Author's summary
Ultra-processed food (UPF), which is growing in consumption worldwide, is salty and sweet, industrially produced, and primarily consists of compounds derived from food with little, if any, whole food. The current study investigated the association between the dietary energy contribution of UPF consumption and blood pressure (BP) in Korean adults using data from the Korea National Health and Nutrition Examination Survey VII 2016–2018. As a result, the UPF consumption was independently associated with elevated BP, and this association was more profound among current smokers and obese adults. These results suggest that lowering the UPF consumption may help prevent BP elevation.
Keywords: Food processing, Blood pressure, Hypertension
Abstract
Background and Objectives
There is growing evidence supporting the association between ultra-processed food (UPF) consumption and metabolic disease risk. However, little is known about the association between UPF consumption and blood pressure (BP). Thus, this study examined the association between UPF consumption and elevated BP in Korean adults.
Methods
This study used data from the Korea National Health and Nutrition Examination Survey (2016–2018) and included 9,188 participants aged 30–79 years without a history of hypertension diagnosis. Food items reported in a one-day 24-hour recall were categorized on the basis of the NOVA (not an acronym) food classification criteria. UPF consumption was estimated as the contribution to total energy intake. Elevated BP was defined as systolic BP ≥120 mmHg or diastolic BP ≥80 mmHg. The independent association between UPF consumption and elevated BP was assessed by multivariable logistic regression analysis.
Results
The upper tertile of UPF consumption was significantly associated with elevated BP compared with the lower tertile, after adjusting for potential confounders. A linear trend was observed for elevated BP across the tertiles of the dietary energy contribution of UPF. Similar results were found in stratified analyses by age group, smoking, obesity, and overall dietary quality. However, a marginal level of association was found in some subgroups, current smokers, and non-obese adults.
Conclusions
The dietary energy contribution of UPF consumption was positively associated with increased prevalence of elevated BP, and these findings suggest that lowering UPF consumption might help prevent BP elevation.
INTRODUCTION
Elevated blood pressure (BP) is a major modifiable risk factor for cardiovascular disease, which is the main contributor to morbidity and mortality globally.1),2) The World Health Organization launched the Global Noncommunicable Diseases Action Plan, which includes a 25% relative reduction in the prevalence of raised BP or contain the prevalence of raised BP, according to national circumstances.3) Among both diagnosed and undiagnosed individuals with hypertension, BP management is essential because high-normal BP can also increase the risk of cardiovascular disease.4) Behavioral risk factors, including tobacco use, physical activity, and diet, play a considerable role in BP control.5),6) Numerous studies have been conducted on the effect of diet on BP, and a positive association between sodium, sugar, and BP has been well established.7)
Ultra-processed food (UPF) is salty and sweet, industrially produced, and primarily consists of compounds derived from food with little, if any, whole food.8) UPF is energy-dense; low in fiber, micronutrients, and other bioactive compounds; and often high in saturated or trans fat.9) Given these nutritional properties, high UPF consumption is linked to unhealthy dietary food profiles and diet-related noncommunicable diseases.9) The worldwide increase in UPF consumption and the prospect of continued industry growth has sparked interest in the health impacts of UPF.10),11),12) As a result, there is growing evidence suggesting a positive association between the consumption of UPF and a higher prevalence of cardiovascular disease, metabolic syndrome, obesity, and cancer.8),13),14),15)
However, studies on the association between UPF and elevated BP are lacking. Considering that most studies have targeted Western populations,16),17),18),19) data on UPF intake and BP in Asian populations are insufficient. Moreover, most research has focused on participants who were diagnosed with hypertension by a health professional or on those who took antihypertensive medication.16),17),19) Therefore, information on individuals with elevated BP but have not yet been diagnosed with hypertension is limited. The current study aimed to examine whether UPF consumption is associated with elevated BP among Korean adults without a history of hypertension. We hypothesized that participants with high UPF consumption have elevated BP compared to individuals with low UPF consumption.
METHODS
Ethical statement
The survey protocols were approved by the Institutional Review Board (No. 2018-01-03-P-A) of the Korea Centers for Disease Control and Prevention and informed consent was obtained from each participant before enrollment in the survey.
Data source and study population
This study used data from the Korea National Health and Nutrition Examination Survey (KNHANES VII) 2016–2018, which is a nationally representative cross-sectional survey on individuals aged ≥1 year via health examinations, health interviews and nutrition surveys.20) Using these 3 component surveys, KNHANES collects information on participants' demographic, socioeconomic, health, and nutritional status.20) In the food intake survey based on the 24-hour recall method of KNHANES, detailed information on the food consumed by the participants during the last 24 hours, the time and place where the food was consumed, and the amount of intake was collected.21) The type of food consumed by the participants (e.g., boiled egg or fried egg) was investigated as is.21) The recipe information of each mixed dish or multi-ingredient food was collected to estimate food or nutrient intake.21) Among the 24,269 participants in KNHANES VII, those who did not undergo the 24-hour recall method (n=2,998), were aged <30 or ≥80 years (n=7,223), and were pregnant or breastfeeding (n=162) were excluded. Among the remaining 13,886 adults, we additionally excluded individuals with missing data on a key variable (n=1,426) and those who reported they had a physician-diagnosed hypertension (n=3,272). Finally, 9,188 participants were included in the study.
Consumption of ultra-processed food
The raw data of the 24-hour recall method provided the names of the food that the participants reported in the survey and showed detailed food information that was disassembled for each food item.21) In the current study, we used information on 3,984 food items and classified them into 4 groups according to the NOVA (not an acronym) system: 1) unprocessed or minimally processed food, 2) processed culinary ingredients, 3) processed food, and 4) UPF.22) This NOVA system classifies food on the basis of the extent, nature, and aim of food processing.9) Unprocessed or minimally processed foods are foods that are derived from direct nature or altered by minimal processes including drying, grinding, boiling, freezing, and pasteurization (e.g., raw corn or steamed corn).9) Processed culinary ingredients are ingredients derived by purified (e.g., salt) from nature or extracted from foods (e.g., corn oil).23) Processed foods are foods made by adding processed culinary ingredients to unprocessed or minimally processed foods, and their storability has been improved by using processes such as bottling, canning, and fermentation (e.g., canned corn).23) UPF is not a type of transformed food but a formulation that consists of additives and substances derived mostly or entirely from food.9) UPF includes soft drinks, distilled alcoholic beverages, instant sauces and spreads, sweet or salty snacks, cookies, and diverse types of ready-to heat or ready-to-eat food (e.g., popcorn, instant noodles, soups, rice, or pizza). More details are described elsewhere.22) UPF consumption was estimated as the dietary energy contribution from UPF.
Elevated BP
All health examination procedures of KNHANES were performed by well-trained medical staff using standardized protocols.20) BP was measured in a managed environment with a noise level ≤ 65 dB and temperature ≤ 20°C–25°C. After resting for more than 5 minutes in a sitting position, BP was measured in the right upper arm 3 times at 5 minutes intervals by using a mercury sphygmomanometer (Baumanometer® Wall Unit 33 [0850]; Baum, Copiague, NY, USA). The mean of the second and third measurements was taken as the final systolic and diastolic BP. Elevated BP was defined as systolic BP ≥ 120 mmHg or diastolic BP ≥ 80 mmHg.
Covariates
We adjusted for potential confounders for sociodemographic, anthropometric and nutritional information. Sociodemographic information included sex, age, income (low or high-middle), education level (≤6 years, 7–12 years, and >12 years), occupation (white, pink, blue, and others), region (rural or urban), smoking status (current, ex-smoker, nonsmoker), exercise (yes, no), and history of disease (dyslipidemia, stroke, myocardial infarction, angina pectoris, diabetes, and kidney failure). Physical activity was examined using the International Physical Activity Questionnaire.24) Exercise was defined as moderate-intensity activity ≥150 min/week, vigorous activity ≥75 min/week, or a combination of the 2. For anthropometric data, body weight was measured using a digital scale (GL-6000-20; G-tech, Uijeongbu, Korea) to the nearest 0.1 kg, and standing height was measured using a stadiometer (SECA 225; SECA, Hamburg, Germany) to the nearest 0.1 cm. Body mass index (BMI) was calculated as body weight divided by height squared (kg/m2) and was included in the model as a continuous variable. For nutritional information, the total energy intake (kcal) and the Korean Health Eating Index (KHEI) score were used as covariates. The KHEI was designed to assess individual's overall diet quality on the basis of the 2010 Korean Dietary Guidelines25) and was measured using dietary information from the 24-hour recall method and dietary behavior questionnaire. The KHEI consisted of a total of 14 components, which are 8 that should be consumed frequently (breakfast, fruits, vegetables, meat/fish/eggs and beans, grains, and milk and dairy products) and 6 that should be balanced consumed (carbohydrates, fat, sodium, saturated fatty acids, sweets and beverages, and energy). The total KHEI score ranges from 0 to 100, with a higher score indicating a better diet quality.23)
Statistical analyses
General characteristic data are presented as mean±standard deviation or number (%). The differences in variables according to the tertiles of the dietary energy contribution of UPF were examined using analysis of variance and the χ2 test for continuous variables and categorical variables, respectively. Sex-specific tertiles were used for sex-stratified analyses. Independent associations between UPF consumption and elevated BP were assessed by logistic regression analyses between sexes. Tests for linear trends in the dietary energy contribution of UPF consumption were performed. Linear association between UPF consumption and BP as a continuous variable was determined via multiple linear regression analyses. Subgroup analyses according to age, smoking status (except for women), menopause status, BMI, and KHEI were conducted, and 2-sided p<0.05 was considered statistically significant. All statistical tests were performed using SAS 9.4 (SAS Institute Inc., Cary, NC, USA).
RESULTS
A total of 9,188 adults (40.2% male and 59.8% female) were included in this study (Table 1). The mean dietary energy contributions of UPF in the participants were 6.9%, 20.3%, and 43.6% in T1 (<13.16%), T2 (≥13.16%, <28.55%), and T3 (≥28.55%), respectively. Those in the highest tertile of UPF consumption were more likely to be male, younger, urban residents, and current smokers and have higher BMI and energy intake. They were also less likely to have a history of disease and had a lower KHEI score than adults in the middle and lowest tertiles of UPF consumption. No differences were observed in income and physical activity according to UPF intake.
Table 1. Baseline characteristics of the study participants according to dietary energy contribution of ultra-processed food.
| Characteristics | Total (n=9,188) | Energy contribution of UPF | p value* | ||
|---|---|---|---|---|---|
| T1 | T2 | T3 | |||
| UPF consumption (% of total energy intake) | 23.6±17.2 | 6.9±3.8 | 20.3±4.4 | 43.6±12.8 | <0.001 |
| Age (years) | 50.5±13.3 | 54.7±12.6 | 50.3±12.3 | 46.6±11.5 | <0.001 |
| Male | 3,695 (40.2) | 1,117 (36.5) | 1,252 (40.9) | 1,326 (43.2) | <0.001 |
| High income† | 4,739 (51.6) | 1,534 (50.2) | 1,623 (53.0) | 1,582 (51.6) | 0.082 |
| Region (urban) | 6,382 (69.5) | 2,054 (67.2) | 2,128 (69.5) | 2,200 (71.7) | 0.001 |
| Current smoker | 1,587 (17.3) | 395 (12.9) | 487 (15.9) | 705 (23.0) | <0.001 |
| Regular physical activity | 4,046 (44.0) | 1,310 (42.8) | 1,390 (45.4) | 1,346 (43.9) | 0.126 |
| Body mass index (kg/m2) | 23.6±3.4 | 23.6±3.4 | 23.5±3.3 | 23.8±3.5 | 0.002 |
| History of diseases‡ | 1,573 (17.1) | 671 (21.9) | 517 (16.9) | 385 (12.6) | <0.001 |
| >12 years of education | 4,081 (44.4) | 1,060 (34.7) | 1,439 (47.0) | 1,582 (51.6) | <0.001 |
| Total energy intake (kcal/day) | 1,983.9±877.9 | 1,806.7±758.1 | 1,987.7±829.6 | 2,156.8±993.7 | <0.001 |
| Korean Healthy Eating Index (score) | 64.6±13.3 | 67.3±12.5 | 66.5±13.0 | 60.0±13.2 | <0.001 |
Values are presented as mean±standard deviation or number (%).
*Analysis of variance or χ2 test where appropriate; †More than the median of income of total participants; ‡Having any one of the following: dyslipidemia, stroke, myocardial infarction, angina pectoris, diabetes, and kidney failure.
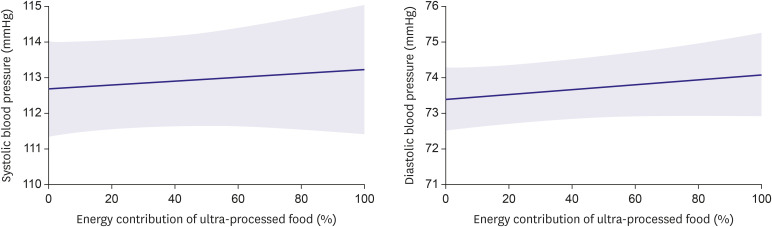
Table 2 shows the associations between UPF energy contribution and potential confounders with elevated BP via logistic regression analyses. The prevalence of elevated BP in the total population were 47.1%, 43.9%, and 46.0% in T1, T2, and T3, respectively. T2 was not significantly associated with elevated BP (odds ratio [OR], 1.02; 95% confidence interval [CI], 0.92–1.14) in model 1, which includes age, sex, BMI, income, education level, occupation, region, smoking status, exercise, total energy intake, and history of disease. However, T3 was associated with a higher prevalence of elevated BP (OR, 1.25; 95% CI, 1.11–1.40) compared to the lowest tertile. This association was also shown in model 2, which adjusted for continuous KHEI score in addition to the covariates in model 1 (OR, 1.22; 95% CI, 1.09–1.37). A significant linear trend was observed in both models 1 and 2 (all p-values for trend: <0.001). The energy contribution of UPF (per 5%kcal increase) was also associated with elevated BP after adjusting for the same covariates of model 2 (OR, 1.02; 95% CI, 1.01–1.04; data not shown). In a model that analyzed bot the energy contribution of UPF and BP as continuous variables (Figure 1), both systolic BP and diastolic BP was slightly higher (β=0.005 and 0.007, respectively) whenever the dietary energy intake of UPF was 1% higher, but not significant (p value=0.577 and 0.245, respectively). Table 3 shows the associations between the energy contribution of UPF and elevated BP according to the subgroup. Increased ORs in T3 compared with T1 were observed for female (OR, 1.26; 95% CI, 1.08–1.46), but not for male (OR, 1.10; 95% CI, 0.92–1.32). The results of subgroup analysis according to age, smoking status, obesity, and overall dietary quality were consistent with our main findings, but there was a marginal level of associations in some subgroups, current smokers, and non-obese adults.
Table 2. Association of energy contribution of ultra-processed food and potential confounders with elevated blood pressure.
| Variables | Total No. | No (%) of elevated BP | Unadjusted | Model 1 | Model 2 | ||||
|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p value | OR (95% CI) | p value | OR (95% CI) | p value | ||||
| UPF consumption | |||||||||
| T1 | 3,059 | 1,442 (47.1) | 1.00 | 1.00 | 1.00 | ||||
| T2 | 3,062 | 1,345 (43.9) | 0.88 (0.79–0.97) | 0.012 | 1.02 (0.92–1.14) | 0.691 | 1.02 (0.92–1.14) | 0.697 | |
| T3 | 3,067 | 1,412 (46.0) | 0.96 (0.87–1.06) | 0.386 | 1.25 (1.11–1.40) | <0.001 | 1.22 (1.09–1.37) | 0.001 | |
| Age | |||||||||
| per 10 years | 1.46 (1.40–1.54) | <0.001 | 1.48 (1.41–1.56) | <0.001 | |||||
| Sex | |||||||||
| Female | 5,493 | 2,081 (37.9) | 1.00 | 1.00 | |||||
| Male | 3,695 | 2,118 (57.3) | 2.02 (1.77–2.31) | <0.001 | 2.01 (1.75–2.30) | <0.001 | |||
| Body mass index | |||||||||
| per 1 kg/m2 | 1.15 (1.13–1.16) | <0.001 | 1.15 (1.13–1.16) | <0.001 | |||||
| Income | |||||||||
| Lower median | 4,449 | 2,073 (46.6) | 1.00 | 1.00 | |||||
| Upper median | 4,739 | 2,126 (44.9) | 0.98 (0.90–1.08) | 0.696 | 0.99 (0.90–1.09) | 0.809 | |||
| Education level | |||||||||
| ≤6 years | 1,315 | 813 (61.8) | 1.00 | 1.00 | |||||
| 7–12 years | 3,792 | 1,792 (47.3) | 0.80 (0.69–0.93) | 0.004 | 0.82 (0.71–0.95) | 0.009 | |||
| >12 years | 4,081 | 1,594 (39.1) | 0.73 (0.61–0.87) | <0.001 | 0.75 (0.63–0.89) | 0.001 | |||
| Occupation | |||||||||
| White | 2,715 | 1,101 (40.6) | 1.00 | 1.00 | |||||
| Pink | 1,228 | 554 (45.1) | 1.01 (0.86–1.17) | 0.947 | 1.00 (0.86–1.17) | 0.974 | |||
| Blue | 2,218 | 1,224 (55.2) | 1.08 (0.94–1.24) | 0.272 | 1.08 (0.94–1.24) | 0.273 | |||
| Others | 3,027 | 1,320 (43.6) | 0.87 (0.76–0.99) | 0.031 | 0.87 (0.76–0.99) | 0.031 | |||
| Region | |||||||||
| Rural | 2,806 | 1,324 (47.2) | 1.00 | 1.00 | |||||
| Urban | 6,382 | 2,875 (45.1) | 1.08 (0.98–1.19) | 0.114 | 1.09 (0.99–1.20) | 0.097 | |||
| Smoking status | |||||||||
| Nonsmoker | 5,705 | 2,331 (40.9) | 1.00 | 1.00 | |||||
| Ex-smoker | 1,896 | 1,043 (55.0) | 0.95 (0.83–1.10) | 0.506 | 0.94 (0.82–1.09) | 0.414 | |||
| Current smoker | 1,587 | 825 (52.0) | 0.96 (0.83–1.12) | 0.604 | 0.94 (0.81–1.09) | 0.400 | |||
| Exercise | |||||||||
| No | 5,142 | 2,359 (45.9) | 1.00 | 1.00 | |||||
| Yes | 4,046 | 1,840 (45.5) | 1.05 (0.96–1.15) | 0.257 | 1.06 (0.97–1.16) | 0.213 | |||
| Total energy intake | |||||||||
| per 100 kcal/day | 1.00 (0.99–1.00) | 0.637 | 1.00 (0.99–1.01) | 0.890 | |||||
| History of disease | |||||||||
| No | 7,615 | 3,339 (43.9) | 1.00 | 1.00 | |||||
| Yes | 1,573 | 860 (54.7) | 0.94 (0.83–1.06) | 0.283 | 0.94 (0.83–1.06) | 0.323 | |||
| KHEI | |||||||||
| per 1 SD | 0.95 (0.90–0.99) | 0.026 | |||||||
All variables whose values appear in each column were included in the statistical model for that column.
BP = blood pressure; CI = confidence interval; KHEI = Korean Health Eating Index; OR = odds ratio; SD = standard deviation.
Figure 1. Multiple linear regression curves on the association between energy contribution of ultra-processed food and blood pressure.
Shaded areas represent 95% confidence intervals. Fully adjusted for age, body mass index, income (lower median/upper median), education level (≤6 years, 7–12 years, >12 years), occupation (white, pink, blue, and others), region (rural, urban), smoking status (never, ex-, current), exercise (yes, no), total energy intake, history of disease (at least one of dyslipidemia, stroke, myocardial infarction, angina pectoris, diabetes, and kidney failure), and Korean Health Eating Index.
Table 3. Associations between energy contribution of ultra-processed food and elevated blood pressure according to subgroup.
| Subgroup | Total No. | No. (%) of elevated BP | Ultra-processed food consumption (% of total energy intake) | |||
|---|---|---|---|---|---|---|
| T1 | T2 | T3 | p for trend | |||
| OR | OR (95% CI) | OR (95% CI) | ||||
| Overall | 9,188 | 4,199 (45.7) | 1.00 | 1.02 (0.92–1.14) | 1.22 (1.09–1.37) | 0.001 |
| Male | 3,695 | 2,118 (57.3) | 1.00 | 0.88 (0.74–1.04) | 1.10 (0.92–1.32) | 0.296 |
| Female | 5,493 | 2,081 (37.9) | 1.00 | 1.07 (0.93–1.24) | 1.26 (1.08–1.46) | 0.004 |
| 30–49 years | 4,685 | 1,683 (35.9) | 1.00 | 0.98 (0.82–1.17) | 1.20 (1.01–1.43) | 0.021 |
| 50–79 years | 4,503 | 2,516 (55.9) | 1.00 | 1.06 (0.92–1.22) | 1.24 (1.06–1.46) | 0.011 |
| Non-, ex-smokers | 7,601 | 3,374 (44.4) | 1.00 | 1.03 (0.92–1.16) | 1.22 (1.07–1.38) | 0.003 |
| Current smokers | 1,587 | 825 (52.0) | 1.00 | 1.05 (0.79–1.40) | 1.29 (0.98–1.70) | 0.053 |
| Normal body weight (<25 kg/m2) | 6,348 | 2,488 (39.2) | 1.00 | 1.02 (0.89–1.16) | 1.15 (1.00–1.33) | 0.052 |
| Obesity (≥25 kg/m2) | 2,840 | 1,711 (60.3) | 1.00 | 1.06 (0.87–1.29) | 1.38 (1.13–1.69) | 0.002 |
| Low KHEI (<64.6) | 4,368 | 2,019 (46.2) | 1.00 | 0.95 (0.80–1.13) | 1.21 (1.02–1.42) | 0.015 |
| High KHEI (≥64.6) | 4,820 | 2,180 (45.2) | 1.00 | 1.07 (0.93–1.23) | 1.20 (1.02–1.42) | 0.029 |
The ORs (95% CI) of subgroup analyses according to sex, smoking status, and body mass index were adjusted for all other factors, not involving the subgroup.
The ORs (95% CI) of subgroup analyses according to age and KHEI score were adjusted for all other factors involving the subgroup.
Fully adjusted for age, sex, body mass index, income (lower median/upper median), education level (≤6 years, 7–12 years, >12 years), occupation (white, pink, blue, and others), region (rural, urban), smoking status (nonsmoker, ex-smoker, current smoker), exercise (yes, no), total energy intake, history of disease (at least one of dyslipidemia, stroke, myocardial infarction, angina pectoris, diabetes, and kidney failure), and KHEI.
BP = blood pressure; CI = confidence interval; KHEI = Korean Health Eating Index; OR = odds ratio.
Table 4 explains the results of the subgroup associations between the energy contribution of UPF and elevated BP by sex. For male participants, the percentages of elevated BP were 58.4%, 54.1%, and 59.4%, in T1 (<14.29%), T2 (≥14.29%, <29.75%), and T3 (≥29.75%), respectively. Increased ORs were found in the analyses according to age, but these were not significant in male participants. In particular, among the male current smoker and obesity group, higher ORs were shown for elevated BP (current smoker: OR, 1.38; 95% CI, 1.03–1.86; obesity: OR, 1.35; 95% CI, 1.00–1.82) compared to T1. The OR increased in a dose-response manner among current smokers (p for trend=0.030).
Table 4. Subgroup associations between energy contribution of ultra-processed food and elevated blood pressure by sex.
| Subgroup | Total No. | No. (%) of elevated BP | Ultra-processed food consumption (% of total energy intake) | ||||
|---|---|---|---|---|---|---|---|
| T1 | T2 | T3 | p for trend | ||||
| OR | OR (95% CI) | OR (95% CI) | |||||
| Male | |||||||
| 30–49 years | 1,867 | 1,018 (54.5) | 1.00 | 0.89 (0.68–1.15) | 1.09 (0.84–1.41) | 0.375 | |
| 50–79 years | 1,828 | 1,100 (60.2) | 1.00 | 0.90 (0.72–1.12) | 1.15 (0.88–1.49) | 0.480 | |
| Non-, ex-smokers | 2,371 | 1,380 (58.2) | 1.00 | 0.79 (0.64–0.97) | 1.00 (0.80–1.26) | 0.861 | |
| Current smokers | 1,324 | 738 (55.7) | 1.00 | 1.15 (0.85–1.55) | 1.38 (1.03–1.86) | 0.030 | |
| Normal body weight (<25 kg/m2) | 2,276 | 1,142 (50.2) | 1.00 | 0.84 (0.69–1.04) | 1.00 (0.80–1.26) | 0.979 | |
| Obesity (≥25 kg/m2) | 1,419 | 976 (68.8) | 1.00 | 1.04 (0.78–1.38) | 1.35 (1.00–1.82) | 0.051 | |
| Low KHEI (<64.6) | 1,975 | 1,142 (57.8) | 1.00 | 0.91 (0.71–1.16) | 1.16 (0.91–1.49) | 0.159 | |
| High KHEI (≥64.6) | 1,720 | 976 (56.7) | 1.00 | 0.85 (0.68–1.07) | 1.03 (0.79–1.35) | 0.980 | |
| Female | |||||||
| 30–49 years | 2,818 | 665 (23.6) | 1.00 | 1.07 (0.84–1.37) | 1.34 (1.06–1.70) | 0.011 | |
| 50–79 years | 2,675 | 1,416 (52.9) | 1.00 | 1.09 (0.91–1.31) | 1.20 (0.98–1.47) | 0.083 | |
| Premenopause | 2,894 | 724 (25.0) | 1.00 | 1.14 (0.89–1.45) | 1.46 (1.15–1.84) | 0.001 | |
| Postmenopause | 2,521 | 1,319 (52.3) | 1.00 | 1.05 (0.87–1.27) | 1.12 (0.91–1.38) | 0.286 | |
| Normal body weight (<25 kg/m2) | 4,072 | 1,346 (33.1) | 1.00 | 1.09 (0.92–1.30) | 1.19 (0.99–1.43) | 0.058 | |
| Obesity (≥25 kg/m2) | 1,421 | 735 (51.7) | 1.00 | 1.05 (0.80–1.37) | 1.42 (1.08–1.87) | 0.014 | |
| Low KHEI (<64.6) | 2,393 | 877 (36.7) | 1.00 | 0.99 (0.78–1.27) | 1.27 (1.01–1.59) | 0.034 | |
| High KHEI (≥64.6) | 3,100 | 1,204 (38.8) | 1.00 | 1.12 (0.93–1.35) | 1.24 (1.01–1.53) | 0.041 | |
ORs (95% CI) of subgroup analyses according to smoking status, body mass index, and menopausal status were adjusted for all other factors not involving the subgroup.
ORs (95% CI) of subgroup analyses according to age and KHEI score were adjusted for all other factors, involving the subgroup.
Fully adjusted for age, body mass index, income (lower median/upper median), education level (≤6 years, 7–12 years
BP = blood pressure; CI = confidence interval; KHEI = Korean Health Eating Index; OR = odds ratio.
For female participants, the percentages of elevated BP were 41.2%, 36.8%, and 35.7% in T1 (<12.46%), T2 (≥12.46%, <27.73%), and T3 (≥27.73%), respectively. Overall, the results of subgroup analyses in females showed an independent association between the energy contribution of UPF, elevated BP, and linear trends, but there was a marginal level of association in older and non-obese adults. The association between the energy contribution of UPF and elevated BP was more profound among the obesity group (OR, 1.42; 95% CI, 1.08–1.87) and premenopause group (OR, 1.46; 95% CI, 1.15–1.84) than in any other group.
DISCUSSION
This study found that a high dietary energy contribution from UPF consumption in Korean adults was independently associated with elevated BP. This association remained after adjusting for potential confounders, and this association was more profound among current smokers and obese adults.
Our results are consistent with those of previous studies. A cross-sectional study that analyzed 13,608 adults aged ≥19 years in Canada reported that participants in the highest tertile (≥58.7%) of UPF intake had 60% higher odds of hypertension than those in the lowest tertile (≤38.5%) after adjusting for socio-demographic covariates.17) This study measured hypertension on the basis of self-reported information and this data could not be examined against clinical records. A prospective cohort study on 14,790 middle-aged Spanish adults who were followed for a mean of 9.1 years found an increased hazard ratio of 1.21 (95% CI, 1.06–1.37) for the incidence of hypertension in the highest consumption group.16) Another prospective cohort study of 1,221 middle-aged Brazilian adult university graduates who were followed-up for 2 years reported that the highest percentage (≥34.6%) of energetic intake of UPF increased the risk of hypertension by 35%, whereas participants who consumed highly unprocessed or minimally processed food and culinary ingredients presented a decreased risk of hypertension.18) This positive association between UPF consumption and hypertension was also observed in another longitudinal study of 8,757 Brazilian adults aged 35–74 years.19) In this study, participants who consumed UPF had a 23% higher risk of hypertension.
The average dietary energy contribution of UPF in our study population was 23.6%, which was relatively lower than the 46.8–56.1% in Western populations.8),17) However, the high energy contribution of UPF was still associated with elevated BP in Korean adults without a history of hypertension. The association between UPF consumption and elevated BP was more profound among participants with less healthy lifestyles, such as current smokers and obese adults. People who consume a large amount of UPF tend to have other unhealthy lifestyles, such as tobacco use, low physical activity, and poor dietary patterns.16) Given that the consumption of UPF is also associated with overall diet quality,16) we adjusted for the KHEI score and stratified it according to the mean KHEI value unlike most similar studies, which did not consider diet quality. The results consistent with the main findings after additionally adjusted for KHEI were found, and the association was stronger in the low KHEI group than high KHEI group.
It is well known that reducing sodium intake, increasing potassium intake, and eating certain food groups such as vegetables and fruits, can reduce BP.26) Although there are many studies on the incidence of hypertension related to diet information, including nutrients, food type, and dietary patterns, relatively few studies have been conducted on hypertension according to UPF intake. The impact of UPF on BP can also be understood in terms of their detrimental nutrient profiles and dietary quality.16) In addition to these characteristics, food additives, neoformed contaminants, and chemicals from food packaging may also be linked to unhealthy outcomes.27) Food additives such as dietary emulsifiers cause a reduction in gut microbial diversity,28) which could contribute to the pathogenesis of hypertension.29)
To the best of our knowledge, this is the first study to analyze the association between UPF consumption and elevated BP in the Korean population. Moreover, we used national data from KNHANES, which is a nationally representative survey that includes various health- and nutrient-related variables that could influence the association between UPF intake and elevated BP.
This study has some limitations. First, given that our study was a cross-sectional study, we were unable to confirm the causality between UPF intake and elevated BP. It might be because those aware of their disease status were likely to have changed their habit (including diet) after diagnosis, and also their BP may be substantially influenced by medication rather than their diet. As expected, the association between UPF consumption and elevated BP were attenuated when analyzing all adults including those with a history of physician-diagnosed hypertension (Supplementary Table 1). Thus, we attempted to minimize reverse causation by excluding individuals with a history of hypertension, Second, the 24-hour recall method, which we used to measure UPF consumption, dose not assess the usual intake of participants; therefore, the participants may have consumed higher or lower amount of UPF, exceptionally. Third, there is a possibility that participants underreported unhealthy food intake owing to social desirability and social approval bias. Finally, although we included risk factors for elevated BP for adjustment, there might be possible covariates that were not included.
In conclusion, we found a significant positive association between UPF consumption and elevated BP among Korean adults without a history of physician-diagnosed hypertension. This independent association was more profound among current smokers and obese adults. These findings suggest that lowering UPF consumption might help prevent an increase BP. Further researches are needed to investigate a causal relationship between UPF consumption and elevated BP and to evaluate the possibility of low UPF consumption being used as a therapeutic strategy.
ACKNOWLEDGMENTS
The authors are grateful to the Korean Centers for Disease Control and Prevention that conducted the Korea National Health and Nutrition Examination Survey (KNHANES) which is the primary source of our study. We also appreciate all participants of KNHANES.
Footnotes
Funding: This work was supported by the National Research Foundation of Korea (NRF-2020R1I1A1A01064904) and the Basic Research Program via the National Research Foundation of Korea funded by MSIT (grant No. 2019R1A4A1028155).
Conflict of Interest: The authors have no financial conflicts of interest.
Data Sharing Statement: The data generated in this study is available from the corresponding authors upon reasonable request.
- Conceptualization: Shim SY, Kim HC, Shim JS.
- Data curation: Shim SY, Shim JS.
- Formal analysis: Shim SY, Shim JS.
- Funding acquisition: Kim HC, Shim JS.
- Methodology: Shim SY, Kim HC, Shim JS.
- Project administration: Shim SY, Kim HC, Shim JS.
- Supervision: Kim HC, Shim JS.
- Writing - original draft: Shim SY.
- Writing - review & editing: Shim SY, Kim HC, Shim JS.
SUPPLEMENTARY MATERIAL
Association of energy contribution of ultra-processed foods and potential confounders with elevated blood pressure among all adults regardless of a history of physician-diagnosed hypertension
References
- 1.Brunström M, Carlberg B. Association of blood pressure lowering with mortality and cardiovascular disease across blood pressure levels: a systematic review and meta-analysis. JAMA Intern Med. 2018;178:28–36. doi: 10.1001/jamainternmed.2017.6015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sheppard JP, Tucker KL, Davison WJ, et al. Self-monitoring of blood pressure in patients with hypertension-related multi-morbidity: systematic review and individual patient data meta-analysis. Am J Hypertens. 2020;33:243–251. doi: 10.1093/ajh/hpz182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Draft comprehensive global monitoring framework and targets for the prevention and control of noncommunicable diseases [Internet] Geneva: World Health Organization; 2013. [cited 2015 May 15]. Available from: http://apps.who.int/gb/ebwha/pdf_files/WHA66/A66_8-en.pdf?ua=1. [Google Scholar]
- 4.Vasan RS, Larson MG, Leip EP, et al. Impact of high-normal blood pressure on the risk of cardiovascular disease. N Engl J Med. 2001;345:1291–1297. doi: 10.1056/NEJMoa003417. [DOI] [PubMed] [Google Scholar]
- 5.Primatesta P, Falaschetti E, Gupta S, Marmot MG, Poulter NR. Association between smoking and blood pressure: evidence from the health survey for England. Hypertension. 2001;37:187–193. doi: 10.1161/01.hyp.37.2.187. [DOI] [PubMed] [Google Scholar]
- 6.Park S, Rink L, Wallace J. Accumulation of physical activity: blood pressure reduction between 10-min walking sessions. J Hum Hypertens. 2008;22:475–482. doi: 10.1038/jhh.2008.29. [DOI] [PubMed] [Google Scholar]
- 7.He FJ, MacGregor GA. Salt and sugar: their effects on blood pressure. Pflugers Arch. 2015;467:577–586. doi: 10.1007/s00424-014-1677-x. [DOI] [PubMed] [Google Scholar]
- 8.Juul F, Martinez-Steele E, Parekh N, Monteiro CA, Chang VW. Ultra-processed food consumption and excess weight among US adults. Br J Nutr. 2018;120:90–100. doi: 10.1017/S0007114518001046. [DOI] [PubMed] [Google Scholar]
- 9.Monteiro CA, Cannon G, Moubarac JC, Levy RB, Louzada ML, Jaime PC. The UN decade of nutrition, the NOVA food classification and the trouble with ultra-processing. Public Health Nutr. 2018;21:5–17. doi: 10.1017/S1368980017000234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Monteiro CA, Levy RB, Claro RM, de Castro IR, Cannon G. Increasing consumption of ultra-processed foods and likely impact on human health: evidence from Brazil. Public Health Nutr. 2011;14:5–13. doi: 10.1017/S1368980010003241. [DOI] [PubMed] [Google Scholar]
- 11.Moubarac JC, Batal M, Martins AP, et al. Processed and ultra-processed food products: consumption trends in Canada from 1938 to 2011. Can J Diet Pract Res. 2014;75:15–21. doi: 10.3148/75.1.2014.15. [DOI] [PubMed] [Google Scholar]
- 12.Monteiro CA, Cannon G, Levy RB, et al. Ultra-processed foods: what they are and how to identify them. Public Health Nutr. 2019;22:936–941. doi: 10.1017/S1368980018003762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Srour B, Fezeu LK, Kesse-Guyot E, et al. Ultra-processed food intake and risk of cardiovascular disease: prospective cohort study (NutriNet-Santé) BMJ. 2019;365:l1451. doi: 10.1136/bmj.l1451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tavares LF, Fonseca SC, Garcia Rosa ML, Yokoo EM. Relationship between ultra-processed foods and metabolic syndrome in adolescents from a Brazilian Family Doctor Program. Public Health Nutr. 2012;15:82–87. doi: 10.1017/S1368980011001571. [DOI] [PubMed] [Google Scholar]
- 15.Fiolet T, Srour B, Sellem L, et al. Consumption of ultra-processed foods and cancer risk: results from NutriNet-Santé prospective cohort. BMJ. 2018;360:k322. doi: 10.1136/bmj.k322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mendonça RD, Lopes ACS, Pimenta AM, Gea A, Martinez-Gonzalez MA, Bes-Rastrollo M. Ultra-processed food consumption and the incidence of hypertension in a Mediterranean cohort: The Seguimiento Universidad de Navarra Project. Am J Hypertens. 2017;30:358–366. doi: 10.1093/ajh/hpw137. [DOI] [PubMed] [Google Scholar]
- 17.Nardocci M, Polsky JY, Moubarac JC. Consumption of ultra-processed foods is associated with obesity, diabetes and hypertension in Canadian adults. Can J Public Health. 2021;112:421–429. doi: 10.17269/s41997-020-00429-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rezende-Alves K, Hermsdorff HH, Miranda A, Lopes AC, Bressan J, Pimenta AM. Food processing and risk of hypertension: cohort of Universities of Minas Gerais, Brazil (CUME Project) Public Health Nutr. 2021;24:4071–4079. doi: 10.1017/S1368980020002074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Scaranni PO, Cardoso LO, Chor D, et al. Ultra-processed foods, changes in blood pressure and incidence of hypertension: the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil) Public Health Nutr. 2021;24:3352–3360. doi: 10.1017/S136898002100094X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kweon S, Kim Y, Jang MJ, et al. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES) Int J Epidemiol. 2014;43:69–77. doi: 10.1093/ije/dyt228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee JS, Shim JS, Kim KN, Lee HS, Chang MJ, Kim HY. Key foods selection using data from the 7th Korea National Health and Nutrition Examination Survey (2016–2018) J Nutr Health. 2021;54:10–22. [Google Scholar]
- 22.Shim JS, Shim SY, Cha HJ, Kim J, Kim HC. Socioeconomic characteristics and trends in the consumption of ultra-processed foods in Korea from 2010 to 2018. Nutrients. 2021;13:1120. doi: 10.3390/nu13041120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shim JS, Shim S, Cha HJ, Kim J, Kim HC. Association between ultra-processed food consumption and dietary intake and diet quality in Korean adults. J Acad Nutr Diet. 2021 doi: 10.1016/j.jand.2021.07.012. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 24.Oh JY, Yang YJ, Kim BS, Kang JH. Validity and reliability of Korean version of international physical activity questionnaire (IPAQ) short form. J Korean Acad Fam Med. 2007;28:532–541. [Google Scholar]
- 25.Shim JS, Oh K, Jung SJ, Kim HC. Self-reported diet management and adherence to dietary guidelines in Korean adults with hypertension. Korean Circ J. 2020;50:432–440. doi: 10.4070/kcj.2019.0230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Flack JM, Adekola B. Blood pressure and the new ACC/AHA hypertension guidelines. Trends Cardiovasc Med. 2020;30:160–164. doi: 10.1016/j.tcm.2019.05.003. [DOI] [PubMed] [Google Scholar]
- 27.Martínez Steele E, Khandpur N, da Costa Louzada ML, Monteiro CA. Association between dietary contribution of ultra-processed foods and urinary concentrations of phthalates and bisphenol in a nationally representative sample of the US population aged 6 years and older. PLoS One. 2020;15:e0236738. doi: 10.1371/journal.pone.0236738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chassaing B, Koren O, Goodrich JK, et al. Dietary emulsifiers impact the mouse gut microbiota promoting colitis and metabolic syndrome. Nature. 2015;519:92–96. doi: 10.1038/nature14232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li J, Zhao F, Wang Y, et al. Gut microbiota dysbiosis contributes to the development of hypertension. Microbiome. 2017;5:14. doi: 10.1186/s40168-016-0222-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Association of energy contribution of ultra-processed foods and potential confounders with elevated blood pressure among all adults regardless of a history of physician-diagnosed hypertension