Abstract
A 40-year-old man with history of prior coronavirus disease 2019 (COVID-19) infection developed pleuritic chest pain 3 days after receiving the first dose of the BNT162b2 mRNA vaccine. Echocardiography results were significant for mild dysfunction and left ventricular hypertrophy. Cardiac magnetic resonance imaging showed myocardial edema as well as delayed enhancement in the inferior wall of the basal left ventricular myocardium, suggestive of acute myocarditis. This case describes the work-up, diagnosis, risk-stratification, and management of acute myocarditis post BNT162b2 mRNA vaccine.
<Learning objective:
-
1.
To suspect acute myocardial inflammation in patients who present with chest symptoms after receiving the BNT162b2 COVID-19 vaccine.
-
2.
To review the clinical presentation and laboratory, electrocardiographic, and imaging parameters for diagnosing acute myocarditis.
-
3.
To review the indications for endomyocardial biopsy in patients presenting with possible myocarditis.>
Keywords: Coronavirus 2019, BNT162b2 mRNA vaccine, Myocarditis, Pneumonia
Introduction
The only cardiac adverse events reported in the BNT162b2 mRNA vaccine trials were paroxysmal ventricular arrhythmias [1]. Since April 2021, there have been more than a thousand reports to the Vaccine Adverse Event Reporting System of cases of myocarditis and pericarditis [2]. The confirmed cases have occurred mostly in male young adults and more often after the second dose of the vaccine [2]. Our case is distinct in that our patient developed myocarditis after receiving the first vaccine dose.
Case report
A 40-year-old man presented to the hospital with acute onset pleuritic chest pain and dyspnea 3 days after receiving the first dose of the BNT162b2 mRNA vaccine. Days prior to his presentation, he experienced nausea, myalgia, and subjective fevers. The patient was diagnosed with coronavirus disease 2019 (COVID-19) pneumonia four months earlier when he presented with cough and loss of taste. He did not require hospitalization and fully recovered with only symptomatic treatment after a couple of weeks.
On examination, he was in moderate distress from his chest discomfort. Temperature was 36.9°C, blood pressure 142/84 mmHg, heart rate 107 beats per minute, and oxygen saturation 100% on ambient air. Lungs were clear bilaterally. He had mild jugular venous distension, but no murmurs, rubs, or gallops. Extremities were warm with no peripheral edema.
Besides his recent diagnosis of COVID pneumonia, the patient had no significant past medical history, allergies, or family history of cardiac disease. Medications included testosterone. The patient endorsed occasional marijuana use, but denied alcohol, tobacco, or intravenous drug use. He works as a nursing assistant.
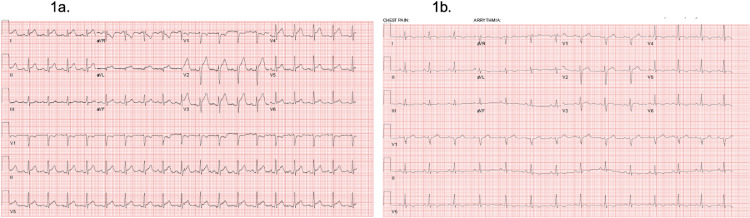
Initial electrocardiogram (ECG) showed normal sinus rhythm with diffuse ST elevations across all leads, except lead III and aVR and V1 where there were ST depressions (Fig. 1a). Chest X-ray showed no evidence of acute cardiopulmonary process. Complete blood count was notable for 15,600 white blood cells per microliter (74% neutrophils, 15.6% lymphocytes, 0.1% eosinophils). Serum creatinine was measured at 1.08 mg/dL, aspartate aminotransferase 66 IU/L, and alanine transaminase 32 IU/L. Initial high sensitivity troponin-I (troponin I-hs) was 8,935 ng/L, and creatinine kinase-MB 26.62 ng/Ml, both peaked 10 hours later at 20301.0 ng/L and 46.65 ng/mL, respectively. Brain natriuretic peptide was 104.6 pg/mL, C-reactive protein 7.6 mg/dL (normal <0.8 mg/dL), and erythrocyte sedimentation rate 19 mm/hour (normal <15 mm/hour). The patient's respiratory viral polymerase-chain reaction panel along with COVID-19 polymerase-chain reaction assay were negative. His anti-severe acute respiratory syndrome coronavirus 2 immunoglobulin G titer was >400 (positive threshold above 15).
Fig. 1.
(a) Electrocardiogram (ECG) at first diagnosis. Normal sinus rhythm with diffuse ST elevations across all leads, except lead III and aVR and V1 where there were ST depressions. (b) Repeat ECG 2 days after admission. Normal sinus rhythm with non-specific T-wave inversions and resolution of diffuse ST elevations.
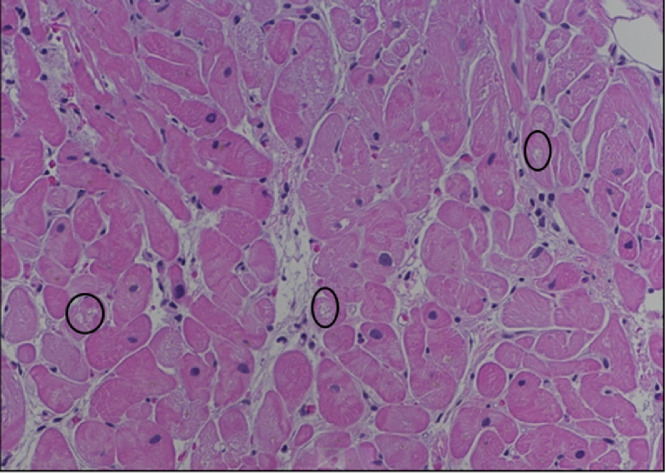
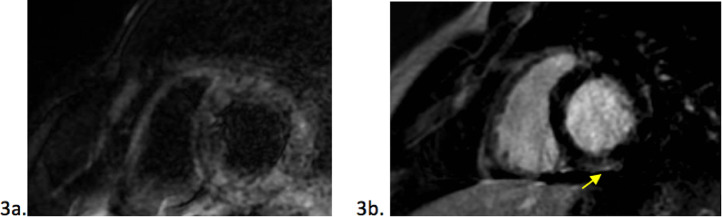
The initial echocardiogram was notable for mild global hypokinesis with an ejection fraction of 47% and a trivial pericardial effusion (Clips 1-3). While his diffuse ST elevations and PR depressions were suggestive of pericarditis, the elevation in cardiac enzymes was disproportionate to what would have been expected in an isolated pericardial process. Right heart catheterization was significant for elevated filling pressures (right atrial pressure was 12 mmHg and pulmonary capillary wedge pressure was 23 mmHg) and a preserved cardiac output and index by thermodilution. Coronary angiography, completed via femoral access without heparin, showed no evidence of coronary artery disease. Because of concern for myocarditis, endomyocardial biopsy was performed and revealed myocyte hypertrophy with rare non-specific myocyte vacuolization, but no evidence of inflammatory cell infiltration (Fig. 2). Electron microscopy, immunohistochemistry, periodic acid-Schiff stain with diastase, trichrome stain, and iron stain demonstrated no significant findings. Cardiac magnetic resonance imaging (MRI) showed left ventricular ejection fraction 52%, and normal regional motion of the ventricles. Myocardial edema and delayed enhancement in the inferior wall of the basal left ventricular myocardium were noted (Fig. 3).
Fig. 2.
Endomyocardial biopsy with no evidence of myocardial inflammation. Non-specific cardiomyocyte vacuolization is demarcated by rings.
Fig. 3.
(a) Cardiac magnetic resonance imaging (MRI) revealing myocardial edema. (b) Cardiac MRI showing delayed enhancement in the basal inferior myocardial wall (yellow arrow).
Clip 1 Echocardiogram on admission (parasternal short view).
Clip 2 Echocardiogram on admission (4-chamber view).
Clip 3 Echocardiogram on admission (2-chamber view).
Clip 4 Echocardiogram on day 4 of admission (parasternal short view).
Clip 5 Echocardiogram on day 4 of admission (4-chamber view).
Clip 6 Echocardiogram on day 4 of admission (2-chamber view).
The patient was admitted to the cardiology service with a diagnosis of acute myocarditis. Due to his elevated filling pressures and rising cardiac markers, the patient was started on intravenous bumetanide and oral prednisone 50 mg daily, which was discontinued after the biopsy results. His volume status improved with resolution of all symptoms including chest pain by day 3 of admission. He had infrequent premature ventricular contractions in the first few days of admission, but no arrhythmias. Repeat ECG 2 days after admission showed normal sinus rhythm with non-specific T-wave inversions and resolution of diffuse ST elevations (Fig. 1b). Repeat echocardiography on day of discharge (4 days after admission) showed improvement in left ventricular ejection fraction to 70% (Clips 4-6).
Four weeks after hospital discharge, the patient was seen for follow-up and was able to perform his job as a nursing assistant, but reported occasional pleuritic, left-sided discomfort. Troponin-I-hs was not elevated and repeat electrocardiogram had no acute ST segment changes. The patient was started on ibuprofen and colchicine at that visit and endorsed full relief of symptoms after 3 weeks. Exercise clearance is pending assessment of his functional capacity, symptoms and potential arrhythmias during an exercise stress test at 6 months [3].
Discussion
This case presents a patient who experienced myocardial injury after the first dose of the BNT162b2 mRNA vaccine. The elevated cardiac enzymes coupled with ventricular dysfunction, edema, and late gadolinium enhancement on cardiac MRI were diagnostic for myocarditis. Acute coronary syndrome was considered but ruled out with coronary angiography. Community acquired pneumonia was also on the differential diagnosis but the patient's chest X-ray did not demonstrate any acute pulmonary process.
In suspected myocarditis, in addition to obtaining an ECG, laboratory results, and imaging, endomyocardial biopsy should be performed when there is: 1) a suspicion for myocarditis, cardiogenic shock, or acute heart failure with ventricular dysfunction, or 2) if myocarditis is diagnosed and significant coronary disease has been ruled out [4]. In this case, histology was negative for lymphocytic infiltration, but did show rare cardiomyocyte vacuolization, a non-specific indicator of cardiomyocyte injury that has been reported in COVID-19 myocarditis [5].
Myocarditis has been reported as a complication of the BNT162b2 mRNA vaccine in the recent literature. The exact pathophysiology remains unknown, but potential etiologies include molecular mimicry between the spike protein of severe acute respiratory syndrome and self-antigens, preexisting dysregulated immune pathways, an exaggerated immune response to mRNA, and defects in cytokine expression [6]. Most cases of myocarditis occur in males around the age of 19 years with a median interval from vaccination to symptom onset of 2 days according to the US Centers for Disease Control [7]. Our report is unique in that our patient is approximately 20 years older than most patients who develop myocarditis post BNT162b2 mRNA vaccine. Thus far, only a few reports review and analyze findings from different diagnostic modalities, such as cardiac biomarkers, ECG, viral pathology panels, echocardiography, and cardiac MRI [8,9]. In our report, we aimed to conduct a comprehensive review of data from the aforementioned modalities. We have several notable findings that should be highlighted: 1) myocyte hypertrophy with rare non-specific myocyte vacuolization, but no evidence of inflammatory cell infiltration on endomyocardial biopsy; 2) myocardial edema and delayed enhancement in the inferior wall of the basal left ventricular myocardium on cardiac MRI; 3) prompt recovery of left ventricular systolic function based on serial echocardiograms.
As the BNT162b2 COVID-19 vaccine becomes more widely used, close monitoring for cardiac injury is recommended, particularly in patients with previous history of COVID-19. Based on this case and other case reports, COVID vaccine-related myocarditis appears to follow a non-fulminant course and conservative management may be all that is warranted.
Declaration of Competing Interest
The authors have no conflicts of interest to disclose.
Acknowledgments
None.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jccase.2021.12.009.
Appendix. Supplementary materials
References
- 1.Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, Perez JL, Pérez Marc G, Moreira ED, Zerbini C, Bailey R, Swanson KA, Roychoudhury S, Koury K, Li P, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020;383:2603–2615. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Myocarditis and pericarditis after mRNA COVID-19 vaccination. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/safety/myocarditis.html.
- 3.Pelliccia A, Solberg EE, Papadakis M, Adami PE, Biffi A, Caselli S, La Gerche A, Niebauer J, Pressler A, Schmied CM, Serratosa L, Halle M, Van Buuren F, Borjesson M, Carrè F, et al. Recommendations for participation in competitive and leisure time sport in athletes with cardiomyopathies, myocarditis, and pericarditis: Position statement of the Sport Cardiology Section of the European Association of Preventive Cardiology (EAPC) Eur Heart J. 2019;40:19–33. doi: 10.1093/eurheartj/ehy730. [DOI] [PubMed] [Google Scholar]
- 4.Kociol RD, Cooper LT, Fang JC, Moslehi JJ, Pang PS, Sabe MA, Shah RV, Sims DB, Thiene G, Vardeny O. Recognition and initial management of fulminant myocarditis: A scientific statement from the American Heart Association. Circulation. 2020;141:E69–E92. doi: 10.1161/CIR.0000000000000745. [DOI] [PubMed] [Google Scholar]
- 5.Bailey AL, Dmytrenko O, Greenberg L, Bredemeyer AL, Ma P, Liu J, Penna V, Lai L, Winkler ES, Sviben S, Brooks E, Nair AP, Heck KA, Rali AS, Simpson L, et al. SARS-CoV-2 infects human engineered heart tissues and models COVID-19 myocarditis. BioRxiv Prepr Serv Biol. 2020 doi: 10.1016/j.jacbts.2021.01.002. 2020 Nov 5:2020.11.04.364315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bozkurt B, Kamat I, Hotez PJ. Myocarditis with COVID-19 mRNA vaccines. Circulation. 2021;144:471–484. doi: 10.1161/CIRCULATIONAHA.121.056135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gargano JW. Use of mRNA COVID-19 vaccine after reports of myocarditis among vaccine recipients: Update from the Advisory Committee on Immunization Practices — United States, June 2021. MMWR Morb Mortal Wkly Rep. 2021;70:977–982. doi: 10.15585/mmwr.mm7027e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sulemankhil I, Abdelrahman M, Negi SI. Temporal association between the COVID-19 Ad26.COV2.S vaccine and acute myocarditis: A case report and literature review. Cardiovasc Revasc Med. 2021 doi: 10.1016/j.carrev.2021.08.012. Aug 16:S1553-8389(21)00578-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Montgomery J, Ryan M, Engler R, Hoffman D, McClenathan B, Collins L, Loran D, Hrncir D, Herring K, Platzer M, Adams N, Sanou A, Cooper LT., Jr. Myocarditis Following Immunization With mRNA COVID-19 Vaccines in Members of the US Military. JAMA Cardiol. 2021;6(10):1202–1206. doi: 10.1001/jamacardio.2021.2833. Oct 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.