Abstract
Background:
Several national guidelines include recommendations for a minimum duration of antidepressant treatment, but these vary from 4–9 months after remission. We aimed to investigate whether there is an optimal minimum duration of antidepressant treatment to reduce relapse risk.
Methods:
A Danish population-based cohort study among 89,442 adults who initiated antidepressants for depression treatment aged 18–60 years, from 2006–2015. We defined antidepressant discontinuation as ≥30 days without treatment. We estimated hazard ratios (HRs) with 95% confidence intervals (CIs) to indicate the risk of restarting antidepressants among those who discontinued antidepressants with <4, 4–6, and 7–9 months of use compared with discontinuation after 10–12 months.
Results:
For individuals on antidepressant treatment <4, 4–6, 7–9 and 10–12 months, cumulative incidence of restarting treatment within one year was 37.4% (95% CI: 36.9–37.8%), 35.1% (95% CI: 34.6–35.7%), 35.0% (95% CI: 34.2–35.8%) and 32.8% (95% CI: 31.7–34.0%), respectively. Individuals on antidepressants <10 months versus 10–12 months had higher risk of restarting antidepressants: the HR for antidepressant treatment <4 months was 1.21 (95% CI: 1.16–1.27), 4–6 months 1.11 (95% CI: 1.06–1.17), and 7–9 months 1.09 (95% CI: 1.04–1.15).
Limitations:
We were not able to ascertain the reasons why individuals discontinued antidepressants, and systematic errors from unmeasured confounders cannot be ruled out.
Conclusions:
Based on our findings, a minimum of 10–12 months of treatment appears to be preferable if there is concern about relapse after discontinuation.
Keywords: Antidepressant, cohort, discontinuation, duration of treatment, population-based, relapse
1. Introduction
Major depression is the most common psychiatric disorder in adults, with an estimated lifetime prevalence of 15–18% worldwide (Bromet et al., 2011); and it is the third leading cause of disability (GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. 2018). Guidelines recommend antidepressants as front-line agents in the treatment of moderate-to-severe depression in adults(American Psychiatric Association, 2010; Kessing, 2018; National Institute for Health and Care Excellence (NICE), 2009; NHG-werkgroep Depressie, 2019; World Health Organization (WHO), 2020). While recommendations exist regarding minimum duration for antidepressant treatment, published clinical guidelines and recommendations vary between countries (American Psychiatric Association, 2010; Kennedy et al., 2016; Kessing, 2018; National Institute for Health and Care Excellence (NICE), 2009; NHG-werkgroep Depressie, 2019). Normally, the duration is related to treatment length once remission is achieved. Most guidelines recommend a minimum of 6 months treatment after remission (complete relief of depressive symptoms and the restoration of social and occupational functioning (Kessing, 2018; National Institute for Health and Care Excellence (NICE), 2009; NHG-werkgroep Depressie, 2019). However, the American Psychiatric Association suggests continued treatment for 4–9 months after achieving remission, and the Canadian Network for Mood and Anxiety Treatments for 6–9 months (American Psychiatric Association,2010; Kennedy et al., 2016). In clinical practice, discontinuation of treatment with antidepressants is challenging and requires careful planning, and concerns about relapse following discontinuation understandably influence decisions about the duration of treatment.
While antidepressants are proven to be more effective than placebo in treating depression (Cipriani et al., 2018; Kato M., et al., 2020), they are no panacea: not all patients respond to antidepressant treatment and many experience side effects (Bull et al., 2002; Kennedy et al., 2016). Consequently, early discontinuation rates are high, with approximately half of the patients discontinuing within 6 months (Bushnell et al., 2016; Hansen et al, 2010). A key concern related to early discontinuation of antidepressants is relapse or worsening of symptoms, which can result in having to restart treatment and a prolonged disease course. Much of the current evidence on the minimum duration of antidepressant treatment comes from randomized controlled trials. A meta-analysis of placebo-controlled trials suggested that 18% of patients who continued antidepressants relapsed compared to 37% who discontinued, and the effect of antidepressant maintenance persists for about 6 months (Borges et al., 2014). Although randomized controlled trials are the gold standard for testing treatment efficacy, they often address active treatment and exclude subjects with significant comorbidity, which tends to bias the study in favor of antidepressant continuation. Therefore, it is difficult to extrapolate to broader population-based depressed subjects from the results of randomized controlled trials and translate them directly into standard recommendations for clinical care. Non-randomized observational studies using administrative data can address some of the limitations of randomized controlled trials and provide large real-world cohorts for pharmacoepidemiological studies, which are currently lacking.
To provide evidence for a minimum recommended duration of antidepressant treatment in order to reduce relapse risk, we used data from a nationally representative population. We assessed whether antidepressant discontinuation earlier than the currently recommended minimum treatment duration was associated with an elevated risk of relapse, indicated by restarting antidepressants.
2. Methods
2.1. Data sources
We conducted a population-based cohort study on individuals who initiated antidepressant treatment between 2006 and 2015 using Danish registry data. All residents in Denmark are assigned a unique 10-digit individual personal identification number at birth or upon immigration, recorded in the Civil Registration System (Pedersen, 2011). This can be used for linkage between and within all national registers. The Danish National Prescription Registry includes records of all prescriptions dispensed to Danish residents in retail pharmacies since 1995 (Kildemoes et al., 2011). The register includes the dispensing date, the dispensed drugs defined using the Anatomic Therapeutic Chemical (ATC) classification code, number of defined daily doses per package, and number of packages. Treatment indication was added from April 2004 onwards (Denmark Statistics, 2013), but there is substantial missing data for this variable until 2006. The Danish Psychiatric Central Research Register contains information on all treatments in psychiatric hospitals and psychiatric wards in general hospitals from 1969 onwards and includes outpatient treatments since 1995 (Mors et al., 2011). The International Classification of Diseases, eighth revision (ICD-8) was used until 1993 and tenth revision (ICD-10) from 1994 onwards.
2.2. Study population
We identified 231,267 individuals born after 1955 who redeemed their first antidepressant prescription for depression treatment (indication codes 168 and 270) (Hvidberg et al., 2016) between age 18 to 60 years, from 2006 to 2015 (Figure 1), through the linkage between the Danish Civil Registration System and the Danish National Prescription Registry. We restricted analyses to new users (rather than those who had had prescriptions prior to age 18 years or before 2006) because such a design allows us to mitigate potential bias owing to previous antidepressant exposure influencing the current treatment strategy. To ensure that we included only individuals with incident depression, we excluded 37,597 individuals with a diagnosis of psychiatric disorders (ICD-8 codes: 290-315 and ICD-10 codes: F00-F99) and 59,401 individuals who received any other psychotropic prescriptions (N05 and N06 in ATC codes excluding N06A) before the first antidepressant prescription.
Figure 1.
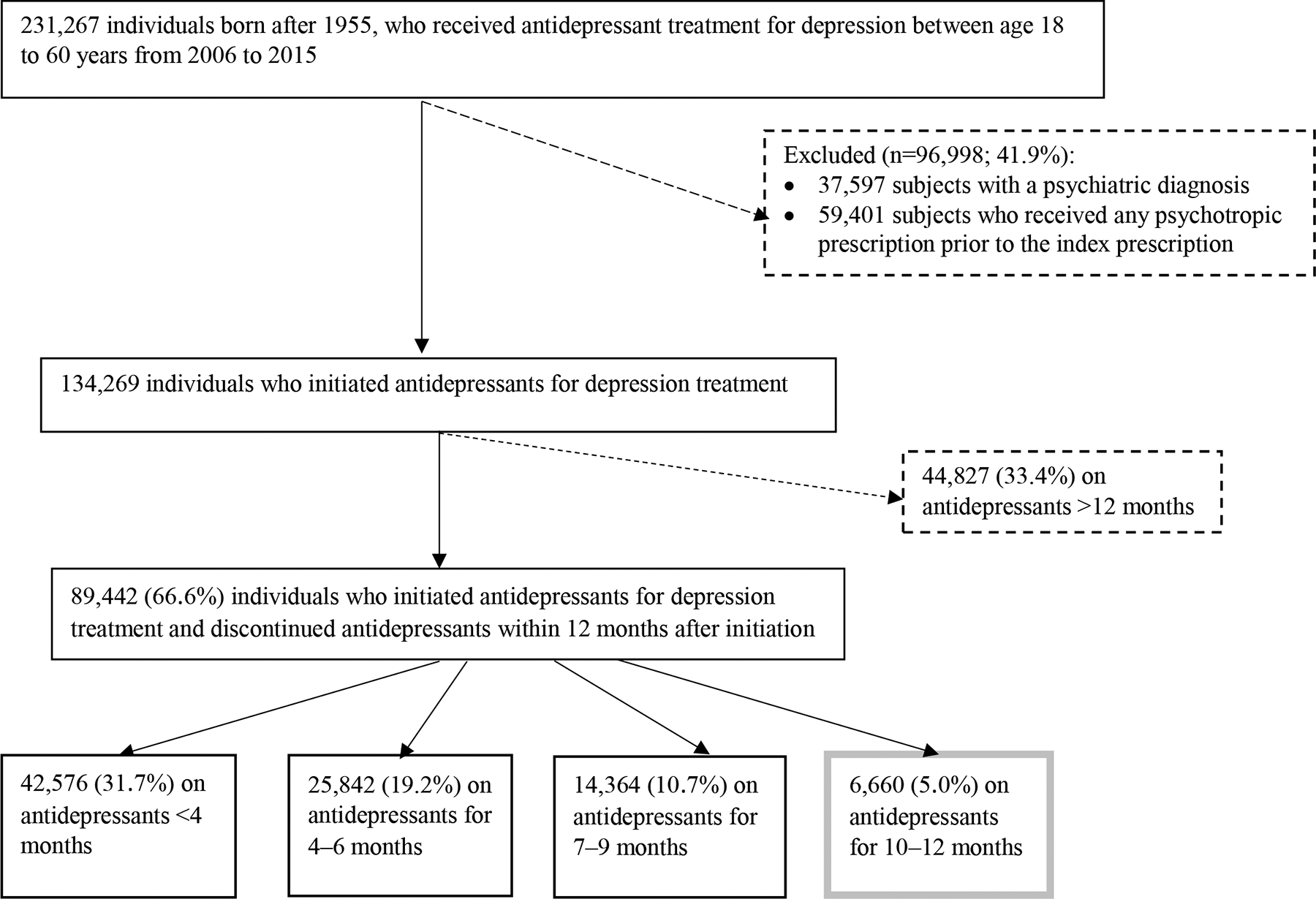
Flowchart of identifying the study population
International guidelines recommend patients stay on antidepressant treatment for at least 4–9 months after achieving remission, which takes typically 1.5–3 months after treatment initiation (American Psychiatric Association, 2010; Kessing, 2018; National Institute for Health and Care Excellence (NICE), 2009; NHG-werkgroep Depressie,2019; World Health Organization (WHO), 2020). Therefore, we focused on the individuals who discontinued antidepressants within 12 months after initiating antidepressants (n=89,442) to explore whether antidepressant discontinuation prior to the recommended 9 months after remission was associated with an elevated risk of relapse. Our reference group comprised individuals who discontinued antidepressant treatment between 10–12 months of use, which was based on considerations illustrated in Figure 2.
Figure 2.
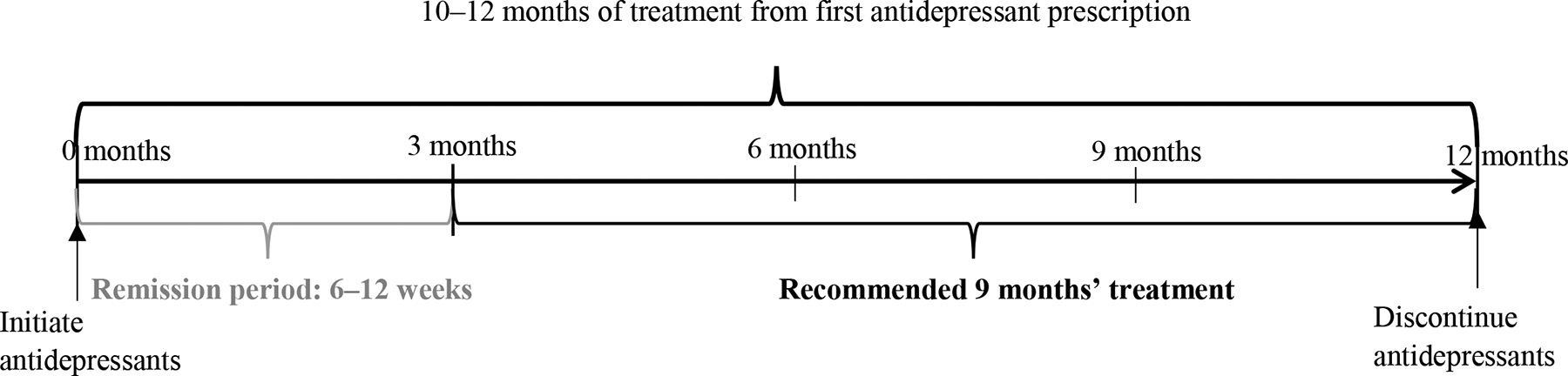
The rationale for the selection of individuals who were on antidepressants for 10–12 months before discontinuation as the comparison group
Please note that we did not have information on the time at remission, and therefore, we applied an average remission period of 6 to 12 weeks based on the current guidelines.
2.3. Exposure of interest: Antidepressant discontinuation
Information on antidepressant use was obtained from the Danish National Prescription Registry, identified with the relevant ATC code for antidepressants (N06A). We calculated the number of days each prescription was expected to last by multiplying the number of defined daily doses per package by the number of packages dispensed. Prescriptions for the same ATC code issued on the same day were counted as a single prescription, and the supplied amounts were combined (Coupland et al., 2015). From this, we could ascertain the date that the redeemed supply was expected to last until.
We defined antidepressant discontinuation based on the supply of antidepressants (number of days), allowing a 30-day grace period to account for missed doses (Bushnell et al., 2016). If another prescription was not redeemed before the date when the supply was expected to finish plus the 30-day grace period, the individual was considered to have discontinued antidepressants on that date. If an individual redeemed two or more prescriptions for each prescription dispensing date, the days of supply were added to a 30-day grace period, and the date of discontinuation was defined by the longest supply of the antidepressant. Treatment duration was calculated as the time from antidepressant initiation to discontinuation. Those who discontinued antidepressant treatment prior to 10 months of use were categorized into three groups according to treatment duration before discontinuation: <4, 4–6, or 7–9 months.
2.4. Outcome of interest: restarting antidepressants
Restarting antidepressant treatment was used as an indicator of depression relapse (Cohen et al, 2004). Individuals who redeemed a prescription for an antidepressant after the supply period plus 30-day grace period and within one year off treatment were considered to have restarted antidepressants.
2.5. Covariates
We adjusted for age at antidepressant initiation, sex, and a number of baseline characteristics at the time of antidepressant discontinuation: highest education (mandatory school, i.e., nine years at school/above mandatory school), cohabitation status (married or cohabiting/single, divorced or widowed), non-psychiatric comorbidity based on the 19 conditions included in the Charlson Comorbidity Index (Christensen et al. 2011), and previous suicide attempts (yes, or no). We retrieved data on comorbidity from the Danish National Patient Registry (Schmidt et al., 2015). Suicide attempts were ascertained if an individual had an inpatient or outpatient visit for self-harm identified in the Danish Psychiatric Central Research Register and the Danish National Patient Register (Gasse et al.,2018). The detailed criteria for defining suicide attempts can be found in the supplementary material.
We also controlled for covariates that indicated the severity of depression ascertained between antidepressant initiation to discontinuation: two or more types of antidepressants with different ATC codes; antidepressant treatment for other indications (anxiety, insomnia, and other disorders); concomitant use of benzodiazepine (ATC codes N05BA, N05CD, and N05CF); concomitant use of other psychotropic drugs (ATC codes N05 and N06 excluding N05BA, N05CD, N05CF, and N06A); inpatient, emergency room, or outpatient visit for psychiatric disorders (ICD-10 codes of F chapter excluding F70–F79); substance abuse disorder (ICD-10 codes F10–F19); and psychiatric diagnosis (depression, neurotic, stress-related and somatoform disorders, other psychiatric diagnoses, or no psychiatric diagnosis). The calendar year of the first prescription was included in the models to account for a possible change in prescription patterns across our defined study period.
2.6. Statistical analysis
We followed all individuals from the date of antidepressant discontinuation until the first of the following events: restarting antidepressants (our defined indicator for relapse), one-year off-treatment, emigration, death, or December 31, 2016. The maximum follow-up time was one year after discontinuing treatment, as restarting antidepressants after this time period is more likely to be due to a new episode of depression rather than relapse.
We constructed Kaplan-Meier curves to illustrate the probability of restarting antidepressants within one year of discontinuation. We estimated the hazard ratios (HRs) with 95% confidence intervals (CIs) to indicate the risk of restarting antidepressants among those who discontinued antidepressants <4, 4–6, and 7–9 months of use compared with our defined reference category: discontinuation after treatment for 10–12 months. HRs were calculated using proportional Cox regression models, with adjustment for the previously listed covariates. Proportionality was verified by visually inspecting “log-log” plots. Data were missing in 8.6% of subjects for any of the covariates; we applied 20 imputations using the Markov Chain Monte Carlo technique for imputing missing values (Royston, et al., 2011). Analyses were performed in Stata, version 15.0 (Stata Corp, College Station, TX).
Sensitivity analysis
Acute withdrawal symptoms after treatment discontinuation may lead to individuals restarting antidepressants, and such symptoms typically emerge within a few days of discontinuation (Fava et al., 2018). Relapse of depressive symptoms, on the other hand, tend to develop more than two weeks after discontinuation (Borges et al., 2014). To exclude individuals who restarted antidepressants due to withdrawal symptoms (rather than relapse), we repeated analyses starting follow-up two weeks after discontinuation. Furthermore, we examined how robust our findings were to a less restrictive grace period and used a minimum of 45 days between the end of one prescription and the next prescription to define antidepressant discontinuation, in contrast to the 30-day grace period applied in the primary analyses. Last, to test whether the observed associations were attributable to our selected models where we adjusted for all covariates, we applied 1:2 propensity-score matching to control for confounding in a different approach (Austin, 2011). The propensity score was the predicted probability of continuing the treatment for 10–12 months as opposed to discontinuing the treatment <4 months, 4–6 months, and 7–9 months, estimated through logistic regression with all of the covariates mentioned above. We constructed three cohorts by matching each individual who was on treatment for 10–12 months to two individuals who discontinued the treatment <4 months, two individuals who discontinued 4–6 months, and two individuals who discontinued 7–9 months on propensity score using the nearest neighbor matching algorithm, within caliper widths of 0.2 without replacement (Austin, 2011). Stratified Cox regression models were used to estimate the HR of restarting antidepressant treatment. Each matched pair constituted a separate stratum, and each stratum had its baseline hazard function.
2.7. Ethics
The study was approved by the Danish Data Protection Agency. No informed consent is required for purely register-based studies on the basis of encrypted data in accordance with the legislation in Denmark.
3. Results
Among the 89,442 individuals who discontinued antidepressant treatment within 12 months of their initial prescription, the mean age was 34.2 years (SD 10.6), and 56.9% (n=50,862) were females. The characteristics of individuals observed at the time of discontinuation are shown in Table 1, by treatment duration before discontinuation. Compared with individuals who were treated with antidepressants for 10–12 months before discontinuation, those who were treated <10 months differed in terms of several characteristics, including they were more likely to be males and to have a mandatory school education.
Table 1.
Characteristics of individuals by the duration of treatment. Values are numbers (percentages)
| Duration of antidepressant treatment | ||||
|---|---|---|---|---|
| Characteristics | Less than 4 months (n= 42,576) | 4–6 months (n=25,842) | 7–9 months (n=14,364) | 10–12 months (n=6,660) |
| Age at antidepressant initiation (years) | ||||
| 18–25 | 11,590 (27.2) ** | 7,963 (30.8) ** | 4,178 (29.1) | 1,854 (27.8) |
| 26–39 | 16,608 (39.0) | 10,186 (39.4) | 5,886 (41.0) | 2,798 (42.0) |
| 40–60 | 14,378 (33.8) | 7,693 (29.8) | 4,300 (29.9) | 2,008 (30.2) |
| Males | 18,615 (43.7) ** | 11,456 (44.3) ** | 5,932 (41.3) ** | 2,577 (38.7) |
| Highest education at the time of discontinuation | ||||
| Mandatory school | 16,006 (37.6) ** | 9,163 (35.5) ** | 4,516 (31.4) ** | 1,891 (28.4) |
| Above mandatory school | 23,225 (54.5) | 14,849 (57.5) | 9,159 (63.8) | 4,473 (67.2) |
| Missing | 3,345 (7.9) | 1,830 (7.1) | 689 (4.8) | 296 (4.4) |
| Cohabitation status at the time of discontinuation | ||||
| Married or cohabiting | 24,352 (57.2) * | 14,217 (55.0) ** | 8,160 (56.8) | 3,813 (57.3) |
| Single, divorced or widow | 17,199 (40.4) | 10,695 (41.4) | 5,682 (39.6) | 2,545 (38.2) |
| Missing | 1,025 (2.4) | 930 (3.6) | 522 (3.6) | 302 (4.5) |
| Physical comorbidity at the time of discontinuation | 6,171 (14.5) | 3,699 (14.3) | 1,963 (13.7) | 918 (13.8) |
| Prior suicide attempts at the time of discontinuation | 835 (2.0) | 513 (2.0) | 253 (1.8) | 118 (1.8) |
| Redemption of ≥2 types of antidepressants | 4,013 (9.4) ** | 4,048 (15.7) ** | 3,073 (21.4) ** | 1,666 (25.0) |
| Other indication for antidepressant treatment | ||||
| Anxiety disorders | 158 (0.4) ** | 373 (1.4) * | 329 (2.3) | 182 (2.7) |
| Other indications, mainly insomnia | 210 (0.5) | 266 (1.0) | 236 (1.6) | 121 (1.8) |
| Concomitant medication uses at the time of discontinuation | ||||
| Benzodiazepine | 2,680 (6.3) ** | 2,075 (8.0) ** | 1,292 (9.0) | 647 (9.7) |
| Other psychotropic medication | 1,041 (2.5) ** | 1,076 (4.2) ** | 842 (5.9) | 412 (6.2) |
| Psychiatric hospital contact at the time of discontinuation | ||||
| Outpatient | 1,137 (2.7) ** | 1,230 (4.8) ** | 939 (6.5) ** | 545 (8.2) |
| Inpatient or emergency room visit | 698 (1.6) ** | 617 (2.4) ** | 450 (3.1) | 238 (3.6) |
| Substance abuse disorders at the time of discontinuation | 154 (0.4) ** | 145 (0.6) * | 98 (0.7) | 54 (0.8) |
| Psychiatric diagnosis at the time of discontinuation | ||||
| No psychiatric diagnosis | 40,995 (96.3) ** | 24,273 (93.9) ** | 13,224 (92.1) ** | 6,011 (90.3) |
| Depression | 653 (1.5) | 708 (2.7) | 539 (3.8) | 358 (5.4) |
| Neurotic, stress-related and somatoform disorders | 570 (1.3) | 493 (1.9) | 350 (2.4) | 157 (2.4) |
| Other psychiatric diagnosis | 358 (0.8) | 368 (1.8) | 251 (1.7) | 134 (2.0) |
| Calendar year at antidepressant initiation | ||||
| 2006–2008 | 14,426 (33.9) ** | 6,171 (23.9) ** | 3,430 (23.9) ** | 1,403 (21.1) |
| 2009–2011 | 14,989 (35.2) | 9,855 (38.1) | 5,460 (38.0) | 2,550 (38.3) |
| 2012–2015 | 13,161 (30.9) | 9,816 (38.0) | 5,474 (38.1) | 2,707 (40.6) |
The p-values were <0.05,
The p-values were <0.01 for the comparison of differences between those who were on antidepressants <4 months, 4–6 months, and 7–9 months with those who were on antidepressants for 10–12 months, using chi-square tests.
Overall, 35.8% (32,033 out of 89,442 individuals) of individuals restarted antidepressants, the indicator of relapse, within one-year off-treatment: for individuals treated with antidepressants <10 months 36.3% (95% CI: 35.9–36.6%) and 10–12 months 32.8% (95% CI: 31.7–34.0%). The cumulative incidence of relapse was <4 months 37.4% (95% CI: 36.9–37.8%), 4–6 months 35.1% (95% CI: 34.6–35.7%), 7–9 months 35.0% (95% CI: 34.2–35.8%) (Figure 3). Risk of relapse was higher among those who were on antidepressants <10 months before discontinuation, in comparison to those who were on antidepressants for 10–12 months, with the greatest risk observed among those who spent < 4 months on treatment (HR=1.21, 95% CI: 1.16–1.27). Furthermore, an elevated risk of relapse was also observed for treatment durations of 4–6 months (HR=1.11, 95% CI: 1.06–1.17) and 7–9 months (HR=1.09, 95% CI: 1.04–1.15) (Table 2).
Figure 3.
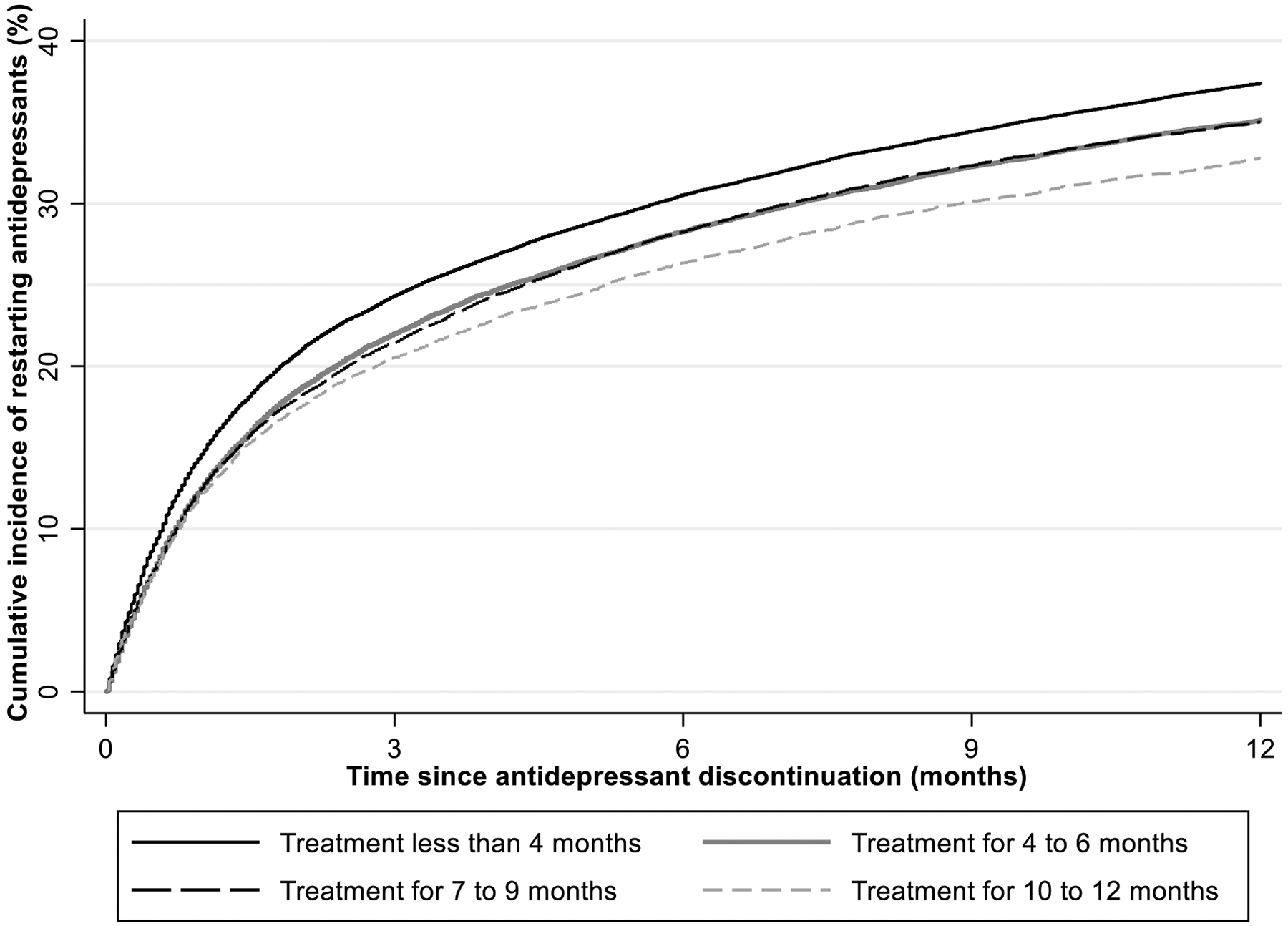
Kaplan Meier Curve indicating the probability of restarting antidepressants by the time of discontinuation
Table 2.
The hazard ratio of restarting antidepressants among those who discontinued antidepressants before 10 months of use, compared with individuals who discontinued antidepressants after 10–12 months
| Timing at antidepressant discontinuation | Cases | Person-years | Crude HR (95% CI) | Adjusted HR (95% CI) † |
|---|---|---|---|---|
| < 4 months | 15,863 | 30,411.3 | 1.18 (1.13–1.23) | 1.21 (1.16–1.27) |
| 4–6 months | 9,032 | 18,912.1 | 1.09 (1.04–1.14) | 1.11 (1.06–1.17) |
| 7–9 months | 4,987 | 10,455.1 | 1.08 (1.03–1.14) | 1.09 (1.04–1.15) |
| 10–12 months | 2,151 | 4,891.7 | 1 (ref) | 1 (ref) |
Models for adjusted HRs include age at the first antidepressant prescription, sex, highest education, cohabitation status, physical comorbidity, antidepressants prescribed for the treatment of anxiety disorders, insomnia or other indications, a concomitant of the benzodiazepine or other psychotropic medication, psychiatric hospital contact, substance abuse disorders and psychiatric diagnoses from antidepressant initiation to discontinuation, and calendar year at antidepressant initiation.
Sensitivity analysis
We applied two additional sets of analyses aimed at testing the time frame we used for defining the restart of antidepressants or antidepressant discontinuation. When redefining restart of antidepressants as a redeemed prescription at least two weeks after discontinuation (as opposed to the first day after discontinuation in our primary analyses), the probability of relapse was reduced from 36.0% (95% CI:35.7–36.3%) to 30.6% (95% CI: 30.3–30.9%). However, the relative risk of relapse after discontinuation was similar in magnitude: <4 months on treatment (HR=1.16, 95% CI: 1.11–1.21), 4–6 months (HR=1.09, 95% CI: 1.04–1.14), 7–9 months (HR=1.12, 95% CI: 1.07–1.18), in comparison with those who were on antidepressants for 10–12 months. When applying the less restrictive grace period of 45-days to define antidepressant discontinuation, findings were similar; however, the associations between antidepressant treatment for < 10 months versus for 10–12 months with restarting antidepressants were attenuated (STable 1 in the supplementary material). When applying propensity score matching as an alternative method for confounder control, the relative risk of relapse after discontinuation remained consistent: <4 months on treatment (HR=1.20, 95% CI: 1.14–1.27), 4–6 months (HR=1.10, 95% CI: 1.04–1.16), 7–9 months (HR=1.07, 95% CI: 1.01–1.13), in comparison with those who were on antidepressants for 10–12 months (STable 2). The distributions of propensity score before matching among individuals on antidepressant treatment for <4 months, 4–6 months, 7–9 months versus 10–12 months are shown in SFigure 1–3.
4. Discussion
In this population-based longitudinal study, we found that over one-third of individuals who discontinued antidepressants restarted treatment within one year. Overall, discontinuation of antidepressant treatment with <10 months of initiation was associated with an increased risk of restarting treatment compared to discontinuation after 10–12 months on antidepressants. The greatest relapse risk was associated with discontinuation of antidepressant treatment <4 months after initiation.
Patients may choose to stop treatment for various reasons, including lack of efficacy, experiencing adverse events that outweigh the benefits, or an individual decision to be medication-free when no depression symptoms are present (Demyttenaere et al., 2001). Our study is based on population registers, and information on the reason for discontinuation and details regarding symptoms and the disease course are lacking. Evidence suggests that not all patients respond to antidepressant treatment, and, on average, it takes seven weeks to achieve remission (Trivedi et al. 2006). We speculate that patients with a short duration of treatment may discontinue antidepressants because of inadequate initial treatment response or significant side effects. Additionally, we speculate these patients are more likely to stop their treatment abruptly, leading to a higher risk of relapse (Baldessarini et al., 2010). On the other hand, patients with a longer treatment duration may be more likely to achieve remission and have a lower risk of subsequent relapse. However, regardless of the underlying reasons for stopping treatment, our results demonstrate that about one in three individuals who discontinued antidepressants likely had symptoms severe enough to prompt their reintroduction.
In line with previous findings (Borges et al., 2014), we note that around two-thirds of individuals discontinued antidepressants without restarting treatment. In contrast, around one-third of individuals who discontinued treatment restarted antidepressants, which is suggestive of relapse within the following 12 months. Although it is impossible to outline a minimum duration for antidepressant treatment that fits all individuals, most national antidepressant treatment guidelines give general recommendations informed by the natural course of depression. Most countries in Europe recommend continued treatment for at least six months after achieving remission (Kessing, 2018; National Institute for Health and Care Excellence (NICE), 2009; NHG-werkgroep Depressie,2019), while 6–9 months is suggested in Canada (Kennedy et al., 2016) and 4–9 months in the USA (American Psychiatric Association, 2010). In the present study, we assumed remission mostly occurs 1.5–3 months after initiation of treatment. We found the lowest relapse risk among individuals on antidepressants for 10–12 months before discontinuation. Please note that 10–12 months of the treatment period in our data covers an assumed 1.5–3 months of treatment until remission plus subsequent 7–10.5 months in maintenance treatment. Although speculative, the 10–12 months treatment period in our data supports the minimum treatment recommendation of most guidelines, whereas the four months suggested by the US guideline as the minimum treatment duration seems too short based on our findings. However, it should be noted that the absolute risk difference (about 3.5%) of restarting antidepressants between individuals on antidepressants for less than ten months and individuals on antidepressants for 10–12 months is relatively small. Because long-term antidepressant treatment may result in severe side effects (Moret C, et al., 2009), a shorter duration of treatment may be favorable for patients experiencing significant side effects. Future studies should investigate if other benefits are expected besides a lower risk of restarting antidepressants within 12 months after discontinuation to guide individual decision on treatment duration after remission is obtained.
Strengths and limitations
To our knowledge, this is the first study on the association between treatment duration and risk of antidepressant reintroduction after discontinuation. It considers the effectiveness of antidepressants at preventing relapse by treatment duration in a nationally representative population. Our study comprised a wide range of symptom severity indicators in patients treated in primary care. The relapse rate found in our study was comparable to the rate of 37% previously reported in the literature (Borges et al., 2014). This supports the use of restarting antidepressants as a measure of relapse. Moreover, the linkage of several national registers enables us to control for several covariates, for instance, psychiatric diagnosis, suicide attempts, concomitant medication use, and other indications for antidepressant treatment, such as anxiety disorders or insomnia.
Our study also has limitations. First, our study was based on administrative data, and we were not able to ascertain why individuals discontinued antidepressants or if they achieved remission. However, the use of treatment duration, although crude, is a straightforward measure that can be directly translated into clinical care and support treatment discontinuation considerations. Second, patients who filled a prescription may not take these antidepressants, and patients defined as in treatment may have taken the drugs for a shorter period than our identified treatment period. Moreover, calculating the duration of antidepressant treatment on the basis of the number of prescribed pills may be inaccurate. We may, therefore, misclassify the duration of antidepressant treatment that potentially can lead to an underestimation of the relapse risk associated with premature antidepressant discontinuation. Third, we do not have detailed information on the mode of stopping and cannot differentiate between gradual, abrupt, or rapid discontinuation. Fourth, we used restarting antidepressants as a proxy of relapse, which we acknowledge is a crude measure of relapse. We also acknowledge that individuals with relapse do not necessarily reinitiate antidepressant treatment but could seek other alternative therapies such as cognitive therapy. Fifth, as for all observational studies based on administrative data, we cannot rule out residual confounding, as some personality traits (e.g., neuroticism) and unhealthy lifestyle factors may have predisposed to both poor adherence to antidepressant treatment with early treatment discontinuation and an increased risk of relapse (Axelsson, et al. 2011). Sixth, we applied an average remission period of 6 to 12 weeks based on the current guidelines; however, the duration of symptoms may vary between individuals. Finally, patients do not discontinue antidepressant treatment at random, and patients with milder symptoms, shorter duration of symptoms, more side effects, inadequate treatment response, or patients’ lack of conviction that antidepressants are needed are more inclined to discontinue (Falcaro et al., 2019; Hansen et al., 2007). Overall, it is possible that the observed differences in the risk of relapse by durations of antidepressant treatment are at least partially attributable to the unmeasured factors.
5. Conclusions
One in three patients relapsed within one year after antidepressant discontinuation. Antidepressant treatment for <10 months was associated with higher relapse risk, and the risk was highest in individuals who were on treatment for <4 months. Based on our overall findings, a minimum treatment duration of 10–12 months appears to be preferable if there is a concern about relapse after discontinuation.
Supplementary Material
Highlights.
It remains unknown whether there is a minimum duration of antidepressant treatment.
We conducted a population-based cohort study comprising 89,442 adults in Denmark.
Individuals on antidepressants <10 versus 10–12 months had a higher relapse risk.
A minimum of 10–12 months of treatment is preferable if the concern is relapse.
Funding
This study is supported by the National Institute of Mental Health (NIMH) (R01MH122869). Liu X. is also supported by the European Union’s Horizon 2020 research and innovation programme under the Marie Sklodowska-Curie grant agreement No 891079. Munk-Olsen T. is also supported by iPSYCH, the Lundbeck Foundation Initiative for Integrative Psychiatric Research (R155-2014-1724), the Lundbeck Foundation (R313-2019-569), AUFF NOVA (AUFF-E 2016-9-25), and Fabrikant Vilhelm Pedersen og Hustrus Legat. The funders of the study had no role in study design, data analysis, data interpretation, writing, or submission for publication.
Footnotes
Declaration of competing interest: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in the paper.
References
- American Psychiatric Association.(2010). Practice guideline for the treatment of patients with major depressive disorder. https://psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/mdd.pdf (Accessed May 8 2020).
- Austin PC (2011). An Introduction to Propensity Score Methods for Reducing the Effects of Confounding in Observational Studies. Multivariate Behav Res, 46(3), 399–424. doi: 10.1080/00273171.2011.568786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Axelsson M, Brink E, Lundgren J, Lötvall J. The influence of personality traits on reported adherence to medication in individuals with chronic disease: an epidemiological study in West Sweden. PLoS One. 2011;6(3):e18241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baldessarini RJ, Tondo L, Ghiani C, Lepri B. (2010). Illness risk following rapid versus gradual discontinuation of antidepressants. Am J Psychiatry, 167(8):934–41. doi: 10.1176/appi.ajp.2010.09060880. [DOI] [PubMed] [Google Scholar]
- Borges S, Chen YF, Laughren TP, Temple R, Patel HD, David PA, Mathis M, Unger E, Yang P, & Khin NA (2014). Review of maintenance trials for major depressive disorder: a 25year perspective from the US Food and Drug Administration. J Clin Psychiatry, 75(3), 205–214. doi: 10.4088/JCP.13r08722 [DOI] [PubMed] [Google Scholar]
- Bromet E, Andrade LH, Hwang I, Sampson NA, Alonso J, de Girolamo G, de Graaf R, Demyttenaere K, Hu C, Iwata N, Karam AN, Kaur J, Kostyuchenko S, Lépine J, Levinson D, Matschinger H, Mora MEM, Browne MO, Posada-Villa J, Viana MC, Willianms DR, & Kessler RC (2011). Cross-national epidemiology of DSM-IV major depressive episode. BMC Med, 9, 90. doi: 10.1186/1741-7015-9-90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bull SA, Hu XH, Hunkeler EM, Lee JY, Ming EE, Markson LE, & Fireman B (2002). Discontinuation of use and switching of antidepressants: influence of patient-physician communication. JAMA, 288(11), 1403–1409. doi: 10.1001/jama.288.11.1403 [DOI] [PubMed] [Google Scholar]
- Bushnell GA, Sturmer T, White A, Pate V, Swanson SA, Azrael D, & Miller M (2016). Predicting persistence to antidepressant treatment in administrative claims data: Considering the influence of refill delays and prior persistence on other medications. J Affect Disord, 196, 138–147. doi: 10.1016/j.jad.2016.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen S, Johansen MB, Christiansen CF, Jensen R, & Lemeshow S (2011). Comparison of Charlson comorbidity index with SAPS and APACHE scores for prediction of mortality following intensive care. Clin Epidemiol, 3, 203–211. doi: 10.2147/clep.S20247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cipriani A, Furukawa TA, Salanti G, Chaimani A, Atkinson LZ, Ogawa Y, Leucht S, Ruhe HG, Turner EH, Higgins JPT, Egger M, Takeshima N, Hayasaka Y, Imai H, Shinohara K, Tajika A, Ioannidis JPA, & Geddes JR (2018). Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis. Lancet, 391(10128), 1357–1366. doi: 10.1016/s0140-6736(17)32802-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen LS, Altshuler LL, Stowe ZN, & Faraone SV (2004). Reintroduction of antidepressant therapy across pregnancy in women who previously discontinued treatment. A preliminary retrospective study. Psychother Psychosom, 73(4), 255–258. doi: 10.1159/000077745 [DOI] [PubMed] [Google Scholar]
- Coupland C, Hill T, Morriss R, Arthur A, Moore M, & Hippisley-Cox J (2015). Antidepressant use and risk of suicide and attempted suicide or self harm in people aged 20 to 64: cohort study using a primary care database. BMJ, 350, h517. doi: 10.1136/bmj.h517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demyttenaere K, Enzlin P, Dewé W, Boulanger B, De Bie J, De Troyer W, & Mesters P (2001). Compliance with antidepressants in a primary care setting, 1: Beyond lack of efficacy and adverse events. J Clin Psychiatry, 62 Suppl 22, 30–33. [PubMed] [Google Scholar]
- Denmark Statistics. (2013). Håndbog til data i Lægemiddelstatistikregisteret [Handbook for data in the Product Statistics Register]. Retrieved from https://docplayer.dk/2089532-Haandbog-til-data-ilaegemiddelstatistikregisteret-senest-opdateret-februar-2013.html. (Accessed September 8 2020)
- Falcaro M, Ben-Shlomo Y, King M, Freemantle N, & Walters K (2019). Factors associated with discontinuation of antidepressant treatment after a single prescription among patients aged 55 or over: evidence from English primary care. Soc Psychiatry Psychiatr Epidemiol, 54(12), 1545–1553. doi: 10.1007/s00127-019-01678-x [DOI] [PubMed] [Google Scholar]
- Fava GA, Benasi G, Lucente M, Offidani E, Cosci F, & Guidi J (2018). Withdrawal Symptoms after Serotonin-Noradrenaline Reuptake Inhibitor Discontinuation: Systematic Review. Psychother Psychosom, 87(4), 195–203. doi: 10.1159/000491524 [DOI] [PubMed] [Google Scholar]
- Gasse C, Danielsen AA, Pedersen MG, Pedersen CB, Mors O, & Christensen J (2018). Positive predictive value of a register-based algorithm using the Danish National Registries to identify suicidal events. Pharmacoepidemiol Drug Saf, 27(10), 1131–1138. doi: 10.1002/pds.4433 [DOI] [PubMed] [Google Scholar]
- GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. (2018). Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet, 392(10159), 1789–1858. doi: 10.1016/s0140-6736(18)32279-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen RA, Dusetzina SB, Dominik RC, & Gaynes BN (2010). Prescription refill records as a screening tool to identify antidepressant non-adherence. Pharmacoepidemiol Drug Saf, 19(1), 33–37. doi: 10.1002/pds.1881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen HV, Kessing LV. Adherence to antidepressant treatment. Expert Rev Neurother. 2007. January;7(1):57–62. doi: 10.1586/14737175.7.1.57. [DOI] [PubMed] [Google Scholar]
- Hvidberg MF, Johnsen SP, Glumer C, Petersen KD, Olesen AV, & Ehlers L (2016). Catalog of 199 register-based definitions of chronic conditions. Scand J Public Health, 44(5), 462–479. doi: 10.1177/1403494816641553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kato M, Hori H, Inoue T Iga J, Iwata M, Inagaki T, Shinohara K, Imai H, Murata A, Mishima K, & Tajika A (2020). Discontinuation of antidepressants after remission with antidepressant medication in major depressive disorder: a systematic review and meta-analysis. Mol Psychiatry. 10.1038/s41380-020-0843-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy SH, Lam RW, McIntyre RS, Tourjman SV, Bhat V, Blier P, Hasnain M, Jollant F, Levitt AJ, MacQueen GM, Mclnerney SJ, Mclntosh D, Milev RV, Müller DJ, Parikh SV, Pearson NL, Ravindran A, Uher R, CANMAT depression Work Group. (2016). Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 Clinical Guidelines for the Management of Adults with Major Depressive Disorder: Section 3. Pharmacological Treatments. Can J Psychiatry, 61(9), 540–560. doi: 10.1177/0706743716659417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessing LV. (2018). Depression behandling. https://www.sundhed.dk/borger/patienthaandbogen/psyke/sygdomme/depression/depressionbehandling/ (Accessed August 5 2020)
- Kildemoes HW, Sorensen HT, & Hallas J (2011). The Danish National Prescription Registry. Scand J Public Health, 39(7 Suppl), 38–41. doi: 10.1177/1403494810394717 [DOI] [PubMed] [Google Scholar]
- Moret C, Isaac M, & Briley M (2009). Problems associated with long-term treatment with selective serotonin reuptake inhibitors. J Psychopharmacol. 2009;23(8):967–974. [DOI] [PubMed] [Google Scholar]
- Mors O, Perto GP, & Mortensen PB (2011). The Danish Psychiatric Central Research Register. Scand J Public Health, 39(7 Suppl), 54–57. doi: 10.1177/1403494810395825 [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence (NICE). (2009). Depression in adults: recognition and management. [CG90]. www.nice.org.uk/guidance/cg90 (Accessed April 8 2020). [PubMed]
- NHG-werkgroep Depressie. (2019). https://richtlijnen.nhg.org/standaarden/depressie. (Accessed 4 August 2020).
- Pedersen CB (2011). The Danish Civil Registration System. Scand J Public Health, 39(7 Suppl), 22–25. doi: 10.1177/1403494810387965 [DOI] [PubMed] [Google Scholar]
- Royston P, & White IR. (2011). Multiple Imputation by Chained Equations (MICE): Implementation in Stata. Journal of Statistical Software, 45(4):1–20. [Google Scholar]
- Schmidt M, Schmidt SA, Sandegaard JL, Ehrenstein V, Pedersen L, & Sørensen HT (2015). The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol, 7, 449–490. doi: 10.2147/clep.S91125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trivedi MH, Rush AJ, Wisniewski SR, Nierenberg AA, Warden D, Ritz L, Norquist G, Howland RH, Lebowitz B, McGrath PJ, Shores-Wilson K, Biggs MM, Balasubramani GK, Fava M, & STAR*D Study Team. (2006). Evaluation of Outcomes With Citalopram for Depression Using Measurement-Based Care in STAR*D: Implications for Clinical Practice. Am J Psychiatry, 163: 28–40. [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO). (2020). https://www.who.int/news-room/factsheets/detail/depression (Accessed July 8, 2020).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


