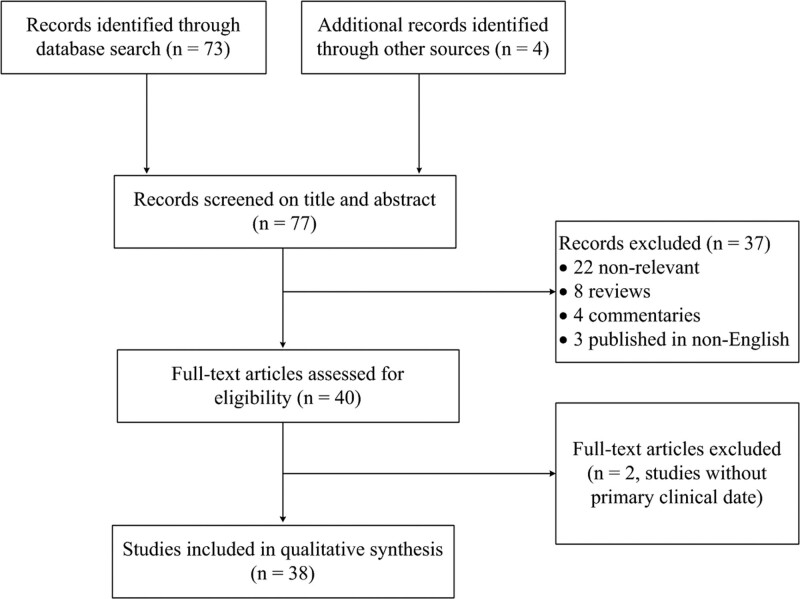
The process of literature selection is shown in Fig. 1. Seventy-three articles were identified through the search from the PubMed database. An additional four articles were identified by browsing the reference lists of the selected articles. Thirty-seven articles were excluded by screening the titles and abstracts: 22 were nonrelevant, eight were reviews, four were commentaries and three were not published in English. Forty full-text articles were assessed for eligibility further. Two articles of pathology without primary clinical data were excluded. At last, 26 cases and 12 case series with a total of 53 patients from March 2017 to February 2021 were enrolled in this study.
Fig. 1.
Flowchart for the selection of the cases of immune-mediated cholangitis induced by immune checkpoint inhibitors in this review.
General characteristics
A total of 53 cases of IMC induced by ICIs were included in this review, consisting of 12 with small-ducts type, 29 with large-ducts type and 12 with mixed type. There were 31 cases from Japan, five cases from the United Kingdom (UK), five cases from France, three cases from Switzerland, two cases from the USA and one case from Australia, Belgium, Canada, Italy, Korea, Norway and Turkey, respectively.
The characteristics of the enrolled cases are summarized in Table 1. There were 35 men and 18 women, with a median age of 68 years (range, 43–89). The most common primary diseases were lung cancer (n = 37). Forty-seven patients received anti-PD-1 therapy, three received anti-PD-L1 therapy, once received anti-CLTA-4 therapy and two received the combination of anti-PD-1/PD-L1 and anti-CLTA-4 therapy. There were no reports of large-ducts cholangitis caused by anti-CTLA-4 monotherapy so far. There were no differences in sex, age, primary disease and ICIs type among the three patterns of IMC. The median numbers of ICIs cycles until IMC onset were five (range, 1–27). The earliest and latest onset time was 8 days and 2 years after the initiation of the ICIs therapy respectively [16,22]. The ICIs cycles until onset were different among the three patterns of IMC (P = 0.025). Pairwise comparisons indicated that the ICI cycles in patients with large-ducts type were significantly longer than those in patients with small-ducts type (7 vs. 2.5; P = 0.027). The mixed type had no significant difference in ICI cycles from large-ducts types or small-ducts type (P = 1.000; P = 0.125).
Table 1.
Clinical characteristics of the patients with IMC of three types induced by ICIs
| Characteristics | All patients (n = 53) | Small-ducts type (n = 12) | Large-ducts type (n = 29) | Mixed type (n = 12) | P value |
|---|---|---|---|---|---|
| Sex, men (%) | 35 (66.0%) | 8 (66.7%) | 17 (58.6%) | 10 (83.3%) | 0.318 |
| Age, median (range, year) | 68 (43–89) | 64.5 (43–83) | 68.5 (50–89) | 67.5 (43–80) | 0.704 |
| Primary cancer type | 0.068 | ||||
| Lung caner | 37 | 5 | 23 | 9 | |
| Melanoma | 7 | 4 | 2 | 1 | |
| Gastric caner | 4 | 1 | 1 | 2 | |
| Bladder cancer | 2 | 0 | 2 | 0 | |
| Other cancers | 3 | 2 | 1 | 0 | |
| ICIs type | 0.577 | ||||
| Nivolumab | 28 | 4 | 17 | 7 | |
| Pembrolizumab | 19 | 6 | 9 | 4 | |
| Atezolizumab | 2 | 1 | 1 | 0 | |
| Avelumab | 1 | 0 | 1 | 0 | |
| Ipilimumab | 1 | 1 | 0 | 0 | |
| Nivolumab + Ipilimumab | 1 | 0 | 0 | 1 | |
| Durvalumab + tremelimumab | 1 | 0 | 1 | 0 | |
| ICIs cycles until onset, median (range) | 5 (1–27) | 2.5 (1–13) | 7 (1–25) | 5 (3–27) | 0.025†; 0.027‡ |
| Biochemical parameters | |||||
| ALP, median (range, IU/L) | 1328 (237–4635) | 678 (237–2837) | 1683 (550–4635) | 1652 (545–2427) | 0.025†; 0.021‡ |
| ALT, median (range, IU/L) | 156 (31–1536) | 217 (31–1536) | 101 (45–516) | 162 (68–331) | 0.105 |
| Pathological findings | |||||
| Small-ducts cholangitis | 24 | 12 | - | 12 | |
| Portal inflammation, n (%) | 21 (87.5%) | 10 (83.3%) | - | 11 (91.7%) | 1.000 |
| Bile duct injury, n (%) | 24 (100%) | 12 (100%) | - | 12 (100%) | - |
| Ductular reaction, n (%) | 13 (54.2%) | 5 (41.7%) | - | 8 (66.7%) | 0.401 |
| Bile duct loss, n (%) | 4 (16.7%) | 3 (25%) | - | 1 (8.3%) | 0.590 |
| Cholestasis, n (%) | 7 (29.2%) | 5 (41.7%) | - | 2 (16.7%) | 0.371 |
| Large-ducts cholangitis | 9 | - | 7 | 2 | |
| Inflammatory infiltration | 9 (100%) | - | 7 (100%) | 2 (100%) | - |
| Noncentricular diffuse fibrosis | 3 (33.3%) | - | 1 (14.3%) | 2 (100%) | 0.083 |
| Imaging of large bile ducts | 38 | 26 | 12 | ||
| Intrahepatic bile ducts | 5 (13.2%) | - | 1 (3.8%) | 4 (33.3%) | 0.027§ |
| Extrahepatic bile duct | 15 (39.5%) | - | 14 (53.8%) | 1 (8.3%) | 0.012§ |
| Intra- and extrahepatic bile duct | 18 (47.4%) | - | 11 (42.3%) | 7 (58.3%) | 0.489 |
| Treatment | |||||
| Without immunosuppression therapy | 5 | 0 | 5 | 0 | - |
| GC monotherapy | 32 | 6 | 18 | 8 | - |
| GC + MMF | 8 | 3 | 4 | 1 | - |
| GC + AZA | 2 | 0 | 1 | 1 | - |
| GC + MMF + TAC | 1 | 0 | 0 | 1 | - |
| GC + TCZ | 3 | 2 | 0 | 1 | - |
| GC + MMF + TAC + TCZ | 1 | 0 | 1 | 0 | - |
| GC + MMF + plasmapheresis | 1 | 1 | 0 | 0 | - |
| UDCA | 20 | 6 | 9 | 5 | - |
| Response to immunosuppressive therapy | |||||
| Biochemical response | 47 | 12 | 23 | 12 | |
| Complete response | 4 (8.5%) | 1 (8.3%) | 2 (8.7%) | 1 (8.3%) | 1.000 |
| Partial response | 33 (70.2%) | 8 (66.7%) | 18 (78.3%) | 7 (58.3%) | 0.505 |
| Poor response | 10 (21.3%) | 3 (25%) | 3 (13.0%) | 4 (33.3%) | 0.277 |
| Imaging response | 6 | - | 6 | NA | |
| Improve / worsen | 4/2 | - | 4/2 | NA | - |
| Histological response | 4 | 2 | 1 | 1 | |
| Reduced inflammation | 4 | 2 | 1 | 1 | - |
| Progressive bile duct injury | 2 | 2 | 0 | 0 | - |
ALP, alkaline phosphatase; ALT, alanine aminotransferase; AZA, azathioprine; GC, glucocorticoid; ICIs, immune checkpoint inhibitors; IMC, immune-mediated cholangitis; MMF, mycophenolate mofetil; NA, unavailable; UDCA, ursodeoxycholic acid.
†P < 0.05 among the three types
‡P < 0.05 small-ducts type vs. large-ducts type
§P < 0.05 large-ducts type vs. mixed type.
Biochemical results
The values of ALP and alanine aminotransferase (ALT) were obtained in 37 cases at the same time. The median values of ALP and ALT were 1328 IU/L (range, 237–4635) and 156 IU/L (range, 31–1536) respectively. ALP level was different among the three patterns of IMC (P = 0.025). Pairwise comparisons indicated that ALP in the patients with large-ducts type was higher than that with small-ducts type (1683 vs. 678 IU/L; P = 0.021). The mixed type had no significant difference in ALP level from large-ducts types or small-ducts type (P = 1.000; P = 0.189). There was no significant difference in ALT level among the three types.
Pathological findings
Liver biopsies were performed in 30 cases, 24 of which had evidence of cholangiopathy. The pathological findings included portal inflammation (n = 21, 87.5%), bile duct injury (n = 24, 100%), ductular reaction (n = 13, 54.2%), bile duct loss (n = 4, 16.7%), cholestasis (n = 7, 29.2%) and lobular injury (n = 11, 45.8%). The biopsies of extrahepatic bile ducts were performed in nine cases. The pathology was characterized by inflammatory infiltration in the lining epithelium (n = 9, 100%) and noncentricular diffuse fibrosis (n = 3, 33.3%).
Imaging findings
Twenty-nine cases of IMC with large-ducts type and 12 with mix type were diagnosed by imaging. The main findings were bile duct dilatation, stenosis and bile duct wall thickening and irregularity, which could be segmental or diffuse. Except for three cases without detailed information, the remaining 38 cases had abnormalities at different anatomical levels of bile ducts. Five cases were at the intrahepatic bile duct, 15 at the extrahepatic bile duct, and 18 at both intra- and extrahepatic bile duct. The patients with large-ducts type had a higher proportion of abnormality at extrahepatic bile duct (53.8 vs. 8.3%, P = 0.012) and lower at intrahepatic bile duct (3.8 vs. 33.3%, P = .027), concerning those with mixed cholangitis.
Positron-emission tomography-computed tomography (PET-CT) was performed in two cases, one of which had increased fluorodeoxyglucose (FDG) uptake in the gallbladder and bile ducts [14]. The other patient had a negative result, probably because PET-CT was carried out 6 weeks before the abnormality of liver function test (LFT) [23]. Peroral cholangioscopy was performed in five cases. Band-like narrowing of the biliary tract wall was revealed in three cases, two of which were accompanied by diverticulum-like outpouching [13]. Ulcerative lesions with the ‘burned-out’ epithelium were detected in one case [24]. Multiple scarred lesions with hemorrhage and narrowing of second-order biliary branches were found in another case [25].
Treatment strategies
The treatment strategies of IMC cases are shown in Table 2. ICIs were discontinued in all of the 53 cases. Five cases did not receive immunosuppression therapy. Two out of the five patients received ursodeoxycholic acid (UDCA) and two underwent biliary drainage. Forty-eight cases were treated with immunosuppression therapy, 32 with glucocorticoid (GC) monotherapy, 11 with GC and immunosuppressive agents, three with GC and immunomodulators, two with the combination of GC, immunosuppressive agents and immunomodulators. UDCA was used in 18 cases concurrently. Most patients were treated with (methyl)prednisone of 0.5–2 mg/kg/day, seven with high dose methylprednisolone of 500–1000 mg/day. The immunosuppressive agents used for the treatment of IMC were mycophenolate mofetil, azathioprine and tacrolimus. Immunomodulators included interleukin-6 receptor neutralizing antibody (tocilizumab) and plasmapheresis.
Table 2.
Treatment and response of the cases of IMC induced by ICIs
| Case | References | IMC patterns | Location of abnormal imaging | Treatment | Biochemcial response | Time for recovery of LTFs | Imgaging response | Histology response |
|---|---|---|---|---|---|---|---|---|
| 1 | Gelsomino et al. [7] | Small-ducts type | - | PSL (1 mg/kg) + UDCA (15 mg/kg) | Partial | >3 months | - | - |
| 2 | Kawakami et al. [8] | Large-ducts type | EBD | PSL (0.5 mg/kg) | Partial | >3 months | - | - |
| 3 | Kawakami et al. [8] | Large-ducts type | EBD | PSL (0.5 mg/kg) + biliary drainage | Partial | >6 months | - | - |
| 4 | Kawakami et al. [8] | Large-ducts type | IEBD | Biliary drainage | - | NA | - | - |
| 5 | Yildirim et al. [62] | Small-duct type | - | PSL (2 mg/kg) | Partial | NA | - | - |
| 6 | Doherty et al. [16] | Small-duct type | - | PSL (1 mg/kg) + MMF (2 g) + UDCA (NA) | Poor | - | - | - |
| 7 | Doherty et al. [16] | Small-duct type | - | PSL (1 mg/kg) + UDCA (NA) | Partial | >6 months | - | - |
| 8 | Doherty et al. [16] | Small-duct type | - | mPSL (2 mg/kg) + MMF (1 g) + UDCA (NA) | Partial | >3 months | - | Reduced inflammation and progressive bile duct injury |
| 9 | Kashima et al. [26] | Large-ducts type | EBD | PSL (2 mg/kg) + biliary drainage | Partial | >3 months | Improve | - |
| 10 | Cho et al. [63] | Large-ducts type | EBD | mPSL (1 mg/kg) | Partial | NA | - | - |
| 11 | Kuraoka et al. [24] | Large-ducts type | EBD | PSL (60 mg) / mPSL (0.5 g) | Poor | - | - | - |
| 12 | Hamoir et al. [17] | Mixed type | IBD | mPSL (0.5 mg/kg) + UDCA (10 mg/kg) | Complete | 3 months | - | - |
| 13 | Noda-Narita et al. [12] | Large-ducts type | IEBD | UDCA (300 mg) | - | NA | Improve | - |
| 14 | Le Tallec et al. [64] | Large-ducts type | IEBD | GC (NA) | NA | NA | - | - |
| 15 | Oda et al. [57] | Small-ducts type | - | PSL (1 mg/kg) / mPSL (1 g) + MMF (2 g) | Poor | - | - | - |
| 16 | Ogawa et al.[10] | Large-ducts type | IEBD | - | - | <3 months | Improve | - |
| 17 | Kono et al. [11] | Large-ducts type | EBD | Biliary drainage | - | NA | - | - |
| 18 | Sawada et al. [30] | Mixed type | EBD | PSL (0.5 mg/kg) + UDCA (NA) | Partial | >3 months | - | - |
| 19 | Fouchard et al. [61] | Large-ducts type | NA | PSL (0.5 mg/kg) + UDCA (NA) + cholecystectomy | Partial | >6 months | - | - |
| 20 | Fouchard et al. [61] | Large-ducts type | NA | PSL (120 mg) + UDCA (NA) + cholecystectomy | Partial | >6 months | - | - |
| 21 | Fouchard et al. [61] | Large-ducts type | NA | PSL (1 mg/kg) | Complete | >6 months | - | - |
| 22 | Koya et al. [25] | Mixed type | IEBD | mPSL (0.5 g) / PSL (1 mg/kg) + UDCA (900 mg) + biliary drainage | Poor | - | - | - |
| 23 | Cǎlugǎreanu et al. [23] | Mixed type | IEBD | PSL (1 mg/kg) | Partial | >6 months | - | - |
| 24 | Anderson et al. [65] | Mixed type | IEBD | PSL (50 mg) + MMF (NA) + TAC (NA) | Poor | - | - | - |
| 25 | Cheung et al. [28] | Large-ducts type | IBD | PSL (40 mg/kg) + UDCA (75 mg) | Partial | >3 months | - | - |
| 26 | Izumi et al. [66] | Large-ducts type | EBD | mPSL (2 mg/kg) + MMF (2 g) | Partial | NA | - | - |
| 27 | Izumi et al. [66] | Large-ducts type | EBD | mPSL (2 mg/kg) + MMF (2 g) | Partial | NA | - | - |
| 28 | Izumi et al. [66] | Large-ducts type | EBD | mPSL (2 mg/kg) | Partial | NA | - | - |
| 29 | Onoyama et al. [13] | Large-ducts type | EBD | PSL (1 mg/kg) + UDCA (600 mg) | Partial | NA | - | - |
| 30 | Onoyama et al. [13] | Large-ducts type | EBD | UDCA (600 mg) | - | NA | - | - |
| 31 | Onoyama et al. [13] | Large-ducts type | EBD | PSL (1 mg/kg) + UDCA (600 mg) | Partial | NA | - | - |
| 32 | Reddy et al. [67] | Large-ducts type | IEBD | PSL (0.85 mg/kg) + MMF (2 g) + TAC (2 mg) + TCZ (4 mg/kg) + UDCA (1500 mg) | Poor | - | Worsen | - |
| 33 | Williams et al. [22] | Large-ducts type | IEBD | GC (NA) | Complete | >3 months | - | - |
| 34 | Kurokawa et al. [19] | Small-ducts type | - | PSL (1 mg/kg) + UDCA (900 mg) | Partial | >3 months | - | - |
| 35 | Imoto et al. [68] | Mixed type | IEBD | mPSL (1 g) / PSL (0.6 mg/kg) + UDCA (600 mg) | Partial | NA | - | - |
| 36 | Onoyama et al. [69] | Large-ducts type | IEBD | mPSL (2 mg/kg) + MMF (2 g) | Partial | NA | - | - |
| 37 | Onoyama et al. [69] | Large-ducts type | EBD | mPSL (2 mg/kg) + MMF (2 g) + biliary drainage | Partial | NA | - | - |
| 38 | Onoyama et al. [69] | Large-ducts type | EBD | mPSL (1.6 mg/kg) | Partial | NA | - | - |
| 39 | Zen et al. [32] | Mixed type | IEBD | PSL (50 mg) | Partial | NA | - | - |
| 40 | Zen et al. [32] | Mixed type | IEBD | PSL (40 mg) | Poor | NA | - | - |
| 41 | Zhang et al. [70] | Small-ducts type | - | GC (NA) | Partial | NA | - | - |
| 42 | Thorsteinsdottir et al. [18] | Small-ducts type | - | PSL (120 mg) + MMF (2 g) + plasmapheresis | Poor | NA | - | - |
| 43 | Mizuno et al. [27] | Large-ducts type | IEBD | PSL (40 mg) | Poor | NA | Worsen | - |
| 44 | Matsumoto et al. [14] | Large-ducts type | IEBD | PSL (80 mg)/mPSL (1 g) + AZA (50 mg) | Partial | NA | Improve | - |
| 45 | Ooi et al. [58] | Mixed type | IBD | PSL (40 mg)/mPSL (1 g) + AZA (50 mg) | Partial | >6 months | - | Reduced inflammation and progressive bile duct injury |
| 46 | McClure et al. [34] | Mixed type | IBD | PSL (50 mg) | Partial | >6 months | - | - |
| 47 | Yoshikawa et al. [71] | Mixed type | IEBD | PSL (1–1.5 mg/kg) + UDCA (600 mg) + MMF (2 g) | Poor | NA | - | - |
| 48 | Fujii et al. [72] | Large-ducts type | IEBD | PSL (30 mg) | Partial | >3 months | Improve | - |
| 49 | Sato et al. [15] | Large-ducts type | IEBD | mPSL (30 mg) + UDCA (300 mg) | Partial | >6 months | Improve | Reduced inflammation |
| 50 | Moi et al. [35] | Small-ducts type | - | mPSL (125 mg)/mPSL (0.5 g) + TCZ (500 mg) | Complete | <3 months | - | Reduced inflammation |
| 51 | Moi et al. [35] | Mixed type | IBD | mPSL (62.5–125 mg) + TCZ (500 mg) | Partial | NA | - | - |
| 52 | Moi et al. [35] | Small-ducts type | - | mPSL (125 mg) + TCZ (500 mg) | Partial | NA | - | - |
| 53 | Nabeshima et al. [36] | Small-ducts type | - | PSL (0.5 mg/kg) + UDCA (NA) | Partial | >6 months | - | - |
AZA, azathioprine; EBD, extrahepatic bile duct; IBD, Intrahepatic bile duct; ICIs, immune checkpoint inhibitors; IEBD, intra- and extrahepatic bile duct; IMC, immune-mediated cholangitis; MMF, mycophenolate mofetil; mPSL, methylprednisone; NA, unavailable; PSL, prednisone; TAC, tacrolimus; TCZ, tocilizumab; UDCA, ursodeoxycholic acid.
Treatment outcomes
Of the five cases without immunosuppressive therapy, liver function tests (LTFs) returned to normal in one patient and got improved in three patients. The outcome was unavailable in the remaining one patient. For the cases with immunosuppressive therapy, the responses were evaluated from biochemical, imaging and histological aspects (Table 2).
Biochemical response to immunosuppressive therapy
Apart from one case unable to obtain the treatment outcome, 8.5% (4/47) of the cases with immunosuppressive therapy had complete biochemical responses, 70.2% (33/47) had partial biochemical responses and 21.3% (10/47) had poor biochemical responses. There was no difference in the biochemical response among the three types of IMC (P = 0.656). The follow-up time of LTFs could be estimated in 21 cases. The abnormality of biliary enzymes persisted for more than 3 months in nine cases and more than 6 months in another ten cases.
Imaging response to immunosuppressive therapy
The imaging was reexamined in six cases with large-duct cholangitis, four of which ameliorated and two progressed. The reexamination time of the imaging ranged from 1.5 to 3 months.
Histological response to immunosuppressive therapy
Liver biopsies were repeated in four cases. The amounts of inflammatory cells in portal tracts decreased in all four patients. While the bile duct injury in two cases was ongoing after 2–4 weeks of GC therapy.
Discussion
Epidemiology
IMC has been recently perceived as an uncommon form of irAEs. To date, the limited data indicate the incidence of IMC with large-ducts type was between 0.05 and 0.7% [26–28]. In a retrospective study during 2011–2018 in the UK, 0.2% (1/453) of the patients receiving immunotherapy for cancer was found with stricture and ectasia of the bile duct [28]. In a real word study during 2014–2019 in Japan, nonobstructive biliary duct dilation was reported in 0.7% (4/546) of the patients treated with ICIs [27]. According to the postmarketing surveillance of nivolumab during 2014–2017 in Japan, ten cases of sclerosing cholangitis were reported, with an incidence of 0.05% [26]. The incidence of IMC with small-ducts type is still unknown and likely to be underestimated because its diagnosis depends on liver biopsy. In the retrospective pathological study of 60 patients treated with ICIs who underwent liver biopsy attributable to abnormal LTFs from 2014 to 2018 in Boston, 16 (27%) patients had a predominantly cholangitic pattern. Twelve (20%) patients confirmed with the presentation of IMC with small-ducts type, 4 (6.7%) patients coincided with that of mixed type entailing large and small bile ducts simultaneously [29]. In our review, a total of 54 cases of IMC were identified from March 2017 to February 2021, comprised of 12 cases with small-ducts type, 29 with large-ducts type and 12 with mixed type. More than half of the cases came from Japan, which perhaps related to the fact that the Japanese scholars paid more attention to IMC. As early as 2017, the Ministry of health, welfare and labor of Japan had already called for more researches on nivolumab-related cholangitis [30]. Hepatologists and oncologists in all countries should pay more attention to IMC induced by ICIs.
Biochemical presentations
The common biochemical feature of IMC was a significant elevation of biliary enzymes relative to hepatic enzymes. Our study showed that the later onset time and higher ALP level were found in the patients with large-ducts cholangitis, as compared to those with small-ducts cholangitis. This was consistent with Hafsteinn O’s research on SSC in patients with drug-induced liver injury (DILI) [31]. In their study, ten out of 102 unselected DILI patients had ductal stricture, irregularity and dilatation on MRCP, conforming to the features of SSC. The SSC group had higher ALP than the patients with the cholestatic pattern.
Histopathologic characteristics
Pathologists and hepatologists are needed to be familiar with the histopathologic characteristics of IMC, which helps to make a timely pathological diagnosis and appropriate treatment decision. Generally, pathological findings of IMC were nonspecific and similar to the biliary injury in DILI. The pathological findings of small-ducts cholangitis were: (1) portal inflammation. Mixed inflammatory cells were mainly composed of lymphocytes with casual neutrophils, eosinophils, macrophages. A predominance of CD8+ T cell infiltration is a characteristic of IMC, which is verified by Zen’s research and coincides with IMH [32,33]. Moreover, Zen et al. compared the ratio of CD8+/CD4+ T cells among IMH, IMC, autoimmune hepatitis (AIH) and heterogeneous DILI. The results showed that the ration of CD8+/CD4+ T cells in the IMH/IMC group was 12.2 ± 5.1, which was much higher than that of the AIH group (2.7 ± 1.1) and DILI group (5.0 ± 1.1) [32]. (2) Small bile duct injuries, such as irregularity of bile duct epithelium, cytoplasmic vacuolization, degeneration of ducts, intraepithelial lymphocytes infiltration, periductal lymphocytes infiltration and periductal fibrosis. Florid duct lesions (n = 4) [23,32,34,35] and concentric periductal fibrosis (n = 2) [16,36] were found in some cases, which are similar to the characteristics of PBC and PSC respectively. (3) Ductular reaction. Proliferative ductules were often located in the periportal areas, which was a repair response to the bile ducts injury. (4) Bile duct loss, a less common pathological finding in DILI. The Drug-Induced Liver Injury Network reported that 7% of the patients with DILI had different extents of bile duct loss [37]. In our review, bile duct loss was found in four cases, one of which had only one small bile duct left and was diagnosed as vanishing bile duct syndrome. To date, only six cases of VBDS related to ICIs were recorded in the US FDA Adverse Event Reporting System [38]. There are two different outcomes of bile duct loss, decided by the balance between biliary apoptosis and regeneration [39]. The one is progressive, irreversible loss leads to biliary cirrhosis and liver failure. The other is the bile ducts regenerate and recover over months to years [39]. The prognosis of drug-induced bile duct loss is slightly better than that of other causes [39,40]. In our review, two of the four patients with bile duct loss had poor outcomes, two improved gradually. (5) Cholestasis and lobular injury. Approximately half of the patients were complicated with various levels of lobular inflammation, necrosis and cholestasis.
The histopathological features of large-ducts cholangitis were inflammatory infiltration in the lining epithelium and noncentricular diffuse fibrosis of the extrahepatic bile duct. Zen et al. reported an interesting IMC case with mixed pattern induced by pembrolizumab [32]. Its intrahepatic duct injury was similar to PBC, with dense infiltration of inflammatory cells around the septal bile duct and a borderline granulomatous change. The pathology of the extrahepatic duct resembled those of IgG4-related cholangitis, with an extensive inflammatory, infiltrate in the fibrotic duct wall. However, IgG4-positive plasma cells are <10/high power field.
Imaging findings
Imaging examination is crucial for the diagnosis and differential diagnosis of IMC. Physicians should know the optimal imaging modality for the detection of IMC and be acquainted with the imaging features of IMC. The imaging findings of intrahepatic and extrahepatic large-ducts cholangitis were comprised of three aspects. (1) Nonobstructive dilatation, or stenosis of bile duct lumen, which could be segmental or diffuse. (2) Enhancement, hypertrophy, and irregularity of bile duct walls. (3) Changes of the adjacent structure, such as gallbladder edema, gallbladder wall thickening and Gleason’s sheath edema. The typical imaging of IMC can be obtained in Fig. 1 in Ogawa et al’s work [10]. Multiple imaging modalities had been used for the diagnosis and evaluation of the large-ducts type of IMC [41,42]. Ultrasound is dependent on the operator and less sensitive for the lesions of the distal common bile duct. The normal presence of bile ducts on ultrasound does not completely exclude biliary obstruction [43]. Magnetic resonance cholangiopancreatography (MRCP) and endoscopic retrograde cholangiography (ERCP) provide an overview of the biliary tree and assess the morphological changes of the ductal system sensitively, such as luminal dilatation, stricture and irregularity. Both contrast-enhanced MRI and computed tomography (CT) scans are useful in the evaluation of the bile duct walls, peribiliary or periportal masses and hepatic and pancreatic parenchymal diseases, while MRI had higher soft-tissue contrast resolution than CT. Contrast-enhanced MRI with MRCP is verified to offer the most comprehensive evaluation of biliary stricture [44]. Anderson et al. also suggested contrast-enhanced MRI with MRCP would be the optimal imaging modality for the detection of IMC [41]. Accumulation of FDG may be noted on PET-CT, even before the symptom appears [42]. Cholangioscopy can observe the lesions of the bile duct and take a biopsy under direct version. Besides, imaging plays an important role in excluding other biliary diseases, such as stones and tumors.
Differential diagnosis
IMC needs to be differentiated carefully from other causes of intrahepatic cholestasis and extrahepatic biliary obstruction, for instance, autoimmune cholangitis (PBC, PSC and IgG4-related cholangitis), malignant disorders, infections and other drug-induced biliary lesions [45,46]. In general, autoimmune cholangitis can be excluded on the basis of past history, past biochemical and imaging tests and negative immunological markers, including antinuclear antibodies, antimitochondrial antibody, antineutrophil cytoplasmic antibodies and IgG4 [45,46]. In clinical practice, it is more difficult to differentiate IMC from malignant diseases and chemotherapy and targeted therapy-induced biliary lesions. In a recent study on the hepatobiliary irAEs, ten out of 16 patients with a cholangitic pattern had competing causes for the biochemical abnormality, including primary disease progression in the liver, concomitant chemotherapy, other drugs and sepsis [29].
It should be noted that periductal-infiltrating cholangiocarcinoma and metastasis grow along the bile ducts, whose imaging manifestation mimics that of IMC [47]. The MRI findings of the periductal-infiltrating tumor were irregular narrowing of the involved bile duct, with and without a visible thickened wall, and dilation of the proximal bile duct. Sometimes, even CT scans are difficult to depict the periductal tumor mass [48]. We need to pay more attention to gastrointestinal cancers, which metastasize to the biliary tract most frequently [48,49]. Especially when the response to steroids of IMC is poor, we must re-review the imaging and carry out biopsies to exclude infiltrating caners as far as possible.
Besides, although very rare, SSC induced by taxane drugs (paclitaxel, docetaxel and nab-paclitaxel) and bevacizumab have been reported, with similar biochemical and imaging findings with that of large-ducts type of IMC [50–54]. Taxol is mainly excreted through bile ducts, and it was hypothesized that the increase of taxol concentration resulted in biliary injury [52]. Bevacizumab is supposed to induce a hypercoagulative condition and promote thrombosis of microvessels supplying biliary ducts, leading to bile duct ischemia [50]. In our review, ICIs were not concurrently combined with chemotherapy in any patients. However, 11 patients received paclitaxel (n = 9) and bevacizumab (n = 3) before or after the use of ICIs. It is not clear whether paclitaxel and bevacizumab had participated in the injuries of bile ducts.
Furthermore, we need to keep in mind that sepsis, a common complication of immunosuppression therapy, is another cause of intrahepatic cholestasis [45]. If ALP or bilirubin rebounds in the process of steroids therapy for IMC, we need to exclude sepsis carefully, rather than increasing the dosage of steroids or initiate additional immunosuppressants immediately. In this review, one patient died due to sepsis [27].
Management
According to the guidelines of management of irAEs published by multiple scientific societies, GC is recommended for the treatment of high-grade irAEs [2,55]. Most cases of IMH are sensitive to GCs and resolve within 6–12 weeks [3]. However, GC seems to be less effective for the treatment of IMC, in contrast to that of IMH. In this review, the treatment response of IMC has two characteristics: (1) biliary enzymes can decrease to varying degrees in the majority of patients by GC therapy, but are hard to drop to normal; (2) biliary enzymes need an extended time to recover. In this study, the biliary enzymes were not normalized even after 18 months of followed-up in a patient [34]. This situation was consistent with bile duct injury caused by other drugs. In Wang’s research on DILI, the recuperation time of LTFs in groups with bile duct damage was 3–4 months, regardless of the severity of hepatocyte injury [56]. Gudnason’s research indicated that patients with SSC induced by the drug had a longer time to resolution of the raise of LFTs [31]. The abnormal LFTs of SCC resolved within 3–6 months in five patients and more than 6 months in three patients. The longest time to resolution was 820 days [31]. Unfortunately, patients with IMC usually have limited survival time because of advanced cancer. Persistent abnormal LTFs probably lead to the loss of the opportunity for further antitumor therapy, which promotes the progression of cancer. Five patients died from progressive primary diseases in this study, rather than irAEs [7,16,36,57].
The results of the second liver biopsy might give us some enlightenment about the therapeutic strategy of IMC. The amounts of inflammatory cells in portal tracts reduced in all four cases that underwent repeated liver biopsy. It suggested that GC was beneficial for reducing inflammatory infiltration, thereby preventing further immune injury mediated by inflammatory cells. Nevertheless, the bile duct injury was still in progress in two cases after 2–4 weeks of GC therapy. We hypothesized that the bile duct lesions of IMC need to be repaired by regeneration for a long time, on the basis of the previous experience of bile duct injury in patients with DILI mentioned above [31,56]. On the basis of real-world experience of IMH from the UK, prednisolone higher than 60 mg/day has not demonstrated any additional benefit regarding time to hepatitis resolution [28]. Therefore, if no inflammation remains in a repeated biopsy, tapering of GC is recommended [58].
UDCA may be a potential choice for the treatment of IMC. UCDA is increasingly used for the treatment of cholestatic liver diseases, for its cytoprotective, antiapoptotic and immunomodulatory effects. It can reduce bile toxicity by removing hydrophobic biliary acids and stimulate biliary secretion of bile acids and other organic anions [19,59]. It also has immunomodulatory properties by inhibiting the release of cytokines and suppressing the overexpression of MHC antigens [19,60]. Twenty patients receiving the treatment of UDCA in this review. After the withdrawal of GCs in some patients, UDCA was continued to use for a long term, the decline of ALP was still going on [15,61]. Unlike GC, UDCA is safe, well-tolerated and appropriate for long-term application. Hence, GC combined with UDCA is possibly a reasonable therapeutic strategy for IMC. The application of GC in the early stage is to control the inflammation induced by ICIs. UDCA is used for the long term to foster the recuperation of bile ducts. More clinical trials are needed to verify this strategy.
Limitations
The limitations of this study were as follows: (1) this study was on the basis of case reports and case series, which were retrospective observational studies with relatively low quality of evidence. Basic researches and prospective controlled clinical studies are required to delineate the molecular mechanisms of IMC and evaluate the efficacy of GC and UDCA for the treatment of IMC. (2) Some cases did not provide complete medical records, such as the values of LFTs, imaging information, dosage and course of GCs, the degree of improvement of LTFs and the time to resolution of abnormal LTFs.
In conclusion, ICIs-associated IMC can involve the entire biliary system. The patients with the large-ducts type of IMC have a later onset time and higher ALP level than the patients with the small-ducts type of IMC. Most IMC cases respond partially to immunosuppression. It takes a long time for IMC to resolution. Awareness of the clinical features and management of IMC is crucial for oncologists and hepatologists, as the use of ICIs is rapidly increasing.
Acknowledgements
This work is supported by the Zhejiang Provincial Natural Science Foundation of China under Grant No.LY21H030011.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Borui Pi and Jin Wang have contributed equally to the writing of this article.
References
- 1.Okoye IS, Houghton M, Tyrrell L, Barakat K, Elahi S. Coinhibitory receptor expression and immune checkpoint blockade: maintaining a balance in CD8+ T cell responses to chronic viral infections and cancer. Front Immunol 2017; 8:1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Haanen JBAG, Carbonnel F, Robert C, Kerr KM, Peters S, Larkin J, Jordan K; ESMO Guidelines Committee. Management of toxicities from immunotherapy: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2017; 28 (Suppl_4):iv119–iv142. [DOI] [PubMed] [Google Scholar]
- 3.Suzman DL, Pelosof L, Rosenberg A, Avigan MI. Hepatotoxicity of immune checkpoint inhibitors: an evolving picture of risk associated with a vital class of immunotherapy agents. Liver Int 2018; 38:976–987. [DOI] [PubMed] [Google Scholar]
- 4.Mok TSK, Wu YL, Kudaba I, Kowalski DM, Cho BC, Turna HZ, et al.; KEYNOTE-042 Investigators. Pembrolizumab versus chemotherapy for previously untreated, PD-L1-expressing, locally advanced or metastatic non-small-cell lung cancer (KEYNOTE-042): a randomised, open-label, controlled, phase 3 trial. Lancet 2019; 393:1819–1830. [DOI] [PubMed] [Google Scholar]
- 5.Tawbi HA, Forsyth PA, Algazi A, Hamid O, Hodi FS, Moschos SJ, et al. Combined nivolumab and ipilimumab in melanoma metastatic to the brain. n Engl j Med 2018; 379:722–730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wolchok JD, Chiarion-Sileni V, Gonzalez R, Rutkowski P, Grob JJ, Cowey CL, et al. Overall survival with combined nivolumab and ipilimumab in advanced melanoma. n Engl j Med 2017; 377:1345–1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gelsomino F, Vitale G, D’Errico A, Bertuzzi C, Andreone P, Ardizzoni A. Nivolumab-induced cholangitic liver disease: a novel form of serious liver injury. Ann Oncol 2017; 28:671–672. [DOI] [PubMed] [Google Scholar]
- 8.Kawakami H, Tanizaki J, Tanaka K, Haratani K, Hayashi H, Takeda M, et al. Imaging and clinicopathological features of nivolumab-related cholangitis in patients with non-small cell lung cancer. Invest New Drugs 2017; 35:529–536. [DOI] [PubMed] [Google Scholar]
- 9.Gelsomino F, Vitale G, Ardizzoni A. A case of nivolumab-related cholangitis and literature review: how to look for the right tools for a correct diagnosis of this rare immune-related adverse event. Invest New Drugs 2018; 36:144–146. [DOI] [PubMed] [Google Scholar]
- 10.Ogawa K, Kamimura K, Terai S. Antiprogrammed cell death-1 immunotherapy-related secondary sclerosing cholangitis. Hepatology 2019; 69:914–916. [DOI] [PubMed] [Google Scholar]
- 11.Kono M, Sakurai T, Okamoto K, Masaki S, Nagai T, Komeda Y, et al. Efficacy and safety of chemotherapy following anti-PD-1 antibody therapy for gastric cancer: a case of sclerosing cholangitis. Intern Med 2019; 58:1263–1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Noda-Narita S, Mizuno S, Noguchi S, Watanabe K, Nakai Y, Koike K, et al. Development of mild drug-induced sclerosing cholangitis after discontinuation of nivolumab. Eur j Cancer 2019; 107:93–96. [DOI] [PubMed] [Google Scholar]
- 13.Onoyama T, Takeda Y, Kato M, Edano M, Tarumoto R, Matsumoto K, Isomoto H. Peroral cholangioscopy of programmed cell death-1 inhibitor-related sclerosing cholangitis: three case reports. Endoscopy 2019; 51:E402–E403. [DOI] [PubMed] [Google Scholar]
- 14.Matsumoto S, Watanabe K, Kobayashi N, Irie K, Yamanaka S, Kaneko T. Pembrolizumab-induced secondary sclerosing cholangitis in a non-small cell lung cancer patient. Respirol Case Rep 2020; 8:e00560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sato K, Hayashi M, Abe K, Fujita M, Takahashi A, Ohira H. Pembrolizumab-induced sclerosing cholangitis in a lung adenocarcinoma patient with a remarkable response to chemotherapy: a case report. Clin j Gastroenterol 2020; 13:1310–1314. [DOI] [PubMed] [Google Scholar]
- 16.Doherty GJ, Duckworth AM, Davies SE, Mells GF, Brais R, Harden SV, et al. Severe steroid-resistant anti-PD1 T-cell checkpoint inhibitor-induced hepatotoxicity driven by biliary injury. esmo Open 2017; 2:e000268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hamoir C, de Vos M, Clinckart F, Nicaise G, Komuta M, Lanthier N. Hepatobiliary and pancreatic: nivolumab-related cholangiopathy. j Gastroenterol Hepatol 2018; 33:1695. [DOI] [PubMed] [Google Scholar]
- 18.Thorsteinsdottir T, Løitegård T, Reims HM, Porojnicu AC. Fatal cholestatic liver injury during treatment with pd1 immune checkpoint inhibitor for malignant melanoma: a case report. Case Rep Oncol 2020; 13:659–663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kurokawa K, Hara M, Iwakami SI, Genda T, Iwakami N, Miyashita Y, et al. Cholestatic liver injury induced by pembrolizumab in a patient with lung adenocarcinoma. Intern Med 2019; 58:3283–3287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reau NS, Jensen DM. Vanishing bile duct syndrome. Clin Liver Dis 2008; 12:203–17, x. [DOI] [PubMed] [Google Scholar]
- 21.Parés A, Caballería L, Rodés J. Excellent long-term survival in patients with primary biliary cirrhosis and biochemical response to ursodeoxycholic Acid. Gastroenterology 2006; 130:715–720. [DOI] [PubMed] [Google Scholar]
- 22.Williams H, Aitchison R. Pembrolizumab-induced autoimmune haemolytic anaemia and cholangitis. bmj Case Rep 2019; 12:e232505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cǎlugǎreanu A, Rompteaux P, Bohelay G, Goldfarb L, Barrau V, Cucherousset N, et al. Late onset of nivolumab-induced severe gastroduodenitis and cholangitis in a patient with stage IV melanoma. Immunotherapy 2019; 11:1005–1013. [DOI] [PubMed] [Google Scholar]
- 24.Kuraoka N, Hara K, Terai S, Yatabe Y, Horio Y. Peroral cholangioscopy of nivolumab-related (induced) ulcerative cholangitis in a patient with non-small cell lung cancer. Endoscopy 2018; 50:E259–E261. [DOI] [PubMed] [Google Scholar]
- 25.Koya Y, Shibata M, Shinohara N, Nebuya S, Oe S, Honma Y, et al. Secondary sclerosing cholangitis with hemobilia induced by pembrolizumab: Case report and review of published work. Hepatol Res 2019; 49:950–956. [DOI] [PubMed] [Google Scholar]
- 26.Kashima J, Okuma Y, Shimizuguchi R, Chiba K. Bile duct obstruction in a patient treated with nivolumab as second-line chemotherapy for advanced non-small-cell lung cancer: a case report. Cancer Immunol Immunother 2018; 67:61–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mizuno K, Ito T, Ishigami M, Ishizu Y, Kuzuya T, Honda T, et al. Real world data of liver injury induced by immune checkpoint inhibitors in Japanese patients with advanced malignancies. j Gastroenterol 2020; 55:653–661. [DOI] [PubMed] [Google Scholar]
- 28.Cheung V, Gupta T, Payne M, Middleton MR, Collier JD, Simmons A, et al. Immunotherapy-related hepatitis: real-world experience from a tertiary centre. Frontline Gastroenterol 2019; 10:364–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cohen JV, Dougan M, Zubiri L, Reynolds KL, Sullivan RJ, Misdraji J. Liver biopsy findings in patients on immune checkpoint inhibitors. Mod Pathol 2021; 34:426–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sawada K, Shonaka T, Nishikawa Y, Hasegawa K, Hayashi H, Hasebe T, et al. Successful treatment of nivolumab-related cholangitis with prednisolone: a case report and review of the literature. Intern Med 2019; 58:1747–1752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gudnason HO, Björnsson HK, Gardarsdottir M, Thorisson HM, Olafsson S, Bergmann OM, Björnsson ES. Secondary sclerosing cholangitis in patients with drug-induced liver injury. Dig Liver Dis 2015; 47:502–507. [DOI] [PubMed] [Google Scholar]
- 32.Zen Y, Chen YY, Jeng YM, Tsai HW, Yeh MM. Immune-related adverse reactions in the hepatobiliary system: second-generation check-point inhibitors highlight diverse histological changes. Histopathology 2020; 76:470–480. [DOI] [PubMed] [Google Scholar]
- 33.Zen Y, Yeh MM. Hepatotoxicity of immune checkpoint inhibitors: a histology study of seven cases in comparison with autoimmune hepatitis and idiosyncratic drug-induced liver injury. Mod Pathol 2018; 31:965–973. [DOI] [PubMed] [Google Scholar]
- 34.McClure T, Cui W, Asadi K, John T, Testro A. Case of nivolumab-induced sclerosing cholangitis: lessons from long-term follow-up. bmj Open Gastroenterol 2020; 7:e000487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Moi L, Bouchaab H, Mederos N, Nguyen-Ngoc T, Perreau M, Fenwick C, et al. Personalized cytokine-directed therapy with tocilizumab for refractory immune checkpoint inhibitor-related cholangiohepatitis. j Thorac Oncol 2021; 16:318–326. [DOI] [PubMed] [Google Scholar]
- 36.Nabeshima S, Yamasaki M, Matsumoto N, Takaki S, Nishi Y, Kawamoto K, et al. Atezolizumab-induced sclerosing cholangitis in a patient with lung cancer: a case report. Cancer Treat Res Commun 2021; 26:100270. [DOI] [PubMed] [Google Scholar]
- 37.Bonkovsky HL, Kleiner DE, Gu J, Odin JA, Russo MW, Navarro VM, et al.; U.S. Drug Induced Liver Injury Network Investigators. Clinical presentations and outcomes of bile duct loss caused by drugs and herbal and dietary supplements. Hepatology 2017; 65:1267–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Raschi E, Mazzarella A, Antonazzo IC, Bendinelli N, Forcesi E, Tuccori M, et al. Toxicities with immune checkpoint inhibitors: emerging priorities from disproportionality analysis of the FDA adverse event reporting system. Target Oncol 2019; 14:205–221. [DOI] [PubMed] [Google Scholar]
- 39.Nakanuma Y, Tsuneyama K, Harada K. Pathology and pathogenesis of intrahepatic bile duct loss. j Hepatobiliary Pancreat Surg 2001; 8:303–315. [DOI] [PubMed] [Google Scholar]
- 40.Visentin M, Lenggenhager D, Gai Z, Kullak-Ublick GA. Drug-induced bile duct injury. Biochim Biophys Acta Mol Basis Dis 2018; 1864:1498–1506. [DOI] [PubMed] [Google Scholar]
- 41.Anderson MA, Kurra V, Bradley W, Kilcoyne A, Mojtahed A, Lee SI. Abdominal immune-related adverse events: detection on ultrasonography, CT, MRI and 18F-Fluorodeoxyglucose positron emission tomography. Br j Radiol 2021; 94:20200663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mekki A, Dercle L, Lichtenstein P, Marabelle A, Michot JM, Lambotte O, et al. Detection of immune-related adverse events by medical imaging in patients treated with anti-programmed cell death 1. Eur j Cancer 2018; 96:91–104. [DOI] [PubMed] [Google Scholar]
- 43.Chu D, Adler DG. Malignant biliary tract obstruction: evaluation and therapy. j Natl Compr Canc Netw 2010; 8:1033–1044. [DOI] [PubMed] [Google Scholar]
- 44.Katabathina VS, Dasyam AK, Dasyam N, Hosseinzadeh K. Adult bile duct strictures: role of MR imaging and MR cholangiopancreatography in characterization. Radiographics 2014; 34:565–586. [DOI] [PubMed] [Google Scholar]
- 45.European Association for the Study of the Liver. EASL Clinical Practice Guidelines: management of cholestatic liver diseases. J Hepatol 2009; 51:237–267. [DOI] [PubMed] [Google Scholar]
- 46.European Association for the Study of the Liver. Electronic address: easloffice@easloffice.eu; Clinical Practice Guideline Panel: Chair; Panel members; EASL Governing Board representative. EASL Clinical Practice Guidelines: drug-induced liver injury. J Hepatol 2019; 70:1222–1261. [DOI] [PubMed] [Google Scholar]
- 47.Lim JH. Cholangiocarcinoma: morphologic classification according to growth pattern and imaging findings. ajr Am j Roentgenol 2003; 181:819–827. [DOI] [PubMed] [Google Scholar]
- 48.Granata V, Fusco R, Catalano O, Avallone A, Palaia R, Botti G, et al. Diagnostic accuracy of magnetic resonance, computed tomography and contrast enhanced ultrasound in radiological multimodality assessment of peribiliary liver metastases. PLoS One 2017; 12:e0179951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Moon SG, Han JK, Kim TK, Kim AY, Kim TJ, Choi BI. Biliary obstruction in metastatic disease: thin-section helical CT findings. Abdom Imaging 2003; 28:45–52. [DOI] [PubMed] [Google Scholar]
- 50.Delis S, Triantopoulou C, Bakoyiannis A, Tassopoulos N, Athanasiou K, Dervenis C. Sclerosing cholangitis in the era of target chemotherapy: a possible anti-VEGF effect. Dig Liver Dis 2009; 41:72–77. [DOI] [PubMed] [Google Scholar]
- 51.von Figura G, Stephani J, Wagner M, Wegener M, Wolf C, Adler G, Kulaksiz H. Secondary sclerosing cholangitis after chemotherapy with bevacizumab and paclitaxel. Endoscopy 2009; 41 (Suppl 2):E153–E154. [DOI] [PubMed] [Google Scholar]
- 52.Horsley-Silva JL, Dow EN, Menias CO, Smith ML, Carballido EM, Lindor KD, Vargas HE. Docetaxel induced sclerosing cholangitis. Dig Dis Sci 2015; 60:3814–3816. [DOI] [PubMed] [Google Scholar]
- 53.Matsuo T, Nakamura Y, Suzuki K. [A case of secondary sclerosing cholangitis caused by chemotherapy with nab-paclitaxel]. Nihon Shokakibyo Gakkai Zasshi 2015; 112:888–895. [DOI] [PubMed] [Google Scholar]
- 54.Kusakabe A, Ohkawa K, Fukutake N, Sakakibara M, Imai T, Abe Y, et al. Chemotherapy-induced sclerosing cholangitis caused by systemic chemotherapy. acg Case Rep j 2019; 6:e00136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Thompson JA, Schneider BJ, Brahmer J, Andrews S, Armand P, Bhatia S, et al. Management of immunotherapy-related toxicities, Version 1.2019. j Natl Compr Canc Netw 2019; 17:255–289. [DOI] [PubMed] [Google Scholar]
- 56.Wang T, Zhao X, Shao C, Ye L, Guo J, Peng N, et al. A proposed pathologic sub-classification of drug-induced liver injury. Hepatol Int 2019; 13:339–351. [DOI] [PubMed] [Google Scholar]
- 57.Oda H, Ishihara M, Miyahara Y, Nakamura J, Kozuka Y, Iwasa M, et al. First case of cytokine release syndrome after nivolumab for gastric cancer. Case Rep Oncol 2019; 12:147–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ooi R, Tobino K, Sakabe M, Kawabata T, Hiramatsu Y, Sueyasu T, Yoshimine K. A case of large-cell lung carcinoma successfully treated with pembrolizumab but complicated with cholangitis. Respir Med Case Rep 2020; 31:101197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Terziroli Beretta-Piccoli B, Mieli-Vergani G, Vergani D, Vierling JM, Adams D, Alpini G, et al. The challenges of primary biliary cholangitis: what is new and what needs to be done. j Autoimmun 2019; 105:102328. [DOI] [PubMed] [Google Scholar]
- 60.Roma MG, Toledo FD, Boaglio AC, Basiglio CL, Crocenzi FA, Sánchez Pozzi EJ. Ursodeoxycholic acid in cholestasis: linking action mechanisms to therapeutic applications. Clin Sci (Lond) 2011; 121:523–544. [DOI] [PubMed] [Google Scholar]
- 61.Fouchard M, Jantzem H, Quere G, Descourt R, Robinet G, Poureau PG. Three cases of immune cholangitis related to anti-programmed cell death and programmed cell death ligand agents for the treatment of non-small cell lung cancer. Eur j Cancer 2019; 115:107–110. [DOI] [PubMed] [Google Scholar]
- 62.Yildirim S, Deniz K, Doğan E, Başkol M, Gürsoy Ş, Özkan M. Ipilimumab-associated cholestatic hepatitis: a case report and literature review. Melanoma Res 2017; 27:380–382. [DOI] [PubMed] [Google Scholar]
- 63.Cho JH, Sun JM, Lee SH, Ahn JS, Park K, Ahn MJ. Late-onset cholecystitis with cholangitis after avelumab treatment in non-small cell lung cancer. j Thorac Oncol 2018; 13:e34–e36. [DOI] [PubMed] [Google Scholar]
- 64.Le Tallec E, Ricordel C, Triquet L, Deniel A, Marcorelles P, Lena H, et al. An Original case of an association of eosinophilic fasciitis with cholangitis induced by nivolumab. j Thorac Oncol 2019; 14:e13–e15. [DOI] [PubMed] [Google Scholar]
- 65.Anderson B, Dawe DE. Nivolumab-induced secondary sclerosing cholangitis with deterioration despite immunosuppression. j Thorac Oncol 2019; 14:e205–e206. [DOI] [PubMed] [Google Scholar]
- 66.Izumi H, Kodani M, Kurai J, Takeda K, Okazaki R, Yamane K, et al. Nivolumab-induced cholangitis in patients with non-small cell lung cancer: Case series and a review of literature. Mol Clin Oncol 2019; 11:439–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Reddy CA, Schneider BJ, Brackett LM, Tai AW. Nivolumab-induced large-duct cholangiopathy treated with ursodeoxycholic acid and tocilizumab. Immunotherapy 2019; 11:1527–1531. [DOI] [PubMed] [Google Scholar]
- 68.Imoto K, Kohjima M, Hioki T, Kurashige T, Kurokawa M, Tashiro S, et al. Clinical features of liver injury induced by immune checkpoint inhibitors in Japanese patients. Can j Gastroenterol Hepatol 2019; 2019:6391712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Onoyama T, Takeda Y, Yamashita T, Hamamoto W, Sakamoto Y, Koda H, et al. Programmed cell death-1 inhibitor-related sclerosing cholangitis: a systematic review. World j Gastroenterol 2020; 26:353–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zhang D, Hart J, Ding X, Zhang X, Feely M, Yassan L, et al. Histologic patterns of liver injury induced by anti-PD-1 therapy. Gastroenterol Rep (Oxf) 2020; 8:50–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Yoshikawa Y, Imamura M, Yamaoka K, Kosaka Y, Murakami E, Morio K, et al. A case with life-threatening secondary sclerosing cholangitis caused by nivolumab. Clin j Gastroenterol 2021; 14:283–287. [DOI] [PubMed] [Google Scholar]
- 72.Fujii M, Ozato T, Mizukawa S, Nasu J, Kawai H, Fujioka SI, et al. A rare case of immunotherapy-induced cholangitis and gastritis. Clin j Gastroenterol 2020; 13:1083–1090. [DOI] [PubMed] [Google Scholar]