Abstract
In Ethiopia, locally available materials, mainly medicinal plants, are commonly utilized to manage livestock diseases. However, this practice is currently being threatened by several factors including loss of traditional knowledge and depletion of plant resources. This calls for an urgent need to document the ethnoveterinary knowledge in the country and conserve the associated medicinal plants. The purpose of this study was, therefore, to document traditional knowledge on use of medicinal plants in the Adea Berga district, Oromia region of Ethiopia, to manage livestock ailments. Ethnobotanical data were collected largely through semistructured interviews conducted with purposively selected traditional healers of the district. The study identified 59 medicinal plants used in ethnoveterinary practices in the district. The great majority (90.4%) of the medicinal plants were used in fresh forms, which were mainly administered orally. The majority (65.4%) of the medicinal plants were gathered from the wild. Data revealed that yoke sore (wound) had the highest informant consensus factor (ICF) value (1.00), followed by leech infestation (0.92) and endoparasite infections (0.90). The highest fidelity level (FL) (100%) and rank order priority (ROP) (100%) values were obtained for the plants Nicotiana tabacum, Malva parviflora, and Calpurnia aurea that were used to treat leech infestation, retained placenta, and snake poisoning, respectively. Priority for further pharmacological and phytochemical investigations needs to be given to the aforementioned three plants with the highest FL and ROP values as such values may indicate their higher potency against the respective ailments.
1. Introduction
Ethiopia is one of the leading countries in the world and the first in Africa in terms of livestock population. However, livestock productivity is far below the possible expectations and, as a result, the country could not fulfill its local demands and hence imports animal products from other countries. One of the major challenges of livestock production in the country is the high prevalence of different diseases affecting domestic animals [1]. As most modern drugs are expensive and not affordable for the majority of Ethiopian farmers and pastoralists, disease control measures largely depend on traditional medicine, which mainly involves the use of medicinal plants [2]. According to estimate of Abebe and Ayehu [3], 95% of traditional medical preparations in Ethiopia are of plant origin.
However, despite the huge contribution of medicinal plants in the Ethiopian animal healthcare system and rich traditional medical knowledge, little effort has so far been made to properly document ethnoveterinary-related knowledge and conserve the associated medicinal plants in an effort to ensure their better and sustainable uses. As a result, the majority of the knowledge has been left undocumented being exposed to serious depletion due to acculturation and expansion of modern education. It is worth noting that in the Ethiopian traditional medical system, knowledge is handed down from generation to generation largely by word of mouth with little culture of documentation and as a result there is high probability that a portion of it could be lost in the process. The continuation of the practice is also negatively affected by the depletion of medicinal plants used in the system mainly due to agricultural expansion and deforestation. Therefore, there is an urgent need for conducting more ethnoveterinary surveys in different parts of the country to save the traditional knowledge and the associated medicinal plants from further loss.
Some ethnobotanical surveys have so far been conducted in the Oromia region of Ethiopia, including that in Borana [2], Bale Mountains National Park [4], Chiro district [5], the Dabo Hana district of Illubabor zone [6], four districts of Jimma zone [7], selected districts of East Wollega zone [8], Horro Gudurru district [9], Yabelo and Liben districts [10], the Melkabello district of East Hararghe zone [11], the Midakegn district of West Shewa zone [12], Eastern Shewa and Arsi zones [13], Kelem Wollega zone [14], the Dale Sadi district of West Hararghe zone [15], the Berbere district of Bale zone [16], Wolmera district [17], and Ambo district [18], with the purpose of documenting knowledge exclusively focused on medicinal plants used to control livestock ailments. However, to the knowledge of the authors, there is no study conducted in the Adea Berga district to document medicinal plants traditionally used to manage livestock ailments. The purpose of this study was, therefore, to document traditional knowledge on the use of medicinal plants by people in the Adea Berga district, West Shewa zone, the Oromia region of Ethiopia, to manage livestock ailments.
2. Materials and Methods
2.1. Description of Study District
Ethnoveterinary study to document medicinal plants used to manage livestock diseases was conducted in the Adea Berga district, West Shewa zone, the Oromia regional state of Ethiopia. The Adea Berga district is located between 9° 12′ and 9° 37′N latitude and 38° 17′ and 38° 36′E longitude [19] at 70 km west of Addis Ababa and 35 km northwest of the Holeta town. The district shares borders with the Walmera district in the south, Ejerie district in the southwest, Meta Robi district in the west, and the Muger River in the north and east. Enchni is the administrative town of Adea Berga district. The district has altitudes that range between 1371 and 3169 meters above sea level [20]. In the district, rainfall ranges between 800 and 1400 mm and temperature between 10°C and 29°C [19]. The district is divided into 34 administrative subdistricts (kebeles), the smallest administrate unit in Ethiopia.
Human population of the district is estimated to be 184,618, of which 92,277 are males and 92,341 are females (Adea Berga District Health Bureau, unpublished report, 2021). Mixed crop and livestock farming systems are the mode of agriculture in the study area. According to unpublished data from Adea Berga District Livestock and Fisheries Resources Office obtained in 2018, the district is estimated to have 165,317 heads of cattle, 56,800 sheep, 30,092 goats, 72,965 poultry, 14,208 donkeys, and 519 mules. Fascioliasis, pasteurellosis, foot-and-mouth disease (FMD), tick infestation, lice infestation, black leg, African horse sickness, lumpy skin diseases, sheep pox, Newcastle diseases, fowl cholera, and fowl pox are the commonly occurring diseases in the district (Adea Berga District Rural and Agricultural Development Office, unpublished report, 2011).
2.2. Selection of Study Sites and Informants
A reconnaissance survey was conducted in the Adea Berga district in November 2018 with the purpose of identifying study sites and identification of informants. Accordingly, nine subdistricts distributed in three agroecological zones of the district were identified for the study with the recommendation of elders and local authorities. These were Bishaan Diimoo, Kaaloo, Haroo Lemman, Oddoo Modjo, Iluu Kitabaa, Caancoo Birrattee, Adadaa Soddolbee, Iluu Coqorsaa, and Odaa Dalotaa. The elders and local authorities also assisted in the purposive sampling of 63 traditional healers from the nine subdistricts of the Adea Berga district to be involved in interviews.
2.3. Data Collection
Ethnoveterinary survey was conducted between November 2018 and March 2019, and data were mainly collected through semistructured interviews conducted with the selected traditional healers following the method of Martin [21]. The interview was based on a checklist of questions prepared in English and later translated to Afaan Oromoo, the local language in the study district. During interviews, data mainly regarding demographic characteristics of respondents, local name of medicinal plants employed in the practice, plant part used, remedy preparation methods, route of administration, disease treated, dosage regimen, remedy storing options, and habitat of medicinal plants used were gathered.
2.4. Collection, Preparation, and Identification of Plant Specimens
After every interview, walks were made with each informant to gather specimens of the claimed medicinal plants. The collected specimens were properly pressed and dried and later identified by their scientific name with the help of botanists at the Aklilu Lemma Institute of Pathobiology (ALIPB), Addis Abba University (AAU), and the National Herbarium (AAU), and vouchers were deposited in a mini-herbarium at ALIPB.
2.5. Data Analysis
Ethnoveterinary data were tabulated in Microsoft Excel spreadsheets and analyzed using SPSS version 20 software. The most useful information gathered on medicinal plants was summarized using descriptive statistical methods such as frequencies and percentages. The fidelity level (FL) value was computed for every medicinal plant reported by three or more informants, which is a measure of the degree of agreement among informants in the selection of a given medicinal plant to treat a given ailment, an indication of the possible level of efficacy. The fidelity level value was calculated using the formula FL = Ip /Iu × 100, where Ip is the number of informants who reported the utilization of medicinal plants against a specific ailment and Iu is the total number of informants who mentioned the same plant against any ailment [22]. However, plants with similar FL values but known to different numbers of informants may vary in their healing potential. Thus, a correlation index known as relative popularity level (RPL) is additionally needed to be computed, and the rank order priority (ROP) value is determined by multiplying FL value by RPL value to differentiate the healing potential of plants of similar FL values [22, 23]. The RPL values range between 0 and 1. The plants are categorized into “popular” (RPL = 1) and “unpopular” (RPL < 1) groups. In this study, popular plants were those cited by more than half of the highest number of informants who cited a plant against an ailment, which is 27. Accordingly, medicinal plants cited by 14 or more informants were considered popular and were assigned with an RPL value of 1, whereas medicinal plants that were mentioned by less than 14 informants were considered unpopular and were assigned with RPL values less than 1 and were determined by dividing the total number of informants who mentioned the plant against a given ailment by 14.
Informant consensus factor (ICF) values were computed to determine the level of agreement of informants in the district on use of medicinal plants to treat a given ailment category. Informant consensus factor values may help in the selection of medicinal plants for phytochemical and pharmacological studies [24]. Informant consensus factor values were calculated using the formula ICF=(nur − nt)/(nur − 1), where nur is the number of use-reports for a particular use category and nt is the number of taxa used for a particular use category by all informants [25].
3. Results
3.1. Demographic Characteristics of Informants
Out of the total 63 informants who were identified for the interviews, 51 (80.95%) were males and 12 (19.05%) were females. The majority (53.73%) of the informants were illiterate (Table 1).
Table 1.
Demographic characteristics of informants in the Adea Berga district.
| Parameters | Frequency | Percent (%) |
|---|---|---|
| Age, years | ||
| 25–40 | 20 | 31.75 |
| 40–45 | 32 | 50.79 |
| Above 55 | 11 | 17.46 |
| Sex | ||
| Females | 12 | 19.04 |
| Males | 51 | 80.95 |
| Education level | ||
| Illiterate | 34 | 53.97 |
| Elementary school | 10 | 15.87 |
| Secondary school | 16 | 25.40 |
| University degree holder | 3 | 4.76 |
3.2. Medicinal Plants Reported and Ailments Treated
The study recorded a total of 59 medicinal plants (distributed in 35 families) used in the Adea Berga district to treat 35 livestock ailments, of which 55 were identified to a species level, three to a genus level, and only one to a family level (Table 2). The family Asteraceae had the highest number of medicinal plants accounting for six (10.17%) of the total medicinal plants, followed by Euphorbiaceae, Lamiaceae, and Solanaceae, each contributing four (6.78%) medicinal plants. The families Cucurbitaceae, Fabaceae, and Poaceae contributed three (5.09%) species each, whereas families Brassicaceae, Myrsinaceae, Rosaceae, and Rutaceae contained two (3.39%) medicinal plants each. Each of the rest 24 families was represented by single species. Of the total medicinal plants, 31(52.54%) were herbs, 18 (30.51%) were shrubs, and 10 (16.95%) were trees.
Table 2.
Lists of medicinal plants used for the treatment of livestock diseases in the Adea Berga district.
| Scientific name (family) | Local name | Habit | Parts used | Local (and English) names of disease treated | Animal treated | Mode of preparation | Administration route | Voucher number | Ethnoveterinary use elsewhere in Ethiopia |
|---|---|---|---|---|---|---|---|---|---|
| Acacia abyssinica Benth. (Fabaceae) | Laaftoo | Tree | Leaf | Biifaa (snake poisoning) | All domestic animals | Chewing | Nasal, oral | MF 040-2018 | Goiter, stomachache [12] |
| Achyranthes aspera L. (Amaranthaceae) | Darguu | Herb | Leaf | Dhiiga dhaabuf (bleeding) | All domestic animals | Squeezing | Topical | MF 036-2018 | Chronic trypanosomiasis, headache, babesiosis, gonorrhea, wound [26]; nasal infection, ophthalmic infection, minor bleeding [27]; mastitis, wound, diarrhea [28]; blackleg, mastitis, bleeding [8]; bloat [29]; blackleg [30]; wound, mastitis [9]; eye infection, anthrax, snake bite, wound, donkey's malaria [31]; abdominal discomfort, febrile disease [11]; blackleg [5] |
| Ajuga integrifolia Buch.-Ham. (Lamiaceae) | Armaa guusaa | Herb | Leaf | Michii (febrile illness) | All domestic animals | Crushing | Oral | MF 043-2018 | Calf diarrhea [26]; internal parasite [32]; sprain [33]; diarrhea [17] |
| Allium sativum L. (Alliaceae) | Qullubii adii | Herb | Bulb | Madaa gogsuuf (wound) | All domestic animals | Crushing | Topical | - | Blackleg, dermatophilosis, mange, scabies, ringworm, parasitic leech, lice infestation in chicken, and helminthiasis [27]; mange and internal parasite [34]; hepatitis [4]; expectorant, antiseptic [2]; mastitis, colic, diarrhea, bloat, internal parasites, septicemia [6]; mastitis, colic diarrhea, bloat, internal parasites [15]; abdominal pain, blackleg, leech, pasteurellosis, bloat [8]; blackleg [7]; abdominal pain, pasteurellosis, bloat [9]; foot-and-mouth disease [14]; abdominal ache, bloat [14]; malaria and stomach problem [12]; mastitis, diarrhea, internal parasite [10]; chicken bloody diarrhea [35]; Salmonella pullorum, fowl cholera, coccidiosis, fowl typhoid, Newcastle disease [36]; cough, fungal infection, leech infestation [17] |
| Aloe pubescens Reynolds (Aloaceae) | Argiisa | Shrub | Sap | Madaa wanjoo (yoke sore) | Cattle | Squeezing | Topical | MF 017-2018 | Wound [18]; trypanosomiasis, tsetse fly repellent [37] |
| Artemisia abyssinica Sch. Bip. ex A. Rich. (Asteraceae) | Arrittaa | Herb | Leaf | Budaa (evil eye) | All domestic animals | Unprocessed | Nasal | MF 029-2018 | Epilepsy [4] |
| Bersama abyssinica Fresen. (Melianthaceae) | Lonchisaa | Tree | Leaf | Albaatii (diarrhea) | All domestic animals | Crushing and squeezing | Oral | MF 041-2018 | Dermatophytes [4]; kidney problems, wound, swelling [38]; trypanosomiasis [6]; trypanosomiasis [15]; blackleg, paralyzed animal [14]; skin parasites [12] |
| Brassica nigra (L.) K. Koch (Brassicaceae) | Sanaficaa | Herb | Seed | Bokoka (bloat), rakkoo dakamuu nyaataa (simple indigestion), cininnaa (colic) | All domestic animals | Roasting | Oral | MF 003-2018 | Bloat [14] |
| Brucea antidysenterica J.F. Mill. (Simaroubaceae) | Qomanyoo | Shrub | Leaf | Dhukkubbi ijaa (eye infection) | All domestic animals | Unprocessed | Ocular | - | Trypanosomiasis [6]; trypanosomosis [15]; rabies [8]; blackleg [7]; rabies, ring worms [9]; blinded and eye discharged animal [14]; epizootic lymphangitis [32]; malaria, rabies, toothache [12]; mastitis [10]; epizootic lymphangitis [39] |
| Buddleja polystachya Fresen. (Buddlejaceae) | Adaddoo | Shrub | Leaf | Hadhaandhula baasuf (leech infestation) | Cattle | Crushing and diluting | Nasal | MF 035-2018 | Leech infestation [31]; eye disease [12]; internal parasite, diarrhea [39] |
| Calpurnia aurea (Aiton) Benth. (Fabaceae) | Ceekaa | Shrub | Leaf | Bofatu hiddee (snake bite), bokoka (bloat) | All domestic animals | Crushing and diluting | Nasal, oral | MF 024-2018 | Tick infestation, helminthiasis, snake bite, sore and parasitic leech [27]; mite infestation, conjunctivitis [34]; dermatophytes [4]; skin disease, rabies [6]; mastitis, skin diseases like dermatophilosis and ectoparasites (lice, ticks) [28]; lice infestation, leech [8]; diarrhea, skin infection, blackleg, respiratory manifestations, ectoparasites [7]; cattle lice [30]; pasteurellosis, dermatophilosis, and ectoparasites [40]; lice infestation, leech infestation, abdominal pain, bloat [9]; ectoparasites, alopecia [14], lice infestation, ticks infestation [31]; mange [41]; internal parasites, pasteurellosis, mastitis, dermathophillosis, ectoparasites (tick, fleas, lice) [32]; scabies [12]; internal parasites [42]; flea and louse infestation [43]; internal and external parasite infection [10]; tsetse fly repellent [37]; Estrus ovis, trypanosomiasis [39]; rabies, external parasite [17] |
| Capsicum annuum L. (Solanaceae) | Barbaree | Herb | Seed | Hadhaandhula baasuf (leech infestation) | Cattle | Grinding and diluting | Nasal | - | Cowdriosis [2]; colic, bloat, septicemia [6]; abdominal pain, bloat, blackleg, pasteurellosis, leech [8]; pasteurellosis, leech infestation, tapeworm [9]; abdominal aches, leech infestation [14]; bloat, blackleg, colic [12]; chicken diarrhea and ectoparasite infection [35]; colic, bloat, internal parasites infection [17] |
| Carissa spinarum L. (Apocynaceae) | Agamsa | Shrub | Seed | Sirna fincanii (urinary tract infection) | All domestic animals | Grinding and diluting | Oral | MF 022-2018 | Helminthiasis, parasitic leech [27]; evil eye, colic [34]; helminthiasis [2]; rabies [6]; ring worm, wound [8]; ring worm, wound [9]; febrile causal disease, evil eye [11]; evil eye, headache, stomachache, gonorrhea [12] |
| Clausena anisata (Willd.) Hook.f. ex Benth. (Rutaceae) | Ulummaa | Shrub | Leaf | Albaatii (diarrhea) | All domestic animals | Crushing and squeezing | Oral | MF 014-2018 | Ectoparasite infestation [6]; lice [15]; blackleg, respiratory manifestations [7]; skin rash [12] |
| Croton macrostachyus Hochst. ex Delile (Euphorbiaceae) | Bakkanisa | Tree | Leaf | Bokoka (bloat), o'ichoo (foot rot) | Cattle, sheep, goat | Crushing and diluting | Oral, topical | MF 023-2018 | Ringworm, dermatophilosis, mange, scabies, wound, minor bleeding, sore [27]; when a cow hates her calf, dermatophytosis, wound, bloat, eye defect [34]; anthelmintic [13]; equine colic, abdominal pain, bloat [38]; bloat [2]; mastitis, rabies, colic, trypanosomiasis, septicemia [6]; wound, fungal infection [15]; febrile illness in donkey (michii), expulsion uterine mass in camels [44]; ring worm, bloat, wound [8]; blackleg, trypanosomiasis, diarrhea, blackleg, helminthic infection, respiratory manifestations, bloat, lesion [7]; wound, fungal infection [40]; ring worm, bloat, wound [9]; bloat, dandruff [14]; equine colic, abdominal pain, bloat [32]; bloat, anthrax [33]; wound healing, antiparasitic [11]; ringworm, gonorrhea, scabies, evil eye, febrile illness, headache, wound, skin infection [12]; diarrhea (dysentery), external parasite [10]; chicken open wound [35]; blackleg, bloat [39]; blackleg, skin wound [17]; bloat, ringworm [5] |
| Cucumis dipsaceus Ehrenb. ex Spach (Cucurbitaceae) | Buqqee sexanaa | Herb | Sap | Maxxantuu alaa (ectoparasites infections), foroforii (scabies) | All domestic animals | Unprocessed | Topical (bathing) | MF 007-2018 | Pneumonia, abdominal pain [26]; snake bite, rabies [40]; animal head parasites [33]; abdominal discomfort, bloat [11]; fowl cholera and coccidiosis [36] |
| Cucumis ficifolius A. Rich. (Cucurbitaceae) | Holotoo | Herb | Root, fruit | Dil'uu ture (retained placenta), rammoo garaa (endoparasites infections) | Cattle, sheep | Crushing and diluting | Oral | - | Coccidiosis, cowdriosis, hepatitis, wound [27]; blackleg [4]; blackleg, colic, emaciation [6]; rabies, anthrax [44]; blackleg [8]; rabies, trypanosomiasis, blackleg, cough [29]; blackleg [7]; rabies [9]; anthrax, abdominal pain [31]; febrile illness, ear pain, stomachache, cattle infection, tetanus, sudden sickness, inflammation [12] |
| Cymbopogon citratus (DC.) Stapf (Poaceae) | Xajjii saraa | Herb | Whole plant | Cininnaa (colic) | All domestic animals | Crushing and squeezing | Oral | MF 018-2018 | Hepatitis, blackleg [4] |
| Cynodon dactylon (L.) Pers. (Poaceae) | Coqorsaa | Herb | Whole plant | Biifaa (snake poisoning) | All domestic animals | Chewing | Topical (spraying) | MF 009-2018 | |
| Datura stramonium L. (Solanaceae) | Manjii | Herb | Leaf | Foroforii (ring worm) | All domestic animals | Crushing and squeezing | Topical (bathing) | MF 047-2018 | Nerve problem [45]; yoke sore, wound, dermatophytosis, mastitis [34]; trypanosomiasis [29]; blackleg, respiratory manifestations [7]; anthrax [31]; blackleg, nasal bleeding [33]; wound [12]; coughing (for horses, mules, and donkeys) [43]; chicken depression and diarrhea [35] |
| Dodonaea angustifolia L. f. (Sapindaceae) | Ittachaa | Shrub | Leaf | Madaa gogsuuf (wound), caba (bone fracture) | All domestic animals | Crushing | Topical | MF 031-2018 | Bloat, sudden diarrhea, ringworm, scabies [27]; saddle sore [34]; anthelmintic [13]; wound [28]; bloat, liver disease, diarrhea [7]; lice infestation [9]; dislocated bone [31]; bone dislocation [41]; retained placenta, dystocia [32]; ectoparasite [11]; wound, tapeworm [12]; blackleg [39] |
| Echinops kebericho Mesfin (Asteraceae) | Korobicho | Herb | Root | Budaa (evil eye) | All domestic animals | Smoking | Nasal | MF 045-2018 | Coughing, pneumonia, pasteurellosis (mich), general illness, evil eye, taeniasis [34]; blackleg, cough [6]; diarrhea, blackleg [15]; blackleg, respiratory manifestations, liver disease, skin infection [7]; febrile illness [30]; diarrhea, blackleg [40]; dislocated bone [31]; anthrax [41]; blackleg, respiratory disease [11]; trypanosomiasis [37] |
| Echinops sp. (Asteraceae) | Kosorruu | Shrub | Root | Dhukkubbi ijaa (ophthalmic disease) | All domestic animals | Chewing | Nasal | MF 044-2018 | |
| Embelia schimperi Vatke (Myrsinaceae) | Hanquu | Shrub | Seed | Cininnaa (colic), maxxantuu keessaa (endoparasites infections) | All domestic animals | Roasting and crushing | Oral | MF 027-2018 | Bloat, mucal diarrhea, bloody diarrhea [27]; anthelmintic [13]; tapeworm [12] |
| Eucalyptus globulus Labill. (Myrtaceae) | Bargamoo adii | Tree | Leaf | Kirkirsuu (shivering), loss of appetite, michii (febrile illness) | Cattle | Crushing and squeezing | Oral | MF 028-2018 | Mich, lumpy skin disease [34]; ectoparasite [44]; blackleg [30]; avian cholera, influenza, skin disease, cough [12]; Salmonella pullorum, fowl cholera, coccidiosis, fowl typhoid, infectious coryza, Newcastle disease, fowl pox [36] |
| Euphorbia sp. (Euphorbiaceae) | Adamii | Shrub | Sap | Madaa gogsuuf (wound), kormammuu (wart) | All domestic animals | Crushing | Topical | MF 049-2018 | |
| Hagenia abyssinica (Bruce ex Steud.) J.F.Gmel. (Rosaceae) | Heexoo | Tree | Leaf | Maxxantuu keessaa (endoparasites infections) | All domestic animals | Crushing And Diluting | Orally | MF 038-2018 | Anthelmintic [13]; internal parasite, nasal bot [38]; GIT parasite [15]; tape worm in dogs [28]; GIT parasite [40]; taeniasis [14]; internal parasite [32]; intestinal worms [11]; fowl cholera, fowl typhoid and Newcastle disease [36]; internal parasites infection [17] |
| Hypericum revolutum Vahl (Hypericaceae) | Hindhee | Tree | Leaf | Albaatii (diarrhea) | Cattle, sheep | Crushing and squeezing | Oral | MF048-2018 | Retained fetal membranes (RFM), metritis [40]; calf diarrhea [32] |
| Juniperus procera Hochst. ex Endl. (Cupressaceae) | Gattiraa | Tree | Leaf | Maxxantuu alaa (ectoparasites infections) | All domestic animals | Crushing and squeezing | Topical (bathing) | MF 005-2018 | Trypanosomiasis [38]; retained placenta/fetal membrane [27]; diarrhea [4]; internal parasite, pasteurellosis [38]; abortion, irregular estrus [15]; abortion, irregular estrus, postpartum bleeding [40]; colic [17] |
| Justicia schimperiana (Hochst. ex Nees) T. Anderson (Acanthaceae) | Sansallii | Shrub | Leaf | Albaatii keelloo (coccidiosis) | Poultry | Crushing and squeezing | Oral | MF 002-2018 | Wound [45]; diarrhea in hens, symptom of mouth, nose, and ocular discharge, blindness, depression, loss of appetence in hens [34]; rabies [6]; otitis [15]; jaundice, wound [28]; blackleg, rabies [8]; bloat, evil spirit [29]; diarrhea, blackleg, helminthic infection [7]; otitis, swollen of lymph node [40]; rabies, coccidiosis [9]; rabies [14]; dysentery [31]; rabies, blackleg, gonorrhea, malaria [12]; circling disease [39]; rabies, blackleg [17] |
| Kalanchoe lanceolata (Forssk.) Pers. (Crassulaceae) | Bosoqqee | Herb | Stem | Itoo maalaa (swelling of dewlap) | Cattle | Unprocessed | Implantation | MF 006-2018 | |
| Leonotis ocymifolia (Burm.f.) Iwarsson (Lamiaceae) | Bokkolluu | Herb | Leaf | Albaatii (diarrhea), michii (febrile illness) | All domestic animals | Crushing and squeezing | Oral | MF 019-2018 | Anthrax, blackleg [27]; anthrax [4]; blackleg [7] |
| Lepidium sativum L. (Brassicaceae) | Feexoo | Herb | Seed | Bokoka (bloat), cininnaa (colic), maxxantuu keessaa (endoparasites infections) | All domestic animals | Grinding and diluting | Oral | - | Blackleg, diarrhea, bloat [34]; blackleg, colic, diarrhea, bloat, internal parasites, septicemia [6]; blackleg, bloat [15]; blackleg [7]; diarrhea, skin infection [7]; blackleg [40]; cough [14]; swelling, anthrax [31]; blackleg, colic, diarrhea, bloat, internal parasite [11]; cough, bloat, malaria, diarrhea, tonsillitis, heart disease [12]; trypanosomiasis, tsetse fly repellent [37]; Salmonella pullorum, fowl cholera, coccidiosis, fowl typhoid, infectious coryza, Newcastle disease, fowl pox [36] |
| Linum usitatissimum L. (Linaceae) | Talbaa | Herb | Seed | Gogiinsa garaa (constipation), dhibee garaa (gastritis), dil'uu ture (retained placenta) | All domestic animals | Roasting, grinding and diluting | Oral | MF 020-2018 | Placenta retention [34]; retained fetal membrane [6]; retained fetal membrane [15]; urine retention, coccidiosis [29]; retained placenta, dandruff [12] |
| Maesa lanceolata Forssk. (Myrsinaceae) | Abbayyii | Tree | Leaf and seed | Cittoo, madaa afaani (stomatitis) | Cattle | Crushing | Topical (painting) | MF 051-2018 | Mange, tick infestation, dermatophilosis, helminthiasis, parasitic leech [27]; eye problem [4]; babesiosis, mastitis, kidney problem, internal parasite, wound, cancer (tumor) [38]; diarrhea, blackleg [15]; internal parasite [7]; diarrhea, blackleg [40]; leech infestation [32]; eye disease, pasteurellosis [12]; leech infestation [10]; leech infestation [10]; bloat [39] |
| Malva parviflora L. (Malvaceae) | Liitii | Herb | Root | Dil'uu ture (retained placenta) | Cattle, sheep | Crushing and squeezing | Oral | MF 013-2018 | Wound, anthrax [28] |
| Millettia ferruginea (Hochst.) Baker (Fabaceae) | Birbirraa | Tree | Leaf | Hadhaandhula baasuf (leech infestation) | Cattle | Crushing and diluting | Nasal | MF 042-2018 | Ectoparasite [34]; diarrhea [4]; tsetse fly repellent [37]; trypanosomiasis [39] |
| Nicotiana tabacum L. (Solanaceae) | Tamboo | Herb | Leaf | Hadhaandhula baasuf (leech infestation), bokoka (bloat) | Cattle, sheep | Crushing and diluting | Nasal, oral | Tick and leech infestation, snake bite, internal parasite, fever, wound infestation [26]; anthelmintic [13]; lice and some ectoparasite infestation, blackleg, trypanosomiasis, leech infestation, snake bite [6]; leech infestation, snake bite [15]; leech [35]; leech [8]; blackleg, respiratory manifestations, liver disease, snake bite, for fattening of cattle [7]; leech infestation [30]; leech infestation [40]; leech infestation, tapeworm [9]; cough, internal parasites [14]; leech infestation, scabies, lice infestation [31]; leech infestation [33]; leech infestation, tick infestation [32]; bloat, leech infestation, internal parasites, trypanosomiasis, eye infection, headache [12]; tick infestation [43]; leech infestation [10]; trypanosomiasis, tsetse fly repellent [37]; chicken depression [35]; trypanosomiasis, leech infestation [39]; snake poisoning, leech infestation [17] | |
| Ocimum lamiifolium Hochst. ex Benth. (Lamiaceae) | Damakase | Shrub | Leaf | Kirkirsuu (shivering), qoqaa fuudhu (inappetence), michii (febrile illness) | Cattle | Crushing and squeezing | Oral | MF050-2018 | Bloat, mucal diarrhea, poor appetite, bloody diarrhea [27]; pasteurellosis (mich) [34]; diarrhea [4]; blackleg [15]; abdominal colic, blackleg, trypanosomiasis, respiratory manifestations [7]; blackleg [40]; dingetengya (sudden sickness), blackleg [11]; diarrhea [10]; blackleg, diarrhea [17] |
| Olea europaea subsp. Cuspidata (Wall. & G.Don) Cif. (Oleaceae) | Ejersaa | Tree | Leaf | Biifaa (snake poisoning) | Cattle, sheep | Chewing | Topical (spraying) | MF 004-2018 | Contagious caprine pleuropneumonia (CCPP) [46]; mange, ringworm, lumpy skin disease [27]; lumpy skin disease (LSD), gait problem [34]; pasteurellosis, calf diarrhea [38]; arthritis [15]; eye infection [7]; arthritis, paralysis, back bone pains [40]; rabies, snake bite [9]; dermatological disease [11]; hemorrhoid [12]; diarrhea [42]; blackleg, pneumonia, and bloat [10]; chicken depression [35] |
| Olinia rochetiana A.Juss. (Oliniaceae) | Dalachoo | Shrub | Leaf | Dhukkubii hir'isuf (pain) | All domestic animals | Chewing | Topical, oral | MF 033-2018 | Calf diarrhea, wound [38]; mastitis, pneumonia, and other swellings or internal organs problems [10] |
| Plantago lanceolata L. (Plantaginaceae) | Qorxobbee | Herb | Leaf | Dhiiga dhaabuf (bleeding control) | All domestic animals | Squeezing | Topical | MF 016-2018 | Rabies [27]; trypanosomiasis [29]; skin cut [12] |
| Ranunculus multifidus Forssk. (Ranunculaceae) | Marfataa | Herb | Root | Albaatii (diarrhea) | Sheep, cattle | Unprocessed | Tying | MF 026-2018 | Dermatophilosis [27]; mastitis, internal parasite, trypanosomiasis [38]; trypanosomiasis [39] |
| Rhamnus prinoides L'Hér. (Rhamnaceae) | Geeshoo | Shrub | Leaf | Bokoka (bloat), hubaa qonqoo (tonsillitis) | Cattle, sheep | Crushing and squeezing | Oral | MF 025-2018 | Abscess swelling [34]; nasal bot [38]; leech infestation [40]; equine colic, leech infestation, dandruff [32]; salmonellosis [11]; skin fungal infection, wound [12]; chicken depression [35]; fowl cholera, coccidiosis, fowl typhoid and Newcastle disease [36]; diarrhea, internal parasite [5] |
| Ricinus communis L. (Euphorbiaceae) | Hobo | Shrub | Leaf | Itoo (abscess), bu'aa (rectal prolapse) | All domestic animals | Chopping | Oral, topical | MF 021-2018 | Blackleg, retained fetal membrane, skin disease [26]; mange, scabies, ringworm, retained placenta/fetal membrane [27]; diarrhea in new born, wound, sudden sickness, bloat, skin rashes/dermatitis [34]; retained fetal membrane [2]; rabies [6]; blackleg, actinomycosis [15]; retained fetal membrane, rabies [8]; blackleg, respiratory manifestations [7]; blackleg, actinomycosis [40]; retained fetal membrane, rabies [9]; wound [31]; anthrax, sudden sickness, bloat, actinomycosis, ulceric lymphangitis, epizootic lymphangitis [12]; mastitis [10]; foot and mouth disease (FMD) [17]; abscess, retained fetal membrane [5] |
| Rubus steudneri Schweinf. (Rosaceae) | Altufaa | Shrub | Leaf | Albaatii (diarrhea) | Cattle, sheep | Crushing and squeezing | Oral | MF 030-2018 | Bloat, mucal diarrhea, bloody diarrhea, blackleg [27]; bloat, diarrhea, blackleg, constipation with mucoid feces [34]; swelling [29] |
| Rumex nepalensis Spreng. (Polygonaceae) | Shultii | Herb | Root | Cininnaa (colic) | All domestic animals | Crushing and squeezing | Oral | MF 012-2018 | Internal parasite, headache [26]; bloody diarrhea [34]; blackleg [4]; fire burn [31] stomachache, spider poison, amoeba [12]; cough [39]; internal parasites infection, external parasites infection, wound [17] |
| Ruta chalepensis L. (Rutaceae) | Xeena adamii | Herb | Leaf, seed | Bokoka (bloat) | Cattle, sheep | Grinding | Oral | MF 011-2018 | Retained placenta, abdominal pain, snake bite [26]; blackleg [4]; blackleg, anthrax [40]; poisoning [14]; equine colic, abdominal pain [32]; ear pain, evil eye, heart failure [11]; stomachache [12]; wound [42]; chicken welling of head [35]; coccidiosis, fowl typhoid & Newcastle disease [36]; bloat [17]; colic, pasteurellosis [5] |
| Salvia nilotica Juss. ex Jacq. (Lamiaceae) | Abbaa jarraa | Herb | Leaf | Albaatii (diarrhea) | All domestic animals | Crushing and squeezing | Oral | MF 015-2018 | Blackleg [4]; mastitis, wound [38] |
| Senecio ochrocarpus Oliv. & Hiern (Asteraceae) | Monyoor | Herb | Leaf | Dhukkubii ijaa (eye infection) | All domestic animals | Chewing | Ocular | MF 032-2018 | |
| Solanum marginatum L. f. (Solanaceae) | Hiddii | Shrub | Sap | Madaa dugdaa (back sore) | Horse | Squeezing | Topical | MF 034-2018 | Dermatophytes [4]; cough [29]; blackleg, respiratory manifestations [7]; blackleg [14]; wound, breathing problem, anthrax [31] |
| Stephania abyssinica (Quart.-Dill. & A.Rich.) Walp. (Menispermaceae) | Kalalaa | Herb | Whole part | bokoka (bloat) | Cattle, sheep | Crushing and diluting | Oral | MF 037-2018 | Contagious bovine pleuropneumonia (CBPP), calf pneumonia [27]; anthrax, rabies, foot, and mouth disease [34]; blocking/difficult in urination [41]; mastitis, blackleg, trypanosomiasis [39]; rabies [17] |
| Tragia plukenetii Radcl.-Sm. (Euphorbiaceae) | Dobbii | Herb | Root | Dil'uu ture (retained placenta) | Cattle, sheep | Crushing and diluting | Oral | - | Myiasis in goat [44] |
| Verbascum sinaiticum Benth. (Scrophulariaceae) | Gurraa harree | Herb | Leaf | Abbaa gorbaa (blackleg), fedhii nyaataf (loss of appetite) | Cattle | Crushing and diluting | Oral | MF 046-2018 | Diarrhea, colic, snake bite, anthrax, wound, blackleg, myiasis, [34]; anthelmintic [13]; skin disease [6]; skin disease [15]; blackleg, swollen body, abdominal pain, loss of appetite [44]; wound [28]; thinning, rabies, trypanosomiasis, eye infection, mich [29]; cough [14]; wound, anthrax, dislocated bone [31]; anthrax [33]; febrile causal disease, heart disease, renal disease [11]; anthrax [17] |
| Vernonia amygdalina Delile (Asteraceae) | Eebicha | Shrub | Leaf | Albaatii (diarrhea) | cattle, sheep, goat | Crushing and squeezing | Oral | MF 001-2018 | Trypanosomiasis, cough, wound, skin disease [26]; retained placenta/fetal membrane, CBPP [27]; colic, leech [34]; anthelmintic [13]; hepatitis [4]; lumpy skin disease, pasteurellosis, internal parasite [38]; GIT parasite, diarrhea, blackleg [15]; increase milk production [8]; diarrhea, blackleg, helminthic infection [7]; blackleg, respiratory manifestations, to improve milk production in cows, retained placenta [7]; GIT parasite, diarrhea, blackleg [40]; retained placenta [9]; wound [14]; equine colic, pasteurellosis, abdominal pain [32]; abdominal pain, mich, febrile disease [11]; internal parasites [42]; diarrhea and skin problem [10]; trypanosomiasis [37]; chicken watery diarrhea [35]; internal parasite, diarrhea, colic [39]; internal parasite, retained placenta [17]; diarrhea, internal parasites [5] |
| Vernonia sp. (Asteraceae) | Osolee | Herb | Leaf | Maxxantuu alaa (ectoparasites infections) | All domestic animals | Unprocessed | Topical (bathing) | MF 008-2018 | |
| Zehneria scabra Sond. (Cucurbitaceae) | Hiddaa adii | Herb | Whole part | Martee (contagious bovine pleuropneumonia (CBPP)) | Cattle | Unprocessed | Tying on the neck | MF 039-2018 | Mich, yoke sore, dermatitis [34]; blackleg, pasteurellosis [8]; thinning [29]; rabies, pasteurellosis [9]; cough, emaciation, lameness, alopecia, colic [14]; trypanosomiasis [32]; swelling, rabies [12]; chicken swelling of head [35] |
| Zingiber officinale Roscoe (Zingiberaceae) | Zanjabilaa | Herb | Root | Cininnaa (colic), bokoka (bloat), dhukubbii ijaa (conjunctivitis) | All domestic animals | Crushing | Oral | - | Bloat, bloody diarrhea, poor appetite, mucal diarrhea [27]; colic, eye defect, diarrhea due to stomach parasite [34]; colic, diarrhea, bloat, internal parasites [6]; colic, diarrhea, bloat, internal parasites [15]; blackleg, pasteurellosis, abdominal pain, leech [8]; eye inflammation [7]; rabies, pasteurellosis, abdominal pain, leech infestation [9]; ascariasis, stomach disorder [14]; contagious caprine pleuropneumonia (CCPP)/cough [42]; Newcastle diseases (fengile) [35]; coccidiosis, fowl typhoid and Newcastle disease [36]; eye inflammation [17] |
| - (Poaceae) | Hadduffaa | Herb | Whole part | Biifaa (snake poisoning) | All domestic animals | Chewing | Topical (spraying) | MF 010-2018 |
Note. Disease names in bold indicate the use of the corresponding medicinal plant for the same purpose elsewhere in Ethiopia.
3.3. Medicinal Plant Parts Used and Methods of Preparation
Most remedies in the district were prepared from leaves accounting for 54.24% of the total medicinal plants reported, followed by plants that were harvested for their root (11.86%) and seeds (10.17%) (Figure 1). The most employed method of remedy preparation was crushing and squeezing or squeezing, accounting for 36 (61.02%) of the total preparations, followed by chewing, which accounted for 7 (11.86%) of the preparations. Seven (11.86%) medicinal plants are used in unprocessed form. Other methods of remedy preparation methods included grinding, chopping, roasting, and smoking.
Figure 1.
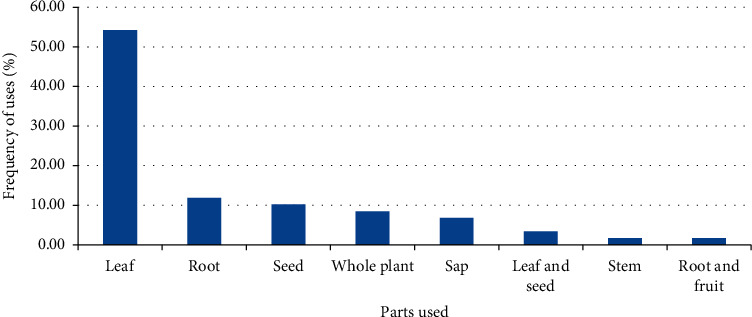
Parts of medicinal plants used in remedy preparation in the Adea Berga district.
3.4. Conditions of Medicinal Plants and Diluents Used in Remedy Preparations
Most of the medicinal plants used in remedy preparations were in their fresh form, accounting for 48 (81.36%) of the total claimed medicinal plants. Six (10.17%) medicinal plants were used either in dry or fresh form, and 5 (8.47%) were used in dry form. The commonly used diluent in the preparation of medicinal plant remedies was water accounting for 54.24% of the total preparations, followed by saliva (11%). Some (33.9%) of the medicinal plant did not need diluents in their preparations.
3.5. Routes of Remedy Administration
Nearly half (45.76) of the medicinal plants were administered through oral route, followed by those were administered topically (25.42) and nasally (10.17) (Table 3).
Table 3.
Route of administration of medicinal plants in the Adea Berga district.
| Route of administration | Frequency | Percent (%) |
|---|---|---|
| Oral | 27 | 45.76 |
| Topical | 15 | 25.42 |
| Nasal | 6 | 10.17 |
| Nasal and oral | 3 | 5.08 |
| Oral and topical | 3 | 5.08 |
| Ocular | 2 | 3.39 |
| Tying | 2 | 3.39 |
| Implantation | 1 | 1.69 |
3.6. Informant Consensus Factor
Informant consensus factor (ICF) values for the different ailment categories were calculated, and the results show the highest score for yoke sore (wound) (1.00), followed by leech infestation (0.92), endoparasites infections (0.90), ectoparasites infections (0.88), retained placenta (0.88), snake poisoning (0.88), and evil eye (0.88) (Table 4). Medicinal plants used to treat ailment categories of high ICF values include Aloe pubescens for treating yoke sore; Buddleja polystachya, Capsicum annuum, Millettia ferruginea, and Nicotiana tabacum for treating leech infestation; and Cucumis ficifolius, Embelia schimperi, Hagenia abyssinica, and Lepidium sativum for treating endoparasites infections.
Table 4.
Informant consensus factor values for the different ailment categories in the Adea Berga district.
| Ailment category | Number of plant species | Number of use-reports | ICF value |
|---|---|---|---|
| Yoke sore (wound) | 1 | 9 | 1.00 |
| Leech infestation | 4 | 41 | 0.92 |
| Endoparasites infections | 4 | 43 | 0.90 |
| Ectoparasites infections | 4 | 27 | 0.88 |
| Retained placenta | 4 | 27 | 0.88 |
| Snake poisoning | 5 | 35 | 0.88 |
| Evil eye | 2 | 10 | 0.88 |
| Bleeding | 2 | 8 | 0.85 |
| Wound | 4 | 18 | 0.82 |
| Diarrhea | 8 | 32 | 0.77 |
| Bloat | 9 | 35 | 0.76 |
| Colic | 7 | 22 | 0.71 |
| Eye infection | 4 | 11 | 0.70 |
3.7. Fidelity Level and Rank Order Priority Values
Medicinal plants that scored the highest fidelity level (FL) (100%) and rank order priority (ROP) (100%) values include Malva parviflora, Nicotiana tabacum, and Calpurnia aurea that were used to expel retained placenta, remove leeches, and treat snake poisoning, respectively (Table 5).
Table 5.
Rank order priority values of medicinal plants in the Adea Berga district scoring fidelity level values of 80% or more.
| Plant name | Ailment category | I U | I P | FL value (100%) | RPL | ROP |
|---|---|---|---|---|---|---|
| Malva parviflora | Retained placenta | 18 | 18 | 100.00 | 1.0 | 100.00 |
| Nicotiana tabacum | Leech infestation | 25 | 25 | 100.00 | 1.0 | 100.00 |
| Calpurnia aurea | Snake poisoning | 24 | 24 | 100.00 | 1.0 | 100.00 |
| Aloe pubescens | Yoke sore | 9 | 9 | 100.00 | 0.7 | 70.00 |
| Senecio ochrocarpus | Eye infection | 11 | 11 | 100.00 | 0.8 | 80.00 |
| Solanum marginatum | Wound | 15 | 13 | 86.66 | 1.0 | 86.66 |
| Cucumis dipsaceus | Ectoparasites | 27 | 24 | 88.89 | 1.0 | 88.89 |
| Vernonia amygdalina | Diarrhea | 20 | 17 | 85.00 | 1.0 | 85.00 |
Note. I U = number of informants who mentioned the same plant against any ailment; IP = number of informants who reported the utilization of medicinal plants against a specific ailment; FL = fidelity level; RPL = relative popularity level; ROP = rank order priority.
3.8. Habitat of Medicinal Plants
As revealed by the study, most (59.32%) of the medicinal plants used in remedy preparation in the study district were gathered from the wild only. Some (22.04%) were harvested from homegardens only, and other few were harvested from the wild or homegardens and from the wild or cultivation fields (Figure 2).
Figure 2.
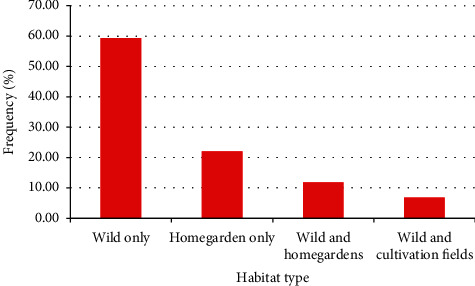
Proportions of medicinal plants harvested from different habitats in the Adea Berga district.
4. Discussion
4.1. Medicinal Plants Used and Ailments Treated
Livestock keeping is one of the most important economic sources of rural community in the Adea Berga district. Farmers in the district not only depend on plants to get fodder for their animals but also for their use as medicines to manage various livestock ailments as revealed by results of the current study. The study showed the use of 59 medicinal plant species distributed across 35 families to treat 35 livestock ailments. The highest number of medicinal plants used in remedy preparations belonged to the family Asteraceae, and this may be attributed to its dominance in terms of species diversity in the Ethiopian flora. Other studies conducted elsewhere in Ethiopia also reported the highest contribution of Asteraceae to the medicinal flora of the country [38, 47, 48]. The fact that herbs were the most frequently used growth forms in the preparation of remedies could be related to their relatively better abundance in the study district (as also witnessed by the investigators) and also due to their ease of preparation. Many other studies conducted elsewhere in the country also indicated the dominance of herbs in remedy preparations [8, 9, 12, 41, 49–52].
Of the 55 medicinal plants (identified to a species level) used in ethnoveterinary practices in the Adea Berga district, 26 were claimed to be used elsewhere in Ethiopia for other medical conditions not reported by the present study as indicated in Table 2 [2, 4–15, 17, 26–29, 31–40, 42–46], whereas 26 were claimed to be used elsewhere in the country at least once to manage same ailments [2, 5–12, 14, 15, 17, 18, 26–28, 30–34, 38–41, 44]. These include Achyranthes aspera (bleeding), Aloe pubescens (wound), Brassica nigra (bloat), Brucea antidysenterica (eye infection), Buddleja polystachya (leech infestation), Calpurnia aurea (snake bite and bloat), Capsicum annuum (leech infestation), Croton macrostachyus (bloat), Dodonaea angustifolia (wound and bone fracture), Echinops kebericho (evil eye), Embelia schimperi (endoparasites infections), Eucalyptus globulus (febrile illness), Hagenia abyssinica (endoparasites infections), Hypericum revolutum (diarrhea), Justicia schimperiana (coccidiosis), Lepidium sativum (bloat, colic, and endoparasites infections), Linum usitatissimum (retained placenta), Nicotiana tabacum (leech infestation and bloat), Ocimum lamiifolium (inappetence and febrile illness), Olea europaea subsp. cuspidata (snake poisoning), Ricinus communis (abscess), Rubus steudneri (diarrhea), Ruta chalepensis (bloat), Verbascum sinaiticum (blackleg and loss of appetite), Vernonia amygdalina (diarrhea), and Zingiber officinale (colic, bloat, and conjunctivitis) (see Table 2). Of these, the most frequently cited medicinal plants include N. tabacum, reported 16 times for its use to treat leech infestation [6, 8–10, 12, 14, 15, 17, 26, 28, 30–32, 39–41]; C. macrostachyus, reported 11 times for its use against bloat [2, 5, 7–9, 14, 32–34, 38, 39]; H. abyssinica, reported seven times for its use to treat endoparasites infections [11, 14, 15, 17, 28, 32, 40]; L. sativum, reported four times for its use to treat bloat [11, 12, 15, 34]; and L. usitatissimum reported four times for its use against retained placenta [6, 12, 15, 34]. High consensus among different communities in the use of a given medicinal plant to manage same ailment may indicate its better potency. According to Trotter and Logan [53], pharmacologically effective remedies are expected to have relatively greater informant consensus. In vitro studies conducted on N. tabacum [54, 55] revealed the killing effect of its leaf extracts against leeches, the effect of which is caused by an alkaloid called nicotine present in the plant [56, 57]. An in vivo experiment carried out on the crude extract of H. abyssinica demonstrated anthelmintic activity against cestodes in goats [58]. The substance kosotoxin present in H. abyssinica is believed to be responsible for the anthelmintic activity [59].
The study conducted in the Adea Berga district revealed for the first time the use of three medicinal plants in the Ethiopian ethnoveterinary practices. These include Cynodon dactylon, Kalanchoe lanceolata, and Senecio ochrocarpus that are used to treat snake poisoning, swelling of dewlap, and eye infection, respectively. Literature review revealed that so far, no study, exclusively conducted on medicinal plants of ethnoveterinary importance in the country, has reported the use of such plants.
4.2. Parts Used and Methods of Remedy Preparation and Routes of Administration
The fact that the leaf was the most commonly used medicinal plant part in remedy preparations in the district could be related to its better availability and ease of processing. It could also be due its richness in secondary metabolites [60]. The dominance of leaves in remedy preparations were also reported by studies conducted elsewhere in the country [61, 62].
The great majority of the remedies were claimed to be prepared from fresh plant materials, which might be attributed to the year-round availability of the same in the immediate environment. The better preference for fresh plant materials in the preparation of remedies was also reported by studies conducted elsewhere in the country [63]. A large proportion of the remedies in the study district were prepared by crushing or squeezing, which could be attributed to its ease of processing. Other studies [18, 31, 33, 40, 64] conducted elsewhere in the country also reported crushing as the commonly used method in the preparation of remedies. Availability and its property in dissolving many active compounds could be the reasons for the common use of water as diluent in the preparation remedies in the district as it is also the case in other parts of the country [18, 65, 66].
Oral is the most frequently employed route of remedy administration in the study district, and this could be related to its environment's suitability for rapid physiological reaction [7, 67]. Other studies conducted elsewhere in the country also reported the common use of oral route in administration of herbal preparations [4, 62].
4.3. Informant Consensus Factor, Fidelity Level, and Rank Order Priority Values
The fact that Nicotiana tabacum scored the highest FL and ROP values for its use to treat leech infestation, an ailment that scored the second highest ICF value, may indicate the high preference among informants in the study district for the plant to treat the ailment. Medicinal plants used to manage ailment categories of high ICF values and those of high FL and ROP values are expected to demonstrate good potency and thus are considered to be good candidates for further pharmacological and phytochemical investigations [22, 25]. Nicotiana tabacum is also used elsewhere in Ethiopia for treating leech infestation [6, 26]. In vitro investigation of leaf extracts of Nicotiana tabacum demonstrated activity against leeches [54, 55, 68], which could be attributed to the presence of nicotine in the leaf extract that interacts with nicotinic acetylcholine receptors to cause muscle weakness [55]. The other plant Calpurnia aurea that scored the highest FL and ROP values for its use to treat snake poisoning in the study district is also used elsewhere in the country against same ailments [27].
4.4. Comparison of Medicinal Plant Knowledge between Different Social Groups
Results of the present study indicate that the great majority of respondents selected for interviews in the study district were males. This may reflect the fact that males are the most favored by practitioners in the district in the transfer of traditional medical knowledge across generations. Other studies conducted elsewhere in the country also showed the dominance of males in traditional medical practices [7, 18, 69]. The majority of the participants selected for participation in ethnoveterinary study in the district were illiterate. This may reveal the fact that illiterate people are more knowledgeable as they are less exposed to cultural change compared with literate ones. Other studies carried out in other parts of the country also revealed that illiterate people held better traditional medical knowledge than literate ones [7, 27].
4.5. Habitats of Medicinal Plants
As shown by the study, the majority of the medicinal plants used in remedy preparations in the study district were harvested from the wild, an indication of the little practice of cultivating medicinal plants in the study district. The common use of plants harvested from the wild was also reported by other studies conducted elsewhere in the country [31, 47, 62, 70, 71].
5. Conclusion
The results of the present study revealed the high dependence of people in the Adea Berga district in the use of medicinal plants to manage livestock ailments, which could be due to the high prevalence of different diseases, limited access to modern veterinary care facilities, high prices of modern drugs, and diversity of local flora. Based on the demographic characteristic of people who participated in the study, knowledge on herbal medicine is mainly held by males and illiterate people. Priority for further pharmacological and phytochemical investigations needs to be given to the plants Nicotiana tabacum, Malva parviflora, and Calpurnia aurea that scored the highest FL and ROP values for their uses to treat leech infestation, retained placenta, and snake poisoning, respectively, as such values may indicate their higher potency against the respective ailments. Urgent action is needed to conserve Aloe pubescens, an Ethiopian endemic plant that has been included in the IUCN Red List as “near-threatened” species. Aloe pubescens is among the five medicinal plants in the study area that scored the highest FL value.
Acknowledgments
The authors thank the Office of the Vice President for Research and Technology Transfer of Addis Ababa University for its support in financing field trip expenses. The authors are also grateful to the informants in the Adea district who unreservedly shared with us their knowledge on medicinal plants used in ethnoveterinary practices and to district officials and experts who facilitated the ethnobotanical data collection work and for provision of data on major livestock health problems and available veterinary healthcare facilities in the district. The research was financially supported by the Office of the Vice President for Research and Technology Transfer of Addis Ababa University (grant number: TR/036/2016). The role of the Office is supporting academic staff and students to conduct problem-solving research and publish their findings.
Data Availability
Ethnoveterinary data were stored in a computer available at the Aklilu Lemma Institute of Pathobiology (ALIPB), Addis Ababa University (AAU), and the Faculty of Veterinary Medicine, Hawassa University. Readers may request the institutions for permission to get access to the data.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
References
- 1.Abraha G. Addis Ababa, Ethiopia: Addis Ababa University; 2007. Major animal health problems of market Oriented livestock development in atsbi Womberta woreda, Tigray regional state. DVM thesis. [Google Scholar]
- 2.Sori T., Bekana M., Adugna G., Kelbessa K. Medicinal plants in the ethnoveterinary practices of Borana pastoralists, Southern Ethiopia. The International Journal of Applied Research in Veterinary Medicine (IJARVM) . 2004;2:220–225. [Google Scholar]
- 3.Abebe D., Ayehu A. Medicinal Plants and Enigmatic Health Practices of Northern Ethiopia . Addis Ababa, Ethiopia: Addis Ababa: B.S.P.E; 1993. [Google Scholar]
- 4.Yineger H., Kelbessa E., Bekele T., Lulekal E. Ethnoveterinary medicinal plants at Bale Mountains National Park, Ethiopia. Journal of Ethnopharmacology . 2007;112(1):55–70. doi: 10.1016/j.jep.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 5.Bekele A., Mussa A. Ethnoveterinary practice in Chiro district, Western Hararge, Ethiopia. Pharmacologyonline . 2009;1:128–139. [Google Scholar]
- 6.Tamiru F., Terfa W., Kebede E., Dabessa G., Roy R. K., Sorsa M. Ethnoknowledge of plants used in veterinary practices in Dabo Hana district, West Ethiopia. Journal of Medicinal Plants Research . 2013;7:2960–2971. [Google Scholar]
- 7.Yigezu Y., Haile D. B., Ayen W. Y. Ethnoveterinary medicines in four districts of Jimma zone, Ethiopia: cross sectional survey for plant species and mode of use. BMC Veterinary Research . 2014;10(1):p. 76. doi: 10.1186/1746-6148-10-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tadesse B., Mulugeta G., Fikadu G., Sultan A. Survey on ethno-veterinary medicinal plants in selected woredas of East Wollega zone, Western Ethiopia. Journal of Biology, Agriculture and Healthcare . 2014;4:p. 17. [Google Scholar]
- 9.Birhanu T., Abera D. Survey of ethno-veterinary medicinal plants at selected Horro Gudurru districts, western Ethiopia. African Journal of Plant Science . 2015;9:185–192. [Google Scholar]
- 10.Romha G., Dejene T. A., Telila L. B., Bekele D. F. Ethnoveterinary medicinal plants: preparation and application methods by traditional healers in selected districts of southern Ethiopia. Veterinary World . 2015;8(5):674–684. doi: 10.14202/vetworld.2015.674-684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mohammed C., Abera D., Woyessa M., Birhanu T. Survey of ethno-veterinary medicinal plants in Melkabello district, eastern Harerghe zone, eastern Ethiopia. Ethiopian Veterinary Journal . 2016;20:1–15. [Google Scholar]
- 12.Kitata G., Abdeta D., Amante M. Ethnoknowledge of plants used in veterinary practices in Midakegn district, west Showa of Oromia region, Ethiopia. Journal of Medicinal Plants Studies . 2017;5:282–288. [Google Scholar]
- 13.Scantlebury C. E., Peachey L., Hodgkinson J., et al. Participatory study of medicinal plants used in the control of gastrointestinal parasites in donkeys in Eastern Shewa and Arsi zones of Oromia region, Ethiopia. BMC Veterinary Research . 2013;9(1):p. 179. doi: 10.1186/1746-6148-9-179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Feyissa T. F., Shigut M. M., Hailemariam T. B., Regassa T., Kergano N. K. Ethnobotanical study of ethnoveterinary plants in Kelem Wollega zone, Oromia region, Ethiopia. Journal of Medicinal Plants Research . 2017;11:307–317. [Google Scholar]
- 15.Bayecha F. B., Hordofa D. L., Nurfeta D. G., Abebe R. A. Survey of ethno-veterinary medicinal plants at Dale Sadi districts of Oromia regional state, western Ethiopia. Journal of Natural Sciences Research . 2018;8:p. 19. [Google Scholar]
- 16.Jima T. T. Medicinal plants used in the treatment of livestock diseases in Berbere district of Bale zone, Oromia region, Ethiopia. Journal of Medicinal Plants Research . 2018;12:270–277. [Google Scholar]
- 17.Abera Y., Mulate B. Ethno-veterinary medicine: a potential alternative to animal health delivery in Wolmera district, Oromia Region, Ethiopia. Ethiopian Veterinary Journal . 2019;23(1):111–130. doi: 10.4314/evj.v23i1.8. [DOI] [Google Scholar]
- 18.Berhanu M., Tintagu T., Fentahun S., Giday M. Ethnoveterinary survey of medicinal plants used for treatment of animal diseases in Ambo District of Oromia Regional State of Ethiopia. Evidence-Based Complementary and Alternative Medicine . 2020;2020:12. doi: 10.1155/2020/8816227.8816227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Serekebrhan T., Animut G., Mekasha Y., Assefa G. Assessment of farmers perception towards production and utilization of improved forages for dairy cattle feeding in the central highlands of Ethiopia. East African Journal of Veterinary and Animal Sciences . 2018;2:45–56. [Google Scholar]
- 20.Diro S. Assessing the Effect of Plant Density on Yield of Irrigated Potato and Analysis of Input Supply Chains at Adea Berga District . Ambo, Ethiopia: Ambo University; 2016. MSc thesis. [Google Scholar]
- 21.Martin G. J. Ethnobotany: A Method Manual . London, UK: Chapman & Hall; 1995. [Google Scholar]
- 22.Friedman J., Yaniv Z., Dafni A., Palewitch D. A preliminary classification of the healing potential of medicinal plants, based on a rational analysis of an ethnopharmacological field survey among Bedouins in the Negev Desert, Israel. Journal of Ethnopharmacology . 1986;16(2-3):275–287. doi: 10.1016/0378-8741(86)90094-2. [DOI] [PubMed] [Google Scholar]
- 23.Ali-Shtayeh M. S., Jamous R. M., Jamous R. M. Traditional Arabic Palestinian ethnoveterinary practices in animal health care: a field survey in the West Bank (Palestine) Journal of Ethnopharmacology . 2016;182:35–49. doi: 10.1016/j.jep.2016.02.005. [DOI] [PubMed] [Google Scholar]
- 24.Giday M., Asfaw Z., Woldu Z., Teklehaymanot T. Medicinal plant knowledge of the Bench ethnic group of Ethiopia: an ethnobotanical investigation. Journal of Ethnobiology and Ethnomedicine . 2009;5(1):p. 34. doi: 10.1186/1746-4269-5-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Heinrich M., Ankli A., Frei B., Weimann C., Sticher O. Medicinal plants in Mexico: healers’ consensus and cultural importance. Social Science & Medicine . 1998;47(11):1859–1871. doi: 10.1016/s0277-9536(98)00181-6. [DOI] [PubMed] [Google Scholar]
- 26.Tekle Y. Study on ethno veterinary practices in Amaro special district Southern Ethiopia. Medicinal & Aromatic Plants . 2015b;4:p. 2. [Google Scholar]
- 27.Lulekal E., Asfaw Z., Kelbessa E., Van Damme P. Ethnoveterinary plants of ankober district, North Shewa zone, Amhara region, Ethiopia. Journal of Ethnobiology and Ethnomedicine . 2014;10(1):p. 21. doi: 10.1186/1746-4269-10-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gebrezgabiher G., Kalayou S., Sahle S. An ethno-veterinary survey of medicinal plants in woredas of Tigray region, Northern Ethiopia. International Journal of Biodiversity and Conservation . 2013;5:89–97. [Google Scholar]
- 29.Birhan Y. S., Kitaw S. L., Alemayehu Y. A., Mengesha N. M. Ethnoveterinary medicinal plants and practices in Enarj Enawga district, East Gojjam zone, Amhara region, Ethiopia. International Journal of Animal Sciences . 2018;2:p. 1014. [Google Scholar]
- 30.Tedila H., Dida G. Ethnobotanical study of traditional medicinal plants used for treatment of human and livestock ailments by traditional healers in Goba woreda, Bale zone, Oromia, South East Ethiopia. Journal of Natural Sciences Research . 2019;9:p. 10. doi: 10.7176/JNSR. [DOI] [Google Scholar]
- 31.Teklay A. Traditional medicinal plants for ethnoveterinary medicine used in kilte awulaelo district, tigray region, northern Ethiopia. Journal of Biology, Agriculture and Healthcare . 2015;5:p. 19. [Google Scholar]
- 32.Tekle Y. An ethno-veterinary botanical survey of medicinal plants in kochore district of gedeo zone, southern nations nationalities and peoples regional state (SNNPRs), Ethiopia. Journal of Scientific and Innovative Research . 2014;3:433–445. [Google Scholar]
- 33.Yirga G., Teferi M., Brhane G., Amare S. Plants used in ethnoveterinary practices in Medebay-Zana district, Northern Ethiopia. Journal of Medicinal Plants Research . 2012;6:433–438. doi: 10.5897/jmpr11.1133. [DOI] [Google Scholar]
- 34.Mengesha A., Dessie D. Ethno veterinary medicine knowledge and practices in and around Gondar, Ethiopia. Journal of Public Health, Pharmacy and Pharmacology . 2018;3:39–68. [Google Scholar]
- 35.Wodegebriel Y. W., Abebe B. F., Tamir A. Medicinal plants used by farmers for treatment of major diseases of chicken in South Wollo zone, Amhara region, Ethiopia. International Journal of Advanced Research in Biological Sciences . 2018;5:45–58. [Google Scholar]
- 36.Markos S. Ethno veterinary medicine and common diseases of chicken producers in western zone of tigray, northern Ethiopia. Journal of Agriculture and Ecology Research International . 2019;20:1–17. doi: 10.9734/jaeri/2019/v20i130096. [DOI] [Google Scholar]
- 37.Endalachew B. E. Practices of ethnoveterinary against animal trypanosomosis in Southern Ethiopia. Global Journal of Biological and Biomedical Research . 2015;3:132–136. [Google Scholar]
- 38.Tekle Y. Medicinal plants in the ethno veterinary practices of Bensa woreda, Southern Ethiopia. OALibrary . 2015;2(1):1–12. doi: 10.4236/oalib.1101258. [DOI] [Google Scholar]
- 39.Moliso M. M., Tessema F., Yilma M., Getachew T., Asrat M. Documentation of ethno veterinary practices in selected sites of wolaita and dawuro zones, Ethiopia. Global Journal of Science Frontier Research: D Agriculture and Veterinary . 2016;16:p. 5. [Google Scholar]
- 40.Usmane A., Birhanu T., Redwan M., Sado E., Abera D. Survey of ethno-veterinary medicinal plants at selected districts of Harari Regional State, Eastern Ethiopia. Ethiopian Veterinary Journal . 2016;20(1):1–22. doi: 10.4314/evj.v20i1.1. [DOI] [Google Scholar]
- 41.Osman A., Sbhatu D. B., Giday M. Medicinal plants used to manage human and livestock ailments in raya kobo district of amhara regional state, Ethiopia. Evidence-Based Complementary and Alternative Medicine . 2020;2020:19. doi: 10.1155/2020/1329170.1329170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mengistu M., Kebede E., Serda B. Ethnobotanical knowledge of pastoral community for treating livestock diseases in Shinle zone, Somali regional state, Eastern Ethiopia. Journal of Veterinary Science & Technology . 2017;8(5):p. 5. doi: 10.4172/2157-7579.1000474. [DOI] [PubMed] [Google Scholar]
- 43.Tolossa K., Debela E., Athanasiadou S., Tolera A., Ganga G., Houdijk J. G. Ethno-medicinal study of plants used for treatment of human and livestock ailments by traditional healers in South Omo, Southern Ethiopia. Journal of Ethnobiology and Ethnomedicine . 2013;9(1):p. 32. doi: 10.1186/1746-4269-9-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kebede A., Ayalew S., Mesfin A., Mulualem G. An ethnoveterinary study of medicinal plants used for the management of livestock ailments in selected kebeles of dire dawa administration, eastern Ethiopia. Journal of Plant Sciences . 2017;5:34–42. doi: 10.11648/j.plant.20170502.13. [DOI] [Google Scholar]
- 45.Giday M., Teklehaymanot T. Ethnobotanical study of plants used in management of livestock health problems by Afar people of Ada’ar District, Afar Regional State, Ethiopia. Journal of Ethnobiology and Ethnomedicine . 2013;9(1):p. 8. doi: 10.1186/1746-4269-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gebrehiwot K., Shumbahri M. An ethnoveterinary survey of medicinal plants used to treat livestock diseases in Abala, northeastern Ethiopia. Journal of Basic and Applied Research International . 2015;10:185–193. [Google Scholar]
- 47.Taddese B., Abera D., Ejeta E. Ethnobotanical study of medicinal plants in selected Horro Gudurru woredas, western Ethiopia. Journal of Biology, Agriculture and Healthcare . 2015;5:p. 1. [Google Scholar]
- 48.Chekole G. Ethnobotanical study of medicinal plants used against human ailments in Gubalafto District, Northern Ethiopia. Journal of Ethnobiology and Ethnomedicine . 2017;13(1):p. 55. doi: 10.1186/s13002-017-0182-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hunde D. Addis Ababa, Ethiopia: Addis Ababa University; 2001. Use and management of traditional plants by indigenous people of Boosat district Welenchiti area. MSc Thesis. [Google Scholar]
- 50.Amenu E. Addis Ababa, Ethiopia: Addis Ababa University); 2007. Use and management of medicinal plants by indigenous people of Ejaji area (Chelya Wereda) west Shewa, Ethiopia: an ethnobotanical approach. MSc Thesis. [Google Scholar]
- 51.Adefa M., Abraha B. Ethnobotanical survey of traditional medicinal plants in Tehuledere district, south Wollo, Ethiopia. Journal of Medicinal Plants Research . 2011;5:6233–6242. doi: 10.5897/jmpr11.1070. [DOI] [Google Scholar]
- 52.Adefa M., Getaneh S. Medicinal plants biodiversity and local healthcare management system in Chencha district; Gamo Gofa, Ethiopia. Journal of Pharmacognosy and Phytotherapy . 2013;2:p. 1. [Google Scholar]
- 53.Trotter R. T., Logan M. H. Informants consensus: a new approach for identifying potentially effective medicinal plants. In: Etkin N. R., editor. Plants in Indigenous Medicine and Diet . New York, NY, USA: Redgrave Publishing Company; 1986. pp. 91–112. [Google Scholar]
- 54.Bahmani M., Farkhondeh T., Sadighara P. The anti-parasitic effects of Nicotina tabacum on leeches. Comparative Clinical Pathology . 2012;21(3):357–359. doi: 10.1007/s00580-012-1413-x. [DOI] [Google Scholar]
- 55.Ogello E. O., Kembenya E. M., Obiero K. O., Munguti J. M. Effects of Nicotina tobacum (Linnaeus) on the survival and behavioral response of the freshwater leeches, Hirudinaria sp. International Journal of Aquatic Science . 2016;7:19–24. [Google Scholar]
- 56.Bahmani M. K., Banihabib E. Comparative assessment of the antiannelida (Limnatis nilotica) activity of nicotine with niclosamide. Global Veterinaria . 2013;10:153–157. [Google Scholar]
- 57.Bahmani M., Karamati S. A., Banihabib E., Saki K. Comparison of effect of nicotine and levamisole and ivermectin on mortality of leech. Asian Pacific Journal of Tropical Disease . 2014;4(Suppl 477):p. S480. doi: 10.1016/s2222-1808(14)60493-x. [DOI] [Google Scholar]
- 58.Abebe G., Dawson L. J., Detweiler G., Gipson T. A., Sahlu T. Hagenia abyssinica (Kosso) for internal parasite control in goats. In: Merkel M. R., Abebe G., Goetsch A. L., editors. Proceedings of a conference the opportunities and challenges of enhancing goat production in East Africa, Awassa, 2000. (E (Kika) de la Garza Institute for Goat Research . Langston, OK, USA: Langston University; 2000. pp. 190–195. [Google Scholar]
- 59.Thomsen H., Reider K., Franke K., et al. Characterization of constituents and anthelmintic properties of Hagenia abyssinica. Scientia Pharmaceutica . 2012;80(2):433–446. doi: 10.3797/scipharm.1109-04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Amsalu N., Bezie Y., Fentahun M., Alemayehu A., Amsalu G. Use and conservation of medicinal plants by indigenous people of gozamin wereda, East gojjam zone of amhara region, Ethiopia: an ethnobotanical approach. Evidence-Based Complementary and Alternative Medicine . 2018;2018:23. doi: 10.1155/2018/2973513.2973513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Eshete A. M., Kelbessa E., Dalle G. Ethnobotanical study of medicinal plants in guji agro-pastoralists, blue hora district of Borana zone, Oromia region, Ethiopia. Journal of Medicinal Plants Studies . 2016;4:170–184. [Google Scholar]
- 62.Atinafu K., Shimels A., Akalu M., Getachew M. An ethnoveterinary study of medicinal plants used for the management of livestock ailments in selected kebeles of dire dawa administration, eastern Ethiopia. Journal of Plant Sciences . 2017;5:34–42. [Google Scholar]
- 63.Yemane B., Berhane Y., Surender Reddy D. K. Ethnobotanical study of medicinal plants in sub region logo anseba, region gash barka, Eritrea. IOSR Journal of Pharmacy and Biological Sciences . 2016;11(04):63–73. doi: 10.9790/3008-1104046373. [DOI] [Google Scholar]
- 64.Belayneh A., Asfaw Z., Demissew S., Bussa F. Medicinal plants potential and use by pastoral and agro-pastoral communities in Erer Valley of Babile Woreda, Eastern Ethiopia. Journal of Ethnobiology and Ethnomedicine . 2012;8:12–16. doi: 10.1186/1746-4269-8-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Giday M., Asfaw Z., Elmqvist T., Woldu Z. An ethnobotanical study of medicinal plants used by the Zay people in Ethiopia. Journal of Ethnopharmacology . 2003;85(1):43–52. doi: 10.1016/s0378-8741(02)00359-8. [DOI] [PubMed] [Google Scholar]
- 66.Feyera T., Mekonnen E., Wakayo B. U., Assefa S. Botanical ethnoveterinary therapies used by agro-pastoralists of Fafan zone, Eastern Ethiopia. BMC Veterinary Research . 2017;13(1):p. 232. doi: 10.1186/s12917-017-1149-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Atnafu H., Awas T., Alemu S., Wube S. Ethnobotanical study of medicinal plants in selale mountain ridges, North Shoa, Ethiopia. Biodiversity International Journal . 2018;2:567–577. [Google Scholar]
- 68.Wan Norhana M. N., Kua B. C., Liyana R. Evaluation of selected plant extracts for in vitro anti-marine leech (Zeylanicobdella arugamensis) activity. Tropical Biomedicine . 2021;38:22–129. doi: 10.47665/tb.38.1.021. [DOI] [PubMed] [Google Scholar]
- 69.Teklehaymanot T. Ethnobotanical study of knowledge and medicinal plants use by the people in Dek Island in Ethiopia. Journal of Ethnopharmacology . 2009;124(1):69–78. doi: 10.1016/j.jep.2009.04.005. [DOI] [PubMed] [Google Scholar]
- 70.Bekalo H. T., Demissew S., Asfaw Z. An ethnobotanical study of medicinal plants used by local people in the lowlands of konta special wereda, southern nations, nationalities and peoples regional state, Ethiopia. Journal of Ethnobiology and Ethnomedicine . 2009;5:3–26. doi: 10.1186/1746-4269-5-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Abdurhman N. Addis Ababa, Ethiopia: Addis Ababa University; 2010. Ethnobotanical study of medicinal plants used by local people in Ofla Wereda, Southern Zone of Tigray region, Ethiopia. MSc thesis. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Ethnoveterinary data were stored in a computer available at the Aklilu Lemma Institute of Pathobiology (ALIPB), Addis Ababa University (AAU), and the Faculty of Veterinary Medicine, Hawassa University. Readers may request the institutions for permission to get access to the data.


