Key Points
Question
Can a 5-day regimen of postoperative, prophylactic, intravenous antibiotics reduce the rate of surgical site infections in patients with a lower extremity bone tumor undergoing complex endoprosthetic reconstruction compared with a 1-day regimen?
Findings
In this randomized clinical trial including 604 patients in the primary analysis, the 5-day regimen did not reduce the rate of surgical site infection compared with the 1-day regimen, although it resulted in a higher rate of antibiotic-related complications, notably Clostridioides difficile–associated colitis.
Meaning
The results of this study suggest that prolonging use of postoperative antibiotics beyond 1 day does not reduce the rate of surgical site infection but increases the risk of clinically significant antibiotic-related complications.
Abstract
Importance
The use of perioperative, prophylactic, intravenous antibiotics is standard practice to reduce the risk of surgical site infection after oncologic resection and complex endoprosthetic reconstruction for lower extremity bone tumors. However, evidence guiding the duration of prophylactic treatment remains limited.
Objective
To assess the effect of a 5-day regimen of postoperative, prophylactic, intravenous antibiotics compared with a 1-day regimen on the rate of surgical site infections within 1 year after surgery.
Design, Setting, and Participants
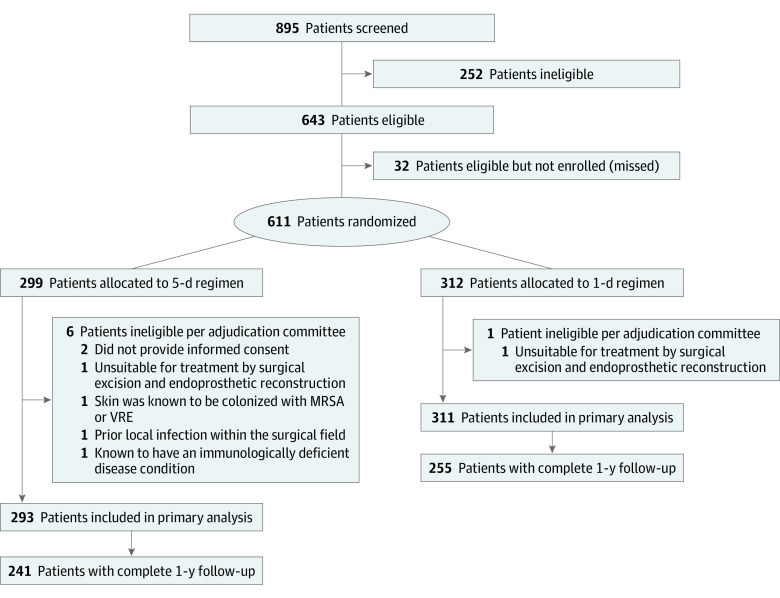
This randomized clinical superiority trial was performed at 48 clinical sites in 12 countries from January 1, 2013, to October 29, 2019. The trial included patients with a primary bone tumor or a soft tissue sarcoma that had invaded the femur or tibia or oligometastatic bone disease of the femur or tibia with expected survival of at least 1 year who required surgical management by excision and endoprosthetic reconstruction. A total of 611 patients were enrolled, and 7 were excluded for ineligibility.
Interventions
A 1- or 5-day regimen of postoperative prophylactic intravenous cephalosporin (cefazolin or cefuroxime) that began within 8 hours after skin closure and was administered every 8 hours thereafter. Those randomized to the 1-day regimen received identical saline doses every 8 hours for the remaining 4 days; patients, care providers, and outcomes assessors were blinded to treatment regimen.
Main Outcomes and Measures
The primary outcome in this superiority trial was a surgical site infection (superficial incisional, deep incisional, or organ space) classified according to the criteria established by the Centers for Disease Control and Prevention within 1 year after surgery. Secondary outcomes included antibiotic-related complications, unplanned additional operations, oncologic and functional outcomes, and mortality.
Results
Of the 604 patients included in the final analysis (mean [SD] age, 41.2 [21.9] years; 361 [59.8%] male; 114 [18.9%] Asian, 43 [7.1%] Black, 34 [5.6%] Hispanic, 15 [2.5%] Indigenous, 384 [63.8%] White, and 12 [2.0%] other), 293 were randomized to a 5-day regimen and 311 to a 1-day regimen. A surgical site infection occurred in 44 patients (15.0%) allocated to the 5-day regimen and in 52 patients (16.7%) allocated to the 1-day regimen (hazard ratio, 0.93; 95% CI, 0.62-1.40; P = .73). Antibiotic-related complications occurred in 15 patients (5.1%) in the 5-day regimen and in 5 patients (1.6%) allocated to the 1-day regimen (hazard ratio, 3.24; 95% CI, 1.17-8.98; P = .02). Other secondary outcomes did not differ significantly between treatment groups.
Conclusions and Relevance
This randomized clinical trial did not confirm the superiority of a 5-day regimen of postoperative intravenous antibiotics over a 1-day regimen in preventing surgical site infections after surgery for lower extremity bone tumors that required an endoprosthesis. The 5-day regimen group had significantly more antibiotic-related complications.
Trial Registration
ClinicalTrials.gov Identifier: NCT01479283
This randomized clinical trial of patients with a primary bone tumor or a soft tissue sarcoma compares the effects of a 5-day vs 1-day regimen of postoperative, prophylactic, intravenous antibiotics on surgical site infections within 1 year after surgery.
Introduction
Operations to remove malignant tumors of the femur or tibia involve the resection of the affected bone and surrounding soft tissue followed by complex reconstruction of the limb. The most common reconstruction involves the use of modular metallic and polyethylene endoprostheses to replace surgically resected bones and joints. Because of the length and intricacies of these procedures and the medical complexity of these patients, the risk of a surgical site infection is high.1,2,3 Attempts to eradicate the organism often fail and result in the eventual need for amputation in nearly 50% of patients, thereby strongly affecting patient function and quality of life and delaying the administration of adjuvant cancer therapies.1,2,3,4
Strategies to minimize surgical site infections in this population include the administration of perioperative intravenous antibiotics. The most effective antibiotic regimen to prevent surgical site infections remains uncertain and current clinical practice is highly varied, particularly with respect to antibiotic duration. Approximately 2 of every 3 surgeons prescribe prolonged courses well beyond the 24-hour recommended duration for standard total joint replacement operations.5,6,7,8 However, overuse of antibiotics can lead to antibiotic-related complications and antibiotic resistance; antibiotic stewardship, therefore, remains a salient issue.9 We conducted the Prophylactic Antibiotic Regimens in Tumor Surgery (PARITY) trial to inform the effect of a 5-day regimen of postoperative, prophylactic, intravenous antibiotics compared with a 1-day regimen on the prevention of surgical site infections and on antibiotic adverse effects in patients requiring surgical resection and endoprosthetic reconstruction for a lower extremity bone tumor.
Methods
Trial Design and Oversight
This intention-to-treat study was an investigator-initiated, international, blinded (patients, surgeons, outcomes assessors, and data analysts), parallel, superiority randomized clinical trial. The rationale, design, and methods of the trial have been previously published.10 Written informed consent was required to participate in the study, and all data were deidentified. Supplement 1 (the Trial Protocol) and Supplement 2 provide information on eligibility criteria, interventions, blinding, follow-up, outcomes definitions, and statistical analysis. The Hamilton Integrated Research Ethics Board as well as the relevant local ethics committee at each participating site approved the trial protocol and its amendments before local study initiation. In addition, the following regulatory bodies also approved the trial protocol and its amendments: Health Canada, the Brazilian National Health Surveillance Agency, the European Medicines Agency (including the competent authorities in Austria and Spain), the Indian Council of Medical Research, and the Republic of South Africa’s Department of Health. The PARITY Data and Safety Monitoring Board, composed of 2 orthopedic oncologists and 1 statistician who were independent of the study team, reviewed the trial outcomes. This study followed the Consolidated Standards of Reporting Trials (CONSORT) reporting guideline.
Patients
From January 1, 2013, to October 29, 2019, investigators at 48 clinical sites across Canada, the US, Argentina, Australia, Austria, Brazil, Egypt, India, the Netherlands, Singapore, South Africa, and Spain recruited patients for the study. Eligible patients included all individuals 12 years or older with a primary bone tumor or a soft tissue sarcoma that had invaded the femur or tibia or oligometastatic bone disease of the femur or tibia with expected survival of at least 1 year who required surgical management by excision and endoprosthetic reconstruction. Patients with previous infections at the surgical site or who were known to be colonized with methicillin-resistant Staphylococcus aureus or vancomycin-resistant Enterococcus were excluded. A total of 895 patients were screened for eligibility, and 7 patients were adjudicated to be ineligible at the time of randomization; thus, of the 611 patients randomized, 604 were included in the final analyses. The final 1-year assessments were completed in March 2021. Details on the eligibility criteria are available in the eAppendix in Supplement 2.
Trial Interventions and Procedures
Surgical procedures were performed according to the standard practices at each clinical site. All patients received standardized preoperative and intraoperative prophylactic intravenous antibiotics. Patients were randomly allocated perioperatively in a 1-to-1 ratio to receive a 1- or 5-day postoperative prophylactic regimen of an intravenous cephalosporin (cefazolin or cefuroxime); they were blinded to the treatment regimen. Those randomized to the 1-day regimen received identical saline (placebo) doses for the remaining 4 days. Randomization, stratified according to tumor location (femur or tibia) and clinical site, was centralized through an internet-based, computer-generated platform that concealed allocation and used randomly permuted blocks of 2 or 4. An unblinded member of the local investigational pharmacy performed the randomization. Patients began their randomly allocated, postoperative, prophylactic antibiotic regimen within 8 hours after skin closure, and the doses were intravenously administered every 8 hours. Clinical sites used their own inventory to prepare the study antibiotics or placebo. Preparation, blinding of study antibiotics or placebo, and storage and administration of the study antibiotics were conducted as per local procedures established at each clinical site and the relevant manufacturers’ labels. Further details on the intravenous antibiotic regimens are available in the eAppendix in Supplement 2.
Outcome Measures
The primary outcome was the development of a surgical site infection (superficial incisional, deep incisional, or organ space [deep prosthetic infection]) within 1 year of the date of surgery. Surgical site infections were classified according to the criteria established by the Centers for Disease Control and Prevention.11 Secondary outcomes included antibiotic-related complications, unplanned additional operations, death, and oncologic and functional outcomes within 1 year after surgical resection and endoprosthetic reconstruction. Validated functional assessments included the Musculoskeletal Tumor Society 1987 (MSTS-87) (range, 0-35, with higher scores indicating better function) and 1993 (MSTS-93) (range, 0-100, with higher scores indicating better function) scores and the Toronto Extremity Salvage Score (TESS) (range, 0-100, with higher scores indicating better function).12,13,14
Patients were assessed for study events by their treating surgeon at 2 and 6 weeks, 3, 6, and 9 months, and 1 year postoperatively. The functional assessments were completed before surgery and at the 1-year follow-up visit. The blinded Central Adjudication Committee adjudicated all primary and key secondary outcome events identified during the 1-year study follow-up as well as all instances when eligibility was in doubt.
Statistical Analysis
The justification for the PARITY trial sample size has been previously published.10,15 At the trial’s onset, we calculated that the definitive sample size would require a total of 920 patients based on a between-group comparison of deep prosthetic infection. The sample size was calculated as a noninferiority trial under the assumption of an overall 10% event rate with an absolute difference of 5% in the risk of deep surgical site infection within 1 year to define noninferiority. After initiating enrollment and then transitioning from the vanguard to the definitive phase of the trial, we expanded the trial’s primary outcome from deep to any surgical site infection and changed the study’s design to a superiority trial to increase the expected event rate and feasibility without compromising clinical importance. The expanded definition of the primary outcome resulted in an overall vanguard phase event rate of 14%.16 Therefore, with a presumed 50% or greater reduction in the relative risk of deep surgical site infection within 1 year and with a 2-sided α of .05 and study power of 80%, we planned the definitive trial’s sample size to include 300 patients per arm, for a total of 600 patients.
When conducting the final analyses, we adhered to the published statistical analysis plan.15 Briefly, for the primary analysis, we used a Cox proportional hazards regression model with time from surgery to the surgical site infection as the primary outcome. The analysis included all patients in the groups to which they were randomly allocated. Postoperative antibiotic duration (treatment group) was the independent variable, and the Cox proportional hazards regression included tumor location and clinical site as stratification variables. Patients who did not experience the primary outcome were censored at 1 year or at the time of last study visit. We tested the proportional hazards assumption of the Cox proportional hazards regression model by examining Schoenfeld residuals. We also performed several sensitivity analyses for the primary outcome, including a competing risks analysis that accounted for deaths and amputation as competing risks. We identified the following 5 subgroups a priori, which we analyzed in the primary model to assess for possible effect modification: tumor type, tumor location, sex, age, and preoperative chemotherapy.
We assessed the effect of postoperative antibiotic duration on the secondary outcomes using Cox proportional hazards regressions with treatment group as the independent variable and tumor location and clinical site as stratification variables. We also estimated the effect of postoperative antibiotic duration on functional outcomes at 1 year using multiple linear regression models that included treatment group, tumor location, clinical site, and baseline score as independent variables. We used multiple imputation to address missing functional outcome data.
The results are presented as hazard ratios (HRs) for time-to-event outcomes and mean difference for continuous outcomes, with corresponding 95% CIs and associated 2-sided P values. No adjustments were made for multiple testing. Kaplan-Meier curves were constructed for the primary outcome. These analyses were first completed using blinded treatment groups by the data analyst (D.H.-A.). Interpretations for the effect of antibiotic duration were developed and documented based on blinded group A vs B. The randomization code was then broken, the correct a priori interpretation selected, and the manuscript drafted. All analyses were conducted using SAS software, version 9.4 (SAS Institute Inc).
Results
Study Patients
Of the 604 patients included in the final analysis (mean [SD] age, 41.2 [21.9] years; 361 [59.8%] male; 114 [18.9%] Asian, 43 [7.1%] Black, 34 [5.6%] Hispanic, 15 [2.5%] Indigenous, 384 [63.8%] White, and 12 [2.0%] other [3 Middle Eastern, 5 mixed race, 2 North African, 1 Polynesian, and 1 Turkish]), 293 were randomized to a 5-day regimen and 311 to a 1-day regimen. Of the 527 patients alive at 1 year, 496 (94%) had 1-year follow-up data available. Figure 1 and the eAppendix (Section 5.0) and eTables 1 and 2 in Supplement 2 provide details regarding patient flow and the reasons for exclusion.
Figure 1. Patient Flow Diagram.
MRSA indicates methicillin-resistant Staphylococcus aureus; VRE, vancomycin-resistant Enterococcus.
Table 1 and eTables 3 to 5 in Supplement 2 present patient characteristics and demonstrate similar characteristics in the 2 groups. The most common tumor type was a primary bone tumor located predominantly in the femur. A total of 290 patients (48.0%) received preoperative chemotherapy; 22 (3.6%) received preoperative radiotherapy. There was an imbalance between treatment groups, with 129 of 293 patients (44.0%) allocated to the 5-day regimen having received preoperative chemotherapy compared with 161 of 311 patients (51.8%) allocated to the 1-day regimen.
Table 1. Baseline Characteristics of the Study Patientsa.
| Characteristic | 5-d Regimen (n = 293) | 1-d Regimen (n = 311) | Total (n = 604) |
|---|---|---|---|
| Patient demographic characteristics and tumor details | |||
| Age, mean (SD), y | 42.6 (21.7) | 39.9 (22.0) | 41.2 (21.9) |
| Sex | |||
| Male | 178 (60.8) | 183 (58.8) | 361 (59.8) |
| Female | 115 (39.2) | 128 (41.2) | 243 (40.2) |
| Race and ethnicity | |||
| Asian | 54 (18.4) | 60 (19.4) | 114 (18.9) |
| Black | 21 (7.2) | 22 (7.1) | 43 (7.1) |
| Hispanic | 14 (4.8) | 20 (6.5) | 34 (5.6) |
| Indigenous | 4 (1.4) | 11 (3.6) | 15 (2.5) |
| White | 194 (66.2) | 190 (61.5) | 384 (63.8) |
| Otherb | 6 (2.0) | 6 (1.9) | 12 (2.0) |
| Unknown | 0 | 2 | 2 |
| Systemic metastases | |||
| No | 244 (83.3) | 255 (82.0) | 499 (82.6) |
| Yes | 49 (16.7) | 56 (18.0) | 105 (17.4) |
| Other cancer treatment modalities | |||
| No | 157 (53.6) | 138 (44.4) | 295 (48.8) |
| Yes | 136 (46.4) | 173 (55.6) | 309 (51.2) |
| Preoperative chemotherapy | 129 (44.0) | 161 (51.8) | 290 (48.0) |
| Preoperative radiation | 10 (3.4) | 12 (3.9) | 22 (3.6) |
| Other | 7 (2.4) | 7 (2.3) | 14 (2.3) |
| Location of tumor | |||
| Tibia | 53 (18.1) | 55 (17.7) | 108 (17.9) |
| Femur | 240 (81.9) | 256 (82.3) | 496 (82.1) |
| Type of tumor | |||
| Bone tumor | 237 (80.9) | 249 (80.1) | 486 (80.5) |
| Soft tissue sarcoma | 28 (9.6) | 34 (10.9) | 62 (10.3) |
| Oligometastatic bone disease | 28 (9.6) | 28 (9.0) | 56 (9.3) |
| Neutropenia at time of surgeryc | |||
| No. of patients | 275 | 286 | 561 |
| No | 231 (84.0) | 234 (81.8) | 465 (82.9) |
| Yes | 44 (16.0) | 52 (18.2) | 96 (17.1) |
| Surgical and perioperative management details | |||
| Length of procedure, median (Q1-Q3), min | 270 (206-377) | 270 (200-377) | 270 (205-377) |
| Antibiotic or silver-coated prosthesis | |||
| No. of patients | 292 | 311 | 603 |
| No | 276 (94.5) | 295 (94.9) | 571 (94.7) |
| Yes | 16 (5.5) | 16 (5.1) | 32 (5.3) |
| Antibiotic | 6 (2.1) | 6 (1.9) | 12 (2.0) |
| Silver-coated prosthesis | 10 (3.4) | 10 (3.2) | 20 (3.3) |
| Suction drain used | |||
| No. of patients | 293 | 310 | 603 |
| No | 63 (21.5) | 74 (23.9) | 137 (22.7) |
| Yes | 230 (78.5) | 236 (76.1) | 466 (77.3) |
Abbreviation: Q1-Q3, quartile 1 to quartile 3.
Data are presented as number (percentage) of patients unless otherwise indicated.
Other ethnicity includes Middle Eastern (n = 3), mixed race (n = 5), North African (n = 2), Polynesian (n = 1), and Turkish (n = 1).
Absolute neutrophil count of 1500/μL or less (to convert to ×109/L, multiply by 0.001).
Adherence to the Allocated Intervention
Two patients (0.6%) who had originally been allocated to a 1-day regimen received a 5-day regimen; no patients originally allocated to a 5-day regimen crossed over to a 1-day regimen. Protocol deviations primarily resulted from inpatient hospital discharge earlier than 5 days postoperatively and were similar between groups. Of those allocated to the 5-day regimen, 248 patients (84.6%) received all but the final 3 doses of intravenous infusions as did 256 patients (82.6%) allocated to the 1-day regimen. eTable 6 in Supplement 2 provides details regarding the administration of the antibiotics.
Primary Outcome
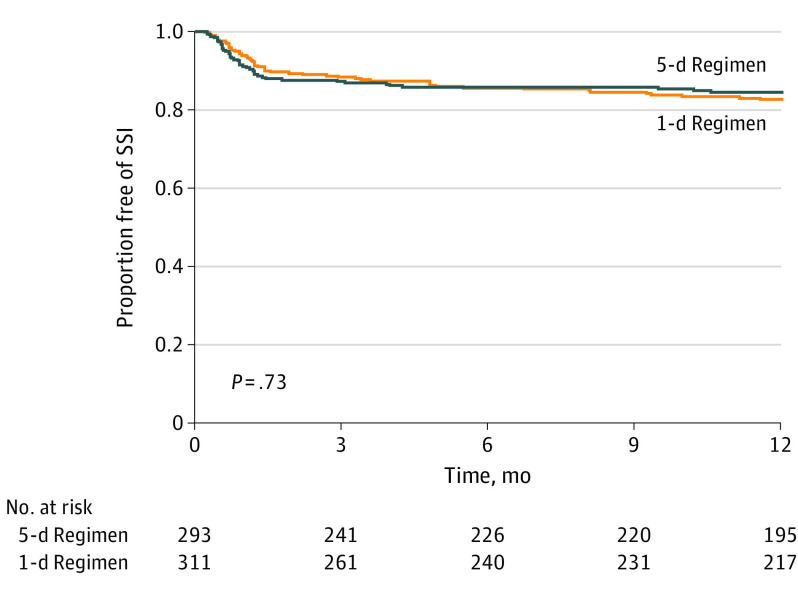
A surgical site infection occurred within 1 year in 44 of 293 patients (15.0%) allocated to the 5-day regimen and in 52 of 311 patients (16.7%) allocated to the 1-day regimen (HR, 0.93; 95% CI, 0.62-1.40; P = .73) (Figure 2 and Table 2). The Schoenfeld residuals demonstrate that the assumption of proportional hazards for the primary outcome was not violated. Table 2 presents the incidence of superficial incisional, deep incisional, and organ space surgical site infections for each group. The most common causative organisms of surgical site infections were S aureus and coagulase-negative staphylococci.
Figure 2. Kaplan-Meier Estimates of the Duration of Primary Outcome-Free Survival at the Time of Final Assessment.
SSI indicates surgical site infection.
Table 2. Study Outcomes by Treatment Group (Primary and Secondary).
| Study end point | 5-d Regimen (n = 293) | 1-d Regimen (n = 311) | HR (95% CI) | P value |
|---|---|---|---|---|
| Primary outcome | ||||
| Any surgical site infection | 44 (15.0) | 52 (16.7) | 0.93 (0.62-1.40) | .73 |
| Superficial incisional | 13 (4.4) | 12 (3.9) | NR | NR |
| Deep incisional | 3 (1.0) | 8 (2.6) | NR | NR |
| Organ or space | 28 (9.6) | 34 (10.9) | 0.97 (0.59-1.62) | .92 |
| Secondary outcomes | ||||
| Any antibiotic-related complications | 15 (5.1) | 5 (1.6) | 3.24 (1.17-8.98) | .02 |
| Clostridioides difficile–associated colitis | 11 (3.8) | 4 (1.3) | NR | NR |
| Opportunistic fungal infection | 0 | 1 (0.3) | NR | NR |
| Oral candidiasis | 1 (0.3) | 0 | NR | NR |
| Diarrhea (unrelated to C difficile) that required intervention | 3 (1.0) | 0 | NR | NR |
| Any unplanned additional operation | 75 (25.6) | 80 (25.7) | 1.06 (0.77-1.46) | .72 |
| Any oncologic events | 85 (29.0) | 89 (28.6) | 1.02 (0.75-1.39) | .90 |
| Local recurrence | 15 (5.1) | 22 (7.1) | 0.78 (0.40-1.51) | .46 |
| Distant metastases | 69 (23.5) | 79 (25.4) | 0.90 (0.65-1.25) | .53 |
| Other oncologic event | 7 (2.4) | 8 (2.6) | NR | NR |
| All-cause mortality | 37 (12.6) | 40 (12.9) | 1.01 (0.64-1.58) | .98 |
| Death from disease progression | 29 (9.9) | 29 (9.3) | 1.08 (0.64-1.81) | .78 |
Abbreviations: HR, hazard ratio; NR, not reported (these study end points did not meet the threshold set in the Statistical Analysis Plan for the minimum number of events required to conduct a statistical comparison).
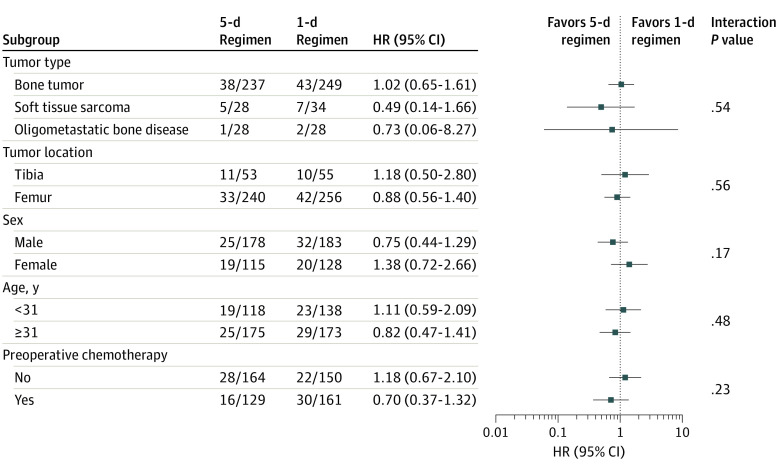
The results were similar in the sensitivity analyses that accounted for deaths and amputation as competing risks. Adjusted analyses yielded similar results to those in the primary analysis. Subgroup analyses did not show any effect modification, including when adjusted for preoperative chemotherapy. Figure 3 and eTables 7 and 8 in Supplement 2 provide details regarding the sensitivity and subgroup analyses.
Figure 3. Forest Plot for Subgroup Analyses.
HR indicates hazard ratio.
Secondary Outcomes
Antibiotic-Related Complications, Unplanned Additional Operations, Oncologic Events, and Mortality
Study-related antibiotic-related complications occurred in 15 patients (5.1%) allocated to the 5-day regimen and in 5 patients (1.6%) allocated to the 1-day regimen (HR, 3.24; 95% CI, 1.17-8.98; P = .02) (Table 2). The most common antibiotic-related complication was Clostridioides difficile–associated colitis (Table 2). Unplanned additional operations occurred in 75 patients (25.6%) allocated to the 5-day regimen and in 80 patients (25.7%) allocated to the 1-day regimen (HR, 1.06; 95% CI, 0.77-1.46) (eTable 9 in Supplement 2). The most common types of additional operations were irrigation and debridement and implant exchange, most of which were to treat a deep incisional or organ space surgical site infection. Oncologic events (HR, 1.02; 95% CI, 0.75-1.39) and mortality (HR, 1.01; 95% CI, 0.64-1.58) proved similar between the treatment groups (Table 2 and eTable 9 in Supplement 2).
Functional Outcomes
Surgeon-reported function was similar between the treatment groups as measured by the MSTS-87 scores (mean difference, −0.49; P = .41) and MSTS-93 scores (mean difference, −1.89; P = .34) as was patient-reported function between the 2 groups as measured by the TESS (mean difference, 0.10; P = .96) (eTable 10 in Supplement 2).
Discussion
The PARITY randomized clinical trial failed to demonstrate a benefit of a 5-day prophylactic antibiotic regimen of intravenous cephalosporins compared with a 1-day regimen in reducing surgical site infections after surgical resection and endoprosthetic reconstruction for a lower extremity bone tumor. However, 3 times as many patients allocated to the 5-day regimen experienced serious antibiotic-related complications.
Our overall primary event rate is higher than previously published studies in the field.5,17 In a meta-analysis5 of retrospective data, the surgical site infection rate after lower extremity endoprosthetic reconstruction was 10% (95% CI, 8%-11%). This meta-analysis5 suggested that antibiotic prophylaxis for longer than 24 hours postoperatively decreases the risk of infection, but the biases of observational research leave only low-quality evidence. Our event rate may be higher than previously reported because of our broader definition of a surgical site infection and the careful prospective collection of study event data.
Perioperative antibiotic prophylaxis is considered essential in minimizing surgical site infections in total joint arthroplasty, in which the infection rate is much lower.18,19,20,21,22 A meta-analysis23 of randomized clinical trials that compared only preoperative antibiotics with both preoperative and postoperative antibiotics in joint replacement surgery did not show efficacy of postoperative antibiotic prophylaxis. Because there is no evidence of additional benefit to a lengthened course, the Surgical Infection Prevention Project recommends the discontinuation of use of prophylactic antibiotics 24 hours postoperatively for all surgical cases.24 However, lower limb oncologic reconstructions are unique in their complexity and the immunocompromised state of the affected patient population; therefore, these recommendations may not be applicable in this particular setting. The second International Consensus Meeting on Musculoskeletal Infection recently identified whether prolonging use of postoperative antibiotics would prevent surgical site infections in patients with bone tumors undergoing endoprosthetic reconstruction as 1 of the most critical orthopedic oncology clinical questions.25 Their recommendation acknowledged that although more than half of orthopedic oncologists prescribe prophylactic antibiotics for longer than 24 hours postoperatively, there is insufficient evidence to support this practice.25
The overuse of antibiotics is a major public health concern associated with increased health care costs from antibiotic-related complications and antibiotic resistance.26 The increase in antibiotic-resistant organisms, particularly in a nosocomial setting, is outpacing the development of new antimicrobial agents. Antibiotic use often results in antibiotic-associated diarrhea, not infrequently caused by C difficile. Although antibiotic-associated diarrhea is generally mild and self-limiting, gut infection with C difficile is universally severe and may lead to toxic megacolon, organ failure, or even death.27 Our study found a significant increase in antibiotic-related complications in the 5-day regimen group, with most complications reported to be C difficile–associated colitis. To avoid this complication, hospital antibiotic stewardship programs in the UK have restricted the use of high-risk antibiotics, including cephalosporins, with a subsequent clear reduction of nosocomial C difficile infections.28,29,30
Strengths and Limitations
Our trial has several strengths. Safeguards against potential bias included concealed randomization and blinding of treatment allocation from patients, caregivers, outcomes assessors, and data analysts. The diagnosis of surgical site infection was independently adjudicated using well-established definitions, thus ensuring objective decision-making and minimizing outcome assessment bias. By documenting our interpretations based on blinded results before breaking the randomization code, we safeguarded against interpretation bias.31 After accounting for the nearly 10% mortality rate, true loss to follow-up was only 5%. Close clinical surveillance and rigorous study monitoring procedures resulted in this relatively small loss to follow-up. Our study’s broad eligibility criteria and conduct in many health care systems strengthens its generalizability. Several of the study outcomes are of unequivocal importance to both patients and health care systems. Finally, answering clinical questions in rare conditions requires an immense international, collaborative effort. To our knowledge, this trial was the first-ever collaborative, interventional trial initiated and led by orthopedic oncologists.
Our trial also has limitations. The large number of participating clinical sites, combined with the rarity of bone tumors, resulted in low enrollment at some sites. More patients in the shorter duration group received preoperative chemotherapy, which may have increased their risk of a surgical site infection. However, our subgroup and adjusted analyses yielded results similar to our primary analysis. Protocol deviations, particularly doses not administered because of early hospital discharge, were not uncommon. Although the deviations were balanced between groups, they would have affected the 5-day regimen group more than the 1-day regimen. However, the discontinuation of antibiotics at hospital discharge is standard procedure; thus, our results are applicable to actual clinical practice. The impact of the postoperative prophylactic antibiotic regimens on late infections that present after the 1-year postsurgery timepoint cannot be inferred from this study; however, these infections are not considered surgical site infections according to the definitions established by the Centers for Disease Control and Prevention. The diagnosis of a surgical site infection is challenging because of the complexities of surgery and wound healing, a concern ameliorated by the rigor and blinding of the adjudication process. Finally, the lack of a statistically significant difference observed may be the result of insufficient study power. However, the observed absolute difference between the 2 treatment groups was small, and the increased sample size needed to show statistical significance would likely not be considered necessary by surgeons in the field.
Conclusions
In this randomized clinical trial, the 5-day regimen did not reduce the rate of surgical site infection compared with the 1-day regimen. Although the results of this randomized clinical trial do not definitively exclude an important benefit of postoperative prophylactic antibiotic therapy longer than 24 hours, the significantly higher risk of antibiotic-related complications in the 5-day regimen represents a critical finding. Clinicians should consider the uncertainty of the benefits and the relative confidence in findings of harm to make an informed decision on antibiotic duration after surgical resection and endoprosthetic reconstruction for lower extremity bone tumors.
Trial Protocol
eAppendix. Supplemental Methods
eTable 1. Reasons for Exclusion Prior to Randomization
eTable 2. Reasons for Exclusion After Adjudication Committee Review
eTable 3. Patient Demographics and Baseline Details
eTable 4. Tumor Details
eTable 5. Surgical and Perioperative Management Details
eTable 6. Prophylactic Antibiotic Administration Details
eTable 7. Sensitivity Analyses
eTable 8. Subgroup Analyses
eTable 9. Study Outcomes by Treatment Group (Primary and Secondary)
eTable 10. Functional and Quality of Life Outcomes by Treatment Group
Nonauthor Collaborators. The PARITY Investigators
Data Sharing Statement
References
- 1.Jeys L, Grimer R. The long-term risks of infection and amputation with limb salvage surgery using endoprostheses. In: Tunn PU, ed. Treatment of Bone and Soft Tissue Sarcomas: Recent Results in Cancer Research. Springer; 2009:75-84. doi: 10.1007/978-3-540-77960-5_7 [DOI] [PubMed] [Google Scholar]
- 2.Morii T, Yabe H, Morioka H, et al. Postoperative deep infection in tumor endoprosthesis reconstruction around the knee. J Orthop Sci. 2010;15(3):331-339. doi: 10.1007/s00776-010-1467-z [DOI] [PubMed] [Google Scholar]
- 3.Jeys LM, Grimer RJ, Carter SR, Tillman RM. Risk of amputation following limb salvage surgery with endoprosthetic replacement, in a consecutive series of 1261 patients. Int Orthop. 2003;27(3):160-163. doi: 10.1007/s00264-003-0429-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Akahane T, Shimizu T, Isobe K, Yoshimura Y, Fujioka F, Kato H. Evaluation of postoperative general quality of life for patients with osteosarcoma around the knee joint. J Pediatr Orthop B. 2007;16(4):269-272. doi: 10.1097/BPB.0b013e3280925670 [DOI] [PubMed] [Google Scholar]
- 5.Racano A, Pazionis T, Farrokhyar F, Deheshi B, Ghert M. High infection rate outcomes in long-bone tumor surgery with endoprosthetic reconstruction in adults: a systematic review. Clin Orthop Relat Res. 2013;471(6):2017-2027. doi: 10.1007/s11999-013-2842-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hasan K, Racano A, Deheshi B, et al. Prophylactic Antibiotic Regimens in Tumor Surgery (PARITY) survey. BMC Musculoskelet Disord. 2012;13:91. doi: 10.1186/1471-2474-13-91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bratzler DW, Dellinger EP, Olsen KM, et al. ; American Society of Health-System Pharmacists; Infectious Disease Society of America; Surgical Infection Society; Society for Healthcare Epidemiology of America . Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am J Health Syst Pharm. 2013;70(3):195-283. doi: 10.2146/ajhp120568 [DOI] [PubMed] [Google Scholar]
- 8.Parvizi J, Gehrke T, Chen AF. Proceedings of the International Consensus on Periprosthetic Joint Infection. Bone Joint J. 2013;95-B(11):1450-1452. doi: 10.1302/0301-620X.95B11.33135 [DOI] [PubMed] [Google Scholar]
- 9.Costelloe C, Metcalfe C, Lovering A, Mant D, Hay AD. Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: systematic review and meta-analysis. BMJ. 2010;340:c2096. doi: 10.1136/bmj.c2096 [DOI] [PubMed] [Google Scholar]
- 10.Ghert M, Deheshi B, Holt G, et al. ; PARITY Investigators . Prophylactic Antibiotic Regimens in Tumour Surgery (PARITY): protocol for a multicentre randomised controlled study. BMJ Open. 2012;2(6):e002197. doi: 10.1136/bmjopen-2012-002197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG. CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Infect Control Hosp Epidemiol. 1992;13(10):606-608. doi: 10.2307/30148464 [DOI] [PubMed] [Google Scholar]
- 12.Tunn PU, Pomraenke D, Goerling U, Hohenberger P. Functional outcome after endoprosthetic limb-salvage therapy of primary bone tumours: a comparative analysis using the MSTS score, the TESS and the RNL index. Int Orthop. 2008;32(5):619-625. doi: 10.1007/s00264-007-0388-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Davis AM, Wright JG, Williams JI, Bombardier C, Griffin A, Bell RS. Development of a measure of physical function for patients with bone and soft tissue sarcoma. Qual Life Res. 1996;5(5):508-516. doi: 10.1007/BF00540024 [DOI] [PubMed] [Google Scholar]
- 14.Schreiber D, Bell RS, Wunder JS, et al. Evaluating function and health related quality of life in patients treated for extremity soft tissue sarcoma. Qual Life Res. 2006;15(9):1439-1446. doi: 10.1007/s11136-006-0001-4 [DOI] [PubMed] [Google Scholar]
- 15.Schneider P, Heels-Ansdell D, Thabane L, Ghert M; PARITY Investigators . Prophylactic Antibiotic Regimens In Tumor Surgery (PARITY): a multi-center randomized controlled study comparing alternative antibiotic regimens in patients undergoing tumor resections with endoprosthetic replacements-a statistical analysis plan. Trials. 2021;22(1):223. doi: 10.1186/s13063-021-05147-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.PARITY Investigators . Prophylactic Antibiotic Regimens in Tumour Surgery (PARITY): a pilot multicentre randomised controlled trial. Bone Joint Res. 2015;4(9):154-162. doi: 10.1302/2046-3758.49.2000482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Langit MB, Miwa S, Yamamoto N, et al. Risk factors for postoperative deep infection after malignant bone tumor surgery of the extremities. Anticancer Res. 2020;40(6):3551-3557. doi: 10.21873/anticanres.14344 [DOI] [PubMed] [Google Scholar]
- 18.Illingworth KD, Mihalko WM, Parvizi J, et al. How to minimize infection and thereby maximize patient outcomes in total joint arthroplasty: a multicenter approach: AAOS exhibit selection. J Bone Joint Surg Am. 2013;95(8):e50. doi: 10.2106/JBJS.L.00596 [DOI] [PubMed] [Google Scholar]
- 19.Voigt J, Mosier M, Darouiche R. Systematic review and meta-analysis of randomized controlled trials of antibiotics and antiseptics for preventing infection in people receiving primary total hip and knee prostheses. Antimicrob Agents Chemother. 2015;59(11):6696-6707. doi: 10.1128/AAC.01331-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.AAOS. Information statement: recommendations for the use of intravenous antibiotic prophylaxis in primary total joint arthroplasty. Accessed June 4, 2021. https://www.aaos.org/globalassets/about/bylaws-library/information-statements/1027-recommendations-for-the-use-of-intravenous-antibiotic-prophylaxis-in-primary-total-joint-arthroplasy.pdf
- 21.British Orthopaedic Association. Primary total hip replacement: a guide to good practice. Accessed June 4, 2021. https://britishhipsociety.com/wp-content/uploads/2020/12/2012-Nov_BOA-Blue-Book.pdf
- 22.New Zealand Orthopaedic Association. Total hip joint arthroplasty good practice guidelines. Accessed June 4, 2021. https://nzoa.org.nz/sites/default/files/Total_Hip_Joint_Arthroplasty_Guidelines_0.pdf
- 23.Thornley P, Evaniew N, Riediger M, Winemaker M, Bhandari M, Ghert M. Postoperative antibiotic prophylaxis in total hip and knee arthroplasty: a systematic review and meta-analysis of randomized controlled trials. CMAJ Open. 2015;3(3):E338-E343. doi: 10.9778/cmajo.20150012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rosenberger LH, Politano AD, Sawyer RG. The surgical care improvement project and prevention of post-operative infection, including surgical site infection. Surg Infect (Larchmt). 2011;12(3):163-168. doi: 10.1089/sur.2010.083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Strony J, Brown S, Choong P, Ghert M, Jeys L, O’Donnell RJ. Musculoskeletal infection in orthopaedic oncology: assessment of the 2018 International Consensus Meeting on Musculoskeletal Infection. J Bone Joint Surg Am. 2019;101(20):e107. doi: 10.2106/JBJS.19.00182 [DOI] [PubMed] [Google Scholar]
- 26.Infectious Diseases Society of America (IDSA) . Combating antimicrobial resistance: policy recommendations to save lives. Clin Infect Dis. 2011;52(suppl 5):S397-S428. doi: 10.1093/cid/cir153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mullish BH, Williams HR. Clostridium difficile infection and antibiotic-associated diarrhoea. Clin Med (Lond). 2018;18(3):237-241. doi: 10.7861/clinmedicine.18-3-237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Aldeyab MA, Kearney MP, Scott MG, et al. An evaluation of the impact of antibiotic stewardship on reducing the use of high-risk antibiotics and its effect on the incidence of Clostridium difficile infection in hospital settings. J Antimicrob Chemother. 2012;67(12):2988-2996. doi: 10.1093/jac/dks330 [DOI] [PubMed] [Google Scholar]
- 29.Talpaert MJ, Gopal Rao G, Cooper BS, Wade P. Impact of guidelines and enhanced antibiotic stewardship on reducing broad-spectrum antibiotic usage and its effect on incidence of Clostridium difficile infection. J Antimicrob Chemother. 2011;66(9):2168-2174. doi: 10.1093/jac/dkr253 [DOI] [PubMed] [Google Scholar]
- 30.Al-Obaydi W, Smith CD, Foguet P. Changing prophylactic antibiotic protocol for reducing Clostridium difficile-associated diarrhoeal infections. J Orthop Surg (Hong Kong). 2010;18(3):320-323. doi: 10.1177/230949901001800312 [DOI] [PubMed] [Google Scholar]
- 31.Järvinen TLN, Sihvonen R, Bhandari M, et al. Blinded interpretation of study results can feasibly and effectively diminish interpretation bias. J Clin Epidemiol. 2014;67(7):769-772. doi: 10.1016/j.jclinepi.2013.11.011 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol
eAppendix. Supplemental Methods
eTable 1. Reasons for Exclusion Prior to Randomization
eTable 2. Reasons for Exclusion After Adjudication Committee Review
eTable 3. Patient Demographics and Baseline Details
eTable 4. Tumor Details
eTable 5. Surgical and Perioperative Management Details
eTable 6. Prophylactic Antibiotic Administration Details
eTable 7. Sensitivity Analyses
eTable 8. Subgroup Analyses
eTable 9. Study Outcomes by Treatment Group (Primary and Secondary)
eTable 10. Functional and Quality of Life Outcomes by Treatment Group
Nonauthor Collaborators. The PARITY Investigators
Data Sharing Statement