Abstract
Very low food security among children (VLFS-C), often referred to as child hunger, can profoundly hinder child development, family well-being, and community health. Food pantries are important community resources that routinely serve at-risk families. This study investigated the influence of various candidate risk factors for VLFS-C within a food pantry population to inform the development of the “Pantry Assessment Tool against Child Hunger (PATCH).” We collected standardized surveys among a representative sample of households with children accessing food pantry services in Oklahoma (n=188). Weighted analyses revealed a large majority of households experienced child-level food insecurity (70.6%), with nearly half reporting low food security and nearly one-quarter reporting VLFS-C. We then used logistic regression to identify factors associated with VLFS-C, followed by chi-square automatic interaction detection (CHAID) to assess if, and in what progression, significant risk factors predicted VLFS-C. In unadjusted models, annual household income <$15,000, non-urban residence, lack of health insurance, unstable housing, heavier food pantry reliance, fair or poor adult health, adult anxiety, and adult smoking to reduce hunger pangs were all positively associated with VLFS-C. Receipt of Special Supplemental Nutrition Program for Women, Infants and Children (WIC) and higher social support were protective against VLFS-C. However, in adjusted models, only receipt of WIC remained significant. CHAID analysis revealed that access to insurance best differentiated groups with and without VLFS-C. Informed by these analyses, the PATCH tool may be useful for the development of screening programs to identify and address potential root causes of VLFS-C in pantry settings.
Keywords: Food supply, adverse childhood experiences, child, hunger, food pantries, child welfare
Introduction
Food insecurity, a household condition of limited access to a reliable or adequate food supply (National Research Council, 2006), occurs in every state and county in the US (Weinfield et al., 2014). Households with children are more likely to experience food insecurity than those without children (Coleman-Jensen et al., 2020), which can perpetuate lifecourse disadvantage across generations through complex and interconnected pathways (Chilton et al., 2017). For example, individuals affected by food insecurity as adults commonly report personal histories of intergenerational violence and other adverse childhood experiences (ACEs) as children (Chilton et al., 2017; Chilton et al., 2015; Lippert & Lee, 2020). Household food insecurity is bidirectionally linked to poor physical and mental health in adulthood (Bruening et al., 2017; Seligman & Schillinger, 2010; Siefert et al., 2001), which can further impede caregivers’ efforts to break the cycle of poverty for their children (Chilton et al., 2017). Among children, food insecurity contributes to poor developmental trajectory delays (Jyoti et al., 2005), as well as poor biological (Mangini et al., 2015; Metallinos-Katsaras et al., 2016; Metallinos-Katsaras et al., 2012; Ryu & Bartfeld, 2012), cognitive (Chilton et al., 2007; Rose-Jacobs et al., 2008), behavioral (Kimbro & Denney, 2015), and socioemotional outcomes (Burke et al., 2016; Jyoti et al., 2005) in early life and adolescence, which can result in lasting consequences throughout adulthood.
Household caregivers employ multiple coping strategies to maximize the quantity of food available for children when resources are limited, including purchase of inexpensive, often unhealthy food (Harvey, 2016), and reliance on friends, extended family members, or community food pantries (Holben et al., 2004). Caregivers will also often reduce their own food intake to shield younger children from physical hunger (McIntyre et al., 2003). As the number and perceived severity of negative life experiences increase (Drucker et al., 2019), caregivers may still be forced to require children to miss meals or reduce children’s portion sizes (Harvey, 2016). This can result in very low food security among children (VLFS-C), a distinct ACE that impacts an estimated 0.6% of households with children in the US (Coleman-Jensen et al., 2020). In Oklahoma, the child food insecurity rate ranks seventh highest in the nation (Feeding America, 2018), which has important implications for personal child development, family well-being, and community health.
Food pantries are important community assets originally designed to meet the needs of families with acute food needs (Greenberg et al., 2010). Families often rely upon these providers to supplement food resources provided through federal food assistance programs, such as the Supplemental Nutrition Assistance Program (SNAP), the Special Supplemental Nutrition Program for Women, Infants and Children (WIC), and the National School Lunch and Breakfast Programs (Weinfield et al., 2014). One major limitation of food pantry programs is that many do not address the root socioeconomic causes of food insecurity, such as unemployment and housing instability. Research led by Feeding America, the nation’s largest network of food bank providers, reveals the high burden of unmet health and basic needs among many clients of charitable food programs (Weinfield et al., 2014). Emerging evidence suggests that food pantries can be leveraged to support long-term food security and nutrition (An et al., 2019) through wrap-around intervention models that include additional services, such as case management and collaborative goal-setting to address barriers to long-term food security (Martin et al., 2019; Martin et al., 2013). However, food pantries are typically limited in personnel and other resources (An et al., 2019), which can prevent delivery and implementation of comprehensive interventions. Since food insecurity is a graded experience of increasing severity, it is likely that families experiencing VLFS-C may require more specialized support to stabilize household needs compared to food insecure families without VLFS-C. The limited infrastructure of the typical food pantry environment requires effective screening tools in order to appropriately triage programmatic responses to unmet social needs of families with and without VLFS-C.
Oklahoma food banks and their partner programs, like many other charitable food networks in the US, increasingly serve at-risk families on a routine basis. Little data are available on the distribution of risk factors for food insecurity among Oklahoma’s food pantry population, including those specific risk factors for VLFS-C. Drawing from studies conducted in the general population, a number of demographic and health indicators could be considered to identify high-risk families. For example, VLFS-C is more prevalent among families headed by single mothers or that include a non-Hispanic black adult. Households earning below 185% of the poverty line also disproportionately experience VLFS-C (Coleman-Jensen et al., 2020). Although participation in food assistance programs supports food security among families in the general population (Ettinger de Cuba et al., 2019; Kreider et al., 2016; Metallinos-Katsaras et al., 2011), their role as an indicator for VLFS-C within food pantry populations remains unclear. In regards to health indicators, household insurance status may not be a useful correlate of VLFS-C (Anderson et al., 2016), while having an adult in poor mental or physical health (Anderson et al., 2016) or with a child in fair or poor physical health (Cook et al., 2006) may be useful predictors of VLFS-C.
Additionally, unmet basic needs, lack of social support, or health risk behaviors may represent potential VLFS-C intervention areas for high-risk families accessing food pantries. For example, in one analysis of determinants of VLFS among households accessing US food banks, unpaid medical bills, frequent moves, and tradeoffs between paying utilities, housing, and transportation bills were associated with VLFS in unadjusted models (Gundersen et al., 2017). However, these analyses did not explore determinants of VLFS at the child level. One study of family caregivers living in South Carolina identified negative work experiences and financial instability as being particularly detrimental to child food security, and positive social relationships during hardships as being supportive (Drucker et al., 2019). Additionally, adults facing food insecurity may engage in avoidant coping behaviors such as smoking (Kim & Tsoh, 2016) or alcohol use (Pryor et al., 2016) to manage unmet emotional (e.g., trauma, chronic stress) or physical (e.g., hunger pangs) needs. For example, adult cigarette smoking (Cutler-Triggs et al., 2008) and adult history of drug rehabilitation (Anderson et al., 2016) are correlated with VLFS-C in the general population. This suggests that trauma-informed cessation support programs represent another potential avenue for VLFS-C prevention. However, it is not feasible for the majority of food pantries to comprehensively screen and intervene in all of these areas. Within this high-risk population, more information is needed on which factors best differentiate households with and without VLFS-C, so that limited resources can be focused to prevent and ameliorate VLFS-C.
This study aims to describe the prevalence of VLFS-C among Oklahoma families with children accessing food pantries, and seeks to identify candidate household risk factors for VLFS-C within this population, including measures of household socioeconomic deprivation, poor psychological and physical health, and avoidant coping strategies. We then describe how affected families experience different combinations of risk factors for VLFS-C. We conclude with our recommendations for a screening intervention framework for future implementation in food pantry settings to address the underlying factors most associated with VLFS-C.
Materials and Methods
Data from the current study were collected through the Food Independence, Security and Health (FISH) study, which was conducted through a university-community research partnership involving the University of Oklahoma Health Sciences Center and Oklahoma’s two food banks, the Community Food Bank of Eastern Oklahoma and the Regional Food Bank of Oklahoma. The FISH study involved primary data collection through surveys between April and October 2016 at three levels (organizational, personnel, and client) to achieve a comprehensive systems-level understanding of opportunities to promote health and food security among client households accessing Oklahoma food pantries. Feeding America, both Oklahoma food bank partners, and University of Oklahoma Health Sciences Center personnel all collaborated on development of the client survey. The University of Oklahoma Health Sciences Center Institutional Review Board approved the FISH study.
Sample population
The FISH study used a two-stage sampling design to survey food pantry clients based on food bank partner input and sampling preference for their region. We included all Food & Resource Centers in Western Oklahoma and used proportionate probability sampling (PPS) to select food pantries in Eastern Oklahoma after initial stratification by rurality (metropolitan, micropolitan, or rural). PPS was based on the pounds of food distributed as a proxy for the number of clients served using 1,000 pounds for the pantry inclusion criteria. In the second stage of sampling at the selected food pantry or Food & Resource Center, adult clients were selected using simple random sampling and invited to participate. Clients were included if they were aged 18 years or older, spoke English, and consented to participate. Only one client per household was allowed to participate. Consented food pantry clients self-reported responses to a survey that was administered either electronically, via REDCap on a tablet or laptop, or on paper if respondents preferred or electronic devices were not an option. The analyses conducted for this study were limited to clients living in households with children (n = 188 of 376 clients surveyed).
Outcome variables
We measured adult- and child-level food security status using the 18-item US Household Food Security Survey Module (Economic Research Service, 2012). The first 10 items are used to estimate food security status among adults, while the last 8 items are used to assess food security status among children in the household. We used USDA’s scoring methodology to classify household children into one of four categories (high food security, marginal food security, low food security, or very low food security among children [VLFS-C]) (Economic Research Service, 2012).
Independent variables
We collected information regarding client sociodemographics, basic needs, food assistance program use, health-related factors, and hunger coping behaviors based on our literature review of risk factors associated with food insecurity in the general US population. When possible, standardized survey items were used from previously published studies.
Sociodemographic
Demographic variables for the respondent included race, ethnicity, education, age, household income (Weinfield et al., 2014), marital status, female-headed household status, and the number of adults and children (under the age of 18) in the household.
Basic needs
Respondent insurance status and employment status were assessed using items adapted for self-administration from the Behavioral Risk Factor Surveillance Survey (BRFSS) 2014. We assessed unpaid medical bills, current housing status, and frequency of housing moves in the past 12 months using questions from the Hunger in America 2014 survey (Weinfield et al., 2014). We defined unstable housing to include temporary housing or no housing, with all other housing types being classified as stable. We further assessed housing and energy instability in the past 12 months using 3 items from the Financial Stress Index (Siahpush & Carlin, 2006), including positive (yes) responses to being: unable to heat or cool the home; unable to pay mortgage or rent on time; and unable to pay electricity, gas, or phone bills on time.
Food assistance program use
Federal foood assistance program use was assessed using questions from the Hunger in America 2014 survey (Weinfield et al., 2014), including Supplemental Nutrition Assistance Program (SNAP), Special Supplemental Nutrition Program for Women, Infants and Children (WIC), National School Lunch Program, and food-bank sponsored School Backpack Program use. We also created a food pantry reliance score based on the sum of responses using three questions from the Hunger in America 2014 study (Weinfield et al., 2014): “How many times in the past 12 months has your household used a food pantry for food?” (0–4 points) “Out of all the food your household eats on an average month, how much comes from a food pantry?” (0–4 points) and “In the past 12 months, did your household get food from any food pantry program other than this one?” (0–1 point). The possible score range was 0 to 9 points, with higher points indicating greater food pantry reliance.
Adult health risk behaviors and hunger coping strategies
We assessed smoking status using two standard items regarding smoking at least 100 cigarettes in the person’s lifetime and if respondents currently smoke everyday or some days, which were used to classify respondents as current smokers (includes daily and some day smokers) vs. non-smokers (including never and former smokers) (National Center for Health Statistics, 2016). We used the AUDIT-C to identify hazardous drinking or active alcohol use disorders (Bush et al., 1998). Additionally, the research team developed a subjective question that asked whether respondents had used any of the following to reduce hunger pangs in the past 12 months, including multi-select options for smoked a cigarette, slept, and drank alcohol.
Adult physical and mental health
We assessed general physical health using the BRFSS question “Would you say that in general your health is…?” with response options of “Excellent,” “Very good,” “Good,” “Fair,” or “Poor.” We assessed poor adult psychological health using two questions from the BRFSS 2014 Mental Health Module (Centers for Disease Control and Prevention, 2014). Frequent mental distress (FMD) was defined as 14 or more days of either feeling sad, blue, or depressed (FMD-Depression) or feeling worried, tense, or anxious (FMD-Anxiety) (Centers for Disease Control and Prevention, 2014). Additionally, we measured perceived stress by summing items from the 4-item version of the Perceived Stress Scale, which has a possible range of 0 to 16 points, with higher scores indicating higher stress (Cohen et al., 1983). Because social support may serve as a protective factor against stress and poor mental health, we also assessed perceived social support taking the mean response of items the Duke-UNC Functional Social Support Questionnaire (Broadhead et al., 1988). Possible points range from 1 to 5, with higher scores indicating higher social support.
Statistical analyses
All analyses were weighted to represent food pantry clients across the state of Oklahoma. Using multiple imputation to handle missingness in the data (Rubin, 2004), descriptive statistics were calculated to characterize households with children accessing food pantries. We then used logistic regression to compare households with very low food security among children (VLFS-C) and households without VLFS-C to identify any potential predictors of VLFS-C. All variables with a p-value less than 0.05 from the univariate analyses of VLFS-C were included in a multiple variable model to identify factors that remained independently associated with VLFS-C. Collinearity among variables was assessed by computing their variance infalation factors (VIF) and variables with values greater than 10 were removed (Hahs-Vaughn & Lomax, 2012).
Finally, since households may experience different combinations of risk factors rather than all risks simultaneously, we used a pattern recognition technique—chi-square automatic interaction detection (CHAID)—to assess if, and in what progression, risk factors predict VLFS-C in this population. This methodological approach may be useful for informing future food pantry screening and intervention strategies for VLFS-C households because CHAID predicts VLFS-C by the simplest means available to food pantries (i.e., using data that is either currently or could be feasibly collected by most providers). This method is an inductive (rather than theory-based) technique that merges variables into nodes based on statistically important variables from chi-square analyses, which form branches that indicate the relative importance of these combined risk factors (Kass, 1980). The CHAID approach requires a minimum frequency of observations in the terminal nodes, which we set at 5% and a minimum number of observations at each split, set at 20. The alpha level was set at 0.05 for all tests, using the Bonferroni correction for each predictor within the model. All analyses except the CHAID were conducted in STATA 14.2. The CHAID analysis was conducted in R (R Core Team, 2017) using the CHAID (Hothorn & Zeileis, 2015a) and Partykit (Hothorn & Zeileis, 2015b) packages.
Results
Characteristics of households with and without very low food security among children
Weighted analyses indicated that only 29.4% of households with children experienced high or marginal food security among children. The remaining 70.6% of households with children experienced some degree of child-level food insecurity, including low food security (47.4%) or very low food security (VLFS-C) (23.2%). Sociodemographic and basic need characteristics of client households with children are summarized in Table 1, including comparisons between households with and without VLFS-C. The mean age of adult client survey respondents was 39.8 years and household composition averaged 2.4 adults and 2.5 children with no difference by VLFS-C status. We found no significant differences by VLFS-C status for age, race, marital status, education level of the adult client, nor for the household-level variable of female-headed single household.
Table 1.
Sociodemographic and basic need characteristics of households with children accessing food pantries, with and without very low child food security
| Characteristic | All participants w/ children n = 186 | Weighted N = 62,975 % or mean (SD) | No very low food security among children % or mean (SD) | Very low food security among children % or mean (SD) | Statistical test value F (df) or t | P-value |
|---|---|---|---|---|---|---|
| DEMOGRAPHICS | ||||||
| Age, mean (SD) | 41.1 (11.5) | 39.8 (11.1) | 39.8 (11.1) | 39.9 (11.3) | t =−.06 | 0.954 |
| Adults in household, mean (SD) | 2.4 (1.2) | 2.4 (1.27) | 2.5 (1.3) | 2.2 (1.0) | t =−1.39 | 0.175 |
| Children in household, mean (SD) | 2.5 (1.4) | 2.5 (1.4) | 2.5 (1.5) | 2.2 (1.01) | t =−1.58 | 0.123 |
| Race, respondent | ||||||
| White, NH | 88 | 43.46 | 42.26 | 47.73 | F (2.68, 83.09) = 0.94 | 0.416 |
| Black or African American, NH | 27 | 20.58 | 21.1 | 18.72 | ||
| American Indian or Alaskan Native, NH | 35 | 11.37 | 12.87 | 6.037 | ||
| Other, NH | 13 | 10.21 | 8.22 | 17.27 | ||
| Hispanic | 19 | 14.38 | 15.55 | 10.24 | ||
| Marital status, respondent | ||||||
| Married | 73 | 32.53 | 36.17 | 19.63 | F (1, 31) = 2.24 | 0.145 |
| Unmarried | 111 | 67.47 | 63.83 | 80.37 | ||
| Female single headed-household (% yes) | 28 | 19.5 | 22.21 | 10.47 | F (1, 31) = 1.53 | 0.225 |
| Locale | ||||||
| Urban | 111 | 76.8 | 72.77 | 87.9 | F (1, 31) = 5.08 | 0.031 |
| Rural | 77 | 23.2 | 27.23 | 12.1 | ||
| Education, respondent | ||||||
| Less than high school | 46 | 20.32 | 20.6 | 19.42 | F (2.61, 80.90) = 0.55 | 0.628 |
| High school diploma/GED | 86 | 49.41 | 46.65 | 58.33 | ||
| Some college/technical school | 44 | 23.84 | 25.2 | 19.45 | ||
| College degree or more | 10 | 6.42 | 7.547 | 2.804 | ||
| Income | ||||||
| Income below $15,000 | 115 | 63.08 | 55.13 | 86.98 | F (1.57, 48.59) = 8.58 | .002 |
| BASIC NEEDS | ||||||
| Insurance, respondent (% no)* | 64 | 33.67 | 24.68 | 62.86 | F (1, 31) = 6.58 | <0.001 |
| Unpaid medical bills (% yes) * | 112 | 59.91 | 58.74 | 63.65 | F (1, 31) = 0.27 | 0.610 |
| Unstable housing (% yes) * | 9 | 4.87 | 2.40 | 13.06 | F (1, 31) = 3.96 | <0.001 |
| Unemployed, respondent (% yes) * | 70 | 36.13 | 35.47 | 38.55 | F (1, 31) = 0.08 | 0.773 |
| Unable to heat or cool home* | 66 | 37.19 | 28.29 | 64.67 | F (1, 31) = 11.65 | 0.002 |
| Could not pay mortgage or rent on time* | 93 | 53.95 | 46.4 | 77.88 | F (1, 31) = 13.51 | 0.001 |
| Could not pay electricity, gas, phone bills on time* | 116 | 58.89 | 54.18 | 74.05 | F (1, 31) = 5.04 | 0.032 |
| FOOD ASSISTANCE PROGRAM USE | ||||||
| SNAP (% yes) | 106 | 60.03 | 64.45 | 45.65 | F (1, 31) = 2.15 | 0.152 |
| WIC (% yes) | 49 | 27.75 | 35.77 | 1.55 | F (1, 31) = 49.04 | <0.001 |
| NSLP (% yes) | 29 | 68.49 | 66.39 | 74.94 | F (1, 7) = 0.10 | 0.759 |
| Backpack (% yes) | 6 | 8.87 | 19.39 | 13.25 | F (1, 31) = 0.69 | 0.412 |
| Food pantry reliance score (0–9 scale), mean (SD) | 4.7 (2.1) | 5.0 (2.09) | 4.7 (1.99) | 6.1 (2.04) | t = 4.08 | <0.001 |
X2 test compares listed group to opposing group
Abbreviations: NH: Non-Hispanic; GED: General Education Diploma; SNAP: Supplemental Nutrition Assistance Program; WIC: Special Supplemental Nutrition Program for Women, Infants, and Children; NSLP: National School Lunch Program
Households with incomes below $15,000 per year more often experienced VLFS-C as compared to those households earning above $15,000 annually, p = 0.0019. VLFS-C was also significantly more prevalent among those households where the adult client lacked health insurance, reported an unstable housing situation, and that reported financial difficulty in heating or cooling the home, paying mortgage or rent on time, and paying other bills on time. Households receiving WIC rarely reported VLFS-C (1.6%), while over one-third of households without WIC (35.8%) experienced VLFS-C. VLFS-C households relied on food pantries more heavily than non-VLFS-C households per the food pantry reliance score, p < 0.001.
Health conditions significantly associated with VLFS-C included the adult client being in fair or poor health, p = 0.020, and experiencing frequent mental distress in the form of anxiety, p = 0.005 (Table 2). Additionally, adult clients living in households with VLFS-C experienced a significantly higher number of poor mental health days in the past month, including depression (M = 12.36, SD = 9.23 vs. M = 7.84, SD = 8.54, p = 0.041) and anxiety (M = 16.58, SD = 10.29 vs. M = 11.91, SD = 10.45, p = 0.007). While problem drinking and smoking were not associated with VLFS-C, reports of smoking to cope with hunger pangs was significantly higher for this group, p = 0.016. Perceived social support was significantly lower among adult clients from VLFS-C (p < 0.001), although perceived stress was similar between the two groups.
Table 2.
Adult health and health risk behavior characteristics of households with children accessing food pantries, with and without very low child food security
| All participants w/ children n = 186 | Weighted N = 62,975 % or mean (SD) | No very low child food security among children % or mean (SD) | Very low food security among children % or mean (SD) | Statistical test value F (1,31) or t | P-value | |
|---|---|---|---|---|---|---|
| ADULT PHYSICAL and MENTAL WELL-BEING | ||||||
| Self-rated physical health | ||||||
| Excellent, very good, good | 106 | 53.48 | 60.68 | 30.68 | F = 6.04 | 0.020 |
| Fair, or poor | 77 | 46.52 | 39.32 | 69.32 | ||
| Mental health | ||||||
| ≥ 14 depression days (% yes) | 50 | 27.66 | 24.14 | 39.3 | F = 2.55 | 0.120 |
| ≥ 14 anxiety days (% yes) | 78 | 43.35 | 37.79 | 61.81 | F = 8.93 | 0.005 |
| Perceived stress (0–16 scale) | 7.3 (2.5) | 7.4 (2.6) | 7.4 (2.62) | 7.5 (2.27) | t =0.15 | 0.880 |
| Social support (1–5 scale) | 3.8 (1.1) | 3.6 (1.2) | 3.8 (1.1) | 3.1 (1.2) | t = −3.68 | 0.001 |
| ADULT HEALTH RISK BEHAVIORS | ||||||
| Problem drinking, respondent (% yes) | 22 | 11.8 | 11.47 | 12.9 | F = 0.04 | 0.843 |
| Smoker, respondent (% yes) | 93 | 49.08 | 46.61 | 58.04 | F = 1.76 | 0.194 |
| ADULT COPING STRATEGIES | ||||||
| Coping Strategies for Hunger Pangs | ||||||
| Sleep (% yes) | 82 | 45.53 | 45.13 | 46.86 | F = 0.04 | 0.8371 |
| Smoke (% yes) | 56 | 27.04 | 22.72 | 41.36 | F = 6.45 | 0.0164 |
| Drink alcohol (% yes) | 11 | 5.18 | 3.91 | 9.41 | F = 1.18 | 0.2848 |
Adult interest in referrals to address factors associated with VLFS-C
Among those households with children with unstable housing (3.34%), 46.2% of respondents reported they would like pantry workers to help them get housing. Among those who were unemployed (36.13%), 35.4% said they would like pantry workers to help them get employment. Among those who were not receiving SNAP (40.0%), 16.8% said they would like pantry workers to help them get SNAP. Among those adult respondents who were current smokers (49.08%), 29.3% said they would like pantry workers to help them quit smoking.
Logistic regression and CHAID results
The financial stress item for not being able to pay electricity, gas, or telephone bills on time was excluded from the regression models due to high collinearity with the financial stress item of not being able to afford rent (r = .541). This item’s removal reduced the average variance inflation factor (VIF) among all variables to 3.61 and no variable was higher than 7.68. In unadjusted analyses, those households earning incomes below $15,000 were more than five-times more likely to experiencing VLFS-C compared to households with higher incomes (Table 3). Unmet basic needs were associated with a four- to six-fold increase in the odds of VLFS-C. Households accessing pantries in urban settings had a 63% lower odds of VLFS-C compared to households accessing pantries in rural settings. A heavier reliance on food pantries was associated with a 41% higher odds of VLFS-C, while use of WIC was highly protective against VLFS-C. Lastly, households with adults in fair or poor physical health and adult clients who reported frequent mental distress in the form of anxiety and use of smoking to cope with hunger pangs were also more likely to experience VLFS-C. Social support was a protective factor against VLFS-C. However, in adjusted analyses, only the use of WIC remained as a protective factor against VLFS-C (AOR = 0.03, 95% CI: 0.01–0.16).
Table 3 –
Factors associated with very low child food security among households accessing food pantries in Oklahoma
| Characteristic | Odds Ratio | Adjusted Odds Ratio (AOR) F(12, 29.0) = 3.11; p = 0.0061 | t | P value |
|---|---|---|---|---|
| DEMOGRAPHICS | ||||
| Household income below $15k/yr. (vs. above $15k) | 5.39 (1.37–21.22) * | 4.41 (0.87–22.4) | 1.87 | 0.07 |
| Urban | 0.37 (0.14–0.94) * | 0.64 (0.14–2.93) | −0.60 | 0.55 |
| BASIC NEEDS | ||||
| No insurance (vs. insurance) | 5.05 (2.48–10.25) ** | 2.39 (0.74–7.67) | 1.53 | 0.14 |
| Unstable housing (vs. stable housing) | 6.20 (2.60–14.78) ** | 1.08 (0.07–15.94) | 0.06 | 0.95 |
| Could not pay mortgage or rent on time* | 4.06 (1.81–9.07) ** | 2.84 (0.66–12.16 | 1.47 | 0.15 |
| Unable to heat or cool home* | 4.81 (1.85–12.53) ** | 1.58 (0.49–5.05) | 0.81 | 0.43 |
| FOOD ASSISTANCE PROGRAM USE | ||||
| WIC (vs. no WIC) | 0.03 (0.01–0.16) ** | 0.03 (0.01–0.31) | −3.14 | 0.00 |
| Food pantry reliance score (for every 1-point increase) | 1.41 (1.14–1.74) ** | 1.3 (0.95–1.77) | 1.73 | 0.10 |
| ADULT PHYSICAL and MENTAL WELL-BEING | ||||
| Adult with fair or poor health (versus excellent, very good, good health) | 3.48 (1.18–10.33) * | 2.44 (0.66–9.05) | 1.39 | 0.17 |
| FMD – Anxiety (vs. no FMD – Anxiety) | 2.66 (1.35–5.27) ** | 1.48 (0.33–6.69) | 0.53 | 0.60 |
| Social support (for every 1-point increase) | 0.61 (0.45–0.82) ** | 0.93 (0.57–1.51) | −0.32 | 0.75 |
| Smoked to reduce hunger pangs | 2.40 (1.17–4.91) * | 1 (0.25–3.94) | 0.00 | 1.00 |
Bolded values are significant:
p<0.05
p<0.01
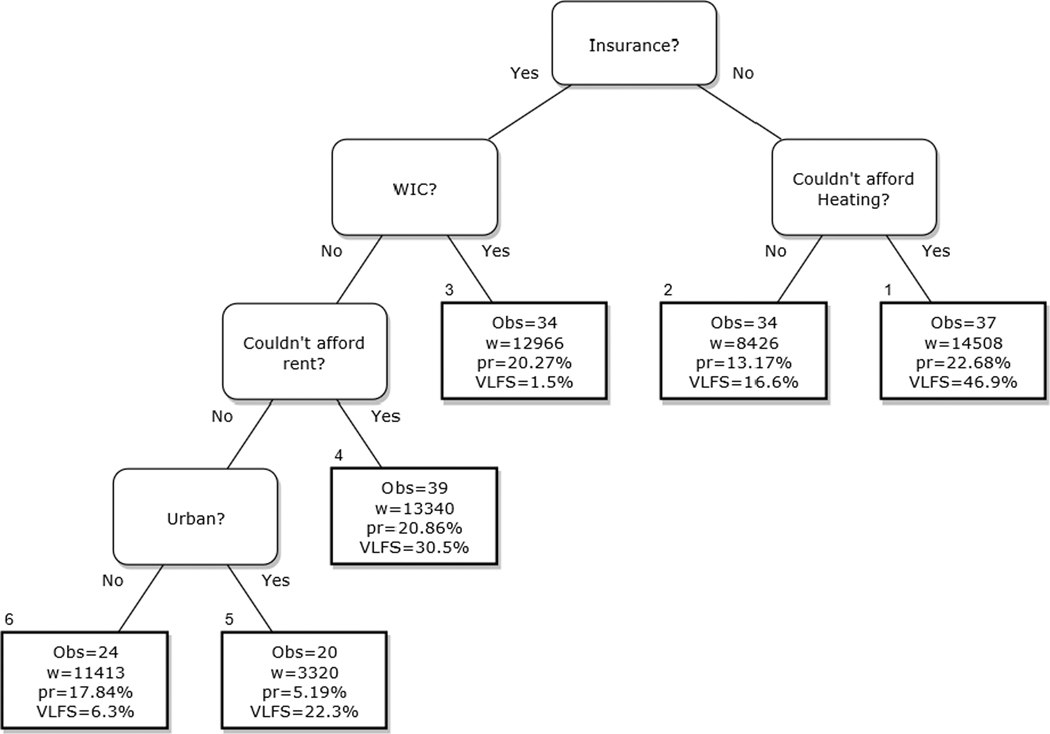
The CHAID analysis identified six groups based on five variables. Among all participants, the most significant predictor of VLFS-C that anchored the CHAID model was having insurance (X2 = 21.19, df = 1,31, p < 0.0001). Participants with insurance had lower rates of VLFS-C (36.22%) compared to those without insurance (61.32%). Branching to the right as shown in Figure 1, those persons without insurance (n =73, N = 22,934) were then bisected based on their ability to pay their heating bills. Households that were able to pay their heating bill had a lower percentage of VLFS-C (16.6%) than those having difficulties (46.9%). Figure 1 depicts branches that further differentiated groups among those with health insurance. For example, among those with insurance, but without WIC, VLFS-C was more common if the client reported difficulty paying rent and accessed a food pantry located in an urban location. Each terminal group provides sample and population sizes, proportion of clients, and the percent of VLFS-C displayed within each terminal node.
Figure 1.
CHAID model showing the decision path among variables classifying childhood food insecurity. The number of observations, weighted representation (w), and proportion (pr) of the population are accompanied with the percent misclassification (err) for each terminal node.
Two groups (nodes 3 and 6) showed much lower rates of VLFS-C (1.5% and 6.3%, respectively) compared to the population average (23.2%). These two groups had the highest percentages of females (90.5% & 85.3%, respectively) among all groups (Table 4). Conversely, two groups (nodes 1 and 4) had much higher prevalence of VLFS-C (46.9% and 30.5%, respectively). Node 1 had the highest proportion of males (44.4%), although node 4 had a lower proportion of males (24.9%). There were no significant differences by race or ethnicity among nodes (p = 0.160). The CHAID tree had an overall accuracy rate of 77.7%. The overall sensitivity of the analysis was 0.444, while the specificity was 0.881, meaning the CHAID was better at predicting the absence of VLFS-C rather than predicting its presence.
Table 4.
Percent of households (N = 63,917) with child level food security status, gender and race, by node.
| Node | No VLFS-C | VLFS-C | Female | Male | White | Black | American Indian | Non-Hispanic Other | Hispanic |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 53.11 | 46.89 | 55.65 | 44.35 | 47.46 | 7.975 | 1.50 | 20.26 | 22.80 |
| 2 | 83.39 | 16.61 | 76.20 | 23.80 | 71.35 | 4.903 | 5.51 | 3.40 | 14.84 |
| 3 | 98.53 | 1.47 | 90.52 | 9.48 | 28.2 | 27.43 | 15.56 | 19.27 | 9.54 |
| 4 | 70.16 | 30.48 | 81.54 | 18.46 | 41.04 | 28.06 | 17.90 | 1.64 | 11.36 |
| 5 | 77.32 | 22.27 | 75.08 | 24.92 | 40.89 | 47.44 | 11.67 | 0.00 | 0.00 |
| 6 | 93.74 | 6.26 | 85.33 | 14.67 | 39.33 | 21.71 | 14.05 | 6.85 | 18.06 |
| Total | 76.84 | 23.16 | 77.11 | 22.89 | 43.46 | 20.58 | 11.37 | 10.21 | 14.38 |
| Design based Chi2 | F(3.84, 118.97) =6.54, P < 0.0001 | F(2.96, 91.68) =3.341, p = 0.023 | F(5.84, 181.15) =1.58, P = 0.160 | ||||||
Abbreviations: VLFS-C: Very Low Food Security among Children
Discussion
This study explored candidate risk factors that may contribute to a household’s inability to provide consistent and adequate food access for children within a representative sample of food pantry clients in Oklahoma. Our analyses suggest the rate of VLFS-C is substantially higher among families accessing food pantries compared to the rate of VLFS-C among US households. These findings support the need for targeted programs to address and prevent VLFS-C in food pantry settings. Our analyses also identified how select risk factors may be shared to define food pantry subpopulations, which indicates the need for tailored food insecurity interventions in these settings. Here, we expand our discussion on these main findings, including our recommendations for food banks, food pantries, and policy makers who wish to reduce VLFS-C in their communities.
The high rates of child-level food insecurity experienced within this population must first be emphasized. A large majority of households with children experienced some degree of child-level food insecurity, with nearly half reporting low food security among children and nearly one-quarter reporting very low food security among children. These data suggest that families accessing food pantry programs represent a highly-vulnerable population who could benefit from interventions to address underlying causes of child food insecurity that extend beyond temporary food assistance. Strengthening the charitable food system’s capacity to address these root causes could substantially improve lifecourse trajectories for children within client households, as VLFS-C can have lasting impacts on child, adolescent, and adulthood outcomes.
To identify potential intervention points, our analyses explored multiple candidate risk factors for VLFS-C that were considered based on their associations with VLFS-C in the general population. Because households accessing food pantries represent a population that is disproportionately impacted by these risk factors, many of these candidate risk factors were not statistically associated with VLFS-C, most likely due to high rates of risk factors and high rates of VLFS-C in this study’s sample. However, our study suggests that charitable food programs should consider targeting client households with incomes below $15,000 who report unmet basic needs including insurance, housing, or utilities, and who rely upon food pantries more heavily as ideal candidates for VLFS-C prevention programs. Children living with adults in poor physical or mental health are also at higher risk, which is consistent with past research from the general population (Anderson et al., 2016). The economic consequences of these health issues may further be worsened among those families who are uninsured. After adjustment for all of these risk factors, our analyses found that WIC is highly protective against VLFS-C, so charitable food programs should prioritize their efforts in first referring eligible families to this program. Food programs with greater resources should work toward models that additionally integrate healthcare access, housing assistance, and mental health to provide wholistic care that better addresses these potential root causes of food insecurity.
This study also explored how risk factors may coalesce to define subgroups within the charitable food population, which is important for tailoring interventions to better meet the needs of families. This component of our analyes revealed that the strongest differentiator among groups is access to health insurance. Among those families without health insurance, not being able to afford heating best predicts VLFS-C risk. Among those families with health insurance and who have WIC, the risk for VLFS-C was virtually absent. However, when WIC is absent, not being able to pay rent and living in an urban community become important risk characteristics among those families with health insurance. In total, these analyses support the fundamental importance of social programs that support household access to health insurance by building on the literature connecting health insurance and household food security. For example, one recent study exploring the effect of Medicaid expansion among low-income childless adults found that expansion states experienced a significant overall decrease in very low food security amoung adults, while states without expansion saw a slight increase (Himmelstein, 2019). These findings also re-affirm the critical role of WIC in protecting against VLSF-C (Kreider et al., 2016). Charitable food organizations can use these data to advocate for state policies that support Medicaid expansion and WIC access.
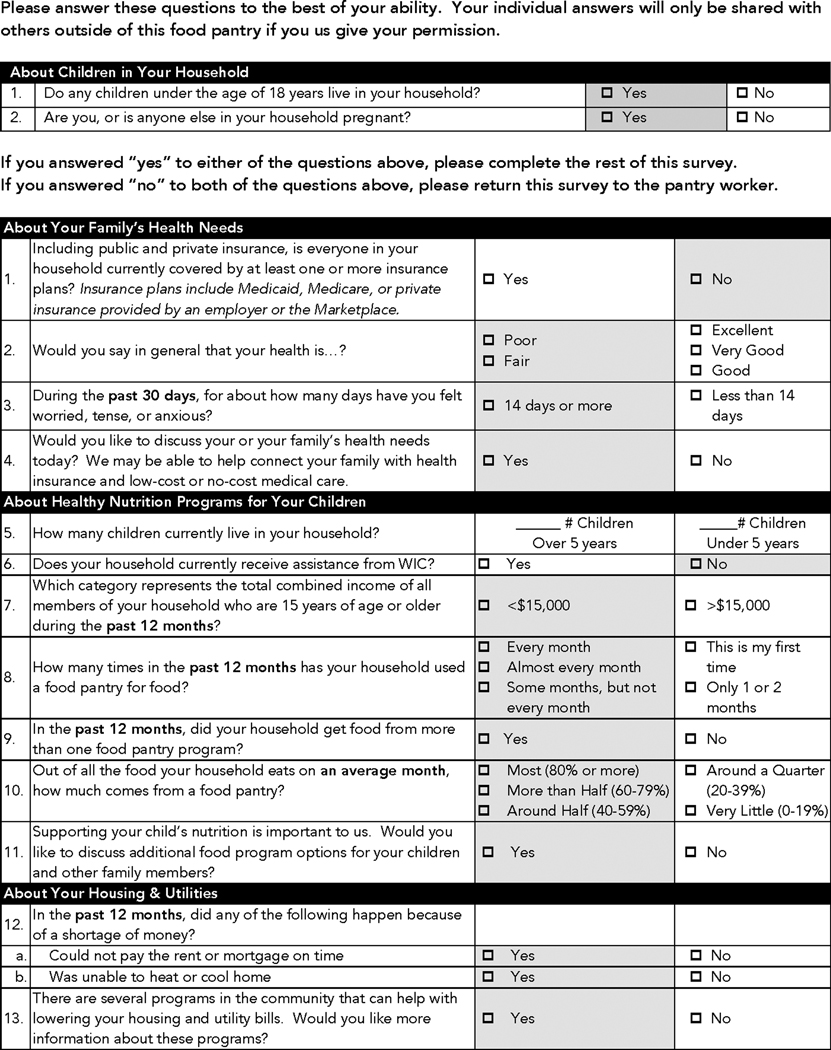
Charitable food programs that wish to act on these study findings should consider screen-and-interevene type initiatives. Figure 2 presents a “Pantry Assessment Tool against Child Hunger (PATCH)” screening form that includes significant variables from our analyses; such a tool could help food pantry staff to identify those underlying factors that may be driving child-level food insecurity within a household. By assessing each household’s individual needs, programs could better direct households to appropriate entities. For example, families who appear eligible for WIC or Medicaid would receive referrals to the local WIC office or the state’s Medicaid agency. More robust screen-and-intervene models could introduce healthcare navigation services to assist eligible families with actively enrolling in Medicaid through the Health Insurance Marketplace or in partnership with that state’s Medicaid agency. Similarly, WIC offices could be strategically placed adjacent to food pantries or in a shared location to better faciliate cross-referral partnerships. For those families with children who are not eligible for WIC, food pantries could implement procedures that would allow for greater levels of food assistance for high risk families.
Figure 2.
Pantry Assessment Tool against Child Hunger (PATCH)
Over time, food programs can use results from the PATCH screenings to more formally conduct a needs assessment of their client population to inform decisions about which types of assistance or referral partnerships should be delivered on-site. This is especially important for smaller programs that are unable to address all types of basic needs. For example, if a program finds that many households report difficulty in paying housing bills, and most are already enrolled in SNAP, that program would prioritize its efforts to develop referral relationships with housing assistance programs over SNAP referrals.
However, the impact of any screening tool will be limited if the majority of the population does not receive the indicated care. Our analysis found that the majority of participants were not interested in receiving housing, employment, or SNAP assistance at the food pantry where they were surveyed. Additional qualitative research is needed to explore reluctance by some families to accept forms of non-food assistance at food pantries. Such hesitation by clients could be due to perceived stigma associated with public assistance programs, privacy concerns, perceived ineligibility, or relationship dynamics between food pantry clients and workers. In this study, perceived social support was lowest among those households with VLFS-C. Thus, qualitative inquiries should explore under what conditions clients perceive food pantries to be a trusted part of their social support network, including unique perspectives among households with VLFS-C. Past qualitative research indicates that food pantries can be a source of social support and hope for clients, which is likely dependent upon food pantry workers’ ability to emotionally connect with clients and deliver assistance in a nonjudgmental way (Jones et al., 2019; Vissing et al., 2017). These factors are likely critical for the successful design and implementation of VLFS-C screening programs, including food pantry staff training on how to administer screenings and serve as a trusted source for indicated referrals.
This cross-sectional study has important limitations. First, we are unable to confirm the directionality of the relationships between the independent variables explored and VLFS-C. Second, this study identified higher VLFS-C rates among urban food pantry providers compared to rural, and we are unable to comment upon community-level factors that may be driving these higher rates. Exploring geographic factors that influence VLFS-C should be the focus of future research and intervention. Since this sample was only taken from food pantries within one state, results may not be applicable in states with vastly different political environments that affect use of public assistance programs and insurance access (e.g., Medicaid expansion). Future research could include comparative studies between various states or could use a national level sample. Because the survey was only available in English, the study’s findings are limited to English-speaking households and may therefore overlook important risks for VLFS-C among non-English speaking households with children. Finally, the PATCH screening tool was developed for households with children and includes programs that are only accessible or primarily utilized by families with children, including WIC and Medicaid. Additional research is needed to develop screening tools to identify risks for VLFS in other vulnerable populations, such as community-dwelling older adults and individuals with physical disabilities without children in the home.
Conclusion
Food pantries serve households with children that experience very high rates of VLFS-C, and may provide a physical location for connecting at risk families with non-food resources to support improved household food security. Our PATCH questionnaire, which emphasizes WIC, health insurance, and utility assistance referrals, may be one screening option for use in these settings to evaluate and respond to client needs in ways beyond acute food assistance. When these forms of assistance are not available or accessible, food pantries should consider providing high-risk families with greater levels of food assistance to possibly prevent VLFS-C. These targeted screening and referral strategies should be further evaluated in longitudinal intervention studies designed to sustainably improve household food security and improve child developmental outcomes by lowering modifiable risks through new food pantry-based programs and referral initiatives.
Acknowledgments:
The authors would like to thank the Community Food Bank of Eastern Oklahoma and the Regional Food Bank of Oklahoma for their collaboration in the development and implementation of the Food Independence, Security, and Health (FISH) study. The authors also thank the following individuals for their assistance in the research that supported the development of this manuscript: Kathryn P. Martin (literature review), Ji Li (data cleaning and preparation), Isaac Washburn (statistical consultation), and Jennifer and Damon Vidrine (original FISH study co-investigators).
Funding Statement:
This work was supported by the National Institute of General Medical Sciences of the National Institutes of Health under Award Number P20GM109097. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Partial funding for the FISH study was provided by the Oklahoma Tobacco Settlement Endowment Trust through a grant to the Oklahoma Tobacco Research Center [092–016-0002; PI: JI Vidrine].
Footnotes
Data Availability Statement:
The de-identified data that support the findings of this study are available from the corresponding author, MSW, upon reasonable request.
Footnote: Eileen Bradshaw is presently the Executive Director of LIFE Senior Services, Tulsa, OK, USA; Shiraya Proffitt is presently the owner and operator of Charcuteray, Tulsa, OK, USA; Kayla C. White is presently an outpatient dietitian at Northwest Texas Healthcare System, Amarillo, TX 79106
References:
- An R, Wang J, Liu J, Shen J, Loehmer E, & McCaffrey J. (2019). A systematic review of food pantry-based interventions in the USA. Public Health Nutrition, 22(9), 1704–1716. 10.1017/S1368980019000144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson PM, Butcher KF, Hoynes HW, & Whitmore Schanzenbach D. (2016). Beyond Income: What Else Predicts Very Low Food Security Among Children? Southern Economic Journal, 82(4), 1078–1105. 10.1002/soej.12079 [DOI] [Google Scholar]
- Broadhead WE, Gehlbach SH, de Gruy FV, & Kaplan BH (1988). The Duke-UNC Functional Social Support Questionnaire. Measurement of social support in family medicine patients. Medical Care, 26(7), 709–723. 10.1097/00005650-198807000-00006 [DOI] [PubMed] [Google Scholar]
- Bruening M, Dinour LM, & Chavez JBR (2017). Food insecurity and emotional health in the USA: A systematic narrative review of longitudinal research. Public Health Nutrition, 20(17), 3200–3208. 10.1017/s1368980017002221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke MP, Martini LH, Cayir E, Hartline-Grafton HL, & Meade RL (2016). Severity of household food insecurity is positively associated with mental disorders among children and adolescents in the United States. Journal of Nutrition, 146(10), 2019–2026. 10.3945/jn.116.232298 [DOI] [PubMed] [Google Scholar]
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, & Bradley KA (1998). The audit alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. Archives of Internal Medicine, 158(16), 1789–1795. 10.1001/archinte.158.16.1789 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2014, ). Behavioral Risk Factor Surveillance System questionnaire. Retrieved November 25, 2019 from http://www.cdc.gov/brfss/questionnaires/pdf-ques/2014_brfss.pdf
- Chilton M, Chyatte M, & Breaux J. (2007). The negative effects of poverty & food insecurity on child development. Indian Journal of Medical Research, 126(4), 262–272. [PubMed] [Google Scholar]
- Chilton M, Knowles M, & Bloom SL (2017). The intergenerational circumstances of household food insecurity and adversity. Journal of Hunger & Environmental Nutrition, 12(2), 269–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chilton M, Knowles M, Rabinowich J, & Arnold KT (2015). The relationship between childhood adversity and food insecurity: ‘It’s like a bird nesting in your head’. Public Health Nutrition, 18(14), 2643–2653. 10.1017/s1368980014003036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein R. (1983, December). A global measure of perceived stress. Journal of Health and Social Behavior, 24(4), 385–396. [PubMed] [Google Scholar]
- Coleman-Jensen A, Rabbitt MP, Gregory CA, & Singh A. (2020). Household Food Security in the United States in 2019, ERR-275. https://www.ers.usda.gov/publications/pub-details/?pubid=99281 [Google Scholar]
- Cook JT, Frank DA, Levenson SM, Neault NB, Heeren TC, Black MM, Berkowitz C, Casey PH, Meyers AF, Cutts DB, & Chilton M. (2006). Child food insecurity increases risks posed by household food insecurity to young children’s health. Journal of Nutrition, 136(4), 1073–1076. 10.1093/jn/136.4.1073 [DOI] [PubMed] [Google Scholar]
- Cutler-Triggs C, Fryer GE, Miyoshi TJ, & Weitzman M. (2008). Increased rates and severity of child and adult food insecurity in households with adult smokers. Archives of Pediatrics and Adolescent Medicine, 162(11), 1056–1062. 10.1001/archpediatrics.2008.2 [DOI] [PubMed] [Google Scholar]
- Drucker ER, Liese AD, Sercy E, Bell BA, Draper C, Fleischer NL, Flory K, & Jones SJ (2019). Food insecurity, childhood hunger and caregiver life experiences among households with children in South Carolina, USA. Public Health Nutrition, 22(14), 2581–2590. 10.1017/S1368980019000922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Economic Research Service. (2012). U.S. Household Food Security Survey Module: Three-stage design, with screeners. https://www.ers.usda.gov/media/8271/hh2012.pdf
- Ettinger de Cuba S, Bovell-Ammon A, Cook J, Coleman S, Black M, Chilton M, Casey P, Cutts D, Heeren T, & Sandel M. (2019). SNAP, young children’s health, and family food security and healthcare access. American Journal of Preventive Medicine, 57(4), 525. 10.1016/j.amepre.2019.04.027 [DOI] [PubMed] [Google Scholar]
- Feeding America. (2018). Child food insecurity. Feeding America. https://www.feedingamerica.org/sites/default/files/research/map-the-meal-gap/2016/2016-map-the-meal-gap-child-food-insecurity.pdf [Google Scholar]
- Greenberg M, Greenberg G, & Mazza L. (2010). Food pantries, poverty, and social justice. American Journal of Public Health, 100(11), 2021–2022. 10.2105/AJPH.2010.201848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gundersen C, Engelhard E, & Hake M. (2017). The determinants of food insecurity among food bank clients in the United States. Journal of Consumer Affairs, 51(3), 501–518. 10.1111/joca.12157 [DOI] [Google Scholar]
- Hahs-Vaughn DL, & Lomax RG (2012). An introduction to statistical concepts (3rd Edition ed.). Routledge. [Google Scholar]
- Harvey K. (2016). “When I go to bed hungry and sleep, I’m not hungry”: Children and parents’ experiences of food insecurity. Appetite, 99, 235–244. 10.1016/j.appet.2016.01.004 [DOI] [PubMed] [Google Scholar]
- Himmelstein G. (2019). Effect of the Affordable Care Act’s Medicaid expansions on food security, 2010–2016. American Journal of Public Health, 109(9), 1243–1248. 10.2105/ajph.2019.305168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holben DH, McClincy MC, Holcomb JP Jr, Dean KL, & Walker CE (2004). Food security status of households in Appalachian Ohio with children in Head Start. Journal of the American Dietetic Association, 104(2), 238–241. 10.1016/j.jada.2003.09.023 [DOI] [PubMed] [Google Scholar]
- Hothorn T, & Zeileis A. (2015a). CHAID: CHi-square Automatic Interaction Detection R package. In (Version 0.1–2) [Google Scholar]
- Hothorn T, & Zeileis A. (2015b). Partykit: A modular toolkit for recursive partytioning in R. Journal of Machine Learning Research, 16, 3905–3909. http://jmlr.org/papers/v16/hothorn15a.html [Google Scholar]
- Jones CL, Ksobiech K, & Maclin K. (2019). “They do a wonderful job of surviving”: Supportive communication exchanges between volunteers and users of a choice food pantry. Journal of Hunger & Environmental Nutrition, 14(1–2), 204–224. 10.1080/19320248.2017.1337535 [DOI] [Google Scholar]
- Jyoti DF, Frongillo EA, & Jones SJ (2005, ). Food insecurity affects school children’s academic performance, weight gain, and social skills. Journal of Nutrition, 135(12), 2831–2839. 10.1093/jn/135.12.2831 [DOI] [PubMed] [Google Scholar]
- Kass G. (1980). An exploratory technique for investigating large quantities of categorical data. Journal of the Royal Statistical Society. Series C (Applied Statistics), 29(2), 119–127. 10.2307/2986296 [DOI] [Google Scholar]
- Kim JE, & Tsoh JY (2016, January 14). Cigarette smoking among socioeconomically disadvantaged young adults in association with food insecurity and other factors. Preventing Chronic Disease, 13, E08. 10.5888/pcd13.150458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbro RT, & Denney JT (2015, ). Transitions into food insecurity associated with behavioral problems and worse overall health among children. Health Affairs, 34(11), 1949–1955. 10.1377/hlthaff.2015.0626 [DOI] [PubMed] [Google Scholar]
- Kreider B, Pepper JV, & Roy M. (2016). Identifying the effects of WIC on food insecurity among infants and children. Southern Economic Journal, 82(4), 1106–1122. 10.1002/soej.12078 [DOI] [Google Scholar]
- Lippert AM, & Lee BA (2020, 2020/March/27). Adult and Child Food Insecurity Among Homeless and Precariously-Housed Families at the Close of the Twentieth Century. Population Research and Policy Review. 10.1007/s11113-020-09577-9 [DOI] [Google Scholar]
- Mangini LD, Hayward MD, Dong YQ, & Forman MR (2015, December). Household food insecurity is associated with childhood asthma. Journal of Nutrition, 145(12), 2756–2764. 10.3945/jn.115.215939 [DOI] [PubMed] [Google Scholar]
- Martin KS, Redelfs A, Wu R, Bogner O, & Whigham L. (2019). Offering more than food: Outcomes and lessons learned from a Fresh Start food pantry in Texas. Journal of Hunger & Environmental Nutrition, 14(1–2), 70–81. 10.1080/19320248.2018.1512925 [DOI] [Google Scholar]
- Martin KS, Wu R, Wolff M, Colantonio AG, & Grady J. (2013, November). A novel food pantry program: food security, self-sufficiency, and diet-quality outcomes. American Journal of Preventive Medicine, 45(5), 569–575. 10.1016/j.amepre.2013.06.012 [DOI] [PubMed] [Google Scholar]
- McIntyre L, Glanville NT, Raine KD, Dayle JB, Anderson B, & Battaglia N. (2003). Do low-income lone mothers compromise their nutrition to feed their children? Canadian Medical Association Journal, 168(6), 686–691. [PMC free article] [PubMed] [Google Scholar]
- Metallinos-Katsaras E, Colchamiro R, Edelstein S, & Siu E. (2016). Household food security status is associated with anemia risk at age 18 months among low-income infants in Massachusetts. Journal of the Academy of Nutrition and Dietetics, 116(11), 1760–1766. 10.1016/j.jand.2016.06.008 [DOI] [PubMed] [Google Scholar]
- Metallinos-Katsaras E, Gorman KS, Wilde P, & Kallio J. (2011). A longitudinal study of WIC participation on household food insecurity. Maternal and Child Health Journal, 15(5), 627–633. 10.1016/j.jand.2012.08.031 [DOI] [PubMed] [Google Scholar]
- Metallinos-Katsaras E, Must A, & Gorman K. (2012). A longitudinal study of food insecurity on obesity in preschool children. Journal of the Academy of Nutrition & Dietetics, 112(12), 1949–1958. 10.1016/j.jand.2012.08.031 [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics. (2016). Survey Description, National Health Interview Survey, 2015. [Google Scholar]
- National Research Council. (2006). Food Insecurity and Hunger in the United States: An Assessment of the Measure. The National Academies Press. 10.17226/11578 [DOI] [Google Scholar]
- Pryor L, Lioret S, Van Der Waerden J, Fombonne É, Falissard B, & Melchior M. (2016). Food insecurity and mental health problems among a community sample of young adults. Social Psychiatry and Psychiatric Epidemiology, 51(8), 1073–1081. 10.1007/s00127-016-1249-9 [DOI] [PubMed] [Google Scholar]
- R Core Team. (2017). R: A language and environment for statistical computing. In R Foundation for Statistical Computing. http://www.R-project.org/ [Google Scholar]
- Rose-Jacobs R, Black MM, Casey PH, Cook JT, Cutts DB, Chilton M, Heeren T, Levenson SM, Meyers AF, & Frank DA (2008). Household food insecurity: associations with at-risk infant and toddler development. Pediatrics, 121(1), 65–72. 10.1542/peds.2006-3717 [DOI] [PubMed] [Google Scholar]
- Rubin D. (2004). Multiple imputation for nonresponse in surveys. Wiley. [Google Scholar]
- Ryu JH, & Bartfeld JS (2012, ). Household food insecurity during childhood and subsequent health status: the early childhood longitudinal study--kindergarten cohort. American Journal of Public Health, 102(11), e50–55. 10.2105/ajph.2012.300971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seligman HK, & Schillinger D. (2010). Hunger and socioeconomic disparities in chronic disease. New England Journal of Medicine, 363(1), 6–9. [DOI] [PubMed] [Google Scholar]
- Siahpush M, & Carlin JB (2006, January). Financial stress, smoking cessation and relapse: results from a prospective study of an Australian national sample. Addiction, 101(1), 121–127. 10.1111/j.1360-0443.2005.01292.x [DOI] [PubMed] [Google Scholar]
- Siefert K, Heflin CM, Corcoran ME, & Williams DR (2001). Food insufficiency and the physical and mental health of low-income women. Women and Health, 32(1–2), 159–177. 10.1300/J013v32n01_08 [DOI] [PubMed] [Google Scholar]
- Vissing Y, Gu J, Jones A, & Gabriel S. (2017, 2017/November/01). Preserving dignity in the face of hunger: A study of food pantry utilization. Humanity & Society, 41(4), 461–481. 10.1177/0160597617733623 [DOI] [Google Scholar]
- Weinfield N, Mills G, Borger C, Gearing M, Macaluso T, Montaquila J, & Zedlewski S. (2014). Hunger in America 2014: National report prepared for Feeding America. http://help.feedingamerica.org/HungerInAmerica/hunger-in-america-2014-full-report.pdf [Google Scholar]