Abstract
Background:
Distal biceps tendon tears can cause weakness and fatigue with activities requiring elbow flexion and supination. Surgical management of chronic tears (>21 days) is not well described in the literature.
Purpose:
To determine the clinical outcomes of chronic distal biceps repairs and reconstructions.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
We performed a search of Medline (PubMed and Ovid), EMBASE, CINAHL physical therapy, Cochrane Database of Systematic Reviews and Central Register of Controlled Trials, and PubMed Central from inception until September 29, 2020, to identify articles on chronic distal biceps ruptures. The inclusion criteria were studies with at least 1 outcome measure and 10 patients with chronic distal biceps ruptures treated surgically. The quality of the included studies was assessed with the methodological index for nonrandomized studies (MINORS) score. Functional outcomes and complications were reviewed.
Results:
A total of 12 studies were included after systematic database screenings. The MINORS scores ranged from 5 to 19. There were a total of 1704 distal biceps ruptures, of which 1270 were acute and 434 were chronic. Average follow-up time was 12 months to 5.1 years. Single-incision (n = 3), 2-incision (n = 2), or both (n = 6) surgical techniques were used in these studies. Four studies described the use of autografts, and 4 articles used allografts in the chronic repair. Range of motion, function, and strength outcomes were similar when compared with the contralateral arm. Pain was reduced to minimal levels. Main postoperative complications were of paresthesia (specifically to the lateral antebrachial cutaneous nerve), which were temporary in 69.1% of cases.
Conclusion:
The results of this review indicate that surgical management of chronic distal biceps ruptures demonstrates improvement in outcomes including pain reduction and functional ability. Although there may be a slightly higher immediate complication rate, the functional outcomes remain comparable with those seen in the patient population with acute distal biceps.
Keywords: chronic distal biceps ruptures, clinical outcomes, reconstruction, repair, surgical management
Operative repair of acute distal biceps tendon ruptures has been shown to result in improved elbow flexion and supination strength when compared with nonoperative management. 22 However, with reconstruction of chronic distal biceps tendon ruptures, the proportion of patients that achieved 90% strength of the contralateral limb after reconstruction is reportedly 65% for peak supination torque and 62% for peak flexion torque. 5
Data from a large US private-payer insurance provider (PearlDiver Patient Record Database; PearlDiver Technologies) identified that chronic distal biceps tendon rupture repairs (using the International Classification of Diseases, Ninth Revision, Clinical Modification code 727.69) account for 19% of all distal biceps tendon repairs. 26
Several studies have reported on the outcomes of surgical management of acute distal biceps injuries. However, there is a paucity of literature reporting outcomes after surgical treatment of chronic distal biceps ruptures. A recent study comparing acutely treated distal biceps ruptures with chronic distal biceps ruptures has shown a higher complication rate in the latter. 8 At least 90% of the complications in the chronic group were transient paresthesias. 8 Another study demonstrated successful outcomes of long-delayed (4 years) reconstruction of a distal biceps tendon rupture; however, article was a single case report. 11 We not only have limited patient numbers but also a large knowledge gap pertaining to surgical management of chronic distal biceps ruptures.
Distal biceps ruptures have been classified as chronic anywhere from 2 to 6 weeks after injury. Here, we define chronic distal biceps ruptures as rupture persisting beyond 21 days of injury, as described previously. 9 The significant variability in defining chronicity is a direct result of the lack of literature on this topic. Our rationale in choosing 21 days to define “chronic” was not only based on previously seen definitions but also because the complication rate variability between chronic and acute ruptures were already apparent at that time point. 8
Currently, there is no systematic review of the literature evaluating outcomes after chronic distal biceps repair or reconstruction. Counseling patients on outcomes and complications of chronic distal biceps injuries is difficult. The primary purpose of this systematic review was to evaluate functional outcomes in patients undergoing surgical treatment of chronic distal biceps ruptures. It was hypothesized that overall outcomes are successful when managing chronic distal biceps ruptures surgically, which yields an acceptable complication profile.
Methods
Identification of Studies
A systematic review was conducted according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) checklist. 12 This protocol was registered with PROSPERO (international prospective register of systematic reviews). 16 A literature search was conducted using Medline (PubMed and Ovid), EMBASE, CINAHL physical therapy, Cochrane Database of Systematic Reviews and Central Register of Controlled Trials, and PubMed Central. The search terms used in the Ovid Medline search are provided in Appendix Table A1. All databases were searched from their inception, except Medline, which was searched from 1946 onward owing to online availability, until September 29, 2020. All studies evaluating chronic distal biceps tendon tears were identified.
Eligibility Criteria
We included all studies on human participants undergoing repair and reconstruction of chronically ruptured distal biceps tendons. Chronicity was defined as a delay from rupture to 21 days or more. Studies had to be written in or translated into the English language, involve at least 10 patients, and have 1 or more postoperative outcome measures presented.
Exclusion criteria included revision surgery, partial tears of distal biceps tendon, presentations of acute ruptures, 12 months or less of follow-up, technique articles, review articles, non-full text articles, conference papers, cadaveric studies, and biomechanical studies.
Studies that included both acute and chronic distal biceps tendon ruptures were included only if they included a subgroup analysis that contained a minimum of 10 patients in the chronic cohort.
Data Extraction
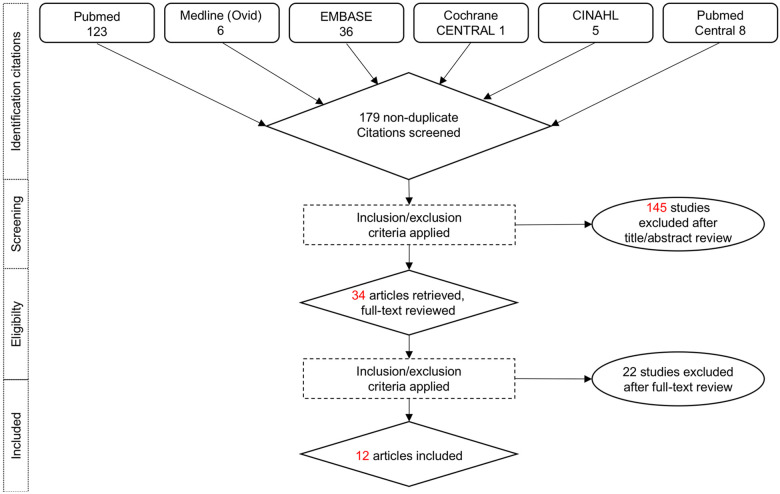
Figure 1 outlines the search process. We identified 179 nonduplicate citations. There were 123 articles in PubMed, 6 in Medline, 36 in EMBASE, 1 in Cochrane CENTRAL, 5 in CINAHL, and 8 in PubMed Central. To be as complete as possible, multiple databases were chosen, given the limited number of publications reporting on chronic distal biceps ruptures.
Figure 1.
Search process in flow diagram using PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines.
A review of titles, abstracts, and full articles was completed by 2 independent reviewers (A.B., M.J.K.S.). Any disagreements were resolved by a third independent reviewer (P.L.). After the title and abstract review, a total of 34 articles were retrieved for full-text review (Figure 1). Ultimately, a total of 12 articles qualified for final analysis and inclusion in this systematic review. #
Level of Evidence
To assess study quality, 2 authors(A.B., M.J.K.S.) applied the methodological index for nonrandomized studies (MINORS) criteria to each publication, as per the protocol outlined by Slim et al. 24 The MINORS criteria is a validated instrument to assess the methodological quality of nonrandomized surgical studies, whether comparative or noncomparative. This instrument contains 12 items, where the first subscale of 8 items is related to noncomparative studies and all 12 items are relevant to comparative studies. Each item is assigned either 0, 1, or 2 points where 0 indicates the item was not reported in the study, 1 indicates it was partially reported, and 2 that it was reported adequately. An ideal score is 16 for noncomparative studies and 24 for comparative studies. 24
Results
Study and Quality Assessment
Of the 12 included studies, 10 were full-length original research articles that could be further subdivided into 6 retrospective reviews 1,13,20,21,23,26 and 4 case series 6,18,25,27 ; 2 research articles 4,15 were retrospective cohort studies with control groups. All studies were performed in a retrospective manner. There were 2 studies with level 3 evidence 4,15 and 10 studies with level 4 evidence. ** MINORS criteria scores ranged from 5 to 12 for the noncomparative studies and 16 to 19 for comparative studies (Table 1).
TABLE 1.
Summary of Study Designs, Level of Evidence, and Methodologic Weaknesses a
| Lead Author (Year) | Data Collection | Data Abstraction | Comparative Group | MINORS Score | Study Design (LOE) | Methodologic Weakness |
|---|---|---|---|---|---|---|
| Alech-Tournier (2019) 1 | Retrospective | Retrospective | No | 10 | Case series (4) | Changed fixation angle in chronic cases from 60° to 90° |
| Frank (2019) 4 | Retrospective comparative | Retrospective | Yes | 19 | Cohort (3) | Several patients lost to follow-up; no preoperative clinical scores; research assistant not blinded |
| Goyal (2020) 6 | Retrospective | Retrospective | No | 10 | Case series (4) | No preoperative scores; analysis not differentiated between surgical techniques |
| Morrell (2012) 13 | Retrospective | Retrospective | No | 8 | Case series (4) | Not all patients had strength testing; ROM and complications were the only consistent outcome measures for all patients; lacking methodological details |
| Morrey (2014) 15 | Retrospective comparative | Retrospective | Yes | 16 | Cohort (3) | Poor postoperative outcome measures (MEPS and ROM), satisfaction, return to work; stratified according to flexion fixation and not chronicity |
| Phadnis (2016) 18 | Prospective | Retrospective | No | 12 | Case series (4) | Incomplete preoperative scores (11/21 preoperative quickDASH) |
| Rantanen (1999) 20 | Retrospective | Retrospective | No | 10 | Case series (4) | No PROMs; multiple surgical techniques used but analysis not stratified accordingly |
| Ryhänen (2006) 21 | N/A | Retrospective | No | 8 | Case series (4) | Data collection not reported (retrospectively or prospectively); no PROMs; main focus on strength and ROM |
| Samra (2020) 23 | Retrospective | Retrospective | No | 10 | Case series (4) | Focus on imaging (retraction distance of distal biceps tendon); less clinically oriented; subgroup analysis excluded long-term tears (>7 wk); chronic defined as >4 wk |
| Snir (2013) 25 | Retrospective | Retrospective | No | 8 | Case series (4) | Strength and a few PROMs collected; strength testing was not objective |
| Wang (2016) 26 | Retrospective | Retrospective | No | 5 | Case series (4) | Database study using CPT codes; focus on complications only |
| Zeman (2020) 27 | Retrospective | Prospective | No | 11 | Case series (4) | Bias of examiner evaluating the strength |
a CPT, Current Procedural Terminology; LOE, level of evidence; MEPS, Mayo Elbow Performance Score; MINORS, methodological index for non-randomized studies; N/A, not available; PROM, patient-reported outcome measure; quickDASH, shortened version of Disabilities of the Arm, Shoulder and Hand; ROM, range of motion.
Demographic Characteristics
A total of 1704 distal biceps tendon ruptures were identified; however, only 434 were chronic (>21 days until repair) distal biceps tendon ruptures (Table 2). Most published studies consisted of analysis of between 10 and 46 patients. The single exception was a database study that evaluated 1443 distal biceps tendon repairs (235 chronic versus 1208 acute tears). 26 Excluding this study, the average sample size was 18.1 patients. Of 434 patients, 9 were female. Average follow-up times ranged from 12 months to 5.1 years (in-office and out-of-office combined) (Table 2).
TABLE 2.
Summary of Patient and Surgery Characteristics a
| Study | Patients | Chronic/Acute Tears, n b | Mean Age (y) | Follow-up (mean ± SD or range) (mo; unless stated differently) | Fixation Method (n) | Graft Type (n) |
|---|---|---|---|---|---|---|
| Alech-Tournier (2019) 1 | 38 | 13/25 | 49.5 | 15 (4-28) | Single incision: endo-osseous (ToggleLoc fixation with ZipLoop technology) | None |
| Frank (2019) 4 | 35 | 35/0 | Primary repair: 49; recon: 46 | 47 ± 25; 45 ± 27 | Delayed direct repair or distal biceps tendon reconstruction with autograft (semitendinosus) | Autograft: semitendinosus (19) |
| Goyal (2020) 6 | 11 | 11/0 | 50 | 46 (10-129) | 3 reconstructions using 1-incision technique with EndoButton, 8 patients with 2-incision technique with transosseous sutures of bone bridge with allograft | Allograft: semitendinosus (8) |
| Morrell (2012) 13 | 12 | 12/0 | 42 | 14.5 (1.5-66) | Distal biceps tendon reconstruction with autograft and suture anchor attachment at radial tuberosity | Autograft: fascia lata (12) |
| Morrey (2014) 15 | 46 | 19 (60° flex), 18 (<30° flex)/4 (60° flex), 5 (<30° flex) | 60° flex: 50 (range, 33-67)/<30° flex: 48 (range, 30-63) | >12 | 2-incision technique: Krakow Locking-stitch through tendon and transosseous suture ties at radial insertion | Allograft: Achilles tendon (1) |
| Phadnis (2016) 18 | 21 | 21/0 | 44 | 15 (6-35) | 2-incision technique, Achilles tendon allograft, Pulvertaft weave and tendon wrap, transosseous Endobutton fixation | Allograft: Achilles tendon (21) |
| Rantanen (1999) 20 | 19 | 10/9 | 43 | 5.1 y (2-11) | 2-incision technique of Boyd and Andersen (12); single-incision technique (7). Transosseous fixation using suture ties for all, except 4 cases (all single-incision technique) used suture anchors. | Autograft: fascia lata (augmentation) (1) |
| Ryhänen (2006) 21 | 16 | 11/5 | 41 | 31 | Anatomic reattachment using bone anchors | Autograft: palmaris longus (1), tensor fasciae latae (2) |
| Samra (2020) 23 | 24 | 10/14 | 45.2 (SD, 7.8) | 47.6 ± 24.9 (13-81) | Single-incision technique with 2 anchor fixations at radial tuberosity, or LARS | Synthetic augmentation: LARS (2) |
| Snir (2013) 25 | 18 | 18/0 | 46.9 | 9.3 (4-14) in office, 21 (7-69) out of office | Single-incision (16) or 2-incision (2) technique; radial tuberosity: cortical button (10); suture (2); Endobutton (6) | Allografts: Achilles (15), semitendinosus (1), gracilis (1), tibialis anterior (1) |
| Wang (2016) 26 | 1443 | 235/1208 | 72% 40-59 | 12 | Radial tuberosity was preferred (95%) over tenodesis to the brachialis (5%) | Unknown |
| Zeman (2020) 27 | 21 | 21/0 | 52 | 26 | Single transverse incision with suture button armed 2 nonabsorbable no. 2 core sutures | 0 |
a flex, flexion; LARS, ligament augmentation and reconstruction system; recon, reconstruction.
b Chronic tear, ≥21 d; acute tear, <21 d.
Fixation Methods
Use of single-incision techniques with transosseous button fixation methods 1,6,25,27 and suture anchor fixation methods at the radial tuberosity 13,19,23 were seen most commonly. Tenodesis to the brachialis tendon/muscle was also performed in 1 study. 26 In addition, a 2-incision technique was described using transosseous suture fixation and 4 different graft fixation methods were described (Table 2).
Graft Choice
Grafts were used in 85 cases. Three of the studies used grafts in all their cases, 13,18,25 but 6 other studies reported the use of a graft only when a direct repair (contact of the distal biceps tendon to the tuberosity) was not possible. 4,6,15,20,21,23 Three studies did not use a graft at all. 1,26,27 Excluding 1 study with 235 cases that did not report repair technique, 26 37.4% (85 of 227) of all surgically treated chronic distal biceps ruptures used a graft. Four studies described the use of autografts. 4,13,20,21 Autografts were obtained from either the fascia lata (n = 15), the semitendinosus (n = 19), or the palmaris longus (n = 1) (Table 2). Allografts were used instead in 4 studies. 6,14,18,25 The most common allograft was the Achilles tendon (n = 37) followed by semitendinosus (n = 9), tibialis anterior (n = 1), and gracilis (n = 1) tendons. One study described the use of a synthetic augmentation graft (n = 2). 23
Functional Outcome Scores
Outcome scores are summarized in Table 3. Range of motion (ROM) was collected in all studies. Postoperative results of ROM demonstrated return of full extension, flexion, supination, and pronation when compared with the contralateral side. Strength testing was described in 9 of 12 articles. 1,4,6,13,15,21,23,25,27 However, the methods of measuring strength varied widely, from observer resistance testing on the operated arm (n = 1) and comparison of the contralateral arm (n = 7) to objective machine testing (n = 1). Nonetheless, strength tests demonstrated good-to-excellent postoperative improvements for flexion and supination strength. Clinical outcome measures were not performed in every study and varied among research groups.
TABLE 3.
Summary of Outcomes a
| Chronic Tears | |||
|---|---|---|---|
| Study | Functional Scores [mean ± SD (range)] | Further Stratification by Current Authors | ROM + Strength |
| Alech-Tournier (2019) 1 | VAS pain, 1.32 (0-8); MEPI, 93.4 (50-100); quickDASH, 4.16 (0-75; SEV, 85 (40%-100%) | 13 chronic: VAS pain, 1; MEPI, 91.92; quickDASH, 14.86; SEV, 82.92% | ROM (133.08° arc); supination strength ratio, 75.08% |
| Frank (2019) 4 | PREE, 4 ± 4 (14 ± 19); DASH, 3 ± 5 (7 ± 10); MEPI, 95 ± 7 (86 ± 14); SANE, 93 ± 10 (88 ± 14) | All patients chronic | ROM n/a at follow-up, supination strength (% of uninjured side): –78 in both study and control; flexion strength: 90% study vs 89% control group |
| Goyal (2020) 6 | Strength and endurance (flexion, supination); ROM (no difference between affected and unaffected arm); DASH, 5.8 (range 0-24.2); MEPS, 97.3 (range 70-100); satisfaction, 9.4 of 10 (range 7-10); return to work, 11.4 mo | All patients chronic; DASH, 5.8; VAS pain, 0.6; MEPS, 97.3 | ROM (no loss of flexion/extension/pronation/supination) compared with contralateral side; strength % peak flexion –12, peak supination –23, flexion endurance –5, supination endurance +4 |
| Morrell (2012) 13 | ROM; strength (flexion, supination) | Not applicable | ROM (126° arc) flexion/extension (167° arc) pronation/supination; 5/12 patients tested for strength revealed 86% of flexion strength, 4/12 patients tested for supination strength 87% |
| Morrey (2014) 15 | ROM, MEPS, pain, satisfaction, strength (no sign difference between groups) | MEPS, 100 (all patients) | 19 chronic patients repaired at >60° flexion; extension, 2.11°; flexion, 138.16°; pronation, 80.53°; supination, 77.11°; strength assessed between control and study group, no difference |
| Phadnis (2016) 18 | OES, 44.7 (35-48); quickDASH, 4 (0-20.5); MEPS, 92.9 (70-100) | All patients chronic | ROM, full extension, pronation, and supination, no strength |
| Rantanen (1999) 20 | Subjective outcome (4-point Likert scale); return to activity level; ROM; no difference between the 2 groups | 5/10 good, 4/10 excellent, 1/10 fair outcome | ROM not stratified for the 10 chronic patients, no strength testing |
| Ryhänen (2006) 21 | Strength (flexion; supination) | No specific outcomes | Strength for chronic patients (12/16), compared with healthy arm; 84.92% strength recovery at 90° flexion, 76.33% supination strength recovery |
| Samra (2020) 23 | DASH, 2.5 (range 0-14.2); OES, 47 (40-48); no correlation of tendon retraction distances and outcome scores (DASH and OES); tendon retraction distance | 10 chronic patients with repairs, mean OES (43.8); DASH 7.08; | 8 chronic patients, strength supination OES (5, for 8 people); strength flexion OES (5, for 8 people) |
| Snir (2013) 25 | Strength (flexion; supination); MEPS, 92.4; DASH, 7.5 ± 17.9 | 18 patients with adequate follow-up- preop MEPS 43.1 postop 94.2; 18/18 patients preop pain, 4/18 mild chronic pain postop, 1/18 moderate postop; postop DASH 7.5 | mean flexion, 137.2°; extension, 2.5°; pronation, 83.6°; supination, 85.6°; gross strength by surgeon, 4.7/5 for supination and flexion |
| Wang (2016) 26 | — | — | — |
| Zeman (2020) 27 | ROM (full); strength (flexion and supination, 5/5): MEPS, 100; ASES, 97.2; OES, 48; VAS, 0 | ASES, 42 -97 (preop-postop); MEPS, 48-100 (preop-postop); OES, 24-48 (preop-postop); VAS, 4.5-0 (preop-postop) | “Full ROM”: mean ROM, 3° extension; flexion, 132°; pronation, 64°; supination, 71°; strength, 5/5 flexion and supination for all patients at final follow-up |
a ASES, American Shoulder and Elbow Surgeons; DASH, Disabilities of the Arm, Shoulder and Hand; MEPI, Mayo Elbow Performance Index; MEPS, Mayo Elbow Performance Score; n/a, not applicable; OES, Oxford Elbow Score; postop, postoperative; PREE, Patient-Rated Elbow Evaluation; preop, preoperative; quickDASH, shortened version of Disabilities of the Arm, Shoulder and Hand; ROM, range of motion; SANE, Single Assessment Numeric Evaluation; SEV, Subjective Elbow Value; VAS, visual analog scale; Dashes indicate not reported.
Postoperative Complications
The most prevalent postoperative complications included paresthesia or neuropraxia of the lateral antebrachial cutaneous nerve (LABCN; n = 39; 8.9%), the radial nerve (n = 7; 1.6%), posterior interosseous nerve (n = 4; 0.9%), and superficial radial cutaneous nerve (n = 4; 0.9%). Most nerve injuries were temporary (n = 38; 69.1%) with resolution within 3 to 6 months, versus 17 permanent injuries (30.9%). The rate of tendon reruptures was reported to be 0.7% according to 3 studies. 4,15,21 The database study by Wang et al 26 recorded a 5.4% rerupture rate, but the authors did not differentiate between acute and chronic cases. Other reported complications included heterotopic ossification (HO) (n = 4; 0.9%) and cosmetic deformities of biceps contour (n = 17; 3.9%) (Table 4).
TABLE 4.
Summary of Complications a
| Study | Complications in Chronic Tears | Paresthesia/Neuropraxia | Other Complications |
|---|---|---|---|
| Alech-Tournier (2019) 1 | No HO and 7 neuropraxias LABCN with 3 persistent | LABCN 17 (10 T; 7 P) | 4 HO (acute tears) |
| Frank (2019) 4 | All patients chronic | LABCN (3 T; 3 P) | 1 rerupture after trauma with reconstruction |
| Goyal (2020) 6 | All patients chronic | LABCN (1 T) | No complications: only coincidental finding of 1 cubital tunnel syndrome with diminished ulnar hand and forearm sensation |
| Morrell (2012) 13 | All patients chronic | Superficial radial cutaneous nerve (4 T) | 1 wound dehiscence; all small thigh bulge due to muscle herniation (hardly noticeable) |
| Morrey (2014) 15 | LABCN ×2, 1 rerupture (in high flexion group) | >60° flexion: LABCN (3 T) <30° flexion: LABCN (1 T); radial nerve palsy (3 T) |
1 rerupture after trauma with reconstruction |
| Phadnis (2016) 18 | All patients chronic | LABCN (2 T) | Extension deficit lag in 2 patients |
| Rantanen (1999) 20 | Not reported | LABCN (2 T) | — |
| Ryhänen (2006) 21 | 1 limited pronation, 1 reoperation, 2 LABCN (T), 1 radial nerve (T); no complications in acute patients | LABCN (2 T); radial nerve (1 T) | 1 patient had 2 reoperations (1 rerupture, revision too stretched) |
| Samra (2020) 23 | 3/8 chronic patients with altered LABCN sensation, 1/8 PIN palsy, 1/8 superficial infection | LABCN (6 P); PIN (2 T) | — |
| Snir (2013) 25 | All patients chronic | PIN (2 T) | Cosmetic deformity in all but 1 patient, but acceptable for all |
| Wang (2016) 26 | — | n/a | Rerupture 5.4%; revision for acute 5.1% and chronic 7.0%; infection 1.1% and peripheral nerve injury 0.6% |
| Zeman (2020) 27 | All patients chronic | Radial nerve (2 T; 1 P) | No reruptures, no contractures, no synostoses, no infections |
a HO, heterotopic ossification; LABCN, lateral antebrachial cutaneous nerve; n/a, not applicable; P, permanent; PIN, posterior interosseous nerve; T, temporary; Dashes indicate not reported.
Reconstructions
In their autograft comparison study, Frank et al 4 demonstrated that the Patient-Rated Elbow Evaluation (PREE) and Mayo Elbow Performance Index (MEPI) were statistically better in the repair group compared with the reconstruction cases. However, final follow-up showed no differences in ROM, supination, and elbow flexion strength (with the use of a dynamometer for the ROM and elbow flexion strength), with similar complication rates. Goyal et al 6 demonstrated that their biceps reconstructions with allograft showed no significant differences in endurance for supination and flexion strength compared with the nonoperated arm, but peak strength for flexion (−12%) and supination (−26%) were decreased, the latter significantly. This was somewhat different from what was reported by Snir et al, 25 who evaluated strength a little more subjectively in their group of allograft reconstructions. Supination and flexion strength testing were evaluated by the surgeon and were averaged to be 4.7 out of 5 for both.
Discussion
Six articles identified in our systematic review of the published literature presented outcomes on chronic distal biceps repairs and reconstructions alone, 4,6,13,18,25,27 whereas the other 6 articles presented outcomes on both acute and chronic distal biceps repairs. 1,15,20,21,23,26 Single- and 2-incision techniques were used for the approach. Three studies used grafts for all their reconstructions, 13,18,25 while primary anatomic repair was achieved in 8 studies. 1,4,6,15,20,21,23,27 If a primary repair was not possible, a reconstruction was performed using a tendon graft. Postoperative ROM and strength tests were almost symmetric to the contralateral side. The most common complications were paresthesia or neuropraxia of surrounding nerves, which were mostly temporary (69.1%) and resolved after 3 to 6 months.
An important concern in chronic distal biceps ruptures is their difference in management based on direct repair versus reconstruction. Frank et al 4 compared direct repair with reconstruction of chronic distal biceps tendon ruptures. Although similar strength, ROM, and complication rates were found among both groups, the direct repair group reported better functional outcome scores. 4 No other study in our systematic review looked at direct repair versus reconstruction of chronic distal biceps tears. The cases had excellent functional outcome scores, in keeping with the observations (Disabilities of the Arm, Shoulder and Hand [DASH], 5 and 3; MEPI, 95 and 86; and PREE, 4 and 14, for delayed repair and reconstruction, respectively) of Frank et al. 4
Of the 6 articles that included only chronic patients, 4 presented data on patients undergoing allograft or autograft reconstructions. 6,13,18,25 The patient-reported outcome measures (PROMs) demonstrated consistently significantly improved results in chronic ruptures that underwent reconstruction.
A caveat of this recommendation would be to avoid autograft reconstruction, which consistently resulted in donor-site complication without demonstrating better functional outcomes in their patients. 13 Overall, however, complications (eg, neuropraxia, cosmetic deformities, rerupture, and HO) were similar in all studies. Further, it should be noted the article by Phadnis et al 18 was the only publication to truly have “chronic” ruptures, with the average time of treatment being 25 months postinjury versus what we have seen as “chronic” in the other articles.
Of the 6 articles reporting on both acute and chronic repairs, 1 presented data comparing high flexion and low flexion of the elbow at time of repair. 15 Despite the difference in elbow fixation position, there were no significant differences between both groups for ROM, strength, return to work, patient satisfaction, and complications (P = .53). Another article was a database study, 26 which provided information on revision rates. This latter study reported a 7% revision rate for chronic repairs and a 5.1% revision rate for acute repairs, but this was not statistically significant (P = .36). 15,26
Of the 6 articles in this group, 4 demonstrated similar outcome results between acute and chronic repairs. 1,20,21,23 Alech-Tournier et al 1 demonstrated excellent outcomes in both chronic and acute direct repairs; however, it was the only study out of 14 that reported 4 cases of HO, all of which occurred in the acute repair group (<9 days to surgery) using a single-incision technique. In their study, 17 patients (44.7%) had postoperative episodes of LABCN paresthesia, which was a much higher rate than that seen in other studies in this review. The other 3 articles demonstrated good outcomes with unlimited use of the operated arm, return to work, muscle strength, and PROMs (DASH and Oxford Elbow Score [OES]) for their chronic repairs (which included a mixture of reconstruction and repair). 20,21,23
Reconstruction and repair of chronic distal biceps ruptures presents a challenge for the orthopaedic surgeon. Direct repair can be technically difficult if there is a significant delay before surgery. The tendon can shorten, retract, atrophy, and scar to adjacent tissue. A number of early complications following direct repair of chronic distal biceps ruptures include nerve injury, HO, and radioulnar synostosis. 3,9,10 Despite these potential complications, many studies have shown similar longer term functional outcomes when comparing acute repair with chronic cases that are treated after 21 days. 2,8,15 In this systematic review, no patients with chronic distal biceps ruptures were reported to have developed radioulnar synostosis or HO. Four patients with an acute tear had an HO.
ROM and strength are important outcome parameters of surgical management and for patient satisfaction. However, assessment of strength varied between studies. When pooling the information from all studies in our systematic review that provided comparative strength outcomes, postoperative strength remained greater than 75% for supination and greater than 85% for flexion, as compared with the nonoperative arm. Of the 12 studies, 6 did not report ROM results 4,6,20,21,23,26 ; however, those that reported on ROM did not reveal any significant limitation of flexion, extension, supination, or pronation. In addition, Morrey et al 15 looked at repair of retracted distal biceps tendon ruptures affixed with the elbow in extreme flexion (>60°), in which most tears were chronic, versus a matched control group with primary tendon repair where flexion of the elbow was ≤30°, and showed no difference in strength or ROM at final follow-up.
Six studies used either the shortened version of the DASH (quickDASH) or DASH, 1,4,6,18,23,25 with scores ranging from 3 to 14.86 for chronic patients. As scores closer to zero imply no disability, 7 the findings suggest that patients with chronic ruptures have a relatively low disability profile. Seven studies used the MEPI/Mayo Elbow Performance Score, 1,4,6,15,18,25,27 with scores greater than 90 again revealing a high level of satisfaction and function. The visual analog scale pain score was used in 3 studies, 1,6,27 with results demonstrating minimal pain in patients with chronic tears. The OES was used in 3 studies. 18,23,27 Other scores used included Subjective Elbow Value, Single Assessment Numeric Evaluation, and PREE. Synthesizing the available PROM scores, patients with chronic tears had a relatively low disability profile, minimal pain, and a high level of satisfaction and function. This review suggests that patients tend to do well overall with repair or reconstruction when treated surgically after 21 days.
Complications were available for 199 patients in this review (as the remaining 235 patients were pooled from the database study by Wang et al 26 ). Of 199 patients, there were 3 reruptures, 24 transient nerve palsies of the LABCN/superficial radial nerve (SRN) and 16 patients with permanent LABCN/SRN paresthesia/neuropraxia. Two other patients also had transient LABCN sensory deficit; however, it was unclear whether these patients were from the chronic or acute rupture group. 20 Further, 7 transient and 1 permanent radial nerve palsy were recorded. Panagopoulos et al 17 published a systematic review of acute distal biceps ruptures. In their review, 8.6% of cases developed transient LABCN neuropraxias, 3.8% developed posterior interosseous nerve palsies, and 1.3% had persistent SRN palsies. This resulted in a total of 14.2% neurologic complications following fixation of acute distal biceps ruptures. In our review, excluding the study of Wang et al, 26 15.4% of patients had a neurologic complication.
With respect to HO, no patients with chronic tears but 4 with acute tears were reported to have developed this complication in the study population. Of 199 patients that had a chronic repair or reconstruction of their distal biceps, 3 reruptures were seen. The database study by Wang et al 26 published information showing a revision rate for rerupture of 7% in chronic distal biceps tendon repairs and 5% in acutely treated repairs. This is more than the rate of 1.5% calculated when pooling our review data. A reason for the greater number of reported reruptures in the database study can be that they collected data by patients having revision surgery, 26 therefore making their study potentially less susceptible to underreporting of this complication as in other studies.
Limitations
The major limitation of this review is the variability in treatment between studies. First, there was no consistent surgical approach used across all studies. Second, the fixation method was variable and included Endobutton, interference screw, a combination of both, and transosseous repair with sutures. Third, repairs were either direct or via reconstruction with use of allograft or autograft. Finally, standardized outcome measures used in the evaluation of distal biceps repairs are not rigorous or consistent. Of the 12 studies in this systematic review, 8 provided functional scores, 3 others provided only ROM and/or strength information, and 1 of 12 provided complication information only.
Every study included in this systematic review had a small number of patients, other than the database study by Wang et al. 26 All articles had an evidence level of 3 or 4. Although all studies had the same indication for surgery, the variability seen in surgical technique, postoperative protocol, and evaluation differed, making direct comparisons difficult. We did not restrict studies based on follow-up times. This can cause certain later complications (eg, HO or ROM deficits) to not fully come to fruition, which will skew complication type depending on studies' follow-up period. Chronic distal biceps rupture definition was a rupture of the named tendon more than 21 days after injury. Other options to classify chronic distal biceps ruptures are based on level of retraction and need for reconstruction with a tendon graft.
Conclusion
This systematic review demonstrated overall successful outcomes after chronic distal biceps repairs and reconstruction. The functional outcomes after surgery of chronic distal biceps ruptures are comparable with those reported in the patient population who have undergone acute distal biceps repair. It appears that authors generally prefer primary fixation to graft repair even at an extreme angle of attachment. Fixation of chronic distal biceps injuries may have a higher immediate complication rate, specifically neuropraxia of the LABCN.
APPENDIX
Table A1.
OVID MEDLINE Search
| 1 | (distal adj5 bicep*).ti, ab. |
| 2 | (distal bicep* or distal tendon* or distal attachment* or distal insertion* or distal end*).ti, ab. |
| 3 | 1 and 2 |
| 4 | exp Chronic Disease/ or exp Time-To-Treatment/ or exp Delayed Diagnosis/ |
| 5 | (chronic* or persist* or refractor* or intractab* or incessan* or neglect* or delay*).ti, ab. |
| 6 | 3 and (4 or 5) |
| 7 | Rupture/ or exp Rupture, Spontaneous/ |
| 8 | (rupture* or ruptura tendinea or tendon disruption).ti, ab. |
| 9 | 6 and (7 or 8) |
| 10 | (tear* and (complete* or full thickness or grade iii or full width)).ti, ab. |
| 11 | avuls*.ti, ab. |
| 12 | 6 and (10 or 11) |
| 13 | (repair* or reattach* or reinsert* or reconstruct* or revis*).ti, ab. |
| 14 | 6 and 13 |
| 15 | 9 or 12 or 14 |
Footnotes
Final revision submitted August 2, 2021; accepted September 10, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: J.M.L. has received teaching fees from Arthrex. T.J.G. has received teaching fees from Acumed and ConMed Linvatec. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Alech-Tournier F, Elkholti K, Locquet V, et al. Outcomes of distal biceps tendon reattachment using the ToggleLoc fixation device with ZipLoop technology with single mini-open technique. Eur J Orthop Surg Traumatol. 2019;29(4):925–931. [DOI] [PubMed] [Google Scholar]
- 2. Bosman HA, Fincher M, Saw N. Anatomic direct repair of chronic distal biceps brachii tendon rupture without interposition graft. J Shoulder Elbow Surg. 2012;21(10):1342–1347. [DOI] [PubMed] [Google Scholar]
- 3. Cohen MS. Complications of distal biceps tendon repairs. Sports Med Arthrosc Rev. 2008;16(3):148–153. [DOI] [PubMed] [Google Scholar]
- 4. Frank T, Seltser A, Grewal R, King GJW, Athwal GS. Management of chronic distal biceps tendon ruptures: primary repair vs. semitendinosus autograft reconstruction. J Shoulder Elbow Surg. 2019;28(6):1104–1110. [DOI] [PubMed] [Google Scholar]
- 5. Goetz TJ, Kilb BKJ, Okada M. Strength, endurance and clinical outcomes of chronic distal biceps rupture reconstruction with tendon graft. Orthop Proc. 2016;98-B(suppl 20):82. [Google Scholar]
- 6. Goyal N, Wilson DJ, Salzano MB, et al. Restoration of peak strength and endurance following distal biceps reconstruction with allograft for chronic ruptures. J Shoulder Elbow Surg. 2020;29(4):853–858. [DOI] [PubMed] [Google Scholar]
- 7. Gummesson C, Atroshi I, Ekdahl C. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: longitudinal construct validity and measuring self-rated health change after surgery. BMC Musculoskelet Disord. 2003;4:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Haverstock J, Grewal R, King GJW, Athwal GS. Delayed repair of distal biceps tendon ruptures is successful: a case-control study. J Shoulder Elbow Surg. 2017;26(6):1031–1036. [DOI] [PubMed] [Google Scholar]
- 9. Kelly EW, Morrey BF, O’Driscoll SW. Complications of repair of the distal biceps tendon with the modified two-incision technique. J Bone Joint Surg Am. 2000;82(11):1575–1581. [DOI] [PubMed] [Google Scholar]
- 10. Klonz A, Reilmann H. Biceps tendon: diagnosis, therapy and results after proximal and distal rupture. Article in German. Orthopade. 2000;29(3):209–215. [DOI] [PubMed] [Google Scholar]
- 11. McCarty LP III, Alpert JM, Bush-Joseph C. Reconstruction of a chronic distal biceps tendon rupture 4 years after initial injury. Am J Orthop (Belle Mead NJ). 2008;37(11):579–582. [PubMed] [Google Scholar]
- 12. Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and Meta-Analysis Protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Morrell NT, Mercer DM, Moneim MS. Late reconstruction of chronic distal biceps tendon ruptures using fascia Lata autograft and suture anchor fixation. Tech Hand Up Extrem Surg. 2012;16(3):141–144. [DOI] [PubMed] [Google Scholar]
- 14. Morrey BF, Askew LJ, An KN, Dobyns JH. Rupture of the distal tendon of the biceps brachii. A biomechanical study. J Bone Joint Surg Am. 1985;67(3):418–421. [PubMed] [Google Scholar]
- 15. Morrey ME, Abdel MP, Sanchez-Sotelo J, Morrey BF. Primary repair of retracted distal biceps tendon ruptures in extreme flexion. J Shoulder Elbow Surg. 2014;23(5):679–685. [DOI] [PubMed] [Google Scholar]
- 16. Page MJ, Shamseer L, Tricco AC. Registration of systematic reviews in PROSPERO: 30,000 records and counting. Syst Rev. 2018;7(1):32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Panagopoulos A, Tatani I, Tsoumpos P, et al. Clinical outcomes and complications of cortical button distal biceps repair: a systematic review of the literature. J Sports Med (Hindawi Publ Corp). 2016;2016:3498403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Phadnis J, Flannery O, Watts AC. Distal biceps reconstruction using an Achilles tendon allograft, transosseous endobutton, and Pulvertaft weave with tendon wrap technique for retracted, irreparable distal biceps ruptures. J Shoulder Elbow Surg. 2016;25(6):1013–1019. [DOI] [PubMed] [Google Scholar]
- 19. Rampoldi M, Ascani C. Chronic biceps distal tendon ruptures: is primary repair still possible? J Orthop Traumatol. 2014;15(suppl 1):30. [Google Scholar]
- 20. Rantanen J, Orava S. Rupture of the distal biceps tendon. A report of 19 patients treated with anatomic reinsertion, and a meta-analysis of 147 cases found in the literature. Am J Sports Med. 1999;27(2):128–132. [DOI] [PubMed] [Google Scholar]
- 21. Ryhänen J, Kaarela O, Siira P, Kujala S, Raatikainen T. Recovery of muscle strength after late repair of distal biceps brachii tendon. Scand J Surg. 2006;95(1):68–72. [DOI] [PubMed] [Google Scholar]
- 22. Safran MR, Graham SM. Distal biceps tendon ruptures: incidence, demographics, and the effect of smoking. Clin Orthop Relat Res. 2002;(404):275–283. [PubMed] [Google Scholar]
- 23. Samra I, Mati W, Blundell C, Lane S, Charalambous CP. Distal biceps tendon ruptures---the relation of radiological retraction and chronicity to the ability of tendon reattachment and long-term functional outcomes. J Orthop. 2020;20:111–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Slim K, Nini E, Forestier D, et al. Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. [DOI] [PubMed] [Google Scholar]
- 25. Snir N, Hamula M, Wolfson T, et al. Clinical outcomes after chronic distal biceps reconstruction with allografts. Am J Sports Med. 2013;41(10):2288–2295. [DOI] [PubMed] [Google Scholar]
- 26. Wang D, Joshi NB, Petrigliano FA, et al. Trends associated with distal biceps tendon repair in the United States, 2007 to 2011. J Shoulder Elbow Surg. 2016;25(4):676–680. [DOI] [PubMed] [Google Scholar]
- 27. Zeman CA, Mueller JD, Sanderson BR, Gluck JS. Chronic distal biceps avulsion treated with suture button. J Shoulder Elbow Surg. 2020;29(8):1548–1553. [DOI] [PubMed] [Google Scholar]