Abstract
Objective
The direct and indirect mental health impacts of the COVID-19 pandemic are considerable. However, it is unclear how suicidal ideation was affected in communities during the acute lockdown phase of the pandemic, and over the longer-term. This study provides longitudinal data on the prevalence of, and risk factors for, suicidal ideation in the Australian national population, during the pandemic.
Method
The Australian National COVID-19 Mental Health and Risk Communication Survey assessed a nationally representative sample of Australian adults (N = 1296) fortnightly for 12 weeks from late-March to June 2020 (7 waves), and again in March 2021 (wave 8). Cox proportional hazards models examined demographic and pandemic-related risk factors for suicidal ideation over time.
Results
Prevalence of suicidal ideation was high but steady at ∼18% across the acute lockdown phase of the pandemic, and 16.2% in March 2021. People who had direct experience with COVID-19 (tested, diagnosed, or contact with someone who was diagnosed) had increased risk for suicidal ideation. Higher pandemic-related work and social impairment, recent adversity, loneliness, and being younger were also associated with increased risk of suicidal ideation over time.
Conclusion
Both the direct and indirect impacts of COVID-19 were associated with increased risk for suicidal ideation over time, although prevalence did not vary over time. The high prevalence of suicidal ideation in our sample flags a critical need for accessible mental health support, and findings provide insights into the factors placing people at risk during the pandemic.
Keywords: COVID-19, coronavirus disease-2019; SI, suicidal ideation; ACT, Australian Capital Territory; NSW, New South Wales; NT, Northern Territory; Qld, Queensland; SA, South Australia; Tas, Tasmania; Vic, Victoria; WA, Western Australia; WSAS, Work and Social Adjustment Scale; PHQ-9, Patient Health Questionnaire-9
Keywords: Suicide, Suicidal ideation, COVID-19, Social support
The effects of the COVID-19 pandemic on population mental health may be considerable. While there are concerns that direct contact with the virus may have physiological impacts that influence mental health (Orsini et al., 2020), it is likely that much of the mental health impact will arise from indirect effects such as lockdown, quarantine, economic changes, job losses and social changes related to the necessary public health responses to the pandemic (Dawel et al., 2020; Fancourt et al., 2021; Reger et al., 2020). There has also been concern that these impacts will lead to increases in suicidal behavior (Gunnell et al., 2020; McIntyre and Lee, 2020), although predictions of large-scale increases of 30% or more by 2021 (Atkinson et al., 2020; McIntyre and Lee, 2020) have not been supported by recent data (Leske et al., 2021; Pirkis et al., 2021). Such alarmist projections and speculation may be unhelpful, and have been criticised (Appleby, 2021) for being publicly disseminated in a way that is inconsistent with media guidelines to decrease suicide contagion effects (Niederkrotenthaler et al., 2020). The most consistent trend in suicide deaths has been stability or decreases across many nations (Appleby, 2021; John et al., 2020; Leske et al., 2021), although a modest increase in suicide deaths has been recorded in Japan (Tanaka and Okamoto, 2021).
Limited data has identified the effect of the pandemic on suicidal ideation. Although most people with suicidal thinking do not engage in suicidal behavior, suicidal ideation remains a strong risk factor for suicide (Baca-Garcia et al., 2011) and confers considerable burden on the population (van Spijker et al., 2011). Social isolation is known to be strongly associated with increased risk for suicidal thinking (Ma et al., 2016). The social disruptions associated with the COVID-19 pandemic may have led to increased perceived isolation for some people, although most studies have found stable levels of loneliness (Groarke et al., 2021; Luchetti et al., 2020; Varga et al., 2021). Financial distress, debt and unemployment are also robust risk factors for suicidal ideation (Elbogen et al., 2020; Gunnell et al., 2009; Meltzer et al., 2011), in addition to being common triggers for suicidal behavior (Coope et al., 2015). Increases in financial distress may have increased sharply in vulnerable communities during the pandemic. Similarly, relationship problems and domestic violence are strongly associated with suicidal thoughts and behaviors (Kazan et al., 2016; Scourfield and Evans, 2015), and may have increased in tandem with social and financial changes related to the pandemic (Morgan and Boxall, 2020). Changes in these multiple factors may consequently have directly influenced the risk of suicidal ideation in the community. It is also acknowledged that for many people, there were positive aspects to the pandemic, with reports of people taking more time to connect with their communities, friends and families (Williams et al., 2021).
Many studies to assess the impact of the pandemic on mental health were rapidly developed and implemented in early 2020. However, few of these studies were longitudinal or started sufficiently early to capture the initial effects of the implementation of public health restrictions in the community. Furthermore, few studies recruited population samples that were representative on the basis of key demographics, such as age, gender and location, with many studies relying on convenience samples that do not provide meaningful prevalence estimates. A UK longitudinal study using a representative sample found that suicidal ideation increased from 8.2% to 9.8% over the first six weeks of lockdown in March to May 2020, although depression symptoms and loneliness did not change significantly (O'Connor et al., 2020). A similar prevalence in suicidal ideation was observed in a US representative sample in June 2020 (10.7%), although no longitudinal data were collected (Czeisler et al., 2020). Other than these studies, limited population data has quantified the effects of COVID-19 on suicidal thinking. Furthermore, no studies have assessed long-term effects of the pandemic on suicidal ideation, nor assessed the impact of psychosocial aspects of the pandemic, such as financial or social change on suicidal ideation.
The aims of this study were: (1) to assess the prevalence of suicidal ideation in a representative population-based sample in the first 12 weeks of the COVID-19 pandemic in Australia, (2) to assess the persistence of suicidal ideation using long-term follow-up data, and, (3) to assess relationships between indirect effects of the pandemic (financial, social, employment) on suicidal ideation, while accounting for demographic factors.
1. Method
1.1. Participants and procedure
We launched a longitudinal survey in March 2020, when major restrictions began in Australia, with data collected every 2 weeks until mid-June 2020. This study was designed to be broadly representative of the Australian population; thus, recruitment was conducted using quota sampling across categories of age group, gender, and geographic location (Australian State/Territory). The inclusion criteria were that participants 1) must be living in Australia at the time of the survey, and 2) were able to respond to an online English language survey. Informed consent was obtained by participants reading an information sheet explaining the study, indicating that they understood this information, and clicking ‘yes’ to agree to start the survey. Any potential participants who did not agree (i.e., clicked ‘no’) were taken to a thank you page. The full study protocol is available here: https://psychology.anu.edu.au/files/COVID_MHBRCS_protocol.pdf
Our target was to retain a final sample of N=600 at Wave 7, assuming 50% attrition over the course of the study. This number of participants was chosen to allow examination of small effects within subgroups (e.g., 80% power to find an effect of d=0.33 between uneven subgroups of ratio 1:4) and allow for identification of up to distinct trajectories of mental health, accounting for attrition over time.We report data from the full study, which comprised eight waves of data. The first seven waves were collected every 2 weeks over a 12-week period from Wave 1 (survey launched 28 March, 2020). Long-term follow up data (12 months) were collected at Wave 8 (1-15 March 2021). Sample sizes at each wave were as follows: Wave 1=1296 (649 Females, 645 males, 2 missing gender), Wave 2=969, Wave 3=952, Wave 4=910, Wave 5=874, Wave 6=820, Wave 7=762, and finally Wave 8=519. The ethical aspects of the study were approved by The Australian National University Human Research Ethics Committee (protocol 2020/152). Written informed consent was obtained from all participants.
1.2. Measures
Suicidal ideation. The suicidal ideation item from the Patient Health Questionnaire-9 (PHQ-9; Spitzer et al., 1999) was used in the current study to assess presence of suicidal ideation: “Over the last 2 weeks, how often have you been bothered by the following problems? - Thoughts that you would be better off dead or of hurting yourself in some way”. Participants who responded “not at all” to the item were classified as having no suicidal ideation, while any other response (“Several days”, “More than half the days”, “Nearly every day”) was classified as having suicidal ideation present.
Loneliness. The 6-item De Jong Gierveld Loneliness Scale (Gierveld and Van Tilburg, 2006) was used to measure loneliness over the previous two weeks. Responses were recorded on a 5-point scale (No!, No, More or Less, Yes, Yes!) and summed after reverse-coding of selected items. Higher scores indicated greater feelings of loneliness, with total scale scores ranging from 6 to 30. The internal consistency of the scale was adequate (α=0.72).
COVID-related impairment. The extent to which work and social activities were impaired by COVID-19 was assessed using the Work and Social Adjustment Scale (WSAS; Mundt et al., 2002). Participants were asked to rate the level of impairment COVID-19 had caused for five work and social domains (ability to work, home management, social leisure activities, private leisure activities, and ability to form and maintain close relationships) on an 8-point scale ranging from 1 (Not at all impaired) to 8 (Very severely impaired). Total scores on this scale ranged from 6 to 30, with higher scores indicative of greater work and social impairment as a result of COVID-19 and adequate internal consistency (α=0.73).
COVID impacts. Three separate measures were used to examine the direct impacts of COVID on the sample at baseline (Dawel et al., 2020). Exposure to the COVID-19 virus was assessed through a series of yes/no items that enquired whether the respondent or a family member had been diagnosed with COVID-19, were awaiting results of a COVID-19 test or had been in direct contact with someone diagnosed with COVID-19. Participants who endorsed any of these items were classified as having exposure to COVID-19. The impact of COVID-19 on financial distress was assessed with the item ‘Over the past 2 weeks, to what extent have you experienced financial distress related to COVID-19?’. Participants responded to this item on a 6-point scale ranging from 1 (not at all) to 6 (extremely), with responses of ‘Quite a lot’ (score of 4) or greater classified as in financial distress. The impact of COVID-19 on employment was also evaluated and was determined as having an impact if the respondent reported either losing their job due to COVID-19, being forced to reduce their hours, or forced to take leave.
Socio-demographic variables. A range of socio-demographic variables were also measured to characterise the sample and to control for these factors in the models. These variables included participant age, gender, education (years), history of mental illness (none, past diagnosis, current diagnosis), having a partner (yes/no), living alone (yes/no) and impact of major adversities in the past year (“somewhat”, “a lot” or “extremely” vs. “not at all” or “a little”).
1.3. Analysis
Sample characteristics were compared on the basis of the identified independent variables, with differences between subgroups assessed using χ2 tests for categorical variables or t-tests for continuous variables. Changes in the prevalence of suicidal ideation between waves of the study were evaluated using McNemar's test in the full sample. A single Cox proportion hazards regression was used to simultaneously assess the independent effects of the identified risk factors on the hazard of suicidal ideation over the first three months of the study. Time to first report of suicidal ideation was the outcome variable, measured in days from the baseline assessment, and participants who reported no suicidal ideation were censored at the date of the final assessment that they completed. Nine (1%) participants were excluded from the model due to missing values on independent variables. To assess whether factors associated with incident suicidal ideation were consistent with those associated with prevalence of suicidal ideation, the model was re-estimated excluding participants who initially reported suicidal ideation at Wave 1 and excluding participants with missing data across Waves 2-7 (N=895). All analyses were conducted in SPSS v25 (IBM Corp, Chicago IL, USA).
2. Results
2.1. Sample characteristics
Tables 1 (categorical variables) and 2 (continuous variables) present participant characteristics, with comparisons based on presence or absence of suicidal ideation at Wave 1. By design, the sample was representative of the Australian population on the basis of age group (median adult age: 44 years in population vs 45 years in this sample) and gender (female: 50.7% in population vs 50.1% in this sample), as well as state of residence (Dawel et al., 2020). Initial prevalence of suicidal ideation was significantly elevated in participants who were male, younger, or reported a history of mental illness diagnosis. In relation to COVID-19 related impacts and outcomes, participants reporting higher levels of loneliness, work and social impairment due to COVID, direct COVID-19 impacts, and COVID effects on employment and financial distress were significantly more likely to report suicidal ideation at Wave 1. No differences were evident between participants reporting the presence or absence of suicidal ideation in terms of having a partner, living situation, location of residence or years of education. Only a few factors were associated with attrition from the study (Supplementary Table 1), including female gender, younger age, and reporting COVID-19 impacts on employment, finances or work/social impairment. However, presence of suicidal ideation or mental illness at Wave 1 and other sociodemographic factors including living situation, education and location had no relationship with survey completion.
Table 1.
Characteristics of the sample, with prevalence of Wave 1 suicidal ideation–Categorical variables.
| n | % | Wave 1 SI (%) | |
|---|---|---|---|
| Total | 1296 | 100.0% | 17.1% |
| Gender | |||
| Female | 649 | 50.1% | 14.8%* |
| Male | 645 | 49.8% | 19.4% |
| History of mental illness | |||
| None reported | 740 | 57.1% | 9.7%⁎⁎⁎ |
| Past diagnosis | 246 | 19.0% | 17.5% |
| Current diagnosis | 310 | 23.9% | 34.5% |
| COVID impacted employment | |||
| Yes | 304 | 23.5% | 24.7%⁎⁎⁎ |
| No | 992 | 76.5% | 14.8% |
| COVID-related financial distress | |||
| Yes | 421 | 32.5% | 29.7%⁎⁎⁎ |
| No | 875 | 67.5% | 11.1% |
| Direct COVID impact | |||
| Yes | 36 | 2.8% | 31.3%⁎⁎ |
| No | 1260 | 97.2% | 16.7% |
| Have a partner | |||
| Yes | 853 | 65.8% | 15.7% |
| No | 443 | 34.2% | 19.9% |
| Live alone | |||
| Yes | 157 | 12.1% | 14.6% |
| No | 1139 | 87.9% | 17.5% |
| State/Territory of residence | |||
| ACT | 37 | 2.9% | 10.8% |
| NSW | 409 | 31.6% | 17.2% |
| NT | 12 | 0.9% | 8.3% |
| Qld | 249 | 19.2% | 19.3% |
| SA | 96 | 7.4% | 18.8% |
| Tas | 36 | 2.8% | 8.3% |
| Vic | 313 | 24.2% | 18.5% |
| WA | 144 | 11.1% | 13.9% |
Notes: COVID: coronavirus disease-2019; SI: suicidal ideation; ACT: Australian Capital Territory; NSW: New South Wales; NT: Northern Territory; QLD: Queensland; SA: South Australia; Tas: Tasmania; Vic: Victoria; WA: Western Australia; Wave 1 prevalence comparisons based on χ2 statistics, with
p<.05,
p<.01,
p<.001
Table 2.
Characteristics of the sample based on Wave 1 suicidal ideation–Continuous variables.
| Total sample (n=1296) |
Wave 1 SI present (n=222) |
Wave 1 SI absent (n=1074) |
||||
|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | |
| Age in years | 46.0 | 17.3 | 39.5 | 15.7 | 47.4 | 17.3⁎⁎⁎ |
| Years of education | 14.6 | 1.8 | 14.5 | 1.7 | 14.6 | 1.8 |
| COVID-related impairment | 20.6 | 9.3 | 25.5 | 10.3 | 19.5 | 8.7⁎⁎⁎ |
| Loneliness | 15.6 | 4.3 | 19.2 | 4.0 | 14.9 | 4.0⁎⁎⁎ |
Notes: COVID: coronavirus disease-2019; SI: suicidal ideation; Wave 1 comparisons for SI present vs. absent based on independent t-tests, with * p<.05, ⁎⁎p<.01, ⁎⁎⁎p<.001
2.2. Prevalence of suicidal ideation
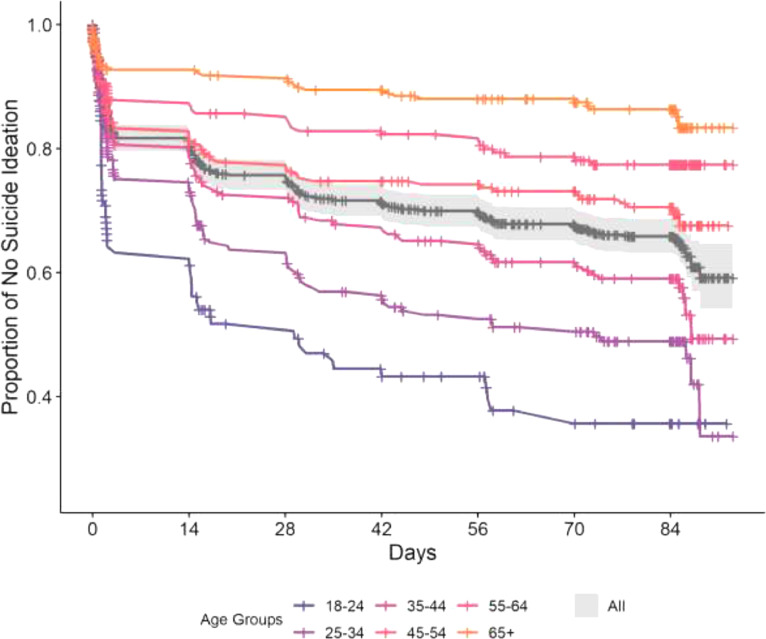
Of the 1296 participants in the study, 395 (30.5%) reported suicidal ideation at one or more time points in the first 12 weeks, including 115 (8.9%) who reported suicidal ideation at every assessment that they completed. Among participants who reported no ideation at Wave 1 (n=1073), 173 (16.1%) reported suicidal ideation at one or more occasions in the subsequent 12 weeks. The Kaplan-Meier curves in Fig. 1 show the proportion of the sample without suicidal ideation over time, both for the whole sample and categorised by age group. While fewer than 15% of participants aged 55 years and older reported suicidal ideation at any time point, young adults had much higher prevalence, with approximately 60% of 18-34 year olds reporting suicidal thoughts.
Fig. 1.
Kaplan-Meier curves of the proportion of the sample reporting suicidal ideation in the first 12 weeks of the COVID-19 pandemic, for the complete sample (N=1296) and by age group.
Note: crosses (+) indicate censored observations, shading indicates 95% confidence interval for total sample.
At Wave 1 (28-31 Mar 2020), 17.1% of participants (222/1295) reported suicidal ideation. Although the prevalence increased marginally at Wave 2 in mid-April (19.0%, 184/969) and Wave 3 in late-April (19.6% 186/950), wave-on-wave changes were not significant based on McNemar's test (p>0.09 for all comparisons). The change between the highest prevalence (Wave 3) and lowest prevalence (Wave 1) was also not significant (Z=-1.85, p=.064). Prevalence of suicidal ideation in subsequent waves remained steady at approximately 18% through until Wave 7 (20-25 June).
2.3. Long-term suicidal ideation
At the long-term follow-up (March 2021), prevalence of suicidal ideation was 16.2% (84/519), which was not significantly different from any of the earlier waves. There were 13 (2.5%, N=519) participants who reported suicidal ideation at the long-term follow-up who had not previously reported suicidal ideation.
2.4. Factors associated with suicidal ideation
To account for emergence of suicidal ideation over time, a fully-adjusted Cox proportional hazards regression was conducted to examine baseline factors associated with suicidal ideation in the first 12 weeks of the study (Table 3 ). Current diagnosis of mental illness was associated with double the risk of suicidal ideation, while past diagnosis was associated with a 38% increase in risk. COVID-related financial distress and having a direct COVID impact were also associated with a 47% and 62% increased risk of suicidal ideation respectively. The risk of suicidal ideation was also 65% higher in participants reporting a recent adversity. Females had a 36% lower risk of suicidal ideation than males, and the risk of suicidal ideation decreased with older age by 2.5% per year. One unit increases in loneliness or work and social impairment due to COVID-19 were also associated with a 16% and 2.2% increase in suicidal ideation risk respectively. There was no association between suicidal ideation and years of education, COVID impacts on employment, having a partner or living alone at baseline.
Table 3.
Cox proportional hazards regression of time to report suicidal ideation (N=1287).
| Variable | Hazard ratio | 95% CI |
|---|---|---|
| Age in years | 0.976 | 0.969, 0.984 |
| Female vs male | 0.638 | 0.519, 0.785 |
| Years of education | 1.013 | 0.954, 1.076 |
| History of mental illness | ||
| No history (reference) | – | – |
| Past diagnosis | 1.383 | 1.046, 1.829 |
| Current diagnosis | 2.027 | 1.596, 2.574 |
| COVID impacted employment | 0.923 | 0.725, 1.175 |
| COVID-related financial distress | 1.466 | 1.170, 1.836 |
| Direct COVID impact | 1.616 | 1.028, 2.539 |
| Have a partner | 0.999 | 0.795, 1.255 |
| Live alone | 0.870 | 0.609, 1.242 |
| COVID impairment (WSAS) | 1.022 | 1.010, 1.036 |
| Loneliness | 1.160 | 1.131, 1.190 |
| Recent adversity | 1.651 | 1.328, 2.054 |
Notes: COVID: coronavirus disease-2019; WSAS: Work and Social Adjustment Scale; bold values represent p<0.05
To assess factors associated with incident suicidal ideation, the model was re-estimated, excluding participants who initially reported suicidal ideation at Wave 1 (n=222), missing outcome data (n=171) or missing data for independent variables (n=8). This model (n=895, Supplementary Table 2) compared participants with no suicidal ideation to those who first reported suicidal ideation at one or more of the follow-up assessments. The outcome of the model was broadly consistent with the original analysis with three exceptions: gender (χ2=2.47, p=0.12), past mental health diagnosis (χ2=0.47, p=0.49) and COVID-related financial distress (χ2=3.65, p=0.06) were not significantly associated with incident suicidal ideation.
3. Discussion
This study found that the prevalence of suicidal ideation did not significantly increase or decrease during the COVID-19 pandemic in a representative Australian population sample. The prevalence of suicidal ideation was higher than in other population-based studies in the United States and United Kingdom during the same period (Czeisler et al., 2020; O'Connor et al., 2020). This difference might reflect the question used to assess suicidal ideation, which also included self-harm ideation. In addition, although the sample was representative of the basis of age, gender and location, it is possible that selection biases were present on the basis of interest in mental health. We made efforts to emphasise the general health focus of the survey, yet participants may have been aware of the considerable mental health focus, based on the questions. Alternatively, it may be the case that the prevalence of suicidal ideation may be higher in Australia compared to other nations, as suggested in previous research (Mortier et al., 2018).
There were a number of psychosocial and demographic factors associated with suicidal ideation. Financial, social and work impairment related to COVID-19 were robustly associated with increased suicidal ideation, as was direct exposure to COVID-19. Although this study was longitudinal, it could still be the case that people who were vulnerable to suicidal ideation were also more vulnerable to financial, social, work and health challenges, rather than these factors having a causal relationship. Evidence was also seen for established risk factors of loneliness (Ma et al., 2016; McClelland et al., 2020), life adversities (Liu and Miller, 2014) and existing mental health conditions (Batterham et al., 2018; Nock et al., 2010) having a considerable influence on suicidal ideation. These relationships suggest that the people in the community with existing vulnerabilities such as social isolation, life adversities, mental ill health or financial hardship might be at particular risk for suicidal ideation during a pandemic. While variation in ideation over time was not observed, it may be the case that subgroups of the population experience magnified risk over time in response to major societal stressors such as a pandemic and the necessary public health response. Younger people were more likely to report suicidal ideation, consistent with previous research (Fairweather et al., 2007). Interestingly in the multivariate model, males were more likely to report suicidal ideation than females, which is inconsistent with previous population data (Johnston et al., 2009) and with trends seen for depression and anxiety during the COVID-19 pandemic (Dawel et al., 2020). However, the difference was non-significant when examining new onset of suicidal ideation.
The findings of this study are somewhat divergent to previous research. Unlike the UK longitudinal study (O'Connor et al., 2020), we found no evidence for an increase in suicidal ideation in the first several weeks of the pandemic in Australia. The UK has had more than 50 times as many COVID-19 cases and deaths per capita, and greater societal disruption compared to Australia, with multiple periods of extended lockdowns. Australia has been fortunate to be spared the high incidence and death rate of COVID-19 infections seen in many other nations. There was a large COVID-19 outbreak in the State of Victoria from June to October 2020, with up to 7000 simultaneous active cases and strict lockdowns, which was not directly captured in these data. While the impacts of the pandemic on suicidal ideation appear to be modest in Australia, the picture may be different in countries with high incidence and greater societal disruption. Changes in suicidal ideation may also be discrepant from variation in suicide attempts and deaths. Previous studies on the effects of SARS suggest that suicide deaths were modestly elevated over several years particularly among older adults following that pandemic in 2003 (Cheung et al., 2008). However, the current findings appear to suggest that the lack of increase in suicide deaths may also be reflected in relatively stable levels of suicidal ideation, which contradicts predictive modelling from early in the pandemic (Atkinson et al., 2020; McIntyre and Lee, 2020). There also appeared to be less change in suicidal ideation than in depression and anxiety symptoms during this period (Batterham et al., In press).
This is one of the first longitudinal studies to assess long-term effects of the COVID-19 pandemic on suicidal thoughts in the population. However, the findings should be interpreted in light of the limitations of the study. First, we used a single-item measure of suicidal ideation that also incorporates self-harm ideation. While these two outcomes are closely connected, there may have been a proportion of participants who endorsed the item who had passive suicidal thinking or a desire to harm themselves without dying. While a more detailed measure of suicidal thinking was not feasible in the context of an anonymized online survey, further research to assess the effects of the pandemic on suicidal thoughts and behaviors would benefit from the use of an established scale (Batterham et al., 2015). Second, while the sample was initially established to be representative on the basis of age group, gender and location, as noted above, it is possible that selection biases were present on the basis of interest in mental health or differential attrition. We also found that females, younger adults and those most impacted by the pandemic were less likely to complete later surveys. Third, while the study began early in the pandemic at the start of restrictions in Australia, the first assessment was not a true baseline as participants were already experiencing or anticipating the impacts of the pandemic. Relatedly, the assessment of incident suicidal ideation did not account for suicidal ideation in the period before the baseline assessment. The episodic nature of suicidal ideation and imprecise recall of past suicidal experience (Klimes-Dougan et al., 2007) are limitations inherent to much suicide prevention research. Fourth, there are a number of other factors that may influence suicidal ideation that were not included in the present models.
It is critical to monitor mental health outcomes and suicidality during large scale crises such as pandemics. Consistent with emerging data on suicide deaths, we found no changes in suicidal ideation during and one year following the early phase of the COVID-19 pandemic in Australia. However, our data showed that robust predictors of suicidal ideation remained salient during the pandemic, highlighting the ongoing need to support those in the community with vulnerabilities that are known to increase suicide risk. As parts of the world continue to be disproportionately impacted by the COVID-19 pandemic, there is a need for further studies to examine cross-national and cross-cultural variability in the prevalence and correlates of suicidal ideation associated with the pandemic. Relatedly, there is also a need for ongoing and long-term monitoring of suicidal ideation in the population, as disruptions related to the pandemic may continue to impact mental health after the most acute phases of the pandemic are over.
Contributors
All authors contributed to the design of the study, contributed to data collection, contributed to the interpretation of findings, critically edited the manuscript and approved of the submitted version of the manuscript. In addition, PJB conducted the analyses and wrote the first draft of the manuscript, YS contributed to the analyses, and AD managed the study.
Funding
This project was supported by funding from the College of Health and Medicine at the Australian National University. PJB and ALC are supported by National Health and Medical Research Council (NHMRC) Fellowships 1158707 and 1173146 respectively. YS and LF are supported by ARC DECRA fellowships DE180100015 and DE190101382 respectively.
Role of the funding source
The funding sources had no role in the study design, collection/ analysis/ interpretation of data, writing of the report, or the decision to submit the article for publication.
Declaration of Competing Interest
None
Acknowledgments
We gratefully acknowledge the team members who contributed to the design and management of the study: Kristen Murray, Michael Smithson, Tambri Housen, and Eryn Newman, Alyssa Morse, Michelle Banfield, Rachael Rodney Harris and Nicolas Cherbuin.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2022.01.022.
Appendix. Supplementary materials
References
- Appleby L. What has been the effect of COVID-19 on suicide rates? BMJ. 2021;372:n834. doi: 10.1136/bmj.n834. [DOI] [PubMed] [Google Scholar]
- Atkinson J.-A., Skinner A., Lawson K., Song Y., Hickie I. 2020. Road to Recovery–Restoring Australia's Mental Wealth. Uncovering the Road to Recovery of our Mental Health and Wellbeing using Systems Modeling and Simulation. Sydney. [Google Scholar]
- Baca-Garcia E., Perez-Rodriguez M.M., Oquendo M.A., Keyes K.M., Hasin D.S., Grant B.F., Blanco C. Estimating risk for suicide attempt–Are we asking the right questions? Passive suicidal ideation as a marker for suicidal behavior. J. Affect. Disord. 2011;134:327–332. doi: 10.1016/j.jad.2011.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batterham, P., Calear, A., McCallum, S., Morse, A., Banfield, M., Farrer, L., Gulliver, A., Cherbuin, N., Rodney Harris, R., Shou, Y., Dawel, A., In press. Longitudinal trajectories of depression and anxiety symptoms during the COVID-19 pandemic in a representative Australian adult cohort. Medical Journal of Australia. [DOI] [PMC free article] [PubMed]
- Batterham P.J., Calear A.L., Christensen H., Carragher N., Sunderland M. Independent effects of mental disorders on suicidal behavior in the community. Suicide Life Threat. Behav. 2018;48:512–521. doi: 10.1111/sltb.12379. [DOI] [PubMed] [Google Scholar]
- Batterham P.J., Ftanou M., Pirkis J., Brewer J.L., Mackinnon A.J., Beautrais A., Fairweather-Schmidt A.K., Christensen H. A systematic review and evaluation of measures for suicidal ideation and behaviors in population-based research. Psychol. Assess. 2015;27:501–512. doi: 10.1037/pas0000053. [DOI] [PubMed] [Google Scholar]
- Cheung Y.T., Chau P.H., Yip P.S. A revisit on older adults suicides and Severe Acute Respiratory Syndrome (SARS) epidemic in Hong Kong. Int. J. Geriatr. Psychiatry. 2008;23:1231–1238. doi: 10.1002/gps.2056. [DOI] [PubMed] [Google Scholar]
- Coope C., Donovan J., Wilson C., Barnes M., Metcalfe C., Hollingworth W., Kapur N., Hawton K., Gunnell D. Characteristics of people dying by suicide after job loss, financial difficulties and other economic stressors during a period of recession (2010-2011)–A review of coroners records. J. Affect. Disord. 2015;183:98–105. doi: 10.1016/j.jad.2015.04.045. [DOI] [PubMed] [Google Scholar]
- Czeisler M.E., Lane R.I., Petrosky E., Wiley J.F., Christensen A., Njai R., Weaver M.D., Robbins R., Facer-Childs E.R., Barger L.K., Czeisler C.A., Howard M.E., Rajaratnam S.M.W. Mental health, substance use, and suicidal ideation during the COVID-19 Pandemic - United States, June 24-30, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020;69:1049–1057. doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawel A., Shou Y., Smithson M., Cherbuin N., Banfield M., Calear A.L., Farrer L.M., Gray D., Gulliver A., Housen T., McCallum S.M., Morse A.R., Murray K., Newman E., Rodney Harris R.M., Batterham P.J. The effect of COVID-19 on mental health and wellbeing in a representative sample of Australian adults. Front. Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.579985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elbogen E.B., Lanier M., Montgomery A.E., Strickland S., Wagner H.R., Tsai J. Financial strain and suicide attempts in a nationally representative sample of US Adults. Am. J. Epidemiol. 2020;189:1266–1274. doi: 10.1093/aje/kwaa146. [DOI] [PubMed] [Google Scholar]
- Fairweather A.K., Anstey K.J., Rodgers B., Jorm A.F., Christensen H. Age and gender differences among Australian suicide ideators–Prevalence and correlates. J. Nerv. Ment. Dis. 2007;195:130–136. doi: 10.1097/01.nmd.0000254746.15325.fa. [DOI] [PubMed] [Google Scholar]
- Fancourt D., Steptoe A., Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England–A longitudinal observational study. Lancet Psychiatry. 2021;8:141–149. doi: 10.1016/S2215-0366(20)30482-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gierveld J.D., Van Tilburg T. A 6-item scale for overall, emotional, and social loneliness–Confirmatory tests on survey data. Res. Aging. 2006;28:582–598. [Google Scholar]
- Groarke J.M., McGlinchey E., McKenna-Plumley P.E., Berry E., Graham-Wisener L., Armour C. Examining temporal interactions between loneliness and depressive symptoms and the mediating role of emotion regulation difficulties among UK residents during the COVID-19 lockdown–Longitudinal results from the COVID-19 psychological wellbeing study. J. Affect. Disord. 2021;285:1–9. doi: 10.1016/j.jad.2021.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunnell D., Appleby L., Arensman E., Hawton K., John A., Kapur N., Khan M., O'Connor R.C., Pirkis J., Collaboration C.-S.P.R. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry. 2020;7:468–471. doi: 10.1016/S2215-0366(20)30171-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunnell D., Platt S., Hawton K. The economic crisis and suicide. BMJ. 2009;338:b1891. doi: 10.1136/bmj.b1891. [DOI] [PubMed] [Google Scholar]
- John A., Pirkis J., Gunnell D., Appleby L., Morrissey J. Trends in suicide during the COVID-19 pandemic. BMJ. 2020;371:m4352. doi: 10.1136/bmj.m4352. [DOI] [PubMed] [Google Scholar]
- Johnston A.K., Pirkis J.E., Burgess P.M. Suicidal thoughts and behaviors among Australian adults–Findings from the 2007 National Survey of mental health and wellbeing. Aust. N. Z. J. Psychiatry. 2009;43:635–643. doi: 10.1080/00048670902970874. [DOI] [PubMed] [Google Scholar]
- Kazan D., Calear A.L., Batterham P.J. The impact of intimate partner relationships on suicidal thoughts and behaviors–A systematic review. J. Affect. Disord. 2016;190:585–598. doi: 10.1016/j.jad.2015.11.003. [DOI] [PubMed] [Google Scholar]
- Klimes-Dougan B., Safer M.A., Ronsaville D., Tinsley R., Harris S.J. The value of forgetting suicidal thoughts and behavior. Suicide Life Threat. Behav. 2007;37:431–438. doi: 10.1521/suli.2007.37.4.431. [DOI] [PubMed] [Google Scholar]
- Leske S., Kolves K., Crompton D., Arensman E., de Leo, D. Real-time suicide mortality data from police reports in Queensland, Australia, during the COVID-19 pandemic–An interrupted time-series analysis. Lancet Psychiatry. 2021;8:58–63. doi: 10.1016/S2215-0366(20)30435-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu R.T., Miller I. Life events and suicidal ideation and behavior–A systematic review. Clin. Psychol. Rev. 2014;34:181–192. doi: 10.1016/j.cpr.2014.01.006. [DOI] [PubMed] [Google Scholar]
- Luchetti M., Lee J.H., Aschwanden D., Sesker A., Strickhouser J.E., Terracciano A., Sutin A.R. The trajectory of loneliness in response to COVID-19. Am. Psychol. 2020;75:897–908. doi: 10.1037/amp0000690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma J., Batterham P.J., Calear A.L., Han J. A systematic review of the predictions of the interpersonal-psychological theory of suicidal behavior. Clin. Psychol. Rev. 2016;46:34–45. doi: 10.1016/j.cpr.2016.04.008. [DOI] [PubMed] [Google Scholar]
- McClelland H., Evans J.J., Nowland R., Ferguson E., O'Connor R.C. Loneliness as a predictor of suicidal ideation and behavior–A systematic review and meta-analysis of prospective studies. J. Affect. Disord. 2020;274:880–896. doi: 10.1016/j.jad.2020.05.004. [DOI] [PubMed] [Google Scholar]
- McIntyre R.S., Lee Y. Projected increases in suicide in Canada as a consequence of COVID-19. Psychiatry Res. 2020;290 doi: 10.1016/j.psychres.2020.113104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meltzer H., Bebbington P., Brugha T., Jenkins R., McManus S., Dennis M.S. Personal debt and suicidal ideation. Psychol. Med. 2011;41:771–778. doi: 10.1017/S0033291710001261. [DOI] [PubMed] [Google Scholar]
- Morgan, A., Boxall, H., 2020. Social isolation, time spent at home, financial stress and domestic violence during the COVID-19 pandemic. Trends Iss Crime Cri.
- Mortier P., Auerbach R.P., Alonso J., Bantjes J., Benjet C., Cuijpers P., Ebert D.D., Green J.G., Hasking P., Nock M.K., O'Neill S., Pinder-Amaker S., Sampson N.A., Vilagut G., Zaslavsky A.M., Bruffaerts R., Kessler R.C., Collaborators W.W.-I. Suicidal thoughts and behaviors among first-year college students–Results from the WMH-ICS project. J. Am. Acad. Child Adolesc. Psychiatry. 2018;57:263–273. doi: 10.1016/j.jaac.2018.01.018. e261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mundt J.C., Marks I.M., Shear M.K., Greist J.H. The work and social adjustment scale–A simple measure of impairment in functioning. Br. J. Psychiatry. 2002;180:461–464. doi: 10.1192/bjp.180.5.461. [DOI] [PubMed] [Google Scholar]
- Niederkrotenthaler T., Braun M., Pirkis J., Till B., Stack S., Sinyor M., Tran U.S., Voracek M., Cheng Q., Arendt F., Scherr S., Yip P.S.F., Spittal M.J. Association between suicide reporting in the media and suicide–Systematic review and meta-analysis. BMJ. 2020;368:m575. doi: 10.1136/bmj.m575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock M.K., Hwang I., Sampson N.A., Kessler R.C. Mental disorders, comorbidity and suicidal behavior–Results from the national comorbidity survey replication. Mol. Psychiatry. 2010;15:868–876. doi: 10.1038/mp.2009.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Connor R.C., Wetherall K., Cleare S., McClelland H., Melson A.J., Niedzwiedz C.L., O'Carroll R.E., O'Connor D.B., Platt S., Scowcroft E., Watson B., Zortea T., Ferguson E., Robb K.A. Mental health and well-being during the COVID-19 pandemic–Longitudinal analyses of adults in the UK COVID-19 mental health & wellbeing study. Br. J. Psychiatry. 2020:1–8. doi: 10.1192/bjp.2020.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orsini A., Corsi M., Santangelo A., Riva A., Peroni D., Foiadelli T., Savasta S., Striano P. Challenges and management of neurological and psychiatric manifestations in SARS-CoV-2 (COVID-19) patients. Neurol. Sci. 2020;41:2353–2366. doi: 10.1007/s10072-020-04544-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirkis J., John A., Shin S., DelPozo-Banos M., Arya V., Analuisa-Aguilar P., Appleby L., Arensman E., Bantjes J., Baran A., Bertolote J.M., Borges G., Brecic P., Caine E., Castelpietra G., Chang S.S., Colchester D., Crompton D., Curkovic M., Deisenhammer E.A., Du C., Dwyer J., Erlangsen A., Faust J.S., Fortune S., Garrett A., George D., Gerstner R., Gilissen R., Gould M., Hawton K., Kanter J., Kapur N., Khan M., Kirtley O.J., Knipe D., Kolves K., Leske S., Marahatta K., Mittendorfer-Rutz E., Neznanov N., Niederkrotenthaler T., Nielsen E., Nordentoft M., Oberlerchner H., O'Connor R.C., Pearson M., Phillips M.R., Platt S., Plener P.L., Psota G., Qin P., Radeloff D., Rados C., Reif A., Reif-Leonhard C., Rozanov V., Schlang C., Schneider B., Semenova N., Sinyor M., Townsend E., Ueda M., Vijayakumar L., Webb R.T., Weerasinghe M., Zalsman G., Gunnell D., Spittal M.J. Suicide trends in the early months of the COVID-19 pandemic–An interrupted time-series analysis of preliminary data from 21 countries. Lancet Psychiatry. 2021 doi: 10.1016/S2215-0366(21)00091-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reger M.A., Piccirillo M.L., Buchman-Schmitt J.M. COVID-19, mental health, and suicide risk among health care workers–Looking beyond the crisis. J. Clin. Psychiatry. 2020:81. doi: 10.4088/JCP.20com13381. [DOI] [PubMed] [Google Scholar]
- Scourfield J., Evans R. Why might men be more at risk of suicide after a relationship breakdown? Sociological insights. Am. J. Mens Health. 2015;9:380–384. doi: 10.1177/1557988314546395. [DOI] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B. Validation and utility of a self-report version of PRIME-MD–The PHQ primary care study. Primary care evaluation of mental disorders. Patient health questionnaire. JAMA. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Tanaka T., Okamoto S. Increase in suicide following an initial decline during the COVID-19 pandemic in Japan. Nat. Hum. Behav. 2021;5:229–238. doi: 10.1038/s41562-020-01042-z. [DOI] [PubMed] [Google Scholar]
- van Spijker B.A., van Straten A., Kerkhof A.J., Hoeymans N., Smit F. Disability weights for suicidal thoughts and non-fatal suicide attempts. J. Affect. Disord. 2011;134:341–347. doi: 10.1016/j.jad.2011.05.020. [DOI] [PubMed] [Google Scholar]
- Varga T.V., Bu F., Dissing A.S., Elsenburg L.K., Bustamante J.J.H., Matta J., van Zon S.K.R., Brouwer S., Bultmann U., Fancourt D., Hoeyer K., Goldberg M., Melchior M., Strandberg-Larsen K., Zins M., Clotworthy A., Rod N.H. Loneliness, worries, anxiety, and precautionary behaviors in response to the COVID-19 pandemic–A longitudinal analysis of 200,000 Western and Northern Europeans. Lancet Reg. Health Eur. 2021;2 doi: 10.1016/j.lanepe.2020.100020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams L., Rollins L., Young D., Fleming L., Grealy M., Janssen X., Kirk A., MacDonald B., Flowers P. What have we learned about positive changes experienced during COVID-19 lockdown? Evidence of the social patterning of change. PLoS One. 2021;16 doi: 10.1371/journal.pone.0244873. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.