Osteonecrosis of the jaw, a rare disease, includes medication-related osteonecrosis of the jaw (MRONJ), which is caused by long-term use of drugs that inhibit bone resorption. The risk factors for MRONJ include surgical invasion such as tooth extraction;1 however, the relationship between MRONJ and implant treatment remains unclear.2 In particular, there are few reports on the pathogenesis of peri-implant MRONJ under stable function.3 In this study, we presented a case of peri-implantitis-induced MRONJ in an 82-year-old man who began taking bisphosphonate (BP) and denosumab (Dmab) during long-term stabilization after implant placement. We also discussed some pathogenic factors for peri-implantitis-induced MRONJ.
A 73-year-old male patient was referred to our hospital in 2010 with a chief complaint of discomfort on the left side of the mandible. The patient was a non-smoker with a history of hypertension. Tooth #36 had chronic apical periodontitis and furcation involvement, and was extracted after being diagnosed as hopeless. After the extraction socket healed, implant surgery was performed in a two-stage approach under local anesthesia according to the manufacturer's recommended protocol (Replace® Groovy Tapered WP, 10 mm, Nobel Biocare, Zürich, Switzerland) (Fig. 1A). In 2011, a maintenance program was started, focusing on professional mechanical tooth cleaning at 3-month intervals.
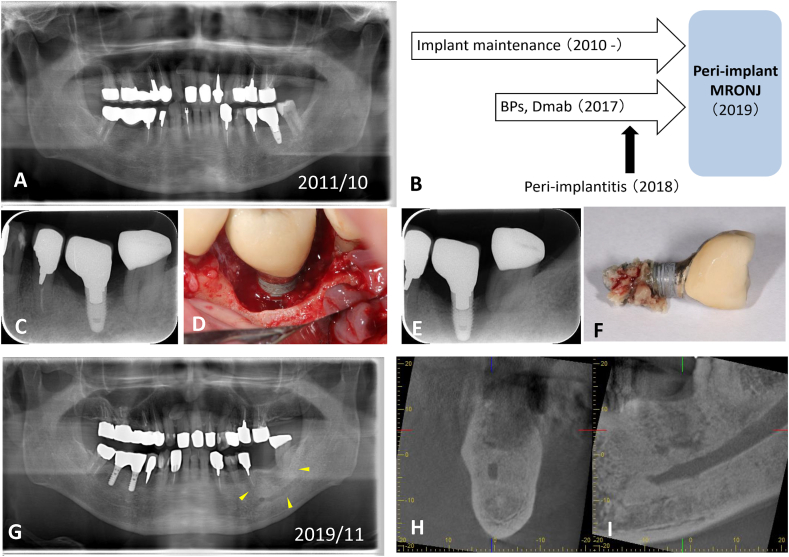
Figure 1.
Radiographic and clinical photographs of our patient with peri-implantitis-induced medication-related osteonecrosis of the jaw (MRONJ). (A) Panoramic radiographs at the start of prosthetic rehabilitation (October 2011). (B) Timeline to the onset of MRONJ. (C) Periapical radiograph of #36 peri-implantitis (2018). (D) Clinical photograph taken during surgical treatment of peri-implantitis. (E) Periapical radiograph of #36 peri-implant MRONJ (2019). (F) Necrotic bone tissue irregularly adhering to the rough surface of the implant, accompanied by a putrid odor. (G) Panoramic radiographs at follow-up showing chronic mandibular osteomyelitis (arrowhead, November 2019). (H) Dental cone-beam computed tomography findings. No sequestrum separation was found (coronal plane). (I) Marked osteosclerosis was observed around the #36 area (sagittal plane).
Within this period, the patient was diagnosed as having osteoporosis in 2017 and was treated with drugs to inhibit bone resorption starting at the age of 80 years. The patient began with the oral BP minodronic acid hydrate (Ricalbon® tablets 50 mg 2 times/day), and then switched to injectable Dmab (Pralia® subcutaneous injection 60 mg once/6 months, RANKL inhibitor), 2 years later (Fig. 1B).
In 2018, peri-implantitis developed around the #36 implant, and the area was surgically decontaminated with debridement and air abrasion, with a good postoperative outcome (Fig. 1C and D).
However, the following year, in June 2019, the implant became mobile and marked swelling of the peri-implant mucosa was observed. On the basis of the radiological findings, MRONJ (stage 2) subsequent to peri-implantitis was diagnosed (Fig. 1E).
The implant body was removed under local anesthesia, and the site was carefully washed with physiological saline solution (Fig. 1F). The postoperative course was good, and the defect was restored with a removable partial denture (Fig. 1G, H and I).
As a related factor associated with the development of MRONJ, the minodronate used in this case is a third-generation BP, which is highly active and has a strong inhibitory effect on bone resorption.4 However, Dmab reduces the risk of spine and hip fractures in osteoporotic patients and is administered only as a subcutaneous injection every 6 months.5
In this case, in addition to the possibility that these cumulative doses affected the bone tissue, we speculate that peri-implantitis was a risk modifier that triggered the development of MRONJ. In an aging society, medication status often changes, and even stabilized implants need to be carefully managed. Attentive maintenance is required, and the risk of developing MRONJ around implants should be recognized.
Declaration of competing interest
The authors declare no conflicts of interest relevant to this article.
References
- 1.Ruggiero S.L., Dodson T.B., Fantasia J., et al. American Association of Oral and Maxillofacial Surgeons. American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw – 2014 update. J Oral Maxillofac Surg. 2014;72:1938–1956. doi: 10.1016/j.joms.2014.04.031. [DOI] [PubMed] [Google Scholar]
- 2.Sher J., Kirkham-Ali K., Luo J.D., Miller C., Sharma D. Dental implant placement in patients with a history of medications related to osteonecrosis of the jaws: a systematic review. J Oral Implantol. 2021;47:249–268. doi: 10.1563/aaid-joi-D-19-00351. [DOI] [PubMed] [Google Scholar]
- 3.Seki K., Namaki S., Kamimoto A., Hagiwara Y. Medication-related osteonecrosis of the jaw subsequent to periimplantitis: a case report and literature review. J Oral Implantol. 2020 doi: 10.1563/aaid-joi-D-19-00385. https://doi:10.1563/aaid-joi-D-19-00385 [DOI] [PubMed] [Google Scholar]
- 4.Shibahara T., Morikawa T., Yago K., Kishimoto H., Imai Y., Kurita K. National survey on bisphosphonate-related osteonecrosis of the jaws in Japan. J Oral Maxillofac Surg. 2018;76:2015–2112. doi: 10.1016/j.joms.2018.04.009. [DOI] [PubMed] [Google Scholar]
- 5.Cummings S.R., San Martin J., McClung M.R., et al. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med. 2009;361:756–765. doi: 10.1056/NEJMoa0809493. [DOI] [PubMed] [Google Scholar]