Abstract
The discriminatory power of gyrB DNA sequence polymorphisms for differentiation of the species of the Mycobacterium tuberculosis complex (MTBC) was evaluated by sequencing and restriction fragment length polymorphism (RFLP) analysis of a 1,020-bp fragment amplified from clinical isolates of M. tuberculosis, Mycobacterium bovis (pyrazinamide [PZA] resistant as well as PZA susceptible), Mycobacterium africanum subtypes I and II, and Mycobacterium microti types vole and llama. We found sequence polymorphisms in four regions described previously and at one additional position. These differences in the gyrB sequences allow an accurate discrimination of M. bovis, M. microti, and M. africanum subtype I. The PZA-susceptible subtypes of M. bovis shared the M. bovis-specific substitution at position 756 with the PZA-resistant strains, but can be unambiguously differentiated by a characteristic substitution at position 1311. As a drawback, M. tuberculosis and M. africanum subtype II showed an identical gyrB sequence that facilitates discrimination from the other species, but not from each other. A PCR-RFLP technique applying three restriction enzymes could be shown to be a rapid and easy-to-perform tool for the differentiation of the members of the MTBC. Based on these results, we present a clear diagnostic algorithm for the differentiation of species of the MTBC.
The closely related species Mycobacterium tuberculosis, Mycobacterium bovis, Mycobacterium africanum, and Mycobacterium microti that form the M. tuberculosis complex (MTBC) are the causative agents of tuberculosis (TB) in humans and animals (20). Their close relationship has been demonstrated by DNA-DNA hybridization, by multilocus enzyme electrophoresis, and sequencing of the 16S ribosomal DNA (rDNA) gene and the 16S-to-23S rDNA internal transcribed spacer (ITS) (4, 5, 7, 11, 14, 19). Despite this close genetic relatedness, the members of the MTBC differ in their host range and pathogenicity (20). The natural habitat of M. tuberculosis and M. africanum is humans. According to the latest figures of the World Health Organization (22), M. tuberculosis infects more than one-third of the world's population. M. africanum has been described as representing up to 60% of the isolates obtained from patients with pulmonary TB in certain regions in Africa (6; V. Sticht-Groh, G. Bretzel, S. Rüsch-Gerdes, S. Bwire, and H. J. S. Kawuma, 28th World Conf. IUATLD/UICTMR, abstr. A169, 1994). Based on their biochemical characteristics, two major subgroups of M. africanum have been described that correspond to their geographic origin in West or East Africa (subtypes I and II) (3, 14). M. bovis can cause disease in a wide range of domestic or wild animals, such as cattle or goats, as well as in humans (20). Resistance to pyrazinamide (PZA) is a major criterion for the differentiation of M. bovis, but some studies report susceptibility to PZA among M. bovis isolates (2, 21), and recently two PZA-susceptible subtypes of M. bovis have been described (14). M. microti has been reported to infect both small rodents like voles and, more recently, humans (19, 20).
All species of the MTBC are characterized by identical 16S rRNA gene and ITS sequences as well as by a number of specific repetitive elements, like the insertion sequence IS6110 or the direct repeat (DR) locus, that allow a rapid identification of the MTBC by gene probes or PCR methods (12, 16). In contrast, routine differentiation is still based on a number of phenotypic characteristics and biochemical tests, such as nitrate reduction or niacin accumulation (20). These tests need sufficient bacterial growth, are time-consuming, do not allow an unambiguous species identification in every case, and may not be performed by every laboratory routinely. Hence, further methods allowing accurate and rapid species identification are urgently needed for clinical and epidemiological purposes. To solve this problem, over the last few years, several DNA-based techniques have been evaluated, and spoligotyping and other molecular methods have been demonstrated to be useful tools for rapid species differentiation (8, 12, 14, 15, 17–19). However, none of these molecular markers could be used solely, and no molecular technique facilitates the differentiation of all four species (e.g., differentiation of M. tuberculosis and M. africanum remained dependent on biochemical tests) (14). Recently, Kasai and coworkers (9) reported DNA sequence variations in the gyrB gene that may be useful for species differentiation of slowly growing mycobacteria and even for the differentiation of members of the MTBC.
The aim of this study was to evaluate the discriminatory power of gyrB sequence polymorphisms for differentiation of clinical MTBC isolates. The gyrB sequences of a 1,020-bp region comprising the four species-specific positions described by Kasai et al. (9) from clinical isolates of M. bovis (PZA resistant as well as PZA susceptible) and M. africanum subtypes I and II have been analyzed. Moreover, clinical isolates of M. tuberculosis and of M. microti types vole and llama have been included.
MATERIALS AND METHODS
Strains analyzed.
A total of 30 MTBC strains comprising 5 M. tuberculosis strains (isolated in 1999 from patients living in the area of Hamburg, Germany), 12 M. bovis strains (isolated in 1998 and 1999 from patients living in different parts of Germany [one strain obtained from cattle]), 10 M. africanum strains (isolated in 1998 from patients living in Germany, Uganda, Cameroon, and Nigeria), and 3 M. microti strains (isolated in 1999 from patients living in different parts of Germany) were analyzed in this study (Table 1). The M. bovis and M. africanum strains are a subset of a collection described previously (14). The main biochemical and genetic characteristics are summarized in Table 1. Furthermore, reference strains M. tuberculosis H37Rv and M. bovis BCG, as well as five drug-resistant M. tuberculosis strains (resistance patterns ranged from single resistance to isoniazid to multidrug resistance to isoniazid, rifampin, ethambutol, and pyrazinamide) isolated in 1998 from patients living in different parts of Germany and five susceptible strains isolated in 1998 and 1999 from patients living in Belgrade, Yugoslavia, were analyzed by gyrB PCR-restriction fragment length polymorphism (RFLP).
TABLE 1.
Selected discriminatory phenotypic and genetic characteristics of the strains analyzeda
| Organism and group (n) | Colony morphology (growth) | Growth in presence of TCH | Change of color of bromcresol medium | PZA sensitivity | Presence of oxyR mutation (G to A) | Spoligotype (characteristic features) |
|---|---|---|---|---|---|---|
| M. tuberculosis (n) | Eugonic | + | + | S | − | At least 1 of spacers 39–43 present |
| M. bovis | ||||||
| Subsp. bovis (5) | Dysgonic | − | − | R | + | Spacers 39–43 not present |
| Subsp. caprae (5) | Dysgonic | − | − | S | + | Spacers 39–43 and 3–16 not present |
| Subsp. C (2) | Dysgonic | − | − | S | + | Spacers 18–43 and 3–16 not present |
| M. africanum | ||||||
| Subtype I (5) | Dysgonic | − | − | S | − | At least 1 of spacers 33–36 and spacers 39–43 present |
| Subtype II (5) | Dysgonic | + | − | S | − | Spacers 33–36 not present and at least 1 of spacers 39–43 present |
| M. microtib | ||||||
| Subtype vole (1) | ND | ND | ND | ND | − | Only spacers 37 and 38 present |
| Subtype llama (2) | ND | ND | ND | S | − | Spacers 37, 38, 26, 24, 23, and 5–7 present |
S, susceptible; R, resistant; +, positive test result; −, negative test result; ND, not determined.
Biochemical tests of M. microti isolates could not be performed because of the limited growth on solid media.
Primary isolation and culturing of mycobacterial isolates were performed as described elsewhere (10). All isolates were identified as MTBC by using ACCUProbe gene probes (GenProbe, San Diego, Calif.).
Biochemical tests and susceptibility testing.
Biochemical analyses for differentiation included colony morphology, nitrate reduction on modified Dubos broth, the niacin accumulation test (INH-test strips; Difco, Detroit, Mich.), and growth in the presence of thiophen-2-carboxylic acid hydrazide (TCH; 1 μg/ml). Growth characteristics on Lebek medium and on bromcresol purple medium were determined as described previously (14). Drug susceptibility was determined by the proportion method on Löwenstein-Jensen medium according to the Deutsches Institut für Normung (DIN) guidelines and/or the modified proportion method in the BACTEC 460TB system according to the manufacturer's instructions.
PCR amplification conditions.
The primers MTUB-f and MTUB-r (9) were used for amplification of a 1,020-bp fragment of the gyrB gene. Three microliters of a sonicated and heat-inactivated bacterial suspension (13) was used for PCR. The 50-μl reaction mixture contained 10 mM Tris-HCl (pH 8.3), 50 mM KCl, 1.5 mM MgCl2, 200 μM (each) deoxynucleoside triphosphate (dNTP) (Boehringer, Mannheim, Germany), 20 pmol of each primer, and 1 U of Taq DNA polymerase (Gibco BRL, Eggenstein, Germany). PCR amplifications were performed in a PTC-100 thermocycler (MJ Research/Biozym, Hessisch Oldendorf, Germany) by the protocol described by Kasai et al. (9), except at an annealing temperature of 65°C.
DNA sequencing analysis.
Direct sequencing of the gyrB PCR fragments was performed by cycle sequencing with the BigDye RR Terminator Cycle Sequencing kit (Perkin-Elmer, Foster City, Calif.) and the ABI Prism 377 DNA sequencer (Perkin-Elmer) as instructed by the manufacturer. The PCR primers were used as sequencing primers too. The DNASIS program V2.1 (Hitachi, San Bruno, Calif.) was used for DNA sequence comparisons. DNA sequences were compared with the most-up-to-date version of the GenBank NR data bank by using the BLASTN algorithm (1).
PCR-RFLP analysis of the oxyR DNA polymorphism at position 285 and of the gyrB DNA polymorphisms.
The PCR-RFLP analysis of oxyR was performed according to Sreevatsan et al. (17). DNA polymorphisms in the 1,020-bp gyrB fragment amplified with the primer pair MTUB-f and MTUB-r were analyzed by restriction with RsaI, SacII, and TaqI in a volume of 10 μl, respectively, as instructed by the manufacturer (New England BioLabs, Schwalbach, Germany). The total reaction mixture was analyzed by 2% agarose gel electrophoresis in Tris-acetate buffer.
RESULTS AND DISCUSSION
Variations in the gyrB DNA sequence in a 1,020-bp region have been analyzed with a collection of MTBC isolates that had also been analyzed for their biochemical and other genetic characteristics in this study and (partially) in our previously published work (14). The most discriminatory characteristics are listed in Table 1. The strain collection comprises clinical isolates of M. tuberculosis, the PZA-resistant and -susceptible subspecies of M. bovis, M. africanum subtypes I and II, and M. microti types vole and llama and thus should be well suited for the evaluation of the discriminatory power of gyrB sequence polymorphisms for differentiation of the MTBC. The strains were assigned to the respective species according to their biochemical and genetic characteristics as listed in Table 1.
The primer pair MTUB-f and MTUB-r was used for amplification of a 1,020-bp fragment of the gyrB gene that comprises the four discriminative regions at positions 675, 756, 1,410, and 1,450. A PCR fragment of the correct size was obtained from all MTBC strains analyzed, but not from 78 validly described non-MTBC species (according to the Deutsche Sammlung von Mikroorganismen und Zellkulturen “Bacterial nomenclature up-to-date” [http://www.dsmz.de/bactnom/bactname.htm]) (data not shown). Hence, our data confirm that the primer pair MTUB-f and MTUB-r allows the MTBC-specific amplification of a part of the gyrB and may be also used for identification of MTBC isolates.
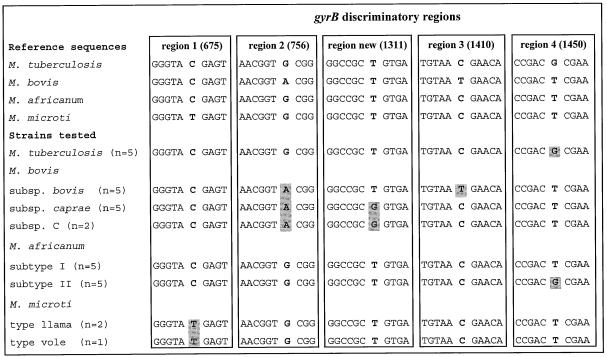
The DNA sequences of all fragments were determined and compared with each other and with the sequences stored in the International Nucleotide Sequence Database. Sequence polymorphisms were found at the four positions described previously (9) and additionally at position 1311 of the gyrB sequence (Fig. 1). In accordance with Kasai and coworkers (9), our data confirm that all M. bovis isolates could be identified by a G-to-A substitution at position 756 and that M. microti isolates of the vole and llama types can be differentiated from the other MTBC species by a single base substitution at position 675 (T instead of C). However, considering the other variable sites, the situation found here was more complex as described by Kasai et al. (9). At position 1410, only the PZA-resistant strains of M. bovis showed the C-to-T substitution proposed for differentiation of M. bovis. In contrast, the gyrB sequences of the PZA-susceptible M. bovis strains were C, as is found in all other isolates. However, the PZA-susceptible M. bovis isolates showed a characteristic and previously unknown T-to-G mutation at position 1311 representing a unique identification sequence for these subspecies. The data presented demonstrate that both PZA-resistant and PZA-susceptible subtypes of M. bovis can be differentiated from the other species by single base substitutions at position 756 of the gyrB gene and from each other by specific substitutions at position 1410 (PZA resistant) and position 1311 (PZA susceptible), respectively. Considering M. africanum and M. tuberculosis, only M. africanum subtype I isolates can be differentiated by a unique gyrB sequence. In contrast, M. tuberculosis and M. africanum subtype II isolates possessed an identical gyrB sequence that allows a differentiation of these two species from the other members of the MTBC by the T-to-G substitution at position 1450, but not from each other. These data confirm the close relationship between M. tuberculosis and M. africanum type II that is also expressed by their biochemical characteristics as described elsewhere (3, 6, 14). However, with the gyrB polymorphisms described here, we present the first molecular marker for differentiation of M. africanum type I from the other members of the MTBC.
FIG. 1.
DNA sequences of the four discriminatory regions in the gyrB gene described by Kasai et al. (9) and of one new region found in this study. Discriminatory base substitutions are shaded.
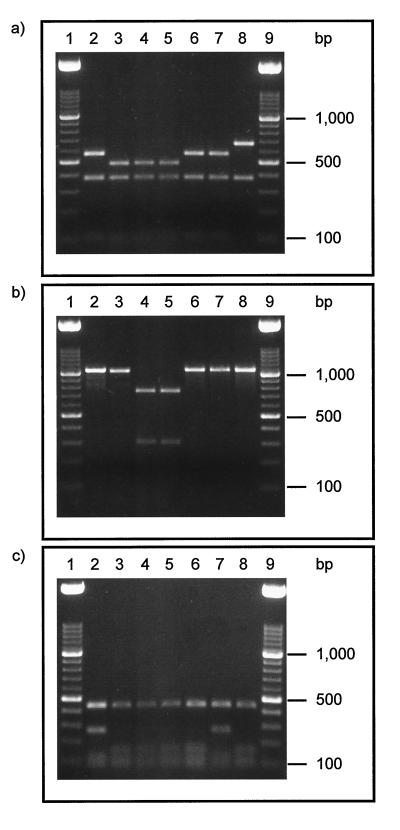
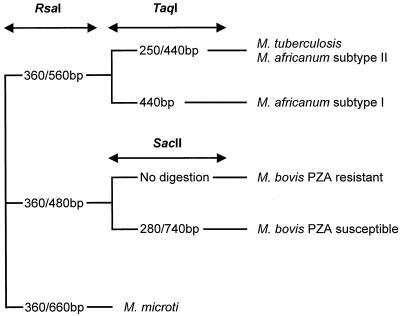
We also have evaluated a PCR-RFLP assay for rapid detection of the DNA sequence polymorphisms in the gyrB gene that can be used for differentiation of the MTBC species. As described by Kasai et al. (9), the restriction enzymes RsaI (targeting the polymorphisms at positions 675 and 756) and TaqI (targeting the polymorphism at position 1450) were used for digestion of the 1,020-bp PCR fragment. In addition, we used SacII to detect the substitution at position 1311 that is characteristic of PZA-susceptible M. bovis isolates. As shown in Fig. 2a, PZA-resistant and -susceptible isolates of M. bovis and M. microti could be identified by their specific RsaI RFLP patterns (360 and 480 bp for M. bovis, 360 and 660 bp for M. microti). The PZA-susceptible isolates of M. bovis could unambiguously be identified by showing two SacII restriction fragments, whereas the gyrB fragment of all other species remained uncleaved (Fig. 2b). M. africanum type I can be differentiated from M. tuberculosis and M. africanum type II by the characteristic TaqI RFLP pattern (Fig. 2c). Based on the clearly visible restriction fragments, a diagnostic algorithm was developed that allows an easy differentiation of the MTBC species (Fig. 3). To further confirm the differentiation system presented, reference strains M. tuberculosis H37Rv and M. bovis BCG as well as five drug-resistant M. tuberculosis strains from patients living in Germany and five susceptible strains isolated from patients living in Belgrade, Yugoslavia, were analyzed by the gyrB PCR-RFLP technique. All M. tuberculosis strains showed the typical M. tuberculosis-specific RsaI-TaqI RFLP patterns, just as M. bovis BCG showed RsaI-SacII RFLP patterns typical for PZA-resistant M. bovis isolates (data not shown).
FIG. 2.
RFLP patterns of PCR products obtained by RsaI digestion (a), SacII digestion (b), and TaqI (c) digestion of the 1,020-bp gyrB PCR fragment. Lanes: 1 and 9, 100-bp ladder; 2, M. tuberculosis; 3, M. bovis resistant to PZA; 4 and 5, M. bovis susceptible to PZA; 6, M. africanum subtype I; 7, M. africanum subtype II; 8, M. microti.
FIG. 3.
Diagnostic algorithm of RFLP patterns for the differentiation of members of the MTBC.
Thus, the gyrB PCR-RFLP using the combination of restriction enzymes presented in this study is a rapid and easy-to-use technique to discriminate between M. tuberculosis/M. africanum type II, M. africanum type I, M. microti, M. bovis, and the M. bovis subtypes. In contrast to the spoligotyping method and DNA sequencing of the gyrB gene, just PCR and easy-to-perform agarose gel electrophoresis are necessary for a highly discriminatory differentiation of the MTBC, making this technique feasible in a wide variety of laboratories.
In conclusion, the DNA sequence polymorphism in the gyrB gene represents a unique marker that facilitates the differentiation of the MTBC by DNA sequencing or a simple PCR-RFLP analysis. This technique complements the collection of molecular differentiation techniques and may be used in addition to other methods or alone, replacing the more time-consuming biochemical test. However, the differentiation of M. tuberculosis and M. africanum type II so far cannot be achieved by analysis of molecular markers and remains based on phenotypic characteristics, such as growth characteristics on bromcresol purple medium (14).
ACKNOWLEDGMENTS
We thank I. Radzio, F. Schaefer, B. Schlüter, and A. Zyzik, Borstel, Germany, for excellent technical assistance; G. Bretzel, Würzburg, Germany, for providing M. africanum isolates; and D. Vukovic, Belgrade, Yugoslavia, for providing M. tuberculosis isolates.
Parts of this work were supported by the Robert Koch-Institut, Berlin, Germany.
REFERENCES
- 1.Altschul S F, Madden T L, Schäffer A A, Zhang J, Zhang Z, Miller W, Lipman D J. Gapped BLAST and PSI-BLAST: a new generation of protein database search programs. Nucleic Acids Res. 1997;25:3389–3402. doi: 10.1093/nar/25.17.3389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Collins C H, Yates M D. A study of bovine strains of Mycobacterium tuberculosis isolated from humans in south-east England, 1977–1979. Tubercle. 1981;62:113–116. doi: 10.1016/0041-3879(81)90018-0. [DOI] [PubMed] [Google Scholar]
- 3.David H L, Jahan M T, Jumin A, Grandry J, Lehman E H. Numerical taxonomy analysis of Mycobacterium africanum. Int J Syst Bacteriol. 1978;28:464–472. [Google Scholar]
- 4.Feizabadi M M, Robertson I D, Cousins D V, Hampson D J. Genomic analysis of Mycobacterium bovis and other members of the Mycobacterium tuberculosis complex by isoenzyme analysis and pulsed-field gel electrophoresis. J Clin Microbiol. 1996;34:1136–1142. doi: 10.1128/jcm.34.5.1136-1142.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Frothingham R, Hills H G, Wilson K H. Extensive DNA sequence conservation throughout the Mycobacterium tuberculosis complex. J Clin Microbiol. 1994;32:1639–1643. doi: 10.1128/jcm.32.7.1639-1643.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haas W H, Bretzel G, Amthor B, Schilke K, Krommes G, Rüsch-Gerdes S, Sticht-Groh V, Bremer H J. Comparison of DNA fingerprint patterns of isolates of Mycobacterium africanum from East and West Africa. J Clin Microbiol. 1997;35:663–666. doi: 10.1128/jcm.35.3.663-666.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Imaeda T. Deoxyribonucleic acid relatedness among selected strains of Mycobacterium tuberculosis, Mycobacterium bovis, Mycobacterium bovis BCG, Mycobacterium microti, and Mycobacterium africanum. Int J Syst Bacteriol. 1985;35:147–150. [Google Scholar]
- 8.Kamerbeek J, Schouls L, Kolk A, van Agterveld M, van Soolingen D, Kuijper S, Bunschoten A, Molhuizen H, Shaw R, Goyal M, van Embden J. Simultaneous detection and strain differentiation of Mycobacterium tuberculosis for diagnosis and epidemiology. J Clin Microbiol. 1997;35:907–914. doi: 10.1128/jcm.35.4.907-914.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kasai H, Ezaki T, Harayama S. Differentiation of phylogenetically related slowly growing mycobacteria by their gyrB sequences. J Clin Microbiol. 2000;38:301–308. doi: 10.1128/jcm.38.1.301-308.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kent P T, Kubica G P. Public health mycobacteriology. A guide for the level III laboratory. U.S. Atlanta, Ga: Department of Health and Human Services, Centers for Disease Control and Prevention; 1985. [Google Scholar]
- 11.Kirschner P, Springer B, Vogel U, Meier A, Wrede A, Kiekenbeck M, Bange F-C, Böttger E C. Genotypic identification of mycobacteria by nucleic acid sequence determination: report of a 2-year experience in a clinical laboratory. J Clin Microbiol. 1993;31:2882–2889. doi: 10.1128/jcm.31.11.2882-2889.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liébana E, Aranaz A, Francis B, Cousins D. Assessment of genetic markers for species differentiation within the Mycobacterium tuberculosis complex. J Clin Microbiol. 1996;34:933–938. doi: 10.1128/jcm.34.4.933-938.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Niemann S, Richter E, Rüsch-Gerdes S. Stability of Mycobacterium tuberculosis IS6110 restriction fragment length polymorphism patterns and spoligotypes determined by analyzing serial isolates from patients with drug-resistant tuberculosis. J Clin Microbiol. 1999;37:409–412. doi: 10.1128/jcm.37.2.409-412.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Niemann S, Richter E, Rüsch-Gerdes S. Differentiation among members of the Mycobacterium tuberculosis complex by molecular and biochemical features: evidence for two pyrazinamide-susceptible subtypes of M. bovis. J Clin Microbiol. 2000;1:152–157. doi: 10.1128/jcm.38.1.152-157.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Scorpio A, Zhang Y. Mutations in pncA, a gene encoding pyrazinamidase/nicotinamidase, cause resistance to the antituberculous drug pyrazinamide in tubercle bacillus. Nat Med. 1996;2:662–667. doi: 10.1038/nm0696-662. [DOI] [PubMed] [Google Scholar]
- 16.Shinnick T M, Good R C. Mycobacterial taxonomy. Eur J Clin Microbiol Infect Dis. 1994;13:884–901. doi: 10.1007/BF02111489. [DOI] [PubMed] [Google Scholar]
- 17.Sreevatsan S, Escalante P, Pan X, Gillies II D A, Siddiqui S, Khalaf C N, Kreiswirth B N, Bifani P, Adams L G, Ficht T, Perumaalla V S, Cave M D, van Embden J D A, Musser J M. Identification of a polymorphic nucleotide in oxyR specific for Mycobacterium bovis. J Clin Microbiol. 1996;34:2007–2010. doi: 10.1128/jcm.34.8.2007-2010.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sreevatsan S, Pan X, Zhang Y, Kreiswirth B N, Musser J M. Mutations associated with pyrazinamide resistance in pncA of Mycobacterium tuberculosis complex organisms. Antimicrob Agents Chemother. 1997;41:636–640. doi: 10.1128/aac.41.3.636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Van Soolingen D, van der Zanden A G M, de Haas P E W, Noordhoek G T, Kiers A, Foudraine N A, Portaels F, Kolk A H, Kremer K, van Embden J D A. Diagnosis of Mycobacterium microti infections among humans by using novel genetic markers. J Clin Microbiol. 1998;36:1840–1845. doi: 10.1128/jcm.36.7.1840-1845.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wayne L G, Kubica G P. The mycobacteria. In: Sneath P H A, Holt J G, editors. Bergey's manual of systematic bacteriology. Vol. 2. Baltimore, Md: The Williams & Wilkins Co.; 1986. pp. 1435–1457. [Google Scholar]
- 21.Wayne L G, Good R C, Krichevsky M I, Blacklock Z, David H L, Dawson D, Gross W, Hawkins J, Levy-Frebault V V, McManus C, Portaels F, Rüsch-Gerdes S, Schröder K H, Silcox V A, Tsukamura M, van den Breen L, Yakrus M A. Fourth report of the cooperative, open-ended study of slowly growing mycobacteria by the International Working Group on Mycobacterial Taxonomy. Int J Syst Bacteriol. 1991;41:463–472. doi: 10.1099/00207713-41-4-463. [DOI] [PubMed] [Google Scholar]
- 22.World Health Organization. Report of the tuberculosis epidemic. Geneva, Switzerland: World Health Organization; 1996. [Google Scholar]