Abstract
Background/purpose
The formation of white spot lesions (WSLs) around fixed orthodontic attachments is a common complication during and following fixed orthodontic treatment, marking the result of a successfully completed treatment. This double-blind, randomized clinical trial study aims to investigate the varying effects of nano-silver, chlorhexidine (CHX) or fluoride mouthwashes on WSLs.
Materials and methods
Double-blind prospective randomized clinical trial, comprised of forty-two patients with mild to moderate crowding, were recruited for this study. Randomization and allocation to trial group were carried out by computer system in college of dentistry, university of Sulaimani from January 2020 to September 2020. The patients were divided into three groups (14 per group) according to the type of mouthwash used during the treatment (nano-silver, CHX or fluoride), using block randomization. The clinical examination for the presence of WSLs was recorded through visual examination of the upper and lower anterior teeth using the International Caries Detection and Assessment System (ICDAS II) score before bonding and at 30, 90 and 180 days after bonding of the upper and lower arches.
Results
The total number of patients was 42 (16 males and 26 females) with a mean age of 23.02 ± 3.841 (18–37) years old, distributed into three groups of 14 patients. There is significant difference in white spot lesions formation between the three groups; the mean of WSLs in nanosilver group is lower than CHX and fluoride group in 90 and 180 days of follow-up (P < 0.05).
Conclusion
Nano-silver mouthwash is more effective than CHX and fluoride mouthwash in reducing WSLs during orthodontic treatment.
Keywords: Chlorhexidine, Dental caries, Fluoride, Mouthwash, Nanosilver particles, Orthodontic appliances
Introduction
A common side-effect of fixed orthodontic treatment is white spot lesions (WSLs). The WSLs can be formed as a result of enamel demineralization and the dissolution of hydroxyapatite as a result of acidic by-products of the bacteria in the dental plaque.1 The incidence of WSLs during orthodontic treatments widely varies from 2 to 97%.2 After removal of the fixed appliances, these lesions are not easily resolved, and their total resolution is hardly achieved, which can affect the patient's satisfaction with their dental appearance, and untreated WSLs can lead to the formation of dental caries and the need for restorative treatment.3
White spot lesions in patients undergoing orthodontic treatment can be prevented with a multifactorial approach. Prevention should begin by educating and motivating the patient to comply with a non-cariogenic diet and careful observation of oral hygiene. Mechanical plaque control and removal should be done through the proper brushing of teeth surfaces with toothpaste containing fluoride.4 Fluoride ions prevent dental caries by modifying the bacterial metabolism in dental plaque through the inhibition of some enzymatic processes.5
In addition to fluoride, chlorhexidine (CHX) has the capacity to prevent and control caries as a result of its antimicrobial effect.6 Some studies showed that CHX is a useful adjunct in controlling the plaque of an orthodontic patient, though it has some side effects, such as brownish teeth, discoloration dorsum of the tongue and taste perturbation.7 Currently, neither fluoride nor CHX can prevent the formation of WSLs.8
Moreover, nanosilver (NS) mouthwash was introduced to the market and preferred as a result of its small size properties as the surface area of the nanoparticles allow for more contact with the bacterial cells. This is due to the capability of nanoparticles to penetrate bacteria and other microorganisms and destroy them. In addition, NS mouthwash has shown potent anti-plaque and anti-gingivitis activity.9
The antibacterial effect of silver on various microorganisms has been well documented since ancient times. It has been suggested that the inhibitory power of silver ions is due to its interaction with the thiol groups of proteins and the phospholipid portion of the bacterial membrane. Recently, NS particles have been used to prevent WSL in modules by adding it to the orthodontic primer, composite and adhesive or coating of orthodontic bands, brackets and arch wires.10,11 This study aims to compare the prevalence of WSLs in patients receiving orthodontic treatment with stainless steel conventional brackets and to investigate the effect of fluoride, CHX and NS mouthwash on WSLs.
Materials and methods
Ethical approval was obtained from the ethical committee of the College of Medicine at the University of Sulaimani with verdict number (7) on March 27, 2019 and registered in IRCT (registration number: IRCT20190611043870N1). Of the 104 total patients, there was an age range from 18 to 40 years old. The patients visited the College of Dentistry's dental clinic in Sulaimani for orthodontic purposes, where 50 patients were recruited for this randomized, double-blind clinical trial.
The full fixed appliance treatment involving upper and lower dentitions for a minimum of six months duration were applied. The inclusion criteria were as follows: patients were selected according to the Index of Orthodontic Treatment Need (IOTN 1, 2 and 3),12 patients were selected according to good oral hygiene, and patients were selected if they were considered healthy and non-smoking with no systemic medical conditions or routine medications. The exclusion criteria were as follows: if the patient demonstrated dentofacial deformities, if the patient were pregnant or lactating, if there were WSLs prior to treatment, and if the patient had received previous orthodontic treatment.
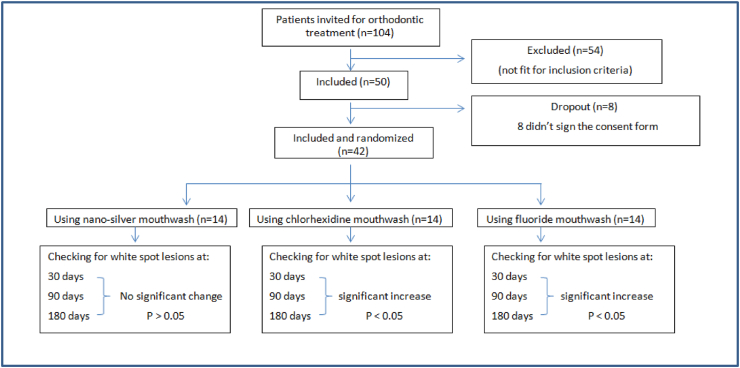
After clinical examination of the patients, those that satisfied the inclusion criteria for the study were then asked to sign informed consent. However, after protocol procedures were explained, eight patients did not wish to participate and did not sign the consent form. A flow chart with dropping out is presented in Fig. 1.
Figure 1.
Flow chart for participants and dropouts in the trial.
In this clinical trial, there are three groups. Open Epi software was used to determine sample size with a confidence level of 95, a power of 80. The minimum accepted participant for each group should be N = 13, according to Fleiss Statistical Methods.
After examining the patient to be fit for the inclusion criteria, the patient was sent to a room with a computer. Then, using Microsoft Excel, the patient was randomly administered a code that was 1, 2 or 3. Codes 1, 2 and 3 referred to a NS, CHX or fluoride mouthwash, respectively. Randomization was conducted using block randomization procedures based on the randomized group numbers given to patients in a sealed envelope. The envelope was opened once the intervention was assigned. The treatment was carried out based on the group assigned in the paper. The mouthwashes were placed into the same kind of containers and labeled with numbers 1, 2 and 3, and all of the patients were blind to the type of mouthwash they used.
Three weeks before the start of the treatment, all subjects received oral hygiene instructions per the correct use of a toothbrush and interdental brushes. All subjects were instructed to use the same fluoridated toothpaste (VITIS, Cerdanyola, Spain). All the patients were then submitted to fixed orthodontic treatment with stainless steel conventional brackets.
The patients were divided into three groups according to different treatment protocols. Group 1 was instructed to rinse with the NS mouthwash (CORAL, Carson city, NV, USA). Group 2 was instructed to rinse with the CHX mouthwash (PERIO.AID, Cerdanyola, Spain). Group 3 was instructed to rinse with the fluoride mouthwash (VITIS). All patients were instructed to use 5 ml of mouthwash for one minute twice daily for six months during the orthodontic treatment. The ingredients of the mouthwashes are shown in Table 1.
Table 1.
The ingredient of the mouthwashes.
| Mouthwash | Ingredient |
|---|---|
| Nanosilver mouthwash | Water, Nanosilver solution, Xylitol, Sorbitol, Aloe Barbadensis, Citric Acid, Melaleuca Alternifolia Leaf Oil, Peppermint and Polysorbate 20 |
| Chlorhexidine mouthwash | Aqua, Glycerin, Propylene Glycol, Xylitol, Peg 40 Hydrogenated Castor Oil, Methylparaben, Cetylpyridinium Chloride, Chlorhexidine Digluconate, Potassium Acesulfame, Ethylparaben, Sodium Saccharin, Neohesperidin Dichalcone, Aroma C.I. 42,051 |
| Fluoride mouthwash | Aqua, Glycerin, Propylene Glycol, Xylitol, Sodium Fluoride, Aloe Barbadensis Leaf Juice, Methylparaben, Cetylpyridinium Chloride, Allantoin, Potassium Acesulfame, Propylparaben, Menthone Glycerin Acetal, Aroma C.I. 19,140,C.I. 42,051 and Limonene |
The participants were motivated at monthly intervals by personal contact, a written instruction on how to use toothbrush and mouthwash on a regular basis. The patients were instructed to use a medium-sized toothbrush, brush their teeth thoroughly with a fluoridated toothpaste in the morning, before bed and after each meal or snack for a minimum of five minutes and to rinse their mouth with the designated mouth wash at least half an hour after brushing their teeth after breakfast and before bedtime. The patients were also instructed not to ingest any liquid or food for at least 30 min after using the mouthwash as it could decrease its efficacy.
All clinical examinations were conducted by two well-trained orthodontists, who were blind to the types of mouthwash used.
In this study, the naked eye method was used for the evaluation of WSLs, which is clinically relevant, more feasible and used in most of the studies.13 The visual examination of WSLs was done on the buccal surface of the upper and lower anterior teeth directly after clinical examinations. The labial surface of each tooth was divided into four areas (gingival, mesial, incisal and distal). Each tooth was assigned an International Caries Detection and Assessment System (ICDAS II) score14 (Table 2) by both examiners magnifying loupes and the aid of a mirror, clinical lightning, triplex syringe and a blunt probe. In case of a disagreement between the two examiners, a third observer (senior orthodontist) was required to perform a third evaluation until consensus was reached.
Table 2.
ICDAS II Scores each tooth as follows.
| Code | Criterion |
|---|---|
| 0 | Sound tooth surface; no evidence of caries after 5 s of air drying |
| 1 | First visual change in enamel; opacity of discoloration is visible after prolong air drying. Cannot be seen when wet. |
| 2 | Distinct visual change in enamel visible when wet. Lesion must be visible when dry. |
| 3 | Localize enamel breakdown (without clinical visual signs of dentinal involvement). Seen when wet and after prolong drying. |
| 4 | Underlying dark shadow from dentine. |
| 5 | Distinct cavity with visible dentine. |
| 6 | Extensive (more than half the surface). Distinct cavity with visible dentine. |
ICDAS, International Caries Detection and Assessment System score.
The investigations of WSLs were done before bonding (T0), and at 30 (T1), 90 (T2) and 180 days (T3) after bonding in the upper and lower arches. Photographs were taken at T0, T1, T2 and T3. All the photographs were taken for legal documentation using a standardized camera (Canon EOS 800D, with a 100 mm macro lens, Japan, shutter speed set to 1/200s, f/22 and ISO100), and the photographs were taken in a well-illuminated environment.
Data were analyzed using SPSS Statistics 23.0, and the normality assumption was tested using the Shapiro–Wilk test. Since the data was not normally distributed, the Kruskal–Wallis test, Friedman test and Fisher's exact test were used for the comparisons between groups. Cohen's kappa statistics were applied to determine the interexaminer and intraexaminer reliability. The level of statistical significance was set at 5%.
Results
The total number of patients was 42 (16 males and 26 females) with a mean age of 23.02 ± 3.841 (18–37) years old, distributed into three groups of 14 patients. The clinical examination was conducted from January 2020 to September 2020. The interexaminer Kappa value was 0.87, and the intraexaminer values were 0.82 and 0.89, respectively.
There were no significant differences (P > 0.05) between NS, CHX and fluoride at 30 days of follow-up, while WSLs were found more frequently in the fluoride and CHX groups compared with the NS mouthwash at 90 and 180 days of follow-up (P < 0.05), using the Kruskal–Wallis Test, as shown in Table 3. All groups showed a significant difference within the different periods of follow-up using the Friedman test (P < 0.05), as there was an increase in WSLs compared with the baseline, with highest mean at 180 days of follow-up, as shown in Table 4.
Table 3.
Relation of mouthwash and white spot lesions (WSLs) in the three different periods of time.
| Follow-up | Mouthwash | N | Median | Range | IQR | Mean | Std. Dev. | P-value |
|---|---|---|---|---|---|---|---|---|
| 30 days | Nanosilver | 14 | 0 | 0.08 | 0 | 0.006 | 0.0222 | 0.128 |
| Chlorhexidine | 14 | 0 | 0.25 | 0.1 | 0.0595 | 0.0948 | ||
| Fluoride | 14 | 0 | 0.25 | 0.08 | 0.0476 | 0.0781 | ||
| 90 days | Nanosilver | 14 | 0 | 0.1 | 0 | 0.0134 | 0.034 | 0.009a |
| Chlorhexidine | 14 | 0.0833 | 0.5 | 0.28 | 0.1488 | 0.1727 | ||
| Fluoride | 14 | 0.0833 | 0.25 | 0.17 | 0.1012 | 0.0875 | ||
| 180 days | Nanosilver | 14 | 0 | 0.25 | 0.03 | 0.037 | 0.079 | 0.011a |
| Chlorhexidine | 14 | 0.2708 | 0.5 | 0.5 | 0.253 | 0.2437 | ||
| Fluoride | 14 | 0.25 | 0.5 | 0.41 | 0.2351 | 0.190 |
IQR, Interquartile range.
Statistically significant at P < 0.05.
Table 4.
Relation of time and white spot lesions (WSLs) in the three groups of mouthwashes.
| Mouthwash | Follow-up | N | Median | Range | IQR | Mean | Std. Dev. | P-value |
|---|---|---|---|---|---|---|---|---|
| Nanosilver | Baseline | 14 | 0 | 0 | 0 | 0 | 0 | 0.067 |
| 30 days | 14 | 0 | 0.08 | 0 | 0.006 | 0.0222 | ||
| 90 days | 14 | 0 | 0.1 | 0 | 0.0134 | 0.034 | ||
| 180 days | 14 | 0 | 0.25 | 0.03 | 0.037 | 0.079 | ||
| Chlorhexidine | Baseline | 14 | 0 | 0 | 0 | 0 | 0 | 0.0001a |
| 30 days | 14 | 0 | 0.25 | 0.1 | 0.0595 | 0.0948 | ||
| 90 days | 14 | 0.0833 | 0.5 | 0.28 | 0.1488 | 0.1727 | ||
| 180 days | 14 | 0.2708 | 0.5 | 0.5 | 0.253 | 0.2437 | ||
| Fluoride | Baseline | 14 | 0 | 0 | 0 | 0 | 0 | 0.0001a |
| 30 days | 14 | 0 | 0.25 | 0.08 | 0.0476 | 0.0781 | ||
| 90 days | 14 | 0.0833 | 0.25 | 0.17 | 0.1012 | 0.0875 | ||
| 180 days | 14 | 0.25 | 0.5 | 0.41 | 0.2351 | 0.190 |
IQR, Interquartile range.
Statistically significant at P < 0.05.
The number of teeth affected by WSLs in different groups at different times is shown in Table 5. At 30 days follow up, in the group that had used the NS mouthwash, four teeth had developed WSLs, while in the group that used the CHX mouthwash, eleven teeth had developed WSLs. Finally, in the group that used the fluoride mouthwash, fifteen teeth had developed WSLs. Although, as the duration increased, the formation of WSLs increased across all groups. At 180 days of follow-up, the NS, CHX and fluoride mouthwash groups’ number of teeth with WSLs increased to 16, 41 and 41 teeth, respectively.
Table 5.
Sum of number of teeth with white spot lesions (WSLs) in each group within 3 periods of time.
| Time | Mouthwash | 13 | 12 | 11 | 21 | 22 | 23 | 33 | 32 | 31 | 41 | 42 | 43 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 30 days | Nanosilver | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 4 |
| Chlorhexidine | 2 | 3 | 2 | 3 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 11 | |
| Fluoride | 1 | 4 | 2 | 3 | 2 | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 15 | |
| Total | 3 | 8 | 5 | 6 | 3 | 0 | 0 | 2 | 0 | 1 | 0 | 2 | 30 | |
| 90 days | Nanosilver | 1 | 2 | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 8 |
| Chlorhexidine | 4 | 4 | 5 | 5 | 3 | 2 | 1 | 0 | 3 | 3 | 2 | 1 | 33 | |
| Fluoride | 1 | 6 | 4 | 6 | 4 | 1 | 0 | 1 | 1 | 1 | 2 | 1 | 28 | |
| Total | 6 | 12 | 10 | 12 | 7 | 4 | 1 | 2 | 4 | 4 | 4 | 3 | 69 | |
| 180 days | Nanosilver | 2 | 3 | 2 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 16 |
| Chlorhexidine | 3 | 5 | 7 | 6 | 4 | 3 | 0 | 1 | 5 | 4 | 2 | 1 | 41 | |
| Fluoride | 1 | 8 | 4 | 7 | 6 | 2 | 1 | 2 | 1 | 3 | 4 | 2 | 41 | |
| Total | 6 | 16 | 13 | 15 | 11 | 6 | 2 | 4 | 7 | 8 | 6 | 4 | 98 |
In this study, the incidence of WSLs per teeth after six months of orthodontic treatment was 19.44% (9.52% NS, 24.4% CHX and 24.4% fluoride).
Regarding the type of tooth, out of the 98 teeth that had WSLs after 180 days follow-up, the right maxillary lateral incisor showed the highest number with sixteen teeth (38.09%), followed by the left maxillary central incisor with fifteen teeth (35.71%), and the right maxillary central incisor with thirteen teeth (30.95%). There were more occurrences of WSLs in the maxillary teeth with 67 total teeth (13.29%), in relation to the mandibular teeth, with 31 total teeth (6.15%), as shown in Table 5.
In this study, 2016 surfaces including incisal, mesial, gingival and distal (672 for each group of mouthwash) were examined; comparing the three groups in each surface during the three follow-up times using Fisher's exact test. At 90 and 180 days of follow-up, there was a significant difference between the groups in the gingival, mesial and incisal surfaces (P < 0.05) with less number of WSLs in nanosilver compare to fluoride and CHX groups, but there is no significant difference in the distal surface (P > 0.05), as shown in Table 6.
Table 6.
Relationship between three different mouthwash, white spot lesions (WSLs) and teeth surfaces (Incisal, mesial, gingival and distal).
| Incisal |
P-value | Mesial |
P-value | Gingival |
P-value | Distal |
P-value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| WSLs |
WSLs |
WSLs |
WSLs |
||||||||||
| yes | No | yes | No | yes | No | yes | No | ||||||
| 30 days | Nanosilver | 2 | 166 | 0.233 | 0 | 168 | 0.0039a | 2 | 166 | 0.012a | 0 | 168 | 0.776 |
| Chlorhexidine | 7 | 161 | 9 | 159 | 6 | 162 | 1 | 167 | |||||
| Fluoride | 7 | 161 | 4 | 164 | 13 | 155 | 2 | 166 | |||||
| 90 days | Nanosilver | 5 | 163 | 0.00046a | 2 | 166 | 0.0001a | 2 | 166 | 0.0026a | 0 | 168 | 0.107 |
| Chlorhexidine | 25 | 143 | 21 | 147 | 12 | 156 | 3 | 165 | |||||
| Fluoride | 16 | 152 | 11 | 157 | 15 | 153 | 5 | 163 | |||||
| 180 days | Nanosilver | 11 | 157 | 0.0149a | 5 | 163 | 0.0001a | 6 | 162 | 0.0001a | 2 | 166 | 0.246 |
| Chlorhexidine | 28 | 140 | 39 | 129 | 39 | 129 | 7 | 161 | |||||
| Fluoride | 19 | 149 | 21 | 147 | 24 | 144 | 6 | 162 | |||||
Statistically significant at P < 0.05.
Discussion
Prevention and reducing of demineralization during orthodontic treatment is one of the greatest challenges faced by orthodontists even with modern advances in caries prevention. A number of scientific studies were performed in order to evaluate the effectiveness of the various remineralization methods, but data of these clinical researches were controversial. In this study nano-silver, CHX and fluoride mouthwash were used to prevent or reduce the amount of demineralization during orthodontic treatment.
The incidence of WSLs in this study was 19.44%, which closely compares to the incidences of other studies.2,15 However, this incidence is smaller than the study done by Richter et al.16 and Julien et al.17 were included mixed dentition that has more risk for WSLs and dental caries.18 Perhaps due to a difference in the duration of orthodontic treatment of the previous study.2 Another cause of the low incidence of WSLs in this study may be due to the monthly reminders patients received regarding oral hygiene instructions, thereby leading to better oral hygiene.4,19
Regarding the incidence of WSLs in each group, the NS group had the lowest incidence at 9.52%, followed by CHX at 24.4% and fluoride at 24.4%, this indicates that NS mouthwash has a greater effect in reducing the development of WSLs than the CHX and fluoride mouthwashes.
Nano-silver has many antibacterial and anti-caries effects.20,21 Streptococcus mutans are considered the main cause of dental caries and contribute to the virulence of dental biofilm in the presence of sucrose. Silver nanoparticles may be effective for controlling Streptococcus Mutans,22 and the antimicrobial effect is enhanced when the nanoparticle is only a few nanometers in diameter. Particles smaller than 10 nm are considered to have a high performance against pathogens of the dental biofilm.23 Silver is typically used in the form of nitrates to cause antimicrobial effects, though when silver-nanoparticles (AgNPs) are used, the surface area available for exposure to the microbe is greatly increased. Moreover, AgNPs are capable of anchoring and penetrating the bacterial cell wall, causing structural changes to the cell membrane, such as cell membrane permeability and cell death.24
In this study, all patients used fluoridated toothpaste, and with the addition of the NS mouthwash, produced a significant effect in reducing WSLs as a result of the synergistic actions of the NS and fluoride combined.24
In this study, long term CHX mouthwash (0.05%) was used as it has significant effects in plaque control,25 although CHX has some side effects such as brownish teeth, discoloration dorsum of the tongue and taste perturbation.7 Walsh et al. showed that using a low concentration of CHX mouthwash for three to six months has the effect of inhibiting S. mutans, leading to a reduction in the development of caries.26 Fluoride is effective in preventing caries as it slows down demineralization by co precipitating calcium and phosphate ions that dissolve and by enhancing the precipitation of fluoridated apatite. According to some studies fluoride could alleviate but not totally prevent the development of WSLs during treatment with fixed orthodontic appliances.5,27
The findings of the present study showed that there was an increase in the number of WSLs present with an increase in the duration of the treatment, which is in agreement with the findings of Buschang et al.2 However, as shown by the results, there were more WSLs formations at 180 days follow-up in the fluoride and CHX groups than the NS group, as NS has better anti-caries effects than CHX and fluoride.6
In the present study the upper arch WSLs are more than the lower arch which agree with Buschang et al.2 might be due to that the maxillary arch had more biofilm than mandibular arch.28
In this study, a high prevalence of WSLs was observed on the right maxillary lateral incisors. Our results are in line with Sonesson et al.5 as it could be due to the fact that the maxillary lateral incisors had more biofilm than the other teeth.17
In regards to the location of WSLs on teeth surfaces, they could be found on all surfaces; however, the gingival margin was the most frequently recorded surface location of WSLs, which is consistent with the work of Mei et al.28 A possible explanation for this could be that the gingival surfaces had more biofilm than other surfaces and were missed while brushing, and this could be exacerbated by the presence of an orthodontic bracket fixed on the tooth surface, leading to bacterial accumulation and the formation of WSLs.28This clinical study had some limitations; one was that the patients' compliance could not be ideally controlled. In addition, the prevalence of white spots in orthodontic treatment was reported in 6 months, however, the longer the treatment is, the more likely the WSLs will develop. Additionally, the patients might not use the mouth wash properly or in regular way as they instructed.
According to the finding of this study, the NS mouthwash was more effective in reducing WSLs than the CHX and fluoride mouthwashes during orthodontic treatment. As the duration of orthodontic treatment increased, the formation of WSLs increased in all groups, though the NS group showed less of an increase in the presence of WSLs compared with the CHX and fluoride group in different follow-up times.
Declaration of competing interest
The authors have no conflicts of interest relevant to this article.
Acknowledgments
Special thanks to Darwn Saeed for his unlimited help and advice in performing statistical analysis. This research received no external funding.
References
- 1.Yadav K., de Ataide I.N., Fernandes M., Lambor R. Minimally invasive treatment of white spot lesions. Indian J Oral Health Res. 2016;2:117. [Google Scholar]
- 2.Buschang P.H., Chastain D., Keylor C.L., Crosby D., Julien K.C. Incidence of white spot lesions among patients treated with clear aligners and traditional braces. Angle Orthod. 2019;89:359–364. doi: 10.2319/073118-553.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Perrini F., Lombardo L., Arreghini A., Medori S., Siciliani G. Caries prevention during orthodontic treatment: in-vivo assessment of high-fluoride varnish to prevent white spot lesions. Am J Orthod Dentofacial Orthop. 2016;149:238–243. doi: 10.1016/j.ajodo.2015.07.039. [DOI] [PubMed] [Google Scholar]
- 4.Khoroushi M., Kachuie M. Prevention and treatment of white spot lesions in orthodontic patients. Contemp Clin Dent. 2017;8:11–19. doi: 10.4103/ccd.ccd_216_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sonesson M., Brechter A., Abdulraheem S., Lindman R., Twetman S. Fluoride varnish for the prevention of white spot lesions during orthodontic treatment with fixed appliances: a randomized controlled trial. Eur J Orthod. 2020;42:326–330. doi: 10.1093/ejo/cjz045. [DOI] [PubMed] [Google Scholar]
- 6.Subramani K., Seo H.N., Dougherty J., et al. In vitro evaluation of antimicrobial activity of chlorhexidine hexametaphosphate nanoparticle coatings on orthodontic elastomeric chains. Mater Res Express. 2020;7 [Google Scholar]
- 7.Fiorillo L. Chlorhexidine gel use in the oral district: a systematic review. Gels. 2019;5:31. doi: 10.3390/gels5020031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Prajapati D., Nayak R., Tandon S., Naidu S., Ratnanag P.V., Kamath N. Efficacy of concomitant therapy with fluoride and chlorhexidine varnish on remineralization of incipient lesions in young children. Int J Clin Pediatr Dent. 2016;9:296–302. doi: 10.5005/jp-journals-10005-1381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Govindankutty D. Applications of nanotechnology in orthodontics and its future implications. Int J Appl Dent Sci. 2015;1:166–171. [Google Scholar]
- 10.Hern A.E., Lara-carrillo E., Robles-navarro J.B., Id R.J.S., Hern S., Medina-sol C.E. Biosynthesis of silver nanoparticles on orthodontic elastomeric modules : evaluation of mechanical and antibacterial properties. Molecules. 2017;22:1–14. doi: 10.3390/molecules22091407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Teixeira J.A., Vieira A., Elias V., De Melo P.C. Effects of a new nano-silver fluoride-containing dentifrice on demineralization of enamel and streptococcus mutans adhesion and acidogenicity. Int J Dent. 2018:1351925. doi: 10.1155/2018/1351925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brook P.H., Shaw W.C. The development of an index of orthodontic treatment priority. Eur J Orthod. 1989;11:309–320. doi: 10.1093/oxfordjournals.ejo.a035999. [DOI] [PubMed] [Google Scholar]
- 13.Kau C.H., Wang J., Palombini A., Abou-Kheir N., Christou T. Effect of fluoride dentifrices on white spot lesions during orthodontic treatment: a randomized trial. Angle Orthod. 2019;89:365–371. doi: 10.2319/051818-371.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ismail A.I. Visual and visuo-tactile. J Dent Educ. 2004;83:56–66. doi: 10.1177/154405910408301s12. [DOI] [PubMed] [Google Scholar]
- 15.Lucchese A., Gherlone E. Prevalence of white-spot lesions before and during orthodontic treatment with fixed appliances. Eur J Orthod. 2013;35:664–668. doi: 10.1093/ejo/cjs070. [DOI] [PubMed] [Google Scholar]
- 16.Richter A.E., Arruda A.O., Peters M.C., Sohn W. Incidence of caries lesions among patients treated with comprehensive orthodontics. Am J Orthod Dentofacial Orthop. 2011;139:657–664. doi: 10.1016/j.ajodo.2009.06.037. [DOI] [PubMed] [Google Scholar]
- 17.Julien K.C., Buschang P.H., Campbell P.M. Prevalence of white spot lesion formation during orthodontic treatment. Angle Orthod. 2013;83:641–647. doi: 10.2319/071712-584.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abbass M.M.S., Mahmoud S.A., El Moshy S., et al. The prevalence of dental caries among egyptian children and adolescences and its association with age, socioeconomic status, dietary habits and other risk factors. F1000Research. 2019;8:1–19. doi: 10.12688/f1000research.17047.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sujay Kumar G., Kashyap A., Raghav S., Bhardwaj R., Singh A., Guram G. Role of text message reminder on oral hygiene maintenance of orthodontic patients. J Contemp Dent Pract. 2018;19:98–101. doi: 10.5005/jp-journals-10024-2219. [DOI] [PubMed] [Google Scholar]
- 20.Tirupathi S., Nirmala S.V.S.G., Rajasekhar S., Nuvvula S. Comparative cariostatic efficacy of a novel nano-silver fluoride varnish with 38% silver diamine fluoride varnish a double-blind randomized clinical trial. J Clin Exp Dent. 2019;11:105–112. doi: 10.4317/jced.54995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu B.Y., Mei L., Chu C.H., Chin E., Lo M. Effect of silver fluoride in preventing the formation of artificial dentinal caries lesions in vitro. Chin J Dent Res. 2019;22:273–280. doi: 10.3290/j.cjdr.a43738. [DOI] [PubMed] [Google Scholar]
- 22.Silva A.V.C., Teixeira J.A., Mota C.C.B.O., et al. In vitro morphological, optical and microbiological evaluation of nanosilver fluoride in the remineralization of deciduous teeth enamel. Nanotechnol Rev. 2018;7:509–520. [Google Scholar]
- 23.Noronha V.T., Paula A.J., Durán G., et al. Silver nanoparticles in dentistry. Dent Mater. 2017;33:1110–1126. doi: 10.1016/j.dental.2017.07.002. [DOI] [PubMed] [Google Scholar]
- 24.Puppala N., Nagireddy V.R., Reddy D., Kondamadugu S., Mareddy A., Chris A. Nanosilver fluoride—aparadigm shift for arrest in dental caries in primary teeth of schoolchildren: a randomized controlled clinical trial. Int J Clin Pediatr Dent. 2019;12:484–490. doi: 10.5005/jp-journals-10005-1703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Leeuwen M.P.C., Slot D.E., Van der Weijden G.A. Essential oils compared to chlorhexidine with respect to plaque and parameters of ingival inflammation: a systematic review. J Periodontol. 2011;82:174–194. doi: 10.1902/jop.2010.100266. [DOI] [PubMed] [Google Scholar]
- 26.Walsh T., Jm O., Moore D., Walsh T., Jm O., Moore D. Chlorhexidine treatment for the prevention of dental caries in children and adolescents. Cochrane Database Syst Rev. 2015;4:CD008457. doi: 10.1002/14651858.CD008457.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ten Cate J.M., Buzalaf M.A.R. Fluoride mode of action: once there was an observant dentist. J Dent Res. 2019;98:725–730. doi: 10.1177/0022034519831604. [DOI] [PubMed] [Google Scholar]
- 28.Mei L., Chieng J., Wong C., Benic G., Farella M. Factors affecting dental biofilm in patients wearing fixed orthodontic appliances. Prog Orthod. 2017:184. doi: 10.1186/s40510-016-0158-5. [DOI] [PMC free article] [PubMed] [Google Scholar]