Abstract
The performance of the Etest for itraconazole susceptibility testing of 50 isolates of filamentous fungi was assessed in comparison with the National Committee for Clinical Laboratory Standards (NCCLS) proposed standard microdilution broth method. The NCCLS method employed RPMI 1640 broth medium, and MICs were read after incubation for 48 h at 35°C. Etest MICs were determined with RPMI agar containing 2% glucose and with Casitone agar and were read after incubation for 24 h (Aspergillus spp. and Rhizopus spp.) and 48 h (all species except Rhizopus spp.) at 35°C. The isolates included Aspergillus flavus, Aspergillus fumigatus, Aspergillus niger, Aspergillus terreus, Fusarium spp., Pseudallescheria boydii, Rhizopus spp., Paecilomyces variotii, and an Acremonium sp. Overall agreement between Etest and microdilution MICs was 96% with RPMI agar and 80% with Casitone agar. The agreement was 100% for all species except Rhizopus spp. (83%) and Paecilomyces varioti (0%) with RPMI agar. When Casitone agar was used, the agreement ranged from 50% with Rhizopus spp. to 100% with Fusarium spp., P. boydii, P. varioti, and an Acremonium sp. Notably, for Aspergillus spp., the agreement between itraconazole Etest MICs read at 24 h and reference microdilution MICs read at 48 h was 100% with both RPMI and Casitone agar. Both media supported the growth of all filamentous fungi tested. Where a discrepancy was observed between Etest and the reference method, the Etest MIC was generally higher. The Etest method using RPMI agar appears to be a useful method for determining itraconazole susceptibilities of Aspergillus spp. and other filamentous fungi.
Testing of susceptibility to antifungal agents has now been standardized for yeasts, and additional efforts to develop more user-friendly testing methods for use in the clinical laboratory have been successful (2, 10, 13). Efforts to adapt the National Committee for Clinical Laboratory Standards (NCCLS) M27-A broth microdilution methodology to testing of molds have also been successful (3, 5, 6, 11). A recent multicenter study documented excellent reproducibility of the microdilution method for testing amphotericin B, ketoconazole, and itraconazole against molds in 11 laboratories (5). A reference method for broth dilution antifungal agent susceptibility testing of filamentous fungi has been proposed by the NCCLS (M38-P) (11). As with yeasts, there is a need to validate alternative approaches for testing of molds.
The Etest stable gradient MIC method (AB BIODISK, Solna, Sweden) has proven to be a remarkably flexible means of performing MIC testing for a wide variety of microbial pathogens and antimicrobial agents (1, 8, 9). In addition to the testing of routine and fastidious bacteria (9), the Etest has proven to be useful in testing yeasts (4, 12, 14, 15, 19). To our knowledge there have been only two published reports describing the adaptation of the Etest for antifungal agent susceptibility testing of molds. Szekely et al. (18) showed that the Etest was a suitable alternative to broth microdilution for testing the susceptibility of molds to amphotericin B and itraconazole. Johnson et al. (7) demonstrated differences in amphotericin B MICs among isolates of Aspergillus spp. using the Etest but failed to find a close clinical correlation with these results in a murine model of aspergillosis. The present report describes the use of the Etest to determine the in vitro susceptibility of 50 clinical mold isolates to a clinically useful antifungal agent, itraconazole. The itraconazole MIC results determined by the Etest using two different agar media are compared to MICs determined by the NCCLS proposed reference microdilution method, NCCLS M38-P (11).
MATERIALS AND METHODS
Test isolates.
A total of 50 isolates were tested. These included clinical isolates of Aspergillus flavus (10 isolates), Aspergillus fumigatus (12 isolates), Aspergillus niger (1 isolate), Aspergillus terreus (1 isolate), Fusarium oxysporum (5 isolates), Fusarium solani (5 isolates), other Fusarium spp. (3 isolates), Pseudallescheria boydii (5 isolates), Rhizopus spp. (6 isolates), Paecilomyces variotii (1 isolate) and an Acremonium sp. (1 isolate). The isolates came from the culture collection of the University of Iowa and were stored on slants or in water suspension at ambient temperature until used in the study. Prior to use in the study isolates were passaged at least twice on potato dextrose agar (Remel, Lenexa, Kans.) to ensure viability and adequate sporulation.
Etest method.
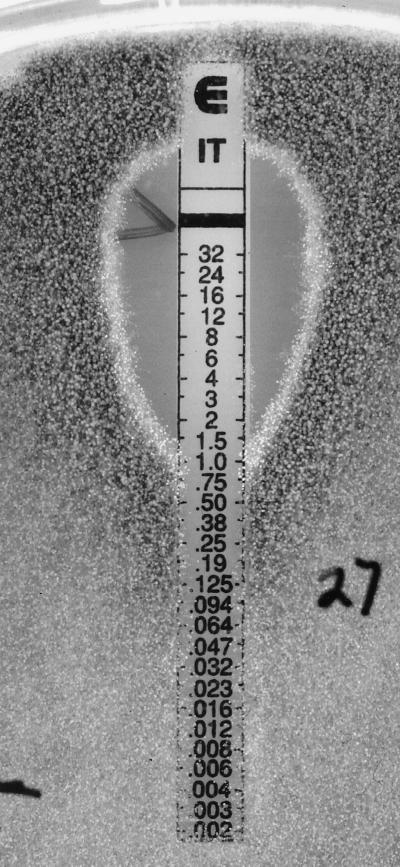
The Etest was performed in accordance with the manufacturer's instructions. Isolates were grown on potato dextrose agar slants (Remel) at 35°C for seven days to ensure adequate sporulation. Spore suspensions were prepared in sterile saline and adjusted to a concentration of 106 spores/ml, corresponding to 68 to 82% transmittance at 530 nm (14). Agar formulations used for the Etest were RPMI 1640 (American Biorganics, Buffalo, N.Y.) supplemented with 1.5% agar and 2% glucose and buffered to pH 7.0 with 0.165 M morpholinepropanesulfonic acid (MOPS) buffer (Sigma, St. Louis, Mo.) and Casitone agar (Difco). The 90-mm-diameter plates contained RPMI or Casitone agar at a depth of 4.0 mm. The plates were inoculated by dipping a sterile swab into the cell suspension and streaking it across the surface of the agar in three directions. The plates were dried at ambient temperature for 15 min before applying the itraconazole Etest strips. The plates were incubated at 35°C and read at 24 (Aspergillus spp. and Rhizopus spp.) and 48 h (all species except Rhizopus spp.). The Etest MIC was read as the drug concentration at the point where dense colonial growth intersected the strip, ignoring sparse subsurface hyphae at the margins (Fig. 1). Microcolonies within the ellipse were ignored.
FIG. 1.
Itraconazole (IT) Etest reading pattern for A. flavus. A clear ellipse on RPMI agar is shown; the MIC is 1.0 μg/ml. The numbers on the scale correspond to the itraconazole concentrations on the strip (in micrograms per milliliter).
Reference broth microdilution method.
The broth microdilution method was performed according to NCCLS proposed guidelines (11) and as described by Espinel-Ingroff et al. (5, 6). Itraconazole was obtained from Janssen Research Foundation (Beerse, Belgium). Stock solutions were prepared in 100% dimethyl sulfoxide (Sigma), diluted to 100 times the final concentrations in dimethyl sulfide, further diluted in RPMI 1640 medium buffered to pH 7.0 with MOPS buffer, and dispensed into 96-well microdilution trays. Trays containing a 0.1-ml aliquot of itraconazole solution (two times the final concentration) in each well were subjected to quality control (QC) and then sealed and stored at −70°C until use in the study. The final concentration of itraconazole in the wells ranged from 0.007 to 8.0 μg/ml. The stock conidial suspension (106 spores/ml) was diluted to a final inoculum concentration of 0.4 × 104 to 5 × 104 CFU/ml and dispensed into the microdilution wells. The inoculated microdilution trays were incubated at 35°C and read at 24 (Rhizopus spp.) and 48 h (all other species). The MIC endpoint for itraconazole was defined as the lowest concentration that produced prominent inhibition of growth (approximately 50% inhibition) relative to the drug-free growth control (11).
QC.
QC was performed in accordance with NCCLS guidelines (11) and as recommended by Espinel-Ingroff et al. (6) using Candida krusei ATCC 6258 (MIC range, 0.12 to 0.5 μg/ml), Candida parapsilosis (MIC range, 0.06 to 0.25 μg/ml), and P. variotii ATCC 22319 (MIC range, 0.03 to 1.0 μg/ml).
Analysis of results.
Etest MICs read at 48 h on the two media were compared to reference microdilution MICs read at 48 h. Due to rapid growth on agar, Etest results for Rhizopus spp. were read at 18 to 24 h. Etest results for Aspergillus spp. were read at both 24 and 48 h. The reference microdilution MICs and Etest MICs were determined in two physically separate laboratories and were read independently; i.e., the testing was blinded. Since the Etest scale has a continuous gradient of concentrations, the MICs in between twofold dilutions were rounded to the next twofold level of the reference method for comparison (14, 15, 18). Off-scale MICs at the upper limit were converted to the next-higher concentration, and off-scale results at the lower end were left unchanged. Discrepancies between MICs of no more than 2 dilutions were used to calculate the percent agreement.
RESULTS AND DISCUSSION
Table 1 summarizes the in vitro susceptibilities of 50 clinical mold isolates to itraconazole as determined by the reference microdilution method. The data are presented as MIC ranges and, where appropriate, as the drug concentrations necessary to inhibit 50 and 90% of the isolates of each species. A broad range of MICs was observed. In general, itraconazole MICs obtained were similar to those reported previously for the individual fungal species (16, 18). In each batch of microdilution tests, the MICs of itraconazole for the three QC strains were within the accepted limits (11).
TABLE 1.
In vitro susceptibility of clinical mold isolates to itraconazole as determined by the reference microdilution broth methoda
| Species (no. of isolates) | MIC (μg/ml)c
|
||
|---|---|---|---|
| Range | 50% | 90% | |
| Fusarium spp.b (13) | >8.0 | >8.0 | >8.0 |
| P. boydii (5) | 0.5–1.0 | 1.0 | |
| Rhizopus spp. (6) | 1.0–>8.0 | 2.0 | |
| A. flavus (10) | 0.25–1.0 | 0.25 | 1.0 |
| A. fumigatus (12) | 0.5–1.0 | 1.0 | 1.0 |
| A. niger (1) | 0.5 | ||
| A. terreus (1) | 0.5 | ||
| P. variotii (1) | 4.0 | ||
| Acremonium sp. (1) | 1.0 | ||
Reference microdilution method MICs read at 48 h of incubation (NCCLS, M38-P).
Includes F. solani (five isolates), F. oxysporum (five isolates) and three isolates of Fusarium spp. (not further identified).
50% and 90%, MICs at which 50 and 90% of isolates are inhibited, respectively.
Table 2 summarizes the percentage of 48-h itraconazole MICs obtained by the Etest on the two agar media that were within 2 dilutions of the reference method result. Overall, the percent agreement was 96% with RPMI and 80% with Casitone agar. The agreement between Etest and microdilution MICs was 100% for all species except Rhizopus spp. (83%) and P. variotii (0%) with RPMI agar. Lower levels of agreement were observed when Casitone agar was used; however, 100% agreement was observed with Fusarium spp., P. boydii, P. variotii, and the Acremonium sp. In virtually every instance when a discrepancy was observed between Etest and reference method results, the Etest provided a higher MIC.
TABLE 2.
Percent agreement of Etest with reference microdilution procedure for testing of activity of itraconazole against moldsa
| Species | No. of isolates | % Agreementb for testing on:
|
|
|---|---|---|---|
| RPMI | Casitone | ||
| Fusarium spp. | 13 | 100 | 100 |
| P. boydii | 5 | 100 | 100 |
| Rhizopus spp.c | 6 | 83 | 50 |
| A. flavus | 10 | 100 | 60 |
| A. fumigatus | 12 | 100 | 50 |
| Aspergillus spp.d | 2 | 100 | 50 |
| P. variotii | 1 | 0 | 100 |
| Acremonium sp. | 1 | 100 | 100 |
| TOTAL | 50 | 96 | 80 |
Both Etest and microdilution MICs were read at 48 h.
Percentage of Etest MICs within 2 dilutions of the reference microdilution MICs when tested on RPMI or Casitone agar.
Etest itraconazole MICs for Rhizopus spp., read at 18 to 24 h.
Includes A. niger and A. terreus.
It is notable that for Aspergillus spp. the agreement between itraconazole Etest MICs read at 24 h and reference microdilution MICs read at 48 h was 100% with both RPMI and Casitone media (Table 3). Thus for the most common species of filamentous fungi encountered clinically, the Etest may be read earlier than the broth method and the choice of test medium may be flexible.
TABLE 3.
Percent agreement of Etest MICs of itraconazole read at 24 h with reference microdilution MICs of itraconazole for isolates of Aspergillus spp.a
| Species (no. of isolates) | % Agreementb for testing on:
|
|
|---|---|---|
| RPMI | Casitone | |
| A. flavus (10) | 100 | 100 |
| A. fumigatus (12) | 100 | 100 |
| A. niger (1) | 100 | 100 |
| A. terreus (1) | 100 | 100 |
Etest results read at 24 h and microdilution results read at 48 h.
Percentage of Etest MICs within 2 dilutions of the reference microdilution MICs when tested on RPMI or Casitone agar.
The results of this study confirm and extend those of Szekely et al. (18) regarding the applicability of the Etest stable agar gradient method for determining the in vitro susceptibilities of filamentous fungi to itraconazole. Szekely et al. (18) used RPMI agar and 48 h of incubation and found that the Etest procedure was reproducible and served as a suitable method for antifungal susceptibility testing of molds. The overall agreement between Etest and broth microdilution was 88% for itraconazole. The agreement was 97.5% when testing Aspergillus spp. (18). Furthermore, they demonstrated that the Etest was able to detect resistance to itraconazole among A. fumigatus and other molds (18).
We found the Etest to be a very simple means of determining the in vitro susceptibilities of molds to itraconazole. RPMI agar with glucose (final concentration, 2%) supported optimal growth of all species tested and provided excellent (96%) agreement with the MICs obtained with the broth microdilution method (Table 2). As noted by Szekely et al. (18), the itraconazole inhibition ellipses were clear for most isolates tested on RPMI medium (Fig. 1).
Although Casitone agar did not perform as well as RPMI agar, it supported growth of the test isolates and achieved 80% agreement with results for the reference method (Tables 2 and 3). Importantly, when read at 24 h, Casitone agar and RPMI agar produced results that were in complete agreement with the 48-h reference MICs in testing of Aspergillus spp. (Table 3). Since Aspergillus spp. constitute the most frequently encountered pathogen among the filamentous fungi (17), an method for determining MICs whose results can be read as early as 24 h may be useful in the clinical laboratory.
In summary, we have provided additional documentation of the ability of Etest to generate itraconazole MIC data for filamentous fungi that are comparable to those obtained by the NCCLS broth microdilution method. RPMI agar with 2% glucose may be used to determine reference-quality MICs of itraconazole as well as amphotericin B (18) when tested against Aspergillus spp. and other less common molds, as well as Candida spp. and Cryptococcus neoformans (14, 15, 18). This will be attractive to laboratories, since it will provide the flexibility to test one or more commonly used antifungal agents selectively against a wide variety of yeasts and molds that may be encountered clinically. It is prudent to keep in mind that these results, as noted by Johnson et al. (7) for amphotericin B and aspergillosis, may not be entirely predictive of clinical outcome.
ACKNOWLEDGMENTS
The excellent secretarial support of Kay L. Meyer is greatly appreciated.
This study was supported in part by AB BIODISK.
REFERENCES
- 1.Baker C N, Stocker S A, Culver D H, Thornsberry C. Comparison of the E test to agar dilution, broth microdilution, and agar diffusion susceptibility testing techniques by using a special challenge set of bacteria. J Clin Microbiol. 1991;29:533–538. doi: 10.1128/jcm.29.3.533-538.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cormican M G, Pfaller M A. Standardization of antifungal susceptibility testing. J Antimicrob Chemother. 1996;38:561–578. doi: 10.1093/jac/38.4.561. [DOI] [PubMed] [Google Scholar]
- 3.Espinel-Ingroff A, Dawson K, Pfaller M, Anaissie E, Breslin B, Dixon D, Fothergill A, Peter J, Rinaldi M, Walsh T. Comparative and collaborative evaluation of standardization of antifungal susceptibility testing for filamentous fungi. Antimicrob Agents Chemother. 1995;39:314–319. doi: 10.1128/aac.39.2.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Espinel-Ingroff A, Pfaller M, Erwin M E, Jones R N. Interlaboratory evaluation of Etest method for testing antifungal susceptibilities of pathogenic yeasts to five antifungal agents by using Casitone agar and solidified RPMI 1640 medium with 2% glucose. J Clin Microbiol. 1996;34:848–852. doi: 10.1128/jcm.34.4.848-852.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Espinel-Ingroff A, Bartlett M, Bowden R, Chin N X, Cooper C, Jr, Fothergill A, McGinnis M R, Menezes P, Messer S A, Nelson P W, Odds F C, Pasarell L, Peter J, Pfaller M A, Rex J H, Rinaldi M G, Shankland G S, Walsh T, Weitzman I. Multicenter evaluation of proposed standardized procedure for antifungal susceptibility testing of filamentous fungi. J Clin Microbiol. 1997;35:139–143. doi: 10.1128/jcm.35.1.139-143.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Espinel-Ingroff A, White T, Pfaller M A. Antifungal agents and susceptibility tests. In: Murray P R, Baron E J, Pfaller M A, Tenover F C, Yolken R H, editors. Manual of clinical microbiology. 7th ed. Washington, D.C.: ASM Press; 1999. pp. 1640–1652. [Google Scholar]
- 7.Johnson E M, Oakley K L, Radford S A, Moore C B, Warn P, Warnock D W, Denning D W. Lack of correlation of in vitro amphotericin B susceptibility testing with outcome in a murine model of Aspergillus infections. J Antimicrob Chemother. 2000;45:85–93. doi: 10.1093/jac/45.1.85. [DOI] [PubMed] [Google Scholar]
- 8.Jorgensen J H, Ferraro M J, McElmeel M L, Spargo J, Swenson J M, Tenover F C. Detection of penicillin and extended-spectrum cephalosporin resistance among Streptococcus pneumoniae clinical isolates by use of the E test. J Clin Microbiol. 1994;32:159–163. doi: 10.1128/jcm.32.1.159-163.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jorgensen J H, Turnidge J D, Washington J A. Antibacterial susceptibility tests: dilution and disk diffusion methods. In: Murray P R, Baron E J, Pfaller M A, Tenover F C, Yolken R H, editors. Manual of clinical microbiology. 7th ed. Washington, D.C.: ASM Press; 1999. pp. 1526–1543. [Google Scholar]
- 10.National Committee for Clinical Laboratory Standards. Reference method for broth dilution antifungal susceptibility testing of yeast. Approved standard M27-A. Wayne, Pa: National Committee for Clinical Laboratory Standards; 1997. [Google Scholar]
- 11.National Committee for Clinical Laboratory Standards. Reference method for broth dilution antifungal susceptibility testing of condidium-forming filamentous fungi. Proposed standard M38-P. Wayne, Pa: National Committee for Clinical Laboratory Standards; 1998. [Google Scholar]
- 12.Pfaller M A, Messer S A, Bolmström A, Odds F C, Rex J H. Multisite reproducibility of the Etest MIC method for antifungal susceptibility testing of yeast isolates. J Clin Microbiol. 1996;34:1691–1693. doi: 10.1128/jcm.34.7.1691-1693.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pfaller M A, Rex J H, Rinaldi M G. Antifungal testing: technical advances and potential clinical applications. Clin Infect Dis. 1997;24:776–784. doi: 10.1093/clinids/24.5.776. [DOI] [PubMed] [Google Scholar]
- 14.Pfaller M A, Messer S A, Karlsson Å, Bolmström A. Evaluation of the Etest method for determining fluconazole susceptibilities of 402 clinical yeast isolates by using three different agar media. J Clin Microbiol. 1998;36:2586–2589. doi: 10.1128/jcm.36.9.2586-2589.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pfaller M A, Messer S A, Bolmström A. Evaluation of Etest for determining in vitro susceptibility of yeast isolates to amphotericin B. Diagn Microbiol Infect Dis. 1998;32:223–227. doi: 10.1016/s0732-8893(98)00120-5. [DOI] [PubMed] [Google Scholar]
- 16.Pfaller M A, Marco F, Messer S A, Jones R N. In vitro activity of two echinocandin derivatives, LY303366 and MK-0991 (L-743,792), against clinical isolates of Aspergillus, Fusarium, Rhizopus, and other filamentous fungi. Diagn Microbiol Infect Dis. 1998;30:251–255. doi: 10.1016/s0732-8893(97)00246-0. [DOI] [PubMed] [Google Scholar]
- 17.Rees J R, Pinner R W, Hajjeh R A, Brandt M E, Reingold A L. The epidemiological features of invasive mycotic infections in the San Francisco Bay area, 1992–1993: results of population-based laboratory active surveillance. Clin Infect Dis. 1998;27:1138–1147. [PubMed] [Google Scholar]
- 18.Szekely A, Johnson E M, Warnock D W. Comparison of E-test and broth microdilution methods for antifungal drug susceptibility testing of molds. J Clin Microbiol. 1999;37:1480–1483. doi: 10.1128/jcm.37.5.1480-1483.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wanger A, Mills K, Nelson P W, Rex J H. Comparison of Etest and National Committee for Clinical Laboratory Standards broth macrodilution method for antifungal susceptibility testing: enhanced ability to detect amphotericin B-resistant Candida isolates. Antimicrob Agents Chemother. 1995;39:2520–2522. doi: 10.1128/aac.39.11.2520. [DOI] [PMC free article] [PubMed] [Google Scholar]