Dear Editor,
Since its outbreak in December 2019, corona virus disease 2019 (COVID-19) has been a challenge for the World including India, especially during its second wave. The chaotic and often tragic situation, especially during May 2021, can be attributed to a combination of various factors, including the significant population burden, low doctor-to-population ratio, and inadequate health infrastructure to cope up with a huge burden of infection. Adding to these challenges is the spread of misinformation such as ill-advised medication—via social media networks. The prescription for the treatment of COVID-19 in India typically contains a cocktail of medicines, including azithromycin, doxycycline, ivermectin, and hydroxychloroquine [1]. Consequently, we experienced four cases of doxycycline-induced pill esophagitis during May 2021, which we saw rather sparingly earlier.
Medication-induced esophageal injury is also known as pill esophagitis. The disruption of the esophageal mucosa occurs due to direct localized toxicity, generally caustic (acidic or alkaline) or hyperosmolar. Tetracyclines are the antibiotics that commonly cause pill esophagitis, with doxycycline being the most frequent [2]. At All India Institute of Medical Sciences (AIIMS), Bhubaneswar, Odisha, the regular outpatient department (OPD) services were closed in May 2021, due to a sudden surge in COVID-19 cases in Odisha and the neighboring states. We served patients through telemedicine facilities and emergency services. The four cases of doxycycline-induced pill esophagitis observed in May 2021 are significantly higher than usual. The departmental records show just one such case in the last 4 years, excluding the said period.
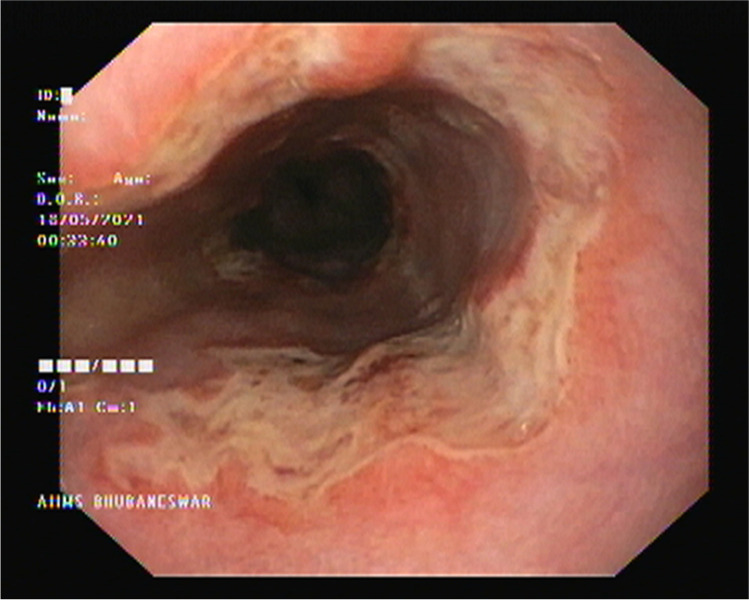
All the four patients, one male and three females, who took doxycycline, presented with sudden onset of odynophagia within 1 to 2 h after taking first dose of doxycycline (100 mg). Interestingly, out of the four, three were apprehensive and took doxycycline as an over-the-counter (OTC) drug as prophylaxis after seeing a prescription revolving around on social media. All of them were well-educated, belonged to the middle-income group, and accessed social media for more than 4 h a day. The fourth patient was COVID-19 positive, and the treating physician prescribed doxycycline to her. Because doxycycline-induced pill esophagitis does not require endoscopy or histology for diagnosis [3], we did not ask two of our patients to visit the hospital. We advised all patients to stop doxycycline and start sucralfate 10 g thrice daily. It was, however, possible for one of the patients residing close to the hospital to have the esophagitis examined endoscopically and histologically. Her esophagogastroduodenoscopy revealed superficial circumferential ulcers at mid and distal esophagus 28 cm and 32 cm from the incisor with the normal intervening area (Fig. 1). All the four patients recovered symptomatically within 5 days of stopping doxycycline and starting sucralfate as assessed through teleconsultation.
Fig. 1.
Esophagogastroduodenoscopy revealed superficial circumferential ulcers at mid and distal esophagus 28 cm and 32 cm from incisor with the normal intervening area
Given the hazards of self-medication as observed above, public awareness needs to be intensified to follow COVID-appropriate behavior and avoiding unnecessary medication based on questionable information. As such, there is no role of doxycycline in COVID-19 management. However, if it is prescribed by a qualified practitioner, it should be appropriately taken, i.e. in an upright posture along with sufficient amount of water (minimum 200 mL). Moreover, one should not lie down immediately after taking the drug. These basic precautions and awareness might go a long way in minimizing morbidity.
Declarations
Consent was obtained from the patients for publication.
Conflict of interest
MKP, HKN, and SCS declare that they have no conflict of interest.
Disclaimer
The authors are solely responsible for the data and the contents of the paper. In no way, the Honorary Editor-in-Chief, Editorial Board Members, the Indian Society of Gastroenterology or the printer/publishers are responsible for the results/findings and content of this article.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bhaumik S, John O, Jha V. Low-value medical care in the pandemic-is this what the doctor ordered? Lancet Glob Health. 2021;9:e1203–4. [DOI] [PMC free article] [PubMed]
- 2.Mason SJ, O’Meara TF. Drug-induced esophagitis. J Clin Gastroenterol. 1981;3:115–20. [DOI] [PubMed]
- 3.Seminerio J, McGrath K, Arnold CA, Voltaggio L, Singhi AD. Medication-associated lesions of the GI tract. Gastrointest Endosc. 2014;79:140–50. [DOI] [PubMed]