Abstract
Background
Vitamin B12 deficiency is an easily treatable cause of reversible dementia. It is likely to be more common in Indian population due to traditionally vegetarian culture. This study was conducted to estimate the prevalence of Vitamin B12 deficiency in elderly patients (>60 years) with dementia attending outpatient department.
Methods
This study was conducted in two phases. The first phase was a cross sectional observational study to estimate the prevalence of Vitamin B12 deficiency in the elderly population with dementia. The second phase was a pilot study done in subjects with Vitamin B12 deficiency to assess the change in cognition following Vitamin B12 supplementation.
Results
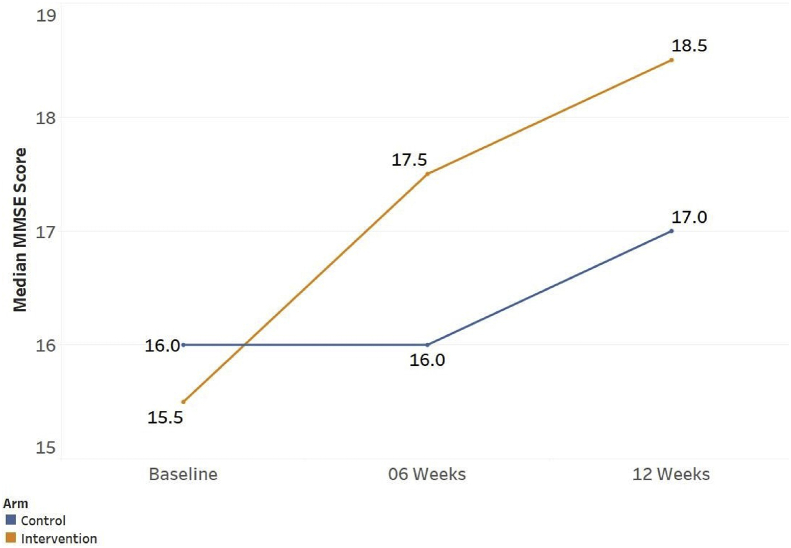
Out of 2920 study eligible subjects, 200 were diagnosed as dementia with Mini Mental Status Examination (MMSE) score of ≤ 24. Vitamin B12 deficiency was seen in 7.5% of patients. Vitamin B12 deficiency was associated with shorter and more severe dementia. Macrocytosis was more common in Vitamin B12 deficiency (p value < 0.001) where as vegetarian diet did not show significant correlation (p value 0.69). There was significant improvement in the median MMSE score in the intervention group with increase in MMSE by 2 points at 6-8 weeks and 3 points at 12 weeks (p value 0.009 and 0.003 by Mann Whitney test).
Conclusion
Prevalence of Vitamin B12 deficiency in dementia was 7.5%. It was associated with macrocytosis, shorter duration and more severe dementia. There was a significant improvement in median MMSE score at 6 weeks and 12 weeks following Vitamin B12 supplementation.
keywords: Alzheimer's disease, Cognitive decline, Dementia, Mini mental status examination, Vitamin B12 deficiency
Introduction
Dementia is a chronic and persistent disorder marked by cognitive decline, personality changes, impaired reasoning and executive functions. The prevalence of dementia rises with increasing age and reaches 20–40% in population above 85 years of age.1 By current demographic projections, the geriatric population in India will double and surpass the paediatric population in next 30 years. By 2050, dementia will pose a major challenge in the health care for the elderly.2 Dementia is usually progressive and irreversible, but reversible causes of dementia are also known. Hence, early identification of reversible and precipitating factors causing dementia is important to stop the progression and if possible to reverse cognitive decline. Vitamin B12 deficiency is an easily treatable cause of reversible dementia. India being a traditionally vegetarian society, Vitamin B12 deficiency is likely to be more common than in the Western countries. Literature on the prevalence of Vitamin B12 deficiency with dementia in Indian population is sparse. Moreover, the literature available till now on response to Vitamin B12 supplementation in these patients is contradictory with few old studies showing beneficial response, whereas majority of recent studies show no significant cognitive improvement. This study was conducted to estimate the prevalence of Vitamin B12 deficiency in elderly patients (>60 years) with dementia, attending outpatient department (OPD). The primary objective of the study was to assess the prevalence of Vitamin B12 deficiency in dementia patients. Secondary objective was to study the clinical presentation, laboratory correlates, diet of the patients of dementia with Vitamin B12 deficiency and also assess the effect of Vitamin B12 supplementation on cognitive function in these patients if any.
Materials and methods
The study was conducted at an OPD of a zonal hospital in North India between October 2013 and December 2015. This study was conducted in two phases. The first phase was a cross-sectional observational study to estimate the prevalence of Vitamin B12 deficiency in the elderly population with dementia. The second phase was a pilot study in which participants identified with Vitamin B12 deficiency were divided to either receive parenteral methylcobalamin or not to receive methylcobalamin. These patients were followed up and closely monitored and re-assessed at 6–8 weeks and 12 weeks for change in cognition using repeat mini mental status examination (MMSE) score.
Inclusion criteria were elderly patients, 60 years and above, educated to at least middle school and diagnosed with dementia by Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM IV), with MMSE score of less than 24. Exclusion criteria included patients who had delirium at presentation, history of taking parenteral/high dose oral (>1000 μg day) Vitamin B12 supplementation in previous one year, acute alcohol intoxication/withdrawal or history of blood transfusions in past 6 months. The study subjects were selected by a systematic random sampling at the registration desk of different OPDs. After assessing the eligibility criteria and taking consent, all the patients were screened for cognitive impairment by mini-cog questionnaire by a trained paramedic. Patients with mini-cog score 3 or less were administered MMSE (English version). Patients with MMSE score of less than 24 were diagnosed as dementia patients and were included in the study. A detailed history was taken from the caregivers of the patients. Further, the participants were subjected to a detailed clinical examination, non-contrast computed tomography of the brain and investigations which included complete blood count, mean corpuscular volume (MCV), peripheral blood smear (PBS), ELISA for HIV, venereal disease research laboratory (VDRL) test, thyroid stimulating hormone and Vitamin B12 estimation. Vitamin B12 estimation was done by ELISA-based assay. The prevalence of Vitamin B12 deficiency in patients with dementia was estimated.
The second phase was a pilot study done on patients with dementia and Vitamin B12 deficiency. Patients of dementia with Vitamin B12 deficiency were divided to either receive injectable methylcobalamin or not. Injectable methylcobalamin was given in the dose of 500 μg intramuscularly once a day for 7 days followed by every week for next 12 weeks. Both the groups were closely followed and monitored for 12 weeks with cognitive assessment at 6–8 weeks and then again at 12 weeks by a repeat MMSE score. During follow-up both groups were closely monitored for any neurological or cognitive worsening. The sample size was estimated to be 197 based on estimated OPD load of geriatric patients of approximately 13,000 and expected prevalence of dementia being 3.5%.3 Hypothesised prevalence of Vitamin B12 deficiency in dementia patients was around 7% with absolute difference of 3% at 95% confidence level and then adding 10% for non-responders. Approval of Institutional Ethics Committee was taken prior to the start of the study.
Results
A total of 2920 elderly OPD patients >60 years of age were eligible and were included for screening with mini-cog questionnaire. Out of these, 231 were found to have mini-cog score of equal to or less than 3. Out of these 231 patients 200 were found to have MMSE score of less than 24 and were included in the study. Median MMSE score was 18 with 80% of subjects having MMSE score of 20 or less. Average age of the patients was 71.3 years with 62% males and 38% females.
The prevalence of Vitamin B12 deficiency (Vitamin B12 levels < 200 pg/dl) in dementia patients was found to be 7.5% (15/200). Commonest cause of dementia was probable Alzheimer's disease (AD) in 35.5% followed by vascular dementia in 29% and Parkinson-related dementia (PRD) in 15.5%. The mean duration of symptoms of dementia was 39.92 months with shortest duration (25.13 months) in patients of dementia with Vitamin B12 deficiency and longest (50.04 months) in PRD. The difference in the duration of symptoms across various causes of dementia was statistically significant (p = <0.001).
Pallor, skin darkening and glossitis were more common in the patients with B12 deficiency, and ataxia was more common in patients with vascular dementia and dementia with lewy bodies (DLB). Neuropsychiatric manifestations were more common in patients with Vitamin B12 deficiency and DLB.
Around 22.5% of dementia patients had borderline Vitamin B12 levels between 200 and 300 pg/dl. The mean age of this group was 71.26 years and MMSE score was 18.08. MCV values in patients with borderline Vitamin B12 levels were significantly high (p = 0.014).
A total of 15 patients of dementia had Vitamin B12 deficiency. The mean age of these patients was 70.93 years and mean MMSE score was 16.13. Details of baseline characteristics of dementia patients with Vitamin B12 deficiency are shown in Table 1. Macrocytosis was significantly more in the patients with Vitamin B12 deficiency as seen in 8 out of 15 patients with Vitamin B12 deficiency as compared to 1 out of 185 patients with normal Vitamin B12 levels (p = <0.001). Vegetarian diet was not significantly associated with Vitamin B12 levels as 10 out of 15 patients with Vitamin B12 deficiency were vegetarian as compared to 80 out of 185 patients with normal Vitamin B12 levels being vegetarian (p = 0.69). Of the 15 dementia patients with Vitamin B12 deficiency, 8 were randomised into the intervention arm and 7 into control arm. There was no significant difference in median age, gender, baseline MMSE score in both the groups (Table 2). There was significant improvement in the median MMSE score in patients receiving methylcobalamin with increase in MMSE score by 2 points at 6–8 weeks and 3 points at 12 weeks (p = 0.009 and 0.003 respectively by Mann–Whitney test). There was no significant improvement in the cognitive status of patients of dementia with B12 deficiency not receiving methylcobalamin (Table 3 and Fig. 1).
Table 1.
Baseline characteristics and clinical profile of participants with dementia due to Vitamin B12 deficiency.
| Variables (n = 15) | Values |
|---|---|
| Mean Age (yrs) | 70.93 |
| Mean MMSE (Score) | 16.13 |
| Mean Duration of Dementia (Months) | 25.13 |
| Mean Haemoglobin (gm%) | 11.40 |
| Mean Corpuscular Volume (fl) | 92.93 |
Table 2.
Comparison of baseline characteristics in intervention and control group.
| Intervention group (n = 8) | Control group (n = 7) | p value | |
|---|---|---|---|
| Median Age (IQR) | 68.50 (63.0, 75.0) | 74.00 (66.5, 77.0) | 0.64a |
| Gender – Male % | 5 (62.5%) | 4 (57.1%) | 0.99b |
| Median MMSE (IQR) | 15.50 (14.0, 16.30) | 16.00 (14.5, 19.5) | 0.38a |
IQR: Interquartile range.
Mann–Whitney U Test.
Fisher extract test.
Table 3.
Median change in MMSE score in intervention and control groupa.
| Intervention group (n = 8) | Control group (n = 7) | P value | |
|---|---|---|---|
| Median increase in MMSE score at 6–8 weeks (IQR) | 2.0 (1.00,3.00) | 0.0 (−0.5, 0.5) | 0.009 |
| Median increase in MMSE score at 12 weeks (IQR) | 3.0 (2.75, 4.25) | 1.0 (0.5, 1.0) | 0.002 |
Mann Whitney U Test.
Fig. 1.
Median change in MMSE in intervention and control group.
Discussion
The prevalence of Vitamin B12 deficiency in dementia patients in our study was 7.5%. The prevalence of Vitamin B12 deficiency in dementia in various international studies varies from 9% to 25%.4,5 In a study by Tripathi et al., the prevalence of B12 deficiency in dementia patients was 7.2%.6 This is consistent with our study. However another Indian study done by Chahal et al. in northwestern India showed the prevalence of Vitamin B12 deficiency in Indian adult population to be much higher, upto 50%.7
In our study, we found that Vitamin B12 deficiency was associated with a shorter duration of dementia, lower MMSE score and macrocytosis. In a study done in South India, 80% of the patients with B12 deficiency had macrocytosis.8 In other studies, dementia associated with Vitamin B12 deficiency was of shorter duration.9,10 These studies however found no association of Vitamin B12 deficiency with more severe dementia. This may be due to the fact that our patients presented at an advanced stage of disease as evidenced by the duration of symptoms being more than 12 months. In our study, 22.5% of the dementia patients had borderline Vitamin B12 levels between 200 and 300 pg/dl. In a recent study done by Mizrahi et al. borderline Vitamin B12 levels <350 pg/dl were found to predict cognitive decline in patients with hip fracture.11 In patients with borderline Vitamin B12 levels, assessment of serum homocysteine and methylmalonic acid (MMA) levels remains a sensitive marker of functional Vitamin B12 deficiency.12, 13, 14 Recent studies have also shown that low and subnormal Vitamin B12 levels may be an independent factor for progression to AD, and supplementation of Vitamin B12 in these patients may halt the progression of dementia.15,16
Various studies on the response to Vitamin B12 replacement on the cognition and neuropsychiatric manifestations in dementia patients with Vitamin B12 deficiency have shown conflicting results. Some older studies have shown improved cognition with Vitamin B12 replacement. This was more marked in the patients with symptoms of less than 12 months duration.17,18 There are a number of recent meta-analyses and trials which have shown that there is no significant improvement in cognitive functions with Vitamin B12 replacement in dementia patients with Vitamin B12 deficiency although there may be improvement in neuropsychiatric manifestations, frontal lobe functions, duration of delirium and normalisation of serum homocysteine and MMA levels.4,19, 20, 21, 22, 23 In our study, there was a significant improvement in the median MMSE score in the intervention group with increase in MMSE at 6–8 weeks and 12 weeks. This may suggest that Vitamin B12 supplementation in dementia patients with Vitamin B12 deficiency may be beneficial. Limitations of our study are that it is a single-center experience and the sample size of the dementia patients with Vitamin B12 deficiency is less. Moreover, the follow-up period of dementia patients with Vitamin B12 deficiency is very short. Another limitation was that MMA and homocysteine levels were not estimated which may have helped to detect functional Vitamin B12 deficiency.
Further studies to estimate prevalence of Vitamin B12 deficiency in patients with dementia can be conducted to find the geographical variation, if any, and also study the impact of Vitamin B12 supplementation on improvement of cognition of these patients.
Conclusion
Our study estimated the prevalence of Vitamin B12 deficiency in elderly patients with dementia to be 7.5%. Macrocytosis, shorter duration and more severe dementia were associated with Vitamin B12 deficiency. In our small pilot study it was noted that with parenteral Vitamin B12 supplementation, there was improvement in median MMSE score of 2 points at 6 weeks and 3 points at 12 weeks although no definite conclusion can be made as the sample size was very small. Multicentric study with a larger sample size is required to assess the impact of Vitamin B12 supplementation in elderly dementia patients with Vitamin B12 deficiency.
Disclosure of competing interest
The authors have none to declare.
Acknowledgement
This paper is based on Armed Forces Medical Research Committee Project No. 4501/2014 granted and funded by the office of the Directorate General Armed Forces Medical Services and Defence Research Development Organization, Government of India.
References
- 1.Seeley William W., Miller Bruce L. 20th ed. McGraw Hills Education; New York: 2018. Harrison's Principles of Internal Medicine; pp. 3108–3314. Chapter 423: Alzheimer’s Disease. [Google Scholar]
- 2.Sathianathan R., Kantipudi S.J. The dementia epidemic: impact, prevention, and challenges for India. Indian J Psychiatry. 2018;60(2):165–167. doi: 10.4103/psychiatry.IndianJPsychiatry_261_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shaji S., Promodu K., Abraham T., Roy K.J., Verghese A. An epidemiological study of dementia in a rural community in Kerala, India. Br J Psychiatr J Ment Sci. 1996;168(6):745–749. doi: 10.1192/bjp.168.6.745. [DOI] [PubMed] [Google Scholar]
- 4.Eastley R., Wilcock G.K., Bucks R.S. vitamin B12 deficiency in dementia and cognitive impairment: the effects of treatment on neuropsychological function. Int J Geriatr Psychiatr. 2000;15(3):226–233. doi: 10.1002/(sici)1099-1166(200003)15:3<226::aid-gps98>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 5.Clarke R., Grimley Evans J., Schneede J., et al. vitamin B12 and folate deficiency in later life. Age Ageing. 2004;33(1):34–41. doi: 10.1093/ageing/afg109. [DOI] [PubMed] [Google Scholar]
- 6.Tripathi M., Sheshadri S., Padma M.V., Jain S., Meheshwari M.C., Behari M. Serum cobalamin levels in dementias. Neurol India. 2001;49(3):284–286. [PubMed] [Google Scholar]
- 7.Chahal J., Raina S., Sharma K., Kaur N. How common is vitamin B12 deficiency - a report on deficiency among healthy adults from a medical college in rural area of North-West India. Int J Nutr Pharmacol Neurol Dis. 2014;4(4):241–245. [Google Scholar]
- 8.Aaron S., Kumar S., Vijayan J., Jacob J., Alexander M., Gnanamuthu C. Clinical and laboratory features and response to treatment in patients presenting with vitamin B12 deficiency-related neurological syndromes. Neurol India. 2005;53(1):55–58. doi: 10.4103/0028-3886.15057. discussion 9. [DOI] [PubMed] [Google Scholar]
- 9.Srikanth S., Nagaraja A.V. A prospective study of reversible dementias: frequency, causes, clinical profile and results of treatment. Neurol India. 2005;53(3):291–294. doi: 10.4103/0028-3886.16926. discussion 4-6. [DOI] [PubMed] [Google Scholar]
- 10.Larson E.B., Reifler B.V., Sumi S.M., Canfield C.G., Chinn N.M. Features of potentially reversible dementia in elderly outpatients. West J Med. 1986;145(4):488–492. [PMC free article] [PubMed] [Google Scholar]
- 11.Mizrahi E.H., Lubart E., Leibovitz A. Low borderline levels of serum vitamin B12 may predict cognitive decline in elderly hip fracture patients. Isr Med Assoc J. 2017;19(5):305–308. [PubMed] [Google Scholar]
- 12.Hathcock J.N., Troendle G.J. Oral cobalamin for treatment of pernicious anemia? Jama. 1991;265(1):96–97. [PubMed] [Google Scholar]
- 13.Metz J., McGrath K., Bennett M., Hyland K., Bottiglieri T. Biochemical indices of vitamin B12 nutrition in pregnant patients with subnormal serum vitamin B12 levels. Am J Hematol. 1995;48(4):251–255. doi: 10.1002/ajh.2830480409. [DOI] [PubMed] [Google Scholar]
- 14.Savage D.G., Lindenbaum J., Stabler S.P., Allen R.H. Sensitivity of serum methylmalonic acid and total homocysteine determinations for diagnosing cobalamin and folate deficiencies. Am J Med. 1994;96(3):239–246. doi: 10.1016/0002-9343(94)90149-x. [DOI] [PubMed] [Google Scholar]
- 15.Chen H., Liu S., Ji L., et al. Associations between Alzheimer's disease and blood homocysteine, vitamin B12, and folate: a case-control study. Curr Alzheimer Res. 2015;12(1):88–94. doi: 10.2174/1567205012666141218144035. [DOI] [PubMed] [Google Scholar]
- 16.Shen L., Ji H.F. Associations between homocysteine, folic acid, vitamin B12 and alzheimer's disease: insights from meta-analyses. J Alzheim Dis. 2015;46(3):777–790. doi: 10.3233/JAD-150140. [DOI] [PubMed] [Google Scholar]
- 17.Abyad A. Prevalence of vitamin B12 deficiency among demented patients and cognitive recovery with cobalamin replacement. J Nutr Health Aging. 2002;6(4):254–260. [PubMed] [Google Scholar]
- 18.Larson E.B., Reifler B.V., Featherstone H.J., English D.R. Dementia in elderly outpatients: a prospective study. Ann Intern Med. 1984;100(3):417–423. doi: 10.7326/0003-4819-100-3-417. [DOI] [PubMed] [Google Scholar]
- 19.Malouf R., Areosa Sastre A. vitamin B12 for cognition. Cochrane Database Syst Rev. 2003;(3) doi: 10.1002/14651858.CD004326. [DOI] [PubMed] [Google Scholar]
- 20.van Dyck C.H., Lyness J.M., Rohrbaugh R.M., Siegal A.P. Cognitive and psychiatric effects of vitamin B12 replacement in dementia with low serum B12 levels: a nursing home study. Int Psychogeriatr. 2009;21(1):138–147. doi: 10.1017/S1041610208007904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.vitamin B12 and cognitive function: an evidence-based analysis. Ontario Health Technol Assess Ser. 2013;13(23):1–45. [PMC free article] [PubMed] [Google Scholar]
- 22.Vogel T., Dali-Youcef N., Kaltenbach G., Andres E. Homocysteine, vitamin B12, folate and cognitive functions: a systematic and critical review of the literature. Int J Clin Pract. 2009;63(7):1061–1067. doi: 10.1111/j.1742-1241.2009.02026.x. [DOI] [PubMed] [Google Scholar]
- 23.Kwok T., Lee J., Lam L., Woo J. vitamin B(12) supplementation did not improve cognition but reduced delirium in demented patients with vitamin B(12) deficiency. Arch Gerontol Geriatr. 2008;46(3):273–282. doi: 10.1016/j.archger.2007.05.001. [DOI] [PubMed] [Google Scholar]