Abstract
To better understand trends in burn treatment patterns related to definitive closure, this study sought to benchmark real-world survey data with national data contained within the National Burn Repository version 8.0 (NBR v8.0) across key burn center practice patterns, resource utilization, and clinical outcomes. A survey, administered to a representative sample of U.S. burn surgeons, collected information across several domains: burn center characteristics, patient characteristics including number of patients and burn size and depth, aggregate number of procedures, resource use such as autograft procedure time and dressing changes, and costs. Survey findings were aggregated by key outcomes (number of procedures, costs) nationally and regionally. Aggregated burn center data were also compared to the NBR to identify trends relative to current treatment patterns. Benchmarking survey results against the NBR v8.0 demonstrated shifts in burn center patient mix, with more severe cases being seen in the inpatient setting and less severe burns moving to the outpatient setting. An overall reduction in the number of autograft procedures was observed compared to NBR v8.0, and time efficiencies improved as the intervention time per TBSA decreases as TBSA increases. Both nationally and regionally, an increase in costs was observed. The results suggest resource use estimates from NBR v8.0 may be higher than current practices, thus highlighting the importance of improved and timely NBR reporting and further research on burn center standard of care practices. This study demonstrates significant variations in burn center characteristics, practice patterns, and resource utilization, thus increasing our understanding of burn center operations and behavior.
Burn injuries comprise approximately 1.2% of nonfatal injuries among U.S. civilians, with nearly 489,000 burn patients seeking medical care through hospital emergency departments, and over 50,000 resulting in hospitalizations in 2017.1–3 Burns vary in terms of the size, location, depth of injury, and associated complications with resulting significant medical costs due to the need for highly individualized and specialized care. The economic burden in the United States has been estimated at over $976.6 million (2019 USD) in direct medical costs for both fatal and nonfatal burn injuries and over $1177 million (2019 USD) for lost work among nonfatal burn injuries.4,5
Effectively managing burns remains a challenge, given significant morbidity and mortality among burn patients.6 Recent statistics indicate that the number of burn fatalities has fallen significantly over time, and that patients with burns covering 90% of their bodies can now be effectively resuscitated and treated.7,8 As of 2018, 97% of all hospital burn admissions resulted in live discharges.2 Despite these high survival rates, burn patients may experience severe complications associated with the burn injury or adverse effects of treatment including pneumonia, cardiac arrhythmia, cellulitis, prolonged respiratory failure, wound infection, bacteremia, septicemia, incapacitation and serious functional limitations, disfigurement, pain, and psychological complications due to scarring, altered cosmesis, and poor wound healing.2,9 New burn care interventions may improve patient and economic outcomes by reducing infection rates, decreasing time to wound closure, reducing length of stay (LOS), reducing number of operations, and/or need for postburn rehabilitation. As new treatment modalities become available in each phase of burn care (wound assessment, excision and debridement, temporary closure, definitive closure, rehabilitation, and reintegration), practice patterns, protocols, and costs will likely shift over time.
Understanding the current treatment landscape in burn care is challenging given the complexity of care involved and a lag in the availability of timely data. Given the resource-intensive nature of burn care, value-based care is becoming increasingly important in the United States, driving health economic evaluation of new burn interventions.10 As new technologies become available, healthcare decision makers such as payers and hospital value analysis committees will need to assess the economic value, in addition to proven clinical outcomes, to understand the potential impact of these new treatment options. Real-world evidence (RWE) can be used to understand how burn care innovations affect practice patterns, resource utilization, and burn center costs. Data from real-world care settings provide insights into the way patients are being diagnosed, treated, and managed. Patient-level real-world data can be obtained from health insurance claims data, electronic medical records, hospital billing data, or from primary data collection methods such as registries, surveys, or time-in-motion studies, which can capture nuanced resource use information not typically available in large billing or claims databases. RWE is increasingly being used by healthcare stakeholders to drive decisions and has been recognized by the Food and Drug Administration for postmarket approval analysis of clinical outcomes.11
The American Burn Association (ABA) maintains the National Burn Repository (NBR), which captures real-world data from over 100 burn centers across the United States. NBR reports are published annually and provide insights into burn care trends such as patient demographics, type and severity of injury, LOS, and hospital charges. In 2019, the ABA created the latest research dataset, which encompasses data from 2009 to 2018 (NBR dataset version 14.0).2 Summary of NBR v14.0 provides insights at an aggregate level into the most frequently performed procedures, which include excision and autologous skin graft placement, but the detail of the number of procedures by TBSA burned, burn depth, or other patient characteristics is lacking. Although the NBR is a large repository of useful data from most U.S. burn centers, one of its potential limitations includes a time delay with respect to data analysis. The lag between accessing, publishing, and using NBR data for evidence-based decision making may delay insights on new interventions and constrain the utility of the NBR report for burn centers to benchmark performance that highlights the need for current real-world trend data. The NBR report also lacks data by region, hence it is not possible to discern regional differences in patient burden, resource use, or outcomes. In addition, the NBR captures charges but not costs, which require additional assumptions when trying to ascertain true burn center costs. Furthermore, charges can vary dramatically with the rate of device usage, labor costs, burn center location, and group purchasing organizations contracts. The NBR also lacks differences in key variables such as LOS and procedure trends by burn depths (full-thickness/mixed depth-thickness [FT], deep partial-thickness [DPT]). Given the recent approvals of new technologies in burn care since 2018 such as autologous skin cell suspension (approved September 2018) as an alternative to split-thickness skin graft as indicated, even the latest NBR data may pre-date shifts in resource use due to innovative technologies.
Real-world data-driven insights can improve understanding of the overall healthcare system, as well as ascertain regional health system variations, supporting more complete patient insights and informing resource allocation decisions in burn care, which are often highly individualized and complex. To best inform treatment decisions, it is crucial to understand present-day practice patterns and resource utilization trends at both the national and regional levels. To understand how the burn care landscape has changed since the NBR v8.0 (2002–2011) and the NBR v14.0 (2009–2018) data as published in the NBR 2019 report, a survey was conducted to collect nuanced, real-world data to identify shifts in burn care that affect the evaluation of novel interventions and to refine our understanding of the current standard of care (SOC) at both the national and regional levels.
METHODS
A benchmarking survey was developed by a team of healthcare economists and burn specialists and administered via a structured interview in-person or by telephone to 14 burn surgeons, representing a 10% convenience sample of U.S. burn centers nationally, across all five regions designated by the ABA (Northeast, Southern, Eastern Great Lakes [EGL], Midwest, and Western) between June and December 2019. The survey collected 73 data points across six domains: 1) burn center characteristics (eg, pediatric center, location, number of beds, teaching status); 2) patient characteristics (eg, total patients undergoing excision and autografting, distribution of patients across burn depths, total body surface area [TBSA], and age groups); 3) procedure trends by TBSA burned (eg, number of autograft procedures, total blood transfused across burn depths); 4) burn center perspective costs, excluding profession fees (eg, bed cost per day, cost of anesthesiology per patient, cost of burn surgery operating room [OR] time per hour); 5) resource use (eg, surgery time at graft and donor sites by burn depth and TBSA burned, LOS for contracture procedure, dressing changes per day, time for each dressing change); and 6) demographic details such as patient mix and age distribution for low TBSA burns (TBSA burned ≤20%). See Supplementary Data for additional information. In addition to capturing burn center average trends, the questionnaire also collected information on care practices and patient outcomes for TBSA burns less than 20%, which account for over 90% of all burns according to NBR v14.0 data, to provide detailed information on practice patterns associated with the treatment of low TBSA burn patients, which is currently lacking in the literature. Burn centers were selected to ensure representativeness across geography, and data were collected from a single burn center surgeon at each site who was experienced with clinical outcomes, hospital charges at their respective institutions, resource utilization, and local value assessment procedures.
Data were reviewed, validated, and synthesized by entering all collected information into an MS Excel file. Once the data were combined, summaries were developed and compared using descriptive statistics based on mean values for all quantitative responses. A comprehensive review of all data was conducted to confirm no data entry errors occurred. Comparisons of key survey outcomes such as number of procedures and costs were made across burn center characteristics (ie, region, number of beds) to understand variations in regional treatment patterns and outcomes from the national averages. Aggregated burn center survey data were also compared to the NBR to identify the differences between NBR version 8.0 and current burn center treatment patterns.12,13 In a publication by Kowal et al,12 detailed analyses of NBR 8.0 were conducted and published, reporting results by TBSA and burn depth which allowed for direct comparisons of resource use to the survey results. Although the NBR 2019 annual report reports rolling 10-year trends, we were not able to compare benchmarking survey results directly to NBR v14.0 through the NBR 2019 annual report because the report publishes data trends in aggregate, and thus evaluation of trends by TBSA burned and burn depth could not be made.
As the study was not interventional, the authors did not seek direct patient data and therefore did not recruit or enroll any human subjects. Data collected from burn centers did not include individually identifiable health information, and therefore, there were no risks and no anticipated medical benefits to patients associated with this study. Hence, an exemption was obtained from the Western Institutional Review Board to conduct the survey.
RESULTS
National and Regional Benchmarking Survey Results
A total of 14 burn centers participated in the survey, representing about a 10% sample of all U.S. burn centers (n = 132). Burn centers were distributed across all five ABA regions: Northeast (4), Southern (5), EGL (2), Midwest (1), and Western (2). For the purposes of this analysis, responses for EGL and Midwest region burn centers were clustered together to maintain anonymity of individual burn center data. Among responders, 50% of burn centers are university centers, 79% are designated as urban teaching hospitals. The majority of centers (79%) treat both adults and pediatric patients. Over 85% of the burn centers had 25 or fewer designated beds (average: 18 beds; Table 1).
Table 1.
Burn center characteristics
| National | Northeast Region | Southern Region | EGL + Midwest Region | Western Region | |
|---|---|---|---|---|---|
| Total number of burn centers (n) | 14 | 4 | 5 | 3 | 2 |
| Pediatric designation | 35.7% | 25.0% | 40.0% | 33.3% | 50.0% |
| Patient type | |||||
| Adults and pediatrics | 78.6% | 75.0% | 80.0% | 66.7% | 100.0% |
| Adults only | 21.4% | 25.0% | 20.0% | 33.3% | 0.0% |
| Burn center type | |||||
| Public | 35.7% | 50.0% | 0.0% | 66.7% | 50.0% |
| Private | 14.3% | 25.0% | 0.0% | 0.0% | 50.0% |
| University | 50.0% | 25.0% | 100.0% | 33.3% | 0.0% |
| Number of beds (mean) | 17.7 | 13.3 | 20.0 | 13.0 | 28.0 |
| Size of burn center (number of beds) | |||||
| <25 | 85.7% | 100.0% | 80.0% | 100.0% | 50.0% |
| 25–49 | 14.3% | 0.0% | 20.0% | 0.0% | 50.0% |
| Burn center teaching status | |||||
| Urban teaching | 78.6% | 50.0% | 80.0% | 100.0% | 100.0% |
| Rural | 7.1% | 25.0% | 0.0% | 0.0% | 0.0% |
| Urban nonteaching | 14.3% | 25.0% | 20.0% | 0.0% | 0.0% |
EGL, Eastern Great Lakes.
On average, burn centers treated 341 patients annually (range: 70–1000; median 241). In 2019, the most common burns treated were superficial partial-thickness (SPT) burns (41.5%), followed by FT/mixed-thickness burns (30.2%) and DPT burns (28.3%). This trend was similar for a subset of patients with low TBSA burns (42.4%, 29.9%, and 27.6% for SPT, FT, and DPT burns, respectively). These distributions varied geographically, with Northeast and Western burn centers seeing over 50% of patients with SPT burns, followed by DPT and FT (Table 2). The age distribution in FT/DPT burns shows that over 80% of FT and DPT burn patients were adults (Table 2).
Table 2.
Burn center patient mix
| Characteristic | National | Northeast Region | Southern Region | EGL + Midwest Region | Western Region |
|---|---|---|---|---|---|
| Average number of patients treated each year in an inpatient setting | 341.2 | 460.8 | 301.8 | 125.0 | 525.0 |
| Distribution of patients across burn depths: all patients | |||||
| FT/mixed | 30.2% | 20.6% | 33.8% | 44.0% | 20.0% |
| DPT | 28.3% | 29.0% | 29.8% | 24.3% | 29.0% |
| SPT | 41.5% | 50.4% | 36.4% | 31.7% | 51.0% |
| Distribution of patients across burn depths: patients with TBSA burned ≤20% | |||||
| FT/mixed | 29.9% | 21.8% | 35.5% | 37.3% | 21.0% |
| DPT | 27.6% | 29.0% | 31.7% | 18.3% | 28.5% |
| SPT | 42.4% | 49.2% | 32.6% | 44.3% | 50.5% |
| Age distribution of FT/mixed and DPT patients: all patients | |||||
| 0–6 years | 8.3% | 5.1% | 10.1% | 4.7% | 16.0% |
| 7–20 years | 10.9% | 11.0% | 11.8% | 11.3% | 8.0% |
| 21 years or older | 80.7% | 83.8% | 78.1% | 84.0% | 76.0% |
| Age distribution of FT/mixed and DPT patients: patients with TBSA burned ≤20% | |||||
| 0–6 years | 10.2% | 8.8% | 13.0% | 4.7% | 14.5% |
| 7–20 years | 12.0% | 9.8% | 13.4% | 12.0% | 13.0% |
| 21 years or older | 77.7% | 81.3% | 73.6% | 83.3% | 72.5% |
| Distribution of patients across TBSA burned: FT/mixed-depth burns only | |||||
| TBSA burned >40% | 15.4% | 13.2% | 14.9% | 18.0% | 17.5% |
| TBSA burned 21–40% | 32.0% | 32.5% | 28.4% | 43.0% | 23.5% |
| TBSA burned 10–20% | 52.5% | 54.3% | 56.6% | 39.0% | 59.0% |
| Distribution of patients across TBSA burned: DPT burns only | |||||
| TBSA burned >40% | 8.5% | 10.2% | 8.8% | 9.0% | 4.0% |
| TBSA burned 21–40% | 26.3% | 30.0% | 19.6% | 32.0% | 27.0% |
| TBSA burned 10–20% | 65.1% | 59.8% | 71.6% | 58.7% | 69.0% |
EGL, Eastern Great Lakes; FT, full thickness; DPT, deep partial thickness; SPT, superficial partial thickness; TBSA, total body surface area.
Autograft operations are the SOC for definitive closure of burn wounds in the United States. A key objective of the survey was to understand how the number of autograft operations varied by burn depth and TBSA burned. Table 3 displays the distribution of autograft procedures by burn depth and TBSA burned. In both DPT and FT burns, the average number of autograft procedures per 10% TBSA burned decreased as the size of the burn increased. For large burns (TBSA burned ≥40%), the average number of autograft procedures per 10% TBSA burned was 0.75 in DPT burns and 0.95 in FT burns. The Northeast region burn centers tended to trend higher, estimating 1.03 and 1.22 autograft procedures per 10% TBSA burned in DPT and FT, respectively. For small burns (TBSA burned ≤10%), the average number of autograft procedures was similar in both DPT and FT burns (1.17 and 1.20, respectively). A review of the average surgical time, defined as the time the surgeon was actively harvesting donor site skin or applying skin to the graft site, by TBSA burned (minutes per TBSA burned) for the donor site and graft site shows that as the burn size increases, the average time per TBSA burned decreases. Detailed surgical time estimates by site, burn depth, and TBSA burned are given in Table 3. Similar trends were reported for dressing time—as TBSA burned increased, the minutes per TBSA burned to perform dressing changes decreased. There was no difference in the number of dressing changes needed per day by TBSA burned.
Table 3.
Resource use and procedure trends
| Characteristic | National | Northeast Region | Southern Region | EGL + Midwest Region | Western Region |
|---|---|---|---|---|---|
| Mean (SD) | |||||
| Average number of autograft procedures: FT/mixed-depth burns only | |||||
| TBSA burned 10% | 1.20 (0.41) | 1.25 (0.29) | 1.07 (0.11) | 1.00 (0.00) | 1.73 (1.03) |
| TBSA burned 20% | 1.97 (0.78) | 2.50 (0.41) | 1.60 (0.88) | 1.50 (0.50) | 2.57 (0.81) |
| TBSA burned 30% | 2.78 (1.03) | 3.38 (0.48) | 1.98 (1.18) | 2.92 (0.88) | 3.42 (0.59) |
| TBSA burned 40% | 3.81 (1.96) | 4.88 (1.31) | 2.46 (1.49) | 4.33 (3.21) | 4.27 (0.38) |
| Total ml of blood transfused by % TBSA burned: FT/mixed-depth burns only (ml/TBSA%) | |||||
| TBSA burned 10% | 30.57 (52.41) | 70.75 (73.55) | 6.83 (11.84) | 0.00 (0.00) | 16.40 (23.19) |
| TBSA burned 20% | 42.57 (42.56) | 51.88 (21.47) | 20.17 (20.00) | 75.00 (106.07) | 25.15 (10.82) |
| Average number of autograft procedures: DPT burns only | |||||
| TBSA burned 10% | 1.17 (0.35) | 1.25 (0.29) | 1.04 (0.08) | 1.00 (0.00) | 1.62 (0.87) |
| TBSA burned 20% | 1.82 (0.79) | 2.50 (0.41) | 1.40 (0.73) | 1.00 (0.00) | 2.35 (0.49) |
| TBSA burned 30% | 2.42 (1.04) | 3.25 (0.50) | 1.67 (1.16) | 2.00 (0.00) | 3.08 (0.11) |
| TBSA burned 40% | 3.00 (1.48) | 4.13 (1.31) | 2.16 (1.51) | 2.00 (0.00) | 3.82 (0.26) |
| Total ml of blood transfused by % TBSA burned: DPT burns only (ml/TBSA%) | |||||
| TBSA burned 10% | 30.57 (52.41) | 70.75 (73.55) | 6.83 (11.84) | 0.00 (0.00) | 16.40 (23.19) |
| TBSA burned 20% | 53.82 (85.44) | 45.31 (32.89) | 20.17 (20.00) | 150.00 (212.13) | 25.15 (10.82) |
| Average total surgical time for the graft site: FT/mixed-depth burns only (minutes/surgical TBSA burned%) | |||||
| TBSA burned 10% | 6.10 (3.41) | 7.95 (5.28) | 5.27 (2.61) | 5.08 (1.01) | 6.00 (4.24) |
| TBSA burned 20% | 5.21 (1.99) | 6.45 (2.95) | 4.73 (1.59) | 4.83 (1.04) | 4.50 (2.12) |
| TBSA burned 30% | 4.51 (1.89) | 5.50 (2.65) | 4.07 (1.32) | 4.08 (1.88) | 4.25 (2.47) |
| TBSA burned 40% | 4.20 (1.82) | 5.13 (2.66) | 3.87 (1.24) | 3.96 (2.06) | 3.50 (1.41) |
| Average total surgical time for the donor site: FT/mixed depth burns only (minutes/surgical TBSA burned%) | |||||
| TBSA burned 10% | 3.04 (2.29) | 2.10 (0.64) | 5.37 (2.34) | 1.75 (0.75) | 1.00 (0.00) |
| TBSA burned 20% | 2.70 (1.82) | 1.65 (0.37) | 4.83 (1.15) | 1.67 (0.76) | 1.00 (0.00) |
| TBSA burned 30% | 2.33 (1.51) | 1.38 (0.48) | 4.17 (0.38) | 1.42 (0.95) | 1.00 (0.00) |
| TBSA burned 40% | 2.22 (1.44) | 1.28 (0.59) | 3.97 (0.06) | 1.38 (0.99) | 1.00 (0.00) |
| Average total surgical time for the graft site: DPT burns only (minutes/surgical TBSA burned%) | |||||
| TBSA burned 10% | 5.78 (3.33) | 6.83 (5.46) | 5.27 (2.61) | 5.08 (1.01) | 6.00 (4.24) |
| TBSA burned 20% | 4.89 (1.67) | 5.33 (2.47) | 4.73 (1.59) | 4.83 (1.04) | 4.50 (2.12) |
| TBSA burned 30% | 4.19 (1.39) | 4.38 (1.25) | 4.07 (1.32) | 4.08 (1.88) | 4.25 (2.47) |
| TBSA burned 40% | 3.87 (1.19) | 4.00 (0.71) | 3.87 (1.24) | 3.96 (2.06) | 3.50 (1.41) |
| Average total surgical time for the donor site: DPT burns only (minutes/surgical TBSA burned%) | |||||
| TBSA burned 10% | 2.93 (2.40) | 1.73 (1.25) | 5.37 (2.34) | 1.75 (0.75) | 1.00 (0.00) |
| TBSA burned 20% | 2.61 (1.92) | 1.35 (0.93) | 4.83 (1.15) | 1.67 (0.76) | 1.00 (0.00) |
| TBSA burned 30% | 2.26 (1.60) | 1.13 (0.85) | 4.17 (0.38) | 1.42 (0.95) | 1.00 (0.00) |
| TBSA burned 40% | 2.16 (1.52) | 1.06 (0.88) | 3.97 (0.06) | 1.38 (0.99) | 1.00 (0.00) |
| Average LOS for contracture procedures: FT/mixed-depth burns only (days) | |||||
| TBSA burned 10% | 1.82 (1.72) | 0.67 (0.58) | 3.00 (2.16) | 1.33 (1.53) | 2.00 (0.00) |
| TBSA burned 20% | 2.00 (1.61) | 1.00 (1.00) | 3.00 (2.16) | 1.67 (1.15) | 2.00 (0.00) |
| TBSA burned 30% | 2.18 (1.72) | 1.67 (2.08) | 3.00 (2.16) | 1.67 (1.15) | 2.00 (0.00) |
| TBSA burned 40% | 2.32 (1.93) | 2.17 (2.93) | 3.00 (2.16) | 1.67 (1.15) | 2.00 (0.00) |
| Average LOS for contracture procedures: DPT burns only (days) | |||||
| TBSA burned 10% | 1.67 (1.72) | 0.50 (0.58) | 3.00 (2.16) | 1.33 (1.53) | 2.00 (0.00) |
| TBSA burned 20% | 1.83 (1.64) | 0.75 (0.96) | 3.00 (2.16) | 1.67 (1.15) | 2.00 (0.00) |
| TBSA burned 30% | 2.00 (1.76) | 1.25 (1.89) | 3.00 (2.16) | 1.67 (1.15) | 2.00 (0.00) |
| TBSA burned 40% | 2.13 (1.96) | 1.63 (2.63) | 3.00 (2.16) | 1.67 (1.15) | 2.00 (0.00) |
| Dressing changes per day: all patients | 0.98 (0.45) | 0.93 (0.54) | 0.85 (0.34) | 1.10 (0.69) | 1.25 (0.35) |
| Dressing changes per day: patients with TBSA burned ≤20% | 0.98 (0.45) | 0.93 (0.54) | 0.85 (0.34) | 1.10 (0.69) | 1.25 (0.35) |
| Average time for each dressing change: all patients (minutes/TBSA burned%) | |||||
| TBSA burned 10% | 2.57 (0.65) | 2.75 (0.50) | 2.60 (0.55) | 2.00 (1.00) | 3.00 (0.00) |
| TBSA burned 20% | 2.41 (0.68) | 2.75 (0.50) | 2.30 (0.67) | 2.00 (1.00) | 2.63 (0.53) |
| TBSA burned 30% | 2.39 (0.68) | 2.75 (0.50) | 2.30 (0.67) | 2.00 (1.00) | 2.50 (0.71) |
| TBSA burned 40% | 2.24 (0.67) | 2.25 (0.61) | 2.30 (0.67) | 2.00 (1.00) | 2.44 (0.79) |
EGL, Eastern Great Lakes; FT, full thickness; DPT, deep partial thickness; SPT, superficial partial thickness; TBSA, total body surface area; LOS, length of stay.
Burn center perspective costs were captured for all burn centers. Detailed costs are given in Table 4. Respondents were able to obtain burn center costs through a review of administrative records at their respective burn centers. The average bed cost per day for all patients was $8362 (median: $7220), and for patients with TBSA burned ≤20% only, the average bed cost per day decreased to $7554 (median: $6500). When considering regional trends, the average cost per day ranged from $14,050 to $6234. It is important to note that institutional variations in which items are included in the reported daily cost such as room and board, nursing or personnel, and management of patient morbidity may account for some portion of the regional cost differences. Operating room time and anesthesiology costs represent significant portions of burn care resources used. The cost of anesthesiology per patient for the inpatient stay was $5186 per patient for all patients and decreased to $4704 for patients with TBSA burned ≤20%, whereas the mean hourly operating room time was $4844 across all patients. Regionally, the average OR hourly cost remained in the $4000 range, with the exception of one region which had an average OR cost of $7139.
Table 4.
Burn center perspective costs (USD 2019)
| Characteristic | National | Northeast Region | Southern Region | EGL + Midwest Region | Western Region |
|---|---|---|---|---|---|
| Mean (SD) | |||||
| Average bed cost per day: all patients | $8362 ($5078) | $7815 ($8117) | $6234 ($1809) | $8664 ($3542) | $14,050 ($7142) |
| Average bed cost per day: patients with TBSA burned ≤20% | $7554 ($5179) | $6620 ($7151) | $5347 ($2727) | $7835 ($3689) | $14,050 ($7142) |
| Cost of anesthesiology per patient: all patients | $5187 ($5860) | $2939 ($86) | $3824 ($1749) | $12,124 ($13,336) | $3222 ($747) |
| Cost of anesthesiology per patient: patients with TBSA burned ≤20% | |||||
| FT/mixed burns | $4706 ($4322) | $2565 ($615) | $4156 ($2386) | $9430 ($9525) | $3222 ($747) |
| DPT burns | $4703 ($4324) | $2552 ($634) | $4156 ($2386) | $9430 ($9525) | $3222 ($747) |
| Cost of burn surgery operating room time per hour: all patients | $4844 ($2349) | $4347 ($2002) | $4230 ($809) | $7139 ($5146) | $4200 ($00) |
EGL, Eastern Great Lakes; FT, full thickness; DPT, deep partial thickness; SPT, superficial partial thickness; TBSA, total body surface area.
Evaluation of Trends in Burn Care
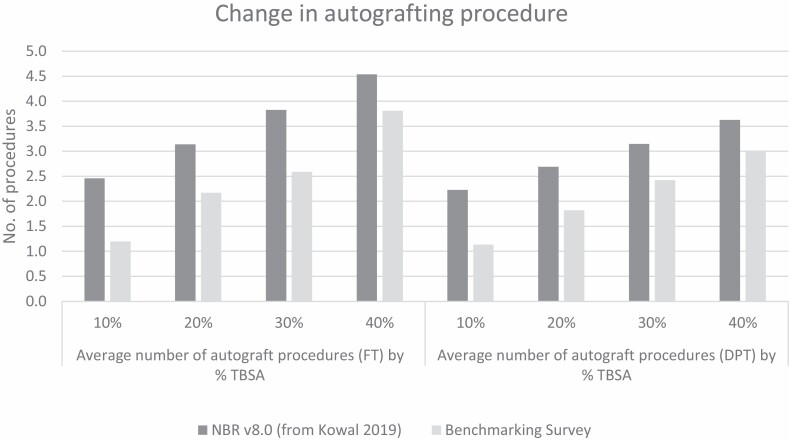
Evaluation of current data relative to previously published data provides insights into shifts in treatment patterns and cost trends. Comparison of the benchmarking survey data for number of autografting procedures for DPT and FT/mixed burn depths to the published estimates derived from the NBR v8.0 shows 49% and 51% decreases, respectively, in the number of procedures required for TBSA burned 10%, and 31% and 32% decreases, respectively, in the number of procedures required for TBSA burned 20% (Figure 1). A recent analysis of the NBR v8.0 data reported the average number of autograft procedures to be between 2.3 for TBSA burned 10% and 4.0 for TBSA burned 40%, confirming a downward shift in the number of procedures reported in the benchmarking survey.13
Figure 1.
Change in autografting procedures.
As part of the BEACON model development, Kowal et al12 published burn center costs and resource use estimates from 2017. Analysis of costs for all patients showed significant increases since 2017. The largest cost difference is in the anesthesiology cost per patient, which is 83.6% higher in the survey data compared to the cost reported in Kowal et al: $2825 vs $5187 (all costs were inflated to 2019 USD for consistency in comparison). Average bed cost per day increased from $7125 to $8362 (17.4%), and OR hourly cost increased from $3900 to $4844 (24.2%). When only considering costs for low TBSA burned patients only (TBSA burned ≤20%), average cost per day and anesthesiology costs were about 10% lower than the average cost for all patients (Table 4).
When evaluating trends over time, survey results were compared to the work of Kowal et al, given the detailed analysis conducted across TBSA burned categories and burn depths. The benchmarking survey results show a decrease in the SPT and DPT burns and an increase in FT burns treated inpatient when compared to Kowal et al (51.0% vs 41.5% SPT burns; 29.0% vs 28.3% DPT burns; 20.0% vs 30.2% FT/mixed-depth burns).12 This is consistent with anecdotal burn surgeon experience, which shows that burn centers are admitting the more serious burns and shifting SPT burns to outpatient care when possible. Kowal reports an average autograft time of 1.6 minutes per TBSA burned for the graft site and 2.1 minutes per TBSA burned for the donor site, both of which are lower than the low-end estimate of 4.12 and 2.24 minutes, respectively (irrespective of TBSA burned or wound depth), from the benchmarking survey. This difference could reflect a true change in procedure time estimates or may be a result of variation due to the sample size of the Kowal et al burn survey (n = 8) compared to the current benchmarking survey.12
DISCUSSION
Burn center directors increasingly rely on RWE, available health economics tools such as the BEACON model,12 and NBR data available for inpatient burn care2 to benchmark burn center performance, track patient outcomes, and inform value analysis committee evaluations. As new burn technologies become available, burn centers can assess their potential impact on high-cost resources such as OR time and LOS relative to national or regional benchmarks. Therefore, an understanding of the nuanced relationships between patient characteristics, healthcare resource use, treatment patterns, and how inpatient costs across patient types of the individual center compare to both national and regional benchmarks can provide valuable insights. The benchmarking survey aggregates the current estimates of burn center patient mix and resource use at both the national and regional levels and provides a contemporary view of real-world resource utilization and costs.
When paired with previously published resources, trends emerge which can be used by burn center administrators for future resource planning. In terms of patient mix, the benchmarking survey shows that there is an overall increase in the proportion of severe burns being treated in the inpatient setting, with more low-TBSA burns and/or superficial burns moving to outpatient care. When drilling down to a regional level, variations in the patient mix are noticeable, with the Northeast and Western regions seeing more of the smaller burns and the plurality of patients treated inpatient in the EGL + Midwest regions are treated for FT burns. Burn surgeons indicate that changes in admission or operative patterns could also be attributed to the shrinking burn workforce and developments in telemedicine.
Changes in overall resources related to the number of autografting procedures and surgical time have also been observed at both the national and regional levels. There is an overall reduction in the number of autografting procedures per percent TBSA burned. A closer look at the average surgical time for both the graft and donor sites shows that the procedure time per TBSA burned decreases as TBSA burned increases. This could be reflective of the fixed portion of time needed for all OR procedures, such as anesthesia induction and preparation time (time from the end of anesthesia to the start of procedure) and exit (the time from procedure end to when the patient leaves the OR) and turnover time. Even procedures that are shorter in duration for smaller burns have to account for these fixed components which could be attributed to operating room efficiencies associated with larger burns.14 Nonetheless, despite these efficiencies found with larger burns, surgeons report spending more time per TBSA burned for both graft and donor sites. The additional time per TBSA burned could be attributed to the increased severity of burns being treated in the inpatient setting as treatment of less severe burns migrates to the outpatient setting. Compared to the 2017 costs reported by Kowal et al, all costs have increased notably, with the largest increase seen in anesthesiology costs per patient followed by OR costs. Finally, the benchmarking survey identifies wide regional differences in surgical time for donor sites. However, the reasons underpinning the regional differences are beyond the scope of the survey, and thus, further research would be needed to understand why these regional differences exist.
This real-world benchmarking survey moves beyond the level of detail captured in current NBR trend reports to understand burn center patient mix and associated treatment resources by TBSA burned and burn depth, both of which are important predictors of the intensity of burn care resource use. However, there are certain limitations inherent in the methods, including some of the data reported may be subject to the respondent’s own anecdotal experience rather than comprehensive empirical data. This may be true when estimating time per TBSA burned for procedures as this data is not explicitly captured in hospital or patient records. The study is also limited by the small number of participants involved, although it was felt to be a valid representation given the number of burn centers across the United States. Finally, trend comparisons were made to the NBR 8.0 dataset (as published in the work of Kowal et al) because the procedure trends were reported by both burn depth and TBSA. Additional analysis of the most recent NBR v14.0 could provide additional insights into how resource use trends have changed since NBR v8.0. Given the learnings of this initial benchmarking survey exercise, future studies can build on this research by gathering data from a larger sample of U.S. burn centers or by conducting an analysis of hospital electronic records to estimate real-world resource utilization and hospital costs. Additionally, enhanced NBR data collection and reporting could provide the burn community with timely benchmarks across resource use and costs. Given that detailed patient data are already captured as part of the NBR dataset, the NBR annual reports could potentially be modified and expanded to provide a more nuanced look at resource use, patient outcomes, and costs by TBSA and burn depth at both the national and regional levels to understand local medical practice patterns. Additionally, the NBR can potentially be enhanced to capture additional data elements such as type of intervention used, time in OR, and number of ICU days which would allow a more practical look at treatment patterns. As new interventions become available, collection and reporting of detailed resource use consumption and costs will allow burn centers and payers to quantify and understand the potential health economic impact of new interventions over time.
When considering the current costs and practice patterns from a sample of US burn centers, we observed a variety of trends that reflect changes in patient mix and practice patterns. This study benchmarks national and regional averages for number of procedures, duration of procedures, and costs. It is observed that the number of autografting procedures is trending downward, which could lead to significant offsets in costly resource use such as OR time and anesthesiology. Additionally, the results suggest that the number of autograft procedures for both FT and DPT burns estimated from NBR version 8.0 may be higher than current practices. This highlights the importance of improved and timely NBR reporting and further research on burn center SOC practices to adequately assess the value of current treatment options, in order to adequately assess the comparative value of new burn care interventions as they become available. Viewing resource utilization and outcomes alongside the full continuum of care has the potential to improve population health through empirical decision support so that patients get the right care, at the right place, and the right time for the best outcome.
Supplementary Material
ACKNOWLEDGEMENTS
We would like to thank the following burn centers for their contributions to this study: Arizona Burn Center at Valleywise Health Medical Center, Phoenix, AZ; Connecticut Burn Center at Bridgeport Hospital, Bridgeport, CT; Lehigh Valley Health Network Regional Burn Center, Allentown, PA; Maine Medical Center, Portland, ME; MedStar Washington Hospital Center, Washington, DC; MetroHealth Burn Care Center, Cleveland, OH; N.C. Jaycee Burn Center, Chapel Hill, NC; Richard M. Fairbanks Burn Center at Eskenazi Health, Indianapolis, IN; UMC Timothy J. Harnar Regional Burn Center, Lubbock, TX; UMC NO Burn Center, New Orleans, LA; University of California San Francisco Fresno, Fresno, CA; University of Missouri Health Care, Columbia, MO; University of Tennessee Health Science Center: Firefighters Regional Burn Center, Memphis, TN; Wake Forest Baptist Medical Center Burn Center, Winston-Salem, NC.
Conflict of Interest and Source of Funding: This study was sponsored by Avita Medical, Valencia, CA. IQVIA received funding from Avita Medical to assist with survey development, data analyses, and manuscript preparation. C.P.F., S.K., and P.V. are employees of IQVIA, Inc., which provides consulting and other research services to biopharmaceutical companies. J.S. and T.W. are employees and shareholders of Avita Medical. J.E.C. is a consultant with SpectralMD, Inc. and Avita Medical, Ltd. Considering the association with Avita Medical, in lieu of compensation, donations are made to a local 501(c)(3) charity supporting local burn prevention, outreach, education, and survivor programs. J.E.C. is a stockholder of Permeaderm Inc. and SpectralMD Inc. and has research supported by Spirit of Charity Foundation Burn Research Fund. H.A. is a consultant for Avita Medical and has received honoraria for consulting services. D.C., J.A.G., S.J. have no conflicts to declare. K.N.F. is the PI for research on studies sponsored by the American Burn Association (ABRUPT), Atox-Bio, BARDA, Polynovo Biomaterials, Mallinckrodt, and Mediwound and is a consultant and former PI for Baxter. K.N.F. is a consultant for Integra. W.L.H. is a consultant with Avita Medical, Vericel, and Avadim Health, Inc. and is a stockholder of PermeaDerm. J.H.H. disclosures include equity positions in Abbott Labs, AbbVie, Change Healthcare, and Imbed Biosciences and is a consultant for Mallinckrodt and Avita Medical. A.K. is an advisor to Avita Medical. N.K. is a consultant with Integra and an advisor for Avita Medical. J.S.L. has received honoraria for consulting services provided to Avita and PolarityTE. A.S. is an advisor for Avita Medical and Exsurco. J.W.S. provides consulting for Avita Medical, Kerecis, and Integra. Commercial Grants/Contracts paid to Institution (NOT individual) for research by Avita Medical, Kerecis, Aceso, Mallinckrodt Pharmaceuticals, MediWound, and SpectralMD. R.S. is an advisor to Avita Medical, Smith and Nephew, and Vericel.
REFERENCES
- 1. Rui P, Kang K. National hospital ambulatory medical care survey: 2017 emergency department summary tables. National Center for Health Statistics; 2017. https://www.cdc.gov/nchs/data/nhamcs/web_tables/2017_ed_web_tables-508.pdf; accessed 17 March 2020. [Google Scholar]
- 2. American Burn Association. National burn repository 2019 report. Dataset version 14.0. Chicago, IL, 2019. [Google Scholar]
- 3. Centers for Disease Control and Prevention National Center for Injury Prevention and Control. Web-based injury statistics query and reporting system (WISQARS). 2020. www.cdc.gov/injury/wisqars; accessed 17 March 2020.
- 4. Centers for Disease Control and Prevention National Center for Injury Prevention and Control. Estimated number of nonfatal emergency department visits, and average and total lifetime costs, united states. 2010. https://wisqars.cdc.gov:8443/costT/cost_Part1_Intro.jsp; accessed 17 March 2020.
- 5. Centers for Disease Control and Prevention National Center for Injury Prevention and Control. Number of deaths and estimated average and total lifetime costs, united states, 2010. 2010. https://wisqars.cdc.gov:8443/costT/cost_Part1_Intro.jsp; accessed 17 March 2020.
- 6. Hranjec T, Turrentine FE, Stukenborg G, Young JS, Sawyer RG, Calland JF. Burn-center quality improvement: are burn outcomes dependent on admitting facilities and is there a volume-outcome “sweet-spot”? Am Surg 2012;78:559–66. [PMC free article] [PubMed] [Google Scholar]
- 7. Klein MB, Goverman J, Hayden DLet al. ; Inflammation and Host Response to Injury, and Large-Scale Collaborative Research Program . Benchmarking outcomes in the critically injured burn patient. Ann Surg 2014;259:833–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. National Institutes for Health. Burns. https://www.nigms.nih.gov/education/fact-sheets/Pages/burns.aspx; accessed 17 March 2020.
- 9. Kauvar DS, Cancio LC, Wolf SEet al. Comparison of combat and non-combat burns from ongoing US military operations. J Surg Res 2006;132:195–200. [DOI] [PubMed] [Google Scholar]
- 10. Padula WV, Sculpher MJ. Ideas about resourcing health care in the United States: can economic evaluation achieve meaningful use? Ann Intern Med 2021;174:80–5.. [DOI] [PubMed] [Google Scholar]
- 11. US Food and Drug Administration. Framework for FDA’s real-world evidence program. Silver Spring (MD): US Food and Drug Administration; 2018. [Google Scholar]
- 12. Kowal S, Kruger E, Bilir Pet al. Cost-effectiveness of the use of autologous cell harvesting device compared to standard of care for treatment of severe burns in the United States. Adv Ther 2019;36:1715–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kruger E, Kowal S, Bilir SP, Han E, Foster K. Relationship between patient characteristics and number of procedures as well as length of stay for patients surviving severe burn injuries: analysis of the American Burn Association National Burn Repository. J Burn Care Res 2020;41:1037–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Madni TD, Imran JB, Clark AT, Arnoldo BA, Phelan HA, Wolf SE. Analysis of operating room efficiency in a burn center. J Burn Care Res 2018;39:89–93. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.