Abstract
Background
: The COVID-19 outbreak has affected the elderly's physical and mental health. The application of information and communication technology, such as mobile health (m-health), can help control this pandemic by changing the behavior and lifestyle of the elderly during this time of crisis.
Objective
: This review aimed to synthesize the capabilities of m-health in providing health services to the elderly during the COVID-19 pandemic, and to identify the factors contributing to the success of these tools.
Methods
: To find the relevant studies, a search was conducted in PubMed, Web of Science, Scopus, ProQuest, and Google Scholar. The inclusion criteria were: studies in English that used m-health intervention in all aspects of elderly healthcare during the COVID-19 outbreak, were published in peer-reviewed journals from 31 December 2019, and had any research design and methodology. Two authors independently took all the steps of this review, and finally performed narrative synthesis to report the findings.
Results
: Our initial search identified 421 studies, of which 10 met the inclusion criteria. The data analysis showed that all the m-health interventions had positive effects on the health of the elderly. The m-health services for the elderly during the current pandemic were used for therapy, information provision, self-help, monitoring, and mental health consultation purposes. The results also indicated that various factors affected the elderly's use of m-health tools.
Conclusion
: The application of m-health keeps the elderly and healthcare providers safe, accelerates health service provision, reduces the costs of service provision, and decreases the risk of morbidity and mortality during the COVID-19 outbreak. The successful use of m-health tools for the elderly in health programs during the current crisis greatly depends on supporting the elderly and overcoming the barriers.
Keywords: M-health, Coronavirus, COVID-19, Outbreak, Elderly
Introduction
On December 31, 2019, a cluster of a genus of the Coronaviridae family was officially reported from Wuhan, Hubei Province, China, which caused the novel coronavirus disease (COVID-19) [1,2]. This infection widely spread to other regions of the world, and primary evidence revealed that the elderly and those with underlying medical problems (e.g. cardiac diseases, diabetes, hypertension, and cancers) are more susceptible to the disease in its most intensive form [3].
As the older population has a much higher risk of mortality compared to younger people during the COVID-19 pandemic, it is emphasized that the elderly should be protected with social distancing or, if necessary, social isolation [4,5]. Loneliness and social isolation may lead to many problems such as depression, cognitive dysfunction, disability, cardiovascular diseases, and increased mortality among older adults [6]. The ongoing COVID-19 pandemic has highlighted the need for mobile technology solutions to diminish the risk of cross-contamination caused by close contact [4,7,8]. Smart technology (e.g. mobile-based technology) has been important for exploring meaning in life, self-care, consultation, and creating a positive feeling for confined older adults [9,10].
The term m-health refers to smart phone applications and is increasingly used in the healthcare sector [11]. It is proposed to be a technology which may be either short- or long-distance, or system-driven [12]. More specifically, m-health is defined as the provision of health intervention using mobile-based tools, including phone calls, video consultation, wearable devices, personal digital assistants, tablets, and personal computers (PCs) [13]. The main concept of m-health is that it can provide health services, anytime and anywhere, to anyone, by removing geographical, temporal, and other barriers [14]. It is also reported that mobile-based tele-visits can improve access for an estimated 6.3 million older people who are inexperienced with technology tools or have visual problems [15,36]. Remote interventions are potentially effective and utilized by older people, but healthcare providers should ensure that digital services are suitable for the older demographic and provide both the technology and the technical support needed for interventions in the current pandemic [16].
Previous studies have reported the potential role of m-health tools in providing long-term support and health promotion for the elderly [17], [18], [19]. For example, the results of a systematic review showed a positive effect of mobile interventions on sexual health outcomes in chronic patients and emphasized that mobile interventions can be more effective in combination with smartphone apps [19]. According to another systematic review, the use of mobile to provide tele-health in the COVID-19 outbreak is very effective in promoting health services [35]. Also, the results of a study showed that mobile applications are a valuable tool for people, healthcare providers and decision makers in the face of critical challenges posed by the COVID-19 epidemic, such as reducing hospital burdens, access to reliable information, tracking symptoms and mental health [37]. However, there is no systematic review on the role of m-health in improving the health of the elderly during the COVID-19 pandemic. Thus, this study aimed to synthesize the literature on the capabilities of m-health in providing health services to the elderly during the COVID-19 outbreak, and to identify the factors associated with the success of these tools. The research questions were:
-
•
What are the capabilities of the available m-health services for the elderly during the COVID-19 pandemic?
-
•
What factors are associated with the success of m-health tools for the elderly during this global emergency?
Materials and methods
Study design
This review was reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. All the steps of this review, namely the search in databases, study selection, quality evaluation, data extraction, and data analysis, were independently performed by two authors (S.AB. and S.F.), and in case of any discrepancies, the opinions of the third author were used. Conflicts were also resolved in such a way that the authors convened a meeting and the Conflicts were discussed. Finally, the authors consensus on how to proceed.
Bibliography search strategy
To identify studies on m-health tools used to help the elderly which were published during the COVID-19 pandemic, a comprehensive search was conducted in PubMed, ProQuest, Web of Science, Scopus, and Google Scholar, since the appearance of COVID-19 in Wuhan, Hubei Province, China, from December 31, 2019. Given the aim for this review, the search was conducted on titles and abstracts via a combination of relevant keywords: [1] COVID19, COVID-19, Coronavirus, Novel Coronavirus, 2019-nCoV, Wuhan Coronavirus, SARS-CoV-2, SARS2 [2], Aging, senior, aged, elderly, old*[3] M-health, m-health, handheld computer, mobile phone, smartphone, mobile application, mobile app, cellular phone, mobile device, mobile technology, SMS, or text message. Hand searching in web-based resources was also accomplished, and the selected articles' references were reviewed to identify additional studies (reference by reference). The sources were managed in EndNote x7. The search strategy was adapted for each bibliography database, and the search was conducted on March 30, 2021. As an example, the full search strategy on PubMed is given in Table 1 .
Table 1.
Search terms and strategy used in PubMed.
| (COVID-19[title/abstract] OR COVID19[title/abstract] OR Coronavirus [title/abstract] OR Novel coronavirus [title/abstract] OR 2019-nCoV [title/abstract] OR Wuhan coronavirus [title/abstract] OR SARS-CoV-2[title/abstract] OR SARS2[title/abstract]) |
|---|
| AND |
| (Elderly [title/abstract] OR Old* [title/abstract] OR Aged [title/abstract] OR Senior [title/abstract] OR Aging [title/abstract]) |
| AND |
| (mhealth [title/abstract] OR m-health [title/abstract] OR Handheld computer [title/abstract] OR Mobile phone [title/abstract] OR Smartphone [title/abstract] OR Mobile application [title/abstract] OR Mobile technology [title/abstract] OR Mobile device [title/abstract] OR Cellular phone [title/abstract] OR Mobile app [title/abstract] OR Text message [title/abstract] OR SMS [title/abstract]). |
Eligibility criteria
All the included studies had to meet the following inclusion criteria:
-
•
Study types: interventional, observational, modeling, or case studies.
-
•
Date of publication: December 31, 2019, to March 30, 2021.
-
•
Language: English.
-
•
Place of publication: peer-reviewed journals.
-
•
Population: elderly people (aged >60 years).
-
•
Analysis criteria: studies on the use of m-health to support the elderly living at home or in a healthcare setting during the COVID-19 outbreak.
Studies about other technologies (e.g. Internet of medical things or IoMT), studies which had not stated the primary objective of the intervention or reported incomplete information, conference abstracts, review articles, letters to the editor, and opinion papers were excluded.
Study selection
In the process of study selection, first, a screening was performed to remove duplicates from the datasets retrieved from the mentioned databases, and the papers were reviewed based on their titles. Subsequently, relevant papers were screened based on their abstracts. After initial screening, the remaining papers were screened in the third phase by reviewing their full text according to predefined inclusion and exclusion criteria.
Data extraction and quality assessment
The authors used Microsoft Word 2016 to design a standard data extraction form. The following information on the eligible studies was extracted: study identification (authors and publication year), study design, country, population (N), the device or technology used, intervention, and key findings.
We assessed the methodology of each included study in accordance with the Critical Appraisal Skills Program (CASP) checklists. The CASP tools were developed to teach people how to critically appraise different types of evidence [34]. It consists of questions that address issues such as goals, participant selection process, data collection, analysis, the role of researchers in the results, and ethical issues associated with the published study. In the CASP tools, the following responses to questions are possible: [1] yes, [2] no, and [3] cannot tell. Quality assessment was performed independently by two experts in this field and in case of any discrepancies, the opinions of the third author were used. Each question at this checklist valued one score, so studies were divided in poor, average and good groups according to their scores. The criteria for giving a complete score to each checklist item was compliance with the instructions and checklist items in the article under review. The included studies were also divided into three categories of weak, medium, and good based on their quality assessment scoring. The studies were ranked in the following manner: if an study scored <30% it belonged to the weak category, if it scored 30–70% the medium category, and if it scored >70% to the good category.
Evidence analysis
Due to the heterogeneity of the designs and objectives of the included studies, a narrative synthesis was performed to summarize the overall evidence by comparing and contrasting the data. The authors reached a consensus on the findings' categorized data according to the details, and qualitatively described and presented the results.
Results
Selection of articles
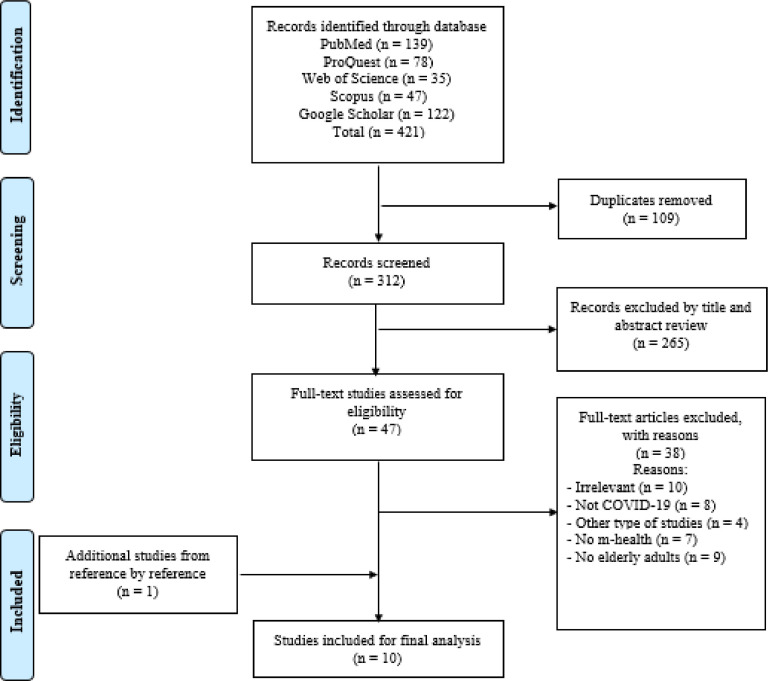
All the identified studies were imported into EndNote X7 which retrieved 312 studies after the removal of duplicates. After screening the titles and abstracts of the studies, 47 relevant studies with a full text were appraised according to the inclusion and exclusion criteria. After reading the full text of the articles, the authors included nine papers for evidence synthesis. One study was also added after reference screening (reference by reference) and, finally, 10 articles were included for final analyses. The details of the screening procedure are depicted in the PRISMA flow diagram in Fig. 1 .
Fig. 1.
Search redults and publication selection procedure.
Characteristics of the included articles
Table 2 presents the details of the included studies. This corpus comprised studies that showed the capability of m-health applications in the elderly's life during this emergency situation, and also reporting factors associated with the success of m-health to ensure the application of m-health tools. The 10 studies that met the eligibility criteria had been conducted in various countries, including the Netherlands, China, Canada, United Kingdom, France, Sweden, Italy, Mexico, Portugal, and Spain. Eight studies (80%) were rated as having good quality, two (20%) had medium quality, and no study was excluded on the basis of the level of quality.
Table 2.
General characteristics and key findings of the included studies.
| Author and year | Study design | Country | Population of study (N) | Device or technology used | Intervention | Key finding |
|---|---|---|---|---|---|---|
| Meinert et al. (2020) [20] | Case study | United Kingdom, France, and Sweden | Older users and their family members (N = 6000 user) | Digital health mobile app | Design, develop, and deploy a digital health mobile app to provide a means of assisting families and peer groups in maintaining contact with older people | Solution with the capacity of connecting vast geographies of individuals Creates a capability for virtual interconnectedness Tackle a new and urgent issue arising to combat the COVID-19 worldwide pandemic Connect the older adults with their family and friends during social distancing To encourage positive nutrition, enhance physical activity, and promote mental |
| Jaana and Paré (2020) [21] | Cross-sectional survey | Canada | Canadian residents/65 years and older (N = 4109) | Not Applicable | To compare older adults' use of m-health technologies to that of the general adult population in Canada and to investigate the factors that affect their use | Considerable number of older adults reported using internet and smart technology Support the m-health technologies of older people health and well-being needs in the community Used mobile apps by users to store and monitor health-related data The potential of m-health technologies for self-tracking purposes in the context of older adults Necessary to culture shift in the provision of care to older adults is deemed keep up with the development of m-health technologies and the changing demographics and expectations of patients and their caregivers |
| Cenzer et al. (2020) [22] | Cross-sectional survey | United States | older veterans (N = 118) | Not Applicable | To examine the capability and willingness of older veterans to participate in a VA Video Connect (VVC) visit during the COVID-19 pandemic | The 77% successful in the scheduled VVC visits There are some lingering issues with capability and willingness to participate in video telehealth visits, particularly among older adults residing in rural areas Education have a stronger influence on internet access - Factor affected the use VA Video Connect (VVC) by older: Availability of internet access (77%) Availability of email access (70%) Availability of a device with a camera (56%) Capable of participating in VVC appointments (56%) Willingness to participate in VVC appointments (58%) Capable and willing to participate in VVC appointments (53%) - Suggestions for more access to VVC appointments: Necessity of policy efforts to bring broadband internet access to rural residents Addressing the digital divide in rural area Needed of targeted educational efforts to train those residing in rural areas Need to distribution of video-capable devices be augmented by the provision of high-speed internet and age-friendly technical assistance |
| van Dyck et al. (2020) [23] | Observational study | United States | Nursing home residents (N = 30) | Telephone Outreach in the COVID-19 Outbreak (TOCO) Program | To address social isolation in nursing home residents, the Student Interest Group initiated a Telephone Outreach in the COVID-19 Outbreak (TOCO) Program that implements weekly phone calls with student volunteers. | Positive effect of TOCO Program among seniors Benefited the seniors from meaningful conversations with their volunteer companions The nursing home residents shared stories of their lives and their families with student volunteers Identify the unique and actionable needs of the senior companions by volunteers Recognized common challenges experienced by many of these older adults (e.g. feelings of restlessness and anxiety as isolation continues, and fearfulness as COVID-19 enters nursing home facilities) Exacerbated challenges for the elderly's due to lack of access to technology (e.g. limited computer and internet access to communicate with loved ones) Alleviate social isolation experienced by nursing home residents during the COVID-19 pandemic |
| Wang et al. (2020) [24] | Qualitative study | China | Elderly people (N = 8) | Not Applicable | How has the COVID-19 pandemic high-lighted the age-based mobile digital divide in China, and what are the implications for gerontological internet-based social work? | Replacing the mobile internet instead the PC to become the dominating online platform in China Need of younger (e.g. their granddaughter) to support older people to seek help through internet-based |
| Used the mobile internet to seek help, purchase masks, or show the Green Code for travelling by older people Need to simple apps for many older people Need to used mobile phone or tablet with a big screen for elderly Expensively of tablet with the call function for bought by elderly Internet-based ICT used by social workers should be better designed and accessible to older people in terms of visibility, price, and operation Urgent need to make more efforts to provide internet-based social work services Need to be better trained for social workers to deliver services tailored to the specific needs of elderly population' Assess the capabilities of each elderly client by social workers to use different forms of internet based methods before they provide services to that client | ||||||
| Van Dijk et al. (2020) [25] | Case study | Netherlands | Elderly patient aged between64 and 70 years (n = 4) | Online psychotherapy day-treatment program | To present first impressions on feasibility of transforming a psychotherapy day-treatment program for older persons into an online program | Comfort in setting up the individual treatment plan by video conferencing Increasing the motivation of therapists for positive change Existence of time for therapists to prepare the psychotherapy sessions Online and therapy of older ran smoothly Providing active movements (gymnastics),relaxation, and mindful exercises (e.g., Tai Chi) to the older patients |
| Office et al. (2020) [26] | Observational study | United States | Older adults at risk for increased social isolation during COVID-19 (N=-) | Phone call outreach program (Seniors Overcoming Social Isolation (SOS)) | Created a phone call outreach program in which medical and health professions student volunteers called older adults, living in long-term-care facilities (LTCFs) and the community, at risk of social isolation during COVID-19 | Creating happy and enjoyment among older patients to have someone to talk Interrupting social isolation of older adults and residents of independent Improving the lives of older adults during the COVID-19 pandemic Understanding the needs of older adults in the community |
| Humboldt et al. (2020) [27] | Qualitative study | Italian, Mexican, Portuguese and Spanish | Older participants aged 65–87 years (N = 351) | Not Applicable | To fill a knowledge gap about older adult perceptions of how smart technology influenced their meaning in life during the Covid-19 | Used of smart technology to connect with family, colleagues and friends and create meaningful relations Important instrument for carrying out older individual activities Helped to develop a sense of spirituality Health and safety-related support of older Allowed to self-growth and reflection about how to achieve self-growth during the Covid-19 To continue physical activity |
| Echeverría et al. (2020) [28] | Observational study | Spain | Older residents and individuals with physical and mental disabilities in long-term care facilities (N=-) | COVIDApp mobile tool | To report the implementation of COVIDApp innovative tool for the management of long-term care facility residents as a high-risk population, specifically for early identification and self-isolation of suspected cases, remote monitoring of mild cases, and real-time monitoring of the progression of the infection. | Helped to institutional staff from long-term care facilities and primary care clinicians address the COVID-19 pandemic Providing a new channel for real-time communication Early detection of suspected COVID-19 cases Rapid development of epidemiological actions (e.g. self-isolation of suspected cases and contacts and relocation after positive or negative results) Remote management of mild COVID-19 cases treated in institutions Knowledge of progression of the infection in long-term care facilities Advise and support older people in nursing homes through a website that enables direct contact between a senior geriatrician and centers for older people Monitor the progression of the infection Decrease in the number of deaths and confirmed cases of COVID-19 Enabled to intervene proactively by isolating residents with suspected infection early and by monitoring contacts Reduce transmission in a vulnerable population |
| McLellan et al. (2020) [29] | Observational study | United Kingdom | Elderly patient (N=-) | Smartphone-based application and web-portal (smartPDT®) | Determine the accuracy of the algorithms used in the commercial SmartPDT® application | Provide treatment for the common pre-malignant condition of chronic photo damaged skin actinic keratosis Creating a more convenient and reliable therapy Reducing risk in an elderly patient population during the Covid-19 pandemic |
Principal findings
Our review identified precious data on how m-health technologies have been used as a means of supporting the elderly during the COVID-19 outbreak. The data analysis revealed that health organizations, researchers, and companies suggest mobile-based tools as a method of providing information [25,28], facilitating communication, remotely monitoring vital signs [28], and limiting the number of times healthcare professionals and patients need to come into close contact during the COVID-19 pandemic [24,25,28]. Furthermore, the m-health technology (text, apps, calls, etc.) is used for other purposes, e.g. connecting older people with their families and friends during social distancing [20,23,27], purchasing masks, showing the green code for traveling [24], storing health information [21], managing chronic diseases [29], making appointments [22], and creating an upbeat feeling in the elderly [23]. According to these studies, systems supporting the elderly range from simple tablet- and telephone-based systems to mostly app-based platforms [20], [21], [22], [23], [24], [25], [26], [27], [28], [29]. Advantages provided by m-health tools include the ability to massively implement them in all healthcare settings [23,25,28], practicing social distancing [20], decreasing the transmission of diseases to the elderly as high-risk individuals, and reducing the mortality and morbidity rate among the elderly during this pandemic [25, [27], [28], [29]]. Despite the challenges, the relevance and impact of m-health solutions during the pandemic are important as they allow health service providers to effectively manage the elderly's well-being to prevent pressures on the healthcare system [20], [21], [22], [23], [24], [25], [26], [27], [28], [29]. This novel contribution will provide an evidence-based exemplar for future mobile-based app development pertaining to social isolation and loneliness during crisis [23,26,28]. Generally, m-health tools for the elderly during the current pandemic are used for therapy [25,29], information provision [21,22], self-help [21,27,28], monitoring [21,28], and mental health consultation purposes [20,28].
The reviewed studies reported factors associated with the use of m-health tools by older adults during the COVID-19 pandemic. Most of the reported factors, e.g. the availability of m-health tools [22], Internet access [22,23,24], and the elderly's willingness and capabilities [22,24], are important determinants of the use of m-health tools. Meanwhile, some of the largest facilitators in the adoption of m-health technologies include support from the government and family [21,24,27,28], empowerment of the elderly, addressing the digital problems in deprived areas [20,22,24], and increasing accessibility to simple mobiles or tablets [24], which can directly contribute to the use of m-health tools by the elderly to improve their health and combat the COVID-19 outbreak.
Discussion
This review exhibited evidence on the scope of m-health capabilities in providing health services for the elderly during the COVID-19 pandemic, and reported the factors associated with the success of these tools. The majority of the included studies aimed to design and develop a mobile-based app to address the health and well-being of the elderly by addressing specific COVID-19-related issues. These included apps, web-portals, video consultations, and telephone outreach, and the research population mainly consisted of older people with social isolation and residents of independent elderly, most often in need of communication and mental health promotion. This is not surprising as many psychological problems during quarantine can be prevented through positive communication or by improving the lives of older adults [23,26].
The global confinement during the COVID-19 pandemic has highlighted the effect of social isolation and loneliness on the older population [30], [31], [32]. In this global isolation, European countries (United Kingdom, France, Sweden, etc.) have designed and deployed health mobile apps to assist families and peer groups in maintaining contact with older people. These mobile apps can tackle new and urgent problems in managing COVID-19, and can be applied as a valuable tool for connecting vast population geographies, especially the elderly [20]. An important issue to consider when using these online services during the pandemic is the willingness and ability of older people to utilize m-health tools. For example, older adults hospitalized in healthcare centers could independently complete phone calls but not video calls, and tended to make phone calls more often than video calls [33]. Older people use phone calls due to their inability and desire, and making video calls is difficult for them and they have problems interacting face to face. Therefore, special attention should be paid to the manner and desire of the elderly to use mobile phones in the COVID-19 epidemic so that they can use the facilities of technology and mobile health without any problems.
Our results showed that m-health tools have been potential solutions for managing the problems of the elderly during the COVID-19 pandemic. For instance, according to a study conducted in the USA, the COVID mobile app is an innovative tool for the management of long-term care facility and can help provide a new channel for real-time communication, promote the early detection of suspected COVID-19 cases, and decrease the number of deaths and confirmed cases of COVID-19 in long-term care settings [28]. Also, the results show that m-health is a more effective way than the old methods of providing services to the elderly during the current epidemic and can promote spirituality, self-growth, physical activity and improve communication the elderly with another peoples [27].
COVID-19 has been a crisis of huge proportions for health delivery services associated with chronic diseases, especially among the elderly, and online services have been recognized as a potential solution for fighting these diseases [25,29]. Van Dijk et al. in the Netherlands have designed an online Psychotherapy Day-treatment Program which provides online psychotherapy sessions, with activities, movements, and mindfulness exercises [25]. This online mobile-based program can help avoid direct physical contact, reduce the risk of exposure to infections, and prevent the potential transmission of infections to the elderly and healthcare providers during the current emergency conditions. Generally, mobile-based online tools can help healthcare institutional staff and clinicians address the COVID-19 pandemic by providing a channel for real-time communication [28].
In this review, we also presented evidence on the factors associated with the use of m-health tools for health promotion among older adults to overcome COVID-19. These factors are major determinants of the use of m-health tools by the elderly. The results of a study in China found that a growing age-based mobile digital divide of China in the last decade and in the COVID-19 pandemic, older people encountered difficulties when using mobile phones to access the internet to seek help, which highlighted the problem of the mobile digital divide [24]. According to Cenzer et al., there are some lingering problems related to the capability and willingness to participate in video visits, particularly among older adults residing in rural areas. Factors affecting the use of VA Video Connect (VVC) by the elderly include Internet access, email access, access to devices with a camera, and the capability/willingness to participate in VVC appointments [22]. To incentivize the elderly and increase their usage of m-health tools, the studies suggest that replacing computers with mobile Internet, providing government and family support, addressing the digital divide, and making educational and policy efforts to combat the COVID-19 pandemic are essential measures [22,24]. Despite the huge potential of m-health tools in the promotion of elderly health, the government and health policy-makers should resolve the mentioned challenges. This can help the management of various problems and improve the control of COVID-19 in the elderly population.
Future research
The majority of the databases reviewed here published studies about the role of m-health tools in the older population, but only a few reports focused on a specific older group during the COVID-19 pandemic. Accordingly, health organizations and researchers should pay more attention to this domain so that the elderly can be taken care of in emergency situations such as COVID-19 with the help of m-health tools. More research has to be conducted to develop and evaluate new methods, and social worker training programs should be provided to ensure that older people can access these services. During this time of crisis, more evidence on the efficacy and cost-effectiveness of m-health tools in promoting the health and well-being of older adults is required. It is recommended that future studies determine how to set up m-health in healthcare settings (e.g. home nursing and elderly care centers), and assess the elderly and healthcare professionals' satisfaction with mobile-based services.
Limitations
The use of multiple and varied outcome measures during the COVID-19 pandemic limits the reliability of judgments about the efficacy of m-health interventions in supporting the elderly. Moreover, we did not have access to some databases such as CINAHL and PsycINFO, and could not access articles published in languages other than English.
Conclusion
The results of this review highlight the potentials of m-health tools in the promotion of health and well-being among the older population, and show that there is a variety of usages of such tools during the current pandemic. The use of m-health keeps the elderly and healthcare providers safe, accelerates health service provision, reduces the costs of service delivery, and decreases the risk of morbidity and mortality during the pandemic. Despite the advantages of using m-health tools for the elderly people, the results of this review showed that there are some challenges in the implementation of m-health to support the elderly which need attention from the government, healthcare providers, and society.
Patient consent
Not required.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethics approval and consent to participate
Not applicable.
CRediT authorship contribution statement
Sara Abbaspur-Behbahani: Conceptualization, Project administration, Data curation, Formal analysis, Investigation, Writing – original draft, Writing – review & editing. Elham Monaghesh: Writing – original draft, Writing – review & editing. Alireza Hajizadeh: Writing – review & editing. Saeedeh Fehresti: Conceptualization, Project administration, Data curation, Formal analysis, Investigation, Writing – original draft, Writing – review & editing.
Declaration of Competing Interest
None declared.
Acknowledgements
None.
References
- 1.WHO. Q&A on . 2020. Coronaviruses (COVID-19)https://www.who.int/news-room/q-a-detail/q-a-coronaviruses Available from. [Google Scholar]
- 2.Tay M.Z., Poh C.M., Rénia L., MacAry P.A., Ng L.F. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol. 2020:1–12. doi: 10.1038/s41577-020-0311-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lipsitch M., Swerdlow D.L., Finelli L. Defining the epidemiology of Covid-19—studies needed. N Engl J Med. 2020;382(13):1194–1196. doi: 10.1056/NEJMp2002125. [DOI] [PubMed] [Google Scholar]
- 4.Verma J., Mishra A.S. COVID-19 infection: disease detection and mobile technology. PeerJ. 2020;8:e10345. doi: 10.7717/peerj.10345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Verity R., Okell L.C., Dorigatti I., Winskill P., Whittaker C., Imai N., et al. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30243-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morley J.E., Vellas B. COVID-19 and older adult. J Nutr Health Aging. 2020;24(4):364–365. doi: 10.1007/s12603-020-1349-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smith A.C., Thomas E., Snoswell C.L., Haydon H., Mehrotra A., Clemensen J., et al. Telehealth for global emergencies: implications for coronavirus disease 2019 (COVID-19) J Telemed Telecare. 2020 doi: 10.1177/1357633X20916567. 1357633X20916567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kouroubali A., Kondylakis H., Kavlentakis G., Logothetides F., Stathiakis N., Petrakis Y., et al. An eHealth platform for the holistic management of COVID-19. Stud Health Technol Inform. 2020;273:182–188. doi: 10.3233/SHTI200636. [DOI] [PubMed] [Google Scholar]
- 9.Martel D., Lauzé M., Agnoux A., de Laclos L.F., Daoust R., Émond M., et al. Comparing the effects of a home-based exercise program using a gerontechnology to a community-based group exercise program on functional capacities in older adults after a minor injury. Exp Gerontol. 2018;108:41–47. doi: 10.1016/j.exger.2018.03.016. [DOI] [PubMed] [Google Scholar]
- 10.Trzebiński J., Cabański M., Czarnecka J.Z. Reaction to the COVID-19 pandemic: the influence of meaning in life, life satisfaction, and assumptions on world orderliness and positivity. J Loss Trauma. 2020:1–14. doi: 10.1080/15325024.2020.1765098. [DOI] [Google Scholar]
- 11.Lindeman D. Center for Technology and Aging; Oakland, CA: 2011. mHealth Technologies: applications to benefit older adults. Ed; 2015. [Google Scholar]
- 12.Mirza F., Norris T. Opportunities and barriers for mobile health in New Zealand. Stud Health Technol Inform. 2007;129(1):102. [PubMed] [Google Scholar]
- 13.Kay M., Santos J., Takane M. mHealth: new horizons for health through mobile technologies. World Health Organ. 2011;64(7):66–71. [Google Scholar]
- 14.Zhang H., Cocosila M., Archer N. Factors of adoption of mobile information technology by homecare nurses: a technology acceptance model 2 approach. CIN. 2010;28(1):49–56. doi: 10.1097/NCN.0b013e3181c0474a. [DOI] [PubMed] [Google Scholar]
- 15.Donaghy E., Atherton H., Hammersley V., McNeilly H., Bikker A., Robbins L., et al. Acceptability, benefits, and challenges of video consulting: a qualitative study in primary care. Br J Gen Pract. 2019;69(686):e586–ee94. doi: 10.3399/bjgp19X704141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Frost R., Nimmons D., Davies N. Using remote interventions in promoting the health of frail older persons following the COVID-19 lockdown: challenges and solutions. J Am Med Dir Assoc. 2020;21(7):992–993. doi: 10.1016/j.jamda.2020.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Czaja S.J. Long-term care services and support systems for older adults: the role of technology. Am Psychol. 2016;71(4):294. doi: 10.1037/a0040258. [DOI] [PubMed] [Google Scholar]
- 18.McMurtrey M.E., Zeltmann S.M., Downey J.P., McGaughey R.E. Seniors and technology: results from a field study. J Comput Inf Syst. 2011;51(4):22–30. [Google Scholar]
- 19.Karim H., Choobineh H., Kheradbin N., Ravandi M.H., Naserpor A., Safdari R. Mobile health applications for improving the sexual health outcomes among adults with chronic diseases: a systematic review. Digit Health. 2020;6 doi: 10.1177/2055207620906956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Meinert E., Milne-Ives M., Surodina S., Lam C. Agile requirements engineering and software planning for a digital health platform to engage the effects of isolation caused by social distancing: case study. JMIR Public Health Surveill. 2020;6(2):e19297. doi: 10.2196/19297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jaana M., Paré G. Mobile health technologies use for self-tracking: a survey comparing seniors to the general adult population in Canada. JMIR Mhealth Uhealth. 2020 doi: 10.2196/24718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Padala K.P., Wilson K.B., Gauss C.H., Stovall J.D., Padala P.R. VA Video connect for clinical care in older adults in a rural state during the COVID-19 pandemic: cross-sectional study. J Med Internet Res. 2020;22(9):e21561. doi: 10.2196/21561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.van Dyck L.I., Wilkins K.M., Ouellet J., Ouellet G.M., Conroy M.L. Combating heightened social isolation of nursing home elders: the telephone outreach in the COVID-19 outbreak program. Am J Geriatr Psychiatry. 2020 doi: 10.1016/j.jagp.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang J., Katz I., Li J., Wu Q., Dai C. Mobile digital divide and older people’s access to ‘Internet plus social work’: implications from the COVID-19 help-seeking cases. Asia Pac J Soc Work Dev. 2021;31(1–2):52–58. doi: 10.1080/02185385.2020.1850332. [DOI] [Google Scholar]
- 25.Van Dijk S., Bouman R., Folmer E., den Held R., Warringa J., Marijnissen R., et al. (Vi)-rushed into online group schema-therapy based day-treatment for older adults by the COVID-19 outbreak in the Netherlands. Am J Geriatr Psychiatry. 2020 doi: 10.1016/j.jagp.2020.05.028. 10.1016/j.jagp.2020.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rodenstein M.S., Merchant T.S., Pendergrast T.R., Lindquist L.A. Reducing social isolation of seniors during COVID-19 through medical student telephone contact. J Am Med Dir Assoc. 2020;21(7):948–950. doi: 10.1016/j.jamda.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Von Humboldt S., Mendoza-Ruvalcaba N.M., Arias-Merino E.D., Costa A., Cabras E., Low G., et al. Smart technology and the meaning in life of older adults during the Covid-19 public health emergency period: a cross-cultural qualitative study. Int Rev Psychiatry. 2020:1–10. doi: 10.1080/09540261.2020.1810643. [DOI] [PubMed] [Google Scholar]
- 28.Echeverría P., Bergas M.A.M., Puig J., Isnard M., Massot M., Vedia C., et al. COVIDApp as an innovative strategy for the management and follow-up of COVID-19 cases in long-term care facilities in Catalonia: implementation study. JMIR Public Health Surveill. 2020;6(3):e21163. doi: 10.2196/21163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McLellan L.J., Morelli M., Simeone E., Khazova M., Ibbotson S.H., SmartPDT® E.E. Smartphone enabled real-time dosimetry via satellite observation for daylight photodynamic therapy. Photodiagn Photodyn Ther. 2020;31 doi: 10.1016/j.pdpdt.2020.101914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Armitage R., Nellums L.B. COVID-19 and the consequences of isolating the elderly. Lancet Public Health. 2020;5(5):e256. doi: 10.1016/S2468-2667(20)30061-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cudjoe T.K., Kotwal A.A. Social Distancing” amid a crisis in social isolation and loneliness. J Am Geriatr Soc. 2020 doi: 10.1111/jgs.16527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Santini Z.I., Jose P.E., Cornwell E.Y., Koyanagi A., Nielsen L., Hinrichsen C., et al. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): a longitudinal mediation analysis. Lancet Public Health. 2020;5(1):e62–70. doi:10.1016/S2468-2667(19)30230-0. [DOI] [PubMed]
- 33.Sacco G., Lléonart S., Simon R., Noublanche F., Annweiler C., Group T.S. Communication technology preferences of hospitalized and institutionalized frail older adults during COVID-19 confinement: cross-sectional survey study. JMIR Mhealth Uhealth. 2020;8(9):e21845. doi: 10.2196/21845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Singh J. Critical appraisal skills programme. J Pharmacol Pharmacotherap. 2013;4(1):76. doi: 10.4103/0976-500X.107697. [DOI] [Google Scholar]
- 35.Monaghesh E., Hajizadeh A. The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC Public Health. 2020;20(1):1–9. doi: 10.1186/s12889-020-09301-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hajizadeh A., Monaghesh E. Telehealth services support community during the COVID-19 outbreak in Iran: activities of Ministry of Health and Medical Education. Inform Med Unlocked. 2021;24 doi: 10.1016/j.imu.2021.100567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kondylakis H., Haridimos D., Kouroubali D., Logothetidis A., Triantafyllidis F., Kalamaras A. COVID-19 mobile apps: a systematic review of the literature. J Med Internet Res. 2020;22(12):e23170. doi: 10.2196/23170. [DOI] [PMC free article] [PubMed] [Google Scholar]