Abstract
Objective
The main purpose of the present study was to assess the risk for major revision surgery after perichondrium transplantation (PT) at a minimum of 22 years postoperatively and to evaluate the influence of patient characteristics.
Design
Primary outcome was treatment success or failure. Failure of PT was defined as revision surgery in which the transplant was removed, such as (unicondylar) knee arthroplasty or patellectomy. The functioning of nonfailed patients was evaluated using the International Knee Documentation Committee (IKDC) score. In addition, the influence of patient characteristics was evaluated.
Results
Ninety knees in 88 patients, aged 16 to 55 years with symptomatic cartilage defects, were treated by PT. Eighty knees in 78 patients were eligible for analysis and 10 patients were lost to follow-up. Twenty-eight knees in 26 patients had undergone major revision surgery. Previous surgery and a longer time of symptoms prior to PT were significantly associated with an increased risk for failure of cartilage repair. Functioning of the remaining 52 patients and influence of patient characteristics was analyzed using their IKDC score. Their median IKDC score was 39.08, but a relatively young age at transplantation was associated with a higher IKDC score.
Conclusions
This 22-year follow-up study of PT, with objective outcome parameters next to patient-reported outcome measurements in a unique group of patients, shows that overall 66% was without major revision surgery and patient characteristics also influence long-term outcome of cartilage repair surgery.
Keywords: articular cartilage, cartilage repair, knee, cartilage transplantation
Introduction
Articular cartilage is a specialized connective tissue that provides a low-friction surface in joints, enabling human movement. 1 However, when damaged, articular cartilage has poor regenerative capacity. When left untreated, cartilage defects eventually catabolically predispose the affected joint for the development of osteoarthritis (OA).2,3 To be able to treat such cartilage defects, several different articular cartilage repair strategies like microfracture, osteochondral allograft transplantation, mosaicplasty, perichondrium transplantation (PT), autologous chondrocyte implantation, and scaffolds have been developed over the past decades.4,5 The aim of these techniques is to form hyaline-like cartilage to create a pain-free functioning of the joint and prevent or postpone the development of OA and subsequent joint replacement.6-9
Various factors are correlated with a positive outcome of cartilage repair surgery. Examples are younger age, short duration of symptoms,10,11 and no history of previous surgery on the knee.12,13 No consensus can be found in the literature on whether the defect location influences outcome, but the occurrence of multiple lesions in one joint is described to impair outcome.10,14 There has been a gain of knowledge over the years on articular cartilage repair strategies and the importance of adequate patient selection to improve surgical outcome. 14 Therefore, several treatment algorithms were developed to aid in patient selection for cartilage repair surgery.15-19 However, these algorithms are mostly based on short- and medium-term clinical outcome of cartilage repair surgeries. To our knowledge, there are no algorithms based on objective outcome parameters such as major revision surgery on the long term.
From 1986 till 1992, 88 patients with symptomatic cartilage defects in 90 knees were treated by PT. 20 After 1-year follow-up Homminga et al. showed that 18 out of 25 patients treated with PT were symptom-free and had resumed their previous work and activities. 21 In 1997, Bouwmeester et al. published the 5-year follow-up results of this study. They described 48 treatment failures, although it should be noted that they applied strict criteria to define a failure: being a reoperation, any change in arthroscopic graft appearance or an Hospital for Special Surgery (HSS) knee score of <75. 20 In 40 out of 88 patients, there was a fair to good outcome of the procedure (HSS knee score above 75 and 85, respectively, combined with a good graft appearance on arthroscopy). 20 Improved short-term results were described in patients with a single defect, without previous debridement operations, a long history of symptoms, age over 40 years, and a grade 2 or worse OA. 20 A follow-up study was published in 1999, which presented the histological and biochemical results of these transplants. 22 Because the overall results were found unsatisfactory, PT was only sporadically performed after its introduction. However, the PT-treated patient group is unique because of the 22-year follow-up period, enabling us to analyze the outcome based not only on patient reported outcome measurements but also on objective parameters, such as revision surgery, over time. The aim of this study was to chart the long-term clinical outcome after 22 years of follow-up after PT and to examine whether patient selection also influences objective outcome parameters such as major revision surgery next to patient-reported outcome measurements in this type of cartilage repair surgery.
Methods
Perichondrium Transplantation Operative Technique
Perichondrium transplantation is a single stage open procedure with 2 operation sites. Complete study details and early findings were described by Homminga et al. and Bouwmeester et al. in 1990, 1997, 1999, and 2001.20-23 In short, as described by Bouwmeester et al. in 1997, 20 the procedure starts with debridement of the articular cartilage lesion up to the subchondral bone and a sharp vertical edge will be created on the surrounding cartilage. An oblique incision will be made over the lower part of the left side of the chest. The fascia of the rectus muscle is split transversely and the muscle is split in the line of its fibers. A piece of perichondrium will be dissected from the cartilaginous part of one of the lower ribs and removed together with its chondrogenic layer. The graft will be cut to match the size of the lesion. The perichondrial graft is then placed into the lesion with the chondral side facing up and will be attached with human fibrin glue. 21
Patients
From September 1986 until December 1992, 90 knees with articular cartilage defects in 88 patients were enrolled in the study. Eligible patients included men and women aged 16 to 55 years with symptomatic cartilage defects of the femoral condyles, patella, or trochlea, who were treated by PT. No exclusion criteria other than age >55 years were used for surgery.
Patient information on preoperative and short-term postoperative pain and function was retrieved from previous studies for 88 patients (90 knees). Based on these data, we were able to contact 78 patients (80 knees). Five patients were deceased and 5 patients were unable or unwilling to cooperate. Other than those lost to follow-up (n = 10), no patients were excluded in this long-term study.
Outcome Assessment
Adequately defining the outcome of cartilage repair surgery is hard because no consensus exists on what is successful or nonsuccessful. In previous literature, failure of cartilage repair surgery has been described ranging from no improvement on functional outcome scores to re-intervention in which the graft is removed.24-27
For the present study, 2 different groups were specified. The first group contained the patients who underwent major revision surgery in which the graft was removed and/or arthroplasty was performed. This group that underwent major revision surgery was defined as treatment failure. Shaving of the transplant was not classified as major revision surgery. Patients who underwent major revision surgery were not asked to complete any questionnaires because their results would reflect the effect of the major revision surgery rather than the effect of the PT. The time of the PT and the time of major revision surgery was known and thus the time to failure of the treatment could be calculated. A survival analysis was performed on these data and the influence of patient characteristics on the time to failure was assessed.
Unfortunately, data on preoperative pain and function was incomplete and could not be used reliably for comparison with our long-term follow-up IKDC score. Patient characteristics at time of surgery we assessed that might be of influence were based on available literature and those found by Bouwmeester et al. at 52-month follow-up.10-14,20,25,26 Patient age, sex, number of lesions, lesion size, previous surgery, duration of symptoms, location in the knee, and grade of OA were described. Preoperative degree of OA, location in the knee, and type of previous surgery were not included in the cox and linear regression analyses. Only 6 people had an arthroscopically graded Outerbridge OA score higher than grade 2 in other parts of the knee in this cohort at the time of surgery. Also, group sizes of location in the knee and type of previous surgery were too small for statistical analysis. To identify predictors of outcome, univariate Cox regression was performed on possibly important preoperative factors with the outcome being treatment failure. Parameters with a P value <0.100 were subsequently analyzed in a multivariate Cox regression analysis. Because a maximum of 2.8 (n = 28/10) characteristics may simultaneously be analyzed, an explorative analysis was performed and by stepwise regression excluding the factor with the highest P value until only characteristics with P values <0.05 were present.
The second group contained the patients without revision surgery. They were asked to complete the International Knee Documentation Committee (IKDC) questionnaire. The IKDC questionnaire is best suitable to depict overall functioning for this ageing patient population with a long-term follow-up. 28 These data were analyzed by linear regression in a similar way. Missing data, caused by patients that failed to complete the questionnaire, were calculated and completed by stochastic regression imputation.
Statistical Analysis
Patient characteristics are presented as medians with corresponding interquartile range (IQR) for numerical variables and as number of patients (n and %) for categorical ones. A Kaplan-Meier survival analysis was performed to provide insight in the time to failure for these patients. Hazard ratios (HR) were subsequently calculated using univariate and multivariate Cox regression analysis. Patients who did not undergo major revision surgery were defined as nonfailures and their clinical functioning was evaluated using the IKDC questionnaire. A simple linear regression was calculated to investigate the association between IKDC score and different patient characteristics. All analyses were conducted using a significance level of 0.05. Statistical analysis was performed using IBM SPSS statistics for Mac, version 25.
Results
Patient Characteristics
Eighty knees in 78 patients were eligible for analysis. The median follow-up time of this included cohort was 25 years (IQR 25-26 years) with a minimum of 22 years of follow-up. The median age at time of surgery was 31.5 years (IQR 23-39 years). The median age at follow-up was 56.5 years (IQR 48-64 years). Knee cartilage lesions were located on the medial femoral condyle, lateral femoral condyle, patella, and trochlea. The median lesion size was 3.0 cm2 (IQR 2.0-4.0 cm2). The median time of symptoms before index surgery was 36 months (IQR 24-60 months). Forty-four right and 36 left knees were treated in 47 men and 33 women ( Table 1 ).
Table 1.
Patient Characteristics of the 80 Knees in 78 Patients Included in the Follow-up Cohort a .
| Patient Characteristics | n (%) | Median (IQR) |
|---|---|---|
| Age at surgery (years) | 31.5 (23-39) | |
| Age at follow-up (years) | 56.5 (48-64) | |
| Follow-up time (years) | 25 (25-26) | |
| Age <40 years | 61 (76%) | |
| Age ≥40 years | 19 (24%) | |
| Male knees | 47 (59%) | |
| Female knees | 33 (41%) | |
| Defect size (cm2) | 3.0 (2.0-4.0) | |
| Defect location | ||
| Medial femoral condyle | 26 (32.5%) | |
| Lateral femoral condyle | 2 (2.5%) | |
| Patella/trochlea | 36 (45%) | |
| Multiple | 16 (20%) | |
| Time since onset symptoms (months) | 36 (24-60) | |
| Knee with previous surgery | 61 (76%) | |
| Knee without previous surgery | 19 (24%) | |
| Arthroscopic degree of osteoarthritis at surgery (Outerbridge classification) | ||
| None (grade 0) | 58 (72.5%) | |
| Little (grades 1-2) | 16 (20%) | |
| Definite (grades 3-4) | 6 (7.5%) | |
n = number of knees; IQR = interquartile range.
Values are described as a count and percentage of the total 80 knees or as a median with subsequent interquartile range.
Outcome at 22-Year Follow-up
Twenty-six patients with 28 operated knees (35%) underwent surgery in which the transplant was removed. In 17 patients a total knee arthroplasty was performed, 2 patients underwent a patellofemoral arthroplasty, and 1 patient received a unicondylar arthroplasty. Also 6 patients underwent a patellectomy, which was used more frequently at that time as a salvage procedure. Finally, in 1 patient the transplant was removed. These surgeries were defined as major revision surgery and the treatment was classified as a failure. These failures occurred throughout the follow-up period of the study. A Kaplan-Meier survival analysis revealed that 95.0% was still without major revision surgery at 1 year (SE 2.4%), 83.8% at 10 years (SE 4.1%), and 66.3% at 20 years (SE 5.3%; Fig. 1 ).
Figure 1.
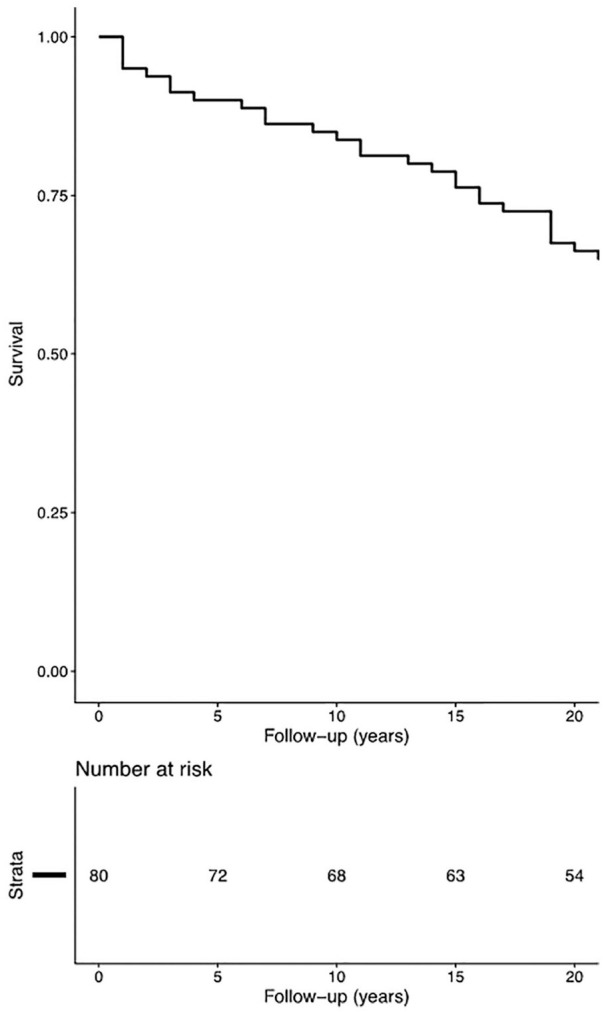
A Kaplan-Meier curve depicting graft survival (i.e., patients with no major revision surgery performed) up until the end of our current follow-up time of at least 22 years.
Influence of Patient Factors on Time-to-Failure of Treatment
A higher percentage (56%) of patients with multiple lesions treatment failed compared to patients with a single lesion (42%), HR 0.471 (0.213-1.043), P = 0.064. Treatment failed in 42% of the female patients and in 30% of the male patients, HR 1.602 (0.763-3.363), P = 0.213. In only 30% of patients younger than 40 years at the moment of primary surgery treatment failed versus 53% of patients older than 40 years at the moment of primary surgery, HR 0.487 (0.225-1.058), P = 0.069. In patients with a lesion size smaller than 3 cm2 33% failed versus 38% in patients with a lesion size greater than 3 cm2, HR 1.166 (0.999-1.361), P = 0.051. In patients without previous surgery only 11% of treatments failed versus 43% in patients with previous surgery, HR 4.894 (1.161-20.642), P = 0.031, and in patients with symptoms shorter than 24 months there were less treatment failures compared to patients with symptoms longer than 24 months (15% vs. 45%, respectively), HR 1.011 (1.004-1.018), P = 0.001 ( Table 2 ). These data was analyzed by univariate Cox regression analysis and subsequently explorative in a multivariate Cox regression analysis for characteristics with a P value <0.100 (duration of symptoms, previous surgery, size of the lesion, age at surgery, and surgery on multiple lesions) with the outcome being treatment failure and subsequent major revision surgery. Definite multivariate Cox regression was carried out with the characteristics “previous surgery” and “time of symptoms.” This definite multivariate Cox regression analysis showed that patients who were without previous knee surgery were significantly less at risk for treatment failure, HR 4.390 (95% confidence interval [CI] 1.036-18.598; P = 0.045). Subsequently, people with a shorter time from onset of symptoms until PT were significantly less at risk for major revision surgery, HR 1.010 (95% CI 1.003-1.017; P = 0.003). No significant differences were found for; size of the lesion, age at surgery, and number of lesions ( Table 2 ).
Table 2.
Overview of the Percentage of Failure of Perichondrium Transplantation in Different Patient Groups a .
| Number of Knees | Fail, n (%) | Univariate |
Multivariate |
|||
|---|---|---|---|---|---|---|
| Hazard Ratio (95% CI) | P Value | Hazard Ratio (95% CI) | P Value | |||
| Total | 80 | 28 (35%) | ||||
| Number of lesions | ||||||
| Single lesion | 64 | 19 (42%) | 0.471 (0.213-1.043) | 0.064 | NA | NA |
| Multiple lesions b | 16 | 9 (56%) | ||||
| Patient age at time of surgery | ||||||
| Age <40 | 61 | 18 (30%) | 0.487 (0.225-1.058) | 0.069 | NA | NA |
| Age ≥40 b | 19 | 10 (53%) | ||||
| Lesion size | ||||||
| Size of the lesion <3 cm2b | 51 | 17 (33%) | ||||
| Size of the lesion ≥3 cm2 | 29 | 11 (38%) | 1.166 (0.999-1.361) | 0.051 | NA | NA |
| Previous surgery | ||||||
| Without previous surgery b | 19 | 2 (11%) | ||||
| With previous surgery | 61 | 26 (43%) | 4.894 (1.161-20.642) | 0.031* | 4.390 (1.036-18.598) | 0.045* |
| Duration of symptoms | ||||||
| Duration of symptoms <24 months b | 27 | 4 (15%) | ||||
| Duration of symptoms ≥24 months | 53 | 24 (45%) | 1.011 (1.004-1.018) | 0.001* | 1.010 (1.003-1.017) | 0.003* |
n = total number; % = percentage of the subgroup that failed; CI = confidence interval; NA = not applicable.
Parameters with a P value <0.100 in univariate Cox regression analysis were subsequently analyzed in an explorative multivariate cox regression analysis (italic text) stepwise excluding characteristics with the highest P value and definite multivariate Cox regression analysis was performed on the characteristics, “previous surgery” and “time of symptoms” (plain text).
Reference group.
Significant influence.
Influence of Patient Factors on Performance of Nonfailed Grafts at 22-Year Follow-up
Fifty-two PT patients (52 knees) were still without major revision surgery after a minimum follow-up of 22 years. To determine their functioning, these remaining patients were analyzed using the IKDC score. Their median IKDC score was 39.08 (IQR 25.57-53.74). Simple linear regression showed a significant relationship between IKDC and age at surgery (P = 0.012). No P values of <0.100 were found for other factors: number of lesions, previous surgery, time of symptoms, and size of the lesion. Therefore, no multivariate testing was performed on these data ( Table 3 ).
Table 3.
Univariate Linear Regression of Preoperative Factors That Possibly Correlate with the IKDC Score at 22 Years of Follow-up.
| B | 95% CI | P Value | |
|---|---|---|---|
| Number of lesions | 8.163 | −8.887 to 25.213 | 0.341 |
| Age at surgery | −0.808 | −1.428 to −0.187 | 0.012* |
| Size of the lesion | −2.496 | −5.674 to 0.682 | 0.121 |
| Previous surgery | −6.238 | −18.632 to 6.156 | 0.317 |
| Time of symptoms | −0.066 | −0.257 to 0.126 | 0.494 |
IKDC = International Knee Documentation Committee; CI = confidence interval.
Significant correlation.
Discussion
The most important finding of this study was that after 22 years of follow-up of cartilage repair surgery in the knee by PT, 66% was still without major revision surgery. Duration of symptoms prior to surgery and previous surgery of the knee are predictors for undergoing major revision surgery and a younger age at primary cartilage repair surgery is associated with a better functioning as measured by IKDC. In the current literature, only limited studies are available with a long-term follow-up of cartilage repair surgery of the knee. Consequently, the outcome on the long term is mainly available by extrapolating short-term results,24,29 or in studies with relatively small group sizes.30,31
On a shorter follow-up term, Moradi et al., Krishnan et al., and de Windt et al. reported a higher patient age and a longer time of symptoms prior to cartilage repair surgery as a negative factor for successful outcome.10,11,32 Furthermore, Krishnan et al., Minas et al., and Pestka et al. found previous surgery of the knee as a negative factor for successful outcome.10,12,13 The follow-up time of many studies is too short for patients to reach an objective endpoint that defines treatment failure (i.e., OA, knee arthroplasty); therefore, published results are often based on patient-reported outcome measurements, and this can however lead to different forms of bias. Knee function deteriorates with increasing age and patient-reported outcome measurements, when not corrected for age, and can underestimate the outcome.33,34 Exceptions are the studies of Gobbi et al. who report increased osteoarthritic changes in older patients at 15 years of follow-up and the study of Minas et al., which did include knee arthroplasty, but with a 10-year follow-up period, n = 210, and 20 years, but with little patients left, n = 23.13,30,35 Our survival rate of 84% at 10-year follow-up is lower than the survival rate of 89% found by Gobbi et al. after microfracture. 35 In contrast to this study we did not apply exclusion criteria (e.g., lesion size) other than age >55. The 79% survival rate reported of autologous chondrocyte implantation by Minas et al. is even lower, but this study treated patients with a larger average lesion size. 13 The only comparison at 20-year follow-up can be made with the study of Ogura et al., who reported a survival rate of 63%, which is similar to our survival rate of 66%. 30 Interestingly, this survival is already reported at their 10-year follow-up, but maintained in their 20-year follow-up. In general, our study has a comparable survival rate and confirms important patient characteristics, but after a longer-term follow-up, in a large patient group and with objective outcome measurements next to patient-reported outcome measurements.
A challenging aspect in cartilage surgery remains to define what treatment failure is. Definitions of failure in the current literature range from total knee arthroplasty or removal of the implant to a lack of improvement on questionnaires or Visual Analog Scales (VAS) for pain. 29 This wide variety of definitions complicates an adequate comparison of different studies and can be a cause of the great differences in described predictors for success.10-14,25-27,36,37 Clinical functioning and quality of life is an important outcome factor, and therefore clinical questionnaires were included. However, with increasing age, knee function decreases. A deterioration of the IKDC score as described by Anderson et al. 38 should therefore not be ignored. This is especially important in studies like this with a very long-term follow-up with an ageing population. 34 Ideally a correction for age like the z-score would be calculated and used for a more valid comparison among individuals, but unfortunately the z-score can only be calculated up to the age of 65. 38 When comparing the individuals younger than 65 in this study, the z-score did not differ between the different age groups 35 to 50 and 51 to 65 (z = −1.5 and −1.3, respectively, P value = 0.27). Thus, in this study, when corrected for age, the IKDC score is not worsened in the older patient age group (51-65) compared to the age group 35 to 50. Furthermore, age was also not found as a confounding factor in the multivariate regression analyses. Still, caution is advised in its interpretation. 34
We conducted a longitudinal cohort study with 22 years of follow-up. However, a limitation of the present study was that some clinical data have been retrieved retrospectively, especially preoperative data and questionnaires were incomplete. Without complete preoperative scores, we considered a comparison with the VAS and HSS Knee Scores at a follow-up of 24 months not reliable and it was not the aim of this article.
Conclusion
We present the long-term survival results of PT. In line with literature presenting mid-term follow-up, a smaller risk of total knee arthroplasty or other major revision surgeries was found in patients with a shorter time of symptoms prior to PT and without previous surgery of the knee. Subsequently a better functional outcome of the knee was found in patients operated at a relatively young age.
Footnotes
Acknowledgments and Funding: We acknowledge the financial support of ReumaNederland (the Dutch Arthritis Foundation) (grant LLP14). We thank Corinne Spooren and Sander van Kuijk for advice on statistical analyses and Liesbeth Jutten for advice and help in performing the data collection.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Emans and TJ Welting are co-founders and shareholders of a start-up company aimed at developing a BMP7 peptide for treatment of OA, PJ Emans is a Consultant for KioMed Pharma and TJ Welting holds 2 patents: WO 2017/178253 A1 and WO 2017/178253 A1. All other authors declare that they have no conflict of interest.
Ethical Approval: This study was approved by the Medical Research Ethics Committee of the Maastricht University Medical Centre+ (METC 13-4-038).
Informed Consent: Renewed informed consent was obtained prior to participation from all patients for this follow-up.
ORCID iD: Maarten P. F. Janssen  https://orcid.org/0000-0002-5134-7368
https://orcid.org/0000-0002-5134-7368
References
- 1. Matsiko A, Levingstone TJ, O’Brien FJ. Advanced strategies for articular cartilage defect repair. Materials (Basel). 2013; 6(2):637-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gelber AC, Hochberg MC, Mead LA, Wang NY, Wigley FM, Klag MJ. Joint injury in young adults and risk for subsequent knee and hip osteoarthritis. Ann Intern Med. 2000; 133(5):321-8. [DOI] [PubMed] [Google Scholar]
- 3. Cicuttini F, Ding C, Wluka A, Davis S, Ebeling PR, Jones G. Association of cartilage defects with loss of knee cartilage in healthy, middle-age adults: a prospective study. Arthritis Rheum. 2005;52(7):2033-9. [DOI] [PubMed] [Google Scholar]
- 4. Alford JW, Cole BJ. Cartilage restoration, part 1: basic science, historical perspective, patient evaluation, and treatment options. Am J Sports Med. 2005;33(2):295-306. [DOI] [PubMed] [Google Scholar]
- 5. Redondo ML, Naveen NB, Liu JN, Tauro TM, Southworth TM, Cole BJ. Preservation of knee articular cartilage. Sports Med Arthrosc Rev. 2018;26(4):e23-e30. [DOI] [PubMed] [Google Scholar]
- 6. Billings E, Jr, von Schroeder HP, Mai MT, Aratow M, Amiel D, Woo SL, et al. Cartilage resurfacing of the rabbit knee. The use of an allogeneic demineralized bone matrix-autogeneic perichondrium composite implant. Acta Orthop Scand. 1990;61(3):201-6. [DOI] [PubMed] [Google Scholar]
- 7. Coutts RD, Woo SL, Amiel D, von Schroeder HP, Kwan MK. Rib perichondrial autografts in full-thickness articular cartilage defects in rabbits. Clin Orthop Relat Res. 1992;(275):263-73. [PubMed] [Google Scholar]
- 8. Engkvist O, Wilander E. Formation of cartilage from rib perichondrium grafted to an articular defect in the femur condyle of the rabbit. Scand J Plast Reconstr Surg. 1979;13(3):371-6. [DOI] [PubMed] [Google Scholar]
- 9. Maruyama Y. An experimental study on cartilage formation in autogenous perichondrial transplantation in rabbits. Keio J Med. 1979;28(2):63-72. [DOI] [PubMed] [Google Scholar]
- 10. Krishnan SP, Skinner JA, Bartlett W, Carrington RW, Flanagan AM, Briggs TW, et al. Who is the ideal candidate for autologous chondrocyte implantation? J Bone Joint Surg Br. 2006;88(1_suppl):61-4. [DOI] [PubMed] [Google Scholar]
- 11. de Windt TS, Bekkers JE, Creemers LB, Dhert WJ, Saris DB. Patient profiling in cartilage regeneration: prognostic factors determining success of treatment for cartilage defects. Am J Sports Med. 2009;37(Suppl 1):58S-62S. [DOI] [PubMed] [Google Scholar]
- 12. Pestka JM, Bode G, Salzmann G, Sudkamp NP, Niemeyer P. Clinical outcome of autologous chondrocyte implantation for failed microfracture treatment of full-thickness cartilage defects of the knee joint. Am J Sports Med. 2012;40(2):325-31. [DOI] [PubMed] [Google Scholar]
- 13. Minas T, Von Keudell A, Bryant T, Gomoll AH. The John Insall Award: a minimum 10-year outcome study of autologous chondrocyte implantation. Clin Orthop Relat Res. 2014;472(1_suppl):41-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. de Windt TS, Concaro S, Lindahl A, Saris DB, Brittberg M. Strategies for patient profiling in articular cartilage repair of the knee: a prospective cohort of patients treated by one experienced cartilage surgeon. Knee Surg Sports Traumatol Arthrosc. 2012;20(11):2225-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Biant LC, McNicholas MJ, Sprowson AP, Spalding T. The surgical management of symptomatic articular cartilage defects of the knee: consensus statements from United Kingdom knee surgeons. Knee. 2015;22(5):446-9. [DOI] [PubMed] [Google Scholar]
- 16. Alford JW, Cole BJ. Cartilage restoration, part 2: techniques, outcomes, and future directions. Am J Sports Med. 2005;33(3):443-60. [DOI] [PubMed] [Google Scholar]
- 17. Cole BJ, Pascual-Garrido C, Grumet RC. Surgical management of articular cartilage defects in the knee. J Bone Joint Surg Am. 2009;91(7):1778-90. [PubMed] [Google Scholar]
- 18. Gomoll AH, Farr J, Gillogly SD, Kercher J, Minas T. Surgical management of articular cartilage defects of the knee. J Bone Joint Surg Am. 2010;92(14):2470-90. [PubMed] [Google Scholar]
- 19. Makris EA, Gomoll AH, Malizos KN, Hu JC, Athanasiou KA. Repair and tissue engineering techniques for articular cartilage. Nat Rev Rheumatol. 2015;11(1_suppl):21-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bouwmeester SJ, Beckers JM, Kuijer R, van der Linden AJ, Bulstra SK. Long-term results of rib perichondrial grafts for repair of cartilage defects in the human knee. Int Orthop. 1997;21(5):313-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Homminga GN, Bulstra SK, Bouwmeester PS, van der Linden AJ. Perichondral grafting for cartilage lesions of the knee. J Bone Joint Surg Br. 1990;72(6):1003-7. [DOI] [PubMed] [Google Scholar]
- 22. Bouwmeester P, Kuijer R, Terwindt-Rouwenhorst E, van der Linden T, Bulstra S. Histological and biochemical evaluation of perichondrial transplants in human articular cartilage defects. J Orthop Res. 1999;17(6):843-9. [DOI] [PubMed] [Google Scholar]
- 23. Bouwmeester PS, Kuijer R, Homminga GN, Bulstra SK, Geesink RG. A retrospective analysis of two independent prospective cartilage repair studies: autogenous perichondrial grafting versus subchondral drilling 10 years post-surgery. J Orthop Res. 2002;20(2):267-73. [DOI] [PubMed] [Google Scholar]
- 24. Nawaz SZ, Bentley G, Briggs TW, Carrington RW, Skinner JA, Gallagher KR, et al. Autologous chondrocyte implantation in the knee: mid-term to long-term results. J Bone Joint Surg Am. 2014;96(10):824-30. [DOI] [PubMed] [Google Scholar]
- 25. Vanlauwe J, Saris DB, Victor J, Almqvist KF, Bellemans J, Luyten FP, TIG/ACT/01/2000 & EXT Study Group. Five-year outcome of characterized chondrocyte implantation versus microfracture for symptomatic cartilage defects of the knee: early treatment matters. Am J Sports Med. 2011;39(12):2566-74. [DOI] [PubMed] [Google Scholar]
- 26. Knutsen G, Drogset JO, Engebretsen L, Grontvedt T, Isaksen V, Ludvigsen TC, et al. A randomized trial comparing autologous chondrocyte implantation with microfracture. Findings at five years. J Bone Joint Surg Am. 2007;89(10):2105-12. [DOI] [PubMed] [Google Scholar]
- 27. Niemeyer P, Porichis S, Steinwachs M, Erggelet C, Kreuz PC, Schmal H, et al. Long-term outcomes after first-generation autologous chondrocyte implantation for cartilage defects of the knee. Am J Sports Med. 2014;42(1_suppl):150-7. [DOI] [PubMed] [Google Scholar]
- 28. Hambly K, Griva K. IKDC or KOOS? Which measures symptoms and disabilities most important to postoperative articular cartilage repair patients? Am J Sports Med. 2008;36(9):1695-704. [DOI] [PubMed] [Google Scholar]
- 29. Mistry H, Connock M, Pink J, Shyangdan D, Clar C, Royle P, et al. Autologous chondrocyte implantation in the knee: systematic review and economic evaluation. Health Technol Assess. 2017;21(6):1-294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ogura T, Mosier BA, Bryant T, Minas T. A 20-year follow-up after first-generation autologous chondrocyte implantation. Am J Sports Med. 2017;45(12):2751-61. [DOI] [PubMed] [Google Scholar]
- 31. Solheim E, Hegna J, Strand T, Harlem T, Inderhaug E. Randomized study of long-term (15-17 years) outcome after microfracture versus mosaicplasty in knee articular cartilage defects. Am J Sports Med. 2018;46(4):826-31. [DOI] [PubMed] [Google Scholar]
- 32. Moradi B, Schonit E, Nierhoff C, Hagmann S, Oberle D, Gotterbarm T, et al. First-generation autologous chondrocyte implantation in patients with cartilage defects of the knee: 7 to 14 years’ clinical and magnetic resonance imaging follow-up evaluation. Arthroscopy. 2012;28(12):1851-61. [DOI] [PubMed] [Google Scholar]
- 33. Rolfson O, Bohm E, Franklin P, Lyman S, Denissen G, Dawson J, et al. Patient-reported outcome measures in arthroplasty registries Report of the Patient-Reported Outcome Measures Working Group of the International Society of Arthroplasty Registries Part II. Recommendations for selection, administration, and analysis. Acta Orthop. 2016;87(Suppl 1):9-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Filardo G, Andriolo L, Sessa A, Vannini F, Ferruzzi A, Marcacci M, et al. Age is not a contraindication for cartilage surgery: a critical analysis of standardized outcomes at long-term follow-up. Am J Sports Med. 2017;45(8):1822-8. [DOI] [PubMed] [Google Scholar]
- 35. Gobbi A, Karnatzikos G, Kumar A. Long-term results after microfracture treatment for full-thickness knee chondral lesions in athletes. Knee Surg Sports Traumatol Arthrosc. 2014;22(9):1986-96. [DOI] [PubMed] [Google Scholar]
- 36. Peterson L, Vasiliadis HS, Brittberg M, Lindahl A. Autologous chondrocyte implantation: a long-term follow-up. Am J Sports Med. 2010;38(6):1117-24. [DOI] [PubMed] [Google Scholar]
- 37. Brittberg M, Recker D, Ilgenfritz J, Saris DBF; SUMMIT Extension Study Group. Matrix-applied characterized autologous cultured chondrocytes versus microfracture: five-year follow-up of a prospective randomized trial. Am J Sports Med. 2018;46(6):1343-51. [DOI] [PubMed] [Google Scholar]
- 38. Anderson AF, Irrgang JJ, Kocher MS, Mann BJ, Harrast JJ; International Knee Documentation Committee. The Inter-national Knee Documentation Committee Subjective Knee Evaluation Form: normative data. Am J Sports Med. 2006;34(1_suppl):128-35. [DOI] [PubMed] [Google Scholar]


